09 June 2021: Clinical Research
Prospective, Single-Center Comparison of Transcranial Direct Current Stimulation Plus Electroacupuncture and Standard Analgesia in Patients After Total Knee Arthroplasty: Effect on Rehabilitation and Functional Recovery
Xuejing Li1ABCEF, Wei Yu1BCEF, Hongbo Li2BCEF, Baoyue Wang3BEF, Jiang Xu1ACEFG*DOI: 10.12659/MSM.930363
Med Sci Monit 2021; 27:e930363
Abstract
BACKGROUND: The aim of this prospective study was to compare transcranial direct current stimulation (tDCS) plus electroacupuncture with standard analgesia in patients after total knee arthroplasty (TKA) to determine the effects on rehabilitation and functional recovery.
MATERIAL AND METHODS: Eighty patients with osteoarthritis of the knee who underwent TKA were included in the study. They were divided into experimental (n=40) and control groups (n=40) according to postoperative analgesia method. The control group received multimodal analgesia after TKA and the experimental group received additional tDCS plus electroacupuncture. Postoperative pain, knee function, and quality of life were compared between the 2 groups.
RESULTS: Compared with the control group, the experimental group had significantly lower visual analog scale scores at 3 and 7 days and 3 and 6 weeks after TKA (P<0.05). At 6 weeks after TKA, knee injury and osteoarthritis outcome and Hospital for Special Surgery scores and maximum knee flexion in the experimental group were significantly better than those in the control group (P<0.05). In the experimental group compared with the control group, the Short Form-36 Health Survey score also was significantly increased (P<0.05).
CONCLUSIONS: The findings from this study showed that tDCS plus electroacupuncture effectively reduced pain after TKA and improved rehabilitation and functional recovery.
Keywords: Arthroplasty, Replacement, Knee, chronic pain, Electroacupuncture, Rehabilitation, Transcranial Magnetic Stimulation, Analgesia, Analgesia, Patient-Controlled, Analgesics, Opioid, Knee Joint, pain management, Pain, Postoperative, Postoperative Period, Prospective Studies, Quality of Life, Range of Motion, Articular, Recovery of Function, Transcranial Direct Current Stimulation
Background
Osteoarthritis of the knee is a chronic, degenerative joint disease caused by a variety of factors and its prevalence increases with age [1]. Worldwide, it is estimated that 9.6% of men and 18.0% of women aged ≥60 years have symptomatic osteoarthritis [2]. In China, the age at onset of osteoarthritis tends to be younger, with a prevalence of approximately 12% in people aged >45 years [3]. Osteoarthritis is a leading cause of chronic pain and disability, which results in an overall decrease in quality of life (QOL) and an increased risk of depression and anxiety [4]. If the trend toward population aging continues, osteoarthritis could become the fourth most disabling disease in the world [2,5].
Total knee arthroplasty (TKA) is an effective treatment for end-stage knee arthritis [6]. The main goals for it are reduction in pain symptoms, improvement in knee function, and correction of joint deformity, which all improve patient QOL [6]. Guidelines for rehabilitation after TKA state that early rehabilitation training is essential to improve outcomes [7]. However, unexplained pain after TKA is one of the most common complications, and even with adequate multimodal analgesic regimens, some patients still have visual analog scale (VAS) scores for pain >8, which often are accompanied by insomnia and emotional problems [8,9]. Pain also can make it impossible for a patient to perform flexion and extension exercises at the optimal time, and lead to joint adhesion, seriously affecting the recovery of joint function [10]. Therefore, further improvement in control of postoperative pain is essential for rehabilitation of patients who have undergone TKA.
Recent studies have shown that transcranial direct current stimulation (tDCS) may have significant value in the treatment of chronic pain disorders [11,12]. Studies suggest that tDCS can reduce pain by regulating thalamic inhibitory networks and intervening in cortico-cortical as well as cortico-subcortical synaptic contacts related to pain formation [13,14]. Recent studies also have confirmed that preoperative central sensitization is a risk factor for persistent pain after TKA in patients with osteoarthritis of the knee [15]. Therefore, tDCS treatment maybe effective for unexplained pain after TKA. Previous studies by Khedr et al showed that tDCS reduced opioid requirements after TKA [16]. Electroacupuncture has been confirmed to be another effective non-drug analgesic treatment for postoperative pain [17], and it also improves muscle nerve function, prevents amyotrophy, and has anti-inflammatory and other effects [18,19]. For osteoarthritis knee pain, electroacupuncture treatment has been shown to have good analgesic effects [5,18]. However, few studies have evaluated the analgesic effect of tDCS plus electroacupuncture, particularly in TKA. Therefore, the aim of the present prospective study was to compare tDCS plus electroacupuncture with standard analgesia in patients after TKA and the effects on their rehabilitation and functional recovery.
Material and Methods
ETHICS STATEMENT:
The study was approved by the Ethics Committee of Huai’an Hospital (no. HA201901A). All patients provided written informed consent.
PARTICIPANTS:
Eighty patients with osteoarthritis of the knee who underwent TKA at the Affiliated Huai’an Hospital of Xuzhou Medical University between June 2019 and June 2020 were included in the present study. Patients were included if they: had severe osteoarthritis according to the 2013 American College of Physicians guidelines for the treatment of knee arthritis [20]; had unilateral knee chronic pain with dysfunction, and conservative treatment was ineffective; met preoperative American Society of Anesthesiologists preoperative grading criteria I–II; signed informed consent before surgery; and had undergone TKA using an anterior midline incision and a medial approach to the patella, which was completed by the same group of surgeons. Patients were excluded if they: were aged <50 or >85 years; had a history of drug dependence or drug allergy to narcotic drugs; had significant abnormalities in preoperative liver and kidney function; had a history of stroke or neuropsychiatric disease; had uncontrolled angina pectoris or bundle branch block (QT prolongation); had a history of severe gastric ulcer or severe gastrointestinal disease; had a coagulation dysfunction; had a fixed deformity or severe ligament instability; or were unable to cooperate with exercise after surgery.
