26 June 2020: Clinical Research
A Prospective Study Comparing Adolescent and Post-Adolescent Periods Regarding Effects of Activator Appliance in Patients with Class II Mandibular Retrognathia by Using 3dMDface Analysis and Cephalometry
Esra Yüksel Coşkun1BEF*, Elçin Esenlik2ACDGDOI: 10.12659/MSM.921401
Med Sci Monit 2020; 26:e921401
Abstract
BACKGROUND: The purpose of this prospective study was to compare adolescent and post-adolescent growth periods regarding the effectiveness of conventional activator appliance in patients with Class II mandibular retrognathia by using lateral cephalometric radiographs and three-dimensional photogrammetry (3dMDface).
MATERIAL AND METHODS: We enrolled 2 groups: 15 patients in the adolescent growth period and 17 patients in the post-adolescent growth period. All patients had Class II anomaly with mandibular retrognathia and were treated with conventional activator appliances. Lateral cephalometric radiographs and three-dimensional photogrammetric views were obtained at the beginning and end of the activator treatment of Class II patients. Maxillomandibular discrepancy, mandibular protrusion and lengths, convexity angles, facial heights, and dental measurements were evaluated cephalometrically. Projections of the lips and the chin and volumetric measurements of the lip and the mandibular area were assessed using three-dimensional photogrammetry.
RESULTS: Conventional activator therapy resulted in similar effects in both growth periods regarding improvements in the mandibular sagittal growth and maxillomandibular relationship (ANB° and the SNB° angles). Mandibular effective length was increased (Co-Gn length) and the maxillary horizontal growth was restricted (decreased SNA° angle) in both groups following the treatment. Treatment duration was significantly longer in the post-adolescent group. Increases in the projections of menton, pogonion, and sublabial points were observed in the three-dimensional photogrammetric views. Total lip volume was reduced while the mandibular volume was significantly increased in both groups. Lower gonial angle showed a greater increase in the post-adolescent group.
CONCLUSIONS: Correction of Class II anomaly with mandibular retrognathia was achieved with a combination of dental and skeletal changes in both growth periods. Conventional activator therapy may be an alternative treatment approach in the late growth period as it led to significant skeletal and dental changes.
Keywords: Imaging, Three-Dimensional, Puberty, retrognathia, young adult, Activator Appliances, Adolescent, Age Factors, Bone Development, Carpal Bones, Cephalometry, Child, Hand Bones, Malocclusion, Angle Class II, Mandible, Maxilla, Maxillofacial Development, Photogrammetry, Prospective Studies
Background
Skeletal Class II anomalies exhibit maxillomandibular sagittal discrepancy and are more commonly associated with mandibular retrognathia [1–4]. Several methods and appliances have been used for decades for treating mandibular retrognathia in growing patients. One of the generic names of these kind of appliances is functional orthopedic appliances, which serve as mandibular advancement splints in the management of mandibular retrognathia. They refer to a variety of removable appliances designed to provide mandibular sagittal growth improvement by rearranging the masticatory muscle groups and are commonly used in growing Class II patients [5]. The effectiveness of this approach in treating mandibular retrognathia has been investigated for decades [6–17]. The conventional activator was the first appliance used for functional orthopedic treatment [18]. Subsequently, many appliances, such as twin block, Bionator, Frankel, or their modifications, were introduced for treating mandibular retrognathia in adolescent-period patients [6–9,19–22]. It has been targeted to increase the mandibular length by stimulating the condylar growth with any of these removable appliances and also to minimize the dental adverse effects. There has been considerable controversy about the skeletal effects of these appliances in treating mandibular retrognathia [23]. Some researchers have advocated that an increase in the mandibular length can be achieved with the functional orthopedic appliances rather than other fixed orthodontic appliances. However, others have suggested that the functional orthopedic therapy did not alter the mandibular length [8,24] and the overjet elimination can only be achieved by dental movement [25,26]. Treatment timing and the effectiveness of these appliances are another important factor as well as the appliance type. Various opinions have been expressed in the literature on the optimal treatment timing for the functional orthopedic treatment to obtain the best skeletal results. Most of the researchers have suggested that it is appropriate to perform functional orthopedic treatment at the beginning of the adolescent period or at the late mixed or permanent dentition to obtain more improvement in sagittal mandibular growth [22,27–29]. However, other researchers have suggested that functional orthopedic treatment may be performed in the post-adolescent period as an alternative to surgical treatment [30,31]. In studies conducted by Ruf and Pancherz, an increase in the mandibular length and mandibular sagittal activation were observed in young adult patients [30–32]. However, another study by the same authors reported undesirable mandibular growth following conventional activator therapy [33]. Therefore, the first purpose of this prospective study was to compare adolescent and post-adolescent periods regarding the effectiveness of conventional activator appliance in patients with Class II mandibular retrognathia by using lateral cephalometric radiographic analyses.
Evaluations of the hard and soft tissues and dentition have an essential role in the planning of orthodontic treatment, especially in patients who require skeletal corrections. Three-dimensional photogrammetry is a useful system for clinicians in assessing the soft tissues of patients [34,35]. Conventional two-dimensional evaluations have been supported by three-dimensional images to diagnose and evaluate outcomes, which has become more popular in the last decade [36–38]. Therefore, the second purpose of this prospective study was to evaluate the effects of conventional activator therapy on facial soft tissues in these Class II patients by using three-dimensional photogrammetry.
Material and Methods
THE CONVENTIONAL ACTIVATOR APPLIANCE DESIGN:
This study included patients with skeletal Class II mandibular retrognathia, and all of them were treated by the conventional activator appliance. The conventional activator appliances were used with one-step advancement (maximum jumping) of the mandible and were activated until the upper and lower incisors were in edge-to-edge position. The thickness of the posterior part of the appliance was approximately 4–5 mm. An ‘acrylic cap’ covering 3 mm of the labial surfaces of the mandibular incisors was used to prevent undesired protrusion of the mandibular incisors. The patients were instructed to wear the conventional activator appliance for 16–18 hours a day. Patients were examined at 4-week intervals. The treatment was continued until the mandible did not slide through backward in both groups (Figure 2).
LATERAL CEPHALOMETRIC RADIOGRAPHIC ANALYSIS (TWO-DIMENSIONAL):
The lateral cephalometric radiographic records of the patients were analyzed with NemoCeph NX (Nemotech, Madrid, Spain), a computerized lateral cephalometric radiographic analysis program. Twenty-one linear and 15 angular lateral cephalometric radiographic measurements were performed (Figure 3, Table 2) [43–47]. A basicranial line passing through the tuberculum sella (T) and the wing points of sphenoid (W) was used as a sagittal reference plane (TW) (Figure 3C, 3D). Another line constructed perpendicular to the basicranial line and passing through the point T was used as a vertical reference line (VRL) (Figure 3C, 3D). The sagittal distances from the A point and the pogonion were calculated. Maxillomandibular angular and linear measurements used in this study are shown in Figure 3. All measurements were repeated by the same orthodontist and the intraobserver variability was non-significant.
THREE-DIMENSIONAL PHOTOGRAMMETRIC ANALYSIS:
Three-dimensional photogrammetry can capture 3D images of the craniofacial complex in 2 milliseconds without ionizing radiation, and three-dimensional images can be formed by photographing with the help of 2 or more cameras from at least 2 different planes [35,48]. Volumetric measurements can be generated with three-dimensional photogrammetry in addition to linear and angular measurements, and these measurements improve diagnosis and evaluation of outcomes.
Three-dimensional images were obtained using the 3dMDface system (3dMDface LLC, Atlanta, GA, USA). The images were transferred to 3dMDface Vultus® software (3dMDface Vultus® software version 2.3.0.2, 3dMDface, Atlanta, GA, USA) and analyzed. After transferring these images to the 3dMDface Vultus® software, they were reoriented for the standardization in 3 dimensions. Unnecessary fields of the images were removed for ease of analysis. Fourteen linear, 7 angular, and 2 volumetric measurements were performed on the 3dMDface Vultus® software (Figures 4–6, Table 3) [46,49]. Perpendicular distances from menton (Me), pogonion (Pg), and sublabial (Sl) points to the coronal and axial planes were calculated (Figures 4, 7). The coronal plane (CP) was defined as the vertical plane passing through the outer canthi of both eyes and the axial plane (AP) was defined as the horizontal line passing through the outer canthi of both eyes, and were positioned parallel to the Frankfort horizontal plane (FH). The mandibular volume was measured from the right (Ch-R) and left lip-edge points (Ch-L) and menton (Me) point, as shown in Figure 6A. For measuring the total lip volume, a contour was formed by placing points at 2-mm intervals on the upper and lower vermilion lines. The volume of the region between these contours was calculated using the software program (Figure 6B).
STATISTICAL ANALYSIS:
All statistical analyses were performed using SPSS statistics 22.0 for Windows (Statistical Package for Social Science for Windows, version 22.0, SPSS Inc, Chicago, IL, US). The paired-sample
Results
LATERAL CEPHALOMETRIC RADIOGRAPHIC FINDINGS:
The results showed that the maxillary growth was restricted (decreased SNA°) and the sagittal mandibular growth was stimulated (increased SNB°). A significant improvement in the sagittal relationship of the jaws (decrease in the ANB° and the wits value) was obvious in both groups (p<0.05). Mandibular ramus length (Co-Gn) was increased by 2.97 mm and 2.68 mm in the adolescent and the post-adolescent groups, respectively (p<0.05). Moreover, convexity angles were increased in both groups. Statistically significant increases were observed in the FH⊥Na-Pg and the SN-GoGn° parameters, while a statistically significant decrease was found in the Pg-NB in both groups (p<0.05). No significant differences were observed between the groups in terms of these parameters, except for the gonial and the lower gonial angles. Increases in these angles were more significant in the adolescent group than in the post-adolescent group (p<0.05, Table 4).
When the face height measurements were examined, statistically significant increases were observed in the anterior and posterior facial heights (AFH, LAFH, and PFH) in both groups (p<0.05). However, there was no significant difference in the Jarabak ratio between the groups (Table 4).
Changes in the parameters related to the upper lip and the upper incisors (UL-S, U1-NA°, and nasolabial angle) were not statistically significant in either the adolescent or in the post-adolescent group. However, the parameters related to the lower lip and the lower incisors (LL-S, labiomental sulcus, labiomental angle, L1-NB°, IMPA°, Pg-VRL, and Ls-VRL) exhibited statistically significant increases in both groups (p<0.05). The mentocervical angle decreased by 5.03° and 2.75° in the adolescent and post-adolescent groups, respectively, and the differences were significant between the groups (p<0.05).
THREE-DIMENSIONAL PHOTOGRAMMETRIC FINDINGS:
Projections of menton, sublabial, and pogonion points showed statistically significant increases in both groups. Significant increases were observed in the anterior, posterior, and lower anterior facial heights, convexity angles, lower lip angle, and labiomental angle.
When the lip and the chin measurements were evaluated in the groups, the lip width, the upper lip length, and the chin height did not show any significant changes, while the lower lip length was significantly increased (p<0.05). The total lip volume was significantly decreased and the mandibular volume was significantly increased in both groups. No significant changes were observed between the groups regarding the treatment changes, except for the nose height and the anterior facial height; these 2 parameters showed greater increases in the adolescent group than in the post-adolescent group (p<0.05, Table 5).
Discussion
The issue of optimal timing for functional orthopedic treatment in Class II patients has been discussed for many years [27,29,50,51]. The discussion involved the age or the stages of dentition such as late mixed dentition and early permanent dentition. However, in the present study, groups were divided based on growth periods because substantial variations are presented in the orthodontic patients regarding dental, chronologic, and skeletal ages [31,32,52]. Most of researchers have stated that the adolescent growth spurt is the most appropriate time for the functional orthopedic treatment for mandibular growth modification [53,54]. However, others have reported that functional orthopedic treatment can be performed in the post-adolescent period as well, and patients with moderately severe mandibular retrognathia can be treated without orthognathic surgery [55,56]. Studies that did not advocate the orthopedic effects of the functional appliances have stated that it does not provide any mandibular stimulation and causes unfavorable growth of the mandible [7,57,58]. In addition to the concerns about the rate of the orthopedic effects of the functional appliances, concerns about patient compliance and certain adverse effects on the incisors have resulted in a very limited number of studies in patients in the late growth period or adulthood. Most of the late growth period studies are related to the effects of the Herbst appliance, which was found to be very effective in the post-adolescent and the young adulthood periods with respect to skeletal responses [32]. In the present study, effects of the conventional activator appliance in the adolescent group and the post-adolescent group were compared with respect to mandibular growth stimulation and soft tissue response, because the conventional activator appliance has been rarely studied in the subjects in late growth period [59].
Overjet correction with the functional orthopedic treatment has been reported by many studies [60–62]. However, there is still a lack of consensus regarding the contribution rates of the orthopedic and the orthodontic components for elimination of overjet using conventional activator therapy. Some clinicians believe that the changes are primarily dentoalveolar, with some maxillary orthopedic effects [8,22,26,60,63–65]. Others stated that functional appliance therapy results primarily in orthodontic changes, with increased mandibular length [28,66–69]. In the present study, the treatment effects for both growth periods were a combination of skeletal and dental improvements. The significant reductions of overjet were 4.57 and 4.13 mm in the adolescent and post-adolescent growth periods, respectively. The restriction of maxillary growth and the stimulation of mandibular growth resulted in significant reduction in the ANB° by 3.47° and 3.01° in the adolescent and the post-adolescent growth periods, respectively. This improvement was mainly due to advancement of the mandible (increase in the SNB° by 2.9° and 2.68°, respectively, in the 2 groups) and due to maxillary growth inhibition (decrease in the SNA° by 0.56° and 0.33°, respectively) to a lesser extent. These results were consistent with previous studies that showed the orthopedic effects of conventional activator therapy on mandibular growth [5,8,30,55,61,66,70,71]. In one of the few studies conducted on untreated Class II patients, SNB° was found to be almost stable (0.17°) compared to growing subjects treated with a functional appliance [66].
