27 November 2020: Clinical Research
The Safety and Efficacy of Apatinib Treatment in Addition to Concurrent Chemoradiotherapy in Patients with Nonoperative Locally Advanced Esophageal Squamous Cell Carcinoma
Lijun Hu1ABCDEF*, Ze Kong1BCDF, Qinghong Meng1BCD, Jianlin Wang1BCF, Mengyun Zhou1BC, Jingping Yu1ACEG, Xiaodong Jiang2ACEGDOI: 10.12659/MSM.927221
Med Sci Monit 2020; 26:e927221
Abstract
BACKGROUND: Esophageal cancer is a common gastrointestinal malignancy in China. We evaluated the efficacy and safety of adding Apatinib to concurrent chemoradiotherapy in patients with locally advanced esophageal squamous cell carcinoma.
MATERIAL AND METHODS: In this single-center retrospective study, we compared short-term efficacy, long-term efficacy, and adverse events between patients who received Apatinib and concurrent chemoradiotherapy (Apatinib group), and those who received only concurrent chemoradiotherapy (CCRT group).
RESULTS: Sixty-five patients with stage II and III esophageal squamous cell carcinoma were enrolled (31 in the Apatinib group, 34 in the CCRT group). After treatment, the therapy response rate (the sum of the complete and partial remission rates) was significantly higher in the Apatinib group than in the CCRT group (P=0.045); the complete remission rate was particularly higher in the Apatinib group. Median progression-free survival in the Apatinib group (12 months) was higher than that of the CCRT group (7 months), and the 1- and 2-year progression-free survival rates were significantly higher in the Apatinib group than in the CCRT group (47.0% vs. 30.3% and 20.2% vs. 12.1%, respectively; P=0.040). The main adverse effects of Apatinib treatment were elevated blood pressure, proteinuria, hand-foot syndrome, fatigue, and oral mucositis, all of which were level 1–2. Cox multivariate regression analysis indicated T stage and short-term efficacy were independent prognostic factors for overall and progression-free survival.
CONCLUSIONS: For patients with locally advanced esophageal squamous cell carcinoma, combining Apatinib with concurrent chemoradiotherapy can improve patient survival and significantly prolong progression-free survival, with tolerable adverse reactions.
Keywords: chemoradiotherapy, Drug-Related Side Effects and Adverse Reactions, Esophageal Neoplasms, esophageal squamous cell carcinoma, Incidence, Multivariate Analysis, nomograms, Proportional Hazards Models, Time Factors
Background
Esophageal cancer is one of the most common gastrointestinal malignant cancers in China. According to a 2019 report from the National Cancer Center, China’s cases of esophageal cancer account for 43% of the global annual new cases and 37% of the annual global deaths due to this disease [1]. Among these cases, 86.3% were esophageal squamous cell carcinoma, and more than 70% of those patients had either advanced esophageal cancer or a complication of heart and lung disease as the primary diagnosis, preventing surgical treatment [2]. Radiation therapy is one of the main treatments for esophageal cancer. Although radiotherapy technology has dramatically improved in recent years, and concurrent chemoradiotherapy has shown good efficacy, the 5-year survival rate of locally advanced esophageal squamous cell carcinoma is still only 23% to 34% [3]. Apatinib is a new anti-angiogenesis small molecule drug, which can selectively inhibit the activity of VEGFR-2 tyrosine kinase and block the signal transmission of VEGF and its receptor, thus inhibiting tumor angiogenesis and tumor growth [4]. Previously, through
Material and Methods
CLINICAL DATA:
We retrospectively analyzed the records of patients admitted to the radiotherapy department of our hospital from May 2016 to April 2019. All patients had been confirmed to have esophageal squamous cell carcinoma by histopathology. The inclusion criteria were (1) age ≥18 years old; (2) Karnofsky Performance Score ≥80 points; (3) patients refused surgery or did not undergo surgery for other reasons; (4) patients received concurrent chemoradiotherapy as the treatment method, and the dose of radiotherapy was ≥50 Gy; (5) complete clinical and follow-up information was available; (6) there were no complications with serious internal disease and/or a second primary tumor. The exclusion criteria were (1) active hemorrhage or severe coagulation dysfunction; (2) severe uncontrolled hypertension; (3) severe cardiopulmonary diseases or abnormal liver and kidney function.
The age, sex, history of hypertension and diabetes, esophageal cancer location and type, TNM stage, tumor markers, treatment method (with or without Apatinib treatment), adverse reactions, and follow-up information of the enrolled patients were recorded. According to the treatment method received, the enrolled patients were divided into 2 groups: (1) concurrent chemoradiotherapy combined with Apatinib treatment (Apatinib group) and (2) concurrent chemoradiotherapy only (CCRT group) (Figure 1). All patients signed an informed consent form. The protocol of this study followed the principles of the Declaration of Helsinki and was approved by the Ethics Committee of our hospital.
TREATMENT METHODS:
The 3 treatment methods that were administered in this study were as follows:
EVALUATION CRITERIA OF SHORT-TERM EFFICACY AND ACUTE ADVERSE REACTIONS:
To evaluate treatment efficacy in the first and third months, all patients received an esophageal X-ray after swallowing barium, chest and abdomen CT, and other relevant examinations. According to WHO standards, treatment efficacy can be divided into complete remission, partial remission, stable disease, and disease progression. Complete remission and partial remission were considered clinically effective. The acute adverse reactions of radiotherapy were evaluated according to the early radiation reaction standard of the American Radiation Oncology Group, and the adverse reactions of chemotherapy were assessed according to the acute and subacute toxicity index scale of anti-cancer drugs established by the WHO.
FOLLOW-UP:
Patients were followed up every 3 months in the first 2 years after treatment and every 6 months after 2 years. Follow-up included medical history, physical examination, laboratory examination, electrocardiogram, abdominal ultrasound, esophageal barium meal, and chest CT. The overall survival (OS), progression-free survival (PFS), and local control rate were used as evaluation indexes. The follow-up ended on April 30, 2020, with a median follow-up time of 30 months (12–48 months). Two cases were lost to follow-up (2.99%).
STATISTICAL METHODS:
SPSS 26.0 software was used to perform the statistical analysis. Normally distributed continuous variables were expressed as mean±standard deviation, and non-normally distributed continuous variables were expressed as median (P50) and interquartile boundary values (P25, P75). Categorical variables were expressed as frequency (%). For comparison between groups, continuous variables were tested using the unpaired
Results
CLINICAL DATA:
A total of 65 patients were enrolled in this study, of which 31 were in the Apatinib group and 34 were in the CCRT group. The comparison of clinical data between the 2 groups is shown in Table 1.
SHORT-TERM EFFICACY EVALUATION:
After treatment, the percentage of patients who achieved complete remission and partial remission in the Apatinib group were 22.6% and 61.3%, respectively, and the combined response rate was 83.9%; the complete remission and partial remission rates in the CCRT group were 2.9% and 70.6%, respectively, and the combined response rate was 73.5%. There was a significant difference in response rate between the 2 groups (
SURVIVAL ANALYSIS:
The median OS of all patients was 16 months, and the median PFS was 9 months. The 1-year and 3-year OS rates for all patients were 67.7% and 20.0%, respectively, and the 1-year and 3-year PFS rates were 40.0% and 6.2%, respectively. In the Apatinib group, the median OS and 1-year and 3-year OS rates were 20 months and 71.0% and 24.1%, respectively; and in the CCRT group, these values were 16 months and 61.8% and 12.4%, respectively; the differences between the 2 groups were not significantly different (χ2=0.711, P=0.399, Figure 3). Moreover, the median PFS and 1-year and 2-year PFS rates in the Apatinib group were 12 months and 47.0% and 20.2%, respectively; and 7 months and 30.3% and 12.1%, respectively, in the CCRT group. These differences between the 2 groups were significantly different (χ2=4.225, P=0.040, Figure 4).
COMPARISON OF ADVERSE REACTIONS BETWEEN THE 2 GROUPS:
The main adverse reactions of Apatinib were increased blood pressure (25.8%), proteinuria (9.7%), fatigue (16.1%), hand-foot syndrome (3.2%), and oral mucositis (3.2%), all of which were level 1 to 2 adverse reactions. The incidences of radiation esophagitis, radiation pneumonia, and bone marrow suppression in the 2 groups are compared in Table 2.
ANALYSIS OF PROGNOSTIC FACTORS:
Univariate analysis showed that T stage, N stage, TNM stage, short-term efficacy, and CEA (>4.3 ng/ml) were the influencing factors of OS time (χ2=9.53–65.50, P<0.05), while sex, age, treatment group, tumor location, pathological type, and SCC (>1.5 ng/ml) had no significant effect on patient OS time (χ2=0.000–1.304, P>0.05). However, treatment group, T stage, N stage, TNM stage, short-term efficacy, and CEA (>4.3 ng/ml) were the influencing factors for PFS time (χ2=4.225–53.690, P<0.05). Cox multivariate regression analysis showed that T stage and short-term efficacy were independent prognostic factors for OS time and PFS time (Table 3). Based on this result, we constructed the nomogram for predicting OS (Figure 5) and PFS (Figure 6) of patients with nonoperative esophageal squamous cell carcinoma. The analysis showed that earlier T stage and better short-term efficacy could predict longer OS and PFS.
