26 August 2021: Clinical Research
The Assessment of Sleep Quality in Patients Following Valve Repair and Valve Replacement for Infective Endocarditis: A Retrospective Study at a Single Center
Xiang-Ming Hu12ABCDEF, Wen-Ting Wei2BCDF, De-Yi Huang2BCD, Cai-Di Lin2BCD, Fen Lu2BCD, Xiao-Ming Li2BCD, Huo-Sheng Liao2BCD, Zhi-Hong Yu3BCD, Xiao-Ping Weng2CDE, Shi-Bin Wang4BCD, Cai-Lan Hou4BCD, Fu-Jun Jia14AEFG*DOI: 10.12659/MSM.930596
Med Sci Monit 2021; 27:e930596
Abstract
BACKGROUND: The aim of this study was to measure sleep quality among patients who underwent infective endocarditis (IE) surgery and identify the risk factors involved in sleep disorders.
MATERIAL AND METHODS: In this study, we used actigraphy, the Pittsburgh Sleep Quality Index (PSQI), and Epworth Sleep Scale (ESS) to determine the clinical characteristics of sleep disorders in 116 patients with IE who were in rehabilitation after surgery.
RESULTS: Our results showed that 46 (39.7%) patients had sleep efficiency over 85%, while 70 (60.3%) patients had sleep efficiency below 85%. The correlation analysis showed that sleep efficiency was related to the duration of the disease, with a longer duration leading to lower sleep efficiency (P=0.031). The sleep efficiency of patients with IE following surgery was also affected by alcohol consumption; however, surprisingly, patients with “heavy” alcohol consumption had higher sleep efficiency (P=0.030). We found a significant correlation between sleep efficiency and postoperative interleukin-6 (IL) levels, C-reactive protein (CRP) levels, and preoperative erythrocyte sedimentation rate (P<0.05). No significant correlation was found between brain natriuretic peptide levels and sleep efficiency, PSQI score, or ESS score. Postoperative hemoglobin (Hb) level was associated with sleep efficiency (R=0.194, P=0.036), but there was no statistically significant correlation between the PSQI and ESS scores. Postoperative alanine transaminase (ALT) showed a significant negative correlation with sleep efficiency (R=-0.27, P=0.003).
CONCLUSIONS: We found a high prevalence of sleep disorders in patients with IE along with an increase in inflammatory factors, including postoperative IL-6, CRP, ALT, and Hb levels.
Keywords: actigraphy, Dyssomnias, Endocarditis, Aortic Valve, cardiac catheterization, Follow-Up Studies, Heart Valve Prosthesis, Postoperative Complications, Reproducibility of Results, Sleep Wake Disorders, Surveys and Questionnaires
Background
Sleep disorders refer to a collection of conditions that affect sleep quality and duration and impact an individual’s ability to function efficiently while they are awake. Sleep disorders have a high incidence in patients with chronic medical conditions, such as diabetes, high blood pressure, and cardiovascular disease, and can aggravate the severity of disease [1,2]. Various sleep-related components, such as sleep efficiency and sleep time, are involved in systemic pathophysiological processes in the body, such as metabolism and the cardiovascular system. Sleep efficiency, one of the most critical components of sleep, is the percentage of total time spent asleep. Infective endocarditis (IE) is an intimal microbial infection that causes local inflammation and persistent bacteremia, followed by pneumonia, septicemia, and intra-abdominal abscess [3]. Even with the best treatment, IE is still a serious disease with poor outcomes. A systematic review of 15 studies including patients from the United States and Europe over the past few decades showed that hospital mortality has not changed since the 1980s, with the average hospital mortality rate ranging from 17% to 20% per decade [4]. This significant risk of hospitalization followed by death requires joint efforts from all medical, cardiac, and health personnel involved in the care of patients with IE to improve the prognosis at all stages of the disease. However, IE is often accompanied by sleep disorders, and increasing evidence indicates that sleep disorders can induce or aggravate cardiovascular disease, damage liver function, cause inflammation or insulin resistance, affect the quality of life of patients, and delay their recovery from disease [5,6]. Previous clinical studies have demonstrated that insufficient sleep causes inflammation, and plasma C-reactive protein (CRP) concentration increases in patients with sleep deprivation and poor sleep quality [7,8]. However, some studies have found no association between sleep time, sleep quality, and CRP levels [9,10]. There are many studies on sleep disorders in patients with somatic diseases; however, there have been few studies reported on sleep disorders in patients with IE. In the present study, we assessed sleep quality in patients following IE surgery using the Pittsburgh Sleep Quality Index (PSQI), Epworth Sleep Scale (ESS), and actigraphy.
Material and Methods
PATIENTS:
This study included patients with IE who underwent cardiac surgery at the Guangdong Provincial People’s Hospital between October 2016 and September 2018. All patients had indications for cardiac surgery and underwent either repair of damaged heart valves (valve repair) or replacement of damaged heart valves with prosthetic valves (valve replacement) according to the 2015 European Society of Cardiology Guidelines for the Management of Infective Endocarditis [11]. Patients received postoperative medical monitoring and care in the cardiac intensive care unit after completing surgical treatment. Once a patient’s condition stabilized and was reviewed and approved by the cardiac surgeons, the patient was transmitted to the rehabilitation ward for postoperative antibiotic and recovery treatment. The exclusion criteria in the study were (1) unconsciousness; (2) history of mental disorders; (3) complication with stroke; and (4) uncontrollable infection. We also included the course of the disease as a research indicator, which included date of disease diagnosis to date of hospitalization. In this study, the subjective scales and objective evaluation methods were carried out within 1 week after a patient entered the rehabilitation ward.
The study was approved by the Hospital Ethics Committee (No. GDREC2016222H R2). All procedures involving human participants were performed following the ethical standards of the institutional and/or national research committee and the Declaration of Helsinki and its later amendments, or comparable ethical standards. Written informed consent was obtained from all participants.
DATA COLLECTION:
Demographic information, inflammatory biomarkers, including white blood count (WBC), erythrocyte sedimentation rate (ESR), CRP, and interleukin 6 (IL-6), embolic complications, other laboratory test results, and ultrasound results (size of the excrescence and multi-valve involvement), were collected from the patients’ electronic medical records.
OBJECTIVE SLEEP MEASURE:
The ActiGraph accelerometer (Actigraph Corporation, Pensacola, FL, USA) is widely used for objective ambulatory measurements. In actigraphy, compared with traditional polysomnography, the wearer can move freely, and the average sleep efficiency can be calculated after completing the sleep test. In this study, participants were given an ActiGraph to examine various aspects of sleep depending on body movement. Actigraphy sleep parameters included sleep efficiency (the percentage of the time spent asleep in bed divided by the total time in bed), total sleep time, wake after sleep onset (total minutes awake after sleep onset), and the number of awakenings. Patients were also asked to keep a daily sleep diary, which included subjective information about their wake time and bedtime. The sleep diary was primarily used to assist with manually identifying sleep onset and wake time intervals each night to calculate each sleep measure collected by actigraphy.