With respect to the effective mandibular length, the Co-Gn parameter presented a significant increase of 2.97 mm and 2.68 mm in the adolescent and the post-adolescent groups, respectively. This increase was not statistically different between the groups. In previous studies, the range of the increase in the growth of the mandible in the late growth period was reported to be 1–4.15 mm following treatment with functional appliances [22,31,71,72]. Most researchers have found that craniofacial growth may extend to the late stages of growth and development in both males and females [73–77]. Björk (1963) revealed that an increase in the condylar growth was recorded even, after age 20 years [78]. Ruf and Pancherz (2006), in their study with the Herbst appliance, reported that the stimulation of mandibular growth in the young adult group was probably due to reactivation of the cells in the chondroblastic region [62]. Uematsu et al. (2002) found a significant increase in the ramus length in both growing and mature patients after 6–8 months of treatment with the conventional activator appliance [59], consistent with the present study. Similarly, McNamara (1985) found that the Frankel appliance resulted in an average increase of 1.2 mm per year in mandibular growth [53]. Cozza et al. (2006) demonstrated that the untreated Class II subjects exhibited significantly lesser improvement in mandibular length when compared with the treated ones (2 mm) [5]. In light of the previous studies and based on our findings, overjet elimination appears to be partly achieved by the skeletal response of the mandible. The remaining part of the correction of the increased overjet was provided by the dentoalveolar compensation with retrusion of the upper incisors and protrusion of the lower incisors. In the present study, more than two-thirds of the overjet correction were skeletal and less than one-third were dental. The results were consistent with previous studies [32,60,61]. Interestingly, the skeletal contribution was greater than the dental contribution in the post-adolescent growth period, with a higher rate of correction than the expected value. The amount of skeletal changes contributing to the overjet elimination was larger in the adolescent group (76%) than in the post-adolescent group (66%). One of the important reasons for this favorable outcome may be good compliance of the patients by considering orthognathic surgical therapy as a possible alternative treatment to functional orthopedics. Another reason may be the nighttime and (partly) the daytime use of the appliance (16–18 hours/day) in the present study. The treatment duration for mandibular advancement was significantly longer (10.12±0.99 months) in the post-adolescent group when compared with the adolescent group (7.33±2.02 months). This difference may have resulted from slower condylar adaptation to the new mandibular position in the late growth period.
Conventional activators have been typically associated with maxillary and mandibular molar extrusion. Although the vertical eruption of maxillary teeth is impeded by the occlusal acrylic part, the eruption of the mandibular posterior teeth is allowed for occlusal settling. This can result in an unfavorable increase in lower anterior facial height [75]. In the present study, lower facial height was significantly increased in both growth periods, and the increase was statistically similar between the groups. However, the Jarabak ratio remained stable with an increase in the posterior facial height, demonstrating that primarily translational mandibular growth occurred even in the post-adolescent group. When the rotational change of the mandible (SN-GoGn°) was evaluated, an approximate increase by 1.5° was observed in both groups. This increase might be related to the increased lower gonial angle, which was one of the remarkable differences between the 2 growth periods. This increase was more prominent in the adolescent group than in the post-adolescent group (p<0.05). This increase might be due to an unstable occlusion or the primary contacts after the conventional activator therapy. Although this change was statistically significant, it may be clinically negligible due to the lack of interdigitation immediately following the conventional activator therapy.
The change in the mentocervical angle in the present study was notable [79]. It was decreased significantly after the conventional activator therapy and returned to normal values (80–95°). The decrease was statistically significant in both groups following the treatment, and it was more prominent in the adolescent group (p<0.05). The natural head posture might have changed with the mandibular advancement.
All patients showed an improved soft tissue profile with significantly increased convexity angles based on lateral cephalometric radiographic and three-dimensional photogrammetric analyses. Lip balance was achieved with the conventional activator therapy in both groups. Some of the previous studies in late growth subjects have also reported that the soft tissue convexity and the total facial convexity angles were significantly increased by the Bionator and the Herbst appliance [30,55,80]. Decreased upper lip projection and increased lower lip projection were reported by Remmer et al. (1985), Almeida et al. (2004), and Cozza et al. (2004) [66,81,82]. Other three-dimensional photogrammetric measurements showed certain favorable results in the post-adolescent group as well. The labiomental angle showed a statistically significant increase in lateral cephalometric radiographic and three-dimensional photogrammetric analyses in both groups. Varlık et al. (2008) reported that the labiomental angle was increased by the twin block and the conventional activator therapies due to relaxation of the lower lip with the decrease of overjet [83]. Another reason for this finding may be a reduction in the depth of labiomental sulcus following twin block therapy, as reported by Singh and Clark (2003) [84]. Labiomental sulcus depth, which exhibited higher values before the treatment, showed a statistically significant decrease after treatment. Total lip volume was slightly decreased in both groups (0.29±0.39 cm3 and 0.36±0.22 cm3 in the adolescent and the post-adolescent groups, respectively). Although the change was statistically significant, it may be negligible clinically. The overjet elimination, the increase of lip closure in the resting position, the decrease in the labiomental sulcus depth, the increase of pogonion projection (Pg-VRL), and the increase in the labiomental angle might have caused a decrease in total lip volume. In accordance with the profile convexity, the H angle showed a significant decrease by 2.37° in the adolescent group and by 2.24° in the post-adolescent group. Morris et al. (1998) found a significant decrease in the H Angle with the three-dimensional laser scanning system using the Bass appliance, the Bionator, and the twin block appliances in the adolescent period [85]. Erdem et al. (2009) also reported a similar decrease in the H Angle following treatment with the conventional activator appliance [86]. Mandibular volume was significantly increased in the adolescent group (mean 0.59 cm3) and the post- adolescent group (mean 0.73 cm3). The decreased H Angle might have resulted in the increased mandibular volume. Consequently, the soft tissue convexity, the lip positions, and the mandibular measurements were favorably affected by the conventional activator therapy, even in the late growth period. The conventional activator therapy may be considered as an alternative treatment approach to camouflage therapy or, to a certain extent, to orthognathic surgery in the post-adolescent period. However, the main disadvantage of this type of removable appliance is patient cooperation. Although outcomes of this treatment approach were satisfactory in both growth periods based on these data, it should be kept in mind that the patient cooperation in use of removable appliances tends to decrease in the post- adolescence period and in young adulthood. Further research is needed to compare the removable appliance to fixed orthodontic appliances in treating Class II anomalies in the post-adolescent period to understand the degree of skeletal effects of these appliances. Another limitation of the present study may be the small sample size, and studies with larger sample sizes are needed.
Conclusions
Favorable outcomes were achieved with the conventional activator therapy in patients with Class II mandibular retrognathia in both growth periods. The contribution of the skeletal changes was greater in the adolescent group than in the post-adolescent group. Conventional activator appliance on a short-term basis was found also to be effective to a certain extent for mandibular growth stimulation in patients in late growth period. However, the treatment duration was significantly longer in the post-adolescent group. This study suggests that conventional activator therapy can be an alternative treatment approach in the late growth period, since it induces considerable skeletal changes. Regarding the soft tissue changes, significant increases in the anterior facial height and the nose height were observed in the three-dimensional photogrammetric measurements in both growth groups. These changes were found to be higher in the adolescent group when compared with the post-adolescent group. The total lip volume was significantly reduced following the treatment, while the mandibular volume was significantly increased in all patients. The present study may serve as the basis for future studies on this subject regarding volumetric measurements.
Figures
![The growth indicators used in the hand-wrist radiograph [41,42]: 1. PP2=(Having the same width of in the second proximal phalanx epiphysis and diaphysis), 2. MP3=(Having the same width of in the third proximal phalanx epiphysis and diaphysis), 3. Pisi, H1, R=(Ossification of the pisiform, ossification of the hamular process of the hamatum, having the same width of in the radius epiphysis and diaphysis) 4. Sesamoid, H2 (Ossification of adductor sesamoid, progressive ossification of the hamular process of the hamatum), 5. MP3cap, PP1cap, Rcap (Capping of the diaphysis in the middle phalanx of the third finger by the epiphysis, capping of the diaphysis in the proximal phalanx of the first finger by the epiphysis, capping of the diaphysis in the radius by the epiphysis), 6. DP3u (Union of the third distal phalanx epiphysis and diaphysis), 7. MP3u (Union of the third medial phalanx epiphysis and diaphysis), 8. PP3u (Union of the third proximal phalanx epiphysis and diaphysis), 9. Ru (Union of the radius epiphysis and diaphysis).](https://jours.isi-science.com/imageXml.php?i=medscimonit-26-e921401-g001.jpg&idArt=921401&w=1000) Figure 1. The growth indicators used in the hand-wrist radiograph [41,42]: 1. PP2=(Having the same width of in the second proximal phalanx epiphysis and diaphysis), 2. MP3=(Having the same width of in the third proximal phalanx epiphysis and diaphysis), 3. Pisi, H1, R=(Ossification of the pisiform, ossification of the hamular process of the hamatum, having the same width of in the radius epiphysis and diaphysis) 4. Sesamoid, H2 (Ossification of adductor sesamoid, progressive ossification of the hamular process of the hamatum), 5. MP3cap, PP1cap, Rcap (Capping of the diaphysis in the middle phalanx of the third finger by the epiphysis, capping of the diaphysis in the proximal phalanx of the first finger by the epiphysis, capping of the diaphysis in the radius by the epiphysis), 6. DP3u (Union of the third distal phalanx epiphysis and diaphysis), 7. MP3u (Union of the third medial phalanx epiphysis and diaphysis), 8. PP3u (Union of the third proximal phalanx epiphysis and diaphysis), 9. Ru (Union of the radius epiphysis and diaphysis).
Figure 1. The growth indicators used in the hand-wrist radiograph [41,42]: 1. PP2=(Having the same width of in the second proximal phalanx epiphysis and diaphysis), 2. MP3=(Having the same width of in the third proximal phalanx epiphysis and diaphysis), 3. Pisi, H1, R=(Ossification of the pisiform, ossification of the hamular process of the hamatum, having the same width of in the radius epiphysis and diaphysis) 4. Sesamoid, H2 (Ossification of adductor sesamoid, progressive ossification of the hamular process of the hamatum), 5. MP3cap, PP1cap, Rcap (Capping of the diaphysis in the middle phalanx of the third finger by the epiphysis, capping of the diaphysis in the proximal phalanx of the first finger by the epiphysis, capping of the diaphysis in the radius by the epiphysis), 6. DP3u (Union of the third distal phalanx epiphysis and diaphysis), 7. MP3u (Union of the third medial phalanx epiphysis and diaphysis), 8. PP3u (Union of the third proximal phalanx epiphysis and diaphysis), 9. Ru (Union of the radius epiphysis and diaphysis).  Figure 2. The conventional activator appliance.
Figure 2. The conventional activator appliance. 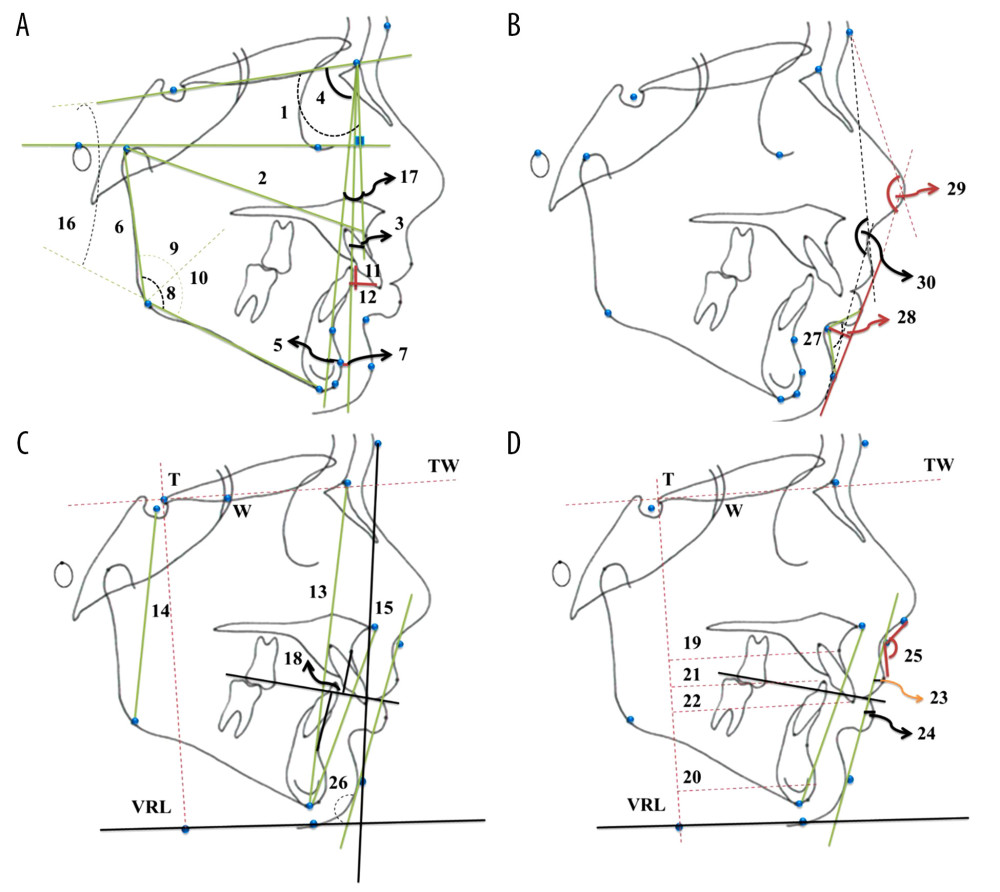 Figure 3. (A–D) Lateral cephalometric radiographic measurements: (A) 1. SNA (°). 2. Co-A (mm). 3. (FH⊥N)-A (mm). 4. SNB (°). 5. Pg-NB (mm). 6. Co-Go (mm). 7. (FH⊥Na)-Pg (mm). 8. Gonial Angle (°). 9. Upper Gonial Angle (°). 10. Lower Gonial Angle (°). 11. Overjet (mm). 12. Overbite (mm). 16. SN-GoGn (°). 17. ANB (°). (B) 27. Labiomental Angle (°). 28. Labiomental Sulcus (mm). 29. Total Facial Convexity Angle (°). 30. Soft Tissue Convexity Angle (°). (C) 13. Anterior Facial Height (AFH) (mm). 14. Posterior Facial Height (PFH) (mm). 15. Lower Anterior Facial Height (LAFH) (mm). 18. Witts (mm). 26. Mentocervical Angle (°). (D) 19. A-VRL (mm). 20. Pg-VRL (mm). 21. L1-VRL (mm). 22. U1-VRL (mm). 23. Upper Lip – S Line (mm). 24. Lower Lip – S Line (mm). 25. Nasolabial Angle (°). (All parameters are defined in Table 2).
