12 June 2021: Clinical Research
Effect of Emerging Major Infectious Diseases on Sleep Quality of Medical Workers: Findings from Medical Workers Providing Support During the COVID-19 Pandemic
Wen Zhu1ABCDEFG, Yue Fang2AF, Zhong-liang Bai3BC, Nian-nian Li4BC, Jia-yun Zhao1BG*, Zhi Hu3BDOI: 10.12659/MSM.931881
Med Sci Monit 2021; 27:e931881
Abstract
BACKGROUND: The coronavirus disease 2019 (COVID-19) outbreak has exerted immense pressure on medical systems in China and abroad. This study aimed to compare the sleep quality of medical personnel conscripted to the Wuhan Union Cancer Centre to offer support during the early stages of the COVID-19 pandemic to the sleep quality of those who remained at Anhui Medical University Hospital and to determine the role of interventions in improving sleep quality.
MATERIAL AND METHODS: Questionnaires were completed by 369 individuals who were conscripted to support Wuhan (N=137) and others who were not (the control group; N=232). The Pittsburgh Sleep Quality Index (PSQI) was used to measure the duration and quality of sleep. The Anhui Provincial Health Commission organized a comprehensive intervention, consisting of physical-psychological-social dimensions, over the course of 2 weeks.
RESULTS: Only 34.21% of the Wuhan support workers reported better sleep quality, as opposed to the 55.60% of the control group at stage 1 (t/χ²=14.005, P<.001). Furthermore, despite the Wuhan support group being more prone to poor sleep quality, their sleep quality significantly improved after the interventions.
CONCLUSIONS: The findings from this study showed that medical staff who were conscripted to offer support during the early stages of the COVID-19 pandemic suffered from impaired quality of sleep. The use of questionnaire-based sleep assessments may provide individualized approaches to supporting medical personnel during future epidemics and pandemics. Furthermore, our results indicate that relevant interventions can significantly improve sleep quality, while a prolonged break after interventions does not affect sleep quality.
Keywords: COVID-19, Medical Staff, Hospital, Sleep, Anxiety, COVID-19, Hospitals, University, Pandemics, SARS-CoV-2, Sleep Initiation and Maintenance Disorders, Surveys and Questionnaires, young adult
Background
The coronavirus disease 2019 (COVID-19) first broke out in Wuhan, China, in December 2019 and rapidly spread, thus becoming a global pandemic [1–4]. This outbreak has had a huge impact on global health and medical systems [5]. COVID-19 is one of the several newly identified forms of coronaviruses that can infect humans; it is a respiratory pathogen, just like SARS CoV, which causes the severe acute respiratory syndrome (SARS), and MERS-CoV, which causes the Middle-East respiratory syndrome (MERS) [6]. The World Health Organization officially named this virus the ‘novel coronavirus’, on February 11, 2020, and declared it a global pandemic on March 11 [7,8]. China responded quickly by halting public transportation and announcing large-scale quarantine measures in many areas, starting from late January [9]. In particular, the China National Health Commission put a series of emergency measures in place, including the establishment of emergency isolation points, infectious disease hospitals, and China-specific ‘Fang cang’ or makeshift hospitals, to deal with the outbreak. In addition, external emergency medical teams were quickly established nationwide and medical assistance was assigned to Hubei Province [10]. By February 26, volunteer medical workers (N=32 395) and over 178 crisis response teams were dispatched to the province to join forces during the medical emergency [11]. As each hospital serves millions of people, the First Affiliated Hospital of Anhui Medical University organized a group of 137 medical personnel to support Wuhan and take over one intensive care unit of the Wuhan Union Cancer Centre.
Epidemiological studies on the SARS and Ebola viruses indicate that newly emerging major infectious diseases can exert great pressure on medical workers [12]. Due to the limited understanding, awareness, and prevention measures in the early stages of the COVID-19 outbreak, 3387 health professionals were infected at 476 clinical support points, 26 of whom died [11]. Additional healthcare workers were deployed to support the front-line workers of Wuhan city. However, the daily infection risk in an unfamiliar environment, as well as the limited medical protective equipment and clinical experience, may have potentially increased fatigue and sleep disturbances, thereby affecting the output of the medical staff [13–15].
Locally, China managed to stabilize the situation and contain the epidemic, thus entering a post-epidemic stage. Since July 14, 2020, the number of related infected cases and deaths (4634 at that stage) has gradually decreased [16]. Simultaneously, the number of infected cases and 576 496 deaths globally reflected a situation that was increasingly detrimental to the physical and psychological wellbeing of medical workers.
Sleep quality is a key indicator of health. Good sleep quality not only helps medical staff to work better when treating patients, but it also maintains their optimal immune function to prevent infections [17]. In addition, sleep quality is affected by physical-psychological-social dimensions and factors [18]. Previous studies showed that during pandemics, people are more likely to experience sleep disorders [19–22]. Environmental stressors, physical illness, separation from family and friends, and other comorbid psychological problems can contribute to this problem.
Most studies about the anxiety and sleep quality of front-line medical workers have had a cross-sectional design, neglecting longitudinal, comparative research [23–26]. Consequently, in the context of COVID-19, we first aimed to analyze the factors influencing the sleep quality of the medical workers who were dispatched to support Wuhan vs those who were not (control group). We based these assessments on the Pittsburgh Sleep Quality Index (PSQI), which we used to measure the duration of sleep and sleep quality during the early stages of the outbreak [25,27,28]. Second, we aimed to assess changes in sleep quality following an intervention by comparing sleep results before and after the intervention, which consisted of physical-psychological-social dimensions, over the course of 2 weeks. Third, we aimed to assess whether, with effective interventions, medical workers can resume their jobs at a post-epidemic stage, following their return from Wuhan, rather than continue to rest and adjust their sleep patterns. This study enhances our own understanding of poor sleep quality and the understanding among Wuhan support staff returning to work in the post-epidemic era.
Material and Methods
ETHICS APPROVAL:
This study was conducted in accordance with the Declaration of Helsinki. All participants provided signed informed consent to participate in the study. The First Affiliated Hospital of Anhui Medical University Ethics Committee approved the study procedures (Approval number: Quick -PJ 2021-04-10).