The ActiGraph accelerometer was used to monitor patients’ sleep for 5 to 14 days. Then, the actigraphy data and sleep diaries were collected from all patients. ActiLife 6 analysis software was used to analyze the actigraphy data. The “automatic interpretation and review” function in the software was used for early-stage data processing. Based on the results from automatic interpretation, manual correction was performed when necessary, using patients’ sleep diaries as references. The average values of the above-mentioned indicators (sleep efficiency, total sleep time, total minutes awake after sleep onset, and the number of awakenings) were recorded. A widely accepted normal range for sleep efficiency is >85%.
SUBJECTIVE SLEEP QUESTIONNAIRES:
On the second day after transfer from the cardiac intensive care unit to the general rehabilitation ward, patients were instructed to complete the PSQI and the ESS questionnaires independently or with help from an investigator. The completed questionnaires were then analyzed by the investigator(s).
PITTSBURGH SLEEP QUALITY INDEX: The PSQI is a self-administered standardized questionnaire used to assess retrospective sleep quality and disturbances in patients over a period of 1 month. The translated PSQI is a 19-item self-rated questionnaire composed of 7 subscales, which include sleep quality, sleep latency, sleep duration, sleep efficiency, sleep disorders, sleep medications, and daily dysfunction. The score for each subscale ranges from 0 to 3. The 7 component scores are summed to produce a PSQI global score, which ranges from 0 to 21 [12]. A PSQI score ≥8 points indicates poor sleep quality, while a PSQI score <8 points represents good sleep quality [13,14].
EPWORTH SLEEP SCALE: The ESS is an 8-item self-reported daytime sleepiness scale. Respondents indicate how often they exhibit sleep behaviors in 8 different situations using a 4-point Likert type scale (0=never to 3=high probability). The total score of responses ranges from 0 to 24. An ESS score of ≥9 indicates excessive sleepiness during the daytime [15].
STATISTICAL ANALYSIS:
All statistical analyses were done using the R language software package (version 3.6.1) and ggplot2 was used to plot the correlations. Descriptive data analysis was presented as mean±standard deviation for continuous variables or n (%) for categorical variables. Variables were tested for normal distribution using the Kolmogorov-Smirnov test. The Pearson correlation coefficient was used to explore the correlation between sleep efficiency, PSQI scores, and ESS scores. A
Results
A total of 116 patients with IE (80 men and 36 women) aged between 18 and 75 years were enrolled in the study. Among them, 41 (35.3%) patients underwent repair of damaged heart valves, while 75 (64.7%) had damaged heart valves replaced with prosthetic valves. The ActiGraph accelerometer was used to measure sleep quality, and the results showed that 46 patients had sleep efficiency above 85%, while 70 patients had sleep efficiency below 85%. Compared with patients with sleep efficiency ≥85%, patients with sleep efficiency <85% had significant differences in alcohol consumption, duration of disease, and inflammation indicators (preoperative ESR, postoperative CRP levels, and IL-6 levels). In the <85% group, alcohol consumption was more frequent, duration of disease was shorter, and levels inflammatory indicators were lower. We found no significant differences in sex, age, body mass index (BMI), coffee or tea consumption, WBC, hemoglobin (Hb), albumin (Alb), alanine transaminase (ALT), and complications of embolism before and after surgery between the 2 groups.
The actigraphy data showed that the median sleep efficiency was 75.7%, median sleep latency was 11.2 min, median total time in bed was 531.0 min, median total sleep time was 399.1 min, and the median occurrence of nocturnal awakenings was 22.1 times. The median duration of awakenings was 93.1 min, with an average of 4.3 min each time in patients with sleep efficiency <85%. Significant differences were observed in sleep efficiency, total time in bed, total sleep time, duration of awakenings, and average awakening duration. Sleep efficiency and total sleep time were significantly lower (
In patients with sleep efficiency <85%, the mean PSQI score and the number of cases with a PSQI score ≥8 were 9.5 and 41 (58.6%), respectively, which were significantly higher than those in patients with sleep efficiency ≥85%. However, there were no significant differences in the mean ESS score and the number of cases with ESS score ≥9 among these patients. Additional results regarding the scale measures are presented in Table 1.
We performed a correlation analysis on the clinical characteristics of patients and sleep efficiency, and the results showed that sleep efficiency was related to the duration of the disease: a longer duration led to lower sleep efficiency (
The numbers of patients who underwent replacement of damaged heart valves with prosthetic valves in the sleep efficiency <85% group (n=70) and the sleep efficiency ≥85 group were 45 (60.0%) and 30 (40.0%), respectively, with no significant difference between the groups (Table 1). We further compared the sleep characteristics of patients undergoing different types of cardiac surgeries (valve repair or valve replacement) and found no significant differences in sleep efficiency, sleep latency, total time in bed, total sleep time, duration of awakenings, average awakening duration, frequency of awakenings, mean PSQI score, number of patients with PSQI ≥8, mean ESS score, and number of patients with ESS score ≥9 between the 2 groups (Table 2).
The laboratory tests showed a clear correlation between sleep efficiency and inflammation factors such as preoperative ESR, postoperative CRP levels, and postoperative IL-6 levels (
Brain natriuretic peptide is a hormone secreted by cardiomyocytes in response to stretching caused by heart failure or increased ventricular pressure. In the present study, all patients, with or without heart failure, underwent cardiac surgery. We studied the association between brain natriuretic peptide levels and sleep efficiency, PSQI scores, and ESS scores and found no significant correlation between them (Figure 2A–2C). Scatter analysis showed that postoperative Hb levels increased with sleep efficiency (R=0.19,
Discussion
Sleep disturbance is a multifactorial process, which occurs in most patients undergoing cardiac surgery [16]. A recent study reported that the sleep quality of patients following coronary artery surgery was poor in the intensive care unit and hospital ward, and remained unimproved up to 6 months after patient discharge [17]. A systematic review by Liao et al showed that sleep quality in patients with heart surgery is associated with physical factors (eg, cardiac function and pain), psychological factors (eg, anxiety and depression), individual factors (eg, age and sex), and environmental factors (eg, noise and light) [18]. Sleep quality evaluation is divided into subjective and objective evaluations, and objective evaluation mainly depends on sleep monitoring tools [19]. Traditionally, sleep research has been mainly based on the use of subjective scales. However, several studies have found that there are some differences between the subjective scale and objective scale, despite there being a correlation between them. Some researchers hold the view that the 2 types of scales should not be applied together [20,21]; however, others believe that studies need a combination of objective and subjective sleep measurements to assess sleep in patients who may have sleep disorders [22]. Currently, the objective scale has been widely used to study clinical sleep, and various sleep monitoring technologies have been developed to detect sleep quality [23]. The ActiGraph is a new sleep monitoring tool that has been widely used for monitoring sleep quality [24]. The motion sensor in the ActiGraph can predict and determine the depth of sleep by recording the motion and rest states of various parts of the human body. Based on individual needs, the body-monitoring instrument can be worn on the waist or on the wrist and ankle, and the wearer is free to move. Polysomnography is a widely used method to determine the quality and quantity of sleep as well as sleep architecture [25]. However, this methodology has limitations in studies involving the general population, especially in areas without access to polysomnography. By contrast, actigraphy is relatively inexpensive and easy to use, which makes the technique more realistic and feasible to use in large patient populations. Several actigraphy sleep monitoring systems have been developed in recent years to help clinicians and scientists. Actigraphy is widely used to objectively detect sleep, and sleep efficiency is calculated from actigraphy data, which objectively reflects the sleep quality of patients. Questionnaires are designed to estimate a patient’s total sleep time, sleep maintenance, wakefulness at night, mood, and physical feelings upon waking. The PSQI is a self-rated questionnaire that measures sleep quality over a 1-month period and is widely used across different age groups [26]. The ESS is a self-administered questionnaire available in different languages to estimate sleep quality in adults [27]. In the present study, we used actigraphy as an objective sleep measure for sleep disorders and combined it with the PSQI and ESS to evaluate the sleep status of patients. Sleep analysis software continuously recorded patients’ sleep information, including waking and sleeping patterns. The sleep latency, total sleep time, number of awakenings at night, and sleep efficiency were investigated in the present study.
