15 August 2020: Clinical Research
Analysis of Clinical Characteristics, Pathological Changes and Changes of Interleukin-6 (IL-6) and C-Reactive Protein (CRP) in Children with Castleman’s Disease
Chao Hu1AE, Yan Zou1BF*, Jing Pan1BD, Jiliang Yang1DF, Tianyou Yang1AG, Tianbao Tan1CE, Jiahao Li1CGDOI: 10.12659/MSM.924783
Med Sci Monit 2020; 26:e924783
Abstract
BACKGROUND: The aim of this study was to analyze the pathological changes, clinical characteristics and changes in immunity, interleukin-6 (IL-6) and C-reactive protein (CRP) in children with Castleman’s disease (CD).
MATERIAL AND METHODS: A total of 15 CD child patients were enrolled as observation group, while 20 normal children receiving healthy examination were enrolled as healthy control group. The pathological changes, clinical characteristics and changes in immunity and serum IL-6 and CRP expressions were retrospectively analyzed in observation group.
RESULTS: The clinical manifestation of unicentric CD (UCD) was mainly enlargement of cervical lymph nodes without liver-spleen enlargement and fever, and the major pathological type was the hyaline-vascular type. Multicentric CD (MCD) child patients all had anemia, fever and other systemic symptoms, and the major pathological type was the plasma-cell type. There were expressions of the immune indexes, including cluster of differentiation 3 (CD3), CD4, CD8, CD20, and CD79, in a certain degree, while CD138 and VS38C expressions displayed the polyclonal proliferation of plasma cells, rather than neoplastic proliferation. The Epstein-Barr virus and human herpes virus-8 detection results were negative, and CD21 in follicular dendritic cells in abnormal germinal center was positive. The expression levels of serum IL-6 and CRP in observation group were higher than those in control group (P<0.05).
CONCLUSIONS: There are immune dysfunction and increased expressions of serum IL-6 and CRP in child patients with CD, so it can be speculated that the immune abnormality and overexpression of serum inflammatory factors may be associated with the occurrence of CD.
Keywords: Anti-Inflammatory Agents, Giant Lymph Node Hyperplasia, Immunity, Adolescent, C-Reactive Protein, Case-Control Studies, Child, Child, Preschool, Immunophenotyping, Interleukin-6
Bacgrround
Castleman’s disease (CD) is a rare disease of lymph nodes and related tissues, the pathogenesis of which remains to be identified. It is frequently characterized as a severe lymph node proliferative disease and associated with non-specific and chronic inflammatory response with diverse clinical manifestations [1]. The incidence rate of CD in children is extremely low, and some patients have accompanied multiple system damage and systemic symptoms. Clinical pathology shows proliferative lymphoid follicles, plasma cells and blood vessels in different degrees. The clinical characteristic of CD includes obvious enlargement of superficial and deep lymph nodes. CD is divided into unicentric CD (UCD) and multicentric CD (MCD) according to the enlargement of multiple systemic nodes or single lymph node [2,3]. Due to atypical clinical characteristics, unreliable diagnostic indexes, and the lack of heterogeneous imaging manifestations, CD is often found by physical examination, resulting in increased misdiagnosis and missed diagnosis [4]. It is of great significance that we identify the clinical characteristics and pathological changes in CD in children, but there are few reports on children with CD in clinical practice [5]. In this regard, the pathological changes, clinical characteristics, and changes in immunity index, interleukin-6 (IL-6), and C-reactive protein (CRP) in CD children were tested and analyzed in the present study, so as to provide leads for future prevention and treatment of CD.
Data and Methods
GENERAL DATA:
A total of 15 child patients with CD treated in our hospital from January 2008 to December 2018 were enrolled as the observation group, including 9 males and 6 females aged 5 to 14 years old with an average of age of 10.4±1.3) years. Inclusion criteria were as follows: child patients definitely diagnosed with CD via imaging, clinical manifestations, and surgical pathological examination; patients aged <18 years old; patients without severe infectious diseases, blood system diseases, congenital diseases, or malignant tumors, and patients with certain comprehension, cognition, and communication ability. This study met the relevant ethical requirements of Guangzhou Women and Children’s Medical Center, and all child patients and their parents were informed and agreed. Another 20 normal children receiving physical examination (including abdominal ultrasound) in our hospital from January 2018 to December 2018 were randomly selected as the healthy control group, including 12 males and 8 females aged 6 to 14 years with an average age of 10.8±1.0 years. The age and gender had no statistically significant differences between the 2 groups (
Material and Methods
DATA COLLECTION:
The general data of 15 child patients in the observation group were retrospectively analyzed, including the age, gender, clinical characteristics, and results of surgical pathological examination. In all patients, pathological CD diagnosis was based on the histopathological characteristics of biopsy specimens from the involved lymph nodes, skin, tissues, or organs with review by at least 2 experienced pathologists. At the same time, CD was divided into UCD and MCD according to the imaging examination and physical examination during the data collection. The pathological typing was based on the pathological results [6].
DETECTION OF IMMUNE INDEXES:
The specimens obtained by surgical resection were fixed with 4% formaldehyde, dehydrated, transparentized, embedded in paraffin, and sliced into sections in a certain thickness, followed by hematoxylin and eosin staining, sealing, and examination under a light microscope. The immune indexes were detected via immunohistochemical staining, including CD3, CD4, CD8, CD20, CD21, CD79, and CD138, while the VS38C expression, Epstein-Barr virus (EBV), and human herpes virus-8 (HHV-8) were detected according to the instructions.
DETECTION OF IL-6 AND CRP:
After 2 mL fasting elbow venous blood was drawn from patients in observation group on the next morning after admission, and 2 mL elbow venous blood was drawn from children in control group at the day of physical examination, they were centrifuged at 2000 rpm for 10 minutes, and the serum was separated and stored in a refrigerator at −20°C to be detected. The serum IL-6 expression was detected via enzyme-linked immunosorbent assay, and the serum CRP expression was detected via immunoturbidimetric assay in accordance with the instructions.