STUDY SAMPLE:
We surveyed 369 medical workers; some were dispatched to support front-line medical workers at the Wuhan Union Cancer Centre (N=137) and others remained at the Anhui Medical University Hospital to support front-line medical staff during the outbreak (control group, N=232). All of the medical workers who participated in the survey did so voluntarily, and the principles of confidentiality were upheld.
STUDY DESIGN:
This was an observational study, in which an online questionnaire link was posted on WeChat, the most common and widely used social media in China, with relatively good confidentiality [29]. We used WeChat to investigate and understand the medical workers (including the front-line medical staff supporting Wuhan and those who remained behind) of the First Affiliated Hospital of Anhui Medical University, from February 12 to May 8, 2020. At the beginning of the questionnaire, we informed the participants that completion of the survey indicated informed consent. Subsequently, the team leader would send links to each member to fill in the questionnaire.
SLEEP QUALITY: The PSQI was used to evaluate sleep quality [27,28]. This index evaluates the sleep quality over the previous month. It consists of 19 self-evaluation items and 7 dimensions: sleep quality, onset latency, duration, efficiency, sleep disturbance, use of sleeping medications, and daytime dysfunction. The score ranges from 0 to 3 for each dimension, and the summed score of the 7 dimensions is the global score (range: 0–21) for subjective sleep quality. Higher scores reflect poorer subjective sleep quality. Researchers found that a PSQI score >7 cut-off point, with a sensitivity of 98% and a specificity of 90% (kappa=0.89, P<.01), is suitable for determining sleep disturbance among Chinese people [30].
OTHER VARIABLES:
We collected information about demographic characteristics, including gender, age, occupation, years of work experience, departments, and titles.
PITTSBURGH SLEEP QUALITY INDEX (PSQI):
The survey was administered in 3 stages. Among the Wuhan support staff, 114 completed the questionnaire (effective response rate=83.21%) in the first stage (March 1) after supporting Wuhan front-line personnel for nearly 3 weeks. During the second stage (March 19), questionnaires were administered to Wuhan support workers after they had been withdrawn from the front line for quarantine; 110 workers responded (effective response rate=80.29%). During stage 3 (May 8), 114 Wuhan support personnel completed the questionnaire (effective response rate=83.21%).
INTERVENTION:
The Anhui Provincial Health Commission organized a comprehensive intervention, consisting of physical-psychological-social dimensions, over the course of 2 weeks. The content reflected 4 categories: (a) arranging a resting place for the medical staff evacuated from Wuhan, which completely differs from the high-intensity working environment that they had experienced there; (b) employing psychological experts to offer centralized psychological counselling 3 times a week; (c) improving medical workers’ daily diet and promoting outdoor exercise to enhance their physical condition and return it to normal (pre-pandemic) life; and (d) establishing a welcoming and positive public opinion and social environment to provide recognition and encouragement to the medical staff. The intervention was only for medical personnel who had supported Wuhan, not for those who had not. The intervention was used to compare the changes in sleep quality of health care workers in Wuhan, before and after the intervention, based on the PSQI.
STATISTICAL ANALYSIS:
Continuous variables are expressed as mean±standard deviation. We used the χ2 test and
Results
The average ages of the medical workers that supported Wuhan and those in the control group were 32.09±5.75 and 30.87±7.31 years, respectively. The average years of clinical work experience for the Wuhan support staff and for the control group were 9.81±6.03 and 8.94±8.47, respectively (Table 1). Our results showed statistically significant differences in occupational category (t/χ2=21.272,
According to the logistic regression analysis of the front-line medical staff’s sleep quality (Table 2), providing support to Wuhan was a risk factor, and the risk of poor sleep quality was 2.41 times higher than that in the control group (
A total of 92 people participated in the questionnaire after matching. As shown in Table 3, the sleep quality score of Wuhan support staff before and after the intervention was 8.02±3.78 and 6.84±3.09, respectively. Furthermore, the sleep score decreased and the sleep quality improved significantly after the inventions were implemented, with statistically significant differences (T=2.773,
The paired chi-square test results before and after the intervention show that the sleep quality of 92 medical workers who supported Wuhan improved significantly (χ2=11.831,
However, the improved sleep quality was unrelated to the rest period duration after intervention by comparison between the groups (Z=−0.800,
Discussion
The findings from this study indicate that, during the early stages of the COVID-19 pandemic, medical staff who were conscripted to the Wuhan Union Cancer Centre to offer support and those who remained at Anhui Medical University Hospital, between March and May 2020, suffered from impaired quality of sleep. In our study, alleviating the sleep disorders of the medical support staff in Wuhan effectively improved their physical and mental health. We supported the returning medical workers (N=137) with effective treatments provided through a series of physical and psycho-social interventions, which included adjusting their work, rest, and daily diet, as well as providing mental health guidance and physical activity recommendations. In particular, the interventions significantly improved their sleep quality, as indicated by the sleep quality scores, which were significantly reduced. This demonstrates that interventions can significantly improve the sleep quality of medical staff.
We examined the impact of COVID-19 on the sleep quality of medical workers who engaged in the treatment of infected patients and the role of relevant interventions to improve sleep quality. In doing so, we applied the PSQI, a brief instrument that can be administered through WeChat and which has shown good predictive value in previous studies [31–33]. Previous studies found that the Wuhan area – the centre of the outbreak – saw many patients in emergency care and fever clinics, exhausted medical resources, and had limited personal protective equipment. These factors affected Wuhan’s medical support staff, who continuously engaged in high-impact work and heavy workload, with little time to rest sufficiently, which affected their sleep time and quality [34]. Our results indicated that the sleep quality of the medical workers supporting Wuhan was significantly worse than that of the control group. This is consistent with a previous study that suggested that being at the center of the epidemic greatly affected the sleep quality of medical workers [35–37].
Although the medical workers supporting Wuhan had left the city, the epidemic was still ongoing, entering the post-epidemic stage, and medical workers needed to return to their posts and still deliver front-line medical service [38]. Some of the medical staff in our study who had supported Wuhan did not return to the hospital immediately, but rather chose to recuperate. However, the enhanced sleep quality after the unified intervention was unrelated to the rest duration after the intervention by comparison between groups. The intervention was the same except for the rest period, which means that the difference in sleep quality may be influenced by factors other than the rest period; in other words, sleep quality was not affected by the length of the rest period. Thus, the results indicated that after administration of the effective intervention, there was no meaningful improvement in sleep quality, even if the medical staff continued to recuperate on their own.
