13 August 2020: Clinical Research
High versus Low Mechanical Index Imaging Diagnostic Ultrasound in Patients with Myocardial Infarction: A Therapeutic Application Study
Zongbao Niu1ABF, Xiaolan Lv1CDF, Jianhua Zhang2ABCF, Tianping Bao3DEF*DOI: 10.12659/MSM.923583
Med Sci Monit 2020; 26:e923583
Abstract
BACKGROUND: High mechanical index impulse of ultrasound is used for diagnosis of microvascular coronary obstruction and the necrotic area, but an experimental model study suggested that it can restore microvascular and epicardial coronary flow. The purposes of the study were to test the safety and therapeutic efficacy of high acoustic energy diagnostic ultrasound in patients with ST-segment elevation myocardial infarction.
MATERIAL AND METHODS: Patients with ST-segment elevation myocardial infarction subjected to a low (n=199) or high (n=251) mechanical index ultrasound before and after percutaneous coronary interventions and echocardiographic parameters were evaluated. Coronary angiographies were performed for the assessment of culprit vessels. Thrombolysis in myocardial infarction flow grade 1 or 2 were considered as culprit vessels.
RESULTS: Patients diagnosed through low acoustic energy ultrasound reported 235 infarct vessels and patients diagnosed through high acoustic energy ultrasound reported 300 infarct vessels. With respect to low acoustic energy, high acoustic energy reduced the number of culprit vessels at post-percutaneous coronary interventions at 48 hours before hospital discharge (P=0.015) and post-percutaneous coronary interventions at 1-month from the baseline interventions (P=0.043). Also, the maximum% ST-segment resolution and an ejection fraction of the left ventricle was increased and microvascular coronary obstruction in infarct vessels was decreased for both evaluation points. High acoustic energy could not affect heart rate (P=0.133) and oxygen saturation (P=0.079).
CONCLUSIONS: High acoustic energy ultrasound is a safe method for diagnosis of ST-segment elevation myocardial infarction and may have therapeutic applications.
Keywords: High-Intensity Focused Ultrasound Ablation, percutaneous coronary intervention, Stroke Volume, Ultrasonography, Coronary Angiography, Echocardiography, Electrocardiography, ST elevation myocardial infarction
Background
Acute myocardial infarction remains a primary health concern all over the world [1] and is the main cause of morbidity and death in China [2]. Current treatment for myocardial infarction is thrombolysis [3] and percutaneous coronary intervention [2]. These treatments lead to microvascular coronary obstruction and a higher necrotic area [4]. Intravascular ultrasound is mainly used to show different aspects of coronary disease [5] because it has high tissue penetration and evaluates plaque vulnerability [6].
Transthoracic high mechanical index impulse of ultrasound is used for diagnosis of microvascular coronary obstruction and the necrotic area [3] but an experimental model study suggests that high mechanical index impulse of ultrasound can restore microvascular and epicardial coronary flow [7]. Also, a study reported that ultrasound waves might dissolve intravascular thrombi [8]. The combination of intravenous tissue plasminogen activator with ultrasound might achieve effective thrombolysis [9]. In short, contrast-enhanced ultrasonography is used for diagnosis of microvascular obstruction, wall motion abnormalities, or ejection fraction [10] and has therapeutic action [11].
The primary objective of the study was to investigate the safety and therapeutic efficacy of the high mechanical index impulse diagnostic ultrasound on microvascular coronary flow and left ventricular systolic functions in patients with ST-segment elevation myocardial infarction. The secondary objective of the study was to access the effect of the high mechanical index impulse diagnostic ultrasound at 30-days post percutaneous coronary interventions.
Material and Methods
ETHICS APPROVAL AND CONSENT TO PARTICIPATE:
The designed protocol (FHB/CL/23/19 dated 21 September 2019) of the established study was approved by the First Central Hospital of Baoding review board and Medical Council of China. The study reporting adheres to the law of China, strengthening the reporting of observational studies in epidemiology (STROBE) statement, and the Declaration of Helsinki (v2008).
PATIENT POPULATION:
Data of patients admitted at the Emergency Department with chest pain who required admission diagnosis and follow-up from January 15, 2019 to September 3, 2019 (n=505) of the Affiliated Hospital of Hebei University, Baoding, Hebei, China, the Handan Shengji Tumor Hospital, Handan, Hebei, China, and the First Central Hospital of Baoding, Baoding, Hebei, China were included for review after written permission from competing authorities. Among them, 5 patients had been put on fibrinolytic therapy, 3 patients had a history of myocardial infarction, 6 patients had been receiving percutaneous coronary interventions, and 41 patients had acute non-ST-segment elevation (transient ST elevation, ST depression, or new T wave inversions) myocardial infarction. Therefore, these patients were excluded from the study. A total of 450 patients with first time ever chest pain with ST-segment elevation myocardial infarction (2 mm of ST elevation in V2 and V3 in male patients (Figure 1A) and 1.5 mm of ST elevation in V2 and V3 in female patients (Figure 1B), age ≥40 years old) and required admission diagnosis were included in the study (Figure 2).
STRATIFICATION:
The patients were subjected to diagnostic ultrasound either a low mechanical index (n=199): only 1.8 MHz diagnostic ultrasound consisting 0.18 low mechanical index imaging at 25 Hz frame rate with not more than 3 high mechanical index for diagnosis of heart wall motion and microvascular coronary circulation before and after percutaneous coronary interventions or high mechanical index (n=251): received 1.8 MHz, 1.1–1.3 mechanical index at 3 μS pulse duration in 2, 3, and 4 apex chamber for diagnosis of heart wall motion and microvascular coronary circulation before and after percutaneous coronary interventions by XG3 (Philips Healthcare System, Andover, MA, USA) based on the decision of physician(s). The intervals between the high mechanical index varied from 10–20 seconds. Transmit line spacings were 2°. We used 132 lines/frame for low mechanical index and 120 lines/frame for the high mechanical index; 0.5 mL Optison™ (perflutren protein-type A microspheres, GE Healthcare Inc., Princeton, NJ, USA) was used as a contrasting age (injected into a peripheral vein). All patients were subjected to study mitral valve movement (as a routine diagnostic practice) [3]. All diagnosis was performed by ultrasound technologists (a minimum of 3-years of experiences) of institutes.
CORONARY ANGIOGRAPHY:
Pre-percutaneous coronary interventions and post-percutaneous coronary interventions (at 48 hours before discharge from the hospital and at 1-month from baseline interventions) coronary angiographies were performed by interventional cardiologists (a minimum of 3-years of experiences) of institutes. Angiograms were analyzed according to thrombolysis in myocardial infarction (TIMI) flow grading [12] by interventional cardiologists (a minimum of 3-years of experiences) of institutes. TIMI flow grade 1 or 2 was considered as culprit vessels (Figure 3). The coronary angiography was performed immediately after echocardiography.
ECHOCARDIOGRAPHIC EVALUATIONS:
All echocardiographic data were evaluated at pre-percutaneous coronary interventions and post-percutaneous coronary interventions (at 48 hours before discharge from the hospital and at 1-month from baseline interventions) by ultrasound technologists (a minimum of 3-years of experiences) of institutes.
MAXIMUM ST-SEGMENT RESOLUTION:
It was calculated as per Eq. 1 [13]:
WALL MOTION SCORE INDEX:
It was assessed from wall thickening of contrast-enhanced apical windows through a 17-segment model [14].
EJECTION FRACTION:
Contrast-enhanced images were used for the evaluation of left ventricular ejection fraction as per Eq. 2 [14]:
MICROVASCULAR CORONARY OBSTRUCTION:
The microvascular coronary perfusion score index was used for the assessment of microvascular coronary obstruction. Score 1: the replenishment of myocardial contrast within 4 s of the applied high mechanical index impulse. Score 2: complete myocardial contrast replenishment of the assessed area but delayed (more than 4 seconds of the applied high mechanical index impulse). Score 3: virtually myocardial contrast non-replenishment (not after 10 seconds of the applied high mechanical index impulse) (Figures 4, 5). The score of 3 was considered as microvascular coronary obstruction. The scoring index was calculated as per Eq. 3. Attenuated basal segments (due to shadowing) were excluded from evaluation [3].
STATISTICAL ANALYSES:
InStat 3.01, GraphPad, San Diego, CA, USA was used to perform statistical analyses. the Mann-Whitney U test (between groups) and paired t-test (within a group) [3] were performed for numerical data and the Fischer’s exact test (between groups) or the chi-square (within a group) test were performed for ordinal data. The results were considered significant at a 95% confidence level.
