31 January 2024: Clinical Research
Impact of COVID-19 on Academic Burnout among Medical College Students in China: Findings from a Web-Based Survey
Ming Zhang12ABCDEFG, Wei Xu2ABCDFG, Haoran Zhou3ABD, Junjun Fan4ABCFG, Huan LiuDOI: 10.12659/MSM.942317
Med Sci Monit 2024; 30:e942317
Abstract
BACKGROUND: Academic burnout can affect students’ academic behavior and performance and especially damages the careers of medical college students. Medical education systems during the COVID-19 pandemic have met unprecedented challenges that have influenced medical students. This study aimed to explore the effects of psychological resilience, stress, and smartphone addiction on academic burnout among Chinese medical students.
MATERIAL AND METHODS: This study utilized a cross-sectional design, from March 13, 2022 to March 31, 2022, within the Wannan Medical College, where students completed a web-based survey. The Chinese version of the Academic Burnout Scale (ABS), the 10-item Smartphone Addiction Scale-Short Version (SAS-SV), the Connor-Davidson Resilience Scale (CD-RISC 10) and the Perceived Stress Scale (PSS-4) were used in this survey. Data entry and analysis were conducted using IBM SPSS ver. 22.0. Pearson’s correlation coefficient (r) was used to examine the correlations between medical college students’ academic burnout and smartphone addiction and mental health. Binary logistic regression analysis was carried out to evaluate the factors influencing academic burnout.
RESULTS: Of 3190 medical college students who completed the survey, 1521 (47.7%) had some degree of academic burnout. Gender, being a student leader, grades, perceived stress, and smartphone addiction were associated with the total score of academic burnout. Psychological resilience and adapting to online classes were protective factors against academic burnout.
CONCLUSIONS: Academic burnout is common among medical college students in China after the COVID-19 pandemic, and it is urgent to address this situation to improve the quality of medical education.
Keywords: Students, COVID-19, Nursing
Background
More than 2 years since the official announcement from the WHO of the COVID-19 pandemic, the worldwide sanitary crisis is still far from its conclusion. The emergence of SARS-CoV-2 Delta and Omicron variants, currently spreading worldwide, has sparked a new wave of the COVID-19 pandemic [1]. Studies have found that due to the high infection risk, significant lifestyle changes, strict restrictions, and disruptions in educational programs, medical students were highly vulnerable to mental health problems during the COVID-19 pandemic [2], and common psychological problems might contribute to decreased medical learning [3–7]. With the development of the COVID-19 pandemic, academic burnout has become very important in the last 2 years. Academic burnout is a long-term negative emotion oriented toward learning, accompanied by inappropriate learning behaviors and a decreased sense of academic achievement [8]. Academic burnout is also defined as a harmful psychological syndrome [9], which usually refers to a series of negative psychological manifestations (eg, exhaustion, anxiety, depression, and decreased personal accomplishment). Data from systematic reviews and meta-analyses suggested that the incidence of burnout among medical students ranges from 7% to 75% [10–12]. Prevalence varies widely with definitions, measurement methods, and cultural differences [13].
Academic burnout can occur during the learning process, indicating that students are bored with learning and develop attitudes and behaviors that lead to negative learning. Academic burnout has become an important indicator reflecting the mental health of medical college students. Numerous studies have found that academic burnout has severe adverse effects, leading to suboptimal academic ability, poor academic performance, and an increase in dropping out of medical college [8–14]. Previous studies also suggest that medical college students with academic burnout are more likely to be dissatisfied with their academic performance and plan to or have already dropped out [15].
The job demand-resource theory (JD-R) assumes that employee well-being comes from a balance of needs and resources [16]. Basic psychological needs such as competence, relatedness, and autonomy may not be met when work and learning demands exceed available resources [17]. Medical education is a long and challenging process that can damage the physical and mental health of medical college students [18]; they experience more stress than college students with other majors [19] and have a higher prevalence of academic burnout compared with other professional college students [20,21]. However, Yang et al found that non-medical undergraduate students showed higher levels of academic burnout [22]. As the COVID-19 pandemic intensified during the investigation period, Wannan Medical College converted all university courses to online learning, which is challenging for medical college students. Previous studies found that online learning is a challenge for Chinese medical college students, and may make them feel tired and frustrated and have extreme difficulty adjusting to this learning style [23].
The COVID-19 pandemic has had an adverse impact on the mental health of medical students [24], especially increasing their stress [25]. Recent research has shown that online teaching can sometimes lead to disruption of the educational process, resulting in considerable stress for college students [26]. The pressure from these changes in learning patterns has detrimental effects and can increase the risk of academic burnout among medical college students [27]. In addition, for medical college students, the shift to the online teaching of their theoretical courses and suspension of laboratory exercises have led to dramatic changes in the learning process, thereby transforming their learning environment [9]. Chinese students face greater risks of stress in dealing with the COVID-19 outbreak, which has lasted over 4 weeks [28], and causes psychological stress that contributes to the increased risk of academic burnout. A more comprehensive assessment of a wider range of academic burnout among medical students and their risk factors will provide universities, hospitals, and health policymakers with more valuable information to identify at-risk students and implement timely psychological interventions.