The results showed that the sleep efficiency of patients with IE was significantly reduced, with 70 (60.3%) patients out of 116 having sleep efficiency lower than 85%. This confirmed that poor sleep quality is common in patients with IE. We found no relationship between sex, education level, marital status, or smoking history and sleep efficiency. Additionally, there was no clear relationship between sleep efficiency and type of cardiac surgery, heart failure or valve involvement. However, we found that sleep efficiency was related to the duration of the disease, whereby patients with longer disease duration had lower sleep efficiency. We found that the patients with a more prolonged course of IE had mental burdens or other negative factors, which affected sleep quality. A cross-sectional survey was performed using structured questionnaires such as the Alcohol Use Disorder Identification Test-Korean (AUDIT-KR), and a revised version. The results of that study demonstrated that the AUDIT-KR score was significantly associated with the patient sleep quality, sleep duration, and sleep disturbance, but not with sleep efficiency and daytime dysfunction [28]. We found a slight correlation between sleep efficiency and alcohol consumption. However, in the present cohort, patients who consumed more alcohol often had high sleep efficiency, which might be explained by the relatively small sample size of the current study.
Sleep plays a vital role in regulating the body’s innate and adaptive immune responses, and poor sleep quality is associated with chronic inflammation. Several cytokines and chemokines, such as IL-1β, IL-6, TNF-α, and high-sensitivity CRP, are related to poor sleep quality [29,30]. A previous study reported that poor sleep quality is equivalent to insulin resistance and is a risk factor for metabolic and cardiovascular diseases [31]. In the present study, we used the PSQI and actigraphy to evaluate sleep quality, and the levels of inflammatory cytokines and chemokines were detected to evaluate the inflammatory state. Consistent with most of the literature, we found that sleep efficiency was related to ESR, postoperative CRP levels, and postoperative IL-6 levels, suggesting that poor sleep quality may be linked to systemic inflammation in patients with IE.
ALT is found in the liver mostly and in other body tissues. Serum ALT, aspartate transaminase (AST), and the ALT/AST ratio are measured as biomarkers of liver health. A cross-sectional study showed that short sleep duration was a risk factor for the incidence of nonalcoholic fatty liver disease, which is reflected in the abnormalities of liver enzymes, including ALT [32]. A survey conducted on children and adolescents found that lack of sleep can lead to abnormalities in AST and ALT levels, which increase insulin resistance and obesity [33]. Another study found that people with breathing and sleeping disorders often experience abnormal changes in liver function, with an increased probability of chronic diseases [34]. Patients with obstructive sleep apnea had higher ALT levels than those without obstructive sleep apnea [35]. In the present study, we found that decreased sleep efficiency was associated with an increase in serum postoperative ALT levels, suggesting that sleep disorders might cause liver damage. This finding is also consistent with a meta-analysis demonstrating that sleep disorders are strongly associated with serum ALT levels.
A major limitation of this study is the absence of a detailed analysis of sleep architecture owing to its nonrandomized design, retrospective nature, and single-center experience. Future investigations on sleep-wake cycles, sleep-wake rhythm disorders, and types of sleep disorders are warranted. Also, we did not evaluate the presence of postoperative complications; therefore, we could not further explore the correlation between sleep quality and persistent infection after surgery. Finally, recall bias and the social desirability effect may have also affected the results of this study. We will address these limitations in a follow-up multicenter study.
Conclusions
In conclusion, we found that sleep disorders are a common problem in hospitalized patients with IE. Sleep inefficiency in patients with IE was correlated with preoperative ESR levels, postoperative CRP levels, postoperative IL-6 levels, and the increase in ALT levels. Additionally, our results showed that sleep inefficiency was related to Hb concentration and the course of the disease.
Figures
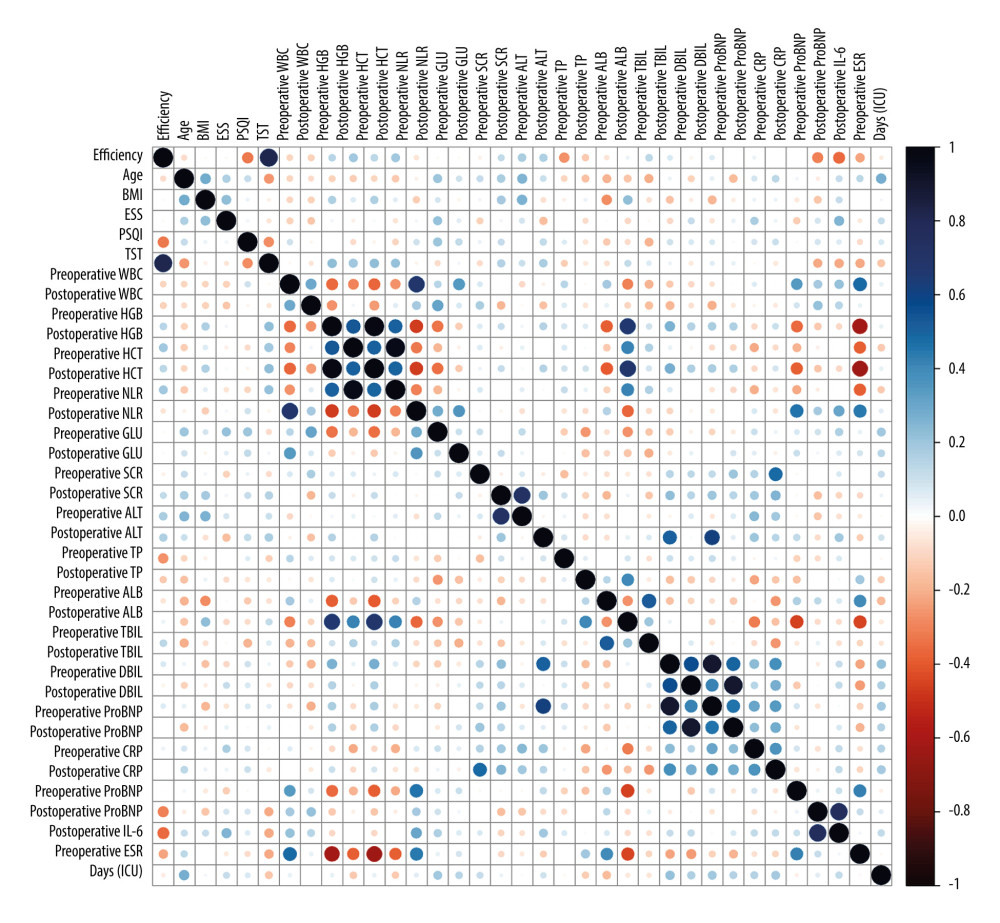 Figure 1. Heat map analysis of factors related to sleep disorders. Statistical analysis of correlation coefficients between sleep disorders and related factors. The color of the bars shows the statistical value. BMI – body mass index; ESS – Epworth Sleepiness Scale; PSQI – Pittsburgh Sleep Quality Index; TST – total sleep time; WBC – white blood count; HGB – hemoglobin; HCT – hematocrit; NLR – neutrophil to lymphocyte ratio; GLU – glucose; SCR – serum creatinine; ALT – alanine transaminase; TP – total protein; ALB – albumin; TBIL – total bilirubin; DBIL – direct-reacting bilirubin; ProBNP – pro-brain natriuretic peptide; CRP – C-reactive protein; IL-6 – interleukin 6; ESR – erythrocyte sedimentation rate; ICU – Intensive Care Unit.