DIAGNOSTIC CRITERIA:
CD was diagnosed based on the diagnostic criteria for CD in children formulated in the 2nd version of the Diagnostic and Therapeutic Effect Criterion for Hematological Diseases [7]. In brief, 1) UCD: there is enlargement of lymph nodes at a single site. Characteristic hyperplasia is confirmed via histopathological examination, and the possible primary hyperplasia is excluded. 2) MCD: systemic symptoms exist, accompanied by systemic involvement in different system. The obvious enlargement of lymph nodes is displayed in imaging examination, invading peripheral lymph nodes at multiple sites. The known pathogenesis is excluded [8,9].
STATISTICAL ANALYSIS:
SPSS 19.0 (SPSS Inc., Chicago, IL, USA) software was used for data processing. Measurement data were expressed as mean±standard deviation (χ̄±
Results
IMAGING EXAMINATION RESULTS:
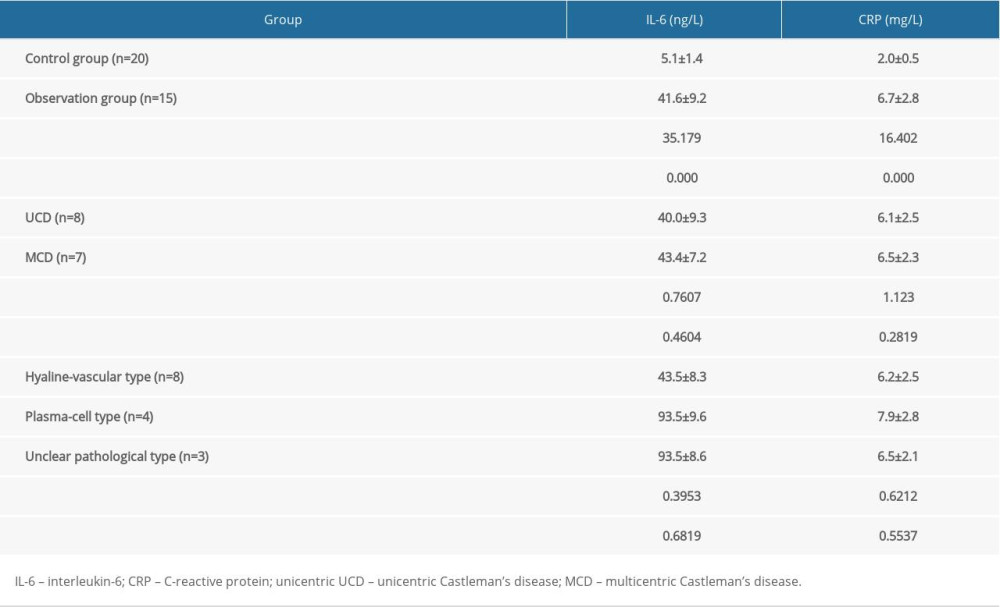
Among 15 CD child patients in observation group, abdominal masses were found in 7 cases and cervical masses were found in 8 cases (Figures 1, 2).
CLINICAL CHARACTERISTICS:
Among the 15 CD child patients, there were 8 cases of UCD and 7 cases of MCD, and the duration from onset to clinical diagnosis was 2 to 10 years. 1) In terms of initial symptoms of CD, there were fever and fatigue in 5 cases, dental ulcer in 2 cases, enlargement of lymph nodes in 8 cases and rash in 3 cases. 2) Enlargement of lymph nodes: with the progression of disease, the obvious enlargement of lymph nodes (4 to 7 cm in diameter) was found in the 15 child patients, including 8 cases of enlargement of superficial lymph nodes, involving the groin, neck, and armpit. The enlargement of deep lymph nodes was found in 5 cases via imaging examination after visit, including that of retroperitoneal and mediastinal lymph nodes. 3) One child patient had UCD complicated with paraneoplastic pemphigus (PNP), manifested as pleomorphic rash, oral and lip mucosa erosion at the onset, the pulmonary interstitial fibrosis occurred later, and the enlargement of retroperitoneal lymph nodes was confirmed via abdominal enhancement computed tomography. 4) Systemic manifestations: fever occurred in 7 MCD patients (37.5–38.5°C), complicated with splenomegaly and moderate-severe anemia. Three patients had growth retardation.
PATHOLOGICAL EXAMINATION RESULTS:
In the observation group, all the 15 child patients were diagnosed with CD via pathological section and immunohistochemical staining, including 8 cases (53.3%) of hyaline-vascular type, 4 cases (26.7%) of plasma-cell type, and 3 cases (20.0%) of unclear pathological type; the mixed-cell type was not detected. Pathological manifestations included: 1) in child patients with the hyaline-vascular type, the basic structure of lymph nodes remained intact, there was significant follicular hyperplasia, and there was hyaline degeneration in the follicular hyperplasia, in which the vacuole follicular dendritic cells were mixed. The peripheral small lymphocytes in germinal center were arranged in an “onion skin” shape, and the vascular proliferation was found among follicles and in the paracortex zone (Figures 3, 4). 2) In child patients in plasma-cell type, diffuse hyperplasia was observed in interfollicular plasma cells, there was no obvious hyaline degeneration in the follicular vessels, and the deposited eosinophilic substances had no type (Figures 5, 6). According to the immunohistochemical detection results, there were expressions of the immune indexes, including CD3, CD4, CD8, CD20, and CD79, in a certain degree, while CD138 and VS38C expressions displayed the polyclonal proliferation of plasma cells, rather than neoplastic proliferation. The EBV detection results were negative, and CD21 in follicular dendritic cells in abnormal germinal center was positive.
IL-6 AND CRP EXPRESSIONS:
The expression levels of serum IL-6 and CRP in observation group were higher than those in control group, and the differences were statistically significant (P<0.05) (Table 1). However, significant differences of IL-6 and CRP were neither found between UCD and MCD, nor among hyaline-vascular type, plasma-cell type, and unclear pathological type (Table 1). Surgical resection was performed for the treatment, along with intravenous infusion of immunoglobulin (IVIG) and glucocorticoid (prednisone, methylprednisolone, or dexamethasone) prior to, during, and after surgical removal. Postoperative observation indicated no recurrence or metastasis over 1-year follow-up among 15 CD child patients in this study.