Figure 3. (A–D) Lateral cephalometric radiographic measurements: (A) 1. SNA (°). 2. Co-A (mm). 3. (FH⊥N)-A (mm). 4. SNB (°). 5. Pg-NB (mm). 6. Co-Go (mm). 7. (FH⊥Na)-Pg (mm). 8. Gonial Angle (°). 9. Upper Gonial Angle (°). 10. Lower Gonial Angle (°). 11. Overjet (mm). 12. Overbite (mm). 16. SN-GoGn (°). 17. ANB (°). (B) 27. Labiomental Angle (°). 28. Labiomental Sulcus (mm). 29. Total Facial Convexity Angle (°). 30. Soft Tissue Convexity Angle (°). (C) 13. Anterior Facial Height (AFH) (mm). 14. Posterior Facial Height (PFH) (mm). 15. Lower Anterior Facial Height (LAFH) (mm). 18. Witts (mm). 26. Mentocervical Angle (°). (D) 19. A-VRL (mm). 20. Pg-VRL (mm). 21. L1-VRL (mm). 22. U1-VRL (mm). 23. Upper Lip – S Line (mm). 24. Lower Lip – S Line (mm). 25. Nasolabial Angle (°). (All parameters are defined in Table 2). 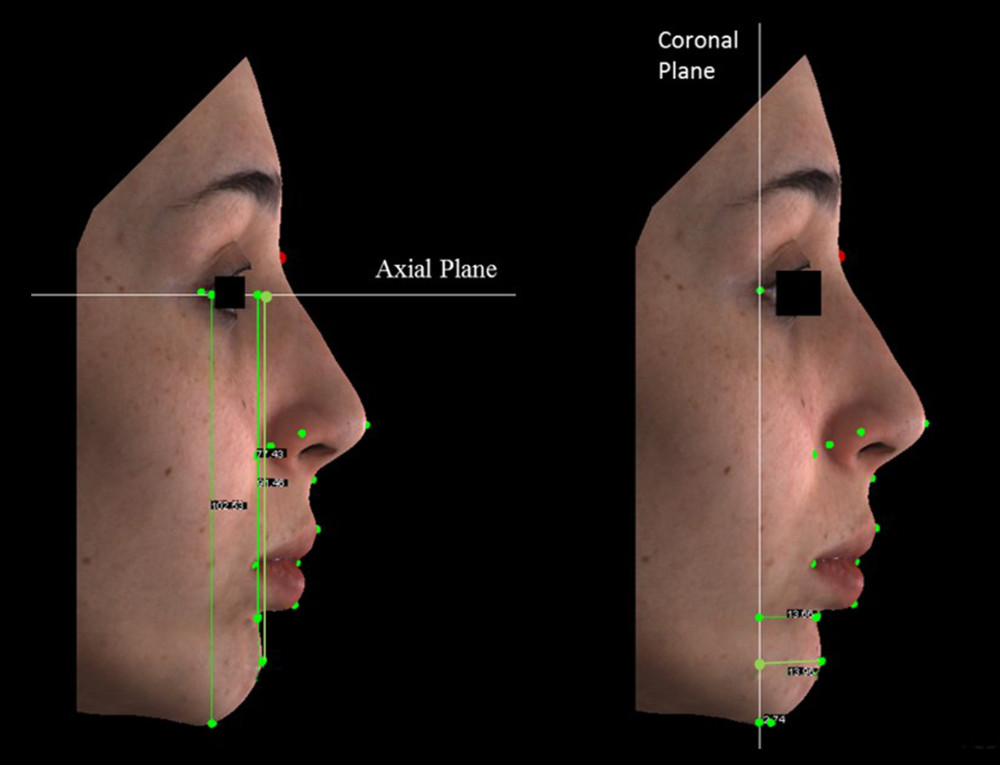 Figure 4. The perpendicular distances of sublabial, pogonion and menton landmarks to coronal and axial plane used in three-dimensional photogrammetric measurements.
Figure 4. The perpendicular distances of sublabial, pogonion and menton landmarks to coronal and axial plane used in three-dimensional photogrammetric measurements. 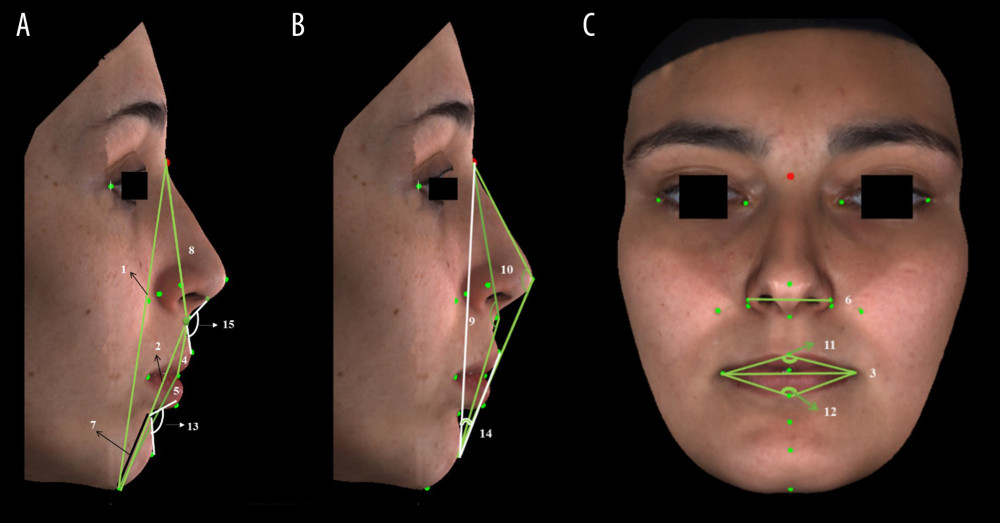 Figure 5. (A–C) Three-dimensional photogrammetric measurements: (A) 1. Anterior Facial Height (mm). 2. Lower Anterior Facial Height (mm). 4. Upper Lip Length (mm). 5. Lower Lip Length (mm). 7. Chin Height (mm). 8. Nose Height (mm). 13. Labiomental Angle (°). 15. Nasolabial Angle (°). (B) 9. Soft Tissue Convexity Angle (°). 10. Total Facial Convexity Angle (°). 14. H Angle (°). (C) 3. Lip Width (mm). 6. Nose Width (mm). 11. Upper Lip Angle (°). 12. Lower Lip Angle (°) (All the parameters are defined in Table 3).
Figure 5. (A–C) Three-dimensional photogrammetric measurements: (A) 1. Anterior Facial Height (mm). 2. Lower Anterior Facial Height (mm). 4. Upper Lip Length (mm). 5. Lower Lip Length (mm). 7. Chin Height (mm). 8. Nose Height (mm). 13. Labiomental Angle (°). 15. Nasolabial Angle (°). (B) 9. Soft Tissue Convexity Angle (°). 10. Total Facial Convexity Angle (°). 14. H Angle (°). (C) 3. Lip Width (mm). 6. Nose Width (mm). 11. Upper Lip Angle (°). 12. Lower Lip Angle (°) (All the parameters are defined in Table 3). 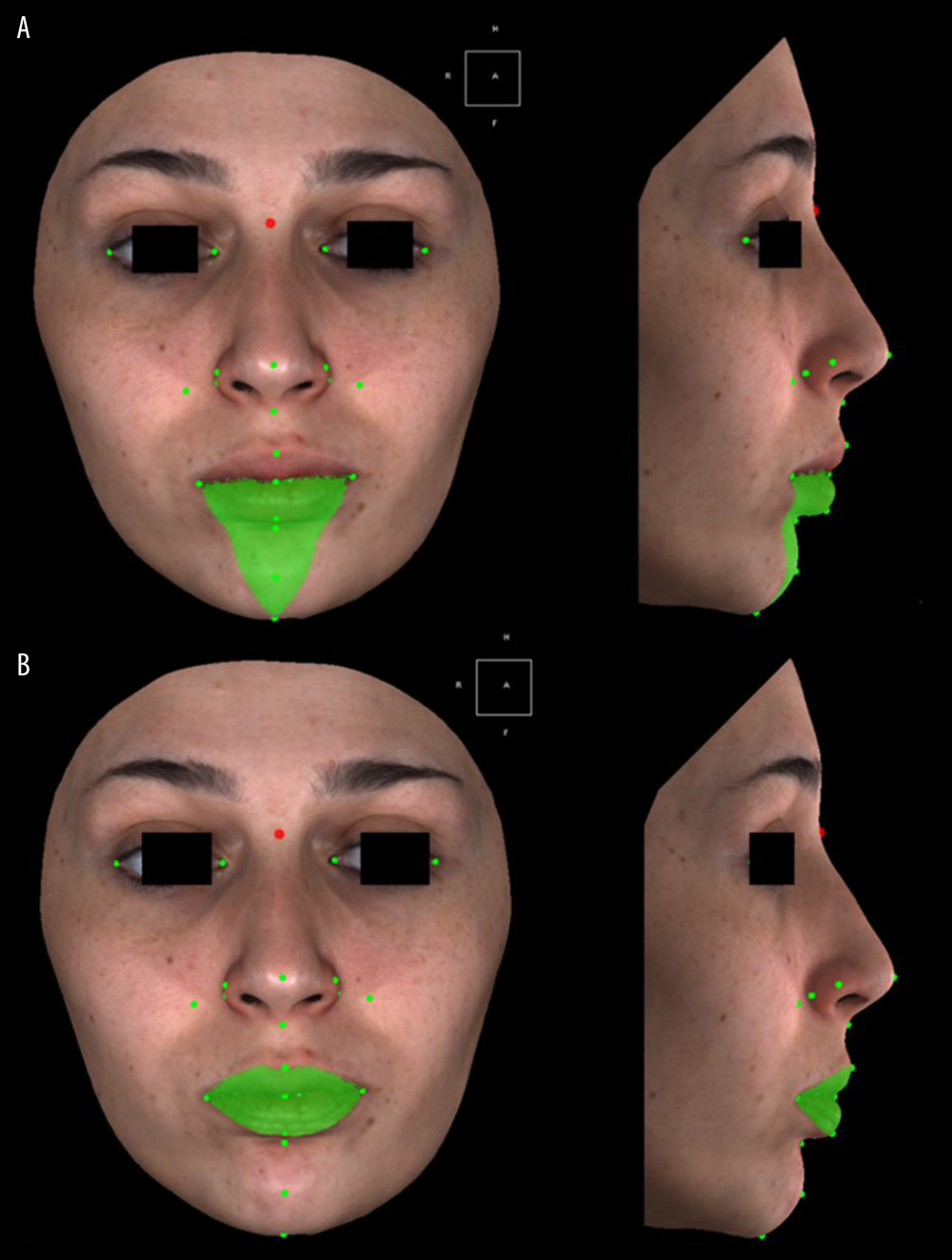 Figure 6. (A, B) Volume measurements used in three-dimensional photogrammetric measurements: (A) Mandibular Volume (cc) (Frontal and profile views). (B) Total Lip Volume (cc) (Frontal and profile views).
Figure 6. (A, B) Volume measurements used in three-dimensional photogrammetric measurements: (A) Mandibular Volume (cc) (Frontal and profile views). (B) Total Lip Volume (cc) (Frontal and profile views). 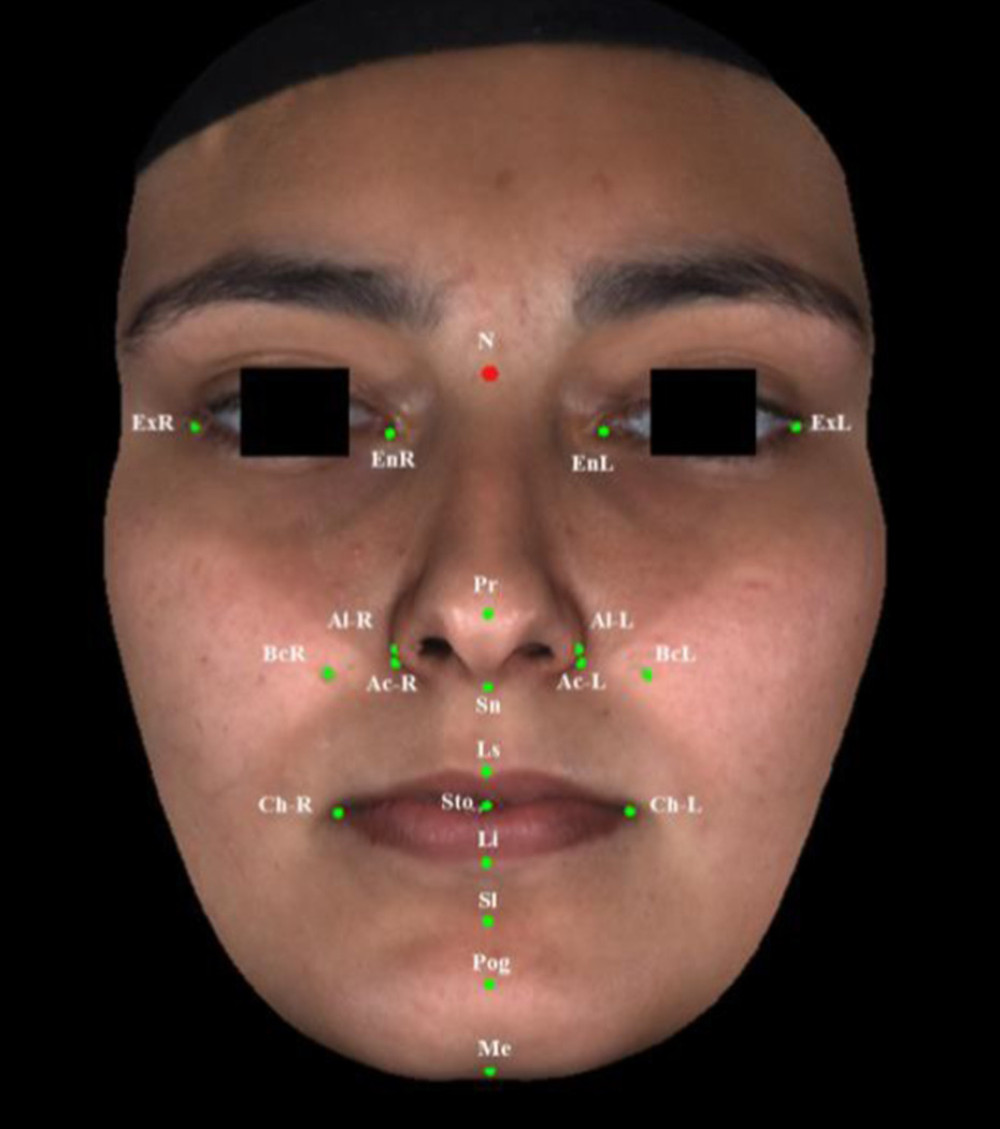 Figure 7. Reference points used in three-dimensional photogrammetric measurements.
