28 November 2020: Clinical Research
Trapezoidal Vertebral Body and Spine-Pelvis Sagittal Alignment in Patients with Lumber Spondylolisthesis
He Xuegang123ACEF*, Fengguang Yang123B, Enhui Ren123C, Liang Yang123E, Yajun Deng123DE, Zhanjun Ma123B, Guangzhi Zhang123E, Yicheng Gao123E, Yonggang Wang12F, Yong Yang12F, Xuewen Kang123ADOI: 10.12659/MSM.927747
Med Sci Monit 2020; 26:e927747
Abstract
BACKGROUND: Trapezoidal changes of the vertebral body are more common in patients with lumbar spondylolisthesis than in others. However, we lack an understanding of factors predisposing to the development of a marked trapezoidal deformity. Also, no associations between a trapezoidal vertebrae (TV) and spine-pelvis sagittal parameters have been previously reported.
MATERIAL AND METHODS: A total of 73 subjects with lumbar spondylolisthesis were enrolled and we collected their clinical data. Vertebral body parameters and spine-pelvis sagittal alignment parameters were measured via lumbar spine X-ray. Using the lumbar index (LI), patients were divided into a TV group (LI >0.8, n=24) and a control group (LI >0.8, n=49). The clinical data and spine-pelvic sagittal parameters of the 2 groups were compared using the t test or chi-squared test. Pearson’s correlation analysis and multiple linear regression were used to determine relationships among the parameters.
RESULTS: The TV and control groups differed significantly in terms of the slipped segment, extent of slippage, intervertebral disc height (IDH), and sagittal parameters (all P<0.05). Pearson’s correlation analysis and multiple linear regression analysis showed that the slipped segment (r=–0.606), extent of slippage (r=–0.660), and IDH (r=0.698) were risk factors for the development of a TV body. Also, vertebral trapezoidal deformation was closely associated with sagittal parameters.
CONCLUSIONS: The vertebral body affected by lumbar spondylolisthesis exhibits a trapezoidal change closely associated with the slipped segment, the extent of slippage, and IDH. The TV group exhibited greater pelvic incidence values and lumbar lordosis, which may have caused wedging of the slipped vertebra.
Keywords: Lumbar Vertebrae, Neurosurgery, Orthopedics, spondylolisthesis, Case-Control Studies, Lordosis, Multivariate Analysis, Pelvis, vertebral body
Background
Lumbar spondylolisthesis is characterized by ventral displacement of a superior vertebra relative to an inferior vertebra. In 1976, Wiltse et al. [1] classified lumbar spondylolisthesis into 5 main categories using etiological and topographical criteria: dysplastic, isthmic, degenerative, traumatic, and pathological. The isthmic and degenerative types are the most common; the isthmic type is more common in the L5–S1 segment, with a prevalence of 11.5% in the general population; degenerative spondylolisthesis is more common in segment L4–L5, with an incidence of 5% to 7% [2,3].
Some patients with lumbar spondylolisthesis exhibit abnormal morphology of the slipped vertebra, which reflects vertebral trapezoidal changes or wedge deformation (Figure 1). The extent of vertebral wedging is represented using the vertebral lumbar index (LI), which is the ratio of the height of the posterior edge of the vertebral body to the height of the leading edge; a value less than 0.8 is considered to be an absolute wedge [4]. Some studies have suggested that a trapezoidal vertebra is a risk factor for spondylolisthesis development and progression, but others have suggested that lumbar spondylolisthesis causes wedging of a slipped vertebra [4–7]. Thus, no consensus is apparent. Pelvic incidence (PI) is an anatomical parameter describing the morphology of the pelvis and spatial orientation of the sacrum, and is thought to be both closely related and proportional to the extent of lumbar lordosis (LL) [8]. Several studies have shown that the PI of lumbar spondylolisthesis patients is significantly greater than that of normal subjects [8–13]. However, the relationships between spinopelvic sagittal parameters and lumbar spondylolisthesis remain highly controversial; very few studies have explored the relationship between trapezoidal deformation of a slipped vertebra and spinopelvic sagittal parameters.
In recent years, most studies on lumbar spondylolisthesis have focused on the relationships between spondylolisthesis, spinopelvic sagittal plane morphology, and the choice of surgical treatment; few studies have examined the morphological abnormalities of spondylolisthetic vertebrae. Therefore, we analyzed the clinical characteristics and imaging data of patients with lumbar spondylolisthesis to define morphological changes in the vertebral body, the relevant risk factors, and relationships to changes in spinal-pelvic sagittal parameters.
Material and Methods
STUDY SUBJECTS:
We retrospectively analyzed patients with single-segment lumbar spondylolisthesis who visited our department from February 2016 to February 2019 for whom complete data were available. The exclusion criteria were incomplete imaging data, multi-segmental spondylolisthesis, vertebral fracture, scoliosis, and any previous history of lumbar surgery. Forty-five healthy subjects who underwent a medical examination at our hospital during the same period as the patients were included in the control group, and their vertebral body parameters were measured. This study was approved by the Medical Ethics Committee of Lanzhou University Second Hospital (approval number 2019A-182), and all procedures were performed in accordance with relevant guidelines and regulations. Written informed consent was obtained from each patient. Of the 143 patients diagnosed with lumbar spondylolisthesis in our department over the study period, 61 lacked complete imaging data, 4 had multiple segmental spondylolisthesis, 2 had vertebral fractures, and 2 had scoliosis. Thus, we finally included 73 patients with single-level lumbar spondylolisthesis (13 males (17.8%) and 60 females (82.2%) of mean age 54.59±11.14 years). Among them, 43 had L4-5 spondylolisthesis and 30 had L5–S1 spondylolistheses; 36 isthmic spondylolysis, and 37 degenerative changes. The patients were divided into trapezoidal vertebral (TV) and control groups based on the LI. The clinical data and spine-pelvic sagittal parameters were compared between the groups.
MEASUREMENTS OF IMAGING DATA:
The subjects were instructed to stand erect with their knees extended and elbows flexed, and to place their hands on a horizontal bar at shoulder level for the X-ray analysis. The film-to-focus distance was maintained at 2 m. The parameters of both the L4 and L5 vertebrae were measured; these included the anterior vertebral height (AH), posterior vertebral height (PH), vertebral body angle (α), and LI (PH/AH). The ratio of the height difference between the anterior and posterior edges of the vertebral body, to the height of the anterior edge, was calculated [R=(AH–PH)/AH]. The measured spine-pelvis sagittal parameters were as follows: (1) the extent of slippage (the ratio of the distance from the posterior edge of the slipped vertebra to the posterior edge of the lower vertebra, and the anteroposterior diameter of the lower vertebral body); (2) the slip angle (by reference to the TV body): the angle between the upper endplate of the slipped vertebra and the upper endplate of the lower vertebra; (3) the intervertebral disc height (IDH) measured at the middle of the disc; (4) LL: the angle between lines parallel to the upper L1 endplate and the S1 endplate; (5) sacral slope (SS): the angle between the S1 endplate and the horizontal plane; (6) pelvic tilt (PT): the angle between the vertical plane and the line connecting the midpoint of the sacral endplate and the hip axis; and (7) PI: the angle between the line connecting the midpoint of the sacral endplate and the hip axis and a line perpendicular to the sacral endplate (Figure 2). All imaging parameters were measured by 2 spine surgeons (Fengguang Yang and Zhanjun Ma). The mean intra- and interobserver reliability values were >0.75 for all parameters (Supplemenrary Tables 1 and 2).
STATISTICAL ANALYSIS:
A statistical software package (SPSS, ver. 25.0; SPSS Inc., Chicago, IL, USA) was used for all statistical analyses. The intraclass correlation coefficient was used as a measure of intra- and interobserver reliability. Descriptive statistics are provided as mean±standard deviation. The independent-sample
Results
COMPARISON OF SLIPPED AND NORMAL VERTEBRAL BODIES:
Measurements of the slipped and normal vertebral bodies are listed in Table 1. The anterior heights of normal and slipped L4 vertebrae did not differ significantly (30.69±2.30 vs. 30.80±2.04 mm, P=0.838). The posterior vertebral height of slipped vertebrae was significantly less than that of normal vertebrae (27.92±2.24 vs. 29.79±2.31 mm, P=0.001). The mean LI of slipped vertebrae was significantly lower than that that of normal vertebrae (0.91±0.08 vs. 0.97±0.03, P<0.001). The height difference between the anterior and posterior edges of slipped vertebrae (AH–PH) and the ratio thereof to the anterior edge height [R=(AH–PH)/AH] were significantly greater than those of normal vertebrae (0.09±0.08 vs. 0.03±0.03, P<0.001). The α of slipped vertebrae was significantly greater than that of normal vertebrae (7.24±5.00 vs. 2.16±1.12°, P<0.001).