Notably, the medical workers who did not provide support in Wuhan (the control group) were at the front line of the medical services during the epidemic but had not worked at the core of the outbreak. Therefore, they could gradually adapt to the impact of the epidemic, which means that their sleep quality problems were not as serious as those of the medical workers who had supported Wuhan. Previous studies have found obvious psychological stress and sleep disorders among medical workers during the SARS outbreak in 2003 and the Ebola epidemic in Africa in 2014. Research has also shown sleep disorders among Chinese medical workers who provided support in Africa [12,39–43]. This is consistent with the results of our study, suggesting that providing support in Wuhan affected the sleep quality of medical workers. Furthermore, various studies showed that effective interventions for medical staff in an epidemic situation could significantly enhance their psychological state and sleep quality, effectively improve their work enthusiasm, and make their return to work in the post-epidemic stage easier [44–47]. Importantly, after effective interventions, front-line medical staff do not need to continue recuperating and can quickly return to work to ensure basic medical needs are met in the post-epidemic stage.
One of the advantages of this study is that, unlike other cross-sectional design studies, we continuously observed and then supported the medical staff assigned to Wuhan after they had left the area. They were able to return to normal clinical work after the 2-week intervention. By following a systematic process, we were able to fully understand the changes in the quality of sleep of the front-line support staff. Furthermore, we have shown that effective interventions considerably improved the sleep quality of front-line medical workers who participated in our study in Wuhan. The support group no longer required continuous rest, which helps ensure that good medical care is available in the stages immediately following a pandemic.
Our study has some limitations. First, the baseline data on the control group and the medical personnel who were dispatched to Wuhan were not available due to the sudden COVID-19 outbreak. Second, due to the epidemic, it was impossible to carry out field investigations, and investigations are only conducted through online questionnaires; however, the authenticity and reliability of the data can be guaranteed. Third, participants included medical personnel from a hospital in Anhui Province, and the data volume was small, which limits the generalizability of our study. More studies with multicenter study designs and large sample sizes are needed.
Conclusions
The findings from this study showed that medical staff who were conscripted to offer support during the early stages of the COVID-19 pandemic suffered from impaired quality of sleep. Using questionnaire-based sleep assessments can provide individualized approaches to supporting medical personnel during future epidemics and pandemics. Furthermore, the study results indicated that relevant interventions could significantly improve sleep quality, while a prolonged break after interventions does not affect sleep quality. Therefore, the sleep quality of medical personnel should be emphasized and interventions implemented because sleep quality played an important role in the overall treatment and prognosis of medical personnel during the pandemic.
Tables
Table 1. General information of respondents.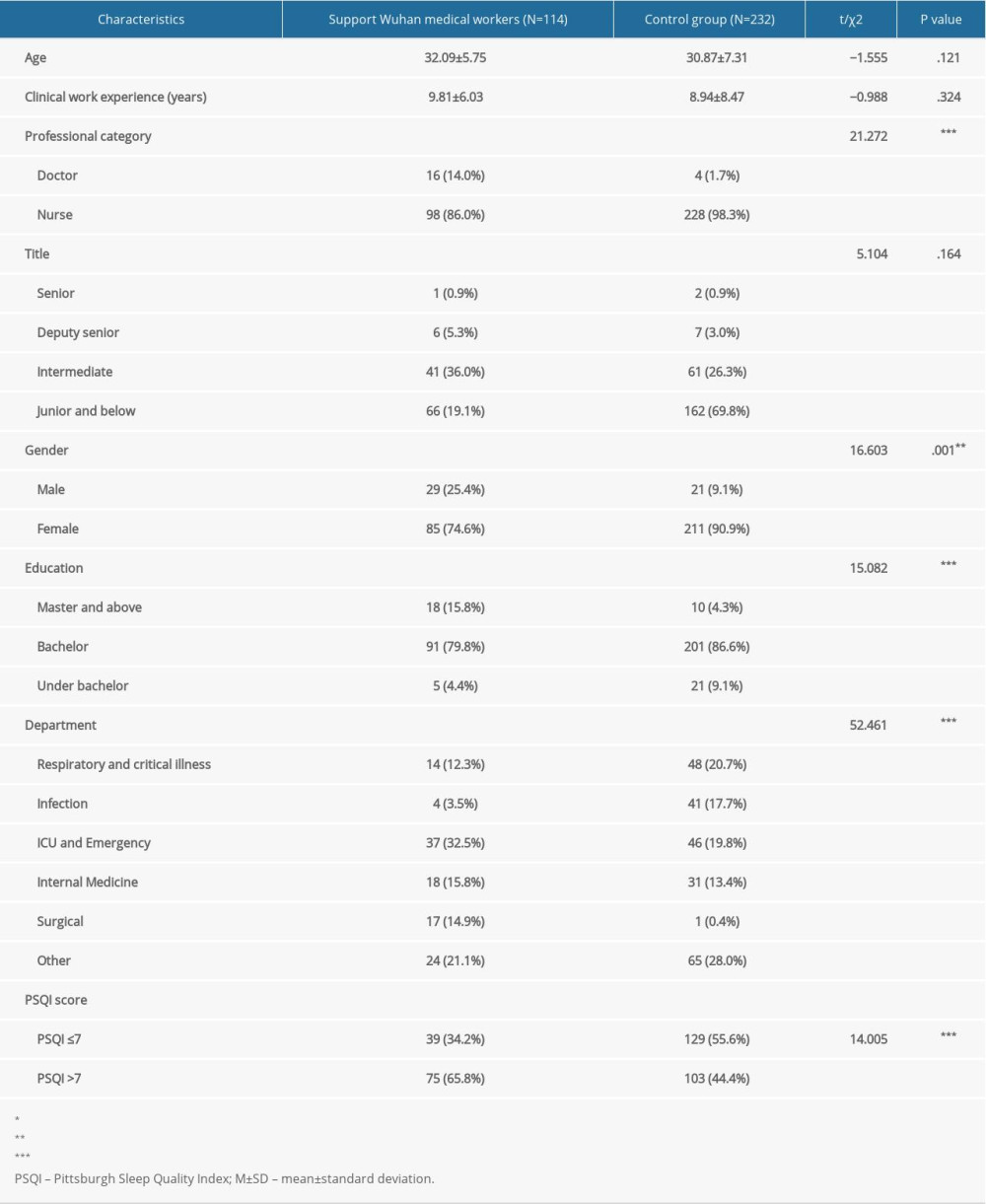 Table 2. Multivariate logistic regression analysis of factors influencing sleep quality of medical staff.