Discussion
The RTOG85-01 trial showed that in patients with T1-3N0-1M0 esophageal cancer, the 5-year survival rate of cisplatin/5-fluorouracil chemotherapy plus 50.4 Gy radiotherapy was significantly higher than 64 Gy radiotherapy alone [6]. This result demonstrated the efficacy of concurrent radiotherapy and chemotherapy in the nonsurgical treatment of locally advanced esophageal cancer. However, even with concurrent therapies, the local recurrence rate is still as high as 45% [6,7]. A multicenter phase II clinical trial (JCOG9516), which included 60 patients with clinical T4 and/or distant lymph node metastasis (M1 Lym) thoracic esophageal squamous cell carcinoma, found that the complete remission rate of concurrent chemoradiotherapy was only 15%, and the 2-year survival rate was 31.5% [8]. Our present study also included patients with clinical T4 esophageal squamous cell carcinoma, and we found that the median OS of the CCRT group was only 16 months, and the 2-year OS rate was only 12.4%. Therefore, for the Southeast Asia countries with a high incidence of esophageal squamous cell carcinoma, improvement of the therapeutic effect, reduction of recurrence and metastasis, and improvement of prognosis are the major goals of esophageal cancer research.
In recent years, the development of molecular targeted therapy has provided new treatment strategies for esophageal cancer. Studies have shown that patients with esophageal cancer with a high expression of VEGF had 1.82 times higher risk of death, indicating that anti-VEGF therapy may improve the efficacy and prognosis of esophageal cancer [9]. Bevacizumab was the first drug approved by the FDA for anti-tumor angiogenesis therapy and has been widely used in the treatment of colorectal cancer, non-small-cell lung cancer, glioma, cervical cancer, and ovarian cancer [10]; however, most patients with squamous cell carcinoma cannot benefit from it [11]. Apatinib is a new small molecule tyrosine kinase inhibitor. It can selectively suppress VEGFR-2 tyrosine kinase activity, block its downstream signal transduction, and effectively inhibit tumor angiogenesis. The phase III clinical study conducted by Li et al. [12] (registration number: NCT01512745) showed that, in patients with advanced gastric cancer or adenocarcinoma of the gastroesophageal junction that failed second-line standard chemotherapy or above, the median OS and median PFS of the Apatinib group were both significantly longer than those of the placebo group (6.5 months
Through
Univariate analysis in the present study indicated that the combined use of Apatinib could improve the prognosis of patients with locally advanced esophageal squamous cell carcinoma, but it was not a prognostic factor in Cox multivariate regression analysis, and the only independent influencing factors were short-term efficacy and T stage. This result was consistent with the observations in our
This study had several limitations. First, the study was a single-center retrospective study, which could have caused the bias in the selection of patients receiving Apatinib treatment. Second this study had a relatively small sample size. Third, the WHO criteria that we used were not as practical as, for instance, the response evaluation criteria in solid tumors (RECIST). Although these limitations existed in our research, we still observed the benefits of Apatinib treatment in patients with esophageal squamous cell carcinoma. However, a large sample and randomized multicenter prospective clinical trial is needed to confirm our results.
Conclusions
In summary, for patients with locally advanced esophageal squamous cell carcinoma, the combined use of Apatinib and concurrent chemoradiotherapy can improve patient survival and significantly prolong PFS, with tolerable adverse reactions.
Figures
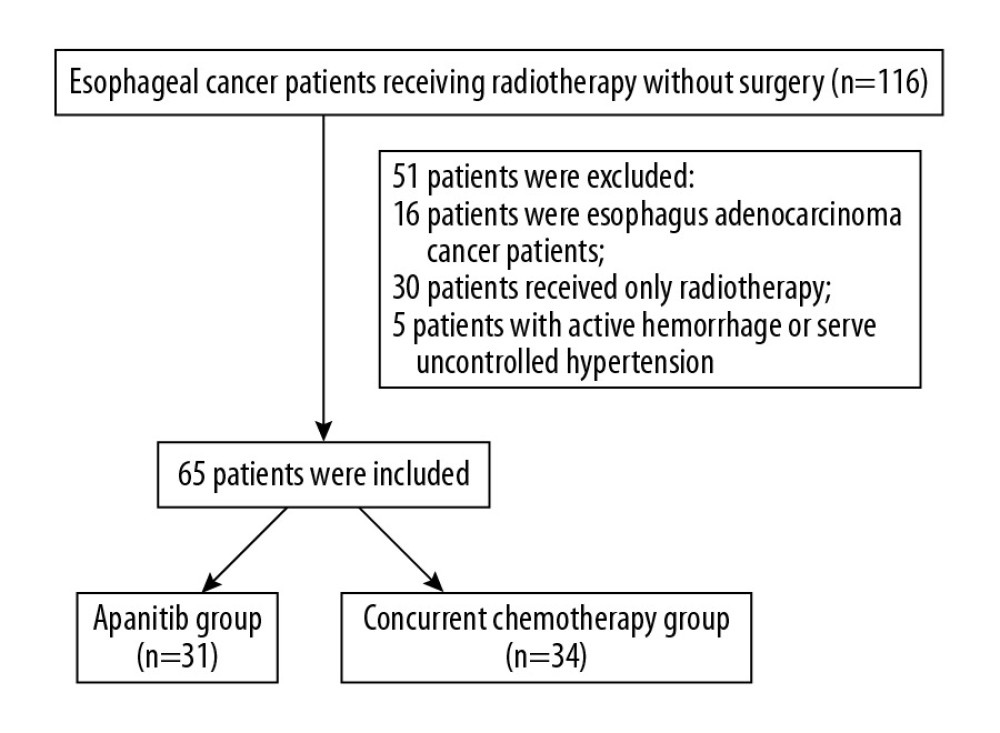 Figure 1. Flowchart of the study.
Figure 1. Flowchart of the study. 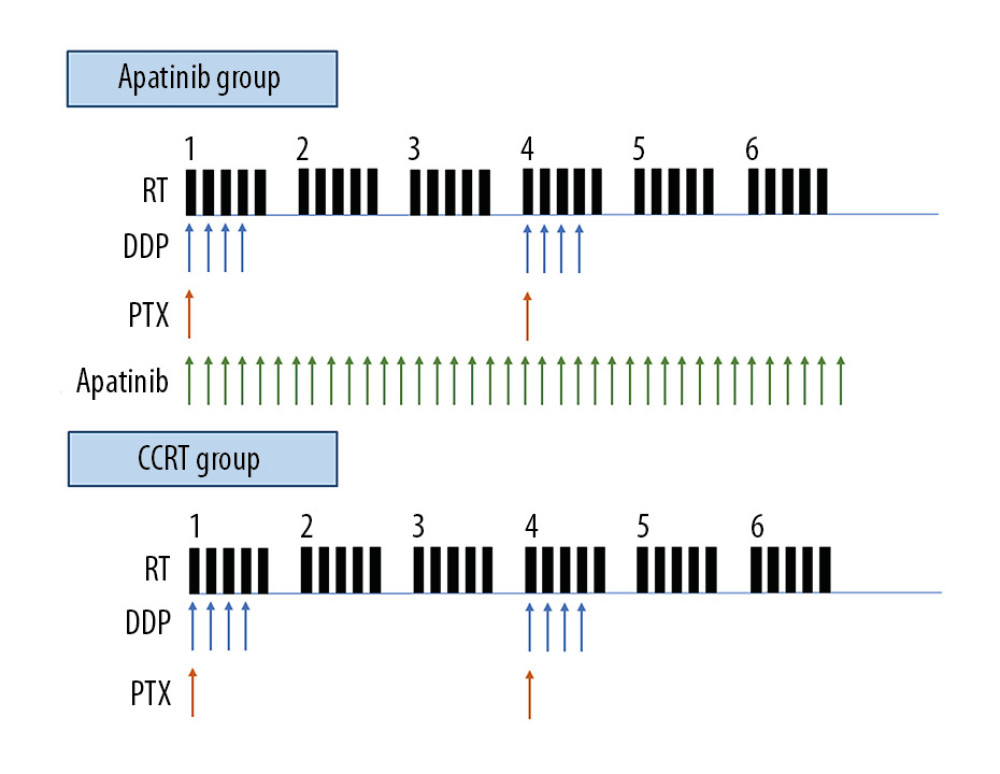 Figure 2. Schematic of the treatment plan for the chemoradiotherapy plus Apatinib (Apatinib) group and the concurrent chemoradiotherapy only (CCRT) group.