Figure 7. Reference points used in three-dimensional photogrammetric measurements. Tables
Table 1. Skeletal growth stages and sex distributions in adolescent and post-adolescent groups.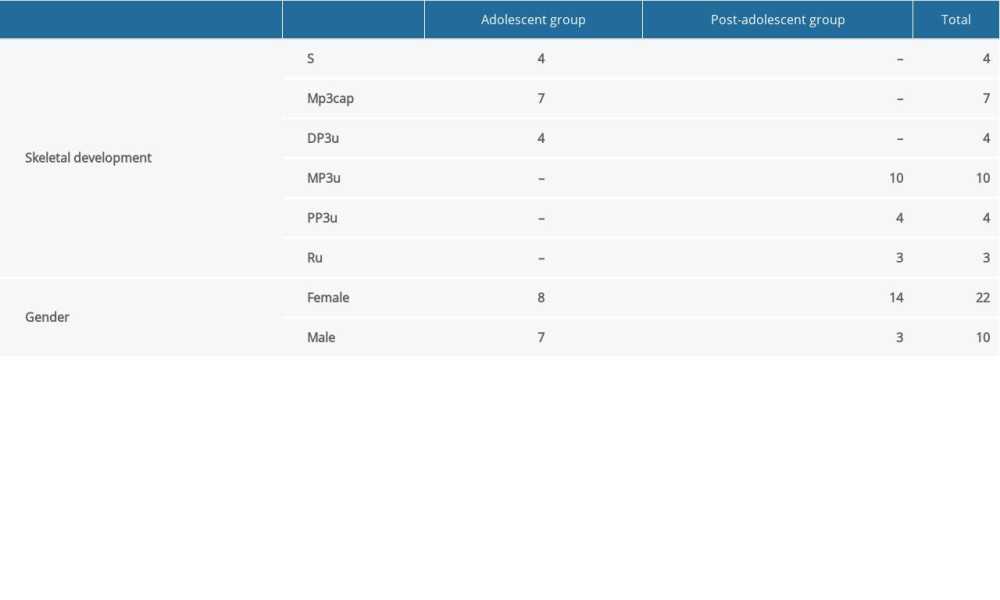 Table 2. Definitions of lateral cephalometric radiographic parameters [43–47].
Table 2. Definitions of lateral cephalometric radiographic parameters [43–47].![Definitions of lateral cephalometric radiographic parameters [43–47].](https://jours.isi-science.com/imageXml.php?i=t2-medscimonit-26-e921401.jpg&idArt=921401&w=1000) Table 3. Definitions of three-dimensional photogrammetric parameters [46,49].
Table 3. Definitions of three-dimensional photogrammetric parameters [46,49].![Definitions of three-dimensional photogrammetric parameters [46,49].](https://jours.isi-science.com/imageXml.php?i=t3-medscimonit-26-e921401.jpg&idArt=921401&w=1000) Table 4. Pre-treatment (T0) and post-treatment (T1) cephalometric mean values and comparisons between the groups.
Table 4. Pre-treatment (T0) and post-treatment (T1) cephalometric mean values and comparisons between the groups.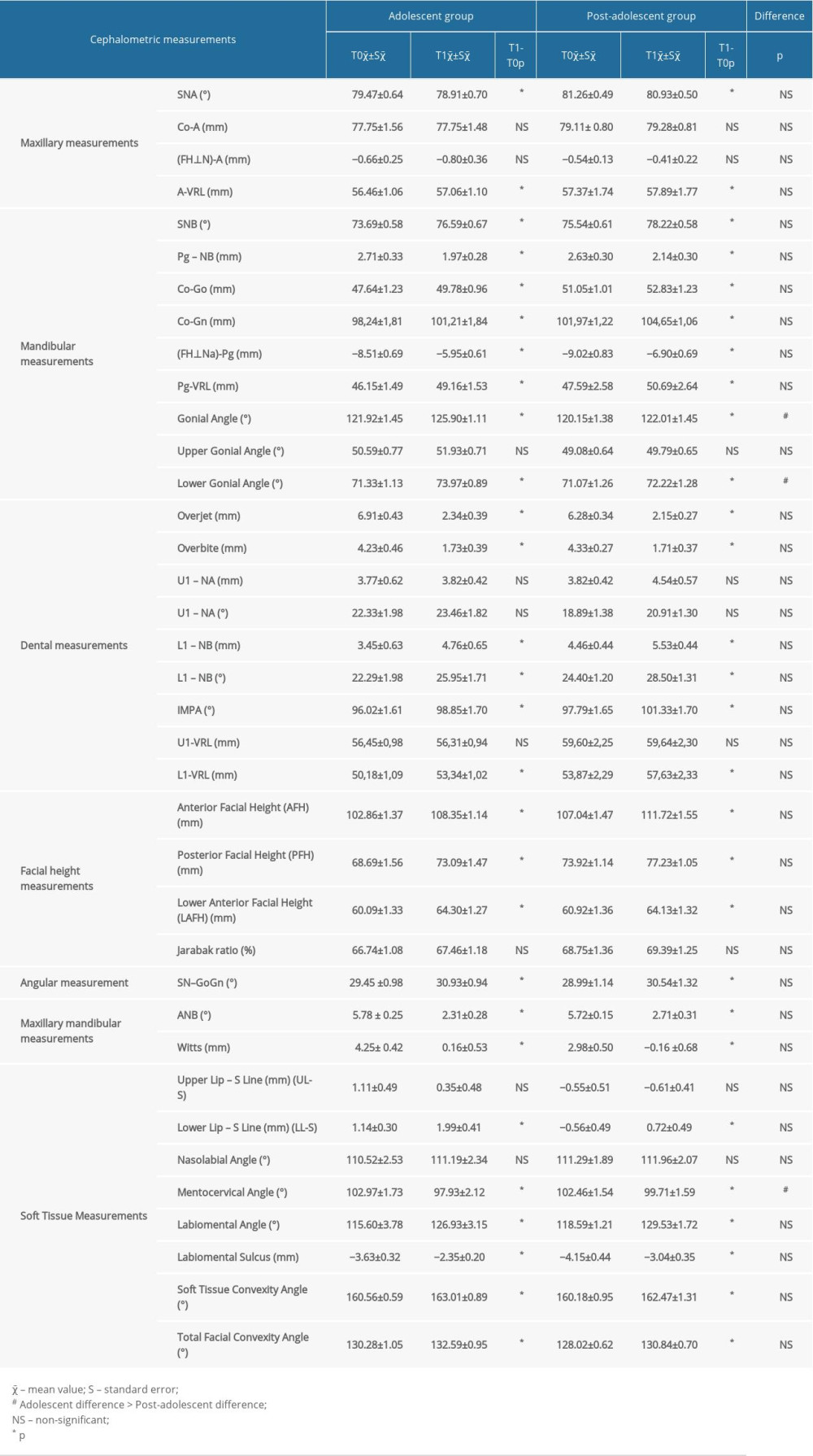 Table 5. Three-dimensional photogrammetry linear, angular and volumetric measurements at T0 and T1 time points and ıntergroup comparisons.
Table 5. Three-dimensional photogrammetry linear, angular and volumetric measurements at T0 and T1 time points and ıntergroup comparisons.
References
1. Proffit WR, Fields HW, Sarver DM: Contemporary orthodontics, 2013; 1-18, St Louis, Mosby
2. Ackerman JL, Nguyen T, Proffit WR, The decision-making process in orthodontics: Orthodontics, Current Principles and Techniques, 2011; 20-48, Philadelphia, Elsevier/Mosby
3. McNamara JA, Components of Class II malocclusion in children 8–10 years of age: Angle Orthod, 1981; 51(3); 177-202
4. Bishara SE, Class II malocclusions: Diagnostic and clinical considerations with and without treatment: Semin Orthod, 2006; 12(1); 11-24
5. Cozza P, Baccetti T, Franchi L, Mandibular changes produced by functional appliances in Class II malocclusion: A systematic review: Am J Orthod Dentofac Orthop, 2006; 129(5); 1-12
6. Ruf S, Baltromejus S, Pancherz H, Effective condylar growth and chin position changes in activator treatment: A cephalometric roentgenographic study: Angle Orthod, 2001; 71(1); 4-11
7. Vargervik K, Harvold EP, Response to activator treatment in Class II malocclusions: Am J Orthod, 1985; 88(3); 242-51
8. Harvold EP, Vargervik K, Morphogenetic response to activator treatment: Am J Orthod, 1971; 60(5); 478-90
9. Righellis E, Treatment effects of Fränkel, activator and extraoral traction appliances: Angle Orthod, 1983; 53(2); 107-21
10. Jakobsson S-O, Paulin G, The influence of activator treatment on skeletal growth in Angle Class II: 1 cases. A roentgenocephalometric study: Eur J Orthod, 1990; 12(2); 174-84
11. Tulley W, The scope and limitations of treatment with the activator: Am J Orthod, 1972; 61(6); 562-77
12. Pancherz H, Long-term effects of activator (Andresen appliance) treatment. A clinical, biometric, cephalometric roentgenographic and functional analysis: Odontol Revy Suppl, 1976; 35; 1-70
13. Forsberg C-M, Odenrick L, Skeletal and soft tissue response to activator treatment: Eur J Orthod, 1981; 3(4); 247-53
14. Williams S, Melsen B, Condylar development and mandibular rotation and displacement during activator treatment: An implant study: Am J Orthod, 1982; 81(4); 322-26
15. Birkebæk L, Melsen B, Terp S, A laminagraphic study of the alterations in the temporo-mandibular joint following activator treatment: Eur J Orthod, 1984; 6(1); 257-66
16. Casutt C, Pancherz H, Gawora M, Ruf S, Success rate and efficiency of activator treatment: Eur J Orthod, 2007; 29(6); 614-21
17. Cesur E, Özdiler O, Köklü A, Effects of wear time differences of removable functional appliances in class II patients: Prospective MRI study of TMJ and masticatory muscle changes: Oral Radiol, 2020; 36(1); 47-59
18. Freunthaller P, Cephalometric observations in Class II, division I malocclusions treated with the activator: Angle Orthod, 1967; 37(1); 18-25
19. Clark W, The twin block technique A functional orthopedic appliance system: Am J Orthod Dentofacial Orthop, 1988; 93(1); 1-18
20. Araujo AM, Buschang PH, Melo ACM, Adaptive condylar growth and mandibular remodelling changes with bionator therapy-an implant study: Eur J Orthod, 2004; 26(5); 515-22
21. de Almeida MR, Henriques JFC, Ursi W, Comparative study of the Fränkel (FR-2) and bionator appliances in the treatment of Class II malocclusion: Am J Orthod Dentofacial Orthop, 2002; 121(5); 458-66
22. Kishnani R, Uppal S, Patel G, Functional appliances: The activator and the functional regulator – a review: Prog Health Sci, 2014; 4(2); 150-56
23. Hirzel HC, Grewe JM, Activators: A practical approach: Am J Orthod, 1914; 66(5); 557-70
24. Björk A, The principle of the Andresen method of orthodontic treatment, a discussion based on cephalometric x-ray analysis of treated cases: Am J Orthod, 1951; 37(6); 437-58
25. Robertson N, An examination of treatment changes in children treated with the function regulator of Fränkel: Am J Orthod, 1983; 83(4); 299-310
26. Chadwick S, Aird J, Taylor P, Bearn D, Functional regulator treatment of Class II division 1 malocclusions: Eur J Orthod, 2001; 23(5); 495-505
27. Baccetti T, Franchi L, Toth LR, McNamara JA, Treatment timing for Twin-block therapy: Am J Orthod Dentofac Orthop, 2000; 118(2); 159-70
28. Baccetti T, Franchi L, McNamara JA, An improved version of the cervical vertebral maturation (CVM) method for the assessment of mandibular growth: Angle Orthod, 2002; 72(4); 316-23
29. Perinetti G, Franchi L, Contardo L, Determination of timing of functional and interceptive orthodontic treatment: A critical approach to growth indicators: J World Fed Orthod, 2017; 6; 93-97
30. Ruf S, Pancherz H, Orthognathic surgery and dentofacial orthopedics in adult Class II Division 1 treatment: Mandibular sagittal split osteotomy versus Herbst appliance: Am J Orthod Dentofac Orthop, 2004; 126(2); 140-52
31. Hägg U, Pancherz H, Dentofacial orthopaedics in relation to chronological age, growth period and skeletal development. An analysis of 72 male patients with Class II division 1 malocclusion treated with the Herbst appliance: Eur J Orthod, 1988; 10(3); 169-76
32. Ruf S, Pancherz H, Dentoskeletal effects and facial profile changes in young adults treated with the Herbst appliance: Angle Orthod, 1999; 69(3); 239-46
33. Ruf S, Baltromejus S, Pancherz H, Effective condylar growth and chin position changes in activator treatment: A cephalometric roentgenographic study: Angle Orthod, 2001; 71(1); 4-11
34. Plooij JM, Maal TJ, Haers P, Digital three-dimensional image fusion processes for planning and evaluating orthodontics and orthognathic surgery. A systematic review: Int J Oral Maxillofac Surg, 2011; 40(4); 341-52
35. Hong C, Choi K, Kachroo Y, Evaluation of the 3dMDface system as a tool for soft tissue analysis: Orthod Craniofac Res, 2017; 20(1); 119-24
36. Mah J, Sachdeva R, Computer-assisted orthodontic treatment: The SureSmile process: Am J Orthod Dentofac Orthop, 2001; 120(1); 85-87
37. Kau CH, Hunter LM, Hingston EJ, A different look: 3-dimensional facial imaging of a child with Binder syndrome: Am J Orthod Dentofac Orthop, 2007; 132(5); 704-9
38. Palomo JM, Hunt DW, Hans MG, Broadbent B, A longitudinal 3-dimensional size and shape comparison of untreated Class I and Class II subjects: Am J Orthod Dentofac Orthop, 2005; 127(5); 584-91
39. Hagg U, Taranger J, Skeletal stages of the hand and wrist as indicators of the pubertal growth spurt: Acta Odontol Scand, 1980; 38; 187-200
40. Fishman LS, Chronological versus skeletal age, an evaluation of craniofacial growth: Angle Orthod, 1979; 49; 181-89
41. Grave KC, Brown T, Skeletal ossification and the adolescent growth spurt: Am J Orthod, 1976; 69(6); 611-19
42. Phulari BS, Maturity Indicators: Orthodontics principles and practice, 2011; 210, New Delhi, JP Medical Ltd
43. English JD, Peltomaki T, Pham-Litschel K: Mosby ’s orthodontic review, 2009; 72-77, St Louis, Mosby
44. Esenlik E, AglarcI C, Albayrak GE, Fındık Y, Maxillary protraction using skeletal anchorage and intermaxillary elastics in Skeletal Class III patients: Korean J Orthod, 2015; 45(2); 95-101
45. Jain SK, Anand C, Ghosh SK, Photometric facial analysis: A baseline study: J Anat Soc India, 2004; 53(2); 11-13
46. Zylinski CG, Nanda RS, Kapila S, Analysis of soft tissue facial profile in white males: Am J Orthod Dentofacial Orthop, 1992; 101; 514-18
47. Ardani GAW, Willyanti I, Narmada IB, Correlation between vertical components and skeletal Class II malocclusion in ethnic Javanese: Clin Cosmet Investig Dent, 2018; 10; 297-302
48. Aldridge K, Boyadjiev SA, Capone GT, Precision and error of three-dimensional phenotypic measures acquired from 3dMD photogrammetric images: Am J Med Genet, 2005; 138; 247-53
49. Swennen GRJ, Three-dimensional cephalometric soft tissue landmarks: Three-dimensional cephalometry A color atlas and manual, 2005; 186-226, Heidelberg, Spinger
