21 May 2021: Clinical Research
Aspiration Thrombectomy in Patients with Large Vessel Occlusion and Mild Stroke: A Single-Center Experience
Jozef Haring12ABEF, Miroslav Mako13BC, Ján Haršány24BC, Georgi Krastev1ADF, Matúš Hoferica4BCD, Andrej Klepanec4ADEF*DOI: 10.12659/MSM.930014
Med Sci Monit 2021; 27:e930014
Abstract
BACKGROUND: The purpose of this study was to evaluate outcomes of patients with mild stroke, defined by National Institutes of Health Stroke Scale (NIHSS) score <6, caused by large vessel occlusion treated with aspiration thrombectomy.
MATERIAL AND METHODS: Data from the endovascular stroke registry of our center were retrospectively analyzed. Anterior or posterior circulation strokes with NIHSS score <6 upon admission were analyzed. The assessment of a good clinical outcome (modified Rankin scale score 0-2) at day 90 was the primary endpoint. Symptomatic intracranial hemorrhage, defined in European Cooperative Acute Stroke Study grade III, and mortality at day 90 were the safety measures. A successful endovascular procedure was defined as a Thrombolysis in Cerebral Infarction (TICI) score of 2b or 3.
RESULTS: We included 27 patients treated with immediate mechanical thrombectomy, 19 (70.4%) in the anterior circulation and 8 (29.6%) in the posterior circulation. The mean age was 69.8±12.3 years and 40.7% were male. Thirteen patients (48.1%) received bridging intravenous thrombolysis before endovascular thrombectomy. Twenty-five patients (92.6%) underwent the direct aspiration first-pass technique “ADAPT” as the first choice of endovascular procedure. Successful recanalization was achieved in 25 patients (92.6%). Twenty-one patients (77.8%) had a good functional outcome at the 3-month follow-up, 1 (3.7%) symptomatic intracranial hemorrhage was observed, and 2 patients (7.4%) died.
CONCLUSIONS: Immediate aspiration thrombectomy may be a safe and feasible first-line treatment option in patients suffering from mild stroke due to large vessel occlusion in the anterior and posterior circulation.
Keywords: Cerebrovascular Disorders, Patient Outcome Assessment, Stroke, Suction, Thrombectomy, ischemic stroke
Background
The endovascular approach is recommended nowadays for the treatment of patients suffering from acute ischemic stroke (AIS) due to intracranial large vessel occlusion (LVO). According to the AHA/ASA 2018 guidelines, mechanical thrombectomy using stent retrievers is recommended for AIS patients when procedure initiation is within 6 h of symptoms onset. Patients should also have pre-stroke modified Rankin scale (mRs) score <1, Alberta Stroke Program Early Computed Tomography score >6, or National Institutes of Health Stroke Scale (NIHSS) score >6, and causative occlusion of the internal carotid artery or proximal middle cerebral artery (MCA) [1]. Treatment of ischemic stroke due to LVO and mild stroke with NIHSS score <6 represents a particular challenge, since the potential risk of thrombectomy must be weighed against the potential disability caused by neurological deterioration. Few studies have reported outcomes of patients with NIHSS scores <6 treated with mechanical thrombectomy [2–6]. In the ESO-ESMINT 2019 Guidelines on Mechanical Thrombectomy in Acute Ischemic Stroke, most experts (9/11) suggested that, for patients with low NIHSS scores (0–5) who are not eligible for a dedicated randomized controlled trial, treatment with mechanical thrombectomy in addition to intravenous thrombolysis (or alone in cases where intravenous thrombolysis is contraindicated) may be reasonable if the patient has clearly disabling deficits (eg, significant motor deficits, aphasia, or hemianopia) at presentation, or if clinical symptoms worsen despite intravenous thrombolysis [7]. The purpose of this study was to evaluate immediate aspiration thrombectomy in patients suffering from mild strokes, defined by an NIHSS score <6, caused by LVO.