Smartphone addiction, also referred to as phone dependence, is defined as the state of excessive use of smartphones by individuals, which can lead to withdrawal symptoms of anxiety and tension when without the smartphone [29]. Studies have found that excessive use of smartphones could lead to health problems such as musculoskeletal pain, vision loss, dizziness, headaches, wrist pain, and neck pain [30]. In addition, excessive use of smartphones could lead to negative learning-related outcomes for students, such as decreased academic performance, symptoms of academic procrastination [31], symptoms of depression and anxiety, poor health, and insomnia [29].
Medical students are at increased risk of academic burnout due to high academic and clinical pressures, coupled with the impact of the COVID-19 pandemic. Properly addressing academic burnout in advance is critical to medical students’ personal and medical education. This study contributes to our understanding of academic burnout among medical students in the context of medical education and provides practical insights for educators. Therefore, we conducted a survey and analysis on the academic burnout status of medical college students after the COVID-19 pandemic with the following purposes: (1) To evaluate the academic burnout status of medical college students in China after the COVID-19 pandemic; (2) To explore the factors influencing academic burnout among medical college students in China; and (3) To explore the correlations between academic burnout with perceived stress, psychological resilience, and smartphone addiction.
Material and Methods
PARTICIPATION AND DESIGN:
A cross-sectional study design was used to describe the status and influencing factors of academic burnout among medical college students after the COVID-19 pandemic. This study strictly followed the Reporting of Enhanced Epidemiological Observational Studies (STROBE) guidelines. This research was conducted on a widely used online questionnaire survey platform (
INSTRUMENTS:
Before the formal survey was conducted, the questionnaire was pre-tested by 40 medical college students. According to the pilot results, the official version of the questionnaire was partially revised.
Through a self-designed literature reviewed questionnaire, we obtained general demographic data of the medical college students, including gender, age, grade, race, being an only child, and whether participants are class cadres.
Academic burnout was measured using the Chinese version of the Academic Burnout Scale (ABS), developed by Lian et al [32]. The 20 items covered 3 domains: dejection (8 items), improper behavior (6 items), and reduced personal accomplishment (6 items). There are 12 forward and 8 reverse questions, the reverse scoring questions were 1, 3, 6, 8, 11, 13, 15, and 18. The respondents rated the items on a scale from 1 to 5. The ABS score ranged from 20 to 100 points, with higher scores indicating greater academic burnout. Subjects with ABS overall scores greater than 60 were considered to have academic burnout. The ABS has been used in previous studies investigating Chinese medical college student academic burnout [33]. The Cronbach’s alpha coefficient for the ABS in this study was 0.887, which demonstrated good reliability.
The 10-item Smartphone Addiction Scale-Short Version (SAS-SV) developed by Kwon in 2013 was used to assess participant smartphone addiction [34]. The SAS-SV questionnaire consists of 10 items with scores ranging from 10 to 60 based on a 6-point Likert scale (1: “strongly disagree” to 6: “strongly agree”), with higher total scores indicating higher levels of smartphone addiction. According to previous similar studies [29], the cutoff value of 31 for females and 33 for males was used to classify smartphone addiction. In this study, the Cronbach’s alpha for the Smartphone Addiction Scale in the study sample was 0.89. This study’s scale showed good internal reliability (Cronbach’s α=0.83).
The Connor-Davidson Resilience Scale (CD-RISC 10) is a 10-item scale that assesses medical college student ‘s mental resilience over the past month [35]. CD-RISC-10 uses a Likert scale with 5 possible responses for each item, ranging from 0 (not true at all) to 4 (true nearly all the time). The 10 items are positively worded, the CD-RISC-10 scores range from 0 to 40, and a higher score indicates greater resilience (cutoff score ≥30). In this study, the Cronbach’s α was 0.878 (Connor-Davidson Resilience Scale [CD-RISC] 10).
The Perceived Stress Scale (PSS-4) [36] is a 4-item questionnaire used to measure a participants’ self-reported level of stress by assessing feelings over the past month. Each item is scored from 0 (not at all) to 4 (nearly every day) with a range of 0 to 16 for the scores of all items. Negative item scores were inversely converted, and a higher level of perceived stress is indicated by higher scores on the PSS-4 scale. The PSS-4 overall value of ≥8 is recommended to indicate a possible diagnosis of higher perceived stress. In this study, the Cronbach’s α was 0.852.