POSTOPERATIVE ANALGESIA:
All patients received multimodal analgesia 48 h after surgery. Before the procedure was completed, the patients received a 1- to 2-mg dose of morphine, which was injected by the anesthesiologist into the epidural space. Postoperatively, all patients had an indwelling epidural analgesia pump. The specific analgesic formula included morphine, ropivacaine, and droperidol in a 96-mL 0.9% sodium chloride solution. The specific doses of morphine, ropivacaine, and droperidol depended upon a patient’s weight, age, sex, and other factors. The conventional administration rate was 2 mL/h, the patient-controlled volume was 0.5 mL/15 min, and the total postoperative analgesic time was 48 h. The day after surgery, routine oral administration of celecoxib capsules, 200 mg twice daily, was begun.
ELECTROACUPUNCTURE THERAPY:
The experimental group was treated with electroacupuncture after surgery. The locations selected, all on the same side as the TKA, were Liangqiu (ST 34), Xuehai (SP 10), Yinlingquan (SP9), Zusanli (ST 36), Fenglong (ST 40), and Qiuxu (GB 40). Liangqiu is located between the rectus femoris and vastus lateralis, about 6.7 cm above the basis patella. Xuehai is on the upper edge of the medial epicondyle of the femur, about 6.7 cm above the medial end of the basis patella. Yinlingquan is between the posterior border of the tibia and the gastrocnemius muscle, above the origin of the soleus muscle. Zusanli is located between the tibialis anterior and long extensor muscle digits. Fenglong is located approximately 26.6 cm above the external malleolus. Qiuxu is located at the origin of the musculus extensor digitorum brevis.
The same acupuncture physician completed every acupuncture operation, under strict aseptic conditions. The disposable acupuncture needle was removed and soaked in 75% ethanol for 30 min and then removed with a sterile needle holder, wiped with sterile gauze, and placed in a disposable dressing change pack for future use. Next, while wearing disposable sterile gloves, the operator exposed the acupuncture site. The dressing change pack then was opened and a sterile forceps was used to grasp 75% ethanol cotton balls, which were used to disinfect the skin around the acupuncture site. Disinfection was repeated 3 times. After each swab, a sterile towel was placed. For each puncture, the same type and brand of acupuncture needle was used (0.25×25 mm, 0.25×40 mm), along with a Hwato SDZ-II Electro Acupuncture Stimulator (Sichuan Changhong Electric Co., Ltd., Mianyang, Sichuan, China). Using a direct puncture, the needle was inserted 25 to 40 mm, and Liangqiu (ST 34) and Xuehai (SP 10), Yinlingquan (SP9) and Zusanli (ST 36), and Fenglong (ST 40), and Qiuxu (GB 40) each were connected to a pair of electrodes, using dense waves at a frequency of 2 Hz/100 Hz and a current intensity of 2 to 5 mA, which was tolerable for patients. Each session of acupuncture plus tDSC lasted 30 min and sessions were held once a day for 6 weeks, for a total of 42 sessions.
TRANSCRANIAL DIRECT CURRENT STIMULATION:
The IS200 transcranial direct current stimulator (Sichuan Changhong Electric Co., Ltd., Mianyang, Sichuan, China) was used. The stimulation time was 20 min, the current intensity was 1.5 mA, and the electrode pad area was 35 cm2. The electrode pad was inserted into the sponge pad and the pad was soaked with sterilized water for injection; different sponge pads were used for each patient. The anode stimulated the M1 area of the left main motor area, which was equivalent to the C3 area use with the electrode placement method, and the cathode was placed on the shoulder. The current intensity was gradually increased to 1.5 mA and anodal stimulation was continued for 20 min. Stimulation was performed once a day for 5 days per week over a 6-week period, for a total of 30 sessions.
REHABILITATION TRAINING:
Rehabilitation training consisted of exercise for muscle strength and joint range of motion and partial weight-bearing training.
To build muscle strength, patients were instructed to perform ankle pump exercises after the anesthetic effect wore off, which was approximately 6 h after surgery. The day after surgery, they performed long contractile training of the quadriceps femoris and hip muscles and increased the intensity of muscle strength training according to their individual circumstances. Two days after surgery, the drainage tube was removed and joint range of motion training was begun by bending a patient’s foot to the buttock. The initial training angle was set at 0° to 30° and the flexion range of motion was increased by 10° every day. Each movement cycle was 60 to 80 s and the movements were performed for 1 h twice a day; 1 week later, knee flexion had reached 90°. Three days after surgery, patients were assisted in performing seated knee extension and flexion exercises to maintain knee flexion; leg extension and elevation were performed for 5 s each. Fifteen repetitions each of the knee extension and flexion exercises and leg extension and elevation were considered a single cycle and 3 cycles were performed each day. One week after surgery, patients were helped to stand and to walk. The first transfer of the center of gravity to the unaffected side was performed for 10 s and the position held for 10 s. Patients also practiced walking on a flat surface with the help of a walker and slowly increased their walking load. The progression of all of the training was based on each patient’s tolerance for the movements and exercises.