The anterior heights of the normal and slipped L5 vertebrae did not differ significantly (32.07±2.01
COMPARISON OF CLINICAL DATA AND SPINE-PELVIC SAGITTAL PARAMETERS BETWEEN THE TV AND CONTROL GROUPS:
Based on the LI, patients were divided into trapezoidal vertebrae (LI ≤0.8) and control (LI >0.8) groups. Significant differences between the groups are listed in Table 2. Higher values were detected in the TV group for R (0.27±0.04 vs. 0.08±0.06, P<0.001), α (18.73±3.87 vs. 6.69±3.99, P<0.001), extent of slippage (0.35±0.07 vs. 0.22±0.05, P<0.001), slip angle (17.58±5.30 vs. 9.27±2.67, P<0.001), LL (55.48±7.07 vs. 47.05±7.50, P<0.001), SS (45.25±5.33 vs. 36.75±6.96, P<0.001), PT (14.93±3.60 vs. 11.72±2.10, P<0.001), and PI (58.34±7.82 vs. 48.36±7.89, P<0.001). In contrast, LI (0.73±0.04 vs. 0.92±0.06, P<0.001) and IDH (2.68±1.12 vs. 5.58±1.96, P<0.001) were smaller in the TV group. The type of slipped segment was significantly different between the 2 groups (L4–L5/L5–S1: 5/19 vs. 38/11, P<0.001). No differences in age (P=0.139), sex (P=0.858), or BMI (P=0.071) were observed. Table 2 shows the details of the comparative analyses.
The comparative analyses of degenerative spondylolisthesis revealed higher values in the TV group compared to the control group for R (0.26±0.03 vs. 0.07±0.06, P<0.001), α (20.08±6.61 vs. 5.73±3.41, P<0.001), extent of slippage (0.36±0.13 vs. 0.20±0.05, P<0.001), slip angle (19.35±4.00 vs. 8.34±1.77, P<0.001), LL (55.83±4.29 vs. 46.94±7.01, P=0.019), SS (44.08±2.68 vs. 36.83±6.55, P=0.037), and PI (58.63±2.94 vs. 47.64±7.15, P=0.005). Conversely, LI (0.74±0.03 vs. 0.93±0.06, P<0.001) and IDH (3.03±1.34 vs. 6.06±1.86, P=0.003) were smaller in the TV group. No group differences were observed for age (P=0.139), sex (P=0.858), BMI (P=0.577), PT (P=0.065), or the type of slipped segment (L4–L5/L5–S1: 2/2 vs. 27/2, P=0.198) (Table 2).
Comparative analyses of isthmic spondylolisthesis revealed higher values in the TV group compared to the control group for R (0.27±0.05 vs. 0.11±0.06, P<0.001), α (18.46±3.29 vs. 8.66±4.48, P<0.001), extent of slippage (0.35±0.06 vs. 0.25±0.04, P<0.001), slip angle (17.23±5.54 vs. 11.17±3.22, P<0.001), LL (55.41±7.58 vs. 47.28±8.67, P=0.005), SS (45.48±5.73 vs. 36.58±8.00, P<0.001), PT (14.95±3.86 vs. 11.78±2.43, P=0.007), and PI (58.27±8.52 vs. 49.84±9.32, P=0.008). In contrast, LI (0.73±0.05 vs. 0.89±0.06, P<0.001) and IDH (2.62±1.10 vs. 4.59±1.83, P=0.001) were smaller in the TV group. The type of slipped segment differed significantly between the 2 groups (L4–L5/L5–S1: 15/17 vs. 11/3, P=0.001). No group differences were observed in age (P=0.389), sex (P=0.925), or BMI (P=0.199) (Table 2).
The clinical data and spine-pelvic sagittal parameters did not differ significantly between the isthmic and degenerative spondylolisthesis TV groups (both
CORRELATIONS BETWEEN LI OF THE SLIPPED VERTEBRA AND THE CLINICAL DATA:
The Pearson’s correlation data on factors influencing the extent of slipped vertebral wedging are listed in Table 3. No significant correlation was evident between age, sex, BMI, and the LI (all P>0.05); but the slipped segment, the type of slippage, extent of slippage, and IDH were closely related to the LI (P<0.001). In particular, the extent of slippage was (significantly) negatively correlated with the LI (r=−0.660, P<0.001). The disc height was significantly (positively) correlated with the LI (r=0.698, P<0.001). The smaller the LI, the greater the extent of vertebral wedging deformity, which was positively correlated with the extent of slippage and negatively correlated with the height of the intervertebral disc (Figure 3).
MULTIVARIATE ANALYSIS:
Multiple linear regression analysis showed that the slipped segment, extent of slippage, and IDH affected the extent of wedge deformation (Table 4). Greater slip (P=0.006), lower disc height (P=0.006), and L5–S1 level slippage (P=0.001) increased the likelihood of the slipped vertebra becoming wedged.
CORRELATIONS BETWEEN LI OF THE SLIPPED VERTEBRA AND SPINE-PELVIC SAGITTAL PARAMETERS:
Pearson’s correlations between the LI and sagittal parameters showed that the slip angle, LL, and PI were negatively correlated with the LI (Table 5). In other words, the greater the slip angle, LL, and PI, the more severe the vertebral wedging (Figure 4).
Discussion
We found that certain patients with lumbar spondylolisthesis exhibited trapezoidal changes in their slipped vertebrae. The height of the posterior edge of the slipped vertebra was significantly lower than that of the normal vertebra (Figure 1). Using the LI, patients were divided into TV and control groups; the groups differed significantly in terms of the slipped segment, extent of slippage, and IDH. Isthmic and degenerative spondylolisthesis are very different in terms of mechanics, typical patient age, and spine level. Interestingly, in our study, the clinical data and spine-pelvic sagittal parameters of the isthmic and degenerative spondylolisthesis TV groups did not differ significantly. Correlation and multiple linear regression analyses revealed that patients with spondylolisthesis at level L5–S1, with lower intervertebral discs, and a greater extent of slippage, were more likely to exhibit wedging of the slipped vertebrae.
Since the discovery of lumbar spondylolisthesis, slipped vertebral wedging has been insufficiently studied, and the relationship between spondylolisthesis and vertebral wedging has remained very controversial. Wiltse et al. [1] suggested that L5 vertebral wedging was a congenital hypoplasia and a risk factor for lumbar spondylolisthesis. Yue et al. [4] found that, on follow-up of 27 patients with lumbar spondylolisthesis, 17 (63%) L5 vertebral bodies exhibited wedge deformation, which might be a risk factor for progression of lumbar spondylolisthesis. In contrast, Sairyo et al. [6] analyzed lateral X-ray measurements of 46 athletes under the age of 18 years in whom vertebral wedge deformation occurred after slippage, and found that the extent of vertebral wedging was closely related to the extent of spondylolisthesis; in patients exhibiting no spondylolisthetic progression, wedge deformation of the vertebral body was not aggravated. Beutler et al. [7] found no significant changes in either the LI or the extent of spondylolisthesis in 30 patients with lumbar spondylolisthesis followed-up for more than 45 years; the childhood LI did not predict the development of spondylolisthesis in adulthood. However, these studies were all holistic in nature; they did not consider the pathological mechanisms and effects of vertebral wedging separately. Here, we focused on the slipped vertebral body. We analyzed the clinical data and sagittal parameters of patients with spondylolisthesis and found that the wedging of spondylolisthetic vertebrae was closely related to a great extent of slippage and a low L5–S1 IDH.
The fifth lumbar vertebra is the vertebra subjected to the greatest amount of static and dynamic stresses associated with daily activities [14]. The gravity load on L5–S1 of the spine features 2 components: a shear force applied parallel to the upper endplate of S1 ventrally and a vertical compressive force applied perpendicular to the upper endplate of S1 inferiorly; the shear force increases gradually from L1 to L5, attaining a maximum at L5 [15]. Ward et al. [16] showed that if the L5 vertebral body lacks interarticular freedom in the craniocaudal direction, the body is clamped by the inferior facet of L4 and the superior facet of S1, triggering isthmic fissure of the L5 body. Terai et al. [17] performed finite element analysis of 10 adolescents with isthmic fissures; the site of maximum stress on the L5 vertebral body lay ventral to the articular process, that is, the posterior part of the vertebral body. Turner et al. [18] suggested that spondylolysis was an acute fracture caused by application of excessive force to the lumbar spine or a fatigue fracture triggered by chronic repeated bending, stretching, or rotation of the spine. The pathology of slipping vertebral wedge deformation may be similar to that of isthmic fissure. We found that only 5 (20.8%) patients in the TV group exhibited L4–L5 segmental slippage, but 19 (79.2%) had L5–S1 slippage; this may be because the L5 vertebral body is subjected to the maximum shear force. In our study, the clinical data and spine-pelvic sagittal parameters of the isthmic and degenerative spondylolisthesis TV groups did not differ significantly, suggesting that trapezoidal changes in the slipped vertebrae are not causal factors in spondylolisthesis, instead being related to the force exerted on the vertebral body after spondylolisthesis; in other words, wedge deformation of the vertebral body may be caused by spondylolisthesis.
We found that slip angle, PI, LL, SS, and PT were all significantly greater in the TV group than the control group. To the best of our knowledge, no study has yet explored the relationship between slipped vertebral wedging and spine-pelvis sagittal parameters. Qi et al. [19] found that the LL, SS, and PI were closely related to lumbar spondylolisthesis and proportional to the extent thereof, and suggested that a larger PI was a risk factor for spondylolisthetic progression and that the LL increased in a compensatory manner. Zhao et al. [10] compared the spine-pelvis sagittal parameters of patients with lumbar spondylolisthesis to those of a normal population, and also concluded that a larger PI increased the risk of spondylolisthesis progression. Roussouly et al. [20] analyzed the sagittal parameters of 82 patients with low-degree spondylolisthesis, and suggested that a higher PI indicated a greater SS. This indicates the presence of a large shear force between L5–S1, which is more likely to trigger the development of, or aggravate, lumbar spondylolisthesis. In adults, the PI value is an invariant anatomical parameter that is positively correlated with LL. The balance between these parameters is key to spinopelvic sagittal stability. In our study, the TV group had larger PI and LL values than the controls, and the LL value was closely related to the degree of wedging of the slipped vertebral body (r=−0.554, P<0.001). Therefore, the wedge shape of the vertebral body may be caused by the increase in LL value to match the larger PI value.