Figure 2. Schematic of the treatment plan for the chemoradiotherapy plus Apatinib (Apatinib) group and the concurrent chemoradiotherapy only (CCRT) group. 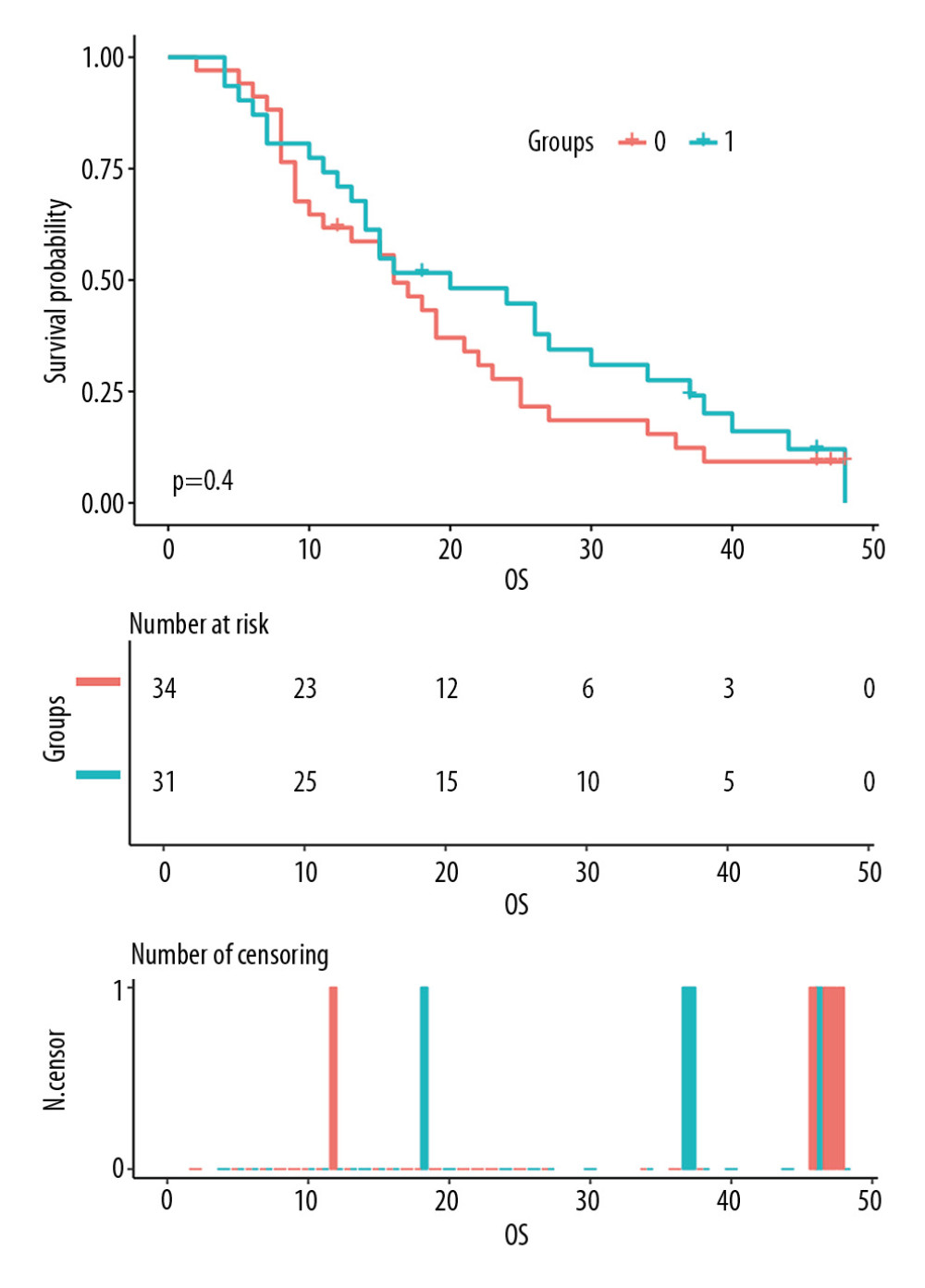 Figure 3. Comparison of overall survival (OS) between the chemoradiotherapy plus Apatinib (Apatinib) group and the concurrent chemoradiotherapy only (CCRT) group. Group 1: Apatinib group; Group 0: CCRT group.
Figure 3. Comparison of overall survival (OS) between the chemoradiotherapy plus Apatinib (Apatinib) group and the concurrent chemoradiotherapy only (CCRT) group. Group 1: Apatinib group; Group 0: CCRT group. 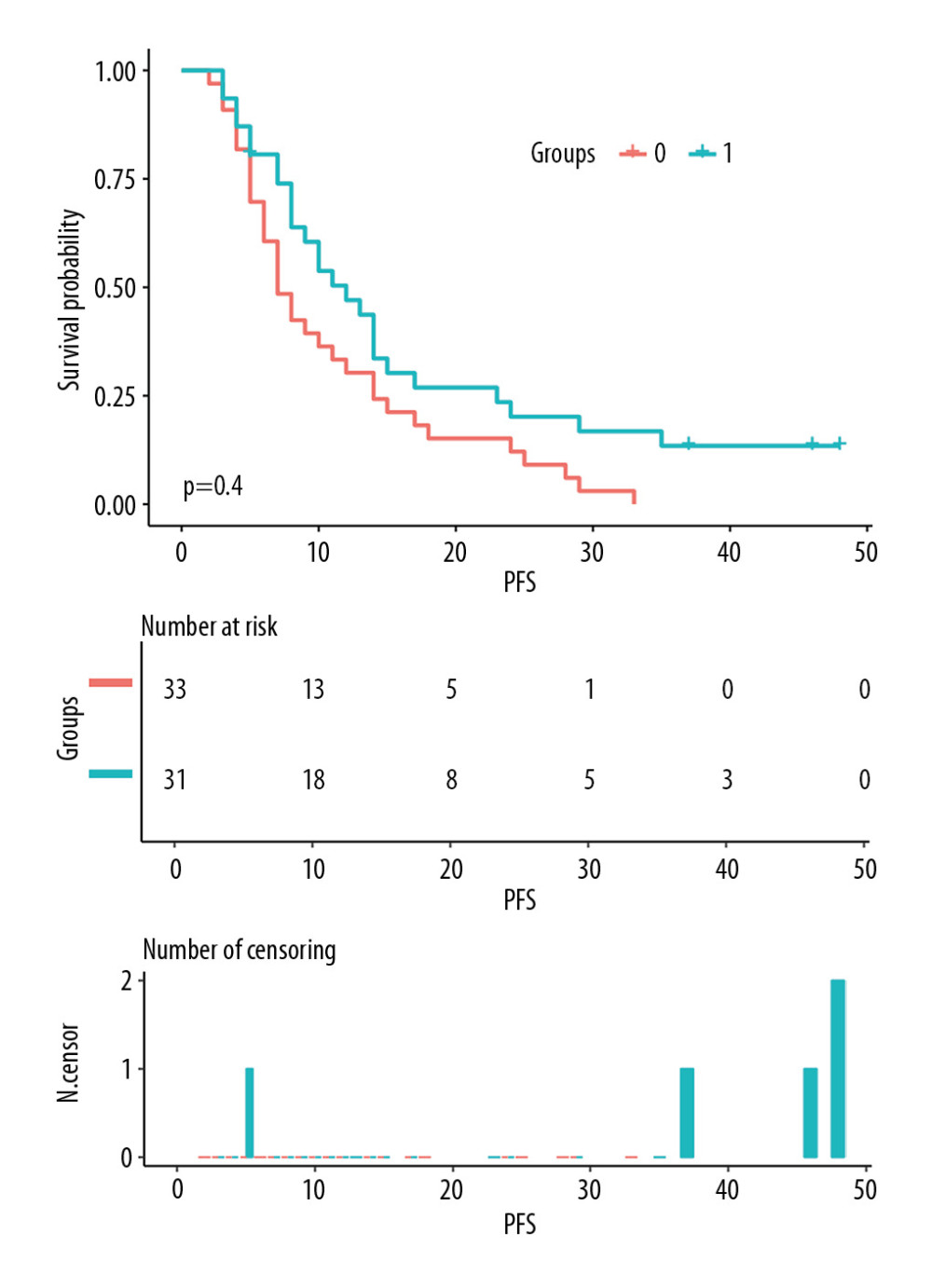 Figure 4. Comparison of progression-free survival (PFS) between the chemoradiotherapy plus Apatinib (Apatinib) group and the concurrent chemoradiotherapy only (CCRT) group. Group 1: Apatinib group; Group 0: CCRT group.
Figure 4. Comparison of progression-free survival (PFS) between the chemoradiotherapy plus Apatinib (Apatinib) group and the concurrent chemoradiotherapy only (CCRT) group. Group 1: Apatinib group; Group 0: CCRT group. 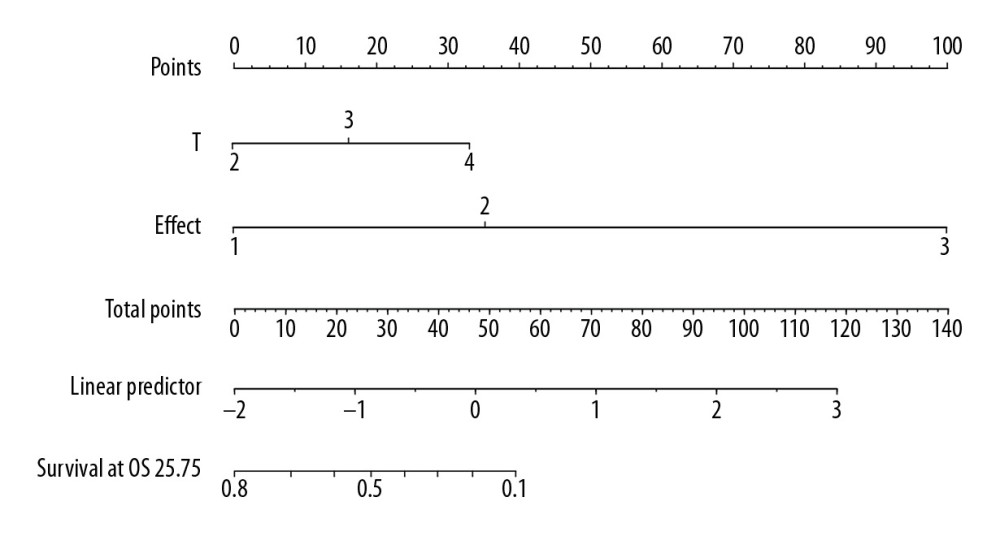 Figure 5. The nomogram predicting the overall survival time of patients with locally advanced esophageal squamous cell carcinoma.
