11 February 2024: Review Articles
A Systematic Review of Publications on Perceptions and Management of Chronic Medical Conditions Using Telemedicine Remote Consultations by Primary Healthcare Professionals April 2020 to December 2021 During the COVID-19 Pandemic
Arzaq Ahmed1ABCDEF, Mahdi Mutahar2ADF*, Arwa A. Daghrery3EFG, Nassreen H. Albar3EFG, Ismail Qasem I. Alhadidi4BG, Ali Mohammed Asiri5DG, Nezar Boreak3BFG, Ahmed Audah S. Alshahrani6DG, Mansoor Shariff7CG, Mosa A. Shubayr8CFG, Mohammed M. Al MoaleemDOI: 10.12659/MSM.943383
Med Sci Monit 2024; 30:e943383
Abstract
ABSTRACT: Telemedicine technologies allow distribution of health-related services and information and can include electronic and telecommunication technologies, remote patient and clinician contact, referral and prescribing, patient education, and monitoring. This systematic review aimed to evaluate publications on the perceptions and management of chronic medical conditions using telehealth remote consultations by primary healthcare professionals between April 2020 and December 2021 during the COVID-19 pandemic. Electronic databases, including Cinhal, PubMed, Science Direct, and ProQuest were searched to extract qualitative studies relevant to the topic. Inclusion criteria were developed based on the Population, Exposure, and Outcomes scoping framework. The target population was healthcare professionals working in primary care settings. Included studies encompassed various types of telemedicine, such as synchronous telemedicine, video conferencing, telephone conversations, and smart devices. Eight studies were included. Synchronous telemedicine was highly effective in ensuring the continuity of care and treatment, providing patients with convenience, improved access to treatment, and earlier disease management. Video conferencing and telephone consultations were the most common methods used. Challenges included concerns about patient privacy, technology literacy, and acceptance. Telemedicine was commended for its ability to provide access to immediate expert medical advice and eliminate the need for long-distance travel, contributing to increased patient compliance. Synchronous telemedicine is a promising solution for managing chronic conditions during and after the COVID-19 pandemic, offering benefits to patients and healthcare professionals. To maximize its potential, concerns regarding patient privacy, confidentiality, and technology literacy need to be addressed. Proper legislation and regulations are required for long-term success of telemedicine, making it a valuable component of healthcare systems.
Keywords: Adult Multisystem Inflammatory Disease, COVID-19 Related, Multiple Chronic Conditions, Telemedicine
Background
In the UK, approximately 15 million individuals are affected by 1 or more incurable long-term health conditions. The prevalence of these chronic conditions is increasing due to factors such as an aging population and socioeconomic changes, which contribute to their frequency and costliness. In addition to the challenges posed by chronic conditions, global pandemics like COVID-19 have significantly disrupted healthcare services worldwide. Social distancing measures and the fear of virus transmission have limited in-person interactions with healthcare providers. Telemedicine has played a pivotal role in ensuring the continuity of essential care and treatments.
Chronic conditions are more prevalent among older individuals, with 58% of those over the age of 60 years affected, compared to only 14% of those under age 40. Moreover, individuals from more disadvantaged areas exhibit a 60% higher prevalence compared to those in wealthier social classes, where the incidence of chronic diseases is 30% lower [1,2]. Consequently, long-term care for people with chronic conditions constitutes approximately 70% of overall healthcare spending in England, and these conditions account for 50% of all general practitioner appointments [3]. During the COVID-19 pandemic, the United Kingdom witnessed a significant decrease in face-to-face primary care visits while experiencing a substantial 35% increase in the utilization of telemedicine in 2020, compared to a mere 1.1% rise in 2019 [4]. On the 11 March 2020, the World Health Organization (WHO) declared the COVID-19 outbreak a pandemic. Consequently, healthcare systems worldwide faced disruptions due to social distancing restrictions [5].
Some initial symptoms of COVID-19 include fever, dry cough, breathing difficulties, and, more recently, loss of smell and taste [6]. COVID-19 can be fatal, particularly for elderly individuals or those with underlying health conditions such as severe respiratory problems, hypertension, and diabetes [7]. Therefore, it is crucial for these patients to take precautions to avoid potential exposure to COVID-19. They should also be provided with remote access to medical advice and treatments in lieu of in-person visits, given social distancing guidelines, limited availability of protective equipment, and the prevalent fear of disease transmission [8]. Any disruption in the treatment of vulnerable patient groups could lead to severe complications and a significant decline in their overall health [9].