Material and Methods
STATISTICAL ANALYSIS:
Continuous variables were calculated as median (interquartile range, IQR) or as mean±standard deviation (SD). Categorical variables are reported as proportions. P-values were calculated using Fisher’s exact test for categorical variables, the Mann-Whitney U test (Wilcoxon rank-sum test) for non-normally distributed continuous variables and Welch’s
Results
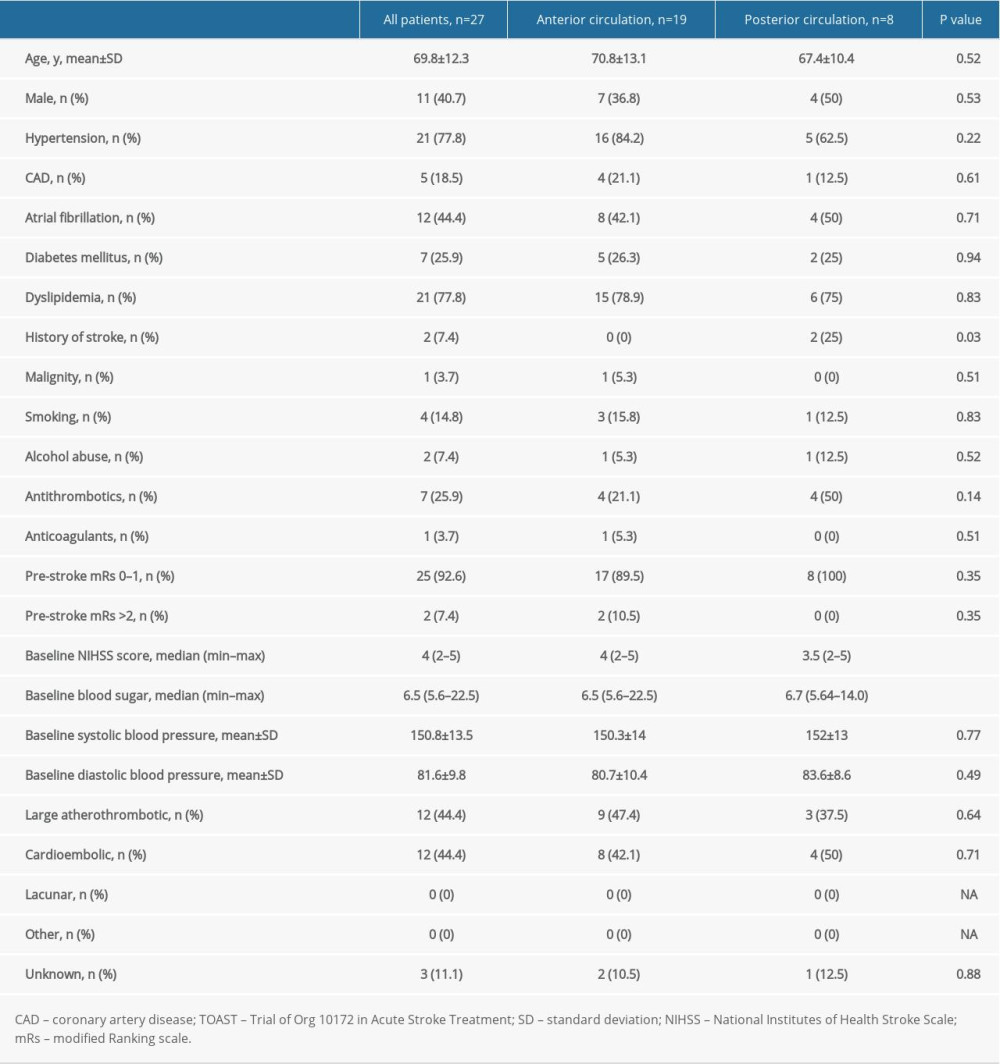
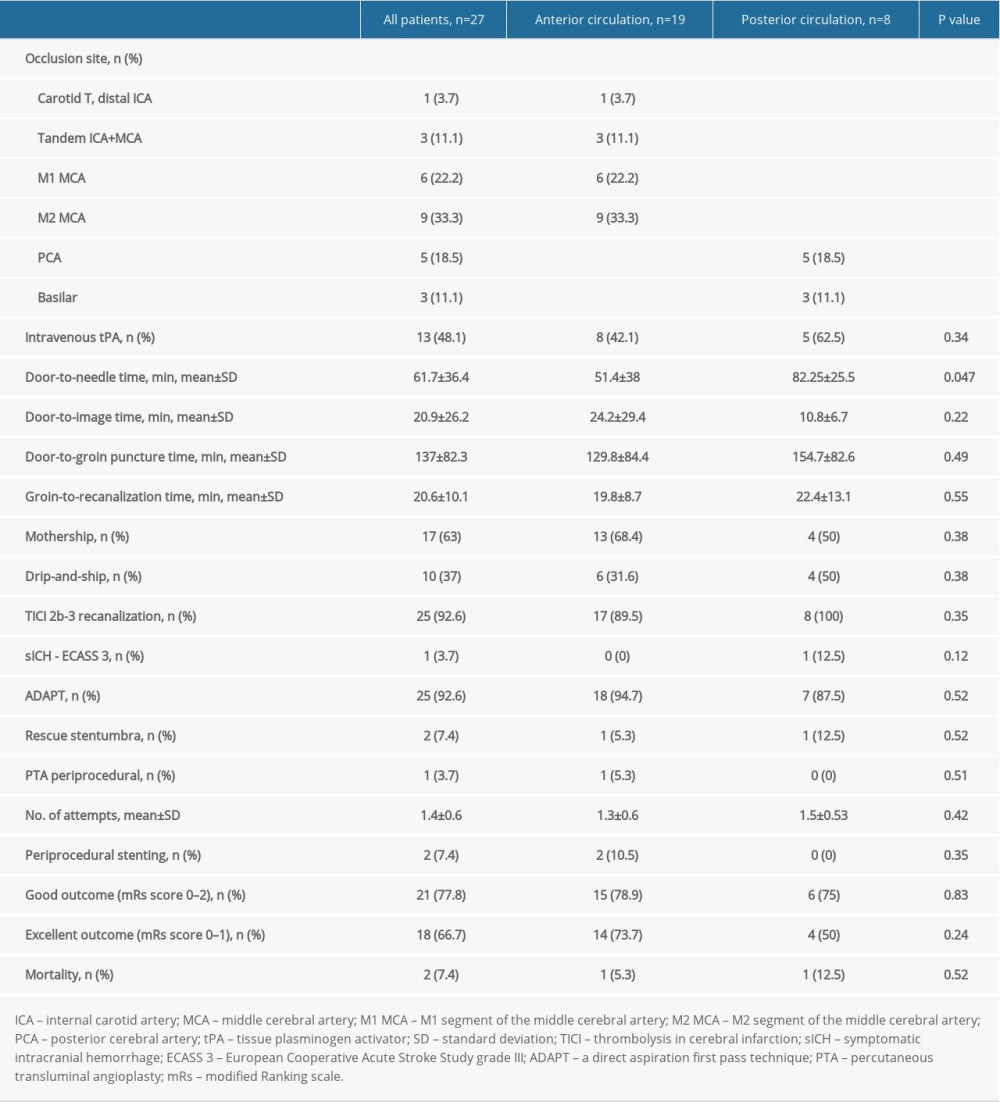
We identified 27 patients with NIHSS scores <6 who underwent endovascular thrombectomy and were included in the analysis. The mean age was 69.8±12.3 years and 40.7% were male. Twenty-five patients (92.6%) had a pre-stroke mRs score 0–1 and 2 patients (7.4%) had an mRs score >2. The median baseline NIHSS score was 4 (2–5). Seven patients (25.9%) were taking antithrombotics and 1 patient (3.7%) was receiving anticoagulation therapy before the stroke onset. Seventeen patients (63%) were treated in the vicinity of the endovascular center (the “mothership” concept) and 10 patients (37%) came from primary stroke centers (the “drip-and-ship” concept). The risk factors for stroke and etiology are presented in Table 1. Radiological findings, logistics, and outcome measures are summarized in Tables 2 and 3. In patients with anterior stroke, 9 patients (33.3%) had M2 MCA occlusion, 6 patients (22.2%) had M1 MCA occlusion, 3 patients (11.1%) had tandem occlusions, and 1 patient (3.7%) had a carotid T occlusion. Eight patients (29.6%) suffered from posterior stroke, 3 patients (11.1%) had occlusions localized in the basilar artery, and 5 patients (18.5%) had occlusions in the posterior cerebral artery. Immediate direct aspiration “ADAPT” was used in 25 patients (92.6%) and rescue therapy aspiration together with stent-retriever thrombectomy was necessary in 2 patients (7.4%). Periprocedural extracranial carotid artery stenting was performed in 2 patients (7.4%). None of the patients suffered early reocclusion of the treated vessel or stroke in other vascular territory within 7 days. The mean number of catheter maneuvers in the target vessel was 1.4±0.6. TICI recanalization scores of 2b or 3 were reached in 25 patients (92.6%); no periprocedural complications were observed either at the site of approach or intracranially. Sixteen patients (59.3%) had TICI recanalization scores of 2b or 3 following a single first pass in the target vessel using ADAPT. At 3-month follow-up, 21 patients (77.8%) had a good functional outcome, with an mRs score of 0–2, and 18 patients (66.7%) had an excellent clinical outcome, with an mRs score of 0–1. Only 1 patient (3.7%) had a symptomatic intracranial hemorrhage, as defined by the ECASS 3 criteria. Two patients (7.4%) died.