Results
PRE-PERCUTANEOUS CORONARY INTERVENTIONS CHARACTERISTICS:
Majorities of patients were between the ages range of 45–55 years and 85% of patients were male. All patients reported high blood pressure of stage I. All patients received Aspirin (Ecosprin 325 mg, US Vitamins Limited, Mumbai, India) and clopidogrel (Plavix 600 mg, Sanofi-Aventi, Paris, France) in the Emergency Department. There was no significant difference for characteristics between the 2 cohorts at pre-percutaneous coronary interventions (P>0.05 for all). The other demographical and clinical parameters at the pre-percutaneous coronary intervention stage are reported in Table 1.
CORONARY ANGIOGRAPHY:
Patients diagnosed with low acoustic energy reported 235 infarct vessels and patients diagnosed with high acoustic energy reported 300 infarct vessels. There was no statistical difference for the location of the infarct vessel between both groups (P=0.594, Table 2).
With respect to low acoustic energy, high acoustic energy reduced the number of obstructed culprit vessels at post-percutaneous coronary interventions at 48 hours before hospital discharge (101(43) versus 98(33), P=0.015) and post-percutaneous coronary interventions at 1-month from baseline interventions (41(17) versus 33(11), P=0.043, Figure 6).
ECHOCARDIOGRAPHIC EVALUATIONS:
Low acoustic energy was successful to increase% ST-segment resolution (P<0.0001) and ejection fraction of left ventricle (P<0.0001) only at 1-month after percutaneous coronary interventions. While, high acoustic energy was successful to increase% ST-segment resolution (P<0.0001) and ejection fraction of left ventricle (P<0.0001). Also, it was decreased wall motion score index (P=0.035) and numbers of microvascular obstruction in infarct vessels (P<0.0001) at 1-month after percutaneous coronary interventions. With respect to low acoustic energy diagnostic ultrasound, maximum% ST-segment resolution was increased by high acoustic energy diagnostic ultrasound post-percutaneous coronary interventions at 48 hours before hospital discharge (P<0.0001) and post-percutaneous coronary interventions at 1-month from baseline interventions (P<0.0001). Wall motion score index was decreased by high acoustic energy diagnostic ultrasound post-percutaneous coronary interventions at 48 hours before hospital discharge (P<0.0001) and post-percutaneous coronary interventions at 1-month from baseline interventions (P<0.0001). However, ejection fraction of left ventricle was increased by high acoustic energy diagnostic ultrasound post-percutaneous coronary interventions at 48 hours before hospital discharge (P=0.003) and post-percutaneous coronary interventions at 1-month from baseline interventions (P<0.0001) and microvascular coronary obstruction in infarct vessels was decreased by high acoustic energy diagnostic ultrasound post-percutaneous coronary interventions at 48 hours before hospital discharge (P=0.045) and post-percutaneous coronary interventions at 1-month from baseline interventions (P=0.049). The detailed values of echocardiographic evaluations are presented in Table 3.
SAFETY STUDY:
High acoustic energy could not affect heart rate (P=0.133) and oxygen saturation (P=0.079). The detailed parameters of heart rate and oxygen saturation are reported in Table 4.
Discussion
The study reported therapeutic effects of contrast-enhanced ultrasound with high acoustic energy e.g., improved coronary flow after percutaneous coronary interventions especially at 1-month from baseline interventions in patients with ST-segment elevation myocardial infarction. Low acoustic energy ultrasound with shorter pulse duration is generally used to diagnose myocardial perfusion and wall motion criteria [15]. The results of the study were consistent with the results of a single-blind randomized trial [3], randomized clinical studies [8,16], experimental model studies [7,17], and CLOTBUST trial [9]. Diagnostic ultrasound with longer pulse duration before and after percutaneous coronary interventions prevents microvascular coronary obstructions and its complications [3] because high acoustic energy ultrasound cause microbubbles to cavitate during the period of insonation [7] which creates shear stress and dissolves thrombus [17]. Moreover, animal model studies provided evidence for microvascular sonothrombolysis by ultrasound-mediated microbubble [7,18,19]. High acoustic energy ultrasound with longer pulse duration can be used to improve the microvascular and epicardial coronary flow. Sonothrombolysis is an emerging technique to improve treatment of myocardial infarction. The authors performed a retrospective study in a remarkable number of patients with ST elevation myocardial infarction. In these patients’ ultrasound enhancing agents were administered and two different imaging techniques were applied. To our knowledge there has been only 1 randomized clinical trial with less patients related to contrast-ultrasound treatment of patients with ST elevation myocardial infarction [3,16]. The results in the current study could become important to further promote sonothrombolysis in patients with myocardial infarction.
High acoustic energy decreased wall motion score index and an improved ejection fraction of the left ventricle. These results of the study were consistent with the results of a single-blind randomized trial [3] and a randomized clinical study [16]. Coronary blood flow abnormalities are associated with morbidities and mortality [20]. High acoustic energy ultrasound might help in the improvement of coronary blood flow for long-term effects.
Contrast-enhanced ultrasound with low-acoustic energy also reported parts of beneficial therapeutic effects like an increase in% ST-segment resolution and ejection fraction. The results of the study were consistent with the animal model study [21]. Low-acoustic energy ultrasound can improve downstream and upstream perfusion but it can be reversed due to the absence of synthetase inhibitor(s) [3]. Ultrasound can improve parameters of patients with ST-segment elevation myocardial infarction in the risk area.
High acoustic energy ultrasound had no effects on heart rate and oxygen saturation. The results of the study were consistent with the results of a single-blind randomized trial [3]. High acoustic energy ultrasound with long-duration impulses may have no potential harm to patients with ST-segment elevation myocardial infarction.
Despite recent warnings regarding contrast agent, the study used the first-generation contrast agent (Optison™). It is useful diagnostic tool for coronary artery diseases and is safe too [22]. The choice of the contrast agent has no effect on sonothrombolysis but definitely has a specific impact on diagnosis of coronary thrombus.
Although the study addressed potential and life-threatening issues by non-invasive methods, there are several limitations of the study, for example, retrospective analysis and absence of the control group, the large multi-central controlled clinical trial is required to validate the hypothesis. Culprit vessels were considered as TIMI flow grades 1 or 2 but flow grades 1 and 2 are different predictors of clinical outcomes [23]. Besides ultrasound, invasive coronary angiographies were performed for the assessment of culprit vessels. The gender differences have an impact on cardiovascular disease [24] but the study did not evaluate such parameters. A lot of confounders and recalling bias reported in the study. Therefore, an adjusted model should be used to calculate the real effect size. The inter- and intra-observer variability did not perform.
Conclusions
The diagnosis of patients with ST-segment elevation myocardial infarction with high acoustic energy ultrasound might improve coronary blood, an ejection fraction of left ventricle, and wall motion score after percutaneous coronary interventions. The study results could be used to address life-threatening salvaging myocardial tissue problems. A dynamic study is required to study the effects of high acoustic energy ultrasound on congestive heart failure and mortality.