Figure 1. Heat map analysis of factors related to sleep disorders. Statistical analysis of correlation coefficients between sleep disorders and related factors. The color of the bars shows the statistical value. BMI – body mass index; ESS – Epworth Sleepiness Scale; PSQI – Pittsburgh Sleep Quality Index; TST – total sleep time; WBC – white blood count; HGB – hemoglobin; HCT – hematocrit; NLR – neutrophil to lymphocyte ratio; GLU – glucose; SCR – serum creatinine; ALT – alanine transaminase; TP – total protein; ALB – albumin; TBIL – total bilirubin; DBIL – direct-reacting bilirubin; ProBNP – pro-brain natriuretic peptide; CRP – C-reactive protein; IL-6 – interleukin 6; ESR – erythrocyte sedimentation rate; ICU – Intensive Care Unit. 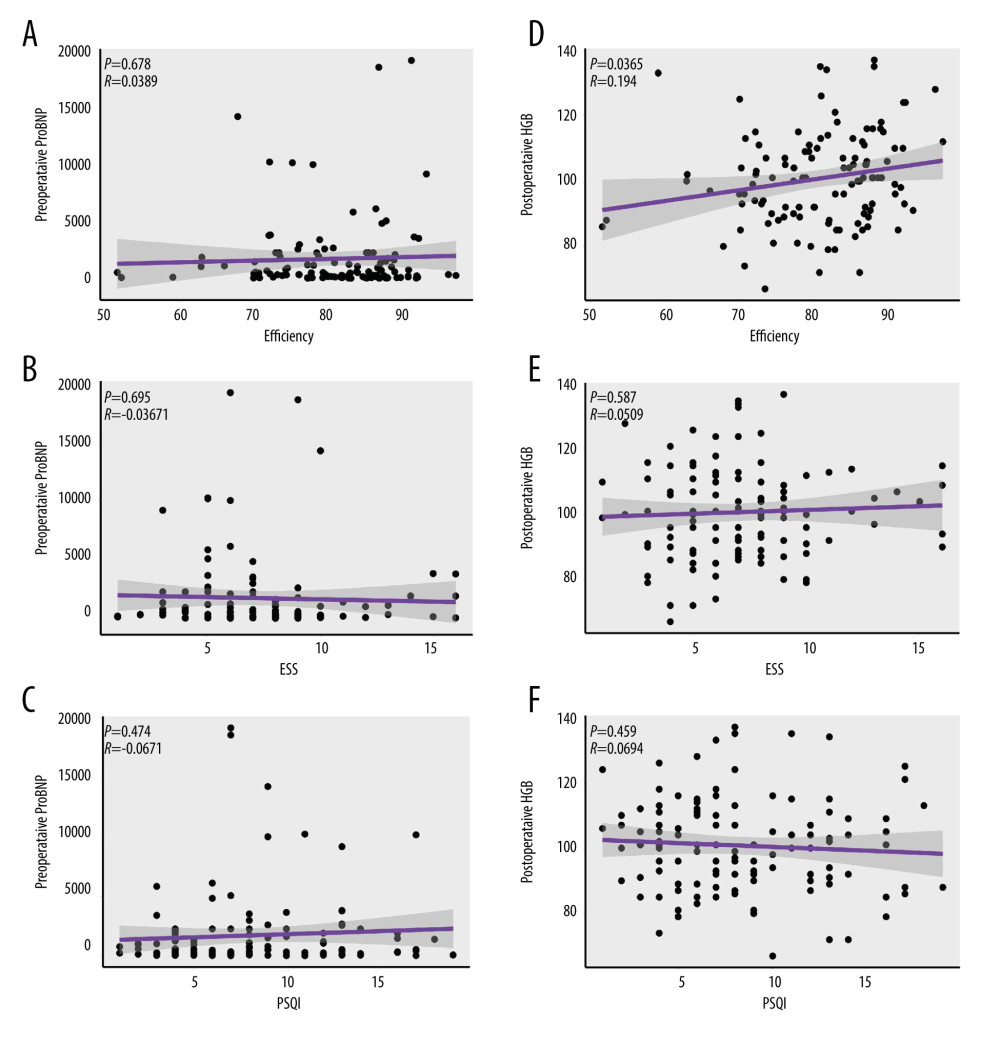 Figure 2. Correlation analysis between preoperative pro-brain natriuretic peptide and (A) sleep efficiency, (B) Epworth Sleepiness Scale (ESS), and (C) Pittsburgh Sleep Quality Index (PSQI), and (D) postoperative Hb and sleep efficiency, (E) Epworth Sleepiness Scale, and PSQI (F). PSQI – Pittsburgh Sleep Quality Index, ESS – Epworth Sleepiness Scale; ProBNP – pro-brain natriuretic peptide; HGB – hemoglobin.