PAIN:
A VAS was used to evaluate the severity of knee pain in patients [21]. Their VAS scores ranged from mild to severe (0 to 10 points), depending upon their own subjective assessments.
KNEE FUNCTION:
Knee function before and after treatment was evaluated using the Knee Injury and Osteoarthritis Outcome Score (KOOS) [22], the Hospital for Special Surgery (HSS) score [23], and maximum degree of knee flexion.
QUALITY OF LIFE:
The Short Form-36 Health Survey (SF-36) [24] was used to evaluate patient QOL before and after treatment.
STATISTICAL ANALYSIS:
SPSS software, version 23.0 (SPSS, Inc., Chicago, Illinois, United States) was used to perform statistical analysis of the data. Numerical data were expressed as the number of cases (percentage) [n (%)], a chi-square test was performed in parallel, and α=0.05 was selected as the test level. The data measured in the study conformed to a normal distribution, expressed as means±standard deviations (±s), an independent sample
Results
The patients were divided into experimental (n=40) and control groups (n=40) according to postoperative analgesia method. Most patients were female (80% and 75%, respectively), with a mean age >65 years. There were no significant differences between the groups in sex, age, disease course, body mass index, TKA operation time, or other baseline data (
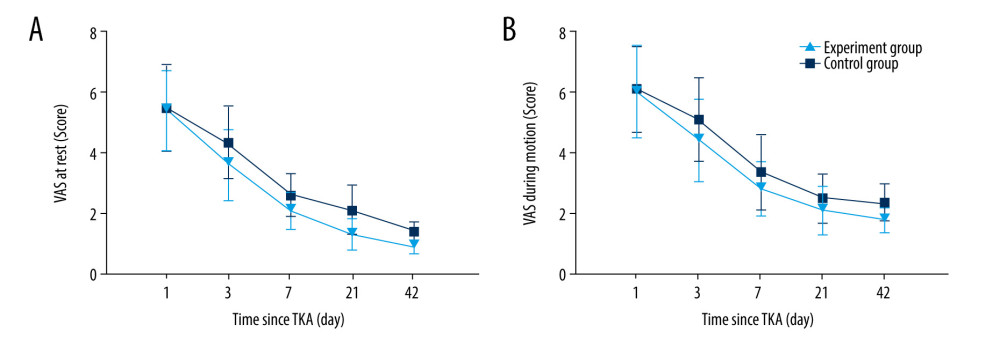
Using VAS scores, we assessed the degree of pain in patients while resting and active on days 1, 3, and 7 and at weeks 3 and 6 after TKA. The results showed a trend of decreasing VAS scores after TKA in both groups (Figure 1). Compared with the control group, the experimental group had significantly lower VAS scores at all time points after TKA when the scores were assessed (
We assessed knee function before and 6 weeks after TKA in both groups using the maximum degree of knee flexion and the KOOS and HSS scores. The results showed that before TKA, there was no significant difference between the groups in any of those measurements. At 6 weeks after TKA, the maximum knee curvature and KOOS and HSS scores had increased significantly in both groups (
Table 4 shows the differences in time spent out of bed postoperatively and lengths of hospital stay between the groups. Compared with the control group, in the experimental group, the time spent out of bed postoperatively was significantly longer and the hospital stay was significantly shorter (
We evaluated the QOL of patients before and 6 weeks after TKA using the SF-36 scale and found no significant differences between the groups before the procedure (
No complications related to tDCS or electroacupuncture were observed in any patients in the experimental group during the treatment period.
Discussion
tDCS is considered to be a promising type of postoperative analgesia [11,13]. Electroacupuncture combines acupuncture and electrical stimulation, and has been studied for use in childbirth, for analgesia, and to improve neuromuscular function [18,19]. In addition, studies have confirmed that electroacupuncture can block or reduce pain by regulating the expression of opioids, serotonin, and norepinephrine in the spinal cord and it can also increase the expression of endogenous anti-pain substances to produce central analgesia [25,26]. In the present study, we used a novel combination of tDCS and electroacupuncture for analgesia after TKA, with the aim of reducing pain and improving rehabilitation quality in patients who had undergone the surgery.
The results of the study showed that tDCS plus electroacupuncture had a significant analgesic effect after TKA. Compared with the control group, the experimental group had lower VAS score on days 3 and 7 and weeks 3 and 6 after TKA, indicating that the degree of knee pain was significantly reduced. Previous studies by Khedr et al [16] showed that tDCS reduced morphine consumption and pain after TKA, but there was no significant difference in VAS between real and sham tDCS. Our study, however, showed that VAS scores at different times after TKA in the experimental group were significantly lower than those in the control group, except on the first day after TKA. We believe that this may be due to the ability of tDCS with electroacupuncture to produce synergistic analgesia. tDCS acts on the central nervous system (CNS) and mainly intervenes in cortex-cortical and cortex-subcortical synaptic contacts related to pain formation to reduce pain [27]. Electroacupuncture, in contrast, exerts local analgesic effects by downregulating local tissue inflammatory mediators, histamine, and prostaglandins, and it has analgesic effects on the spinal cord and CNS [25,26].
Effective pain control significantly improves the quality of postoperative rehabilitation. The results of our study showed that, compared with the control group, the experimental group had significantly improved maximum knee flexion and KOOS and HSS scores at 6 weeks after surgery and significantly shorter time to ambulation and hospital stays. Previous studies have shown that controlling pain in patients after TKA results in better knee function 6 weeks after surgery [28,29]. Pain also is a key factor affecting postoperative mood and QOL in patients. We found that the experimental group had higher SF-36 scores 6 weeks after surgery, which indicates that their QOL was significantly improved.