Table 2. Multivariate logistic regression analysis of factors influencing sleep quality of medical staff.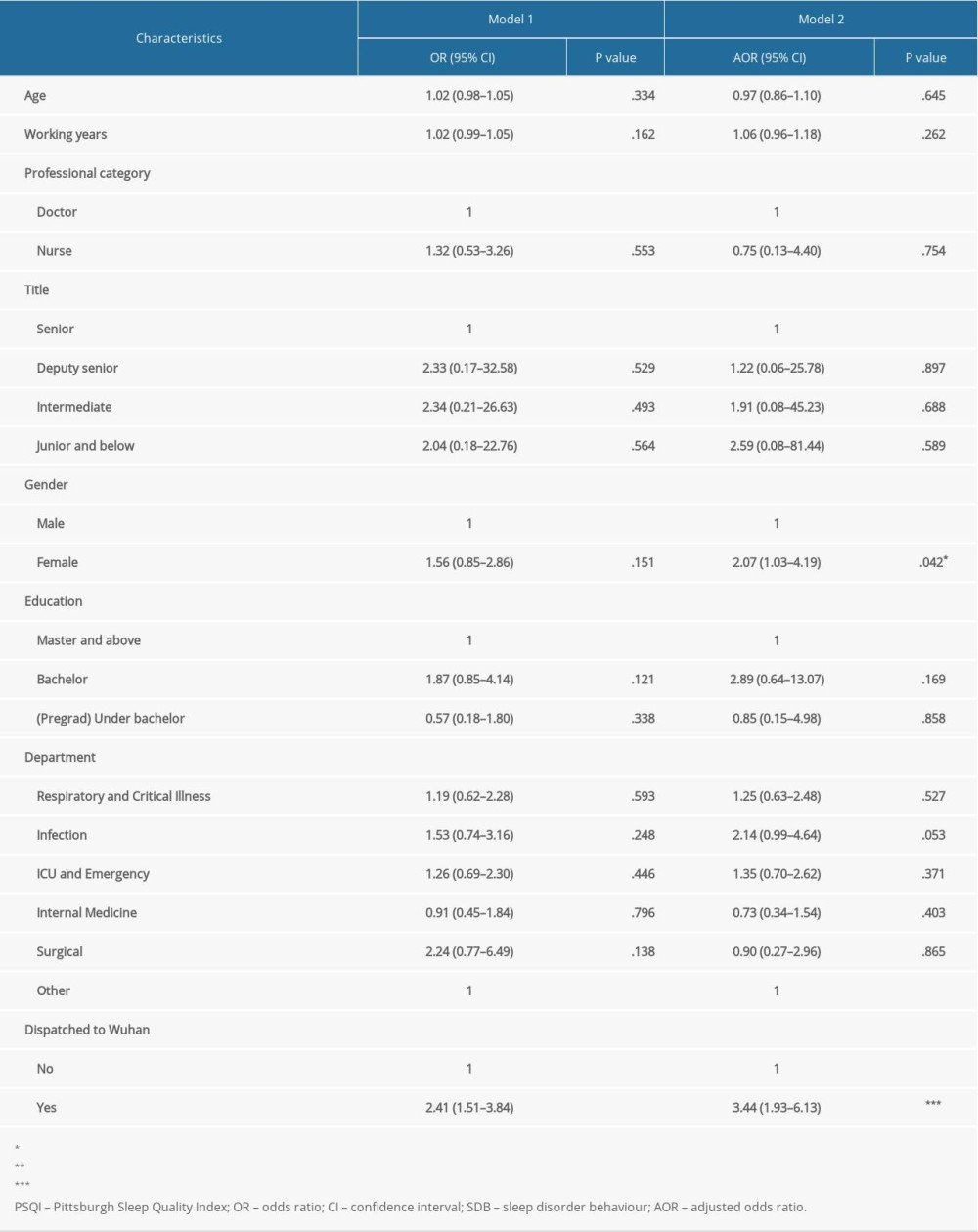 Table 3. Comparison of sleep quality scores among Wuhan medical support workers before and after intervention (N=92).
Table 3. Comparison of sleep quality scores among Wuhan medical support workers before and after intervention (N=92).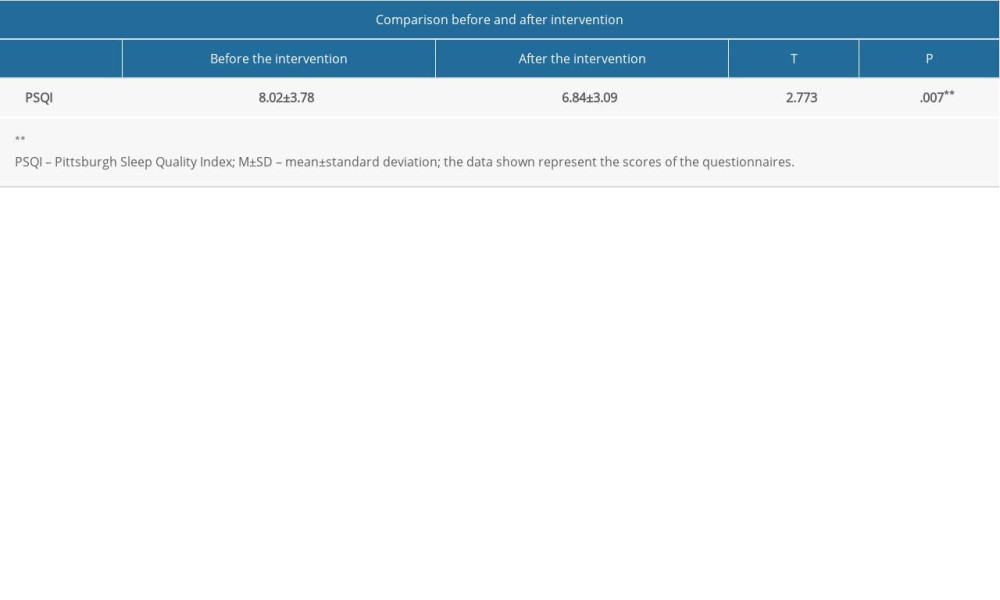 Table 4. Comparison of sleep disorder rates before and after intervention among medical workers in Wuhan (N=92).