Figure 2. Correlation analysis between preoperative pro-brain natriuretic peptide and (A) sleep efficiency, (B) Epworth Sleepiness Scale (ESS), and (C) Pittsburgh Sleep Quality Index (PSQI), and (D) postoperative Hb and sleep efficiency, (E) Epworth Sleepiness Scale, and PSQI (F). PSQI – Pittsburgh Sleep Quality Index, ESS – Epworth Sleepiness Scale; ProBNP – pro-brain natriuretic peptide; HGB – hemoglobin. References
1. Vilas D, Iranzo A, Tolosa E, Assessment of alpha-synuclein in submandibular glands of patients with idiopathic rapid-eye-movement sleep behaviour disorder: A case-control study: Lancet Neurol, 2016; 15; 708-18
2. Altman MT, Knauert MP, Pisani MA, Sleep disturbance after hospitalization and critical illness: A systematic review: Ann Am Thorac Soc, 2017; 14; 1457-68
3. Bin Abdulhak AA, Baddour LM, Erwin PJ, Global and regional burden of infective endocarditis, 1990–2010: A systematic review of the literature: Glob Heart, 2014; 9; 131-43
4. Slipczuk L, Codolosa JN, Davila CD, Infective endocarditis epidemiology over five decades: A systematic review: PLoS One, 2013; 8; e82665
5. Kent BD, McNicholas WT, Ryan S, Insulin resistance, glucose intolerance and diabetes mellitus in obstructive sleep apnoea: J Thorac Dis, 2015; 7; 1343-57
6. Poroyko VA, Carreras A, Khalyfa A, Chronic sleep disruption alters gut microbiota, induces systemic and adipose tissue inflammation and insulin resistance in mice: Sci Rep, 2016; 6; 35405
7. Okun ML, Coussons-Read M, Hall M, Disturbed sleep is associated with increased C-reactive protein in young women: Brain Behav Immun, 2009; 23; 351-54
8. Simpson N, Dinges DF, Sleep and inflammation: Nutr Rev, 2007; 65; S244-52
9. Taheri S, Austin D, Lin L, Correlates of serum C-reactive protein (CRP) – no association with sleep duration or sleep disordered breathing: Sleep, 2007; 30; 991-96
10. Guilleminault C, Kirisoglu C, Ohayon MM, C-reactive protein and sleep-disordered breathing: Sleep, 2004; 27; 1507-11
11. Habib G, Lancellotti P, Antunes MJ, 2015 ESC Guidelines for the management of infective endocarditis: The Task Force for the Management of Infective Endocarditis of the European Society of Cardiology (ESC). Endorsed by: European Association for Cardio-Thoracic Surgery (EACTS), the European Association of Nuclear Medicine (EANM): Eur Heart J, 2015; 36; 3075-128
12. de la Vega R, Tome-Pires C, Sole E, The Pittsburgh Sleep Quality Index: Validity and factor structure in young people: Psychol Assess, 2015; 27; e22-27
13. Liu X, Tang M, Hu L, Reliability and validity of the Pittsburgh sleep quality index: Chinese J Psychiatr, 1996; 29; 103-7
14. Buysse DJ, Hall ML, Strollo PJ, Relationships between the Pittsburgh Sleep Quality Index (PSQI), Epworth Sleepiness Scale (ESS), and clinical/polysomnographic measures in a community sample: J Clin Sleep Med, 2008; 4; 563-71
15. Guideline for primary care of adult obstructive sleep apnea (2018): Chinese J Gen Pract, 2019; 18; 21-29 [in Chinese]
16. Redeker NS, Hedges C, Sleep during hospitalization and recovery after cardiac surgery: J Cardiovasc Nurs, 2002; 17; 56-68 quiz 82–83
17. Caruana N, McKinley S, Elliott R, Gholizadeh L, Sleep quality during and after cardiothoracic intensive care and psychological health during recovery: J Cardiovasc Nurs, 2018; 33; E40-49
18. Liao WC, Huang CY, Huang TY, Hwang SL, A systematic review of sleep patterns and factors that disturb sleep after heart surgery: J Nurs Res, 2011; 19; 275-88
19. Crönlein T, Lehner A, Schüssler P, Changes in subjective-objective sleep discrepancy following inpatient cognitive behavior therapy for insomnia: Behav Ther, 2019; 50; 994-1001
20. Volkovich E, Tikotzky L, Manber R, Objective and subjective sleep during pregnancy: Links with depressive and anxiety symptoms: Arch Womens Ment Health, 2016; 19; 173-81
21. Klumpp H, Roberts J, Kapella MC, Subjective and objective sleep quality modulate emotion regulatory brain function in anxiety and depression: Depress Anxiety, 2017; 34; 651-60
22. Hughes JM, Song Y, Fung CH, Measuring sleep in vulnerable older adults: A comparison of subjective and objective sleep measures: Clin Gerontol, 2018; 41; 145-57
23. De Crescenzo F, Licchelli S, Ciabattini M, The use of actigraphy in the monitoring of sleep and activity in ADHD: A meta-analysis: Sleep Med Rev, 2016; 26; 9-20