STATISTICAL ANALYSES:
Study data were downloaded from the “Questionnaire Star” as a Microsoft Excel spreadsheet and were stored using encryption and security to protect the participants’ privacy. All statistical analyses were performed using IBM SPSS V.22. Continuous variables were described as mean±standard deviation (SD), and categorical variables were described as frequencies and percentages. The χ2 test was applied to explore the differences in the prevalence of academic burnout. Based on univariate analysis, binary logistic regression analysis was used to identify the potential influencing factors of academic burnout. Pearson’s correlations were used to examine academic burnout, perceived stress, resilience, and smartphone addiction. For all statistical tests, statistical differences were determined using a two-tailed test, and a
Results
PARTICIPANTS’ CHARACTERISTICS:
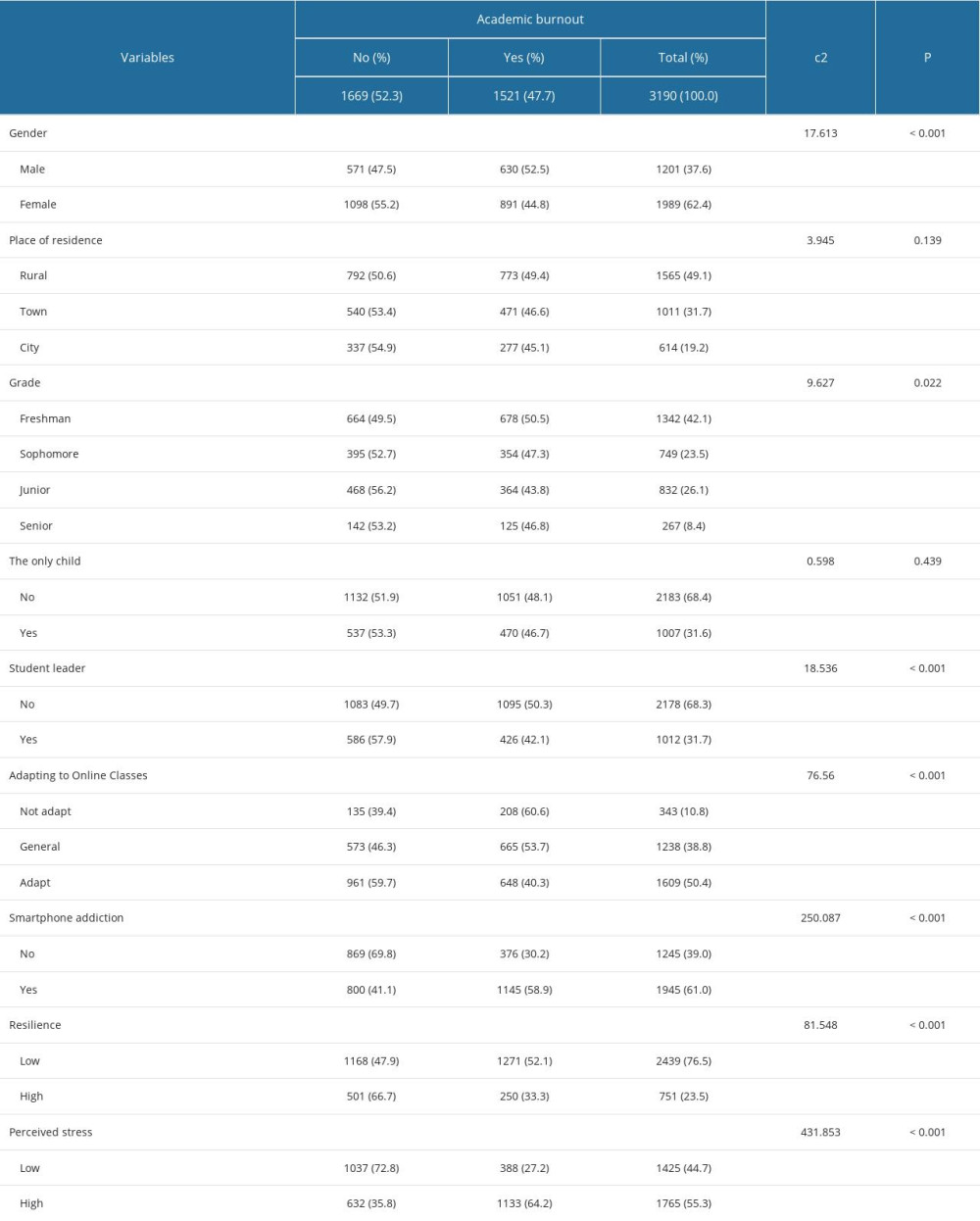
Of the participants, 1989 (62.4%) were women and 1201 men (37.6%). Their ages ranged from 18 to 25, with a mean of 21.6±1.83. 1007 (31.6%). Of the participants, 1007 (31.6) were an only child, 1012 (31.7%) were student leaders, 1565 (49.1%) lived in rural areas, 1011 (31.7%) lived in towns, and 614 (19.2%) lived in cities. The distribution of medical college students in year 1, 2, 3, and 4 was 1342 (42.1%), 749 (23.5%), 832 (26.1%), and 267 (8.4%), respectively. The socio-demographic characteristics of the medical college students are represented in Table 1.