50. King GJ, Keeling SD, Hocevar RA, Wheeler TT, The timing of treatment for Class II malocclusions in children: A literature review: Angle Orthod, 1990; 60(2); 87-97
51. Faltin KJ, Faltin RM, Baccetti T, Long-term effectiveness and treatment timing for Bionator therapy: Angle Orthod, 2003; 73(3); 221-30
52. Pancherz H, Hägg U, Dentofacial orthopedics in relation to somatic maturation: An analysis of 70 consecutive cases treated with the Herbst appliance: Am J Orthod, 1985; 88(4); 273-87
53. McNamara JA, Bookstein FL, Shaughnessy TG, Skeletal and dental changes following functional regulator therapy on Class II patients: Am J Orthod, 1985; 88(2); 91-110
54. Malmgren O, Ömblus J, Hägg U, Pancherz H, Treatment with an orthopedic appliance system in relation to treatment intensity and growth periods A study of initial effects: Am J Orthod Dentofac Orthop, 1987; 91(2); 143-51
55. Kinzinger G, Frye L, Diedrich P, Class II treatment in adults: Comparing camouflage orthodontics, dentofacial orthopedics and orthognathic surgery – a cephalometric study to evaluate various therapeutic effects: J Orofac Orthop, 2009; 70(1); 63-91
56. Nalbantgil D, Arun T, Sayinsu K, Işık F, Skeletal, dental and soft-tissue changes induced by the Jasper Jumper appliance in late adolescence: Angle Orthod, 2005; 75(3); 426-36
57. Gianelly AA, Brosnan P, Martignoni M, Bernstein L, Mandibular growth, condyle position and Fränkel appliance therapy: Angle Orthod, 1983; 53(2); 131-42
58. Creekmore TD, Radney LJ, Frankel appliance therapy: Orthopedic or orthodontic?: Am J Orthod, 1983; 83(2); 89-108
59. Uematsu H, Ichida T, Masumi S-I, Diagnostic image analyses of activator treated temporomandibular joint in growth and maturing stages: Cranio, 2002; 20(4); 254-63
60. Ahlgren J, Laurin C, Late results of activator-treatment: A cephalometric study: Br J Orthod, 1976; 3(3); 181-87
61. Basciftci FA, Uysal T, Büyükerkmen A, Sari Z, The effects of activator treatment on the craniofacial structures of Class II division 1 patients: Eur J Orthod, 2003; 25(1); 87-93
62. Ruf S, Pancherz H, Herbst/multibracket appliance treatment of Class II division 1 malocclusions in early and late adulthood. A prospective cephalometric study of consecutively treated subjects: Eur J Orthod, 2006; 28(4); 352-60
63. Wieslander L, Lagerström L, The effect of activator treatment on Class II malocclusions: Am J Orthod, 1979; 75(1); 20-26
64. Gianelly AA, Arena SA, Bernstein L, A comparison of Class II treatment changes noted with the light wire, edgewise and Frankel appliances: Am J Orthod, 1984; 86; 269-76
65. Hiniker JJ, Ramfjord SP, Anterior displacement of the mandible in adult rhesus monkeys: J Prosthet Dent, 1966; 16; 503-12
66. Cozza P, De Toffol L, Colagrossi S, Dentoskeletal effects and facial profile changes during activator therapy: Eur J Orthod, 2004; 26(3); 293-302
67. Tulloch JC, Phillips C, Koch G, Proffit WR, The effect of early intervention on skeletal pattern in Class II malocclusion: A randomized clinical trial: Am J Orthod Dentofac Orthop, 1997; 111(4); 391-400
68. Eirew HL, The bionator: Br J Orthod, 1981; 8(1); 33-36
69. Joho JP: Eur Orthod Soc Rep Congr, 1968; 44; 161-73
70. Toth LR, McNamara JA, Treatment effects produced by the Twin-block appliance and the FR-2 appliance of Fränkel compared with an untreated Class II sample: Am J Orthod Dentofac Orthop, 1999; 116(6); 597-609
71. Meach CL, A cephalometric comparison of bony profile changes in Class II, Division 1 patients treated with extraoral force and functional jaw orthopedics: Am J Orthod, 1966; 52(5); 353-70
72. Alvares JCdC, Cançado RH, Valarelli FP, Class II malocclusion treatment with the Herbst appliance in patients after the growth peak: Dental Press J Orthod, 2013; 18(5); 38-45
73. Foley TF, Mamandras AH, Facial growth in females 14 to 20 years of age: Am J Orthod Dentofac Orthop, 1992; 101(3); 248-54
74. Hunter CJ, The correlation of facial growth with body height and skeletal maturation at adolescence: Angle Orthod, 1966; 36(1); 44-54
75. Bishara SE, Peterson LC, Bishara EC, Changes in facial dimensions and relationships between the ages of 5 and 25 years: Am J Orthod, 1984; 85(3); 238-52
76. Lewis AB, Roche AF, Late growth changes in the craniofacial skeleton: Angle Orthod, 1988; 58(2); 127-35
77. Love R, Murray J, Mamandras A, Facial growth in males 16 to 20 years of age: Am J Orthod Dentofac Orthop, 1990; 97(3); 200-6
78. Björk A, Variations in the growth pattern of the human mandible: Longitudinal radiographic study by the implant method: J Dent Res, 1963; 42(1); 400-11
79. Panfilov DE, The definition of facial beauty: Aesthetic Surgery of the Facial Mosaic, 2007; 43-51
80. Lange DW, Kalra V, Broadbent BH, Changes in soft tissue profile following treatment with the bionator: Angle Orthod, 1995; 65(6); 423-30
81. Remmer KR, Mamandras AH, Hunter WS, Way DC, Cephalometric changes associated with treatment using the activator, the Fränkel appliance, and the fixed appliance: Am J Orthod, 1985; 88(5); 363-72
82. Almeida MR, Henriques JF, Almeida RR, Treatment effects produced by the Bionator appliance. Comparison with an untreated Class II sample: Eur J Orthod, 2004; 26(1); 65-72
83. Varlık SK, Gültan A, Tümer N, Comparison of the effects of Twin Block and activator treatment on the soft tissue profile: Eur J Orthod, 2008; 30(2); 128-34
84. Singh G, Clark W, Soft tissue changes in patients with Class II division 1 malocclusions treated using Twin Block appliances: Finite-element scaling analysis: Eur J Orthod, 2003; 25(3); 225-30
85. Morris DO, Illing HM, Lee RT, A prospective evaluation of Bass, Bionator and Twin Block appliances: Eur J Orthod, 1998; 20(6); 663-84
86. Erdem A, Kilic N, Eroz B, Changes in soft tissue profile and electromyographic activity after activator treatment: Aust Dent J, 2009; 25(2); 116-22
Figures
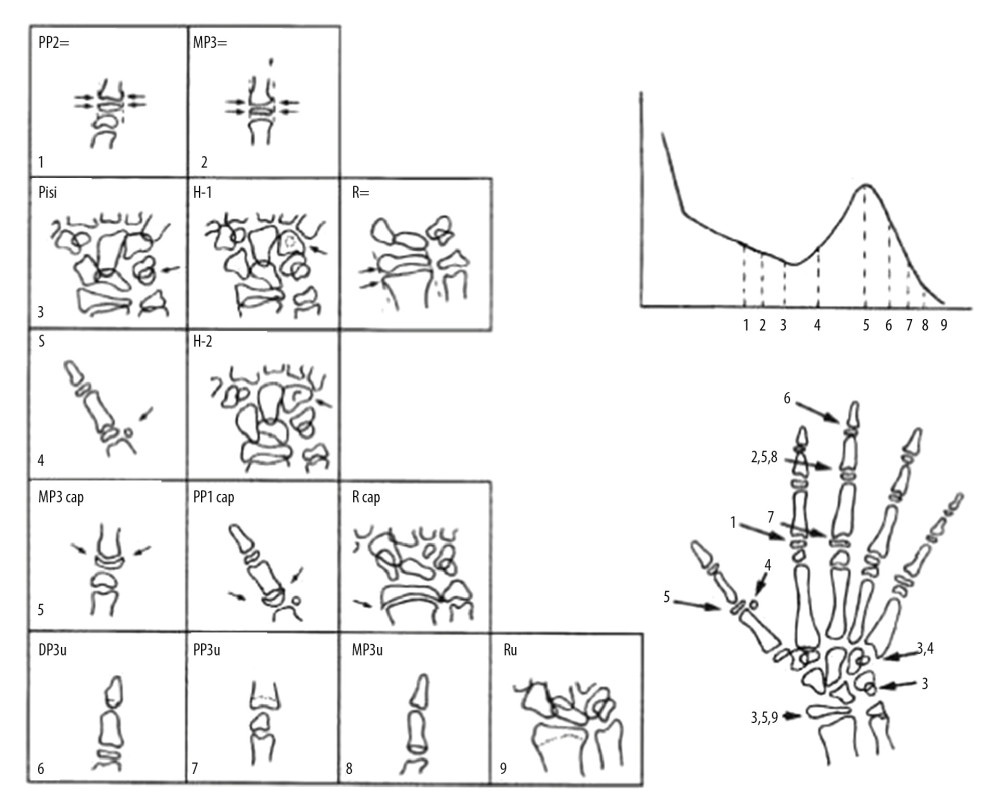 Figure 1. The growth indicators used in the hand-wrist radiograph [41,42]: 1. PP2=(Having the same width of in the second proximal phalanx epiphysis and diaphysis), 2. MP3=(Having the same width of in the third proximal phalanx epiphysis and diaphysis), 3. Pisi, H1, R=(Ossification of the pisiform, ossification of the hamular process of the hamatum, having the same width of in the radius epiphysis and diaphysis) 4. Sesamoid, H2 (Ossification of adductor sesamoid, progressive ossification of the hamular process of the hamatum), 5. MP3cap, PP1cap, Rcap (Capping of the diaphysis in the middle phalanx of the third finger by the epiphysis, capping of the diaphysis in the proximal phalanx of the first finger by the epiphysis, capping of the diaphysis in the radius by the epiphysis), 6. DP3u (Union of the third distal phalanx epiphysis and diaphysis), 7. MP3u (Union of the third medial phalanx epiphysis and diaphysis), 8. PP3u (Union of the third proximal phalanx epiphysis and diaphysis), 9. Ru (Union of the radius epiphysis and diaphysis).
Figure 1. The growth indicators used in the hand-wrist radiograph [41,42]: 1. PP2=(Having the same width of in the second proximal phalanx epiphysis and diaphysis), 2. MP3=(Having the same width of in the third proximal phalanx epiphysis and diaphysis), 3. Pisi, H1, R=(Ossification of the pisiform, ossification of the hamular process of the hamatum, having the same width of in the radius epiphysis and diaphysis) 4. Sesamoid, H2 (Ossification of adductor sesamoid, progressive ossification of the hamular process of the hamatum), 5. MP3cap, PP1cap, Rcap (Capping of the diaphysis in the middle phalanx of the third finger by the epiphysis, capping of the diaphysis in the proximal phalanx of the first finger by the epiphysis, capping of the diaphysis in the radius by the epiphysis), 6. DP3u (Union of the third distal phalanx epiphysis and diaphysis), 7. MP3u (Union of the third medial phalanx epiphysis and diaphysis), 8. PP3u (Union of the third proximal phalanx epiphysis and diaphysis), 9. Ru (Union of the radius epiphysis and diaphysis). Figure 2. The conventional activator appliance.
Figure 2. The conventional activator appliance.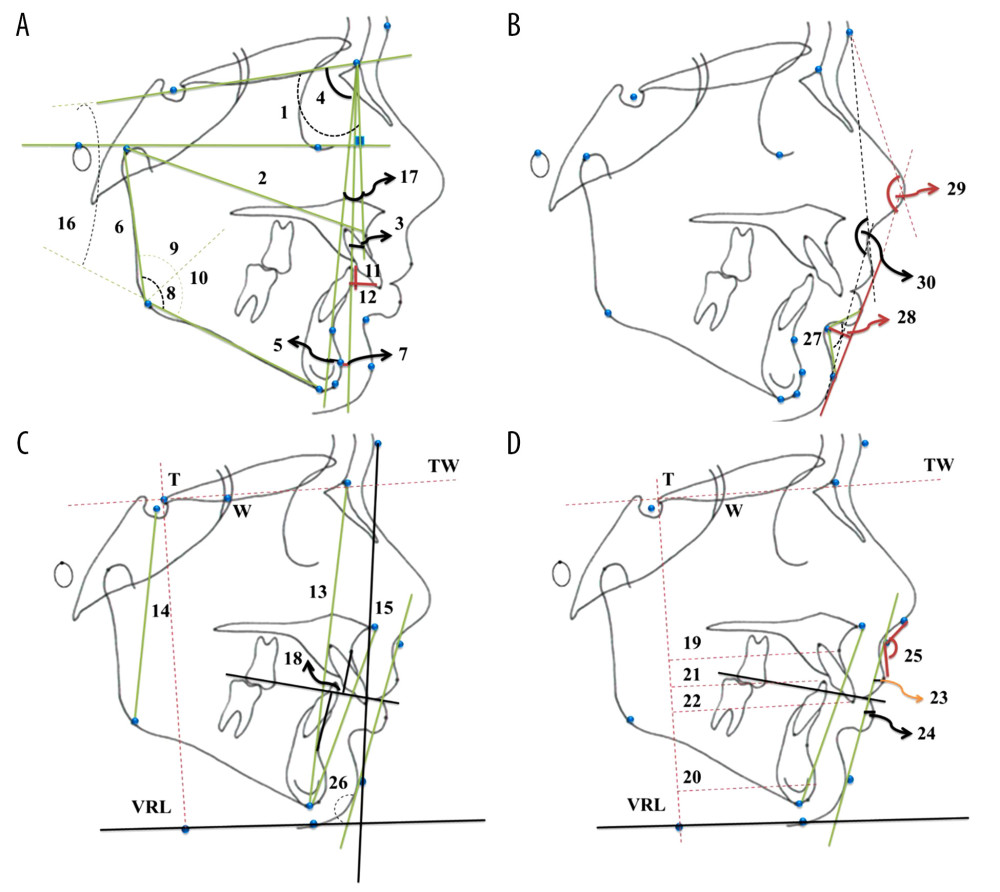 Figure 3. (A–D) Lateral cephalometric radiographic measurements: (A) 1. SNA (°). 2. Co-A (mm). 3. (FH⊥N)-A (mm). 4. SNB (°). 5. Pg-NB (mm). 6. Co-Go (mm). 7. (FH⊥Na)-Pg (mm). 8. Gonial Angle (°). 9. Upper Gonial Angle (°). 10. Lower Gonial Angle (°). 11. Overjet (mm). 12. Overbite (mm). 16. SN-GoGn (°). 17. ANB (°). (B) 27. Labiomental Angle (°). 28. Labiomental Sulcus (mm). 29. Total Facial Convexity Angle (°). 30. Soft Tissue Convexity Angle (°). (C) 13. Anterior Facial Height (AFH) (mm). 14. Posterior Facial Height (PFH) (mm). 15. Lower Anterior Facial Height (LAFH) (mm). 18. Witts (mm). 26. Mentocervical Angle (°). (D) 19. A-VRL (mm). 20. Pg-VRL (mm). 21. L1-VRL (mm). 22. U1-VRL (mm). 23. Upper Lip – S Line (mm). 24. Lower Lip – S Line (mm). 25. Nasolabial Angle (°). (All parameters are defined in Table 2).