Our study has certain limitations. First, we enrolled only a small number of patients, and those with asymptomatic spondylolisthesis were not included. Also, in the context of wedge deformation of the L4 vertebral body, we did not evaluate the effect of a change in sacral doming, which may also be a risk factor for L5 vertebral wedge deformation.
Conclusions
We found that some patients with lumbar spondylolisthesis, particularly those with a low IDH and a greater extent of slippage at L5–S1, tend to exhibit wedge-shaped changes in their slipped vertebrae. Wedge deformation of the vertebral body may be caused by spondylolisthesis. Also, such patients exhibited a greater PI and LL, suggesting that the TV body may be caused by a larger PI. Finally, we wish to address the unique nature of wedged vertebrae in patients requiring surgery for intervertebral cage fusion. The selection of cage shapes/sizes and the position of the cage implantation may differ between patients with wedging plus spondylolisthesis and patients with spondylolisthesis alone, in terms of the effects of the spine-pelvis sagittal balance and postoperative restoration of nerve function. The surgical plan must be chosen according to the severity of wedge deformation, and further research is needed regarding this point.
Figures
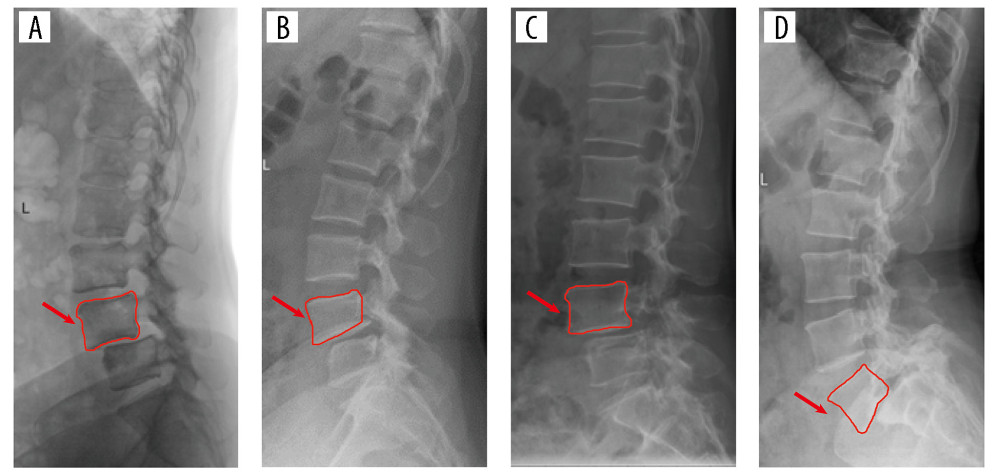 Figure 1. Degenerative spondylolisthesis: (A) Normal vertebral body, (B) Trapezoidal vertebral body; isthmic spondylolisthesis: (C) Normal vertebral body, (D) Trapezoidal vertebral body.
Figure 1. Degenerative spondylolisthesis: (A) Normal vertebral body, (B) Trapezoidal vertebral body; isthmic spondylolisthesis: (C) Normal vertebral body, (D) Trapezoidal vertebral body. 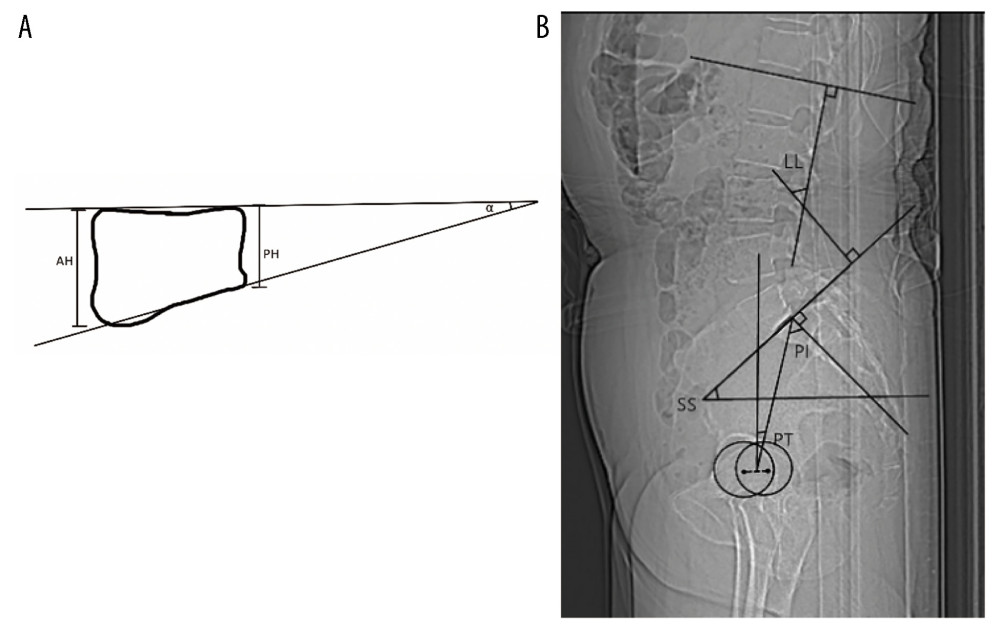 Figure 2. Visual representations of the methods applied to measure vertebral parameters and spine-pelvis sagittal parameters in radiographs are shown as follows: (A) AH: Anterior vertebral height. PH: Posterior vertebral height. Vertebral body angle (α): Angle between superior and inferior endplate of the vertebrae. (B) LL: The angle between lines parallel to the superior L1 endplate and the S1 endplate. SS: The angle between the superior S1 endplate and the horizontal plane. PT: The angle between the vertical plane and the line connecting the midpoint of the sacral endplate and the hip axis. PI: The angle between the line connecting the midpoint of the sacral endplate and the hip axis and a line perpendicular to the sacral endplate.
Figure 2. Visual representations of the methods applied to measure vertebral parameters and spine-pelvis sagittal parameters in radiographs are shown as follows: (A) AH: Anterior vertebral height. PH: Posterior vertebral height. Vertebral body angle (α): Angle between superior and inferior endplate of the vertebrae. (B) LL: The angle between lines parallel to the superior L1 endplate and the S1 endplate. SS: The angle between the superior S1 endplate and the horizontal plane. PT: The angle between the vertical plane and the line connecting the midpoint of the sacral endplate and the hip axis. PI: The angle between the line connecting the midpoint of the sacral endplate and the hip axis and a line perpendicular to the sacral endplate. 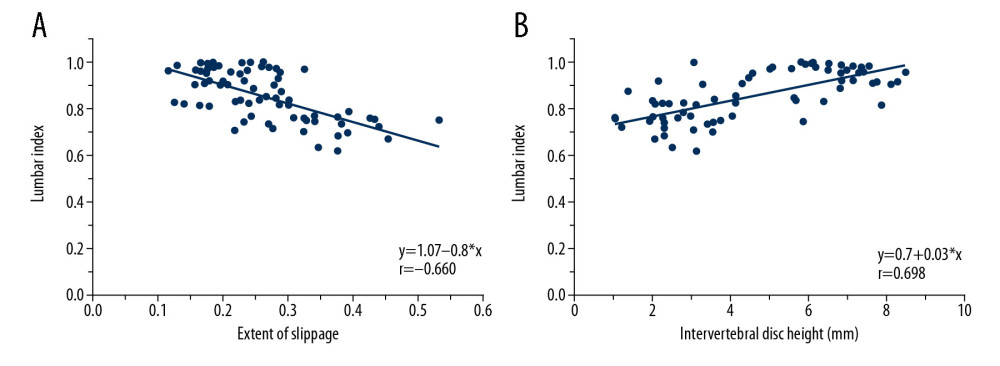 Figure 3. (A) A negative correlation was observed between the extent of slippage and the lumbar index. (B) A positive correlation was observed between the intervertebral disc height and lumbar index.
Figure 3. (A) A negative correlation was observed between the extent of slippage and the lumbar index. (B) A positive correlation was observed between the intervertebral disc height and lumbar index. 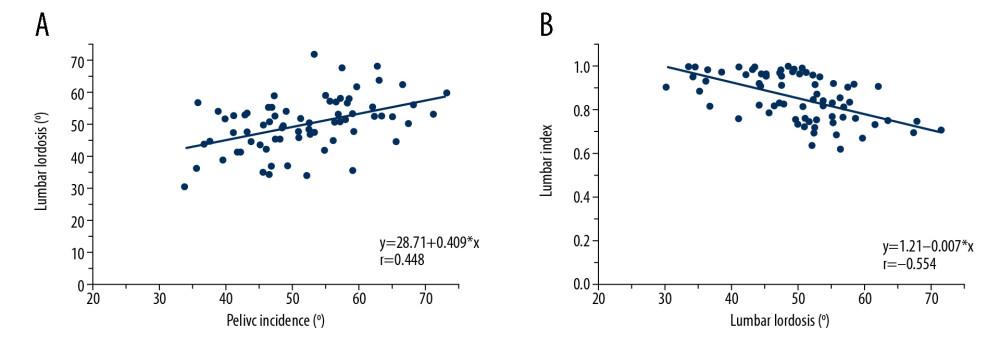 Figure 4. (A) A positive correlation was observed between pelvic incidence and lumbar lordosis. (B) A negative correlation was observed between lumbar lordosis and the lumbar index.