In terms of safety, there were no complications related to tDCS or electroacupuncture during the trial, which indicates that combining them is safe. Previous studies have shown that tDCS is safe in children and pregnant women [30,31]. Also, risk of complications such as skin infection or puncture site bleeding with electroacupuncture is low when strict skin disinfection protocols are followed and the operation and needle insertion are performed by a skilled professional.
The present study was limited as it was performed in a single center and had a small sample size. The clinical characteristics of patients also may have resulted in selection bias; therefore, the ability to extrapolate from the results is limited. This was not a randomized controlled trial (RCT); therefore, the efficacy of tDCS plus electroacupuncture needs to be verified in a multicenter, prospective RCT with a large sample size.
Conclusions
The findings from the present study show that tDCS plus electroacupuncture effectively reduces pain following TKA and improves rehabilitation and functional recovery.
Tables
Table 1. Characteristics of all participants. Table 2. VAS scores in the 2 groups at different time points after TKA.
Table 2. VAS scores in the 2 groups at different time points after TKA.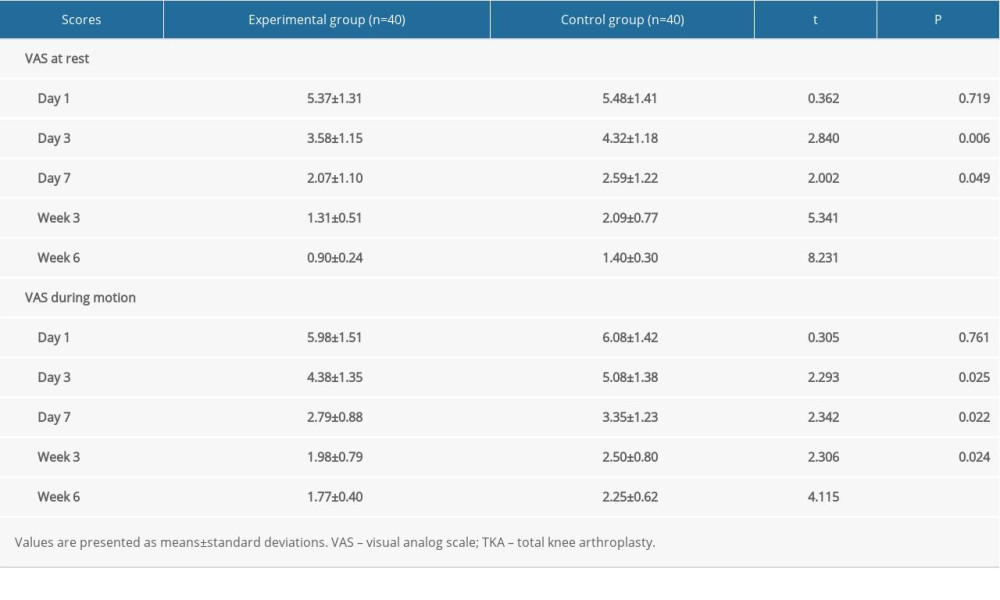 Table 3. Knee function in the 2 groups before and 6 weeks after TKA.
Table 3. Knee function in the 2 groups before and 6 weeks after TKA.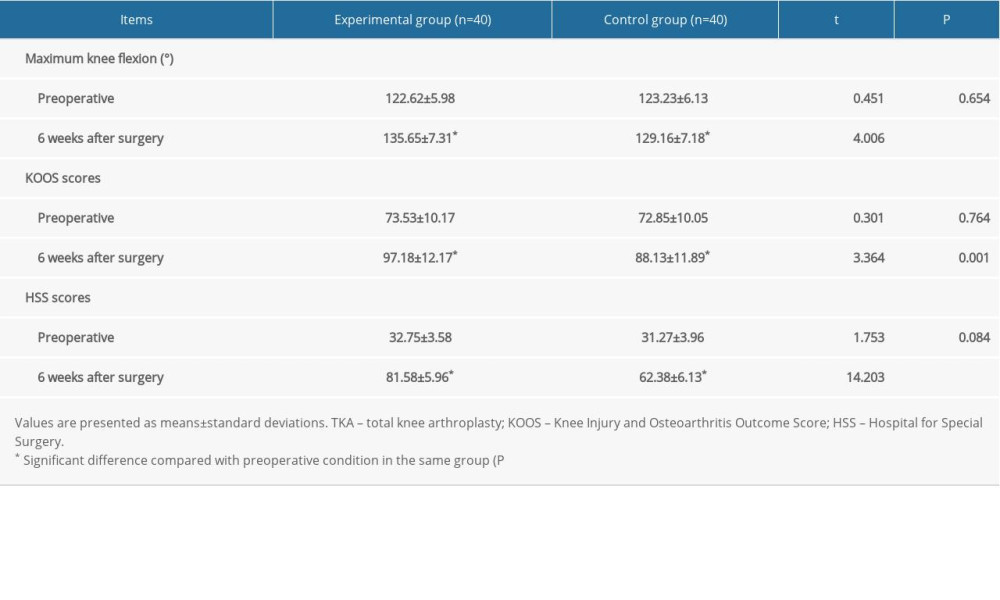 Table 4. Time spent out of bed and length of hospital stay in the 2 groups.
Table 4. Time spent out of bed and length of hospital stay in the 2 groups. Table 5. SF-36 scores in the 2 groups before and 6 weeks after TKA.