Figures
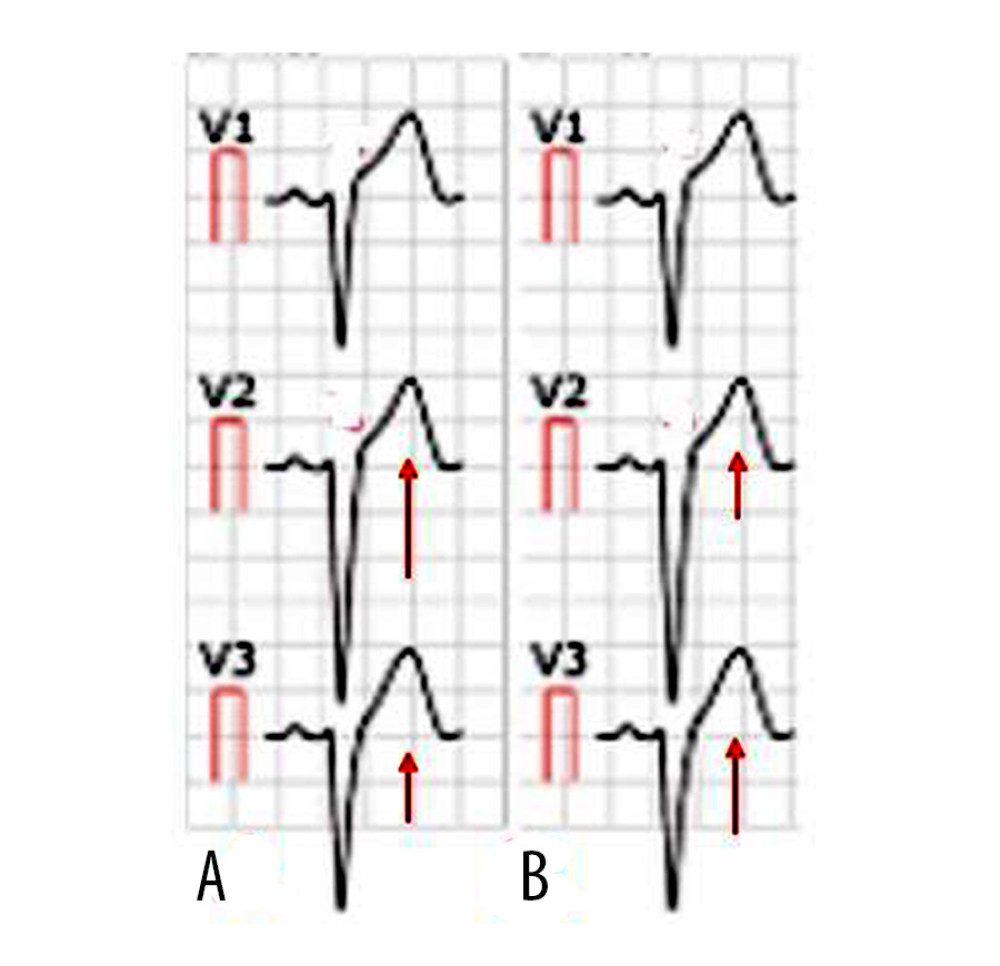 Figure 1. Electrocardiogram. (A) Electrocardiogram of male patient aged 45 years. (B) Electrocardiogram of female patient aged 44 years. The red arrow indicates elevation in ST-segment.
Figure 1. Electrocardiogram. (A) Electrocardiogram of male patient aged 45 years. (B) Electrocardiogram of female patient aged 44 years. The red arrow indicates elevation in ST-segment. 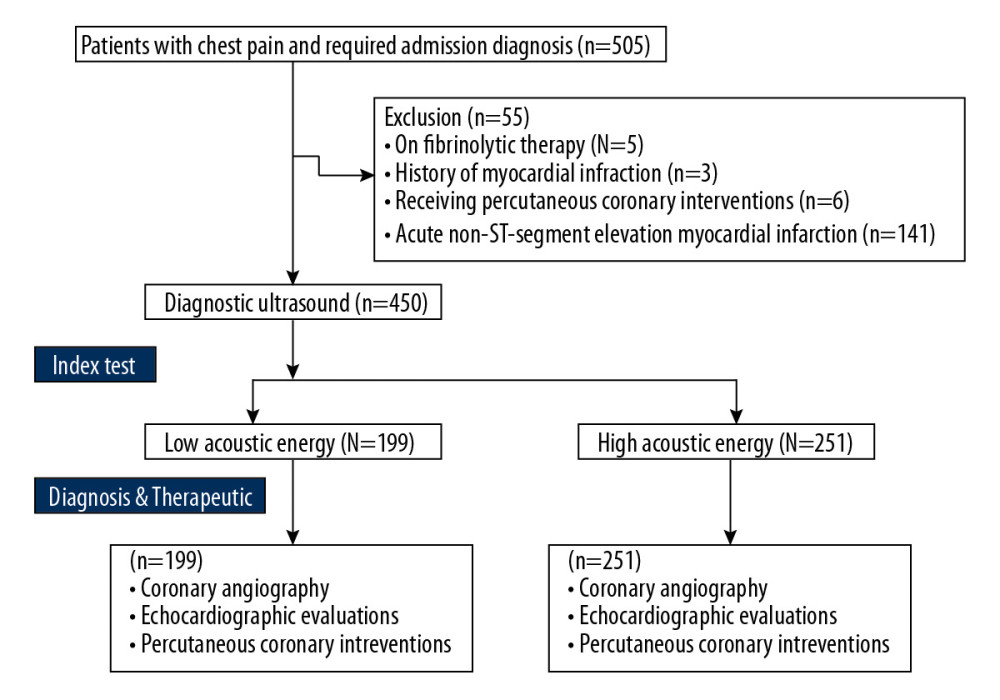 Figure 2. Flowchart of the diagnosis and treatment.
Figure 2. Flowchart of the diagnosis and treatment. 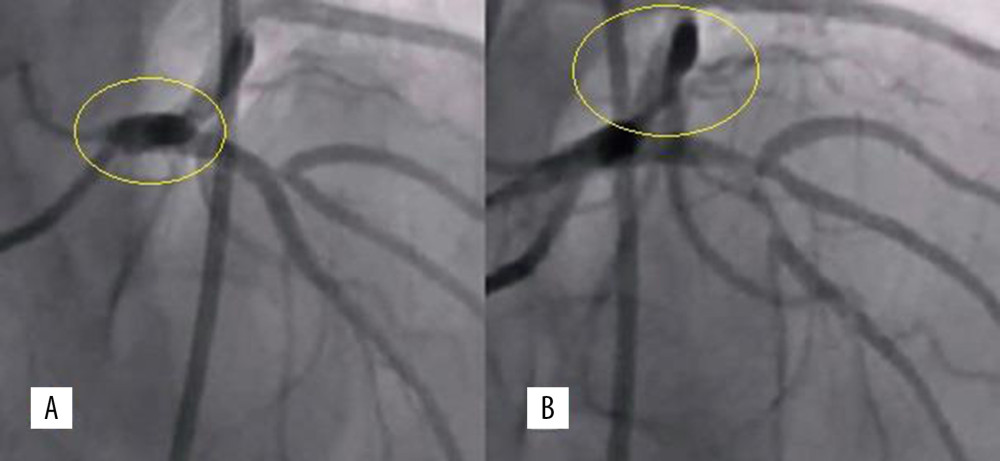 Figure 3. Thrombolysis in myocardial infarction flow grading. (A) Thrombolysis in myocardial infarction flow 2. (B) Thrombolysis in myocardial infarction flow 1.
Figure 3. Thrombolysis in myocardial infarction flow grading. (A) Thrombolysis in myocardial infarction flow 2. (B) Thrombolysis in myocardial infarction flow 1. 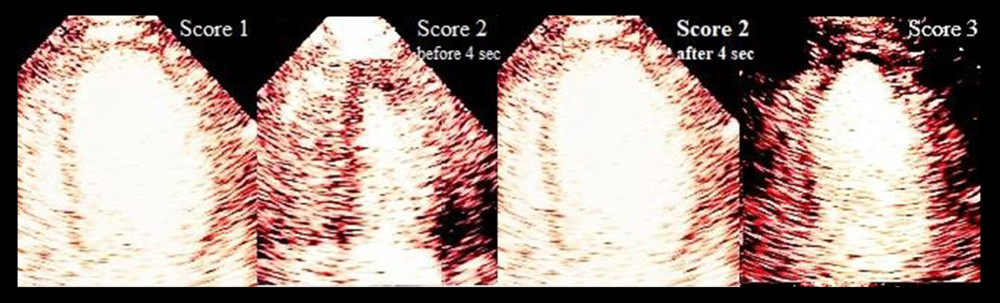 Figure 4. The assessment of microvascular coronary obstruction for low acoustic energy.
Figure 4. The assessment of microvascular coronary obstruction for low acoustic energy. 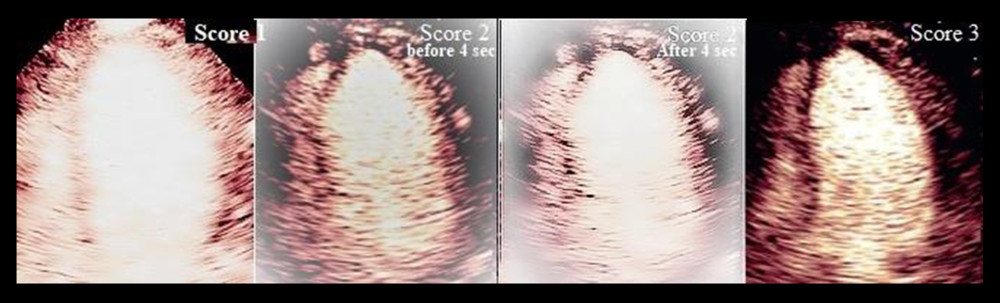 Figure 5. The assessment of microvascular coronary obstruction for high acoustic energy.