Figure 4. (A) A positive correlation was observed between pelvic incidence and lumbar lordosis. (B) A negative correlation was observed between lumbar lordosis and the lumbar index. Tables
Table 1. Comparison of the parameters between slipped and normal vertebral bodies.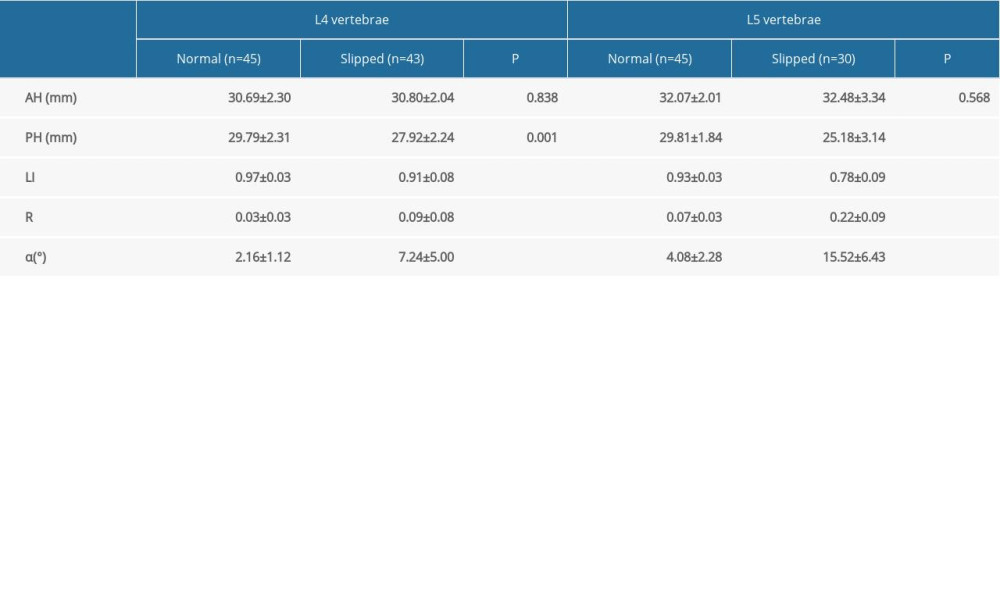 Table 2. Comparison of clinical data and spine-pelvis sagittal parameters between TV group and control group.
Table 2. Comparison of clinical data and spine-pelvis sagittal parameters between TV group and control group.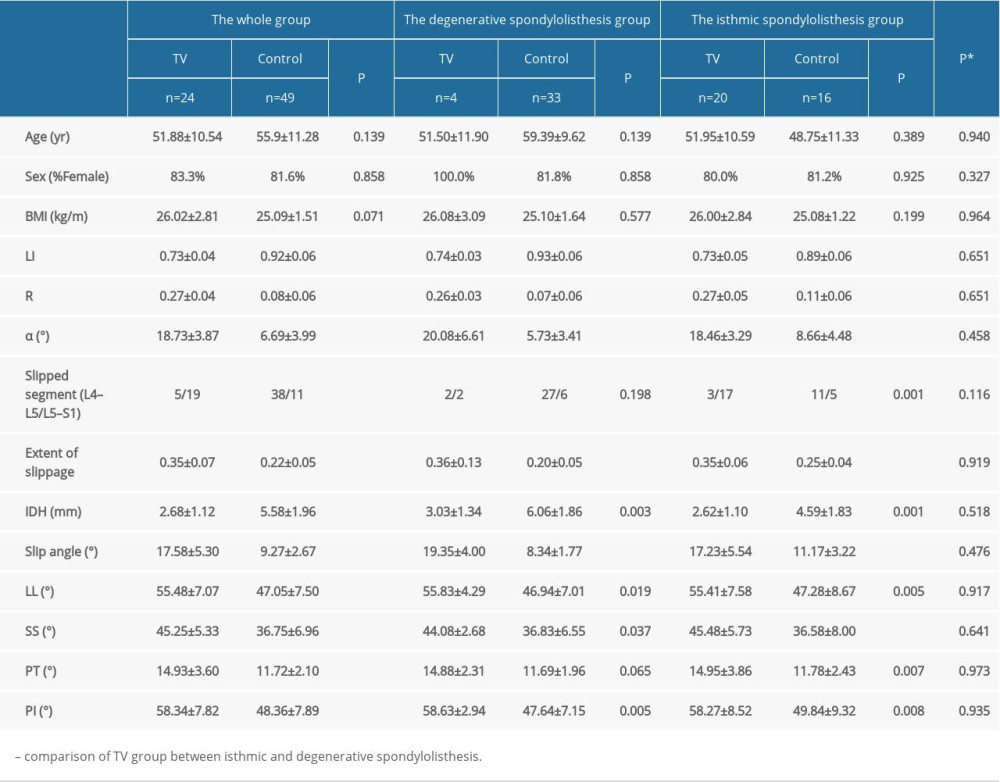 Table 3. Pearson correlation analysis between LI of slipped vertebra and clinical characteristics.
Table 3. Pearson correlation analysis between LI of slipped vertebra and clinical characteristics.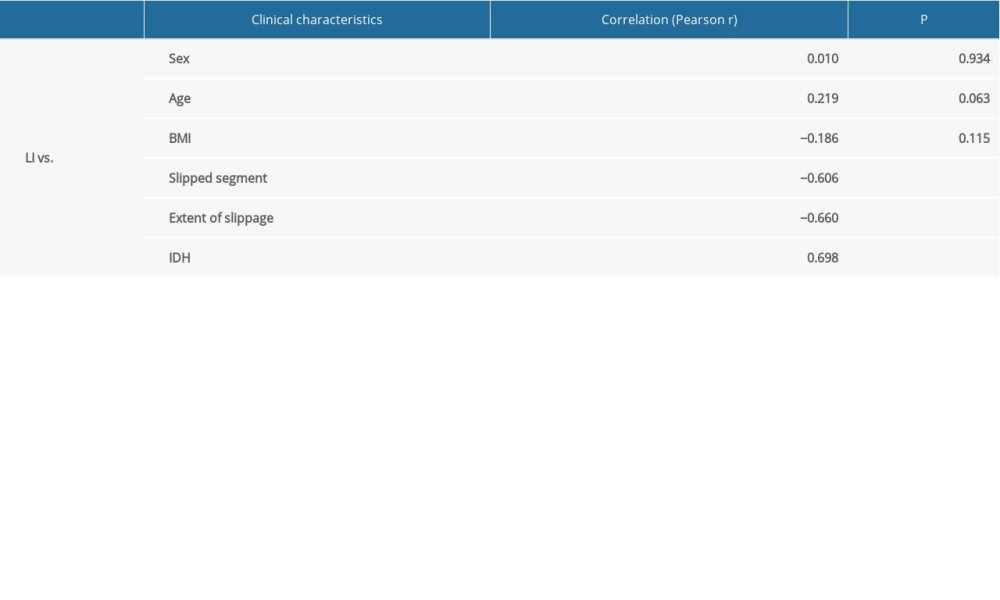 Table 4. Multiple regression model for trapezoid deformation of slipped vertebral body.
Table 4. Multiple regression model for trapezoid deformation of slipped vertebral body.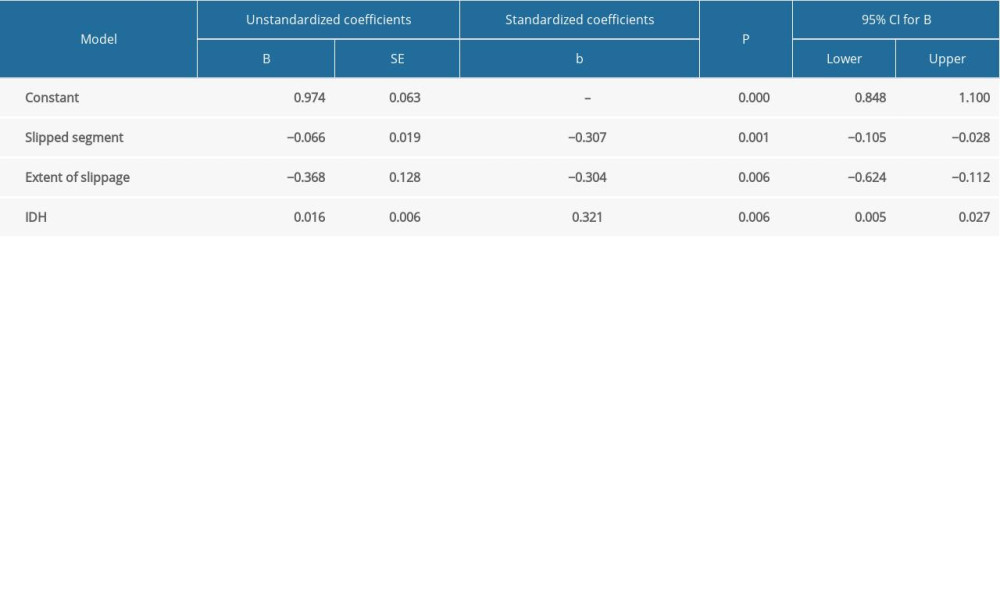 Table 5. Pearson correlation analysis between LI of slipped vertebra and spine-pelvis sagittal parameters.