Table 4. Comparison of sleep disorder rates before and after intervention among medical workers in Wuhan (N=92).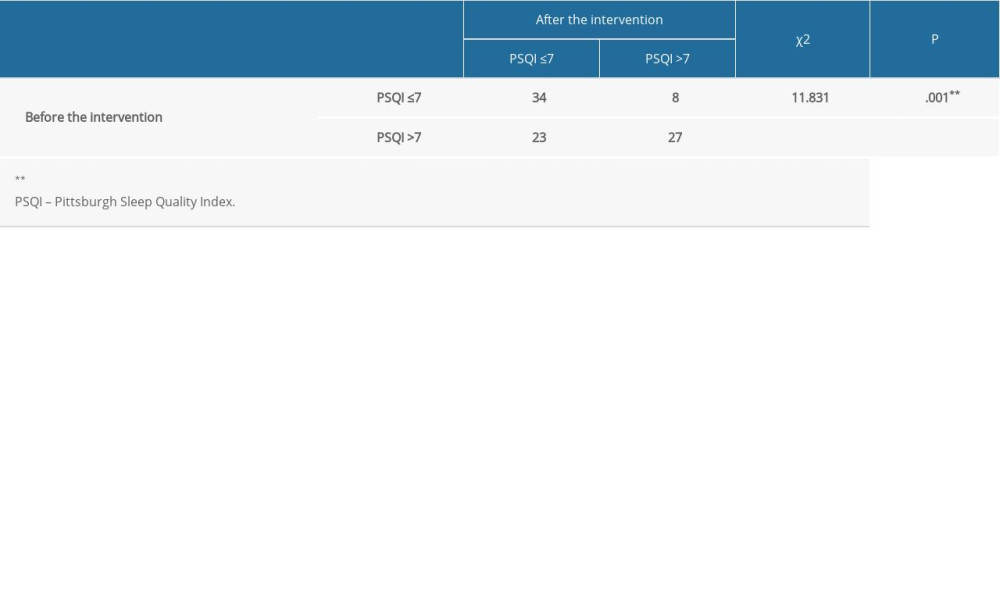 Table 5. Influence of continuous break on sleep quality after intervention (N=92).
Table 5. Influence of continuous break on sleep quality after intervention (N=92).
References
1. Ramadan N, Shaib H, Middle East respiratory syndrome coronavirus (MERS-CoV): A review: Germs, 2019; 9; 35-42
2. Zhong NS, Zheng BJ, Li YM, Epidemiology and cause of severe acute respiratory syndrome (SARS) in Guangdong, People’s Republic of China, in February, 2003: Lancet, 2003; 362; 1353-58
3. Chatterjee P, Nagi N, Agarwal A, The 2019 novel coronavirus disease (COVID-19) pandemic: A review of the current evidence: Indian J Med Res, 2020; 151; 147-59
4. Lai THT, Tang EWH, Chau SKY, Stepping up infection control measures in ophthalmology during the novel coronavirus outbreak: An experience from Hong Kong: Graefes Arch Clin Exp Ophthalmol, 2020; 258; 1049-55
5. Munster VJ, Koopmans M, van Doremalen N, A novel coronavirus emerging in China – key questions for impact assessment: N Engl J Med, 2020; 382; 692-94
6. Yuan S, Liao Z, Huang H, Comparison of the indicators of psychological stress in the population of Hubei province and non-endemic provinces in China during two weeks during the coronavirus disease 2019 (COVID-19) outbreak in February 2020: Med Sci Monit, 2020; 26; e923767
7. Shi Y, Wang G, Cai XP, An overview of COVID-19: J Zhejiang Univ Sci B, 2020; 21; 343-60
8. Wu K, Wei X, Analysis of psychological and sleep status and exercise rehabilitation of front-line clinical staff in the fight against COVID-19 in China: Med Sci Monit Basic Res, 2020; 26; e924085
9. Xiang YT, Yang Y, Li W, Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed: Lancet Psychiatry, 2020; 7; 228-29
10. Li W, Yang Y, Liu ZH, Progression of mental health services during the COVID-19 outbreak in China: Int J Biol Sci, 2020; 16; 1732-38
11. Zhou Y, Yang Y, Shi T, Prevalence and demographic correlates of poor sleep quality among frontline health professionals in Liaoning province, China during the COVID-19 outbreak: Front Psychiatry, 2020; 11; 520
12. Liu X, Kakade M, Fuller CJ, Depression after exposure to stressful events: Lessons learned from the severe acute respiratory syndrome epidemic: Compr Psychiatry, 2012; 53; 15-23
13. Preti E, Di Mattei V, Perego G, The psychological impact of epidemic and pandemic outbreaks on healthcare workers: Rapid review of the evidence: Curr Psychiatry Rep, 2020; 22; 43
14. Stuijfzand S, Deforges C, Sandoz V, Psychological impact of an epidemic/pandemic on the mental health of healthcare professionals: A rapid review: BMC Public Health, 2020; 20; 1230
15. Wu W, Zhang Y, Wang P, Psychological stress of medical staffs during outbreak of COVID-19 and adjustment strategy: J Med Virol, 2020; 92(10); 1962-70