RELATIONSHIP BETWEEN ACADEMIC BURNOUT AND OTHER VARIABLES:
In this research, 1521 (47.7%) of all the medical college students had a certain degree of academic burnout. A statistically significant difference between those with or without academic burnout was found in the variability of gender, grade, student leader or not, adapting to online classes, smartphone addiction, resilience, and perceived stress, with a
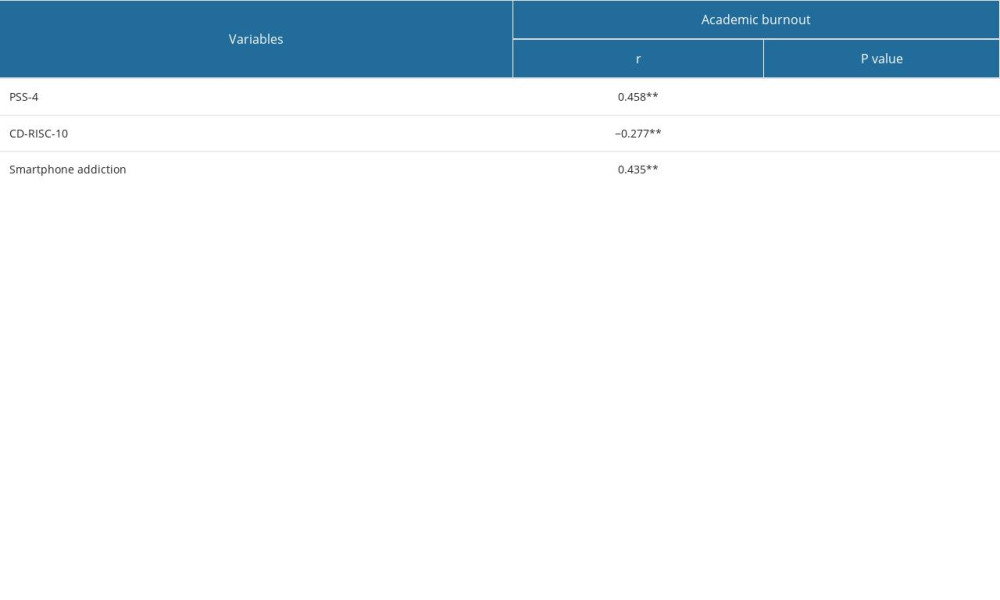
CORRELATIONS OF THE INVESTIGATED VARIABLES:
The inter-correlations of the study’s variables are illustrated in Table 2. All the investigated variables were significantly associated. ABS overall scores were strongly and positively correlated with PSS-4 (P<0.001; r=0.458), and smartphone addiction scores (P<0.001; r=0.435). Academic burnout was negatively correlated with resilience (P<0.01; r=−0.277).
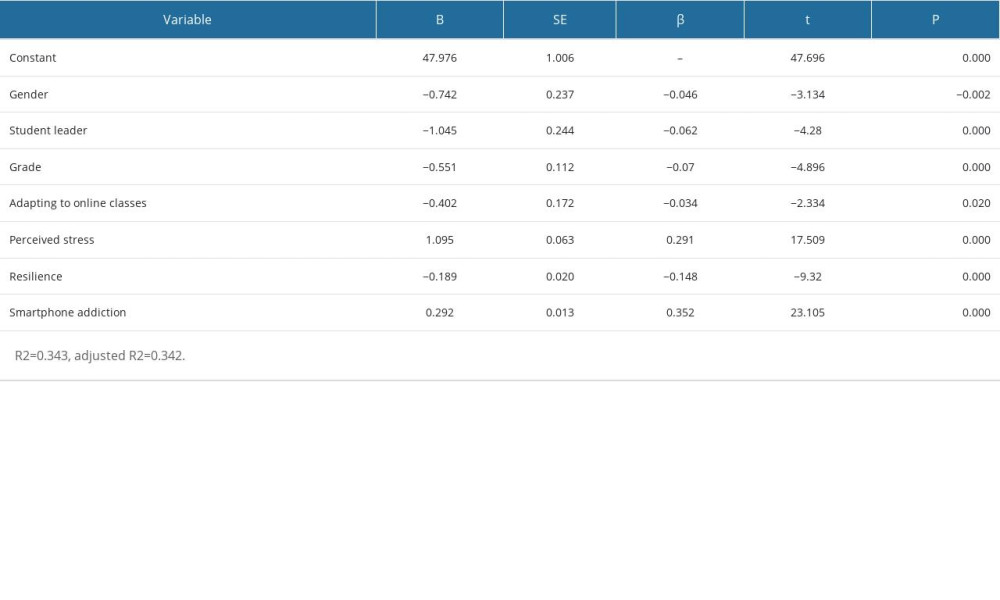
FACTORS ASSOCIATED WITH ACADEMIC BURNOUT:
The binary logistic regression analysis outcomes indicated that gender, being a student leader, year in college, perceived stress, and smartphone addiction were associated with the total academic burnout score. Psychological resilience and adapting to online classes were protective factors for academic burnout. As show in Table 3, the model could explain 34.3% (adjusted R2 scores: 34.2%) of the variance of Chinese medical students’ academic burnout scores.