Figure 3. (A–D) Lateral cephalometric radiographic measurements: (A) 1. SNA (°). 2. Co-A (mm). 3. (FH⊥N)-A (mm). 4. SNB (°). 5. Pg-NB (mm). 6. Co-Go (mm). 7. (FH⊥Na)-Pg (mm). 8. Gonial Angle (°). 9. Upper Gonial Angle (°). 10. Lower Gonial Angle (°). 11. Overjet (mm). 12. Overbite (mm). 16. SN-GoGn (°). 17. ANB (°). (B) 27. Labiomental Angle (°). 28. Labiomental Sulcus (mm). 29. Total Facial Convexity Angle (°). 30. Soft Tissue Convexity Angle (°). (C) 13. Anterior Facial Height (AFH) (mm). 14. Posterior Facial Height (PFH) (mm). 15. Lower Anterior Facial Height (LAFH) (mm). 18. Witts (mm). 26. Mentocervical Angle (°). (D) 19. A-VRL (mm). 20. Pg-VRL (mm). 21. L1-VRL (mm). 22. U1-VRL (mm). 23. Upper Lip – S Line (mm). 24. Lower Lip – S Line (mm). 25. Nasolabial Angle (°). (All parameters are defined in Table 2).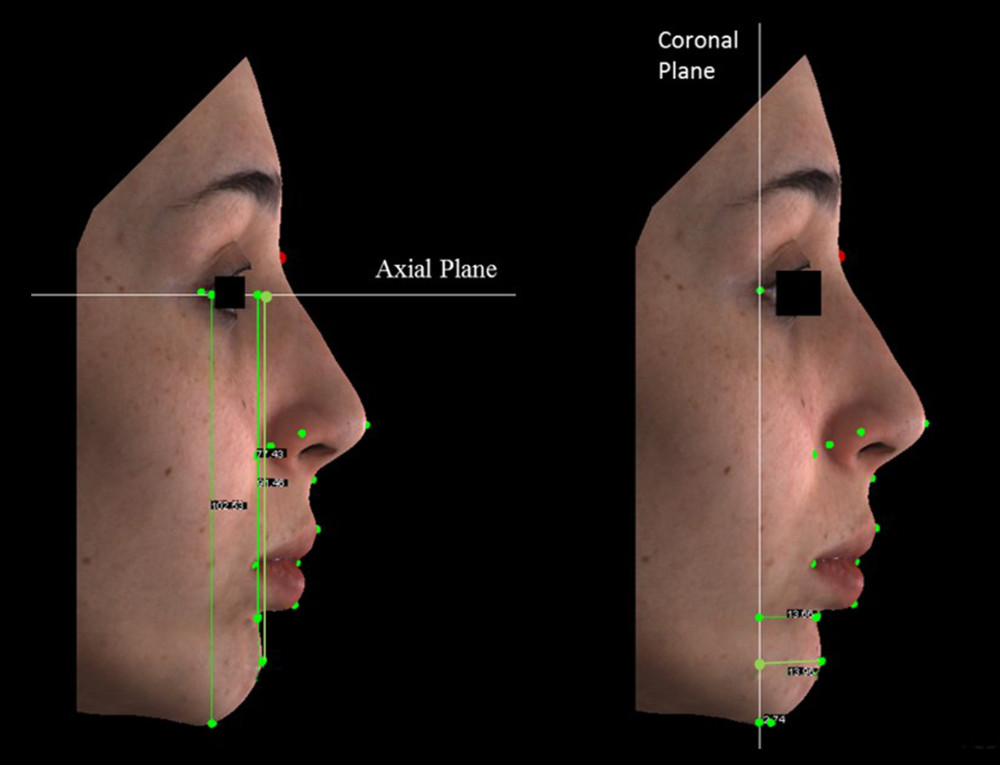 Figure 4. The perpendicular distances of sublabial, pogonion and menton landmarks to coronal and axial plane used in three-dimensional photogrammetric measurements.
Figure 4. The perpendicular distances of sublabial, pogonion and menton landmarks to coronal and axial plane used in three-dimensional photogrammetric measurements.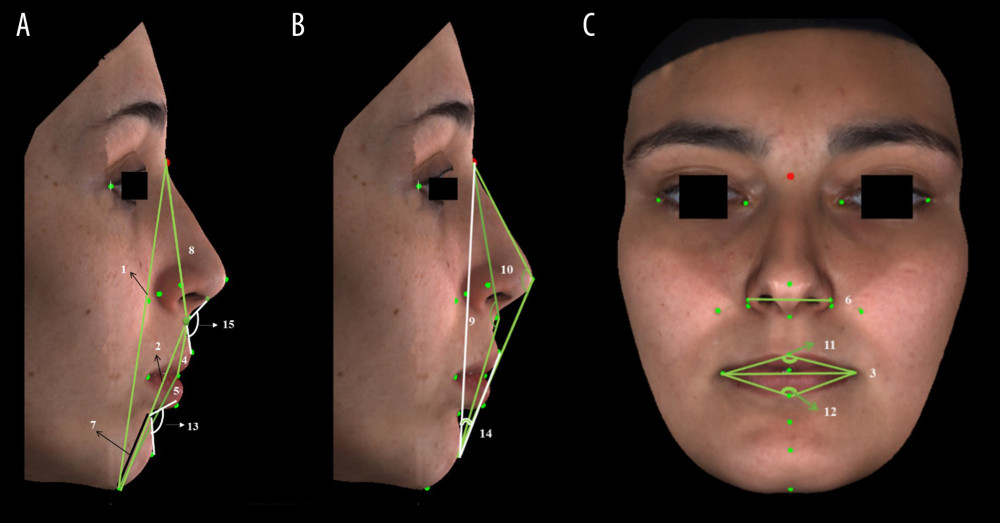 Figure 5. (A–C) Three-dimensional photogrammetric measurements: (A) 1. Anterior Facial Height (mm). 2. Lower Anterior Facial Height (mm). 4. Upper Lip Length (mm). 5. Lower Lip Length (mm). 7. Chin Height (mm). 8. Nose Height (mm). 13. Labiomental Angle (°). 15. Nasolabial Angle (°). (B) 9. Soft Tissue Convexity Angle (°). 10. Total Facial Convexity Angle (°). 14. H Angle (°). (C) 3. Lip Width (mm). 6. Nose Width (mm). 11. Upper Lip Angle (°). 12. Lower Lip Angle (°) (All the parameters are defined in Table 3).
Figure 5. (A–C) Three-dimensional photogrammetric measurements: (A) 1. Anterior Facial Height (mm). 2. Lower Anterior Facial Height (mm). 4. Upper Lip Length (mm). 5. Lower Lip Length (mm). 7. Chin Height (mm). 8. Nose Height (mm). 13. Labiomental Angle (°). 15. Nasolabial Angle (°). (B) 9. Soft Tissue Convexity Angle (°). 10. Total Facial Convexity Angle (°). 14. H Angle (°). (C) 3. Lip Width (mm). 6. Nose Width (mm). 11. Upper Lip Angle (°). 12. Lower Lip Angle (°) (All the parameters are defined in Table 3).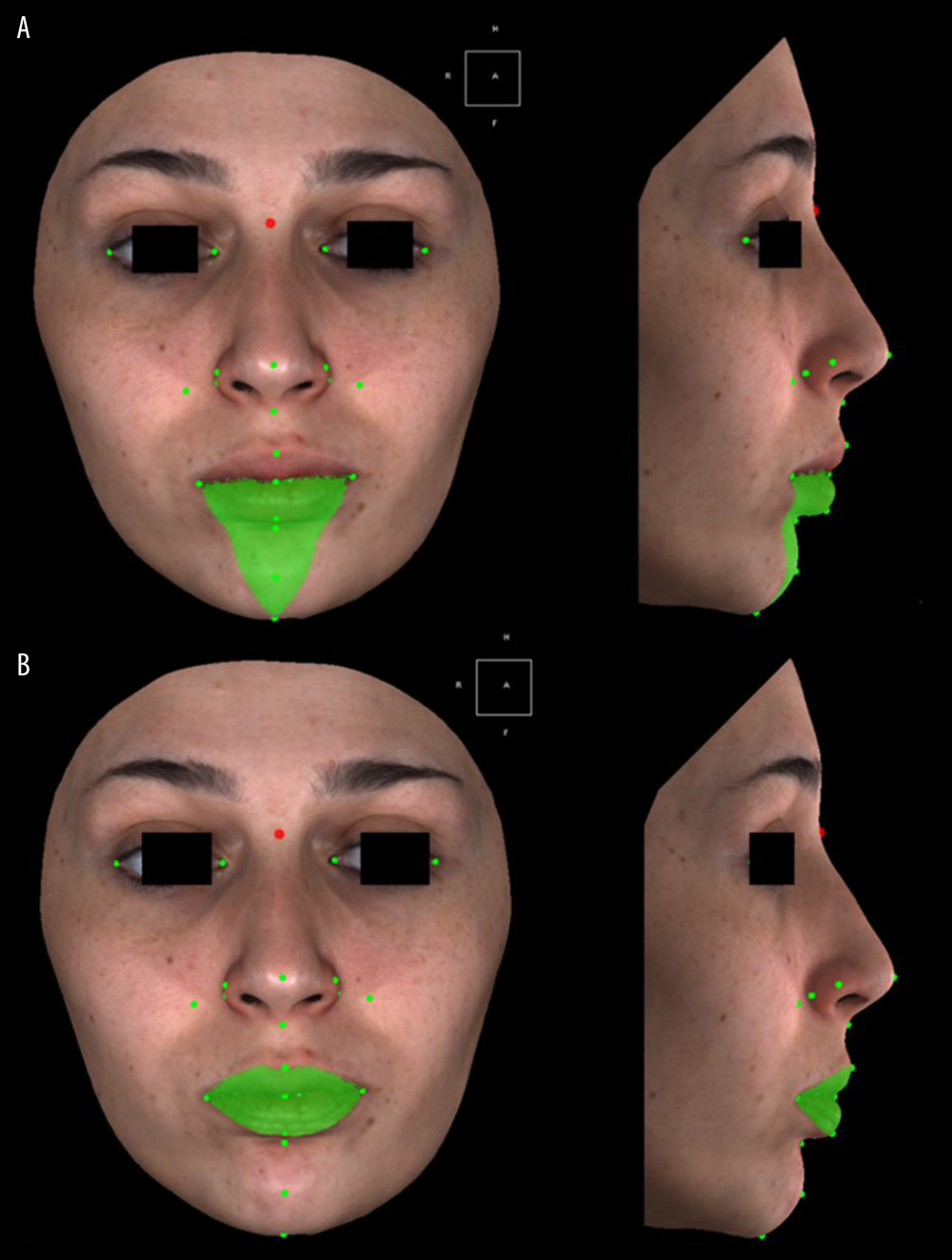 Figure 6. (A, B) Volume measurements used in three-dimensional photogrammetric measurements: (A) Mandibular Volume (cc) (Frontal and profile views). (B) Total Lip Volume (cc) (Frontal and profile views).
Figure 6. (A, B) Volume measurements used in three-dimensional photogrammetric measurements: (A) Mandibular Volume (cc) (Frontal and profile views). (B) Total Lip Volume (cc) (Frontal and profile views).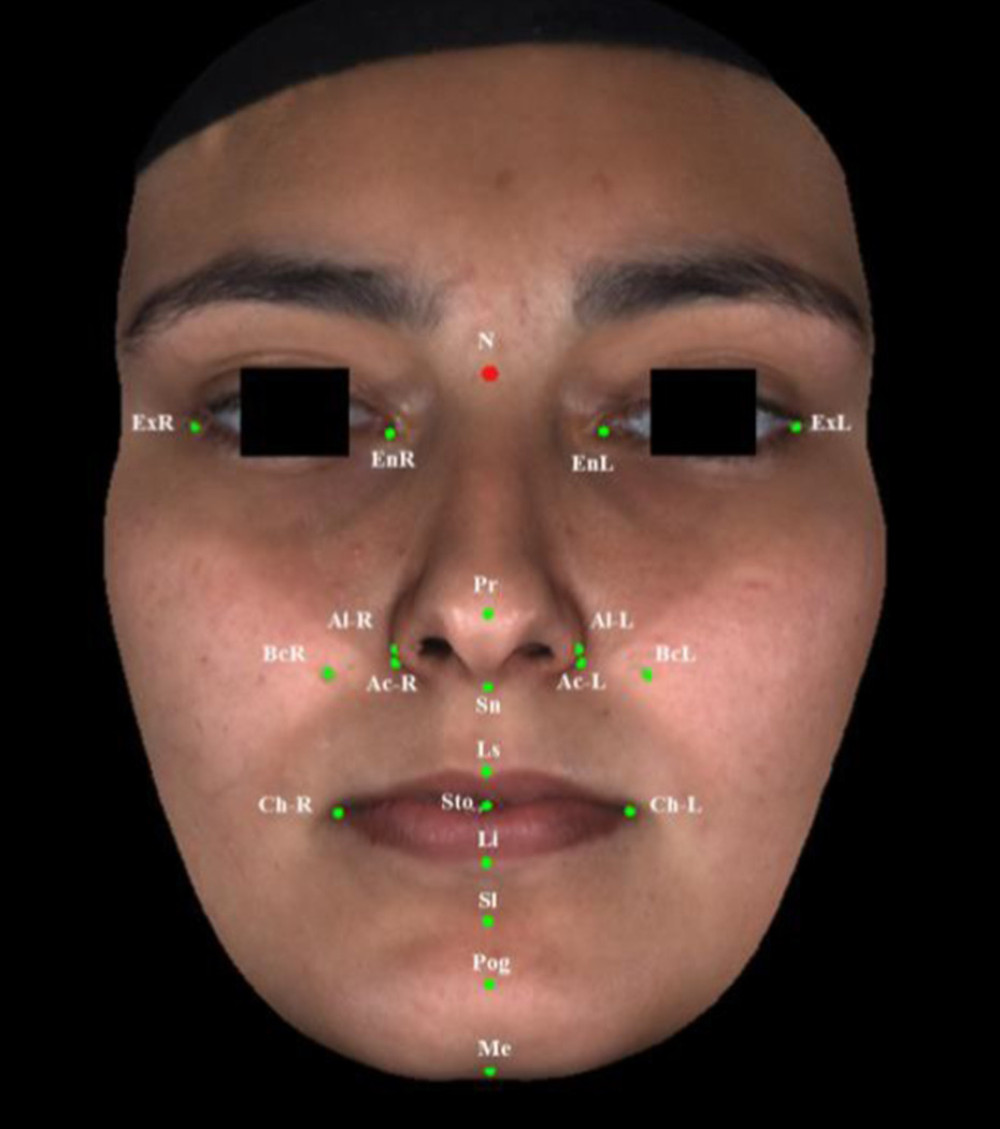 Figure 7. Reference points used in three-dimensional photogrammetric measurements.