16. Worldometers: COVID-19 Coronavirus Outbreak, 2020
17. Lange T, Dimitrov S, Born J, Effects of sleep and circadian rhythm on the human immune system: Ann NY Acad Sci, 2010; 1193; 48-59
18. Yao KW, Yu S, Cheng SP, Chen IJ, Relationships between personal, depression and social network factors and sleep quality in community-dwelling older adults: J Nurs Res, 2008; 16; 131-39
19. Ji D, Ji YJ, Duan XZ, Prevalence of psychological symptoms among Ebola survivors and healthcare workers during the 2014–2015 Ebola outbreak in Sierra Leone: A cross-sectional study: Oncotarget, 2017; 8; 12784-91
20. Lin CY, Peng YC, Wu YH, The psychological effect of severe acute respiratory syndrome on emergency department staff: Emerg Med J, 2007; 24; 12-17
21. Mohammed A, Sheikh TL, Gidado S, An evaluation of psychological distress and social support of survivors and contacts of Ebola virus disease infection and their relatives in Lagos, Nigeria: A cross sectional study – 2014: BMC Public Health, 2015; 15; 824
22. Jiang Z, Zhu P, Wang L, Psychological distress and sleep quality of COVID-19 patients in Wuhan, a lockdown city as the epicenter of COVID-19: J Psychiat Res, 2021; 136; 595-602
23. Jahrami H, BaHammam AS, AlGahtani H, The examination of sleep quality for frontline healthcare workers during the outbreak of COVID-19: Sleep Breath, 2021; 25(1); 503-11
24. Wang S, Xie L, Xu Y, Sleep disturbances among medical workers during the outbreak of COVID-2019: Occup Med (London), 2020; 70; 364-69
25. Xiao H, Zhang Y, Kong D, The effects of social support on sleep quality of medical staff treating patients with coronavirus disease 2019 (COVID-19) in January and February 2020 in China: Med Sci Monit, 2020; 26; e923549
26. Pappa S, Ntella V, Giannakas T, Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis: Brain Behav Immun, 2020; 88; 901-7
27. Lim SK, Yoo SJ, Koo DL, Stress and sleep quality in doctors working on-call shifts are associated with functional gastrointestinal disorders: World J Gastroenterol, 2017; 23; 3330-37
28. Khaksarian M, Behzadifar M, Behzadifar M, Sleep disturbances rate among medical and allied health professions students in Iran: Implications from a systematic review and meta-analysis of the literature: Int J Environ Res Public Health, 2020; 17(3); 1011
29. Zhang X, Wen D, Liang J, Lei J, How the public uses social media wechat to obtain health information in china: A survey study: BMC Med Inform Decis Mak, 2017; 17; 66
30. Liu X, Tang MQReliability and validity of the Pittsburgh Sleep Quality Index: Chinese Journal of Psychiatry, 1996; 29; 29103-7 [in Chinese]
31. Lima DVG, Kluthcovsky A, Fernandes LGR, Okarenski G, Quality of sleep and use of computers and cell-phones among university students: Rev Assoc Med Bras (1992), 2019; 65; 1454-58
32. Sedov ID, Cameron EE, Madigan S, Tomfohr-Madsen LM, Sleep quality during pregnancy: A meta-analysis: Sleep Med Rev, 2018; 38; 168-76