24. Quante M, Kaplan ER, Cailler M, Actigraphy-based sleep estimation in adolescents and adults: A comparison with polysomnography using two scoring algorithms: Nat Sci Sleep, 2018; 10; 13-20
25. Korotinsky A, Assefa SZ, Diaz-Abad M, Comparison of American Academy of Sleep Medicine (AASM) versus Center for Medicare and Medicaid Services (CMS) polysomnography (PSG) scoring rules on AHI and eligibility for continuous positive airway pressure (CPAP) treatment: Sleep Breath, 2016; 20; 1169-74
26. Guo S, Sun W, Liu C, Wu S, Structural validity of the Pittsburgh Sleep Quality Index in Chinese undergraduate students: Front Psychol, 2016; 7; 1126
27. Janssen KC, Phillipson S, O’Connor J, Johns MW, Validation of the Epworth Sleepiness Scale for Children and Adolescents using Rasch analysis: Sleep Med, 2017; 33; 30-35
28. Park SY, Oh MK, Lee BS, The effects of alcohol on quality of sleep: Korean J Fam Med, 2015; 36; 294-99
29. Wang M, Wei J, Yang X, The level of IL-6 was associated with sleep disturbances in patients with major depressive disorder: Neuropsychiatr Dis Treat, 2019; 15; 1695-700
30. Gamsiz-Isik H, Kiyan E, Bingol Z, Does obstructive sleep apnea increase the risk for periodontal disease? A case-control study: J Periodontol, 2017; 88; 443-49
31. Kline CE, Hall MH, Buysse DJ, Poor sleep quality is associated with insulin resistance in postmenopausal women with and without metabolic syndrome: Metab Syndr Relat Disord, 2018; 16; 183-89
32. Okamura T, Hashimoto Y, Hamaguchi M, Short sleep duration is a risk of incident nonalcoholic fatty liver disease: A population-based longitudinal study: J Gastrointestin Liver Dis, 2019; 28; 73-81
33. Sookoian S, Pirola CJ, Obstructive sleep apnea is associated with fatty liver and abnormal liver enzymes: A meta-analysis: Obes Surg, 2013; 23; 1815-25
34. Sayin FK, Buyukinan M, Sleep duration and media time have a major impact on insulin resistance and metabolic risk factors in obese children and adolescents: Child Obes, 2016; 12; 272-78
35. Kim D, Ahmed A, Kushida C, Continuous positive airway pressure therapy on nonalcoholic fatty liver disease in patients with obstructive sleep apnea: J Clin Sleep Med, 2018; 14; 1315-22
Figures
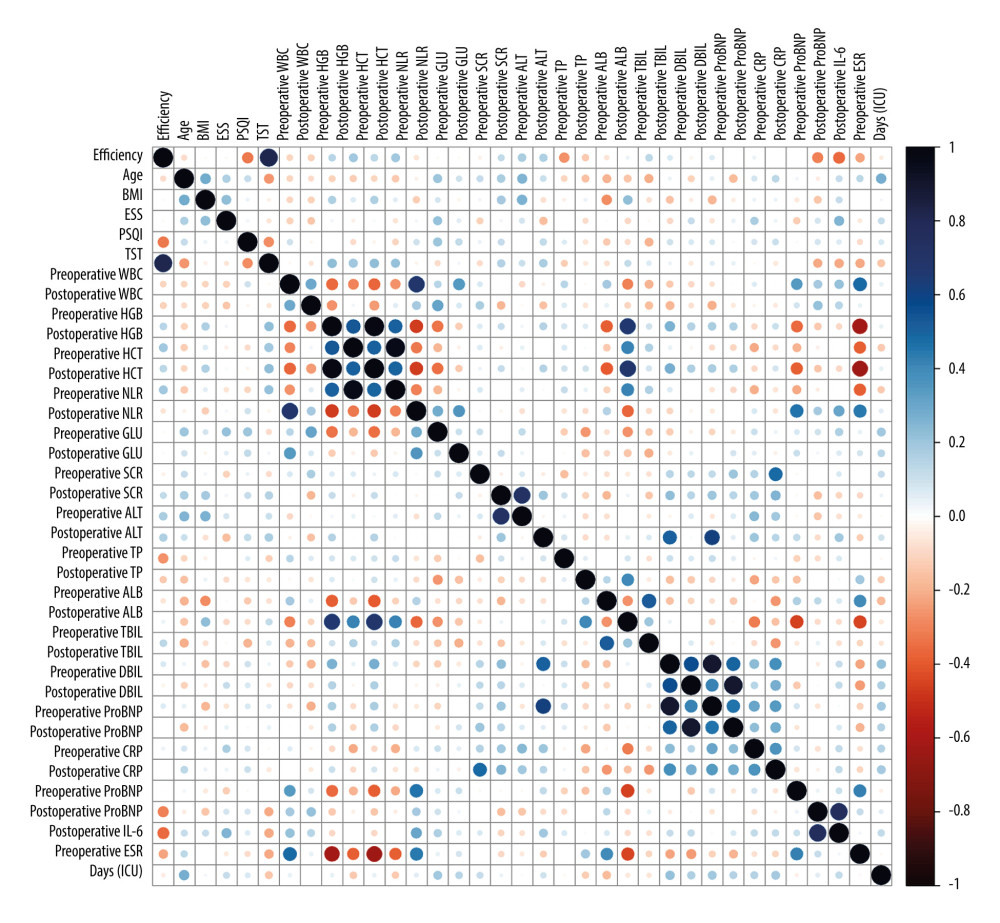 Figure 1. Heat map analysis of factors related to sleep disorders. Statistical analysis of correlation coefficients between sleep disorders and related factors. The color of the bars shows the statistical value. BMI – body mass index; ESS – Epworth Sleepiness Scale; PSQI – Pittsburgh Sleep Quality Index; TST – total sleep time; WBC – white blood count; HGB – hemoglobin; HCT – hematocrit; NLR – neutrophil to lymphocyte ratio; GLU – glucose; SCR – serum creatinine; ALT – alanine transaminase; TP – total protein; ALB – albumin; TBIL – total bilirubin; DBIL – direct-reacting bilirubin; ProBNP – pro-brain natriuretic peptide; CRP – C-reactive protein; IL-6 – interleukin 6; ESR – erythrocyte sedimentation rate; ICU – Intensive Care Unit.
Figure 1. Heat map analysis of factors related to sleep disorders. Statistical analysis of correlation coefficients between sleep disorders and related factors. The color of the bars shows the statistical value. BMI – body mass index; ESS – Epworth Sleepiness Scale; PSQI – Pittsburgh Sleep Quality Index; TST – total sleep time; WBC – white blood count; HGB – hemoglobin; HCT – hematocrit; NLR – neutrophil to lymphocyte ratio; GLU – glucose; SCR – serum creatinine; ALT – alanine transaminase; TP – total protein; ALB – albumin; TBIL – total bilirubin; DBIL – direct-reacting bilirubin; ProBNP – pro-brain natriuretic peptide; CRP – C-reactive protein; IL-6 – interleukin 6; ESR – erythrocyte sedimentation rate; ICU – Intensive Care Unit.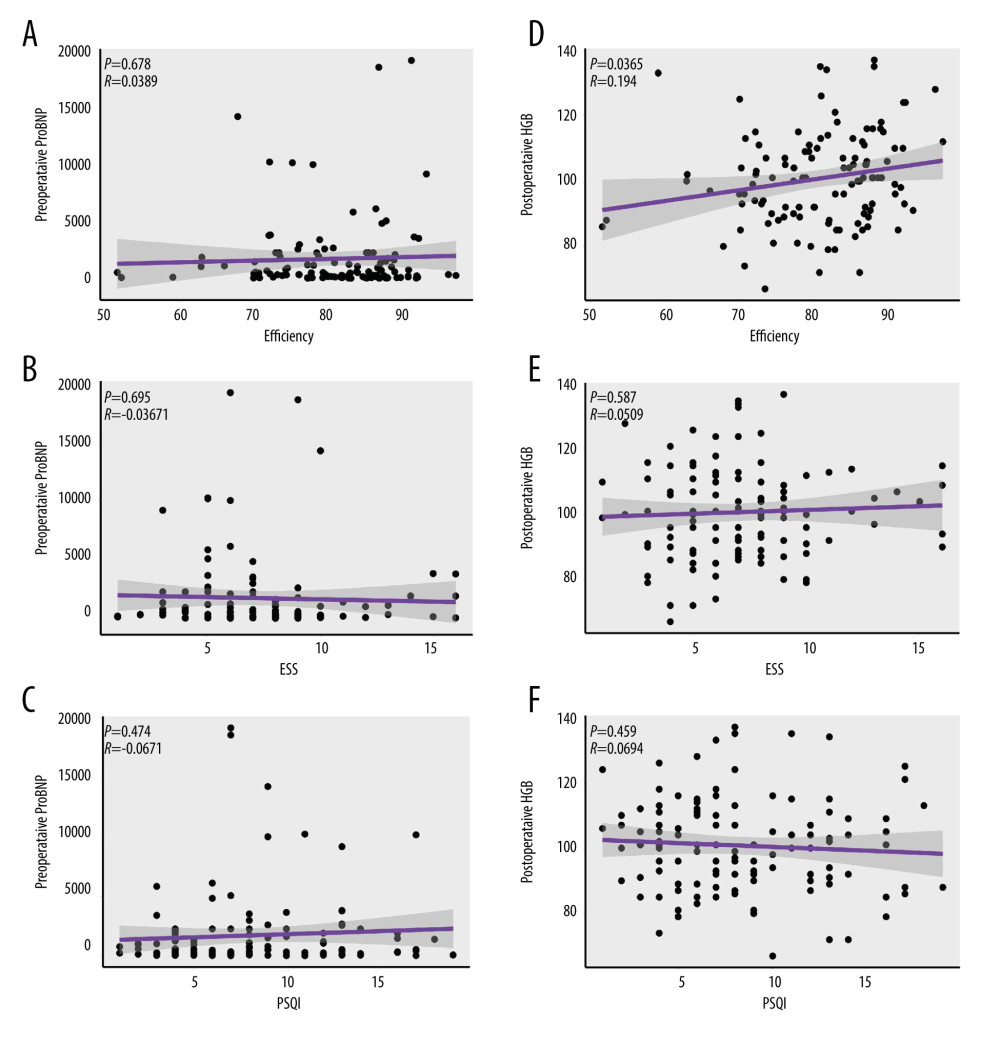 Figure 2. Correlation analysis between preoperative pro-brain natriuretic peptide and (A) sleep efficiency, (B) Epworth Sleepiness Scale (ESS), and (C) Pittsburgh Sleep Quality Index (PSQI), and (D) postoperative Hb and sleep efficiency, (E) Epworth Sleepiness Scale, and PSQI (F). PSQI – Pittsburgh Sleep Quality Index, ESS – Epworth Sleepiness Scale; ProBNP – pro-brain natriuretic peptide; HGB – hemoglobin.