Discussion
CD, also known as vascular follicular lymphoid hyperplasia, clinically manifests as enlargement of multiple systemic or single lymph node, with a low morbidity rate but great patient harm [10]. CD can occur at any age, often in young people and occasionally in children [11]. Currently, the cause and pathogenesis of CD have not been clarified in clinical medicine, but some studies have suggested that it is associated with the increased expressions of serum inflammatory factors (IL-6 and CRP), immune dysfunction, and human herpesvirus-8 (HHV-8) and human immunodeficiency virus (HIV) infection [12]. Studies have demonstrated that the expressions of some follicular dendritic cells in the serum and germinal center of lymph nodes and IL-6 and CRP in B cells in CD child patients are increased, and IL-6 overexpression can induce manifestations similar to MCD in rats [7]. IL-6 is a cell-derived cytokine that plays an important role in the body’s inflammatory response and cellular immunity, which can play a dual role in protecting and damaging the central nervous system [13,14]. CRP, a sensitive acute-phase protein synthesized by human liver, has important immunoregulation effects, including stimulating the tissue factor expression of monocytes and macrophages, and increasing the motion and activity of macrophages, which can reflect the degree of inflammatory response in the body [15]. The load of HHV-8, a major pathogenic factor of MCD, is related to the condition of MCD, and HHV-8 can encode the virus-derived IL-6 during replication, accelerating the onset of disease [16].
It was found in the present study that the expression levels of serum IL-6 and CRP in CD child patients were significantly higher than those in the healthy control group, and fever occurred in MCD patients and the autoantibodies were positive in some of them, indicating that the inflammatory factors and immune abnormality participate in the occurrence and development of CD. At the same time, pathological analysis revealed that the major pathological type of UCD and MCD was the hyaline-vascular type and plasma-cell type, respectively. In this study, there were 8 cases of progressive enlargement of lymph nodes (4.0–7.0 cm in diameter), including 2 cases in retroperitoneal lymph nodes, 4 cases in cervical lymph nodes, and 2 cases in mediastinal lymph nodes, suggesting that the risk of enlargement of lymph nodes is higher in CD child patients, showing differences from adults with enlargement of abdominal and mediastinal lymph nodes [17]. There is a lack of significant lymphatic symptoms in the initial stage of the disease, but local compression can occur with the constant enlargement of lymph nodes, leading to different symptoms based on the different sites of compression. In the present study, 1 child patient had UCD complicated with PNP, manifested as pleomorphic rash in skin mucosa at the onset, which had complex clinical manifestations and retroperitoneal enlarged lymph nodes, thus making clinical diagnosis more difficult. As an autoimmune skin disease, PNP can induce benign and malignant tumors, with a certain risk of CD [18]. The results of this study also showed that 7 child patients had enlargement of multiple lymph nodes, accompanied by liver-spleen enlargement, fever, emaciation, night sweat and fatigue, and the laboratory examination confirmed anemia, increased expression of gamma globulin and other relevant changes. At the same time, growth retardation was found in 3 patients, and the possible reason was that the overexpression of inflammatory factors in the body makes the child patients remain in a consuming and fever state for a long time, thus affecting normal development.
Studies have demonstrated that the clinical manifestations of CD are complex, so it is hard to find and determine the disease in the early stage and develop therapeutic measures, and there is a higher risks of misdiagnosis and missed diagnosis, if clinicians have insufficient understanding of CD. In particular, the enlargement of lymph nodes occurs at multiple sites in MCD child patients, accompanied by multiple systemic dysfunctions, and the laboratory detection results are abnormal, combined with the diverse clinical manifestations and lack of specificity, so the pathological diagnosis is often needed to improve the diagnostic reliability, namely diagnosis via immunohistochemical staining and observation of typical pathological morphology [19]. The chronic lymphadenitis and lymphoid hyperplasia associated with the disease are mostly detected in lymph node biopsies, so there are some deficiencies in confirming CD via needle biopsy. Based on the diagnostic criteria for CD, with the exception of the characteristic clinicopathological changes of patients, other related primary changes are often excluded in clinical diagnosis, thus, connective tissue disease, tumor disease, and infectious disease should be excluded in clinical diagnosis of CD, so as to improve the accuracy, sensitivity and specificity of clinical diagnosis [20]. The limitations in this study were that the potential value of IL-6 and CRP as diagnostic markers of CD children requires further validation within a large sample size, and by using comparison of histological and immunohistochemical analysis, including staining for CD3, CD5, CD10, CD20, CD23, CD79, and Ki-67 as previously reported [21]. The evaluation also needs to include the incorporation of the comprehensive treatment and follow-up details.
Conclusions
In conclusion, CD in children has a low morbidity rate, and its clinical characteristics are similar to those in adults, such as enlargement of lymph nodes, fever, and anemia. we found in pathological examination that the major pathological type of UCD and MCD was the hyaline-vascular type and plasma-cell type, respectively. At the same time, there are immune dysfunction and increased expressions of serum IL-6 and CRP in child patients, so it is speculated that the immune abnormality and overexpression of serum inflammatory factors may be associated with the occurrence of CD. Anti-CD20 monoclonal antibodies and protease inhibitors of IL-6 autocrine can be applied in the treatment of CD.