Figure 7. Reference points used in three-dimensional photogrammetric measurements. Tables
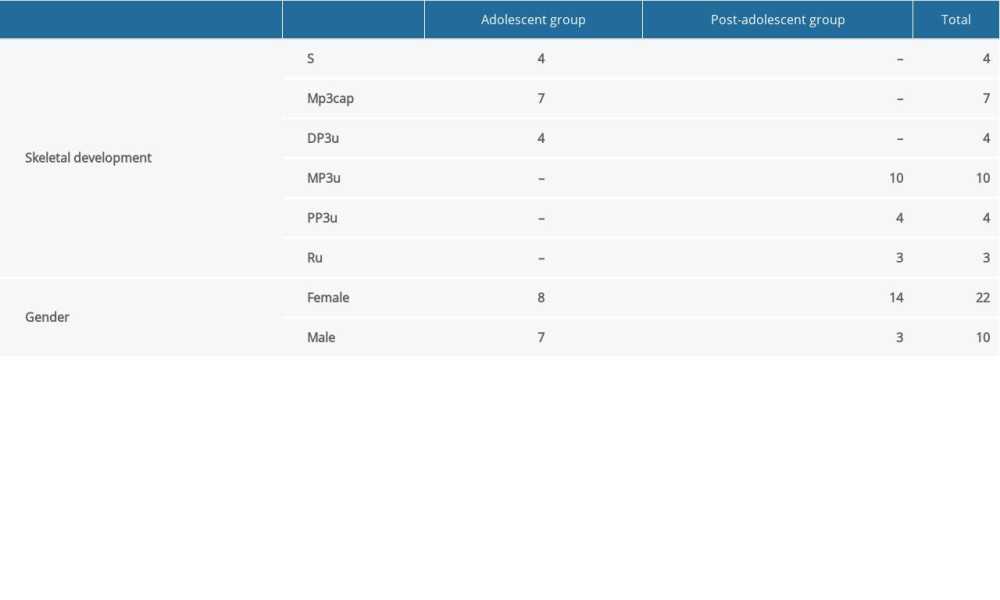 Table 1. Skeletal growth stages and sex distributions in adolescent and post-adolescent groups.
Table 1. Skeletal growth stages and sex distributions in adolescent and post-adolescent groups.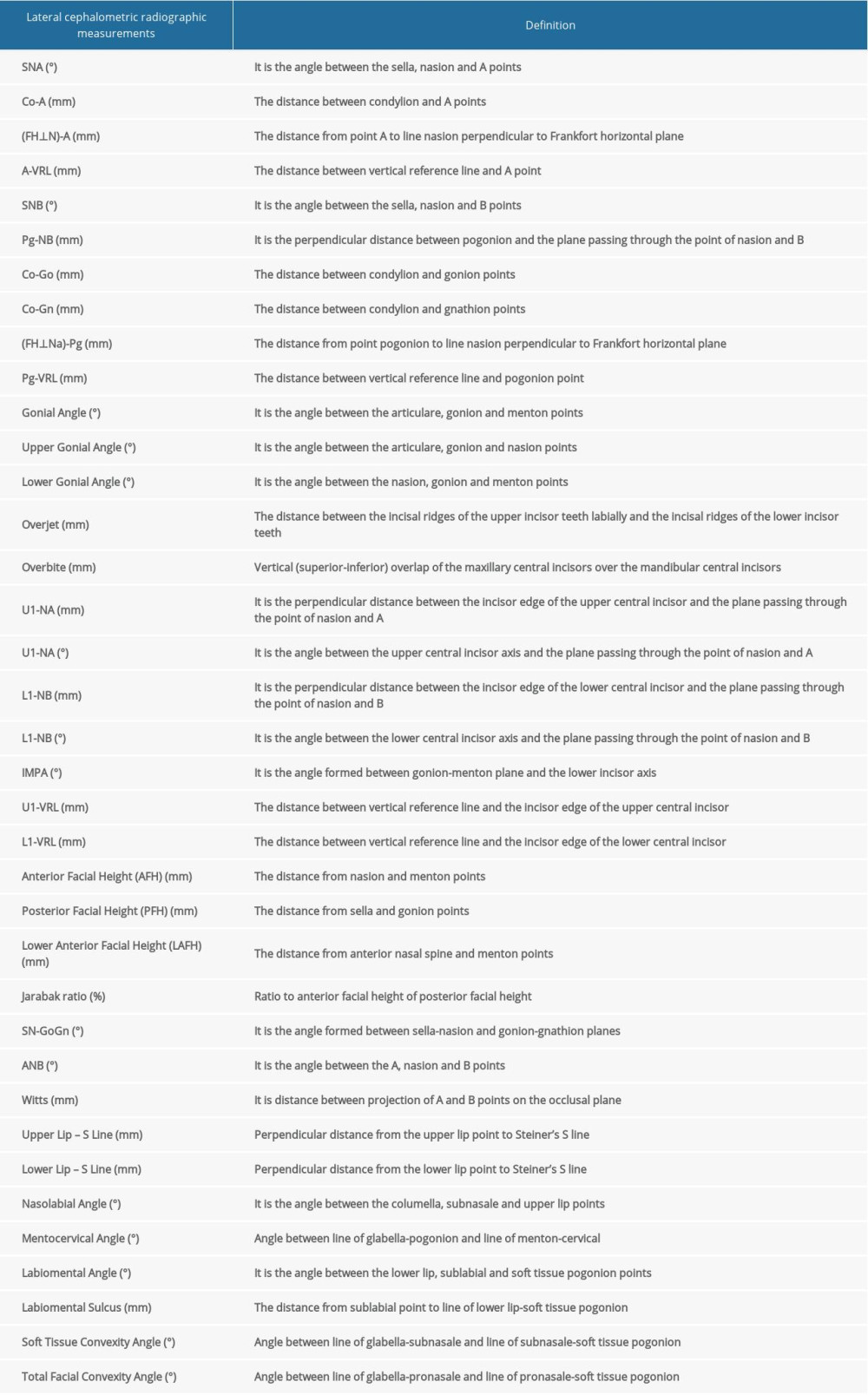 Table 2. Definitions of lateral cephalometric radiographic parameters [43–47].
Table 2. Definitions of lateral cephalometric radiographic parameters [43–47].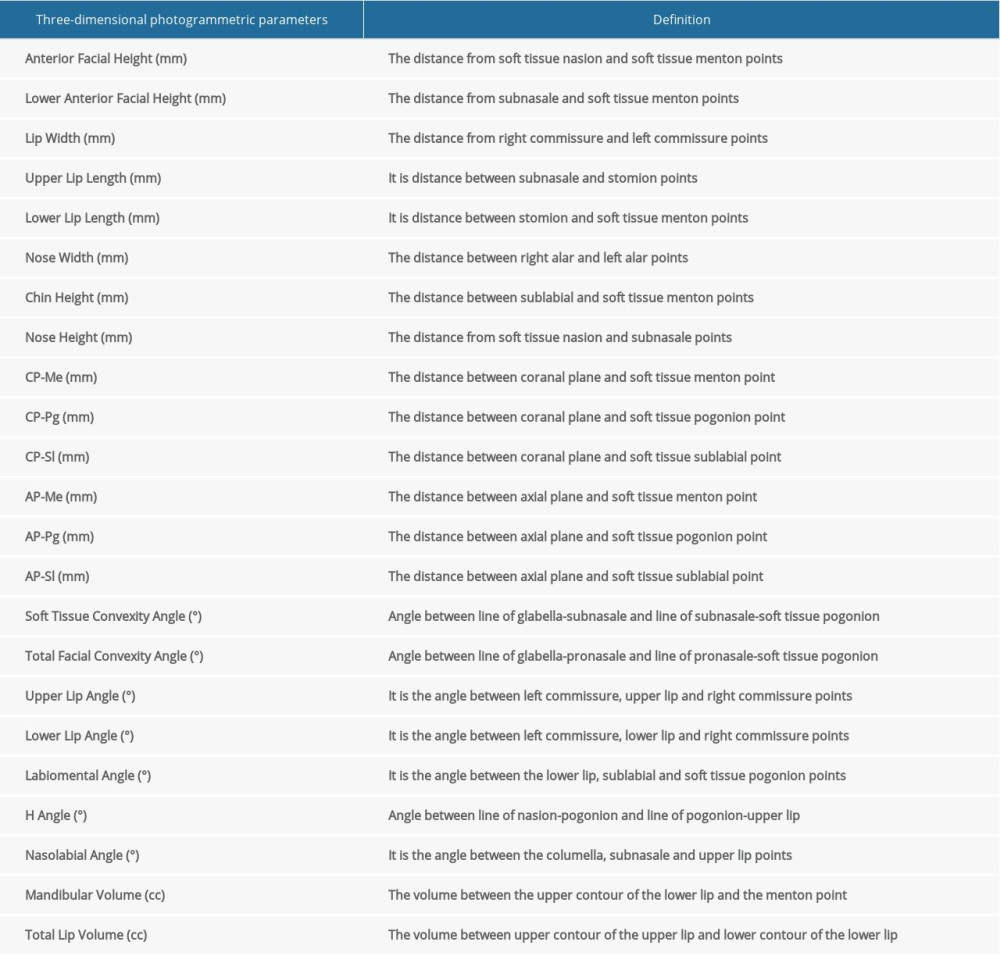 Table 3. Definitions of three-dimensional photogrammetric parameters [46,49].
Table 3. Definitions of three-dimensional photogrammetric parameters [46,49].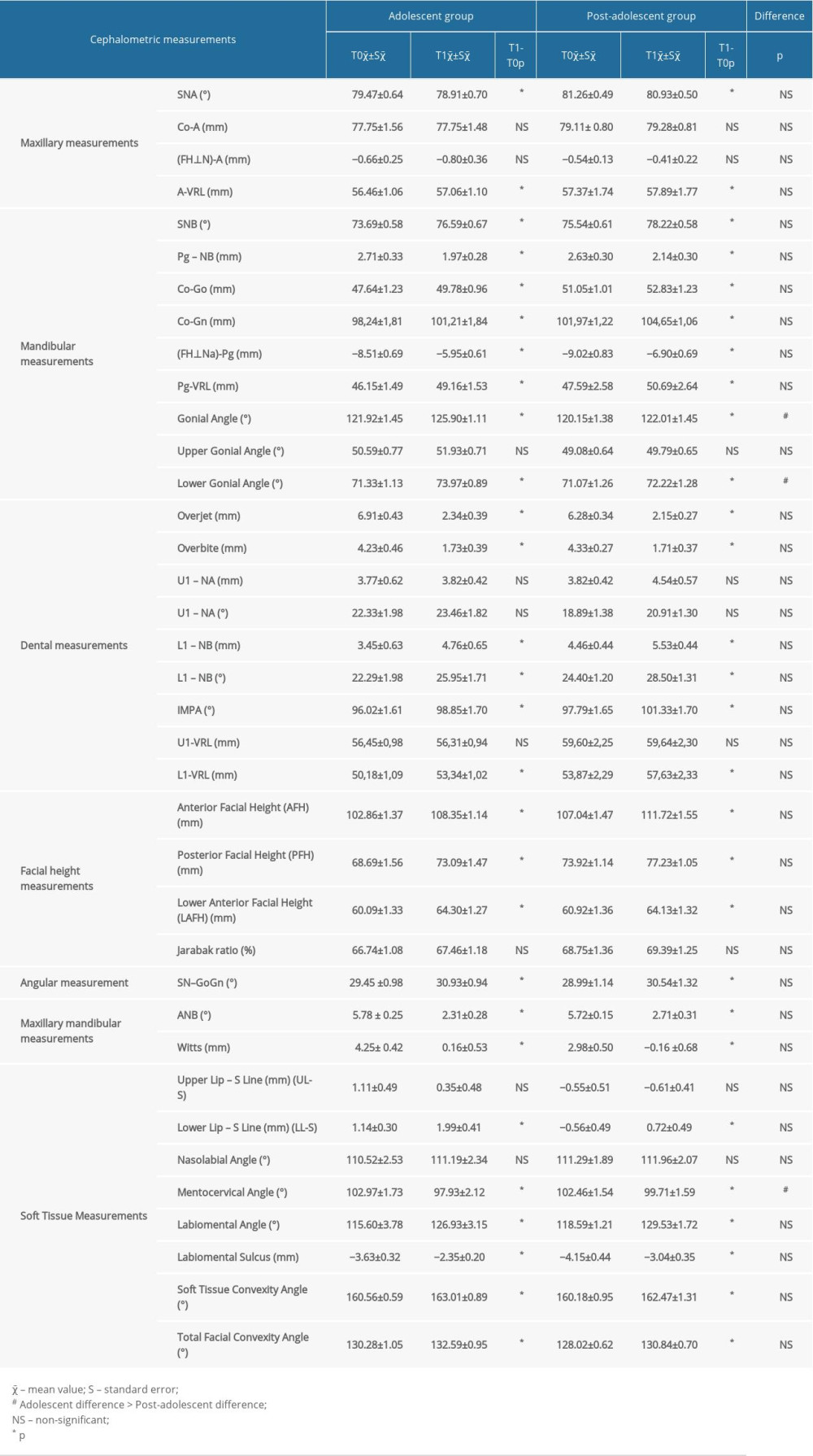 Table 4. Pre-treatment (T0) and post-treatment (T1) cephalometric mean values and comparisons between the groups.
Table 4. Pre-treatment (T0) and post-treatment (T1) cephalometric mean values and comparisons between the groups. Table 5. Three-dimensional photogrammetry linear, angular and volumetric measurements at T0 and T1 time points and ıntergroup comparisons.