Table 5. Pearson correlation analysis between LI of slipped vertebra and spine-pelvis sagittal parameters.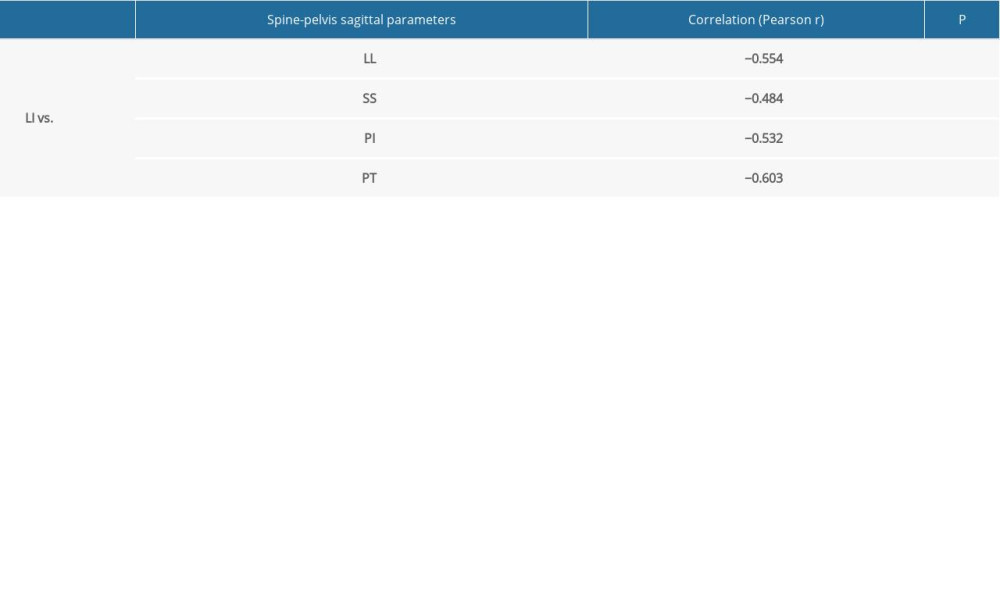 Supplementary Table 1. Intraobserver reliability.
Supplementary Table 1. Intraobserver reliability. Supplementary Table 2. Interobserver reliability.
Supplementary Table 2. Interobserver reliability.
References
1. Wiltse LL, Newman PH, Macnab I, Classification of spondylolisis and spondylolisthesis: Clin Orthop Relat Res, 1976; 117; 23-29
2. Kalichman L, Kim DH, Li L, Spondylolysis and spondylolisthesis: Prevalence and association with low back pain in the adult community-based population: Spine (Phila Pa 1976), 2009; 34; 199-205
3. Jacobsen S, Sonne-Holm S, Rovsing H, Degenerative lumbar spondylolisthesis: An epidemiological perspective: The Copenhagen Osteoarthritis Study: Spine (Phila Pa 1976), 2007; 32; 120-25
4. Yue WM, Brodner W, Gaines RW, Abnormal spinal anatomy in 27 cases of surgically corrected spondyloptosis: Proximal sacral endplate damage as a possible cause of spondyloptosis: Spine (Phila Pa 1976), 2005; 30; S22-26
5. Lindholm TS, Ragni P, Ylikoski M, Lumbar isthmic spondylolisthesis in children and adolescents. Radiologic evaluation and results of operative treatment: Spine (Phila Pa 1976), 1990; 15; 1350-55
6. Sairyo K, Katoh S, Ikata T, Development of spondylolytic olisthesis in adolescents: Spine J, 2001; 1; 171-75
7. Beutler WJ, Fredrickson BE, Murtland A, The natural history of spondylolysis and spondylolisthesis: 45-year follow-up evaluation: Spine (Phila Pa 1976), 2003; 28; 1027-35
8. Legaye J, Duval-Beaupère G, Hecquet J, Pelvic incidence: A fundamental pelvic parameter for three-dimensional regulation of spinal sagittal curves: Eur Spine J, 1998; 7; 99-103
9. Vaz G, Roussouly P, Berthonnaud E, Sagittal morphology and equilibrium of pelvis and spine: Eur Spine J, 2002; 11; 80-87
10. Zhao J, Xiao Y, Zhai X, Difference of sagittal alignment between adolescents with symptomatic lumbar isthmic spondylolisthesis and the general population: Sci Rep, 2018; 8; 10956
11. Lim JK, Kim SM, Difference of sagittal spinopelvic alignments between degenerative spondylolisthesis and isthmic spondylolisthesis: J Korean Neurosurg Soc, 2013; 53; 96-101
12. Jabłońska-Sudoł K, Maciejczak A, Relationship between the spino-pelvic parameters and the slip grade in isthmic spondylolisthesis: Neurol Neurochir Pol, 2015; 49; 381-88
13. Aono K, Kobayashi T, Jimbo S, Radiographic analysis of newly developed degenerative spondylolisthesis in a mean twelve-year prospective study: Spine (Phila Pa 1976), 2010; 35; 887-91
14. Leone A, Cianfoni A, Cerase A, Lumbar spondylolysis: A review: Skeletal Radiol, 2011; 40; 683-700
15. Kim MW, Lee KY, Lee S, Factors associated with the symptoms of young adults with L5 spondylolysis: Asian Spine J, 2018; 12; 476-83
16. Ward CV, Latimer B, Human evolution and the development of spondylolysis: Spine (Phila Pa 1976), 2005; 30; 1808-14
17. Terai T, Sairyo K, Goel VK, Spondylolysis originates in the ventral aspect of the pars interarticularis: A clinical and biomechanical study: J Bone Joint Surg Br, 2010; 92; 1123-27
18. Turner RH, Bianco AJ, Spondylolysis and spondylolisthesis in children and teen-agers: J Bone Joint Surg Am, 1971; 53; 1298-306
19. Lai Q, Gao T, Lv X, Correlation between the sagittal spinopelvic alignment and degenerative lumbar spondylolisthesis: A retrospective study: BMC Musculoskelet Disord, 2018; 19; 151
20. Roussouly P, Gollogly S, Berthonnaud E, Sagittal alignment of the spine and pelvis in the presence of L5–S1 isthmic lysis and low-grade spondylolisthesis: Spine (Phila Pa 1976), 2006; 31; 2484-90
Figures
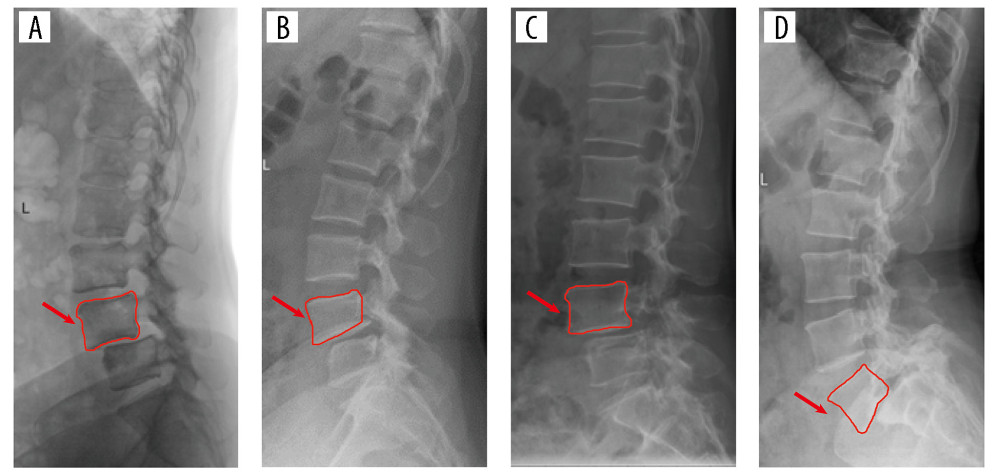 Figure 1. Degenerative spondylolisthesis: (A) Normal vertebral body, (B) Trapezoidal vertebral body; isthmic spondylolisthesis: (C) Normal vertebral body, (D) Trapezoidal vertebral body.
Figure 1. Degenerative spondylolisthesis: (A) Normal vertebral body, (B) Trapezoidal vertebral body; isthmic spondylolisthesis: (C) Normal vertebral body, (D) Trapezoidal vertebral body.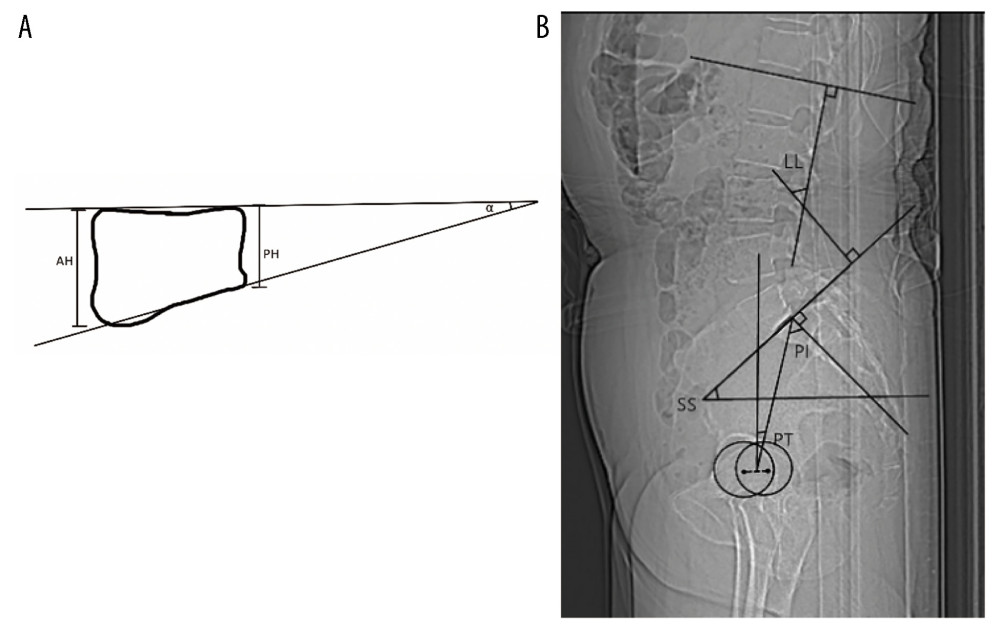 Figure 2. Visual representations of the methods applied to measure vertebral parameters and spine-pelvis sagittal parameters in radiographs are shown as follows: (A) AH: Anterior vertebral height. PH: Posterior vertebral height. Vertebral body angle (α): Angle between superior and inferior endplate of the vertebrae. (B) LL: The angle between lines parallel to the superior L1 endplate and the S1 endplate. SS: The angle between the superior S1 endplate and the horizontal plane. PT: The angle between the vertical plane and the line connecting the midpoint of the sacral endplate and the hip axis. PI: The angle between the line connecting the midpoint of the sacral endplate and the hip axis and a line perpendicular to the sacral endplate.