Figures
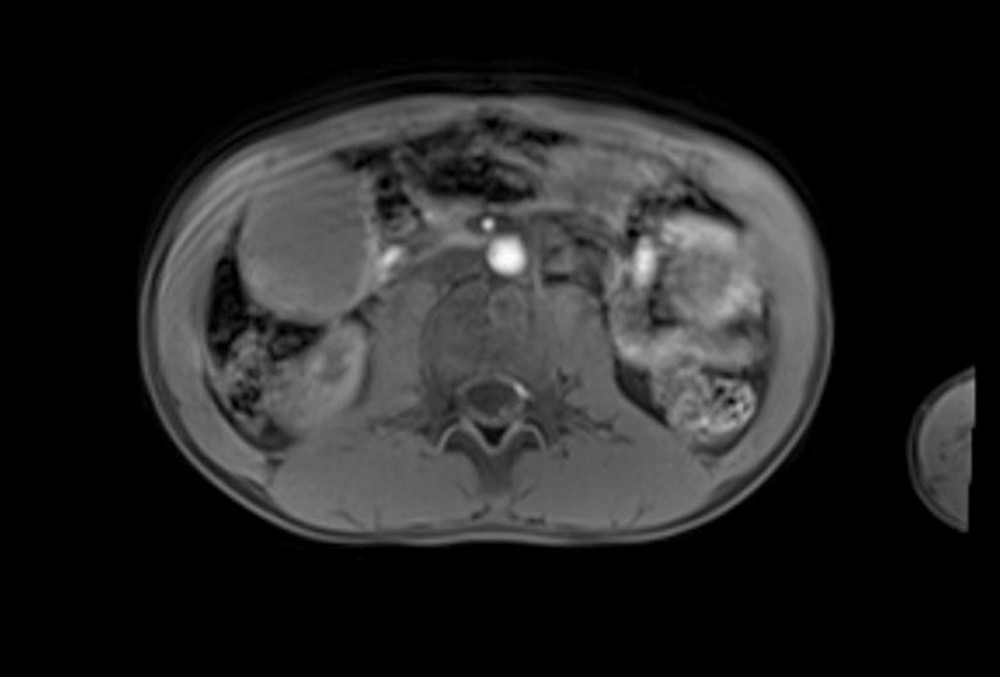 Figure 1. An 11-year-old child patient with mesenteric lesions, abdominal mass is shown in a magnetic resonance image.
Figure 1. An 11-year-old child patient with mesenteric lesions, abdominal mass is shown in a magnetic resonance image. 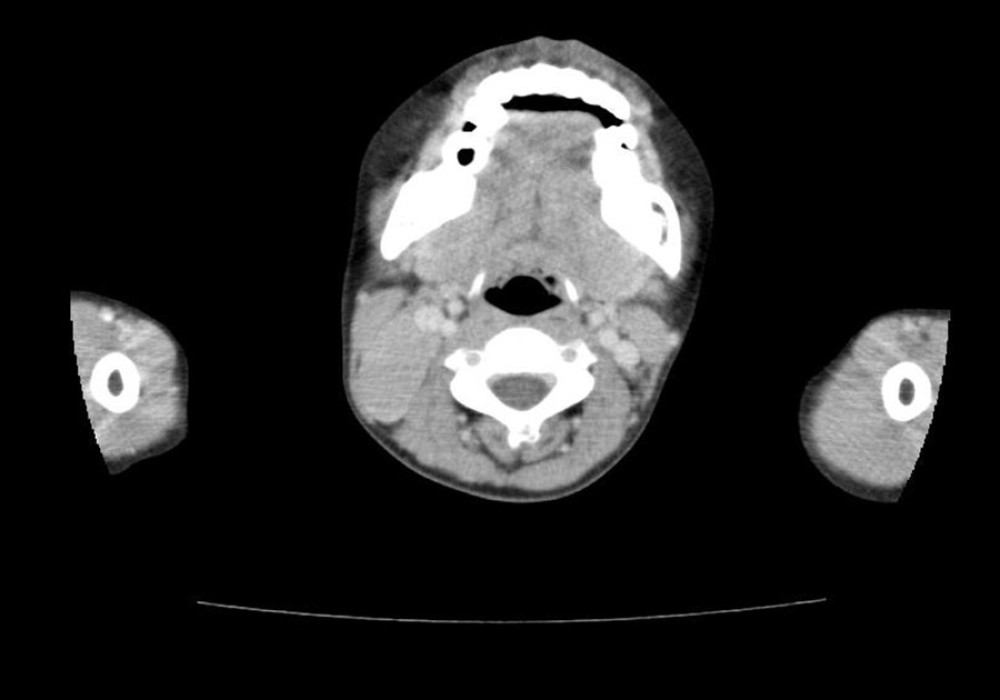 Figure 2. A 10-year-old child patient, the right cervical mass is shown in a computed tomography examination.
Figure 2. A 10-year-old child patient, the right cervical mass is shown in a computed tomography examination. 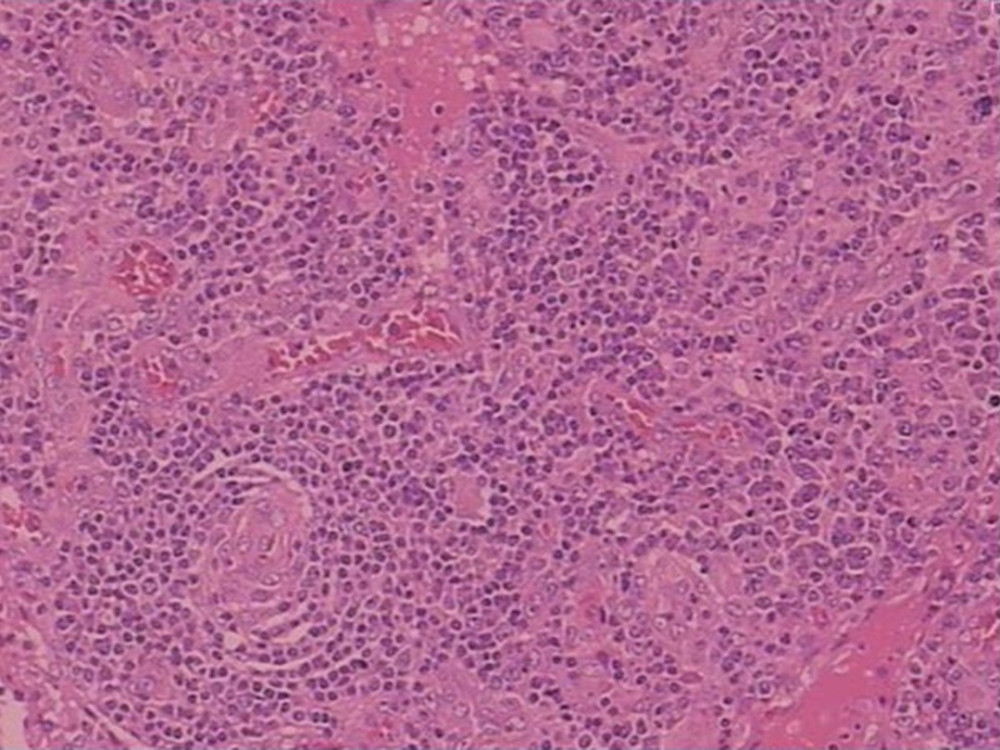 Figure 3. Hematoxylin and eosin staining. Lymph nodes are unclear, the lymphoid sinus is expanded, sinus histiocytosis is obvious, and there is proliferation of small vessels in some areas.