Figure 5. The assessment of microvascular coronary obstruction for high acoustic energy. 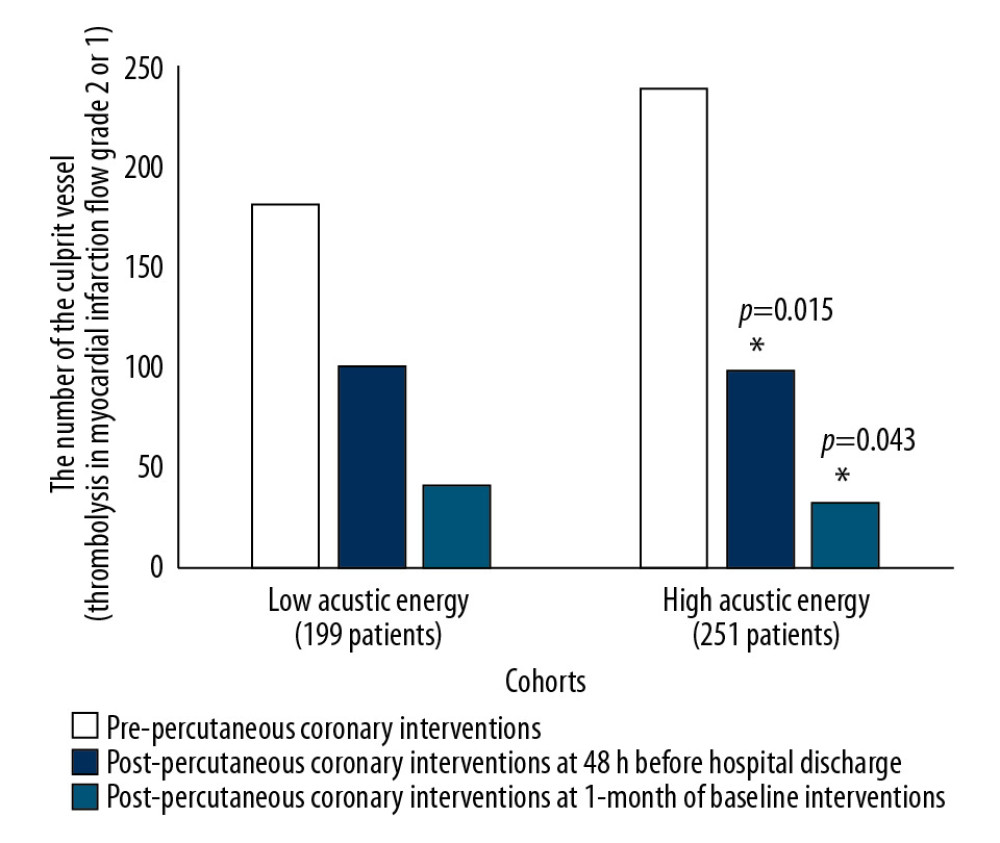 Figure 6. Culprit vessel evaluation by coronary angiography. Data are represented as a frequency. The Fischer’s exact test was performed for statistical analyses. A P<0.05 was considered significant. * Significantly lower than low acoustic energy.
Figure 6. Culprit vessel evaluation by coronary angiography. Data are represented as a frequency. The Fischer’s exact test was performed for statistical analyses. A P<0.05 was considered significant. * Significantly lower than low acoustic energy. References
1. Sadhukhan D, Pal S, Mitra M, Automated identification of myocardial infarction using harmonic phase distribution pattern of ECG data: IEEE Trans Med Imaging, 2018; 67; 2303-13
2. Atkins ER, Du X, Wu Y, Use of cardiovascular prevention treatments after acute coronary syndrome in China and associated factors: Int J Cardiol, 2017; 241; 444-49
3. Mathias W, Tsutsui JM, Tavares BG, Diagnostic ultrasound impulses improve microvascular flow in patients with STEMI receiving intravenous microbubbles: J Am Coll Cardiol, 2016; 67; 2506-15
4. Pantsios C, Kapelios C, Vakrou S, Effect of elevated reperfusion pressure on “no reflow” area and infarct size in a porcine model of ischemia-reperfusion: J Cardiovasc Pharmacol Ther, 2016; 21; 405-11
5. Vidal-Perez R, Abou Jokh Casas C, Agra-Bermejo RM, Gonzalez-Juanatey JR, Myocardial infarction with non-obstructive coronary arteries: A comprehensive review and future research directions: World J Cardiol, 2019; 11; 305-15
6. Gao Z, Chung J, Abdelrazek M, Privileged modality distillation for vessel border detection in intracoronary imaging: IEEE Trans Med Imaging; 2019 [Epub ahead of print]
7. Xie F, Gao S, Wu J, Diagnostic ultrasound induced inertial cavitation to non-invasively restore coronary and microvascular flow in acute myocardial infarction: PLoS One, 2013; 8; e69780
8. Eggers J, Konig IR, Koch B, Sonothrombolysis with transcranial color-coded sonography and recombinant tissue-type plasminogen activator in acute middle cerebral artery main stem occlusion: Results from a randomized study: Stroke, 2008; 39; 1470-75
9. Barlinn K, Tsivgoulis G, Barreto AD, Outcomes following sonothrombolysis in severe acute ischemic stroke: Subgroup analysis of the CLOTBUST trial: Int J Stroke, 2014; 9; 1006-10
10. Gaydos SS, Varga-Szemes A, Judd RN, Imaging in adult congenital heart disease: J Thorac Imaging, 2017; 32; 205-16
11. Feinstein SB, The evolution of contrast ultrasound: from diagnosis to therapy: J Am Coll Cardiol, 2016; 67; 2516-18
12. Lenz CJ, Abdelmoneim SS, Anavekar NS, A comparison of infarct mass by cardiac magnetic resonance and real time myocardial perfusion echocardiography as predictors of major adverse cardiac events following reperfusion for ST elevation myocardial infarction: Echocardiography, 2016; 33; 1539-45
13. Majidi M, Kosinski AS, Al-Khatib SM, Implications of ventricular arrhythmia “bursts” with normal epicardial flow, myocardial blush, and ST-segment recovery in anterior ST-elevation myocardial infarction reperfusion: A biosignature of direct myocellular injury “downstream of downstream”: Eur Heart J Acute Cardiovasc Care, 2015; 4; 51-59