Table 5. SF-36 scores in the 2 groups before and 6 weeks after TKA.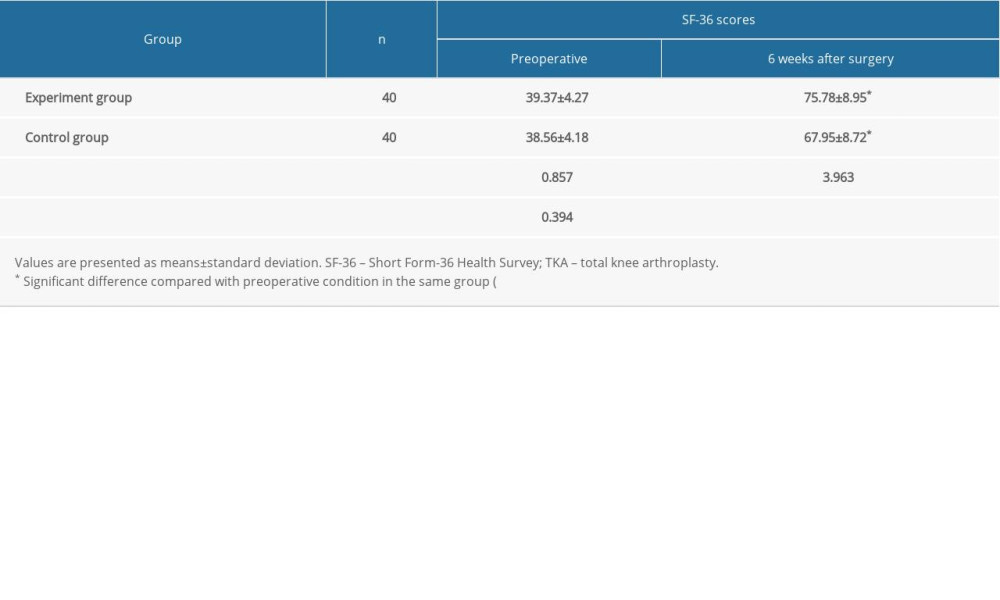
References
1. Glyn-Jones S, Palmer AJ, Agricola R, Osteoarthritis: Lancet, 2015; 386; 376-87
2. Nelson AE, Osteoarthritis year in review 2017: Clinical: Osteoarthritis Cartilage, 2018; 26; 319-25
3. Zeng SY, Gong Y, Zhang YP, Changes in the prevalence of rheumatic diseases in Shantou, China, in the Past three decades: A COPCORD study: PLoS One, 2015; 10; e0138492
4. Deveza LA, Loeser RF, Is osteoarthritis one disease or a collection of many?: Rheumatology (Oxford), 2018; 57; iv34-42
5. Litwic A, Edwards MH, Dennison EM, Epidemiology and burden of osteoarthritis: Br Med Bull, 2013; 105; 185-99
6. Macías-Hernández SI, Morones-Alba JD, Miranda-Duarte A, Glenohumeral osteoarthritis: overview, therapy, and rehabilitation: Disabil Rehabil, 2017; 39; 1674-82
7. Mistry JB, Elmallah RD, Bhave A, Rehabilitative guidelines after total knee arthroplasty: A review: J Knee Surg, 2016; 29; 201-17
8. Karlsen AP, Wetterslev M, Hansen SE, Postoperative pain treatment after total knee arthroplasty: A systematic review: PLoS One, 2017; 12; e0173107
9. Lewis GN, Rice DA, Mcnair PJ, Predictors of persistent pain after total knee arthroplasty: a systematic review and meta-analysis: Br J Anaesth, 2015; 114; 551-61
10. Rice DA, Kluger MT, Mcnair PJ, Persistent postoperative pain after total knee arthroplasty: A prospective cohort study of potential risk factors: Br J Anaesth, 2018; 121; 804-12
11. David M, Moraes AA, Costa MLD, Transcranial direct current stimulation in the modulation of neuropathic pain: A systematic review: Neurol Res, 2018; 40; 555-63
12. Zortea M, Ramalho L, Alves RL, Transcranial direct current stimulation to improve the dysfunction of descending pain modulatory system related to opioids in chronic non-cancer pain: An integrative review of neurobiology and meta-analysis: Front Neurosci, 2019; 13; 1218
13. Pinto CB, Teixeira Costa B, Duarte D, Transcranial direct current stimulation as a therapeutic tool for chronic pain: J ECT, 2018; 34; e36-50
14. Castelo-Branco L, Uygur Kucukseymen E, Duarte D, Optimised transcranial direct current stimulation (tDCS) for fibromyalgia-targeting the endogenous pain control system: A randomised, double-blind, factorial clinical trial protocol: BMJ Open, 2019; 9; e032710
15. Kim SH, Yoon KB, Yoon DM, Influence of centrally mediated symptoms on postoperative pain in osteoarthritis patients undergoing total knee arthroplasty: A prospective observational evaluation: Pain Pract, 2015; 15; E46-53
16. Khedr EM, Sharkawy ESA, Attia AMA, Role of transcranial direct current stimulation on reduction of postsurgical opioid consumption and pain in total knee arthroplasty: Double randomized clinical trial: Eur J Pain, 2017; 21; 1355-65