Discussion
ANALYSIS OF INFLUENCING FACTORS OF ACADEMIC BURNOUT:
In this study, gender was a variable contributing to academic burnout, with male medical college students being more prone to academic burnout. This result is consistent with Hao’s research [46], but contrary to the meta-analysis of Peng et al [39]. The huge changes in study and life brought about by the COVID-19 pandemic have had a great impact on medical students, while the social isolation policy had a greater impact on males who are more energetic. The self-determination theory [47] holds that unsatisfied psychological needs will cause psychological stress, increasing academic burnout [48,49]. In addition, male medical college students generally have more academic responsibilities and employment pressures than female medical college students, which can lead to academic burnout.
This study found that medical college student class leaders had less academic burnout than non-class leader student, which was in line with the results of previous research [50]. This result has some unique Chinese educational cultural background characteristics associated with it. Student leaders are relatively good academically, perform well in college, and serve as role models for other medical college students. Student leaders typically set higher learning requirements and standards and are less likely to experience academic burnout behaviors [46]. Student leaders, as role models, continue to influence student motivation and enthusiasm for learning. It is beneficial for medical college students to enhance their professional identity to set a positive example.
Moreover, first-and second-year medical college students showed higher academic burnout levels than third- and fourth-year medical college students. The possible reason may be that first-and second-year medical college students are less experienced in online learning, and were more susceptible to university academic pressure as compared to the third- and fourth-year medical college students who are accustomed to a rich online learning experience and are also well-adapted and well-adjusted to academic stress. Furthermore, medical college students in the first and second year may not be accustomed to college learning and examination styles, which are dramatically different from high school. Therefore, they must constantly refine their learning objectives and plans and spend more time studying after class.
To our knowledge, no previous research has yet explored the association between academic burnout and adapting to online classes among medical college students. We also found that online course adaptation was negatively associated with academic burnout. During the COVID-19 pandemic, many districts and schools adopted lockdown policies, forcing students to learn through online learning. Some studies have reported that due to the lack of teacher-student interaction in some networks, students were prone to a lack of enthusiasm for online course learning [23], resulting in inappropriate behaviors such as playing on smartphones and dozing off, causing them to struggle with online learning, thus leading to academic burnout. Research has also shown that among medical college students and nursing students, stress from online learning was their top stressor during the COVID-19 pandemic [51]. With increasing online class adaptation, individuals are more likely to not worry about their academic performance, which may subsequently reduce their academic burnout status. The literature has shown that promoting medical college student academic engagement in online learning is essential [23]. Therefore, it is vital to enhance medical college students’ adaptation to online classes to reduce academic burnout and actively adopt coping strategies to improve higher medical education practice.
CORRELATIONS BETWEEN ACADEMIC BURNOUT AND PERCEIVED STRESS:
Our results show that perceived stress is a significant positive predictor of academic burnout, which is consistent with previous research findings [52]. According to general strain theory, stress is a major factor contributing to individual behavior problems [53]. We know that student stress causes depersonalization and reduces empathy [54,55]. Medical college students’ high degree of attention during the COVID-19 pandemic caused them to bear a huge stress burden, producing negative psychological emotions such as psychological fear and anxiety [56], which caused their low enthusiasm for learning, and finally led to academic burnout. The COVID-19 pandemic and its accompanying uncertainties have significantly impacted both medical education and medical students, further exacerbating medical student stress. These stressors associated with the COVID-19 pandemic have increased the stress on medical college students’ personal and academic life, but the underlying mechanisms require further research.
THE CORRELATIONS BETWEEN ACADEMIC BURNOUT AND PSYCHOLOGICAL RESILIENCE:
As expected, our study found a negative correlation between psychological resilience and academic burnout, consistent with previous research findings [57]. Research has shown that college students with high psychological resilience are more likely to perceive their learning environment as satisfying [58], while medical college students with low psychological resilience are more likely to exhibit unsatisfactory behavior in school. Psychological resilience can be used as an important resource for medical college students to cope with various kinds of stress, and can also help them effectively cope with stress and relieve negative emotions, such as anxiety and depression. Psychological resilience has been shown to protect against the high frequency of stress during the COVID-19 pandemic [59]. The acquired characteristics of psychological resilience may influence the prevalence of academic burnout in medical college students after a stressful COVID-19 event. Previous research suggests that systematic interventions can improve psychological resilience [60]. Therefore, educators should emphasize psychological resilience and foster vigorous development in their students to reduce their academic burnout.
CORRELATIONS BETWEEN ACADEMIC BURNOUT AND SMARTPHONE ADDICTION:
In our study, smartphone addiction was significantly associated with academic burnout, which was consistent with the findings of Zhang [20]. Smartphone addiction is a form of behavioral addiction that leads to decreased productivity, denial of negative effects, preoccupation, feelings of annoyance, and even extreme panic if the smartphone is lost [61]. During the COVID-19 pandemic, medical students’ smartphone addiction detection rate was high [62], and was associated with depression, anxiety, and poor sleep quality [63]. When medical college students become addicted to smartphones and spend many hours using them, it can affect their academic performance and can cause stress and academic burnout. Currently, common and effective treatments for smartphone addiction are psychological interventions such as cognitive behavioral therapy [64] and exercise interventions such as running, basketball, and cycling [65]. From the student development perspective, Chinese authorities should encourage companies to design an anti-addiction system limiting smartphone time. Furthermore, school administrators and teachers should actively guide students to use smartphones scientifically and reasonably. This study extends previous research findings regarding academic burnout.