14. Lang RM, Badano LP, Mor-Avi V, Recommendations for cardiac chamber quantification by echocardiography in adults: An update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging: J Am Soc Echocardiogr, 2015; 28; 1-39.e14
15. Porter TR, Adolphson M, High RR, Rapid detection of coronary artery stenoses with real-time perfusion echocardiography during regadenoson stress: Circ Cardiovasc Imaging, 2011; 4; 628-35
16. Mathias W, Tsutsui JM, Tavares BG, Sonothrombolysis in ST-segment elevation myocardial infarction treated with primary percutaneous coronary intervention: J Am Coll Cardiol, 2019; 73; 2832-42
17. Porter TR, Xie F, Lof J, The thrombolytic effect of diagnostic ultrasound-induced microbubble cavitation in acute carotid thromboembolism: Invest Radiol, 2017; 52; 477-81
18. Leeman JE, Kim JS, Yu FT, Effect of acoustic conditions on microbubble-mediated microvascular sonothrombolysis: Ultrasound Med Biol, 2012; 38; 1589-98
19. Pacella JJ, Brands J, Schnatz FG: Ultrasound Med Biol, 2015; 41; 456-64
20. Rezkalla SH, Stankowski RV, Hanna J, Kloner RA, Management of no-reflow phenomenon in the catheterization laboratory: JACC Cardiovasc Interv, 2017; 10; 215-23
21. Xie F, Lof J, Everbach C, Treatment of acute intravascular thrombi with diagnostic ultrasound and intravenous microbubbles: JACC Cardiovasc Imaging, 2009; 2; 511-18
22. Dolan MS, Gala SS, Dodla S, Safety and efficacy of commercially available ultrasound contrast agents for rest and stress echocardiography a multicenter experience: J Am Coll Cardiol, 2009; 53; 32-38
23. Ge H, Ding S, An D, Frame counting improves the assessment of post-reperfusion microvascular patency by TIMI myocardial perfusion grade: Evidence from cardiac magnetic resonance imaging: Int J Cardiol, 2016; 203; 360-66
24. Shah T, Palaskas N, Ahmed A, An update on gender disparities in coronary heart disease care: Curr Atheroscler Rep, 2016; 18; 28
Figures
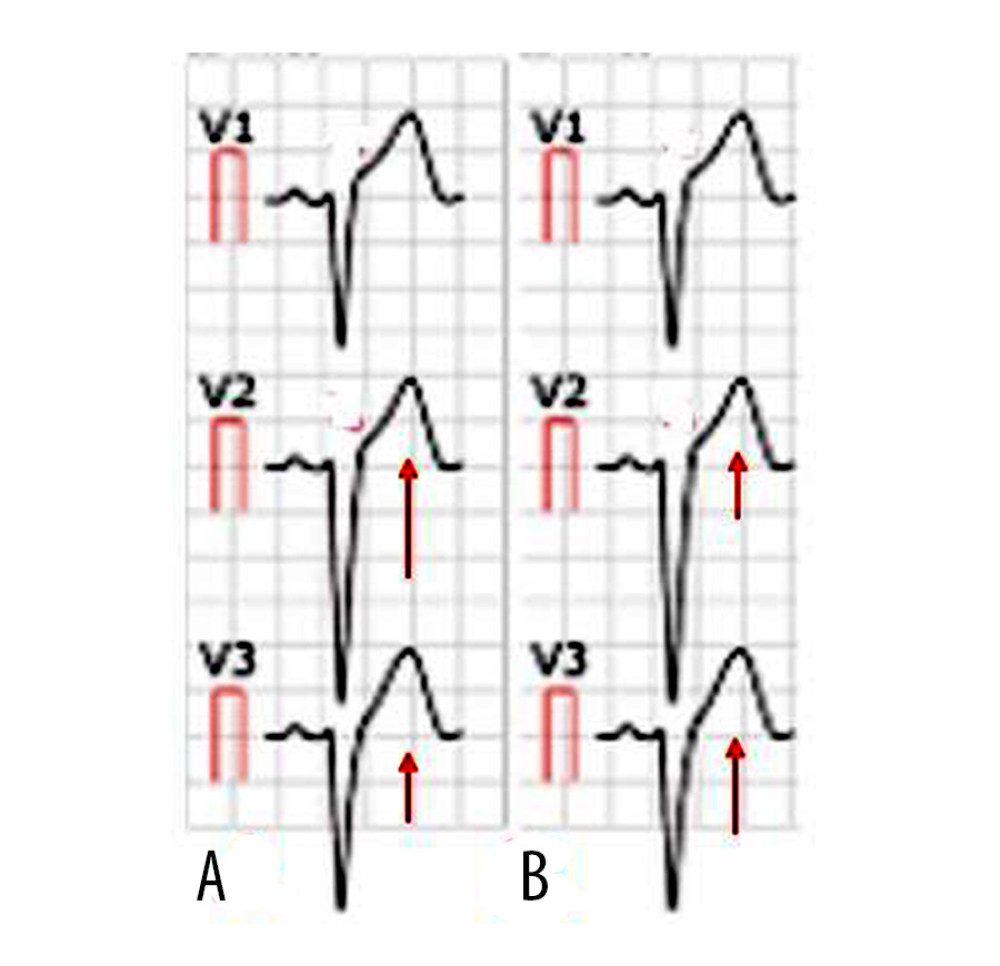 Figure 1. Electrocardiogram. (A) Electrocardiogram of male patient aged 45 years. (B) Electrocardiogram of female patient aged 44 years. The red arrow indicates elevation in ST-segment.
Figure 1. Electrocardiogram. (A) Electrocardiogram of male patient aged 45 years. (B) Electrocardiogram of female patient aged 44 years. The red arrow indicates elevation in ST-segment.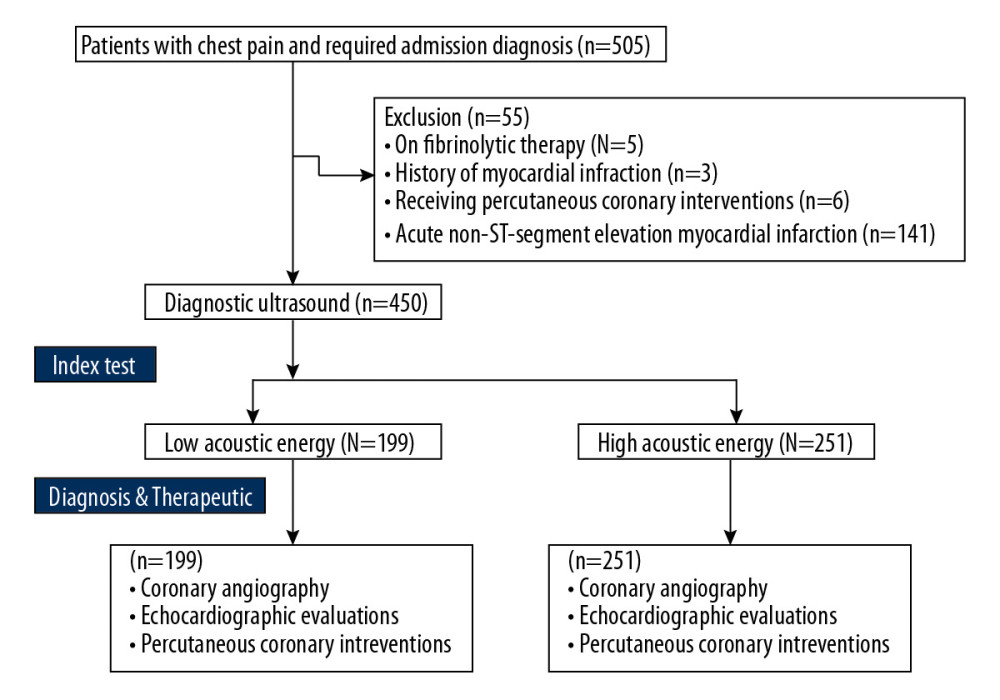 Figure 2. Flowchart of the diagnosis and treatment.
Figure 2. Flowchart of the diagnosis and treatment.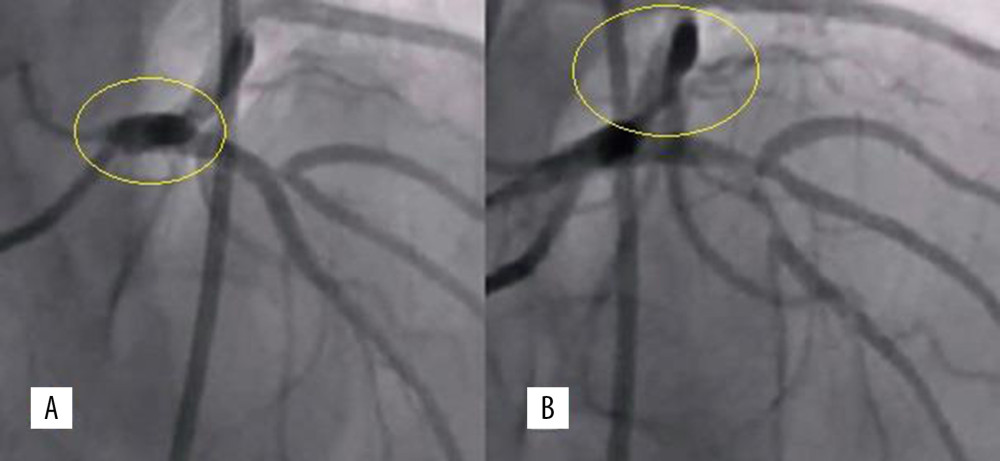 Figure 3. Thrombolysis in myocardial infarction flow grading. (A) Thrombolysis in myocardial infarction flow 2. (B) Thrombolysis in myocardial infarction flow 1.
Figure 3. Thrombolysis in myocardial infarction flow grading. (A) Thrombolysis in myocardial infarction flow 2. (B) Thrombolysis in myocardial infarction flow 1.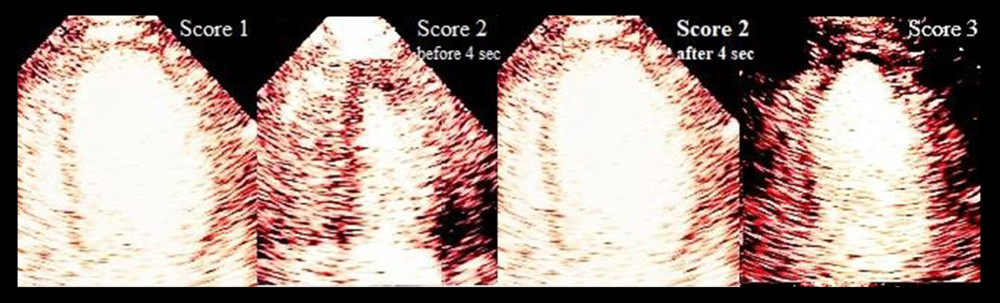 Figure 4. The assessment of microvascular coronary obstruction for low acoustic energy.