17. Li X, Dai Q, Shi Z, Clinical efficacy and safety of electroacupuncture in migraine treatment: A systematic review and network meta-analysis: Am J Chin Med, 2019; 47; 1755-80
18. Chen J, Liu XX, Tackling osteoarthritic knee pain with electroacupuncture: Chin J Integr Med, 2018; 24; 803-5
19. Liu PR, Cao F, Zhang Y, Electroacupuncture reduces astrocyte number and oxidative stress in aged rats with surgery-induced cognitive dysfunction: J Int Med Res, 2019; 47; 3860-73
20. Croke LM, Treatment of knee osteoarthritis: A clinical practice guideline from the AAOS: Am Fam Physician, 2014; 89; 918-20
21. Sung YT, Wu JS, The Visual Analogue Scale for Rating, Ranking and Paired-Comparison (VAS-RRP): A new technique for psychological measurement: Behav Res Methods, 2018; 50; 1694-715
22. Collins NJ, Prinsen CA, Christensen R, Knee Injury and Osteoarthritis Outcome Score (KOOS): Systematic review and meta-analysis of measurement properties: Osteoarthritis Cartilage, 2016; 24; 1317-29
23. Keeney LG, Hargett MJ, Liguori GA, Charles Burstein, MD: First director of anesthesiology at hospital for special surgery: J Anesth Hist, 2018; 4; 171-76
24. Gornet MF, Copay AG, Sorensen KM, Assessment of health-related quality of life in spine treatment: Conversion from SF-36 to VR-12: Spine J, 2018; 18; 1292-97
25. Zhang R, Lao L, Ren K, Mechanisms of acupuncture-electroacupuncture on persistent pain: Anesthesiology, 2014; 120; 482-503
26. Bianco G, Fascial neuromodulation: An emerging concept linking acupuncture, fasciology, osteopathy and neuroscience: Eur J Transl Myol, 2019; 29; 8331
27. Ahn H, Woods AJ, Kunik ME, Efficacy of transcranial direct current stimulation over primary motor cortex (anode) and contralateral supraorbital area (cathode) on clinical pain severity and mobility performance in persons with knee osteoarthritis: An experimenter- and participant-blinded, randomized, sham-controlled pilot clinical study: Brain Stimul, 2017; 10; 902-9
28. Chughtai M, Elmallah RD, Mistry JB, Nonpharmacologic pain management and muscle strengthening following total knee arthroplasty: J Knee Surg, 2016; 29; 194-200
29. Rutherford RW, Jennings JM, Dennis DA, Enhancing recovery after total knee arthroplasty: Orthop Clin North Am, 2017; 48; 391-400
30. Vigod S, Dennis CL, Daskalakis Z, Transcranial direct current stimulation (tDCS) for treatment of major depression during pregnancy: Study protocol for a pilot randomized controlled trial: Trials, 2014; 15; 366
31. Vigod SN, Murphy KE, Dennis CL, Transcranial direct current stimulation (tDCS) for depression in pregnancy: A pilot randomized controlled trial: Brain Stimul, 2019; 12; 1475-83
Tables
 Table 1. Characteristics of all participants.
Table 1. Characteristics of all participants.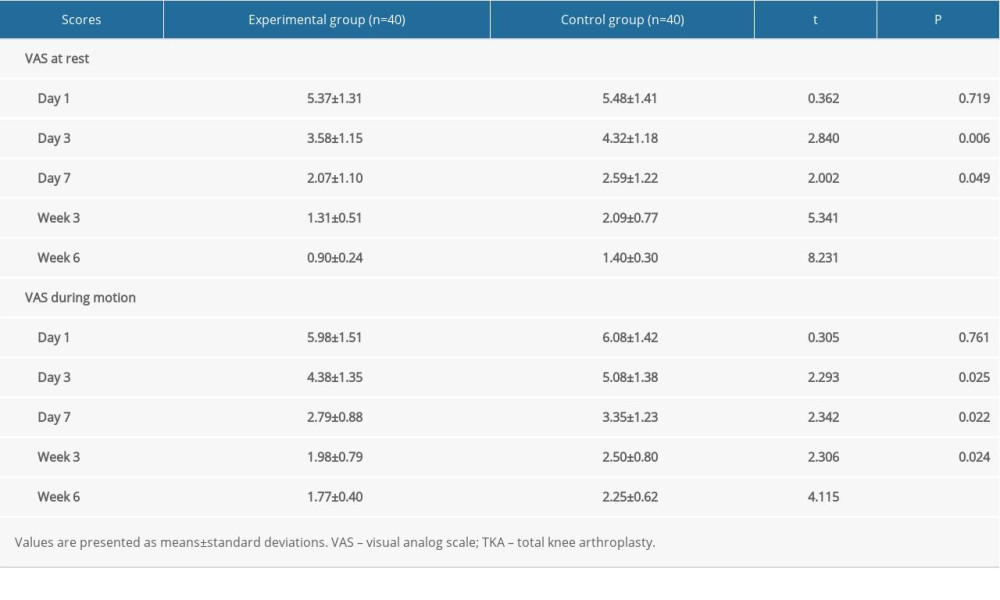 Table 2. VAS scores in the 2 groups at different time points after TKA.