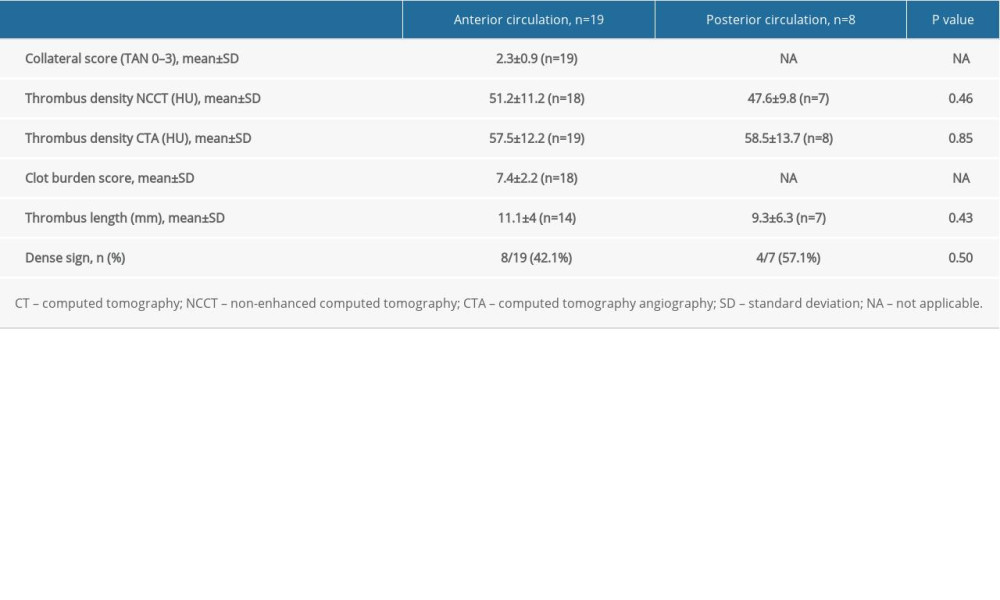
Nineteen occlusions (70.4%) were localized in the anterior circulation and 8 (29.6%) were localized in the posterior circulation. There were no statistically significant differences in observed parameters, except for a history of stroke in the group with posterior circulation stroke, and a shorter “door-to-needle” time in strokes involving the anterior circulation. Characteristics of occlusions in the anterior and posterior circulation are summarized in Table 3. Positive dense artery signs were observed in 8 out of 19 anterior circulation patients (42.1%) and in 4 out of 7 (57.1%) posterior circulation patients. No statistically significant differences in thrombus density were detected by non-contrast CT and no differences in thrombus length were detected by CTA in the anterior and posterior vasculature. Good functional outcomes (mRs 0–2) were achieved in 78.9% of the subgroup of patients with anterior circulation stroke and in 75% of patients with posterior stroke. Overall, 73.7% of patients with AIS in the anterior circulation and 50% of patients in the posterior stroke group had an excellent clinical outcome (mRs 0–1) at 90-day follow-up.
All patients underwent an immediate thrombectomy approach. Thirteen patients (48.1%) received bridging IVT before the endovascular thrombectomy (EVT), 8 patients with anterior circulation stroke and 5 patients with posterior circulation stroke. None of the patients receiving IVT before the EVT reached successful recanalization of the target vessel after the administration of tissue plasminogen activator (tPA).