Figure 4. The assessment of microvascular coronary obstruction for low acoustic energy.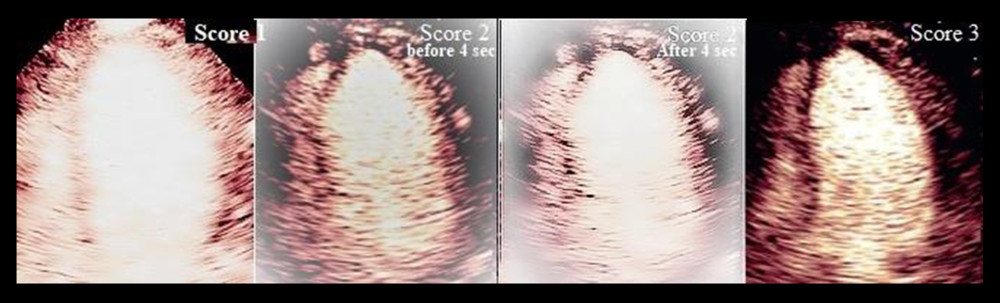 Figure 5. The assessment of microvascular coronary obstruction for high acoustic energy.
Figure 5. The assessment of microvascular coronary obstruction for high acoustic energy.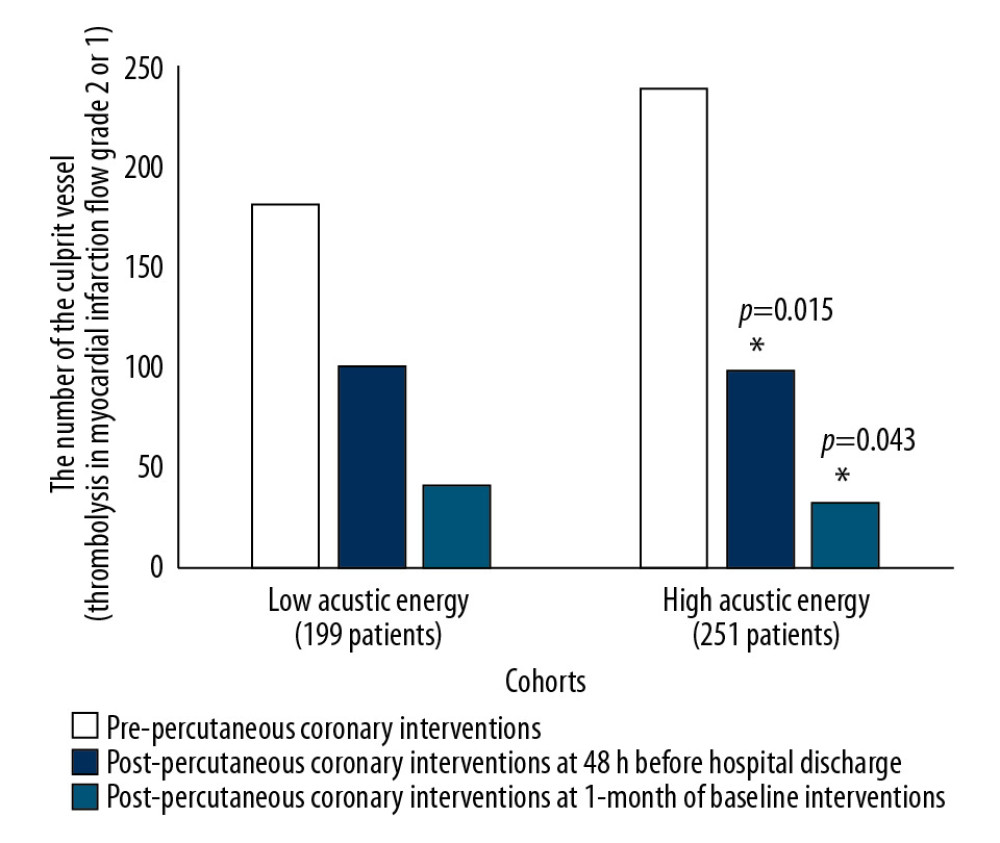 Figure 6. Culprit vessel evaluation by coronary angiography. Data are represented as a frequency. The Fischer’s exact test was performed for statistical analyses. A P<0.05 was considered significant. * Significantly lower than low acoustic energy.
Figure 6. Culprit vessel evaluation by coronary angiography. Data are represented as a frequency. The Fischer’s exact test was performed for statistical analyses. A P<0.05 was considered significant. * Significantly lower than low acoustic energy. Tables
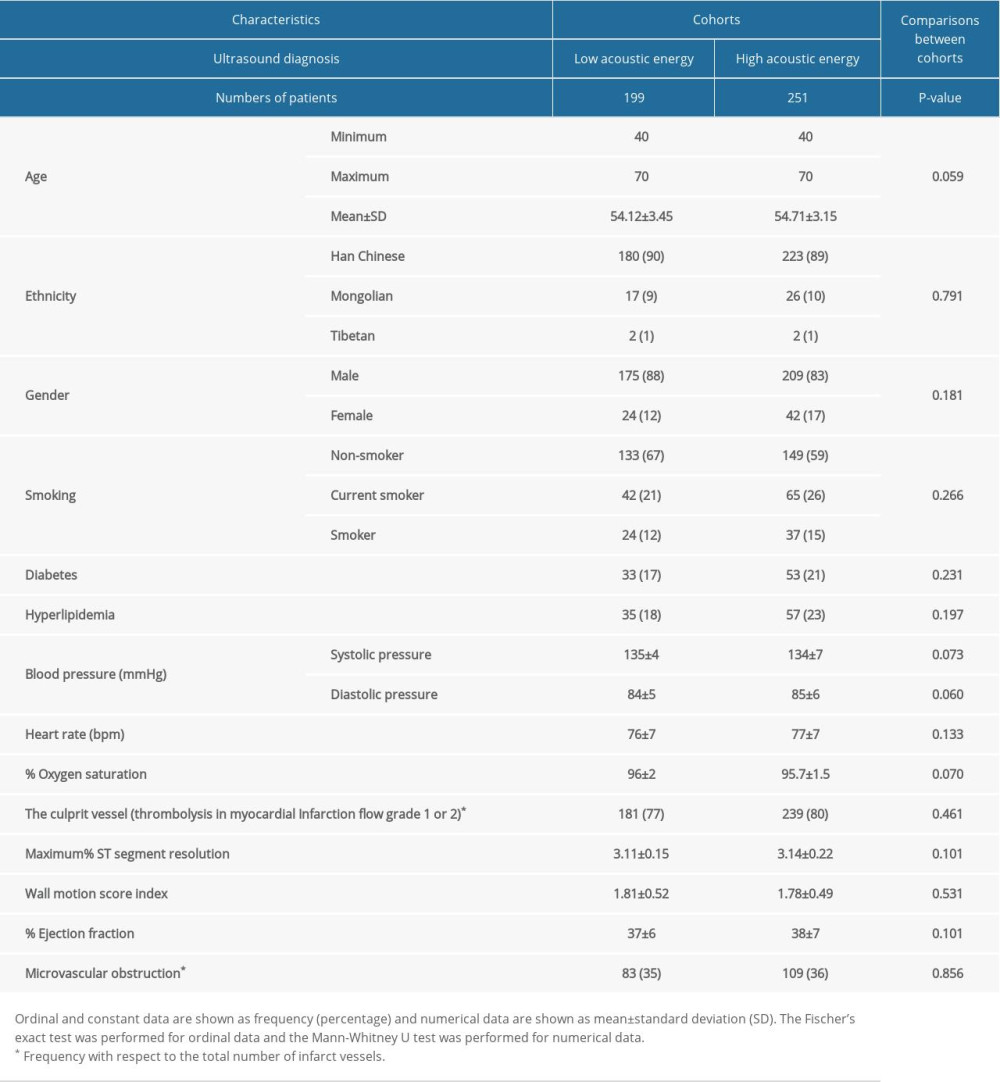 Table 1. Demographical, clinical, and pre-percutaneous coronary interventions characteristics.