Figure 2. Visual representations of the methods applied to measure vertebral parameters and spine-pelvis sagittal parameters in radiographs are shown as follows: (A) AH: Anterior vertebral height. PH: Posterior vertebral height. Vertebral body angle (α): Angle between superior and inferior endplate of the vertebrae. (B) LL: The angle between lines parallel to the superior L1 endplate and the S1 endplate. SS: The angle between the superior S1 endplate and the horizontal plane. PT: The angle between the vertical plane and the line connecting the midpoint of the sacral endplate and the hip axis. PI: The angle between the line connecting the midpoint of the sacral endplate and the hip axis and a line perpendicular to the sacral endplate.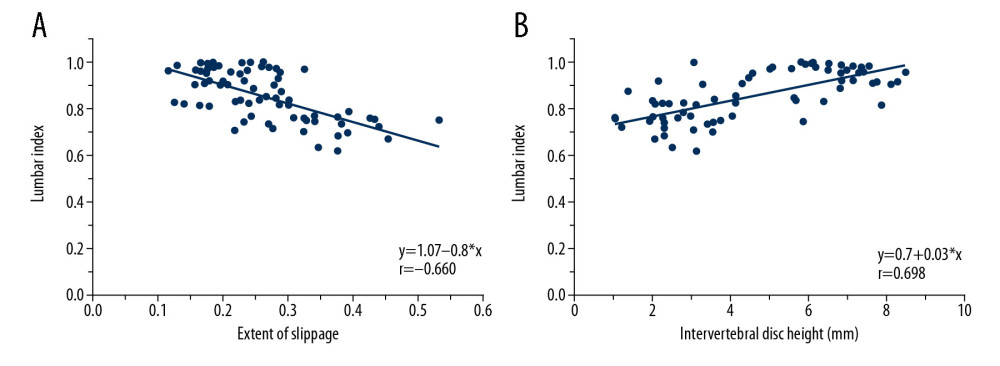 Figure 3. (A) A negative correlation was observed between the extent of slippage and the lumbar index. (B) A positive correlation was observed between the intervertebral disc height and lumbar index.
Figure 3. (A) A negative correlation was observed between the extent of slippage and the lumbar index. (B) A positive correlation was observed between the intervertebral disc height and lumbar index.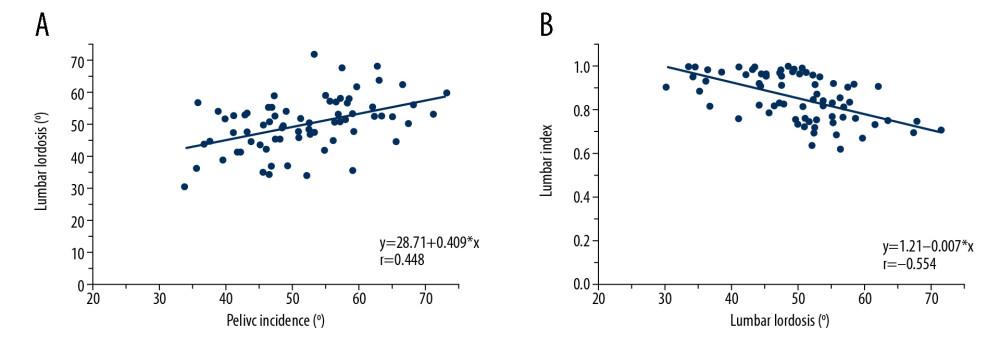 Figure 4. (A) A positive correlation was observed between pelvic incidence and lumbar lordosis. (B) A negative correlation was observed between lumbar lordosis and the lumbar index.
Figure 4. (A) A positive correlation was observed between pelvic incidence and lumbar lordosis. (B) A negative correlation was observed between lumbar lordosis and the lumbar index. Tables
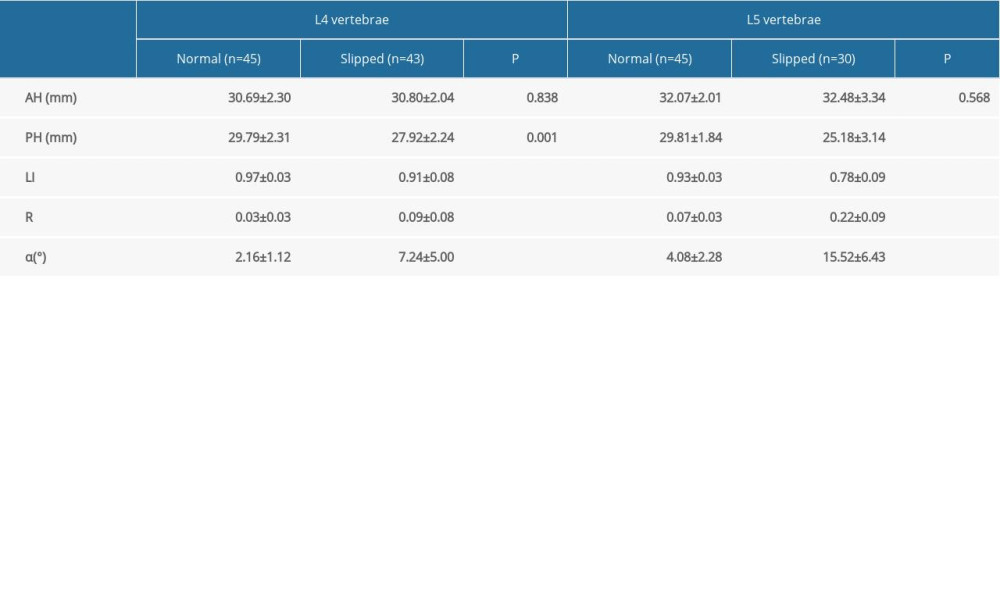 Table 1. Comparison of the parameters between slipped and normal vertebral bodies.
Table 1. Comparison of the parameters between slipped and normal vertebral bodies.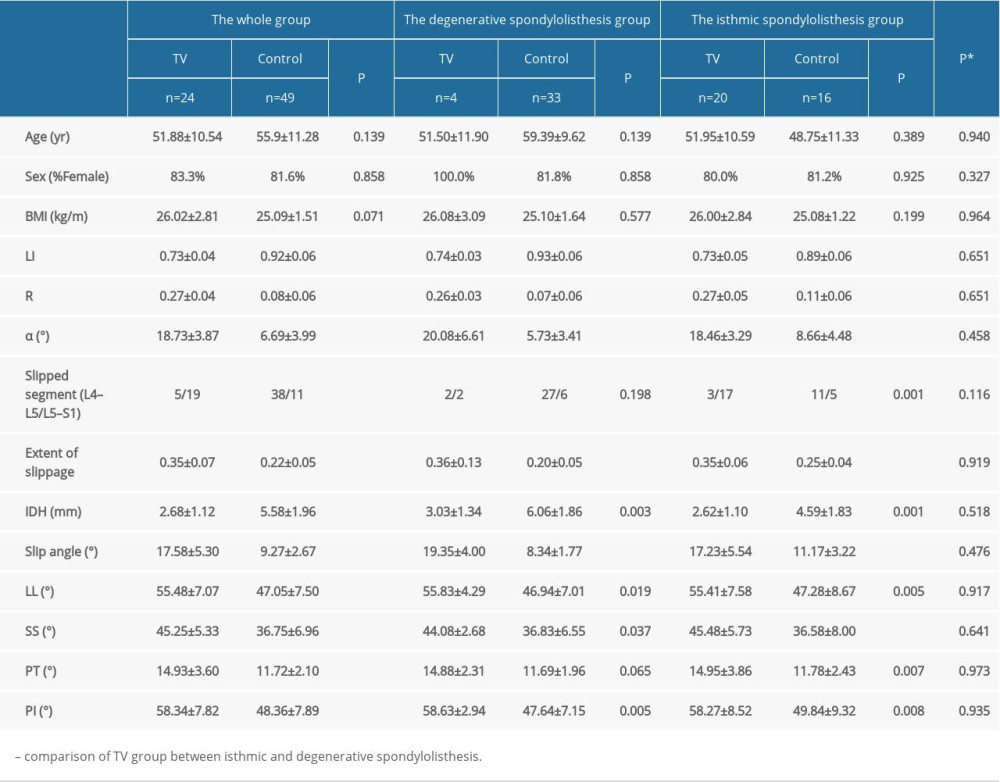 Table 2. Comparison of clinical data and spine-pelvis sagittal parameters between TV group and control group.