Three patients suffered from tandem artery occlusion in the anterior circulation, affecting the internal carotid artery (ICA) and the M2 segment of the MCA. In 2 patients, the anterograde approach was necessary with angioplasty of the proximal ICA and aspiration thrombectomy of the MCA afterwards, and 1 patient had periprocedural carotid artery stenting because tight stenosis with plaque ulcerations persisted after the percutaneous transluminal angioplasty (PTA). One patient had the retrograde approach, with periprocedural angioplasty of the proximal ICA and delayed internal carotid artery stenting 6 days after thrombectomy. All of the patients with TAO received dual antiplatelet therapy with acetylsalicylic acid (ASA) and clopidogrel per protocol. The patient with periprocedural stenting of the ICA during thrombectomy had immediate initiation of secondary stroke prevention with a loading dose of ASA (300 mg) and clopidogrel (300 mg), as no IVT was given in this case.
Discussion
LIMITATIONS OF THE STUDY:
Our study has significant limitations, most of them due to its retrospective observational nature, non-controlled design, and small cohort of patients. The limitations also include the potential for selection bias, as well as treatment procedures in different vascular territories without a matched cohort.
Conclusions
In conclusion, aspiration thrombectomy with ADAPT in LVO patients with low NIHSS scores may be safe and feasible. Our results support the use of mechanical thrombectomy in this group of patients, but randomized clinical trials are needed to establish the optimal management approach for this challenging patient population.
References
1. Powers WJ, Rabinstein AA, Ackerson T, 2018 Guidelines for the early management of patients with acute ischemic stroke: A Guideline for Healthcare Professionals from the American Heart Association/American Stroke Association: Stroke, 2018; 49; e46-99
2. Nagel S, Bouslama M, Krause LU, Mechanical thrombectomy in patients with milder strokes and large vessel occlusions. A multicenter matched analysis: Stroke, 2018; 49; 2391-97
3. Griessenauer JC, Medin C, Maingard J, Endovascular mechanical thrombectomy in large-vessel occlusion ischemic stroke presenting with low national institutes of health stroke scale: Systematic review and meta-analysis: World Neurosurg, 2018; 110; 263-69
4. Haussen DC, Bouslama M, Grossberg JA, Too good to intervene? Thrombectomy for large vessel occlusion strokes with minimal symptoms: An intention-to-treat analysis: J Neurointerv Surg, 2017; 9(10); 917-21
5. Bhogal P, Bücke P, Ganslandt O, Mechanical thrombectomy in patients with M1 occlusion and NIHSS score ≤5: A single-centre experience: Stroke Vasc Neurol, 2016; 1(4); 165-71
6. Goldhoorn RB, Mulder MJHL, Jansen IGV, Safety and outcome of endovascular treatment for minor ischemic stroke: Results from the multicenter clinical registry of endovascular treatment of acute ischemic stroke in the Netherlands: J Stroke Cerebrovasc Dis, 2019; 28(3); 542-49
7. Turc G, Bhogal P, Fischer U, European Stroke Organisation (ESO) – European Society for Minimally Invasive Neurological Therapy (ESMINT) Guidelines on mechanical thrombectomy in acute ischaemic stroke Endorsed by Stroke Alliance for Europe (SAFE): Eur Stroke J, 2019; 4(1); 6-12
8. Kim JT, Park MS, Chang J, Proximal arterial occlusion in acute ischemic stroke with low NIHSS scores should not be considered as mild stroke: PLoS One, 2013; 8; e70996
9. Saleem Y, Nogueira RG, Rodrigues GM, Acute neurological deterioration in large vessel occlusions and mild symptoms managed medically: Stroke, 2020; 5; 1428-34
10. Ospel JM, Kim B, Heo JH, Endovascular treatment decision-making in acute ischemic stroke patients with large vessel occlusion and low National Institutes of Health Stroke Scale: Insights from UNMASK EVT, an international multidisciplinary survey: Neuroradiology, 2020; 62(6); 715-21