Table 1. Demographical, clinical, and pre-percutaneous coronary interventions characteristics.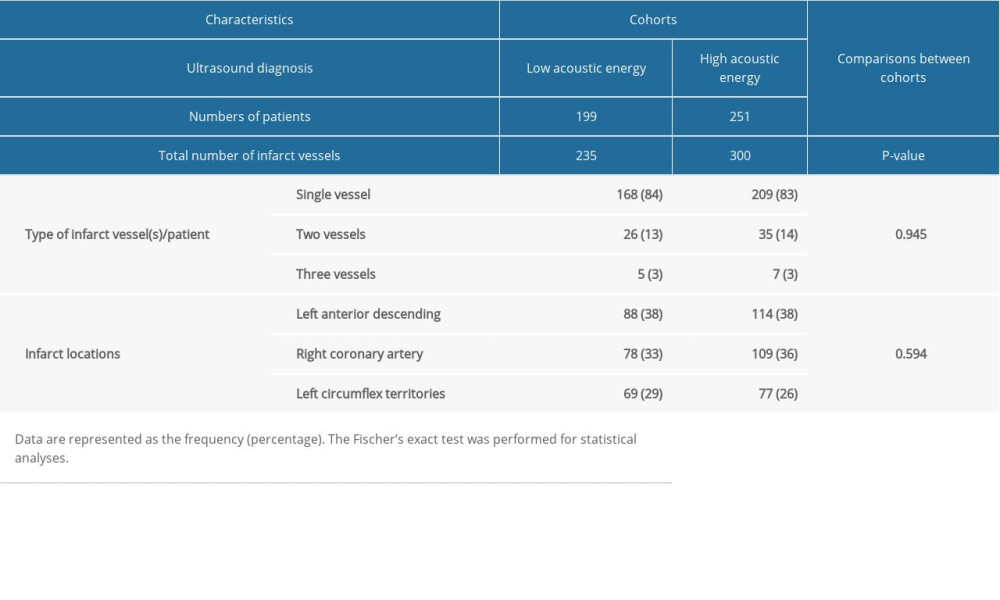 Table 2. Coronary angiography characteristics.
Table 2. Coronary angiography characteristics.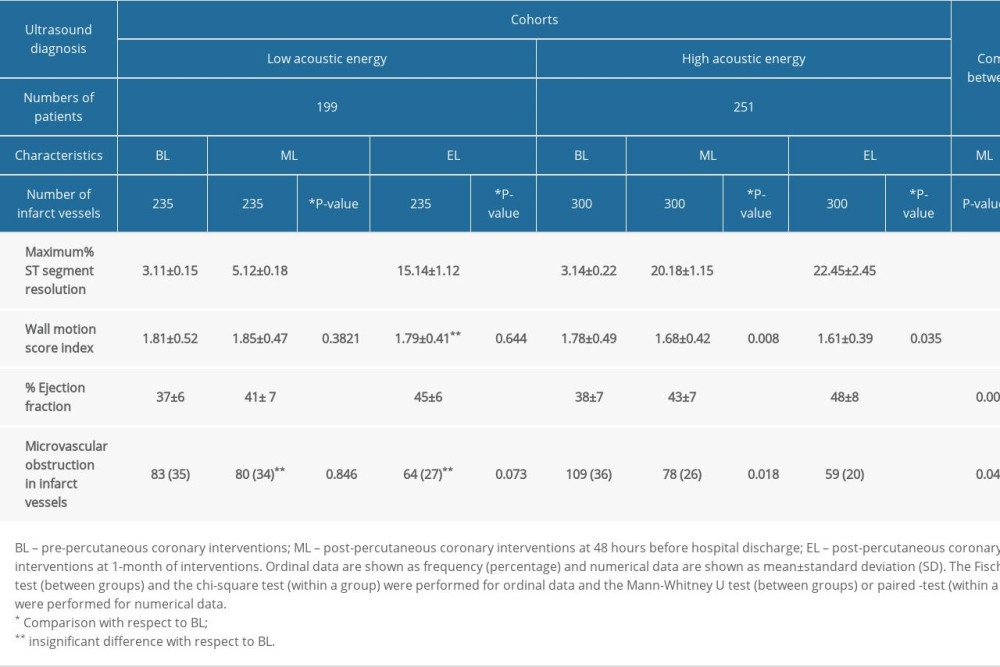 Table 3. Echocardiographic evaluations.
Table 3. Echocardiographic evaluations.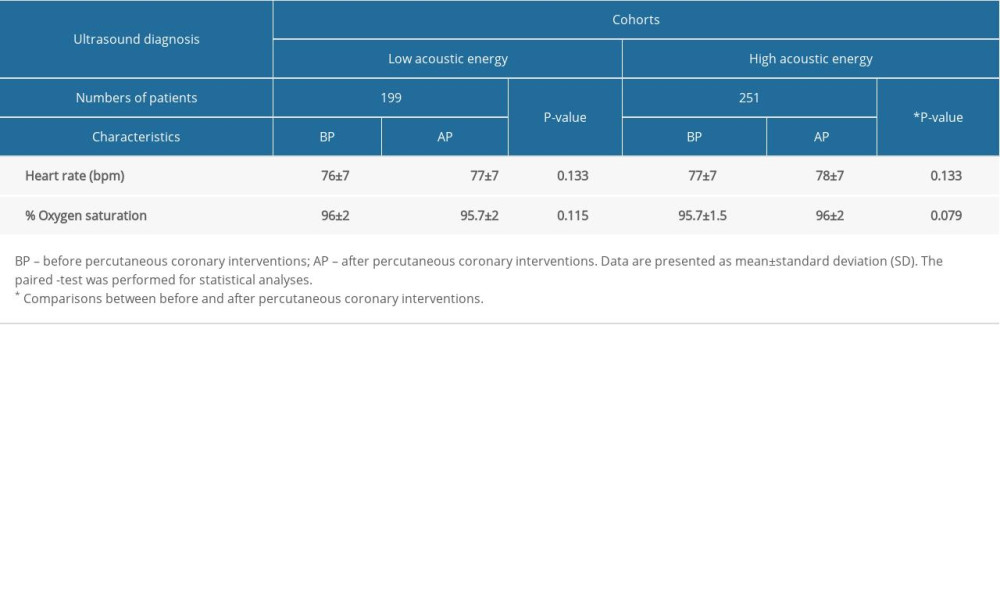 Table 4. Safety study.
Table 4. Safety study.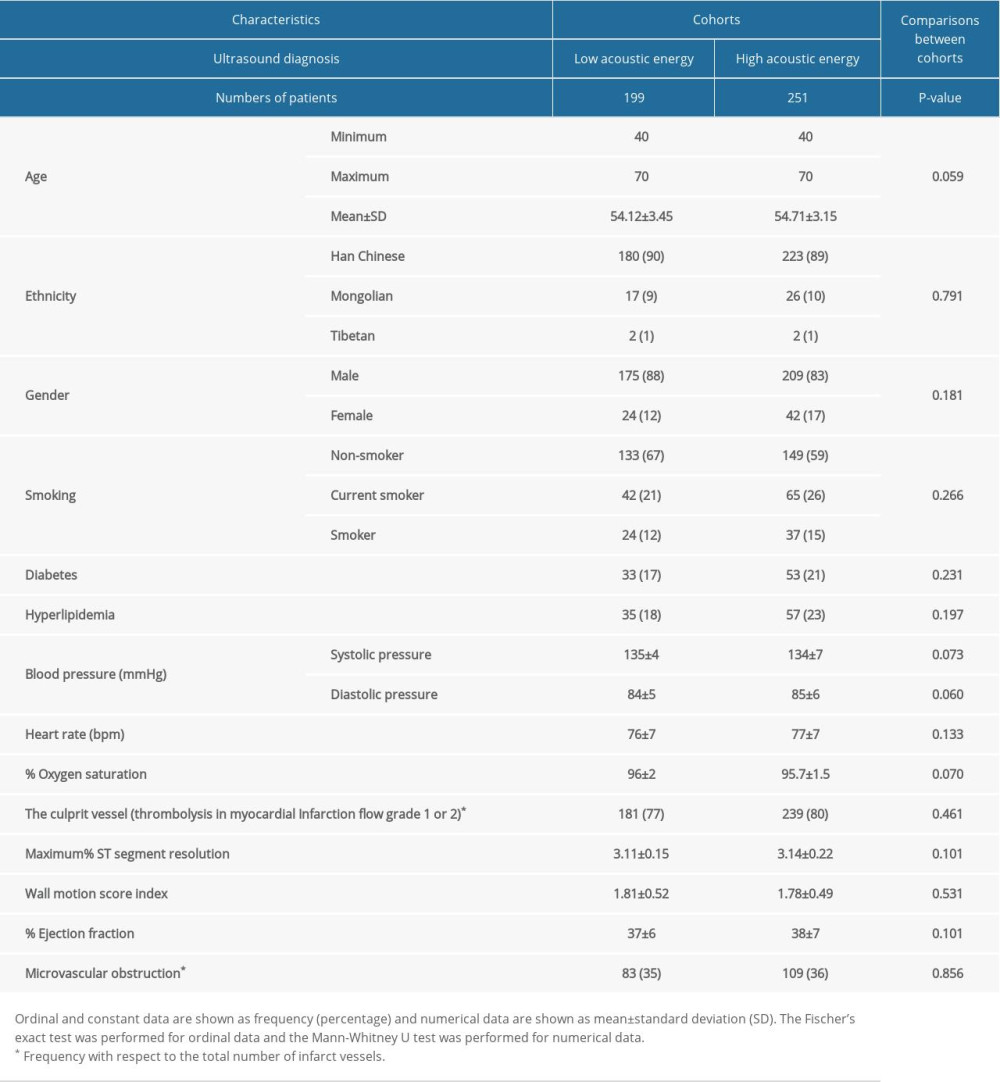 Table 1. Demographical, clinical, and pre-percutaneous coronary interventions characteristics.