Table 2. Comparison of clinical data and spine-pelvis sagittal parameters between TV group and control group.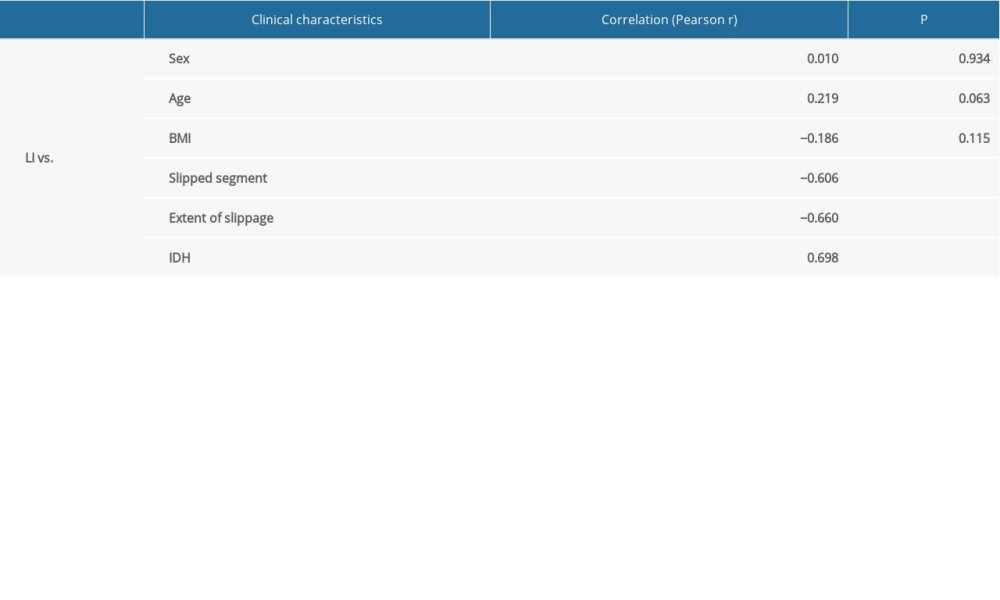 Table 3. Pearson correlation analysis between LI of slipped vertebra and clinical characteristics.
Table 3. Pearson correlation analysis between LI of slipped vertebra and clinical characteristics.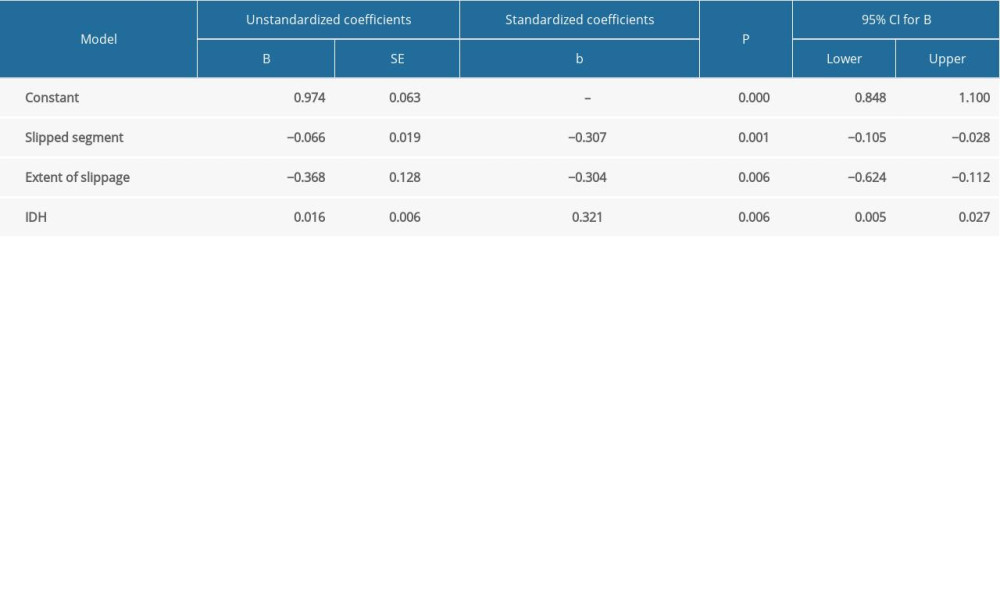 Table 4. Multiple regression model for trapezoid deformation of slipped vertebral body.
Table 4. Multiple regression model for trapezoid deformation of slipped vertebral body.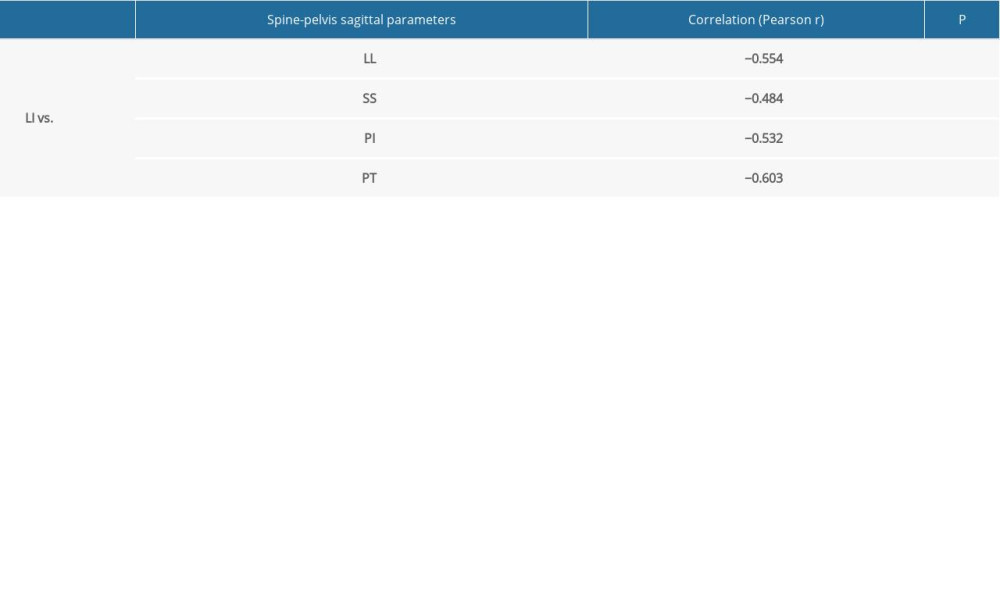 Table 5. Pearson correlation analysis between LI of slipped vertebra and spine-pelvis sagittal parameters.
Table 5. Pearson correlation analysis between LI of slipped vertebra and spine-pelvis sagittal parameters.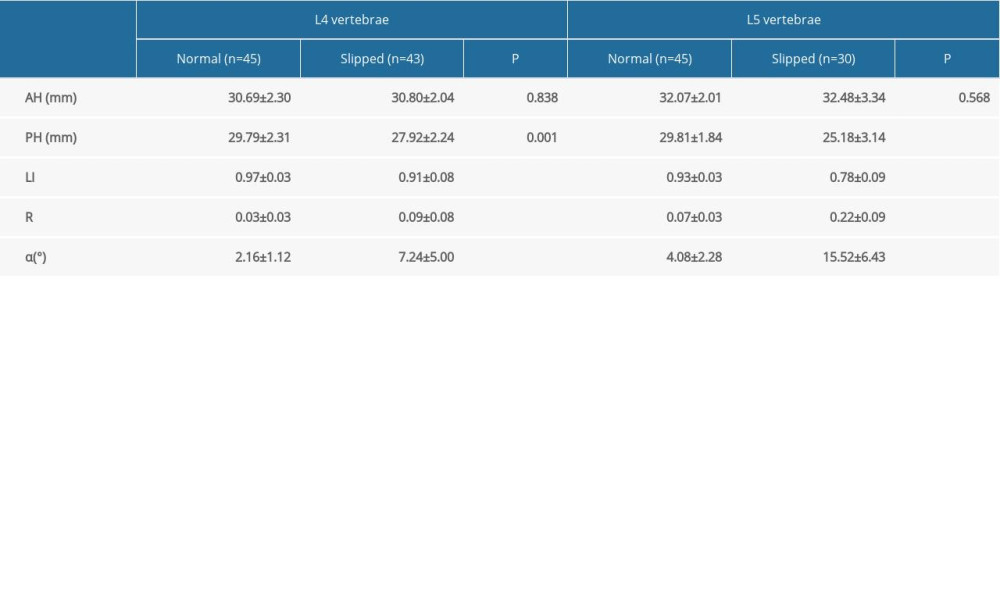 Table 1. Comparison of the parameters between slipped and normal vertebral bodies.