Academic burnout can disrupt medical students’ daily learning and harm their physical and mental health and career development. Future research should apply longitudinal or experimental designs to validate causal relationships among the observed variables. In addition, schools and teachers should adopt various measures to reduce medical students’ academic burnout and alleviate medical students’ learning pressure and dependence on smartphones.
The limitations of this study are as follows. First, all medical college students in this study were from one medical college, so caution should be exercised when generalizing the results to all medical college students in China. Second, all information was based on self-reported symptoms of medical college students; therefore, could not reveal the real emotions they have suffered. Third, the cross-sectional study design used in this study cannot demonstrate a causal relationship between medical college students’ academic burnout and each influencing factor. Future research should explore other factors that influence academic burnout and potential interactions or moderating effects among factors.
Conclusions
The Chinese medical college students we studied experienced high levels of academic burnout during the COVID-19 pandemic. The results revealed significant effects that gender, student leadership, grades, adapting to online classes, perception of stress, resilience, and smartphone addiction have on academic burnout. Considering the negative impact on academic burnout on medical college students, administrators and teachers should pay more attention to the factors affecting their academic burnout to adopt corresponding strategies to reduce academic burnout and improve the quality of learning.
References
1. Wang C, Han J, Will the COVID-19 pandemic end with the Delta and Omicron variants?: Environ Chem Lett, 2022; 20(4); 2215-25
2. Eleftheriou A, Rokou A, Arvaniti A, Sleep quality and mental health of medical students in Greece during the COVID-19 pandemic: Front Public Health, 2021; 9; 775374
3. Deng J, Que J, Wu S, Effects of COVID-19 on career and specialty choices among Chinese medical students: Med Educ Online, 2021; 26(1); 1913785
4. Khalafallah AM, Jimenez AE, Lam S, Burnout among medical students interested in neurosurgery during the COVID-19 era: Clin Neurol Neurosurg, 2021; 210; 106958
5. Peng P, Yang WF, Liu Y, High prevalence and risk factors of dropout intention among Chinese medical postgraduates: Med Educ Online, 2022; 27(1); 2058866
6. Wang Y, Li Y, Jiang J, COVID-19 outbreak-related psychological distress among healthcare trainees: A cross-sectional study in China: BMJ Open, 2020; 10(10); e041671
7. Yang X, Gao L, Zhang S, The professional identity and career attitude of Chinese medical students during the COVID-19 pandemic: A cross-sectional survey in China: Front Psychiatry, 2022; 13; 774467
8. Fitzpatrick O, Biesma R, Conroy RM, Prevalence and relationship between burnout and depression in our future doctors: A cross-sectional study in a cohort of preclinical and clinical medical students in Ireland: BMJ Open, 2019; 9(4); e023297
9. Lian R, Yang LX, Wu LH, The relationship between professional commitment and learning burnout of undergraduates and scales developing: Acta Psychol Sin, 2005; 37(5); 632-36
10. Erschens R, Keifenheim KE, Herrmann-Werner A, Professional burnout among medical students: Systematic literature review and meta-analysis: Med Teach, 2019; 41(2); 172-83
10. Frajerman A, Morvan Y, Krebs M-O, Burnout in medical students before residency: A systematic review and meta-analysis: Eur Psychiatry, 2019; 55; 36-42
12. Low ZX, Yeo KA, Sharma VK, Prevalence of burnout in medical and surgical residents: A meta-analysis: Int J Environ Res Public Health, 2019; 16(9); 1479
13. El Mouedden I, Hellemans C, Anthierens S, Experiences of academic and professional burn-out in medical students and residents during first COVID-19 lockdown in Belgium: A mixed-method survey: BMC Med Educ, 2022; 22(1); 631
14. Dyrbye LN, Thomas MR, Power DV, Burnout and serious thoughts of dropping out of medical school: A multi-institutional study: Acad Med, 2010; 85(1); 94-102
15. Feng D, Zhao W, Shen S, The influence of perceived prejudice on willingness to be a nurse via the mediating effect of satisfaction with major: A cross-sectional study among Chinese male nursing students: Nurse Educ Today, 2016; 42; 69-72
16. Schaufeli WB, Taris TW, A critical review of the job demands-resources model: Implications for improving work and health: Bridging occupational, organizational and public health, 2014; 43-68
17. Demerouti E, Bakker AB, Nachreiner F, The job demands-resources model of burnout: J Appl Psychol, 2001; 86(3); 499-512