Figure 3. Hematoxylin and eosin staining. Lymph nodes are unclear, the lymphoid sinus is expanded, sinus histiocytosis is obvious, and there is proliferation of small vessels in some areas.  Figure 4. Immunohistochemistry. The brown color indicated positive immunostaining of CD138.
Figure 4. Immunohistochemistry. The brown color indicated positive immunostaining of CD138. 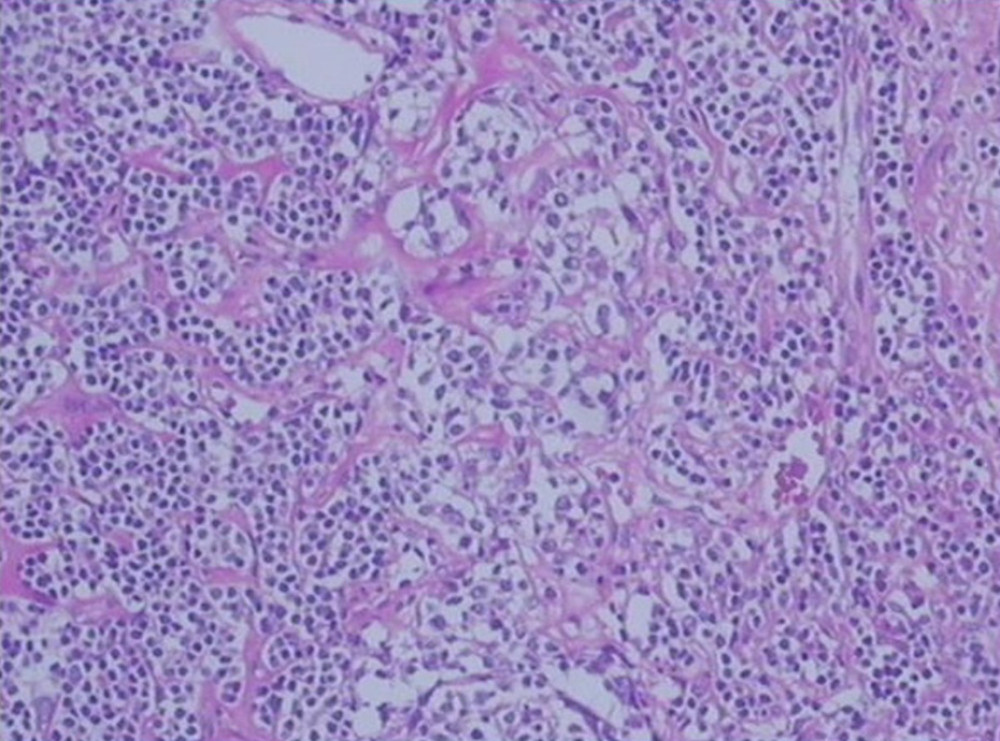 Figure 5. Hematoxylin and eosin staining. Deposit of red-stained substance can be seen in germinal center of some lymphoid follicles. There are significantly more interfollicular small vessels often accompanied by hyaline degeneration. There is a large amount of scattered infiltration of plasma cells around the proliferative follicles.
Figure 5. Hematoxylin and eosin staining. Deposit of red-stained substance can be seen in germinal center of some lymphoid follicles. There are significantly more interfollicular small vessels often accompanied by hyaline degeneration. There is a large amount of scattered infiltration of plasma cells around the proliferative follicles. 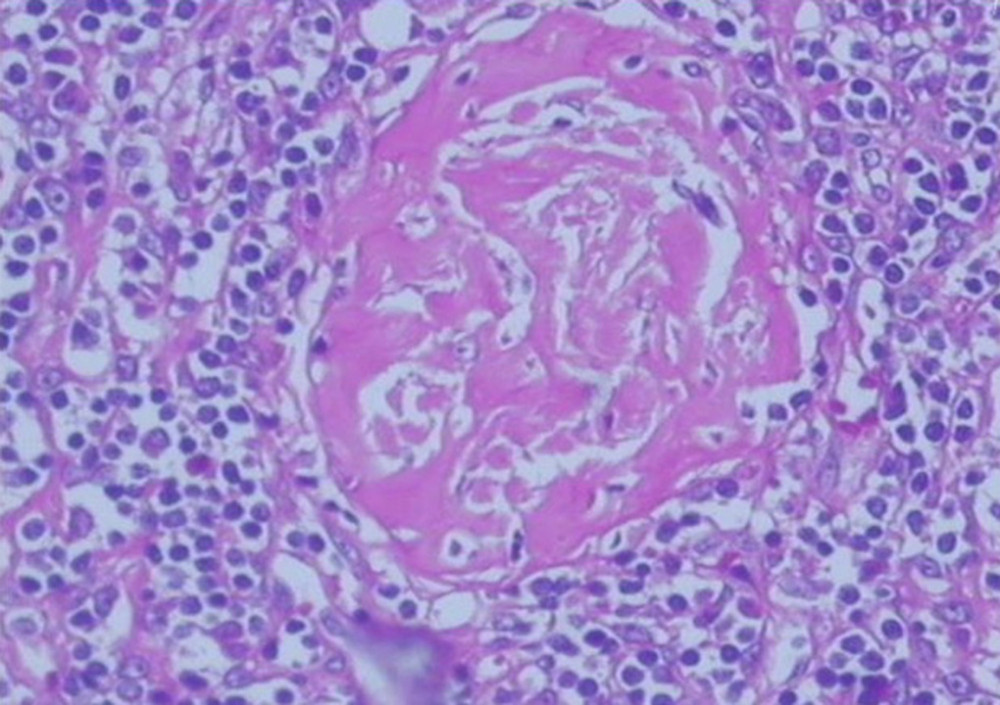 Figure 6. Hematoxylin and eosin staining. Enlarged lymph node.