Table 5. Three-dimensional photogrammetry linear, angular and volumetric measurements at T0 and T1 time points and ıntergroup comparisons.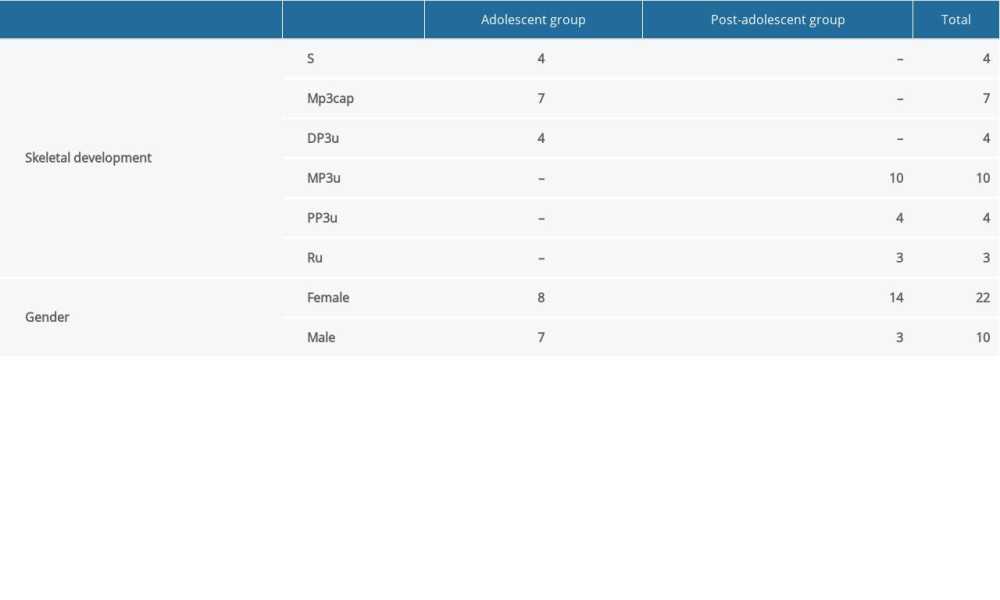 Table 1. Skeletal growth stages and sex distributions in adolescent and post-adolescent groups.
Table 1. Skeletal growth stages and sex distributions in adolescent and post-adolescent groups.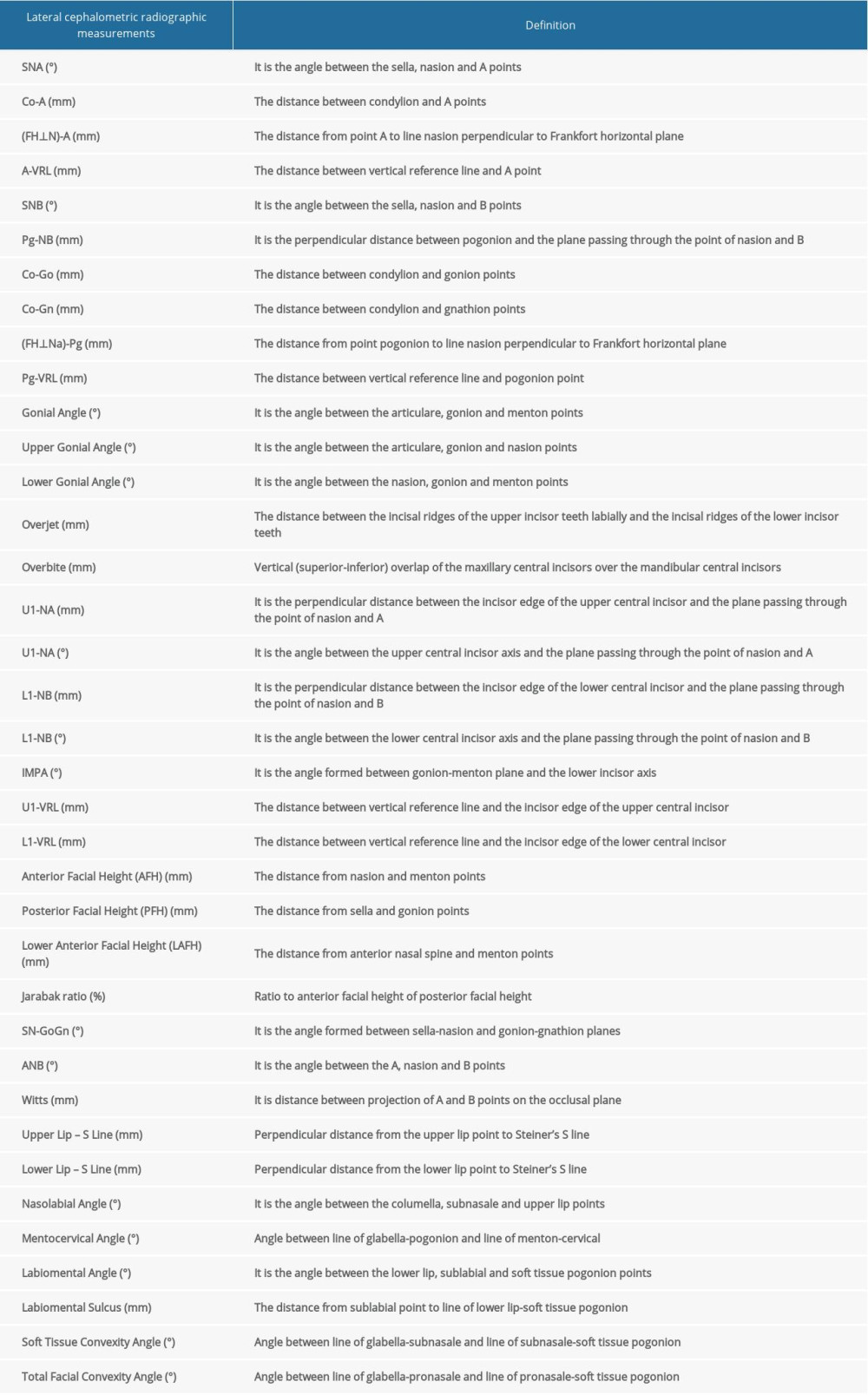 Table 2. Definitions of lateral cephalometric radiographic parameters [43–47].
Table 2. Definitions of lateral cephalometric radiographic parameters [43–47].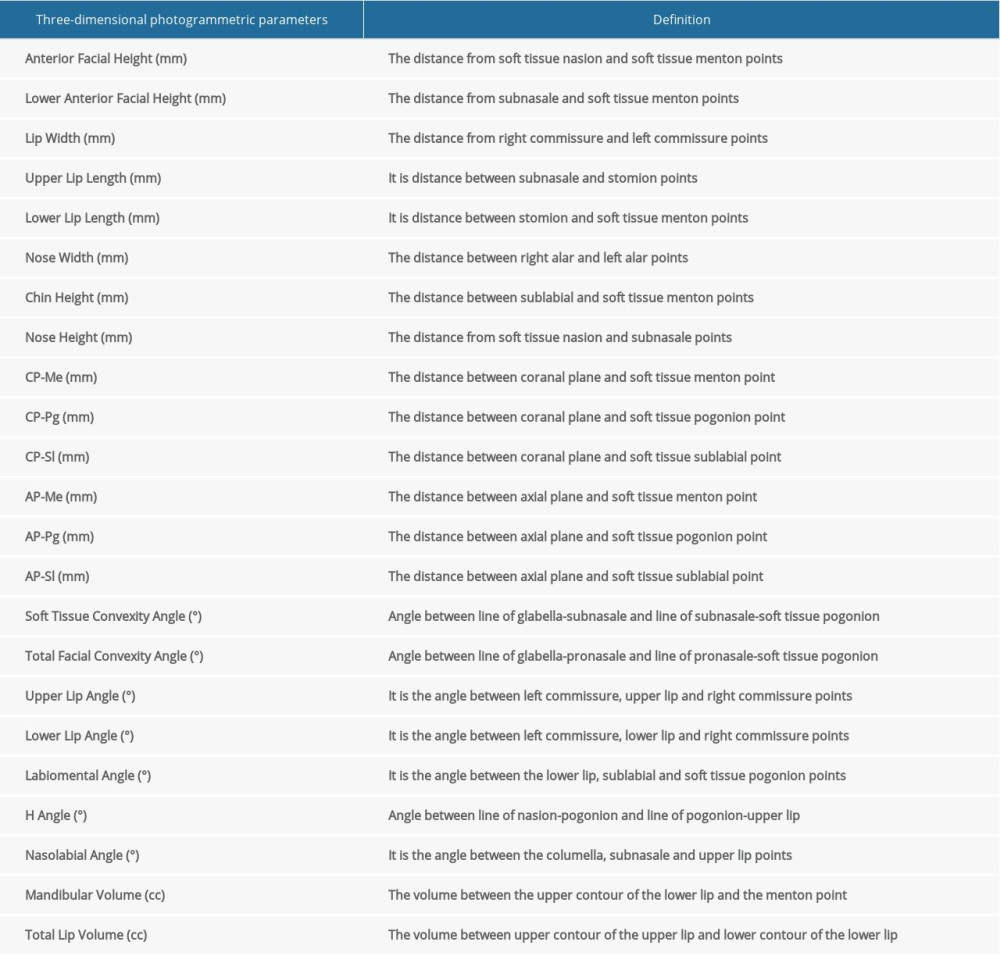 Table 3. Definitions of three-dimensional photogrammetric parameters [46,49].
Table 3. Definitions of three-dimensional photogrammetric parameters [46,49].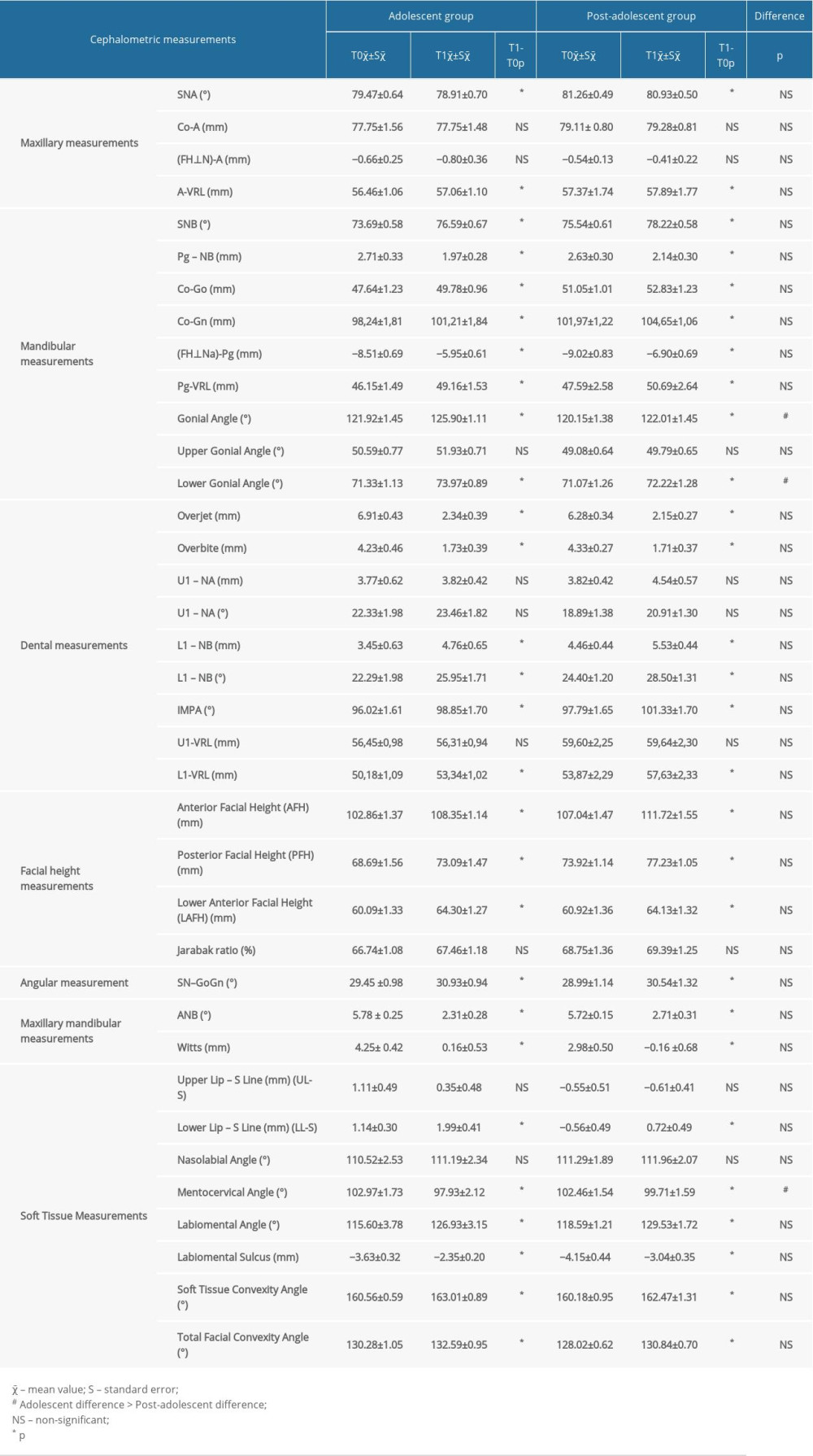 Table 4. Pre-treatment (T0) and post-treatment (T1) cephalometric mean values and comparisons between the groups.
Table 4. Pre-treatment (T0) and post-treatment (T1) cephalometric mean values and comparisons between the groups. Table 5. Three-dimensional photogrammetry linear, angular and volumetric measurements at T0 and T1 time points and ıntergroup comparisons.
Table 5. Three-dimensional photogrammetry linear, angular and volumetric measurements at T0 and T1 time points and ıntergroup comparisons. In Press
06 Mar 2024 : Clinical Research
Comparison of Outcomes between Single-Level and Double-Level Corpectomy in Thoracolumbar Reconstruction: A ...Med Sci Monit In Press; DOI: 10.12659/MSM.943797
21 Mar 2024 : Meta-Analysis
Economic Evaluation of COVID-19 Screening Tests and Surveillance Strategies in Low-Income, Middle-Income, a...Med Sci Monit In Press; DOI: 10.12659/MSM.943863
10 Apr 2024 : Clinical Research
Predicting Acute Cardiovascular Complications in COVID-19: Insights from a Specialized Cardiac Referral Dep...Med Sci Monit In Press; DOI: 10.12659/MSM.942612
06 Mar 2024 : Clinical Research
Enhanced Surgical Outcomes of Popliteal Cyst Excision: A Retrospective Study Comparing Arthroscopic Debride...Med Sci Monit In Press; DOI: 10.12659/MSM.941102
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