Figure 5. The nomogram predicting the overall survival time of patients with locally advanced esophageal squamous cell carcinoma. 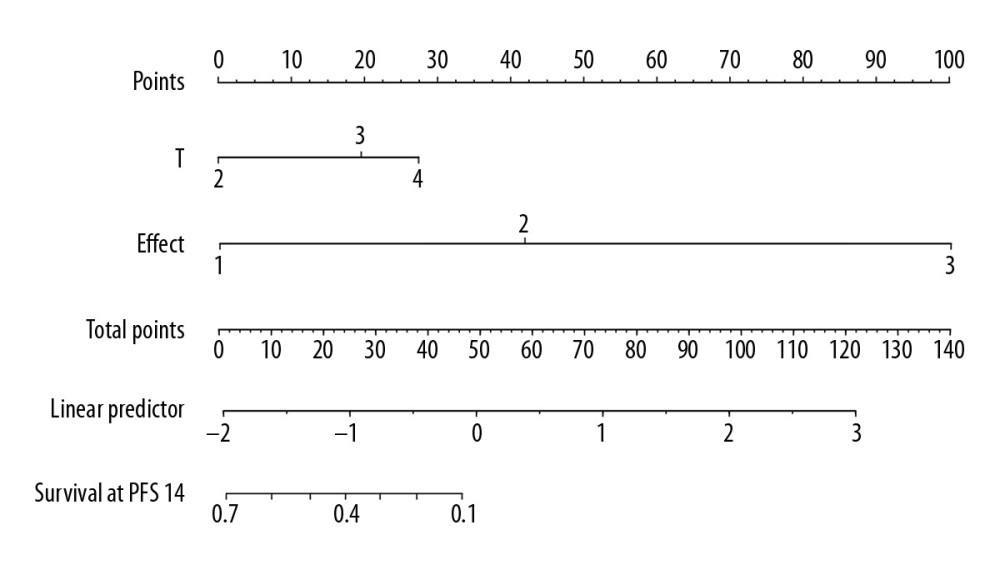 Figure 6. The nomogram predicting the progression-free survival time of patients with locally advanced esophageal squamous cell carcinoma.
Figure 6. The nomogram predicting the progression-free survival time of patients with locally advanced esophageal squamous cell carcinoma. Tables
Table 1. Baseline characteristics of study participants.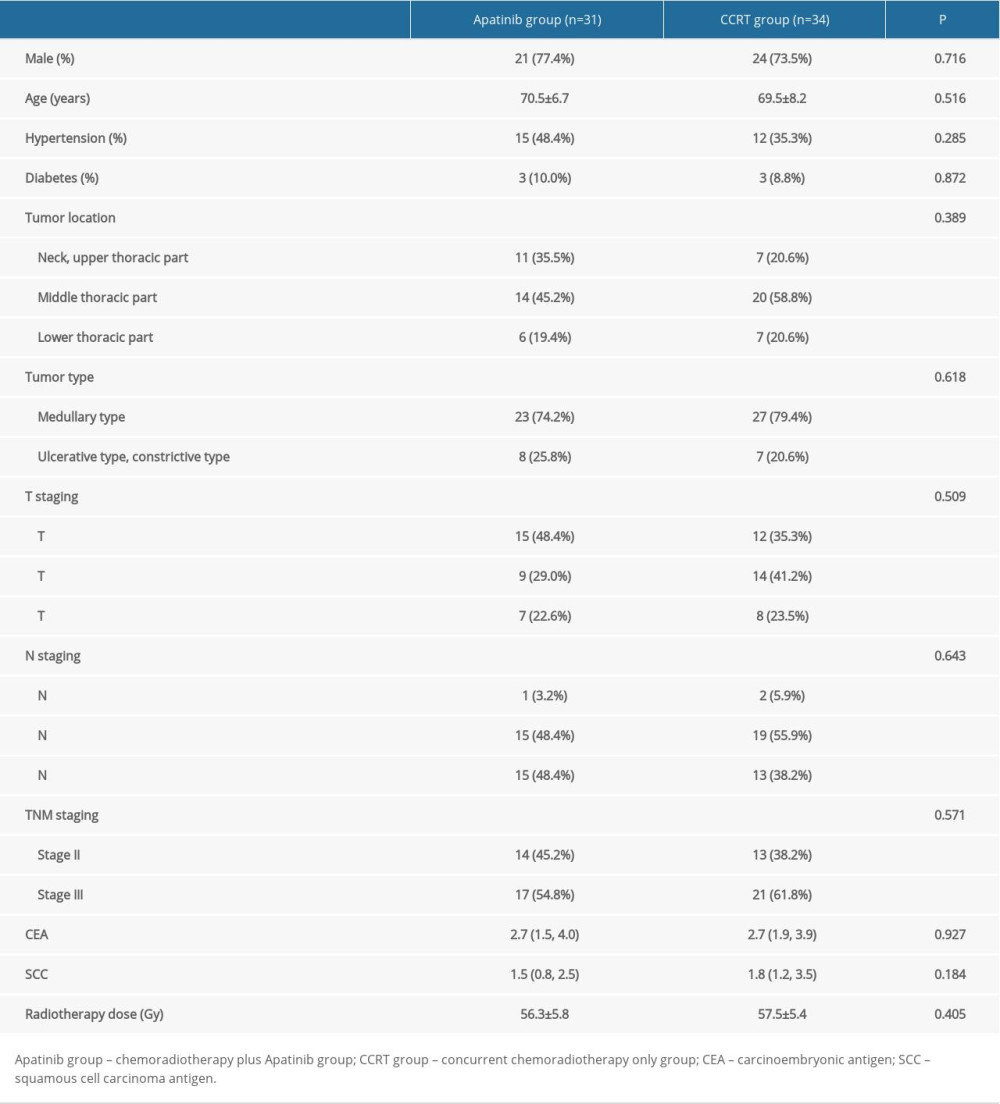 Table 2. Comparing the incidences of radiation esophagitis, radiation pneumonia, and bone marrow suppression between the 2 groups.
Table 2. Comparing the incidences of radiation esophagitis, radiation pneumonia, and bone marrow suppression between the 2 groups.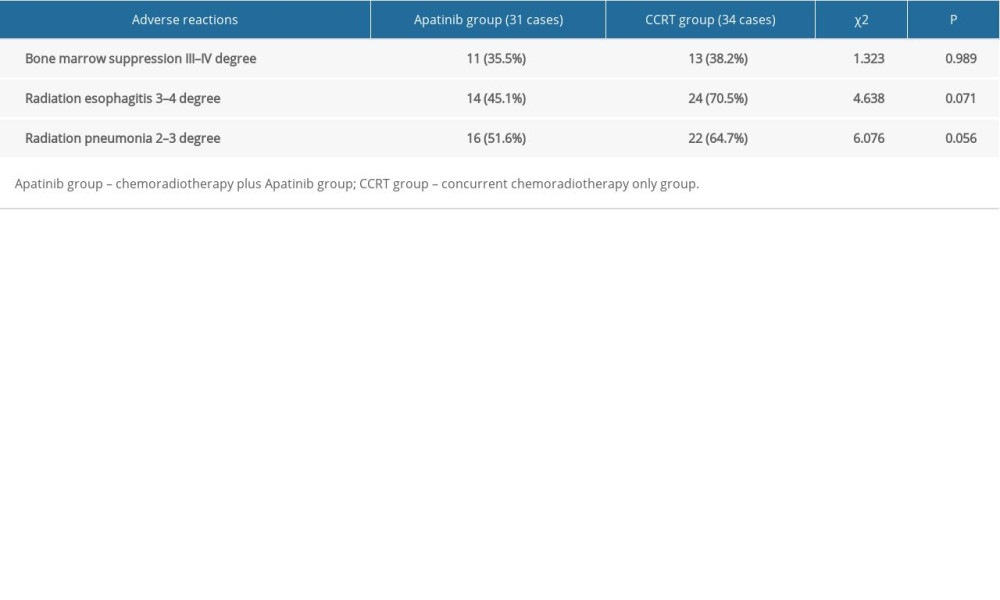 Table 3. Cox multivariate regression analysis of the prognostic factors for nonoperative esophageal squamous cell carcinoma patients.