Table 1. Comparison of the parameters between slipped and normal vertebral bodies.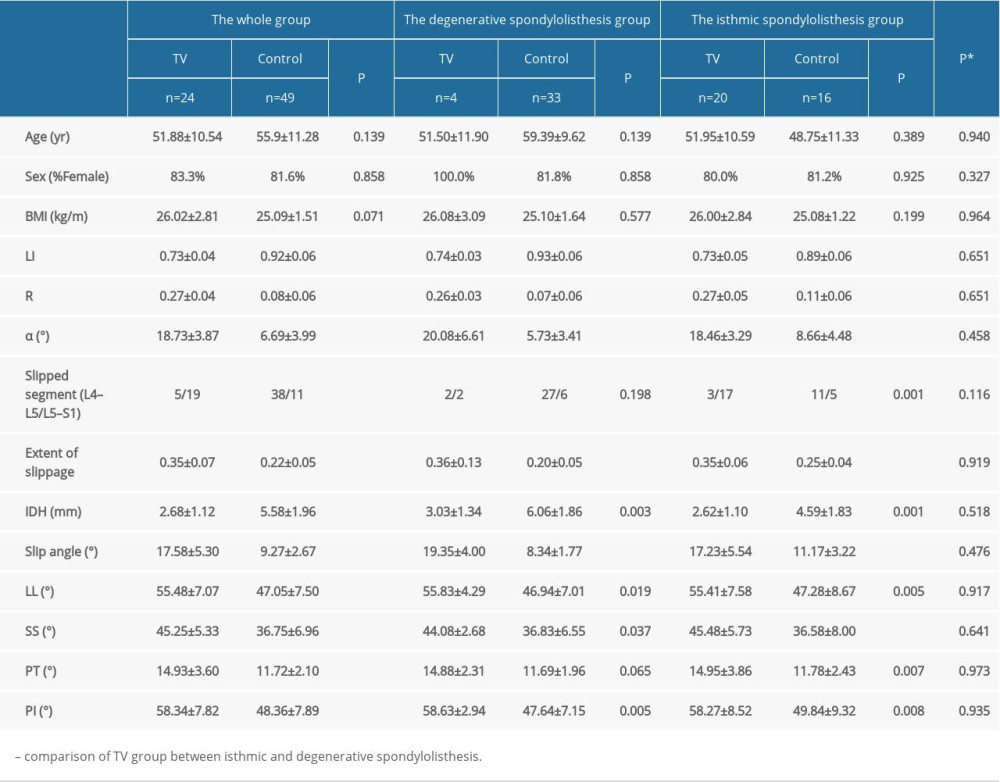 Table 2. Comparison of clinical data and spine-pelvis sagittal parameters between TV group and control group.
Table 2. Comparison of clinical data and spine-pelvis sagittal parameters between TV group and control group.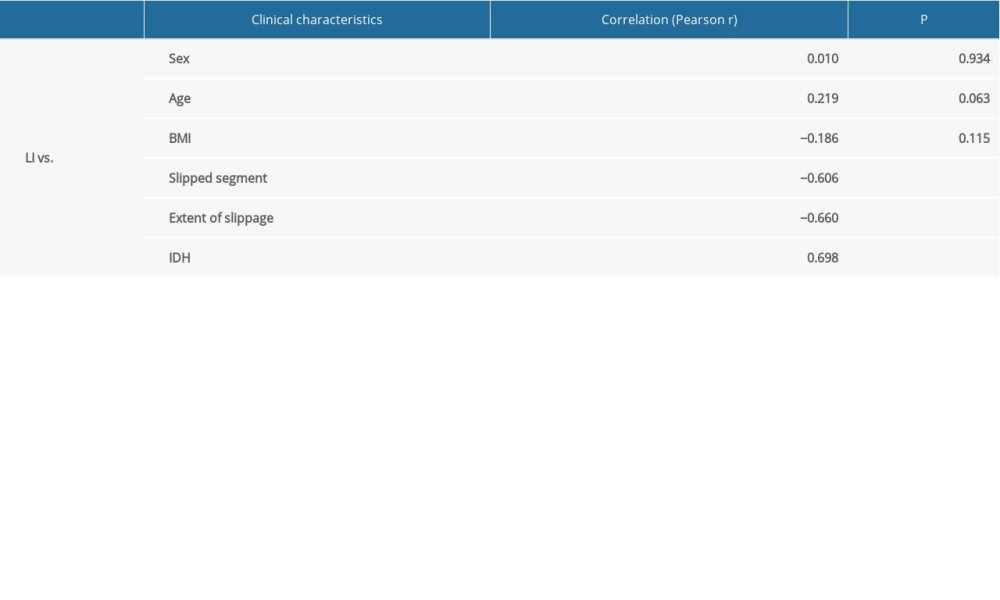 Table 3. Pearson correlation analysis between LI of slipped vertebra and clinical characteristics.
Table 3. Pearson correlation analysis between LI of slipped vertebra and clinical characteristics.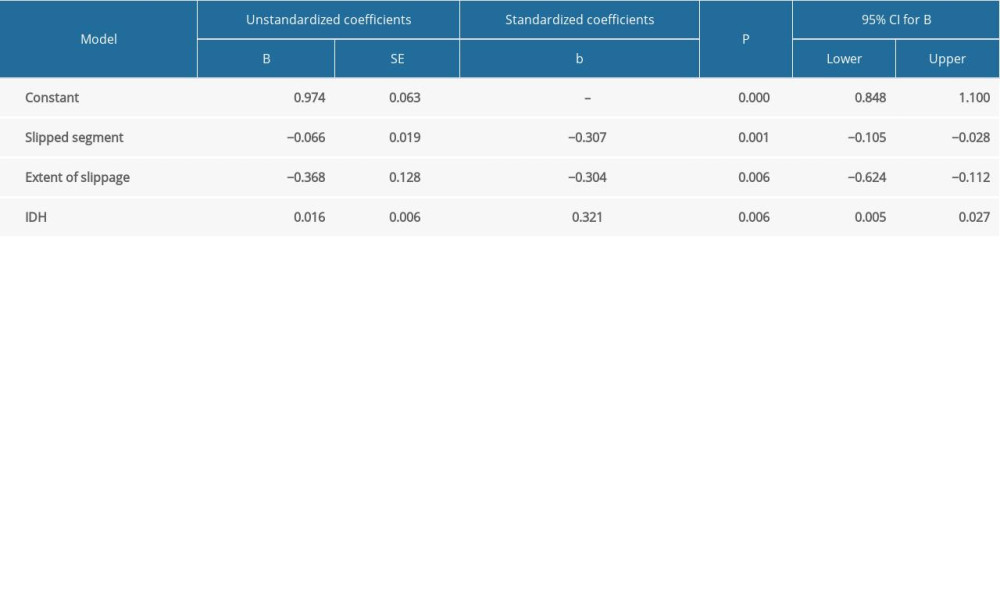 Table 4. Multiple regression model for trapezoid deformation of slipped vertebral body.
Table 4. Multiple regression model for trapezoid deformation of slipped vertebral body.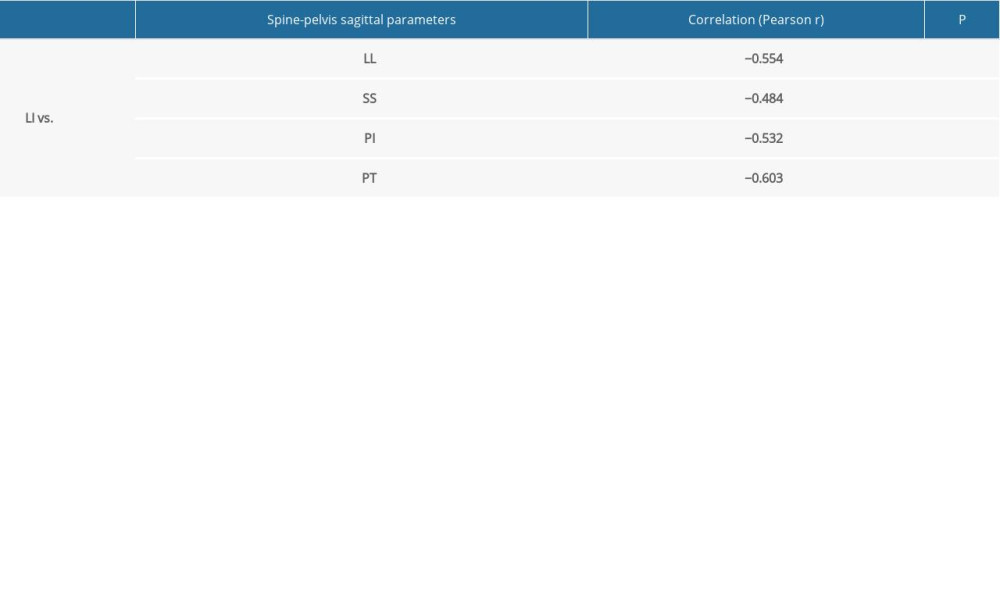 Table 5. Pearson correlation analysis between LI of slipped vertebra and spine-pelvis sagittal parameters.
Table 5. Pearson correlation analysis between LI of slipped vertebra and spine-pelvis sagittal parameters. Supplementary Table 1. Intraobserver reliability.
Supplementary Table 1. Intraobserver reliability. Supplementary Table 2. Interobserver reliability.
Supplementary Table 2. Interobserver reliability. In Press
05 Mar 2024 : Clinical Research
Muscular Function Recovery from General Anesthesia in 132 Patients Undergoing Surgery with Acceleromyograph...Med Sci Monit In Press; DOI: 10.12659/MSM.942780
05 Mar 2024 : Clinical Research
Effects of Thermal Insulation on Recovery and Comfort of Patients Undergoing Holmium Laser LithotripsyMed Sci Monit In Press; DOI: 10.12659/MSM.942836
05 Mar 2024 : Clinical Research
Role of Critical Shoulder Angle in Degenerative Type Rotator Cuff Tears: A Turkish Cohort StudyMed Sci Monit In Press; DOI: 10.12659/MSM.943703
06 Mar 2024 : Clinical Research
Comparison of Outcomes between Single-Level and Double-Level Corpectomy in Thoracolumbar Reconstruction: A ...Med Sci Monit In Press; DOI: 10.12659/MSM.943797
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