Figure 6. Hematoxylin and eosin staining. Enlarged lymph node. References
1. Liu YC, Stone K, van Rhee F, Siltuximab for multicentric Castleman disease: Expert Rev Hematol, 2014; 7; 545-57
2. Hamilton J, Mandel L, Rare submandibular presentation of pediatric Castleman disease: Case report: J Oral Maxillofac Surg, 2017; 75; 763-66
3. Chamorro-Oscullo J, Robles-Ramirez F, Valenzuela-Tamariz JUnicentric Castleman’s disease in cervical back space neck: Rev Med Inst Mex Seguro Soc, 2017; 55; 660-65 [in Spanish]
4. Calabro N, Henriksen K, Lim SH, Successful use of rituximab in glomerular basement membrane nephritis associated with HIV interstitial nephritis secondary to Castleman disease: Clin Nephrol, 2018; 89; 469-73
5. Li J, Wang J, Yang Z, Castleman disease versus lymphoma in neck lymph nodes: A comparative study using contrast-enhanced CT: Cancer Imaging, 2018; 18; 28
6. Shams AA, Ahmed MM, Scalzitti NJ, A Multidisciplinary approach to Castleman disease of the neck: South Med J, 2016; 109; 78-82
7. Khan MK, Talukder RH, Kamruzzaman M, The Castleman’s disease and related disorders – a case report: Mymensingh Med J, 2016; 25; 168-75
8. Kligerman SJ, Auerbach A, Franks TJ, Castleman disease of the thorax: Clinical, radiologic, and pathologic correlation: From the radiologic pathology archives: Radiographics, 2016; 36; 1309-32
9. Fajgenbaum DC, Kurzrock R, Siltuximab: A targeted therapy for idiopathic multicentric Castleman disease: Immunotherapy, 2016; 8; 17-26
10. Hawkins JM, Pillai V, TAFRO syndrome or Castleman-Kojima syndrome: A variant of multicentric Castleman disease: Blood, 2015; 126; 2163
11. Fajgenbaum DC, Uldrick TS, Bagg A, International, evidence-based consensus diagnostic criteria for HHV-8-negative/idiopathic multicentric Castleman disease: Blood, 2017; 129; 1646-57
12. Iwaki N, Fajgenbaum DC, Nabel CS, Clinicopathologic analysis of TAFRO syndrome demonstrates a distinct subtype of HHV-8-negative multicentric Castleman disease: Am J Hematol, 2016; 91; 220-26
13. Arcadu A, Moua T, Yi ES, Lymphoid interstitial pneumonia and other benign lymphoid disorders: Semin Respir Crit Care Med, 2016; 37; 406-20
14. Shivane A, Pearce A, Khatib N, EBV+ HHV-8+ multicentric Castleman disease with plasmablastic aggregates in an HIV+ man: An evolving clinicopathologic entity: Int J Surg Pathol, 2018; 26; 338-41
15. Li P, Yang Z, Wang Z, Clinical features of clear cell meningioma: A retrospective study of 36 cases among 10,529 patients in a single institution: Acta Neurochir (Wien), 2016; 158; 67-76
16. Bracale U, Pacelli F, Milone M, Laparoscopic treatment of abdominal unicentric Castleman’s disease: A case report and literature review: BMC Surg, 2017; 17; 38
17. Oshima Y, Hoshino J, Suwabe T, Multicentric Castleman’s disease associated with IgA vasculitis (Henoch-Schonlein purpura) responding well to tocilizumab: A case report: Clin Rheumatol, 2017; 36; 729-33
18. Fajgenbaum DC, Ruth JR, Kelleher D, The collaborative network approach: a new framework to accelerate Castleman’s disease and other rare disease research: Lancet Haematol, 2016; 3; e150-52
19. Wang HW, Pittaluga S, Jaffe ES, Multicentric Castleman disease: Where are we now?: Semin Diagn Pathol, 2016; 33; 294-306
20. Izumi Y, Takeshita H, Moriwaki Y, Multicentric Castleman disease mimicking IgG4-related disease: A case report: Mod Rheumatol, 2017; 27; 174-77
21. Aguilar-Rodriguez R, Milea SL, Demirci I, Localized retroperitoneal Castleman’s disease: A case report and review of the literature: J Med Case Rep, 2014; 8; 93
Figures
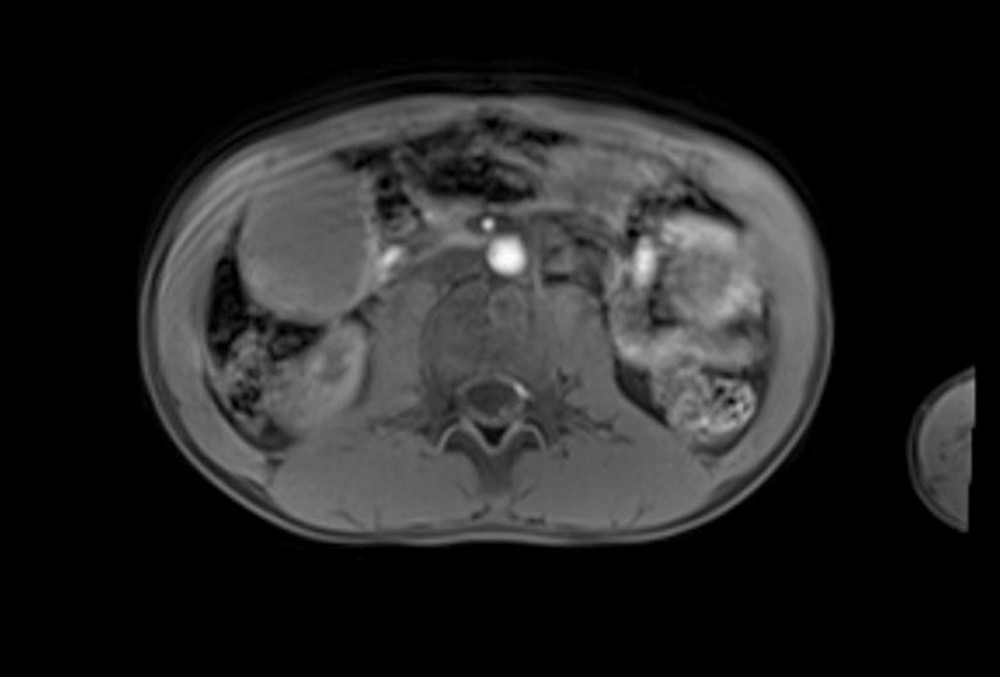 Figure 1. An 11-year-old child patient with mesenteric lesions, abdominal mass is shown in a magnetic resonance image.