Table 3. Cox multivariate regression analysis of the prognostic factors for nonoperative esophageal squamous cell carcinoma patients.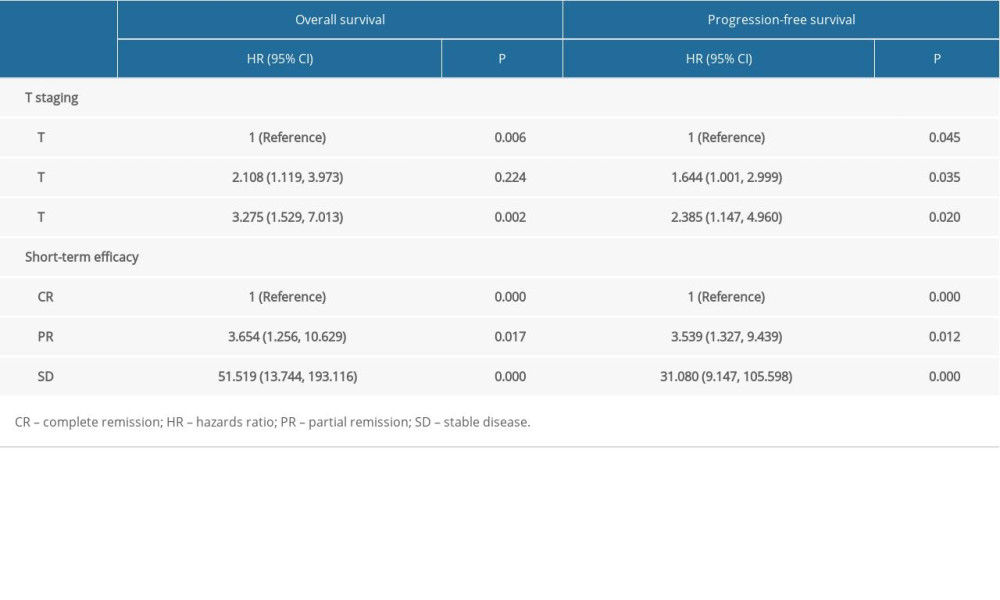
References
1. Sun K, Zheng R, Zhang S, Report of cancer incidence and mortality in different areas of China, 2015: Chin J Cancer, 2019; 28; 1-11
2. Wang X, Wang L, Chen J, Prognostic analysis of definitive three-dimensional radiotherapy for non-surgically resectable esophageal squamous cell carcinoma: A multi-center retrospective study (3JECROG R-01): Chin J Radiat Oncol, 2018; 27; 959-64
3. Welsh J, Settle SH, Amini A, Failure patterns in patients with esophageal cancer treated with definitive chemoradiation: Cancer, 2012; 118; 2632-40
4. Yanwei L, Feng H, Ren P, Safety and efficacy of Apatinib monotherapy for unresectable, metastatic esophageal cancer: A single-arm, open-label, phase II study: Oncologist, 2020 [Online ahead of print]
5. Hu L, Sun F, Sun Z, Apatinib enhances the radiosensitivity of the esophageal cancer cell line KYSE-150 by inducing apoptosis and cell cycle redistribution: Oncol Lett, 2019; 17; 1609-16
6. Cooper JS, Guo MD, Herskovic A, Chemoradiotherapy of locally advanced esophageal cancer: Long-term follow-up of a prospective randomized trial (RTOG 85-01). Radiation Therapy Oncology Group: JAMA, 1999; 281; 1623-27
7. Minsky BD, Pajak TF, Ginsberg RJ, INT 0123 (Radiation Therapy Oncology Group 94-05) phase III trial of combined-modality therapy for esophageal cancer: High-dose versus standard-dose radiation therapy: J Clin Oncol, 2002; 20; 1167-74
8. Ishida K, Ando N, Yamamoto S, Phase II study of cisplatin and 5-fluorouracil with concurrent radiotherapy in advanced squamous cell carcinoma of the esophagus: A Japan Esophageal Oncology Group (JEOG)/Japan Clinical Oncology Group trial (JCOG9516): Jpn J Clin Oncol, 2004; 34; 615-19
9. Wang J, Yu JP, Wang JLPathologic response and changes of serum VEGF during chemoradiotherapy may predict prognosis in non-surgical patients with esophageal carcinoma: Zhonghua Zhong Liu Za Zhi, 2016; 38; 589-95 [in Chinese]
10. Teleanu RI, Chircov C, Grumezescu AM, Teleanu DM, Tumor angiogenesis and anti-angiogenic strategies for cancer treatment: J Clin Med, 2019; 9(1); 84
11. Manzo A, Montanino A, Carillio G, Angiogenesis inhibitors in NSCLC: Int J Mol Sci, 2017; 18; 2021
12. Li J, Qin S, Xu J, Randomized, double-blind, placebo-controlled phase III trial of Apatinib in patients with chemotherapy-refractory advanced or metastatic adenocarcinoma of the stomach or gastroesophageal junction: J Clin Oncol, 2016; 34; 1448-54
13. Tang J, Li XY, Liang JB, Apatinib plus chemotherapy shows clinical activity in advanced NSCLC: A retrospective study: Oncol Res, 2019; 27; 635-41
14. Liao J, Jin H, Li S, Apatinib potentiates irradiation effect via suppressing PI3K/AKT signaling pathway in hepatocellular carcinoma: J Exp Clin Cancer Res, 2019; 38; 454
15. Liu J, Liu Q, Li Y, Efficacy and safety of camrelizumab combined with apatinib in advanced triple-negative breast cancer: An open-label phase II trial: J Immunother Cancer, 2020; 8(1); e000696
16. Feng Y, Zhou MY, Sun FThe inhibition effects of apatinib on cell proliferation, migration and apoptosis in esophageal carcinoma via Ras/Raf/MEK/ERK and JAK2/STAT3 pathways: Zhonghua Zhong Liu Za Zhi, 2019; 41; 263-75 [in Chinese]
17. Sun NN, Liu C, Ge XL, Wang J, Dynamic contrast-enhanced MRI for advanced esophageal cancer response assessment after concurrent chemoradiotherapy: Diagn Interv Radiol, 2018; 24; 195-202
Figures
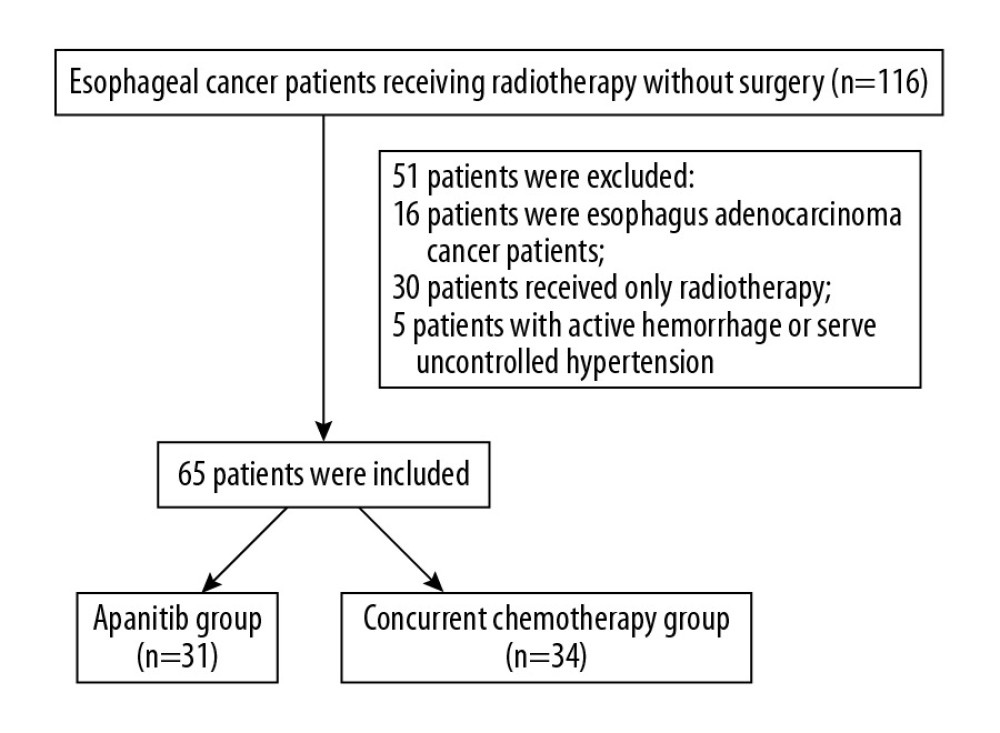 Figure 1. Flowchart of the study.
Figure 1. Flowchart of the study.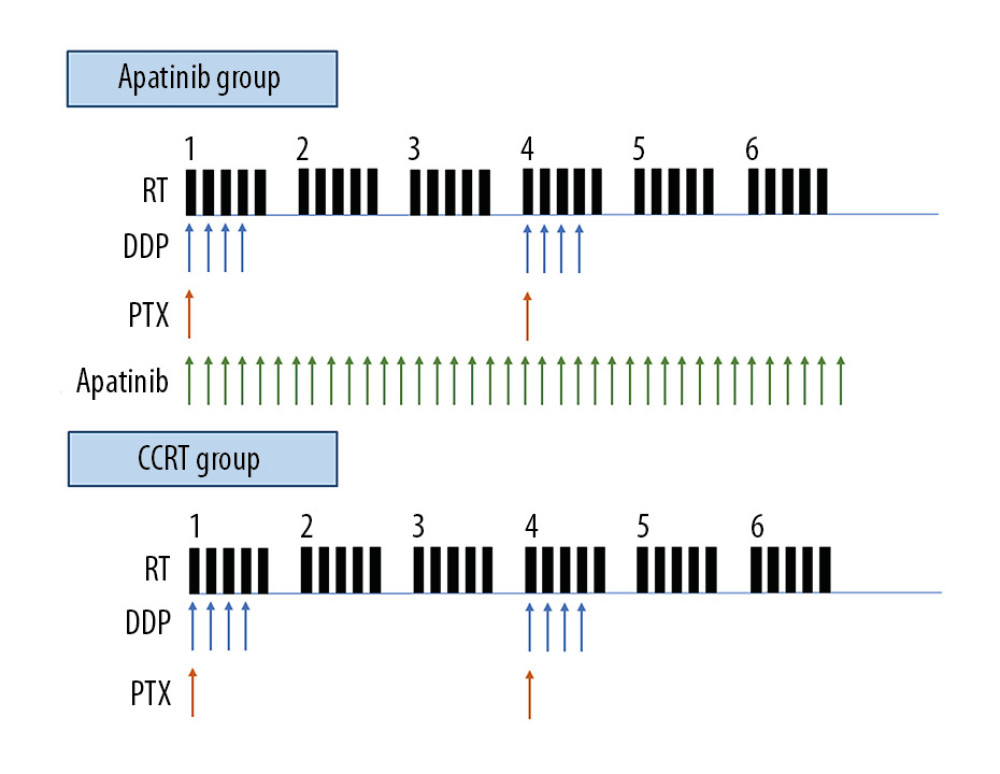 Figure 2. Schematic of the treatment plan for the chemoradiotherapy plus Apatinib (Apatinib) group and the concurrent chemoradiotherapy only (CCRT) group.