Figure 2. Correlation analysis between preoperative pro-brain natriuretic peptide and (A) sleep efficiency, (B) Epworth Sleepiness Scale (ESS), and (C) Pittsburgh Sleep Quality Index (PSQI), and (D) postoperative Hb and sleep efficiency, (E) Epworth Sleepiness Scale, and PSQI (F). PSQI – Pittsburgh Sleep Quality Index, ESS – Epworth Sleepiness Scale; ProBNP – pro-brain natriuretic peptide; HGB – hemoglobin. Tables
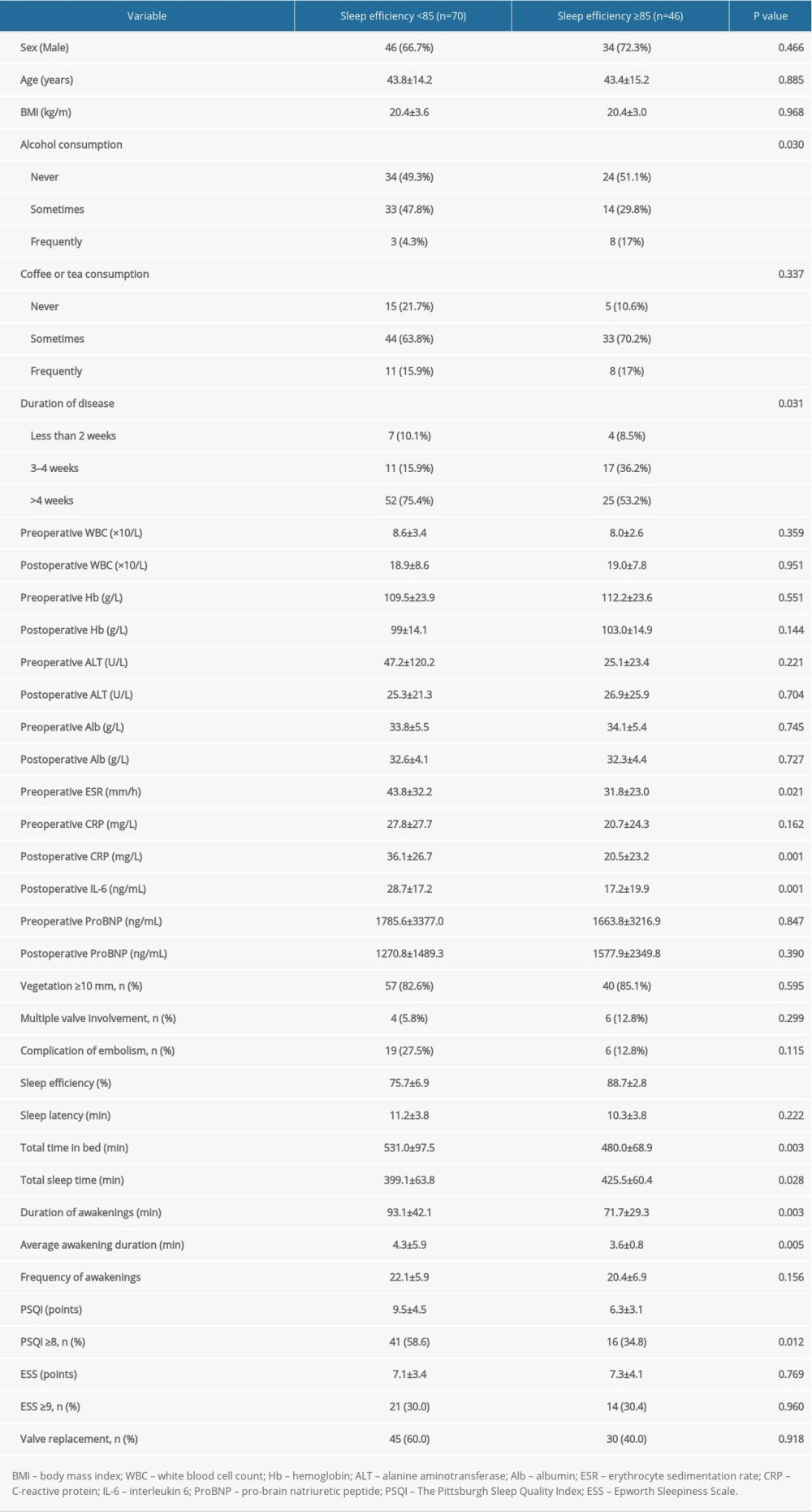 Table 1. Analysis of clinical features of patients with infective endocarditis according to sleep efficiency (n=116).
Table 1. Analysis of clinical features of patients with infective endocarditis according to sleep efficiency (n=116).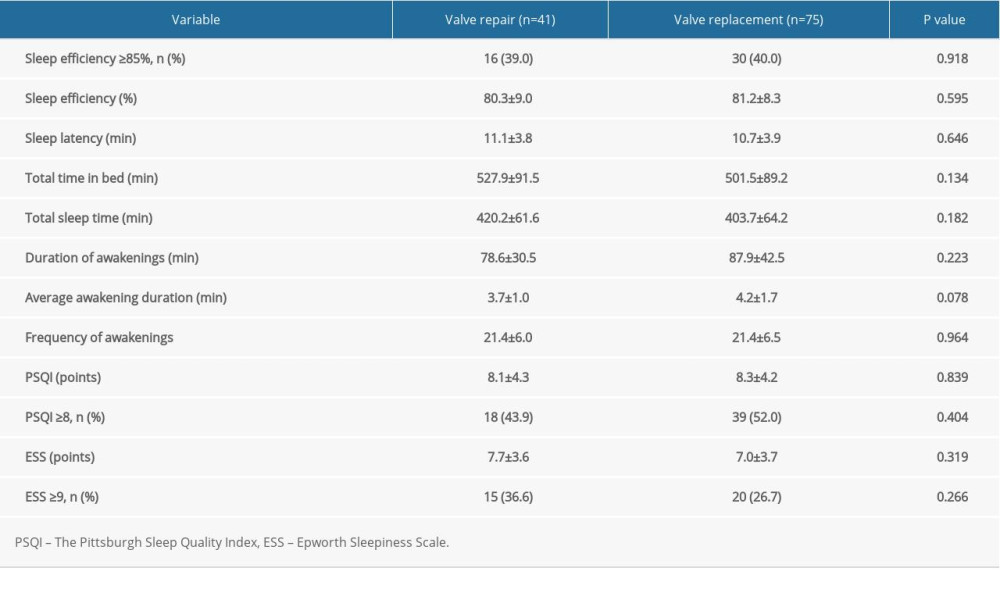 Table 2. Sleep characteristics of patients undergoing different types of cardiac surgery.