33. Sheng X, Liu F, Zhou J, Liao RPsychological status and sleep quality of nursing interns during the outbreak of COVID-19: Nan Fang Yi Ke Da Xue Xue Bao, 2020; 40; 346-50 [in Chinese]
34. Zhang WR, Wang K, Yin L, Mental health and psychosocial problems of medical health workers during the COVID-19 epidemic in China: Psychother Psychosom, 2020; 89; 242-50
35. Qi J, Xu J, Li BZ, The evaluation of sleep disturbances for Chinese frontline medical workers under the outbreak of COVID-19: Sleep Med, 2020; 72; 1-4
36. Yu BY, Yeung WF, Lam JC, Prevalence of sleep disturbances during COVID-19 outbreak in an urban Chinese population: A cross-sectional study: Sleep Med, 2020; 74; 18-24
37. Pinto J, van Zeller M, Amorim P, Sleep quality in times of COVID-19 pandemic: Sleep Med, 2020; 74; 81-85
38. Tang Y, Xing Y, Cui L, Neurology practice during the COVID-19 outbreak and post-pandemic era: experiences and challenges: Eur J Neurol, 2020; 27(12); e81-e83
39. Chen CS, Wu HY, Yang P, Yen CF, Psychological distress of nurses in Taiwan who worked during the outbreak of SARS: Psychiatr Serv, 2005; 56; 76-79
40. Tam CW, Pang EP, Lam LC, Chiu HF, Severe acute respiratory syndrome (SARS) in Hong Kong in 2003: Stress and psychological impact among frontline healthcare workers: Psychol Med, 2004; 34; 1197-204
41. Chan AO, Huak CY, Psychological impact of the 2003 severe acute respiratory syndrome outbreak on health care workers in a medium size regional general hospital in Singapore: Occup Med (Lond), 2004; 54; 190-96
42. Maunder RG, Lancee WJ, Rourke S, Factors associated with the psychological impact of severe acute respiratory syndrome on nurses and other hospital workers in Toronto: Psychosom Med, 2004; 66; 938-42
43. Li L, Wan C, Ding R, Mental distress among Liberian medical staff working at the China Ebola Treatment Unit: A cross sectional study: Health Qual Life Outcomes, 2015; 13; 156
44. Chersich MF, Gray G, Fairlie L, COVID-19 in Africa: Care and protection for frontline healthcare workers: Global Health, 2020; 16; 46
45. Chew NWS, Lee GKH, Tan BYQ, A multinational, multicentre study on the psychological outcomes and associated physical symptoms amongst healthcare workers during COVID-19 outbreak: Brain Behav Immun, 2020; 88; 559-65
46. Blake H, Bermingham F, Johnson G, Tabner A, Mitigating the psychological impact of COVID-19 on healthcare workers: A digital learning package: Int J Environ Res Public Health, 2020; 17; 2997
47. Schwartz R, Sinskey JL, Anand U, Margolis RD, Addressing postpandemic clinician mental health: A narrative review and conceptual framework: Ann Intern Med, 2020; 173(12); 981-88
Tables
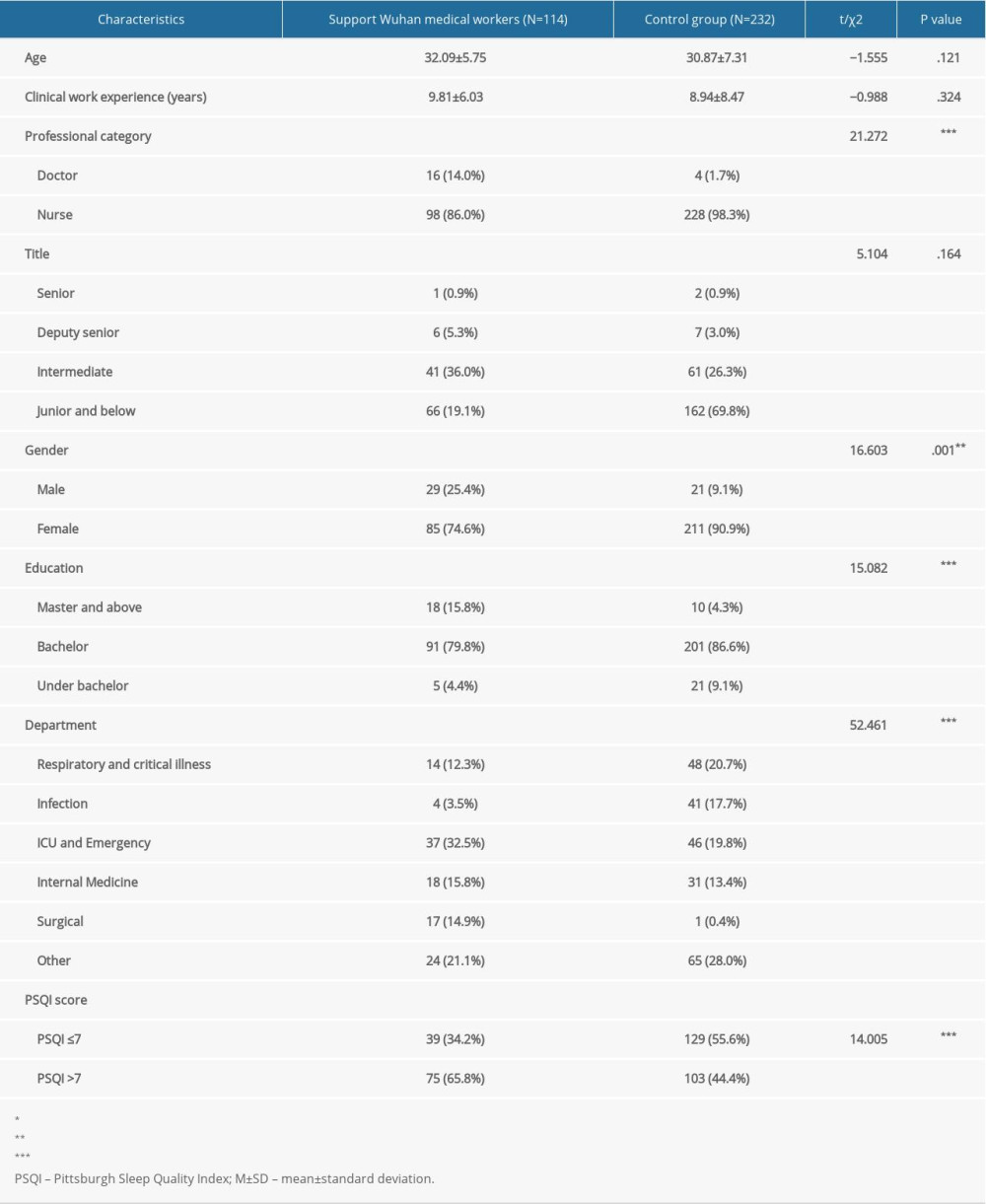 Table 1. General information of respondents.
Table 1. General information of respondents.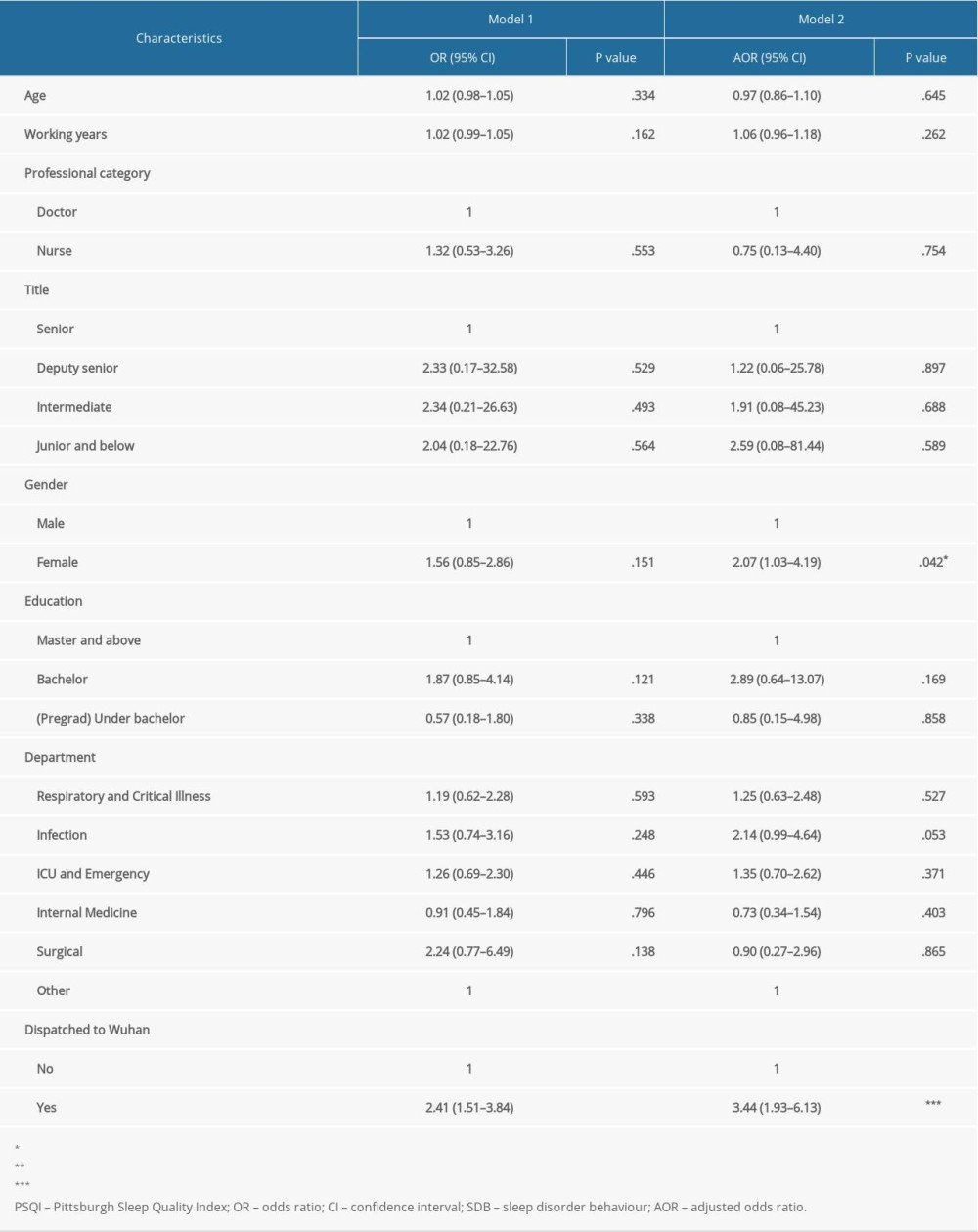 Table 2. Multivariate logistic regression analysis of factors influencing sleep quality of medical staff.