Figure 1. An 11-year-old child patient with mesenteric lesions, abdominal mass is shown in a magnetic resonance image.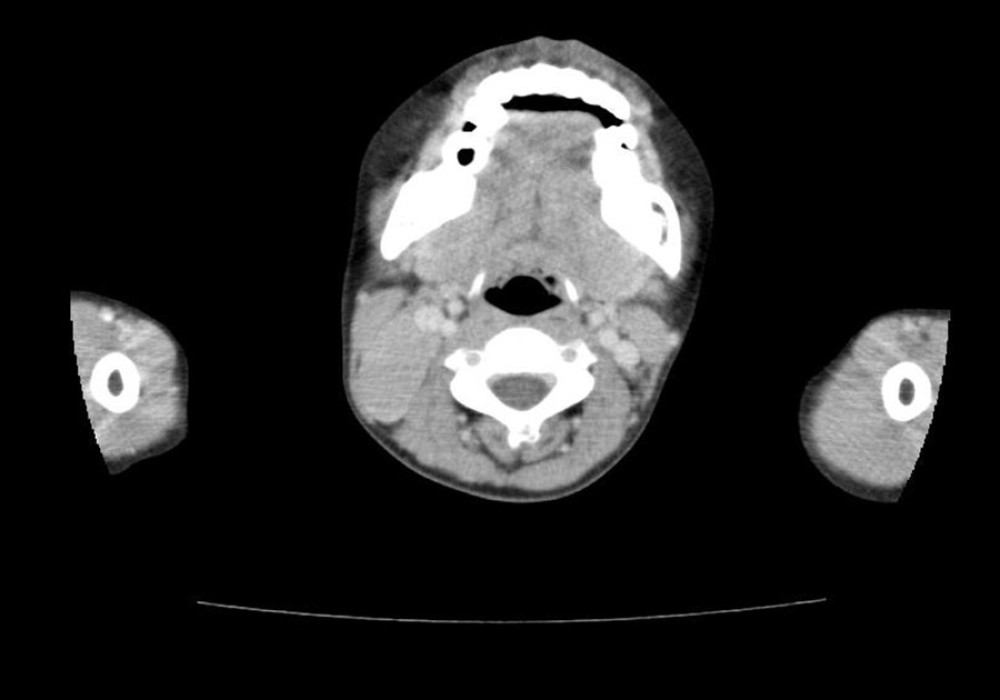 Figure 2. A 10-year-old child patient, the right cervical mass is shown in a computed tomography examination.
Figure 2. A 10-year-old child patient, the right cervical mass is shown in a computed tomography examination.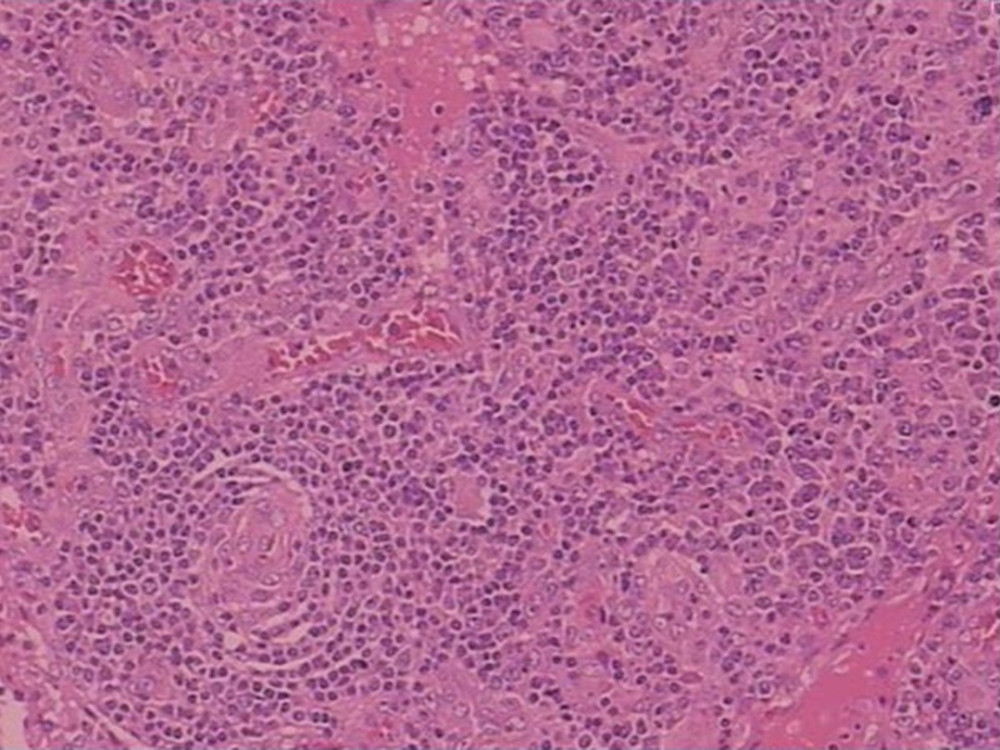 Figure 3. Hematoxylin and eosin staining. Lymph nodes are unclear, the lymphoid sinus is expanded, sinus histiocytosis is obvious, and there is proliferation of small vessels in some areas.
Figure 3. Hematoxylin and eosin staining. Lymph nodes are unclear, the lymphoid sinus is expanded, sinus histiocytosis is obvious, and there is proliferation of small vessels in some areas. Figure 4. Immunohistochemistry. The brown color indicated positive immunostaining of CD138.