18. Qiu Y, Yao M, Guo Y, Health-related quality of life of medical students in a Chinese University: A cross-sectional study: Int J Environ Res Public Health, 2019; 16(24); 5165
19. Worku D, Dirriba AB, Wordofa B, Perceived stress, depression, and associated factors among undergraduate health science students at Arsi University in 2019 in Oromia, Ethiopia: Psychiatry J, 2020; 2020; 4956234
20. Zhang C, Li G, Fan Z, Psychological capital mediates the relationship between problematic smartphone use and learning burnout in Chinese medical undergraduates and postgraduates: A cross-sectional study: Front Psychol, 2021; 12; 600352
21. Zhang CH, Li G, Fan ZY, Mobile phone addiction mediates the relationship between alexithymia and learning burnout in Chinese medical students: A structural equation model analysis: Psychol Res Behav Manag, 2021; 14; 455-65
22. Yang Q, Liu Y, Yang WF, Mental health conditions and academic burnout among medical and non-medical undergraduates during the mitigation of COVID-19 pandemic in China: Environ Sci Pollut Res Int, 2022; 29(38); 57851-59
23. Wang J, Bu L, Li Y, The mediating effect of academic engagement between psychological capital and academic burnout among nursing students during the COVID-19 pandemic: A cross-sectional study: Nurse Educ Today, 2021; 102; 104938
24. Vazquez Morgan M, Promoting student wellness and self-care during COVID 19: The role of institutional wellness: Front Psychiatry, 2021; 12; 797355
25. Ghafari R, Mirghafourvand M, Rouhi M, Osouli Tabrizi S, Mental health and its relationship with social support in Iranian students during the COVID-19 pandemic: BMC Psychol, 2021; 9(1); 81
26. Hanani A, Badrasawi M, Zidan S, Effect of cognitive behavioral therapy program on mental health status among medical student in Palestine during COVID pandemic: BMC Psychiatry, 2022; 22(1); 310
27. Sani I, Hamza Y, Chedid Y, Understanding the consequence of COVID-19 on undergraduate medical education: Medical students’ perspective: Ann Med Surg (Lond), 2020; 58; 117-19
28. Han L, Zhan Y, Li W, Associations between the perceived severity of the COVID-19 pandemic, cyberchondria, depression, anxiety, stress, and lockdown experience: Cross-sectional survey study: JMIR Public Health Surveill, 2021; 7(9); e31052
29. Liu H, Zhou Z, Zhu E, Smartphone addiction and its associated factors among freshmen medical students in China: A cross-sectional study: BMC Psychiatry, 2022; 22(1); 308
30. Soni R, Upadhyay R, Jain M, Prevalence of smart phone addiction, sleep quality and associated behaviour problems in adolescents: International Journal of Research in Medical Sciences, 2017; 5(2); 515
31. Mohamed SM, Mostafa MH, Impact of smartphone addiction on depression and self-esteem among nursing students: Nurs Open, 2020; 7(5); 1346-53
32. Lian R, Yang L, Wu L, A study on the professional commitment and learning burnout of undergraduates and their relationship: Psychol Sci, 2006(1); 47-51
33. Hao Z, Jin L, Huang J, Academic burnout and problematic smartphone use during the COVID-19 pandemic: The effects of anxiety and resilience: Front Psychiatry, 2021; 12; 725740
34. Kwon M, Kim DJ, Cho H, The smartphone addiction scale: Development and validation of a short version for adolescents: PLoS One, 2013; 8; e83558
35. Ye Z, Ruan X, Zeng Z, Psychometric properties of 10-item Connor-Davidson Resilience Scale among nursing students: Nurs, 2016; 23(21); 9-13
36. Guo AA, Crum MA, Fowler LA, Assessing the psychological impacts of COVID-19 in undergraduate medical students: Int J Environ Res Public Health, 2021; 18(6); 2952
37. Batista RDS, Santos MSD, Melo EC, Burnout and academic satisfaction of nursing students in traditional and integrated curricula: Rev Esc Enferm USP, 2021; 55; e03713
38. Hao Z, Jin L, Huang J, Stress, academic burnout, smartphone use types and problematic smartphone use: The moderation effects of resilience: J Psychiatr Res, 2022; 150; 324-31
39. Peng P, Hao Y, Liu Y, The prevalence and risk factors of mental problems in medical students during COVID-19 pandemic: A systematic review and meta-analysis: J Affect Disord, 2023; 321; 167-81
40. Lai J, Ma S, Wang Y, Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019: JAMA Netw Open, 2020; 3(3); e203976
41. Zhang J-Y, Shu T, Xiang M, Learning burnout: Evaluating the role of social support in medical students: Front Psychol, 2021; 12; 277
42. Zis P, Artemiadis A, Bargiotas P, Medical studies during the COVID-19 pandemic: The impact of digital learning on medical students’ burnout and mental health: Int J Environ Res Public Health, 2021; 18(1); 349
43. Coenen L, Poel LV, Schoenmakers B, The impact of COVID-19 on the well-being, education and clinical practice of general practice trainees and trainers: A national cross-sectional study: BMC Med Educ, 2022; 22(1); 1-12