11. Wolman DN, Marcellus DG, Lansberg MG, Endovascular versus medical therapy for large-vessel anterior occlusive stroke presenting with mild symptoms: Int J Stroke, 2020; 15(3); 324-31
12. Turk AS, Siddiqui A, Fifi JT, Aspiration thrombectomy versus stent retriever thrombectomy as first-line approach for large vessel occlusion (COMPASS): A multicentre, randomised, open label, blinded outcome, non-inferiority trial: Lancet, 2019; 393(10175); 998-1008
13. Lapergue B, Blanc R, Gory B, Effect of endovascular contact aspiration vs stent retriever on revascularization in patients with acute ischemic stroke and large vessel occlusion. The ASTER randomized clinical trial: JAMA, 2017; 318(5); 443-52
14. Kayan Y, Meyers PM, Prestigiacomo CJSociety of NeuroInterventional Surgery, Current endovascular strategies for posterior circulation large vessel occlusion stroke: Report of the Society of NeuroInterventional Surgery Standards and Guidelines Committee: J NeuroIntervent Surg, 2019; 11(10); 1055-62
15. Peschillo S, Diana F, Berge J, Missori P, A comparison of acute vascular damage caused by ADAPT versus a stent retriever device after thrombectomy in acute ischemic stroke: A histological and ultrastructural study in an animal model: J Neurointerv Surg, 2017; 9(8); 743-49
16. Chueh JY, Puri AS, Wakhloo AK, Gounis MJ, Risk of distal embolization with stent retriever thrombectomy and ADAPT: J Neurointerv Surg, 2016; 8(2); 197-202
17. Goyal N, Tsivgoulis G, Malhotra K, Medical management vs mechanical thrombectomy for mild strokes: An international multicenter study and systematic review and meta-analysis: JAMA Neurol, 2020; 77(1); 16-24
18. Haussen DC, Lima FO, Bouslama M, Thrombectomy versus medical management for large vessel occlusion strokes with minimal symptoms: An analysis from STOPStroke and GESTOR cohorts: Neurointerv Surg, 2018; 10(4); 325-29
19. Sarraj A, Hassan A, Savitz SI, Endovascular thrombectomy for mild strokes: How low should we go? A multicenter cohort study: Stroke, 2018; 49; 2398-405
20. Emberson J, Lees KR, Lyden P, Effect of treatment delay, age, and stroke severity on the effects of intravenous thrombolysis with alteplase for acute ischaemic stroke: A meta-analysis of individual patient data from randomised trials: Lancet, 2014; 384(9958); 1929-35
21. Kamalian S, Morais LT, Pomerantz SR, Clot length distribution and predictors in anterior circulation stroke: implications for IA therapy: Stroke, 2013; 44; 3553-56
22. Yoo AJ, Khatri P, Mocco J, Impact of thrombus length on outcomes after intra-arterial aspiration thrombectomy in the THERAPY trial: Stroke, 2017; 48(7); 1895-900
23. , Endovascular Therapy for Low NIHSS Ischemic Strokes (ENDOLOW): ClinicalTrials.gov Identifier: NCT04167527
24. , Minor Stroke Therapy Evaluation (MOSTE): ClinicalTrials.gov Identifier: NCT03796468
25. Schonewille WJBASICS Study Group, The Basilar Artery International Collaboration Study (BASICS): A randomized controlled trial of endovascular therapy in basilar artery occlusion: Int J Stroke, 2020; 15(1S); 3-4
26. Zi W, Qiu Z, Wu D, Assessment of endovascular treatment for acute basilar artery occlusion via a nationwide prospective registry: JAMA Neurol, 2020; 77(5); 561-73
In Press
05 Mar 2024 : Clinical Research
Muscular Function Recovery from General Anesthesia in 132 Patients Undergoing Surgery with Acceleromyograph...Med Sci Monit In Press; DOI: 10.12659/MSM.942780
05 Mar 2024 : Clinical Research
Effects of Thermal Insulation on Recovery and Comfort of Patients Undergoing Holmium Laser LithotripsyMed Sci Monit In Press; DOI: 10.12659/MSM.942836
05 Mar 2024 : Clinical Research
Role of Critical Shoulder Angle in Degenerative Type Rotator Cuff Tears: A Turkish Cohort StudyMed Sci Monit In Press; DOI: 10.12659/MSM.943703
06 Mar 2024 : Clinical Research
Comparison of Outcomes between Single-Level and Double-Level Corpectomy in Thoracolumbar Reconstruction: A ...Med Sci Monit In Press; DOI: 10.12659/MSM.943797
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952