Table 1. Demographical, clinical, and pre-percutaneous coronary interventions characteristics.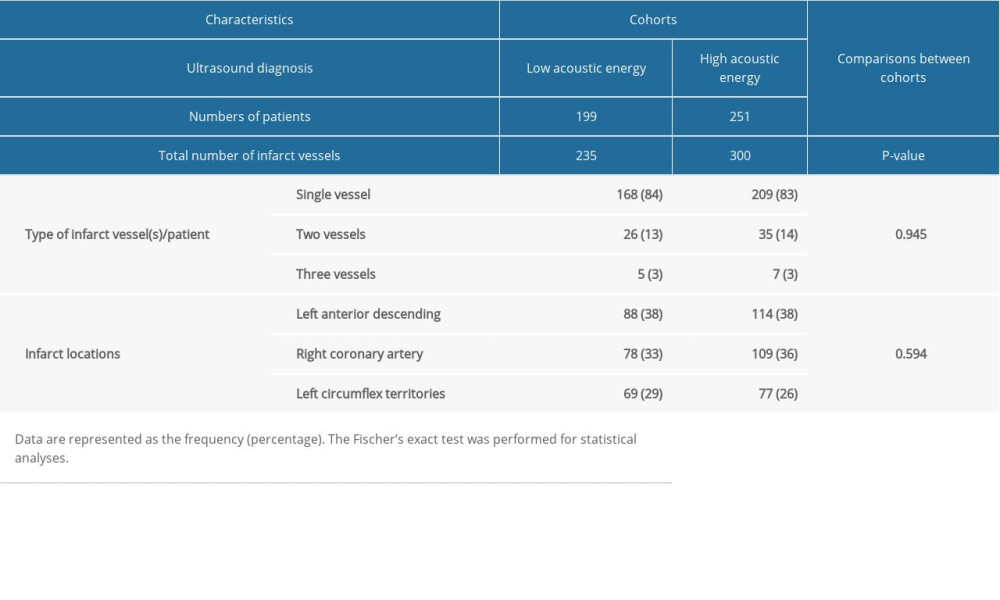 Table 2. Coronary angiography characteristics.
Table 2. Coronary angiography characteristics.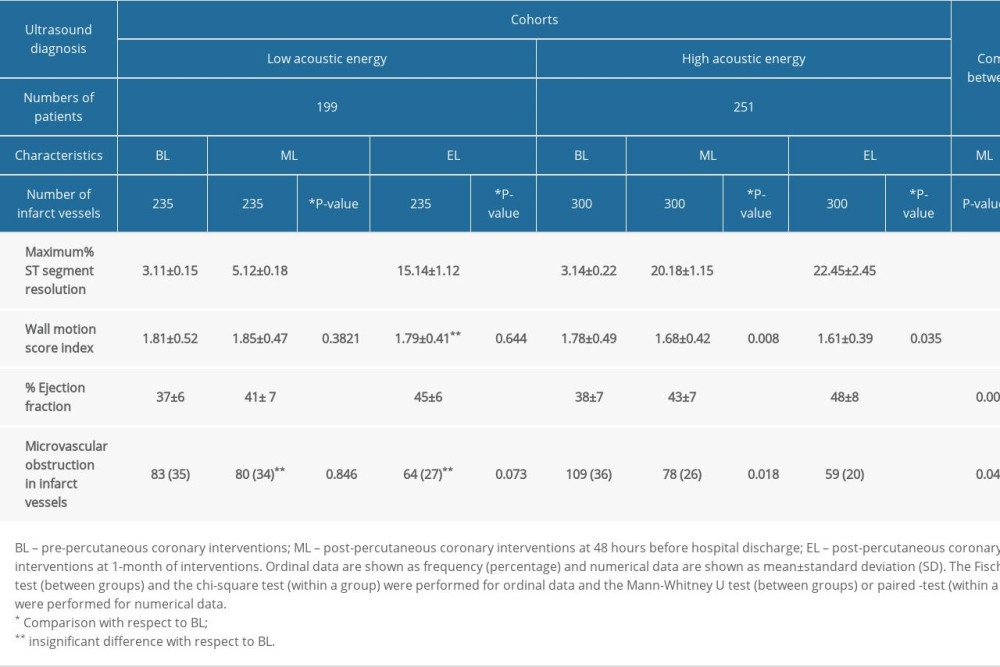 Table 3. Echocardiographic evaluations.
Table 3. Echocardiographic evaluations.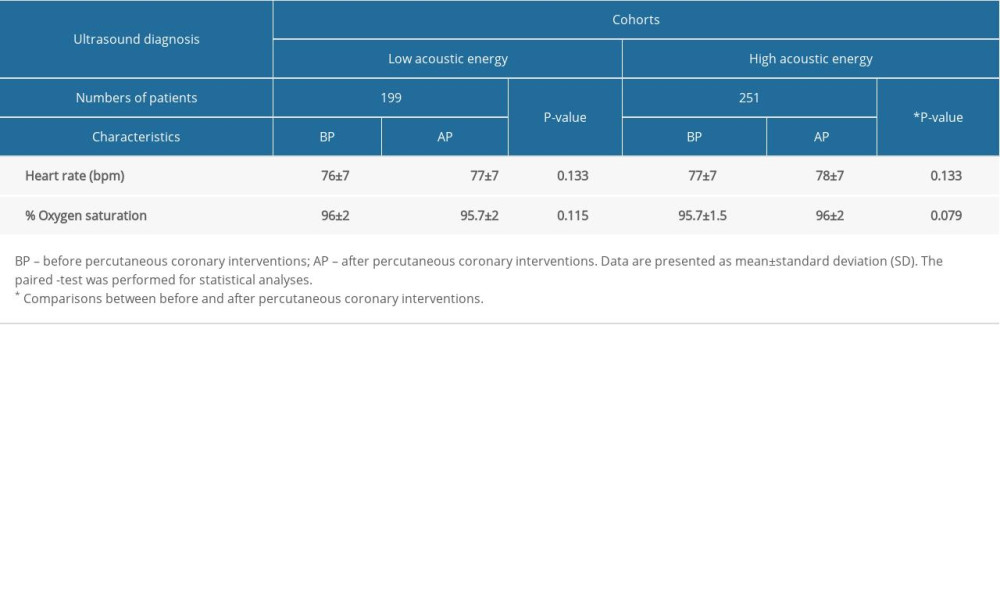 Table 4. Safety study.
Table 4. Safety study. In Press
06 Mar 2024 : Clinical Research
Comparison of Outcomes between Single-Level and Double-Level Corpectomy in Thoracolumbar Reconstruction: A ...Med Sci Monit In Press; DOI: 10.12659/MSM.943797
21 Mar 2024 : Meta-Analysis
Economic Evaluation of COVID-19 Screening Tests and Surveillance Strategies in Low-Income, Middle-Income, a...Med Sci Monit In Press; DOI: 10.12659/MSM.943863
10 Apr 2024 : Clinical Research
Predicting Acute Cardiovascular Complications in COVID-19: Insights from a Specialized Cardiac Referral Dep...Med Sci Monit In Press; DOI: 10.12659/MSM.942612
06 Mar 2024 : Clinical Research
Enhanced Surgical Outcomes of Popliteal Cyst Excision: A Retrospective Study Comparing Arthroscopic Debride...Med Sci Monit In Press; DOI: 10.12659/MSM.941102
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