44. Bolatov AK, Seisembekov TZ, Askarova AZ, Online-learning due to COVID-19 improved mental health among medical students: Med Sci Educ, 2021; 31(1); 183-92
45. Cao W, Fang Z, Hou G, The psychological impact of the COVID-19 epidemic on college students in China: Psychiatry Res, 2020; 287; 112934
46. Wang M, Guan H, Li Y, Academic burnout and professional self-concept of nursing students: A cross-sectional study: Nurse Educ Today, 2019; 77; 27-31
47. Deci EL, Ryan RM: Intrinsic motivation and self-determination in human behavior, 1985, New York, Plenum Press
48. Andrés S, Lombas , Esteban MN, The confounding role of basic needs satisfaction between self-determined motivation and well-being: Journal of Happiness Studies, 2018; 19(5); 1305-27
49. Novak CJ, Chang EC, Xu J, Basic psychological needs and negative affective conditions in Chinese adolescents: Does coping still matter?: Personality and Individual Differences, 2021; 179; 110889
50. Li Y, Jiang R, Zhang D, The current status of academic burnout and analysis of influential factors in 282 undergarauate nursing students: J Nurs, 2017; 24(02); 57-60
51. Labrague LJ, Resilience as a mediator in the relationship between stress-associated with the COVID-19 pandemic, life satisfaction, and psychological well-being in student nurses: A cross-sectional study: Nurse Educ Pract, 2021; 56; 103182
52. Sveinsdóttir H, Flygenring BG, Svavarsdóttir MH, Predictors of university nursing students burnout at the time of the COVID-19 pandemic: A cross-sectional study: Nurse Educ Today, 2021; 106; 105070
53. Agnew R, Building on the foundation of general strain theory: Specifying the types of strain most likely to lead to crime and delinquency: Journal of Research in Crime & Delinquency, 2001; 38(4); 319-61
54. West CP, Shanafelt TD, Kolars JC, Quality of life, burnout, educational debt, and medical knowledge among internal medicine residents: JAMA, 2011; 306(9); 952-60
55. Bonanno GA, Loss, trauma, and human resilience: Have we underestimated the human capacity to thrive after extremely aversive events?: Am Psychol, 2004; 59(1); 20-28
56. Zhao Y, Zhou Q, Li J, Influence of psychological stress and coping styles in the professional identity of undergraduate nursing students after the outbreak of COVID-19: A cross-sectional study in China: Nurs Open, 2021; 8(6); 3527-37
57. Gong Z, Li C, Jiao X, Does resilience help in reducing burnout symptoms among chinese students? A meta-analysis: Front Psychol, 2021; 12; 707792
58. Romano L, Consiglio P, Angelini G, Between academic resilience and burnout: the moderating role of satisfaction on school context relationships: Eur J Investig Health Psychol Educ, 2021; 11(3); 770-80
59. Zou H, Tao Z, Zhou Y, Perceived stress positively relates to insomnia symptoms: The moderation of resilience in Chinese pregnant women during COVID-19: Front Psychiatry, 2022; 13; 856627
60. Kreitzer MJ, Klatt M, Educational innovations to foster resilience in the health professions: Med Teach, 2017; 39(2); 153-59
61. Al Qudah MF, Albursan IS, Hammad HI, Anxiety about COVID-19 infection, and its relation to smartphone addiction and demographic variables in Middle Eastern countries: Int J Environ Res Public Health, 2021; 18(21); 11016
62. Liu H, Zhou Z, Huang L, Prevalence of smartphone addiction and its effects on subhealth and insomnia: A cross-sectional study among medical students: BMC Psychiatry, 2022; 22(1); 305
63. Alhassan AA, Alqadhib EM, Taha NW, The relationship between addiction to smartphone usage and depression among adults: A cross sectional study: BMC Psychiatry, 2018; 18(1); 148
64. Augner C, Vlasak T, Aichhorn W, Tackling the ‘digital pandemic’: The effectiveness of psychological intervention strategies in problematic Internet and smartphone use-A meta-analysis: Aust NZJ Psychiatry, 2022; 56(3); 219-29
65. Liu S, Xiao T, Yang L, Exercise as an alternative approach for treating smartphone addiction: A systematic review and meta-analysis of random controlled trials: Int J Environ Res Public Health, 2019; 16(20); 3912
In Press
08 Mar 2024 : Animal Research
Modification of Experimental Model of Necrotizing Enterocolitis (NEC) in Rat Pups by Single Exposure to Hyp...Med Sci Monit In Press; DOI: 10.12659/MSM.943443
18 Apr 2024 : Clinical Research
Comparative Analysis of Open and Closed Sphincterotomy for the Treatment of Chronic Anal Fissure: Safety an...Med Sci Monit In Press; DOI: 10.12659/MSM.944127
08 Mar 2024 : Laboratory Research
Evaluation of Retentive Strength of 50 Endodontically-Treated Single-Rooted Mandibular Second Premolars Res...Med Sci Monit In Press; DOI: 10.12659/MSM.944110
11 Mar 2024 : Clinical Research
Comparison of Effects of Sugammadex and Neostigmine on Postoperative Neuromuscular Blockade Recovery in Pat...Med Sci Monit In Press; DOI: 10.12659/MSM.942773
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952