Table 2. VAS scores in the 2 groups at different time points after TKA.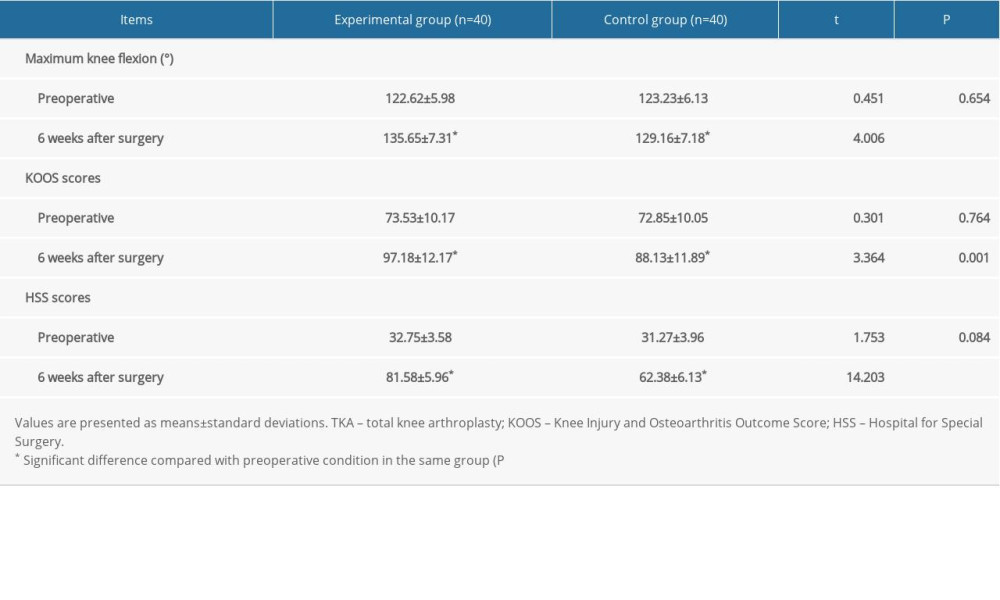 Table 3. Knee function in the 2 groups before and 6 weeks after TKA.
Table 3. Knee function in the 2 groups before and 6 weeks after TKA. Table 4. Time spent out of bed and length of hospital stay in the 2 groups.
Table 4. Time spent out of bed and length of hospital stay in the 2 groups.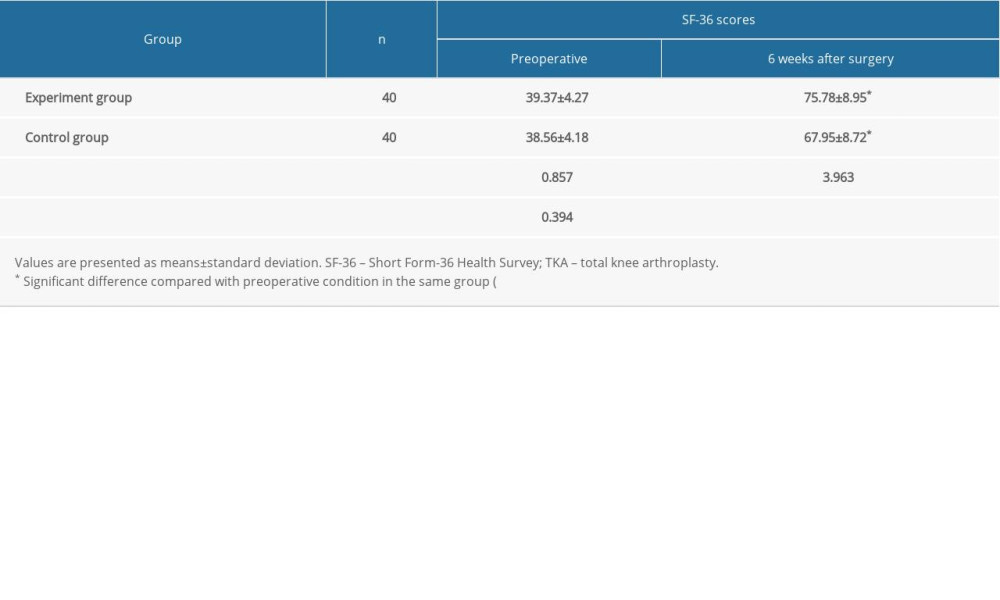 Table 5. SF-36 scores in the 2 groups before and 6 weeks after TKA.
Table 5. SF-36 scores in the 2 groups before and 6 weeks after TKA. Table 1. Characteristics of all participants.
Table 1. Characteristics of all participants.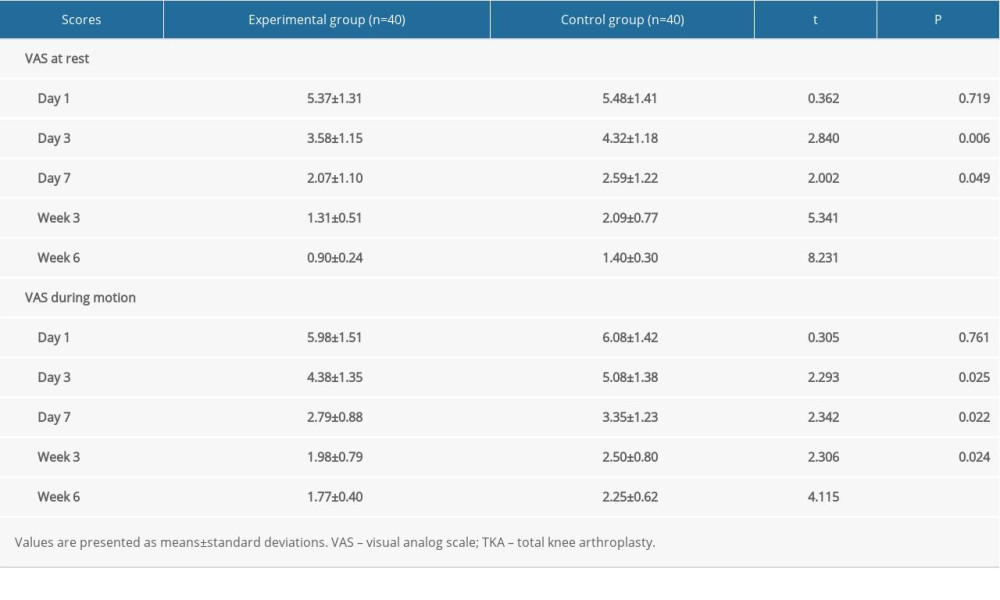 Table 2. VAS scores in the 2 groups at different time points after TKA.