Figure 2. Schematic of the treatment plan for the chemoradiotherapy plus Apatinib (Apatinib) group and the concurrent chemoradiotherapy only (CCRT) group.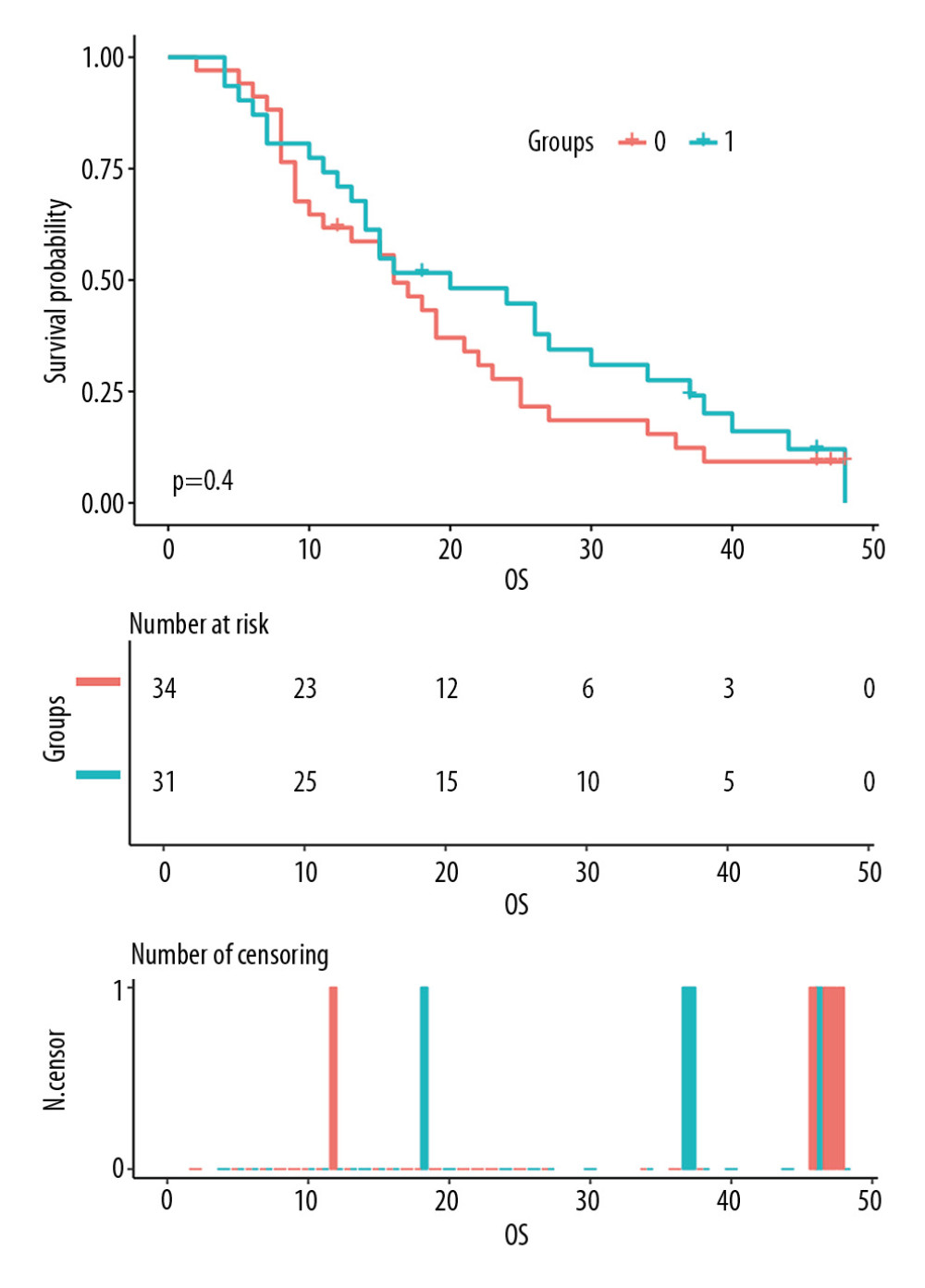 Figure 3. Comparison of overall survival (OS) between the chemoradiotherapy plus Apatinib (Apatinib) group and the concurrent chemoradiotherapy only (CCRT) group. Group 1: Apatinib group; Group 0: CCRT group.
Figure 3. Comparison of overall survival (OS) between the chemoradiotherapy plus Apatinib (Apatinib) group and the concurrent chemoradiotherapy only (CCRT) group. Group 1: Apatinib group; Group 0: CCRT group.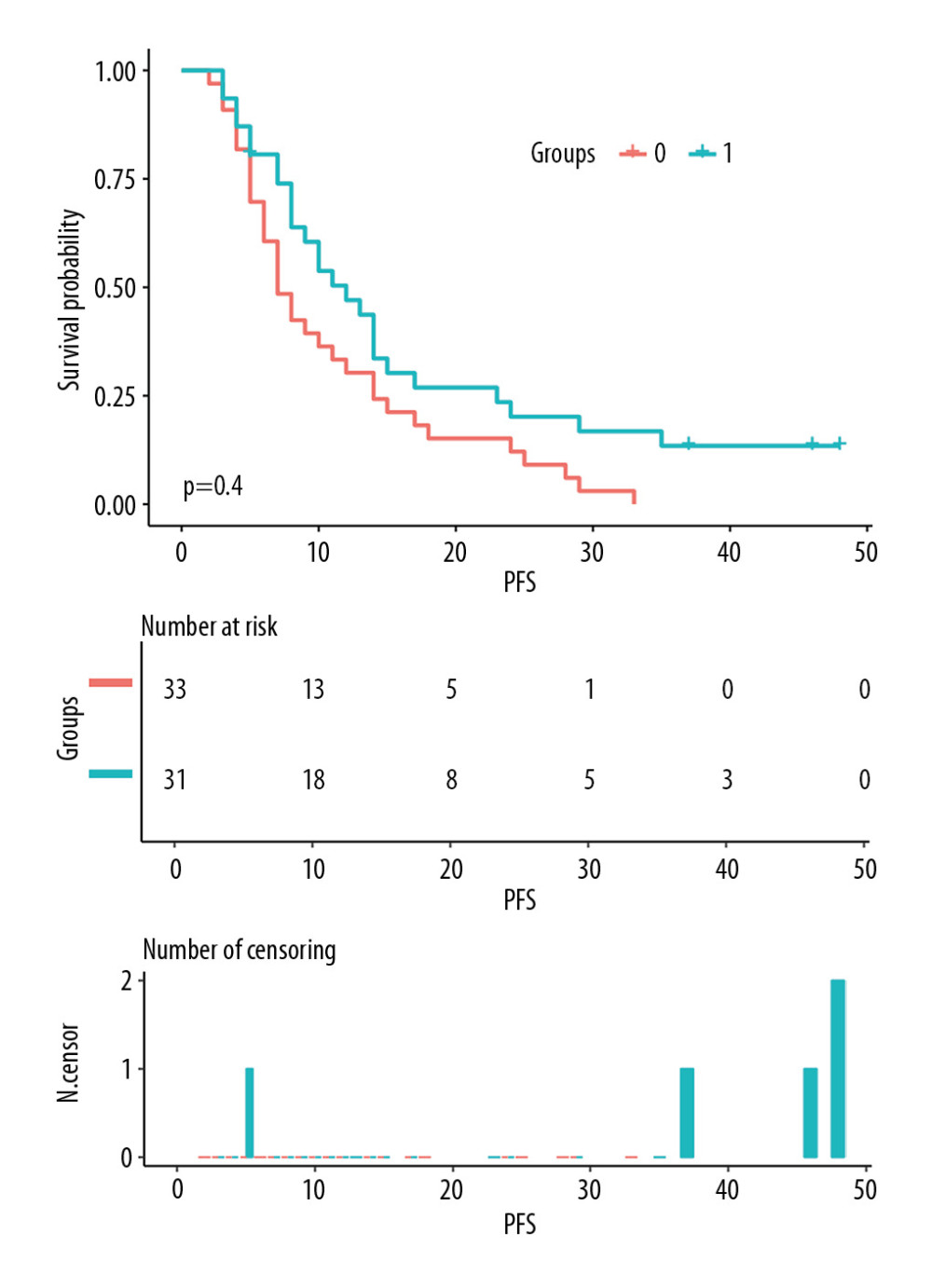 Figure 4. Comparison of progression-free survival (PFS) between the chemoradiotherapy plus Apatinib (Apatinib) group and the concurrent chemoradiotherapy only (CCRT) group. Group 1: Apatinib group; Group 0: CCRT group.
Figure 4. Comparison of progression-free survival (PFS) between the chemoradiotherapy plus Apatinib (Apatinib) group and the concurrent chemoradiotherapy only (CCRT) group. Group 1: Apatinib group; Group 0: CCRT group.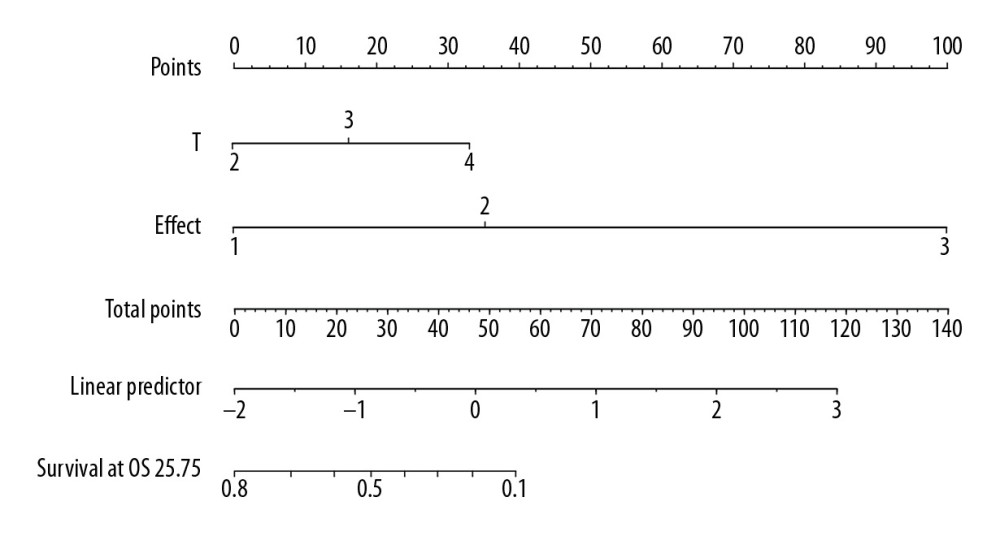 Figure 5. The nomogram predicting the overall survival time of patients with locally advanced esophageal squamous cell carcinoma.