Table 2. Multivariate logistic regression analysis of factors influencing sleep quality of medical staff.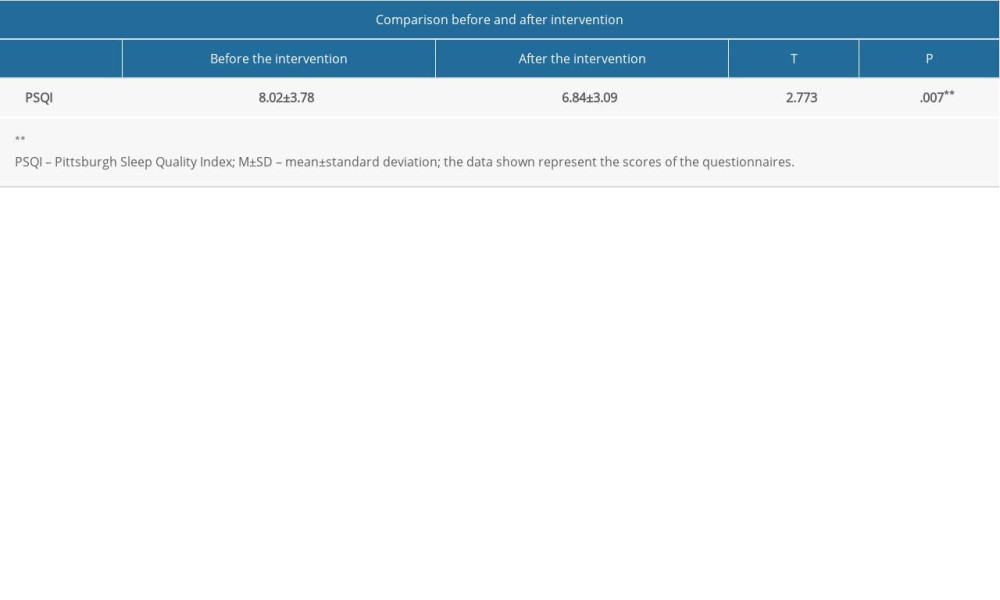 Table 3. Comparison of sleep quality scores among Wuhan medical support workers before and after intervention (N=92).
Table 3. Comparison of sleep quality scores among Wuhan medical support workers before and after intervention (N=92).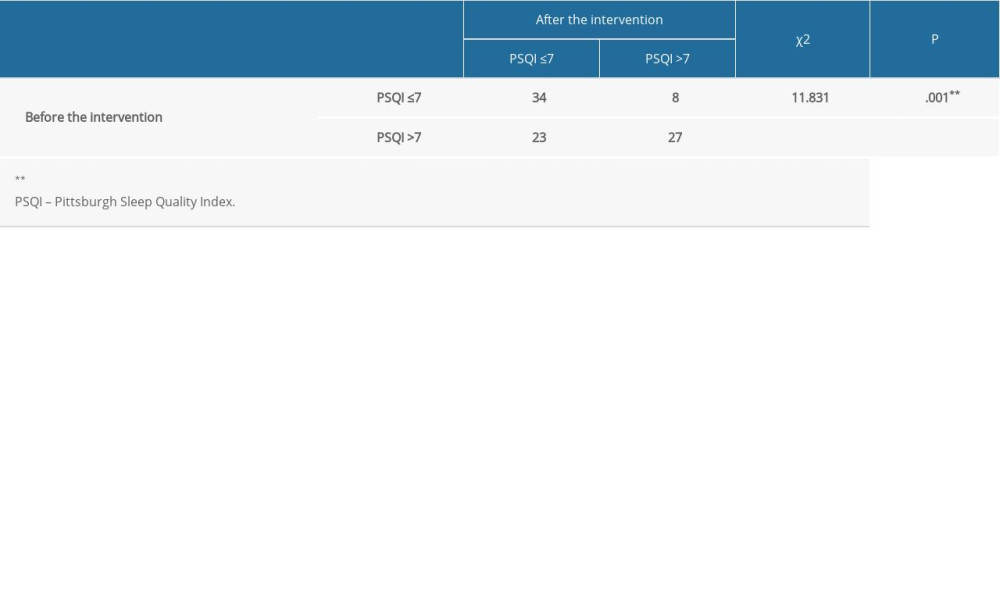 Table 4. Comparison of sleep disorder rates before and after intervention among medical workers in Wuhan (N=92).
Table 4. Comparison of sleep disorder rates before and after intervention among medical workers in Wuhan (N=92). Table 5. Influence of continuous break on sleep quality after intervention (N=92).
Table 5. Influence of continuous break on sleep quality after intervention (N=92). In Press
21 Mar 2024 : Meta-Analysis
Economic Evaluation of COVID-19 Screening Tests and Surveillance Strategies in Low-Income, Middle-Income, a...Med Sci Monit In Press; DOI: 10.12659/MSM.943863
10 Apr 2024 : Clinical Research
Predicting Acute Cardiovascular Complications in COVID-19: Insights from a Specialized Cardiac Referral Dep...Med Sci Monit In Press; DOI: 10.12659/MSM.942612
06 Mar 2024 : Clinical Research
Enhanced Surgical Outcomes of Popliteal Cyst Excision: A Retrospective Study Comparing Arthroscopic Debride...Med Sci Monit In Press; DOI: 10.12659/MSM.941102
06 Mar 2024 : Clinical Research
Prevalence and Variation of Medical Comorbidities in Oral Surgery Patients: A Retrospective Study at Jazan ...Med Sci Monit In Press; DOI: 10.12659/MSM.943884
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