Table 2. Sleep characteristics of patients undergoing different types of cardiac surgery.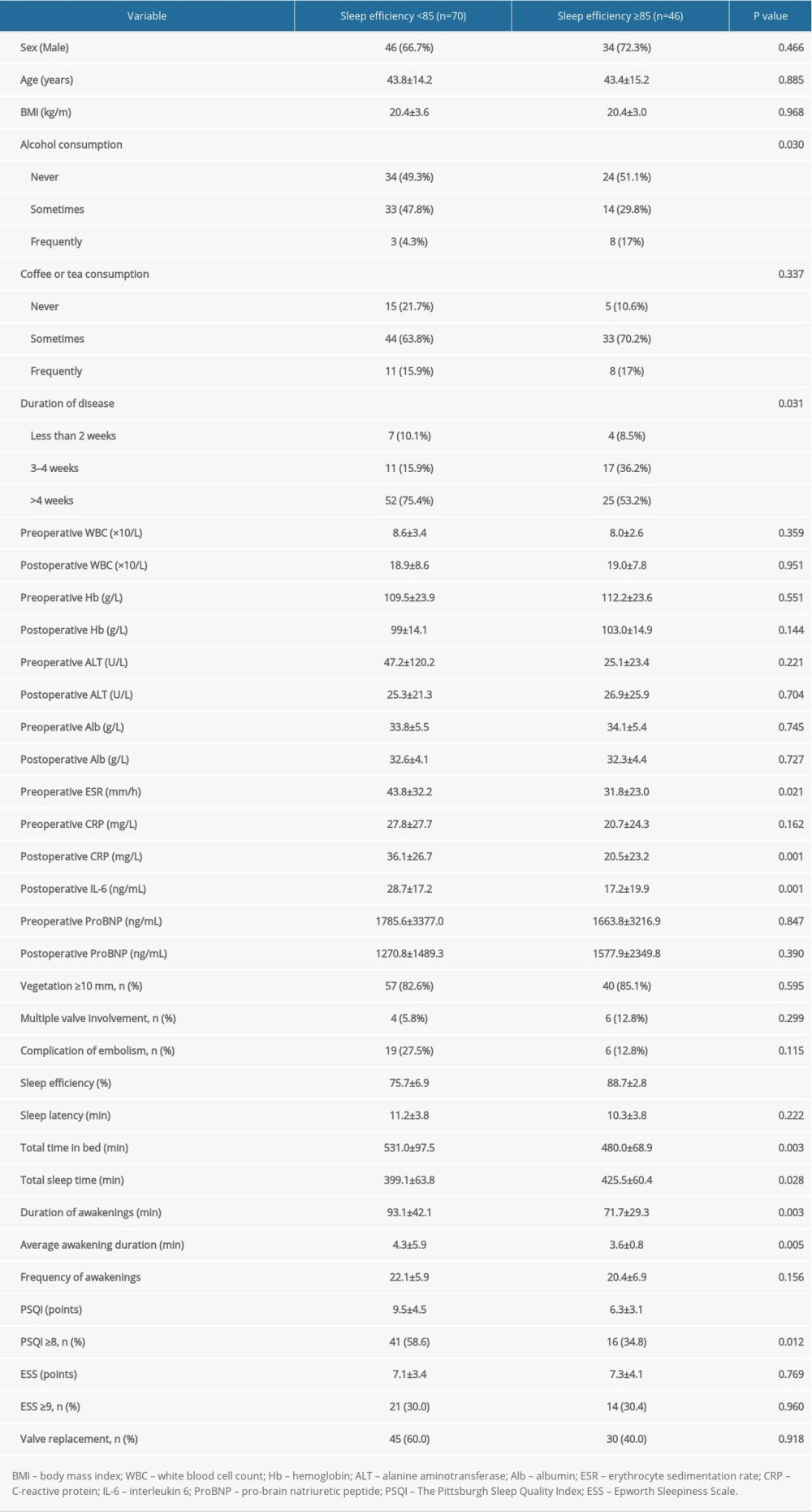 Table 1. Analysis of clinical features of patients with infective endocarditis according to sleep efficiency (n=116).
Table 1. Analysis of clinical features of patients with infective endocarditis according to sleep efficiency (n=116).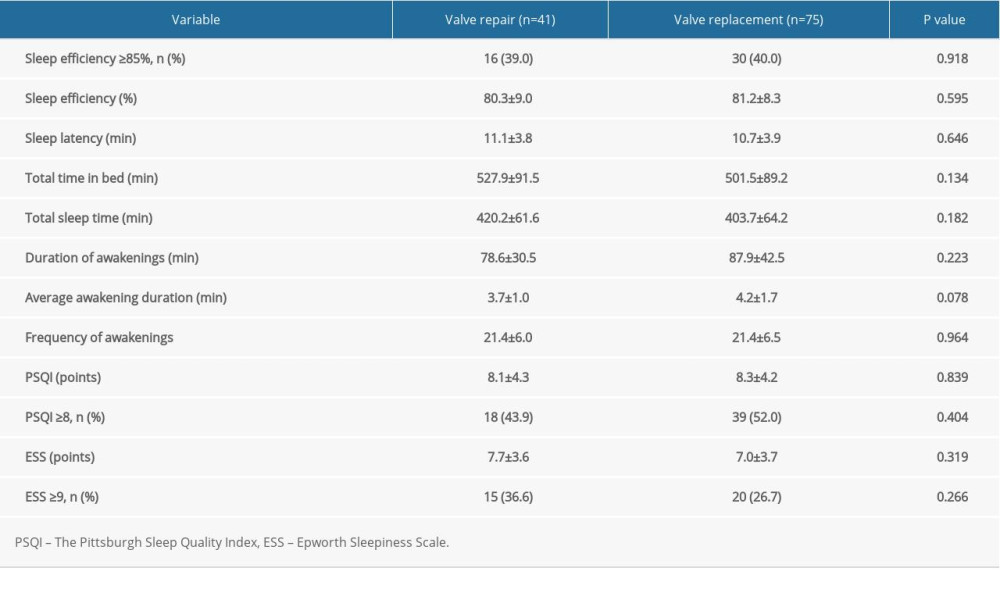 Table 2. Sleep characteristics of patients undergoing different types of cardiac surgery.
Table 2. Sleep characteristics of patients undergoing different types of cardiac surgery. In Press
06 Mar 2024 : Clinical Research
Comparison of Outcomes between Single-Level and Double-Level Corpectomy in Thoracolumbar Reconstruction: A ...Med Sci Monit In Press; DOI: 10.12659/MSM.943797
21 Mar 2024 : Meta-Analysis
Economic Evaluation of COVID-19 Screening Tests and Surveillance Strategies in Low-Income, Middle-Income, a...Med Sci Monit In Press; DOI: 10.12659/MSM.943863
10 Apr 2024 : Clinical Research
Predicting Acute Cardiovascular Complications in COVID-19: Insights from a Specialized Cardiac Referral Dep...Med Sci Monit In Press; DOI: 10.12659/MSM.942612
06 Mar 2024 : Clinical Research
Enhanced Surgical Outcomes of Popliteal Cyst Excision: A Retrospective Study Comparing Arthroscopic Debride...Med Sci Monit In Press; DOI: 10.12659/MSM.941102
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