Figure 5. The nomogram predicting the overall survival time of patients with locally advanced esophageal squamous cell carcinoma.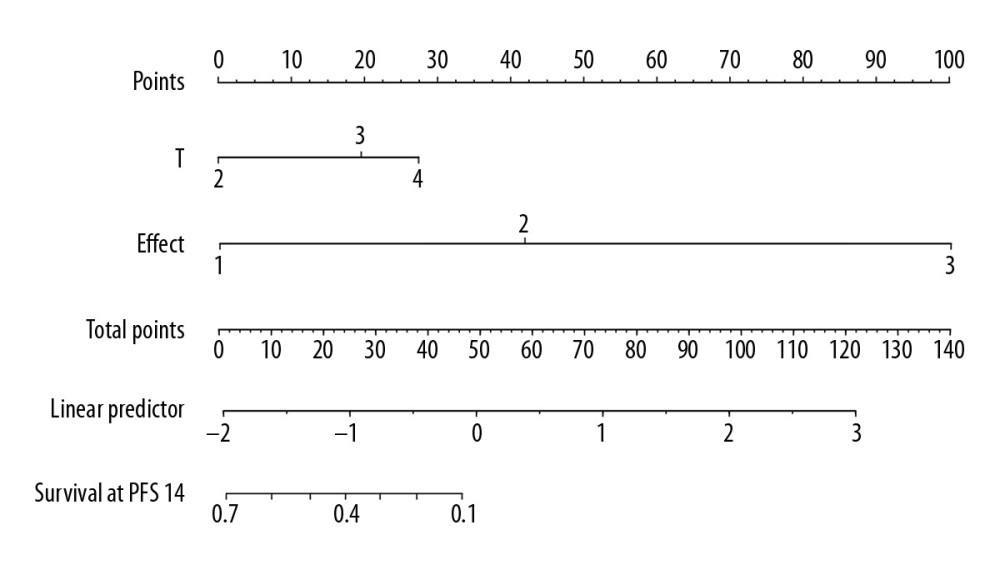 Figure 6. The nomogram predicting the progression-free survival time of patients with locally advanced esophageal squamous cell carcinoma.
Figure 6. The nomogram predicting the progression-free survival time of patients with locally advanced esophageal squamous cell carcinoma. Tables
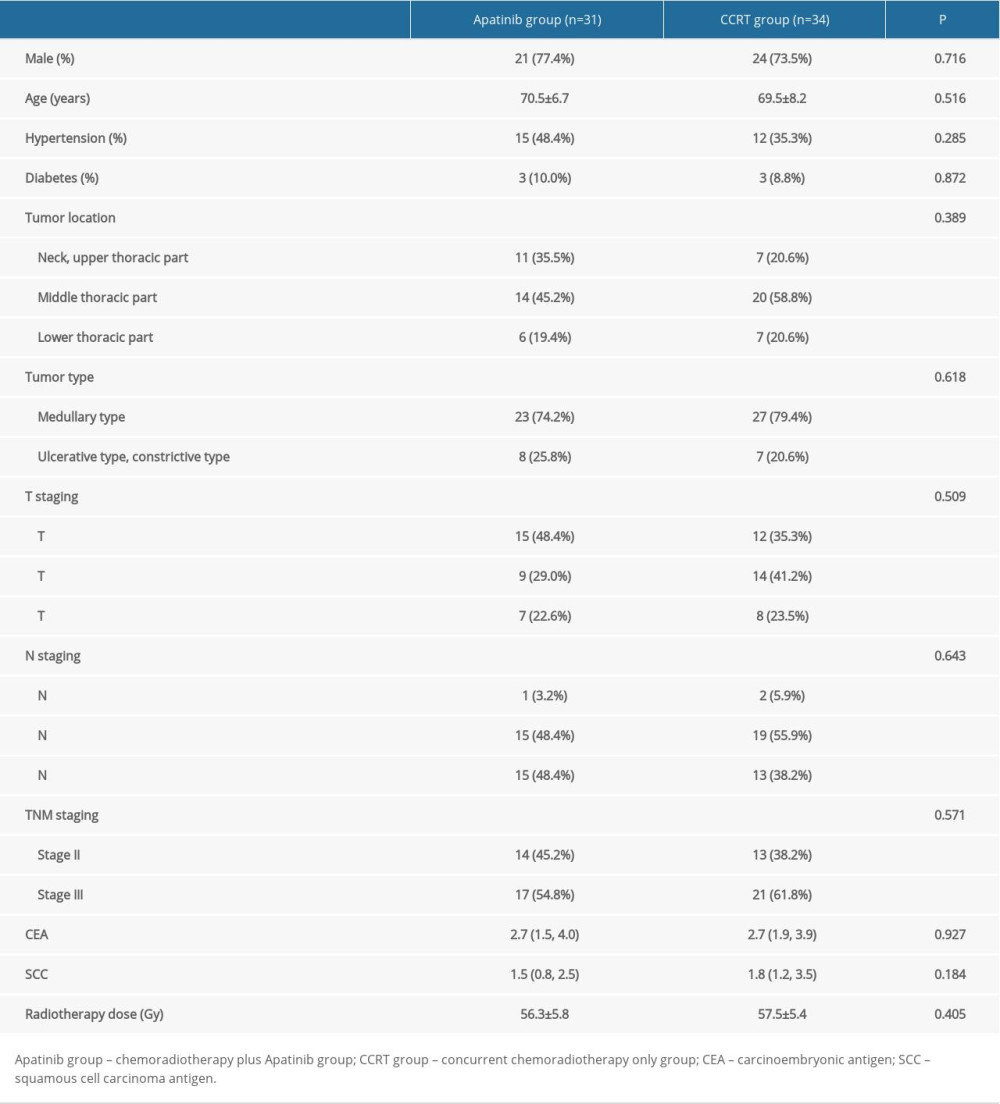 Table 1. Baseline characteristics of study participants.
Table 1. Baseline characteristics of study participants.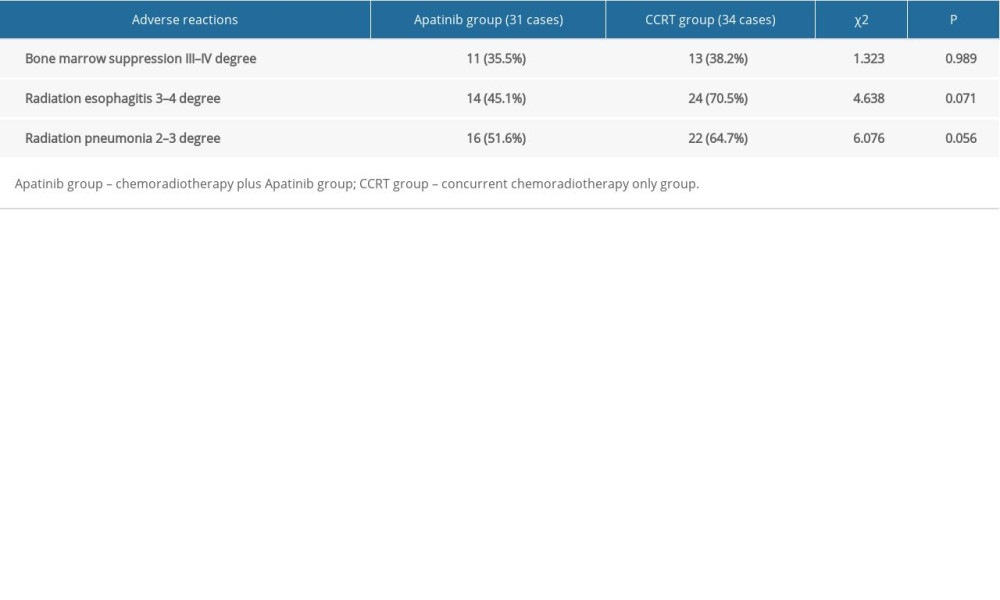 Table 2. Comparing the incidences of radiation esophagitis, radiation pneumonia, and bone marrow suppression between the 2 groups.
Table 2. Comparing the incidences of radiation esophagitis, radiation pneumonia, and bone marrow suppression between the 2 groups.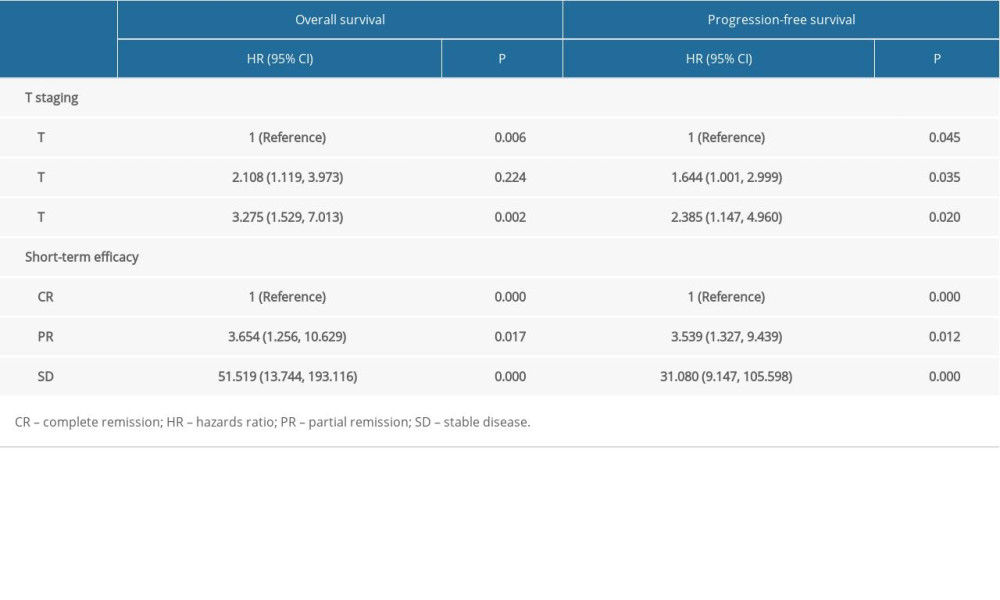 Table 3. Cox multivariate regression analysis of the prognostic factors for nonoperative esophageal squamous cell carcinoma patients.