Figure 4. Immunohistochemistry. The brown color indicated positive immunostaining of CD138.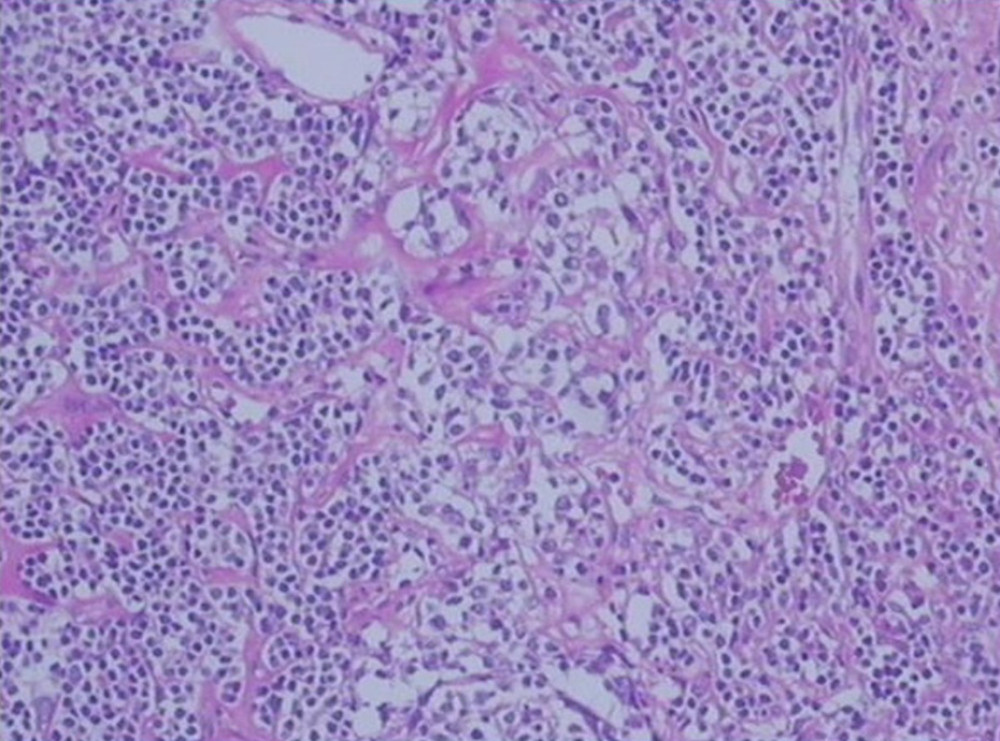 Figure 5. Hematoxylin and eosin staining. Deposit of red-stained substance can be seen in germinal center of some lymphoid follicles. There are significantly more interfollicular small vessels often accompanied by hyaline degeneration. There is a large amount of scattered infiltration of plasma cells around the proliferative follicles.
Figure 5. Hematoxylin and eosin staining. Deposit of red-stained substance can be seen in germinal center of some lymphoid follicles. There are significantly more interfollicular small vessels often accompanied by hyaline degeneration. There is a large amount of scattered infiltration of plasma cells around the proliferative follicles.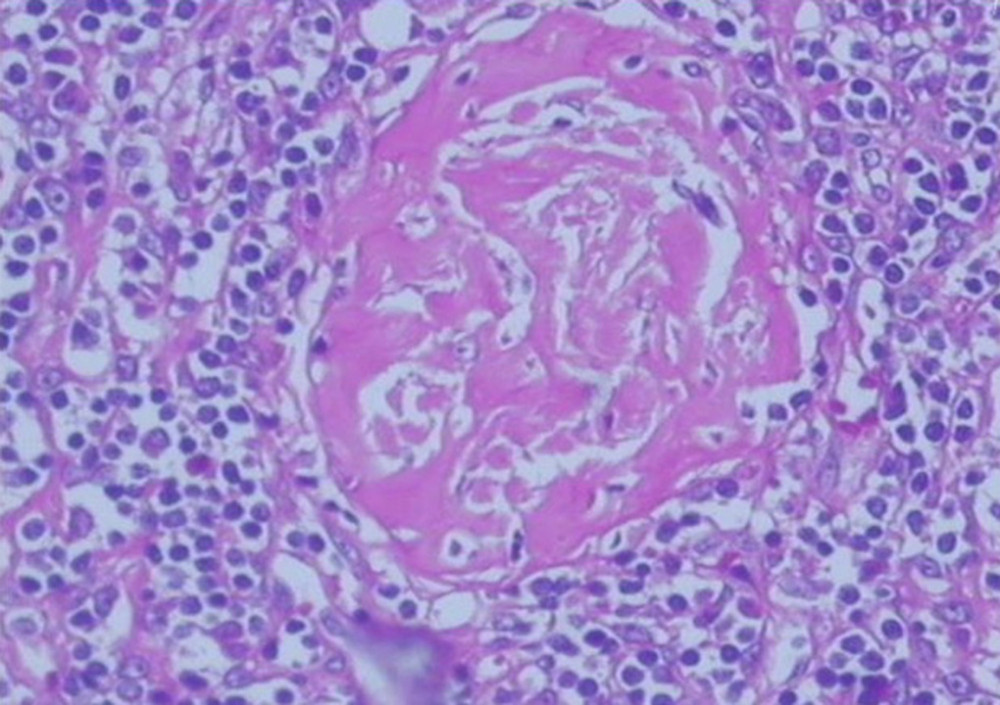 Figure 6. Hematoxylin and eosin staining. Enlarged lymph node.
Figure 6. Hematoxylin and eosin staining. Enlarged lymph node. In Press
08 Mar 2024 : Clinical Research
Evaluation of Foot Structure in Preschool Children Based on Body MassMed Sci Monit In Press; DOI: 10.12659/MSM.943765
15 Apr 2024 : Laboratory Research
The Role of Copper-Induced M2 Macrophage Polarization in Protecting Cartilage Matrix in OsteoarthritisMed Sci Monit In Press; DOI: 10.12659/MSM.943738
07 Mar 2024 : Clinical Research
Knowledge of and Attitudes Toward Clinical Trials: A Questionnaire-Based Study of 179 Male Third- and Fourt...Med Sci Monit In Press; DOI: 10.12659/MSM.943468
08 Mar 2024 : Animal Research
Modification of Experimental Model of Necrotizing Enterocolitis (NEC) in Rat Pups by Single Exposure to Hyp...Med Sci Monit In Press; DOI: 10.12659/MSM.943443
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952