Table 2. VAS scores in the 2 groups at different time points after TKA.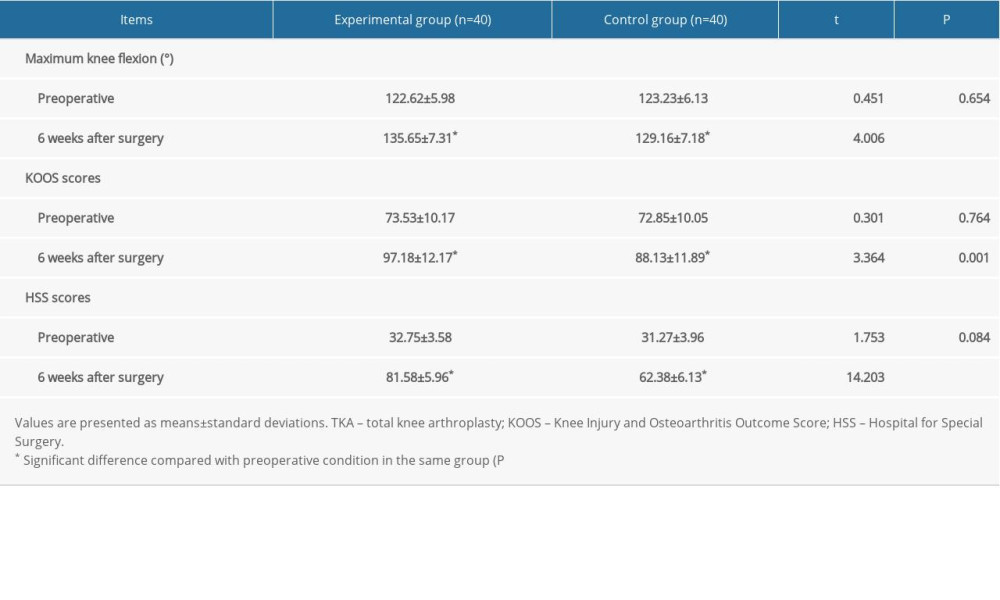 Table 3. Knee function in the 2 groups before and 6 weeks after TKA.
Table 3. Knee function in the 2 groups before and 6 weeks after TKA. Table 4. Time spent out of bed and length of hospital stay in the 2 groups.
Table 4. Time spent out of bed and length of hospital stay in the 2 groups.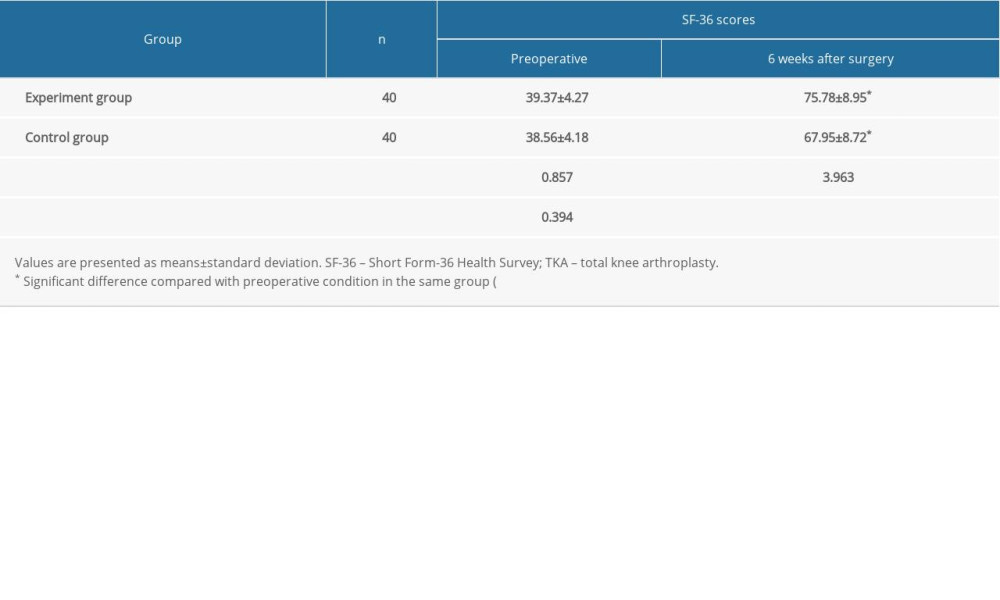 Table 5. SF-36 scores in the 2 groups before and 6 weeks after TKA.
Table 5. SF-36 scores in the 2 groups before and 6 weeks after TKA. In Press
06 Mar 2024 : Clinical Research
Comparison of Outcomes between Single-Level and Double-Level Corpectomy in Thoracolumbar Reconstruction: A ...Med Sci Monit In Press; DOI: 10.12659/MSM.943797
21 Mar 2024 : Meta-Analysis
Economic Evaluation of COVID-19 Screening Tests and Surveillance Strategies in Low-Income, Middle-Income, a...Med Sci Monit In Press; DOI: 10.12659/MSM.943863
10 Apr 2024 : Clinical Research
Predicting Acute Cardiovascular Complications in COVID-19: Insights from a Specialized Cardiac Referral Dep...Med Sci Monit In Press; DOI: 10.12659/MSM.942612
06 Mar 2024 : Clinical Research
Enhanced Surgical Outcomes of Popliteal Cyst Excision: A Retrospective Study Comparing Arthroscopic Debride...Med Sci Monit In Press; DOI: 10.12659/MSM.941102
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952