Table 3. Cox multivariate regression analysis of the prognostic factors for nonoperative esophageal squamous cell carcinoma patients.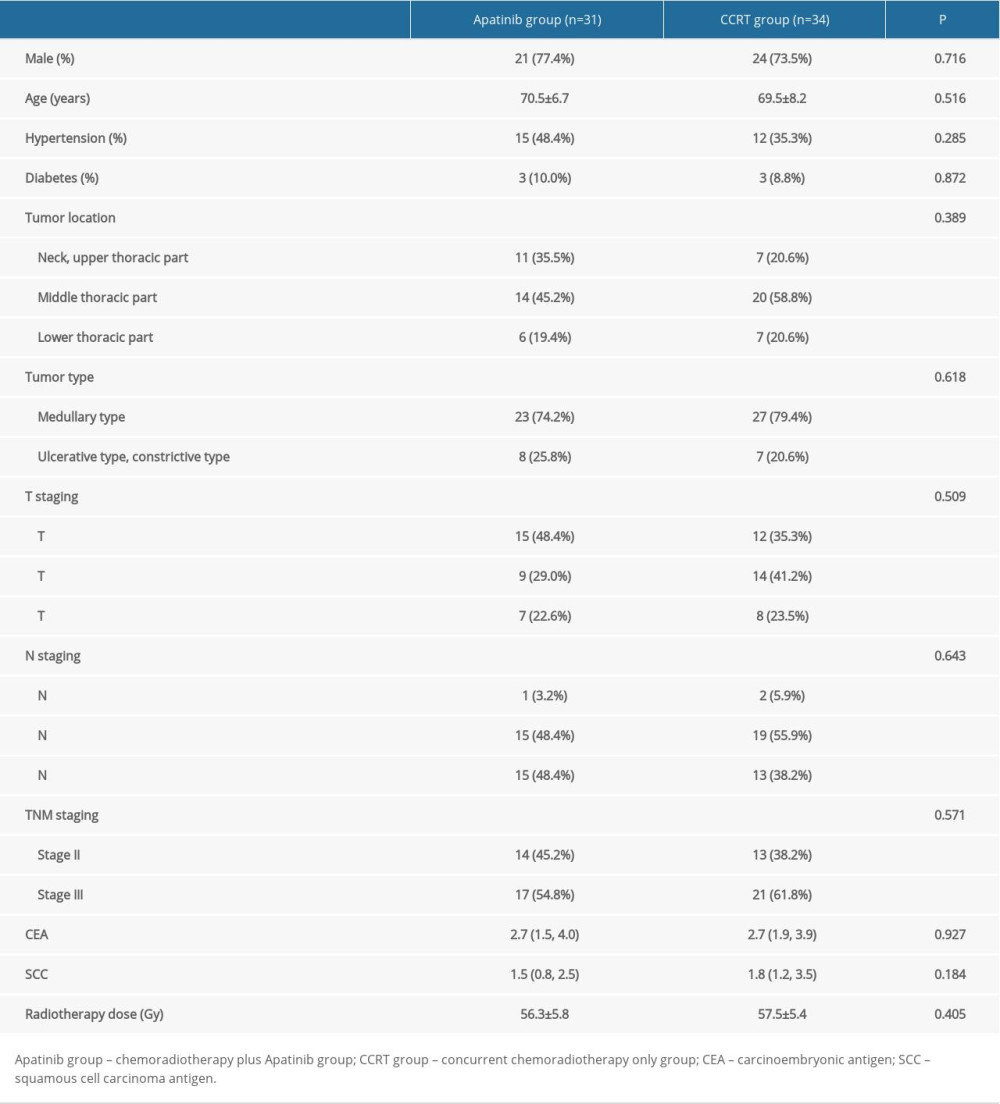 Table 1. Baseline characteristics of study participants.
Table 1. Baseline characteristics of study participants.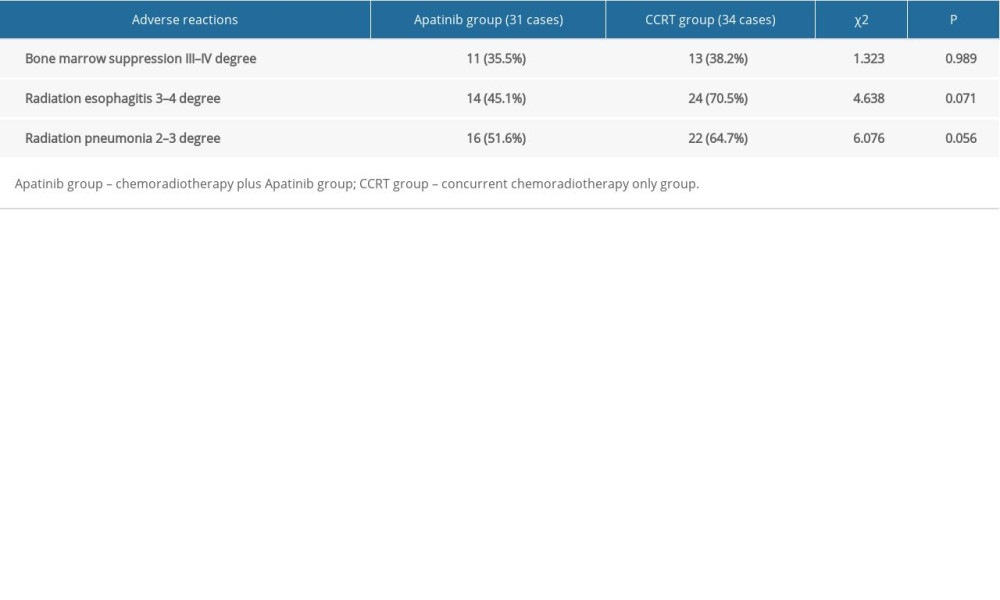 Table 2. Comparing the incidences of radiation esophagitis, radiation pneumonia, and bone marrow suppression between the 2 groups.
Table 2. Comparing the incidences of radiation esophagitis, radiation pneumonia, and bone marrow suppression between the 2 groups.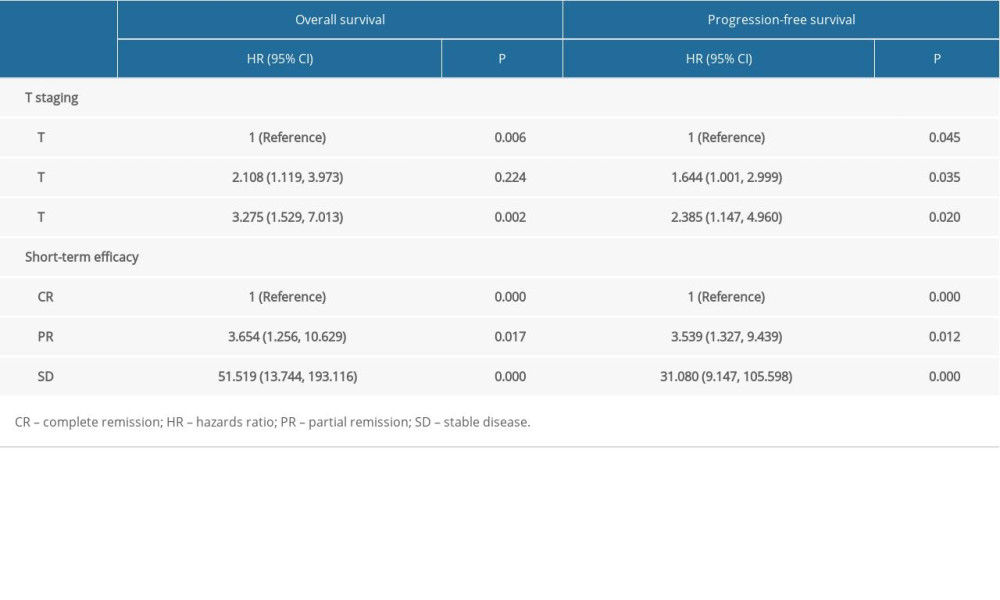 Table 3. Cox multivariate regression analysis of the prognostic factors for nonoperative esophageal squamous cell carcinoma patients.
Table 3. Cox multivariate regression analysis of the prognostic factors for nonoperative esophageal squamous cell carcinoma patients. In Press
05 Mar 2024 : Clinical Research
Role of Critical Shoulder Angle in Degenerative Type Rotator Cuff Tears: A Turkish Cohort StudyMed Sci Monit In Press; DOI: 10.12659/MSM.943703
06 Mar 2024 : Clinical Research
Comparison of Outcomes between Single-Level and Double-Level Corpectomy in Thoracolumbar Reconstruction: A ...Med Sci Monit In Press; DOI: 10.12659/MSM.943797
21 Mar 2024 : Meta-Analysis
Economic Evaluation of COVID-19 Screening Tests and Surveillance Strategies in Low-Income, Middle-Income, a...Med Sci Monit In Press; DOI: 10.12659/MSM.943863
10 Apr 2024 : Clinical Research
Predicting Acute Cardiovascular Complications in COVID-19: Insights from a Specialized Cardiac Referral Dep...Med Sci Monit In Press; DOI: 10.12659/MSM.942612
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