Telemedicine, also known as telehealth, is the term used for the distribution of health-related services and information and can include electronic information and telecommunication technologies, remote patient and clinician contact, patient management referral and prescribing, advice, patient education, and monitoring [10,11]. While “Telemedicine” is a type of telehealth and is defined as “practicing medicine at a distance” to deliver clinical care only to patients through information technology and electronic communication [11,12]. Telemedicine is documented to be cost-effective [13] and is commonly used in the management of chronic diseases, specialist consultations, follow-ups, and various other clinical services [12]. It can be categorized into 3 basic types: synchronous, asynchronous, and remote patient monitoring [14]. Synchronous or real-time telemedicine involves the individual being simultaneously present for immediate interaction through either telephone or live video conferencing using modern technological devices such as smartphones or webcam-enabled computers [15]. A benefit of synchronous telemedicine is that it allows the patient and their healthcare professional to interact in a way that appears to be as effective as face-to-face, enabling the healthcare professionals to make a comprehensive assessment based on visual clues [11], which is particularly useful in primary and urgent care, follow-up visits, and the management of medications and chronic illnesses [16,17]. Thus, this type tends to be more expensive due to the complexity of video conferencing software [18] requiring a reliable internet connection [19]. Nevertheless, with the advancement of technology, the data from the Office for National Statistics [20] reported that 84% of UK adults over the age of 16 years owned a smartphone in 2020; thus, this population has access to video software allowing patients to benefit from the features of synchronous telemedicine.
The modern form of telemedicine technology was first established in the 1960’s as healthcare delivery when the Nebraska Psychiatry Institute created the first video link to provide medical care treatment across 112 miles and to transmit neurological examination information [21]. They also used closed-circuit TV to facilitate consultations between specialists at a psychiatric institute and general practitioners at a state mental health hospital [14,15]. They set up two-way television transmission to send information to medical students across campus. Live psychiatrists’ interactions with patients were broadcast even though they were not present in the same room. Additionally, expert medical advice was also facilitated from a major teaching hospital to an airport medical center. From 1960 to 1964, NASA pushed for funding to explore ways to provide healthcare to astronauts and enhance telecommunication technology [22]. Initially, NASA scientists were concerned regarding the physiological effects of zero gravity on astronauts, which led to constant monitoring of psychological functions, including heart rate, blood pressure, respiratory rate, and body temperature [23].
Despite existing research focusing on patients’ perspectives on telemedicine, there is a dearth of studies examining primary healthcare professionals’ perceptions. Therefore, this review fills a critical knowledge gap by concentrating on healthcare professionals’ viewpoints and differentiates itself from existing systematic reviews on telemedicine in primary care. It aims to provide insights and guidance for future healthcare interventions [24].
This systematic review explores the perspectives and experiences of primary healthcare professionals regarding the use of synchronous telemedicine for managing chronic conditions during and after the COVID-19 pandemic. It sheds light on the benefits, challenges, and barriers encountered during implementation. Therefore, this systematic review aimed to evaluate publications on the perceptions and management of chronic medical conditions using telehealth remote consultations by primary healthcare professionals between April 2020 and December 2021 during the COVID-19 pandemic.
Review Design
This systematic review was guided by the standards of the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) 2020. The 5-step approach developed by Khan et al in 2003 [25] for conducting a systematic review was used to guide this systematic review to provide a concise structure to the project [26].
Formulating Research Question
Systematic reviews and meta-analysis are considered to be the best evidence for a conclusive response to a research question, but there are some inherent weaknesses associated with them, such as the location and selection of studies, heterogeneity, lack of knowledge on important findings, inappropriate subgroups, and being time-consuming to conduct [27,28]. Bettany-Saltikov and McSherry (2016) reported that use of the Population (Healthcare professionals working in primary care services managing chronic conditions), Exposure (Synchronous telemedicine), and Outcome (Benefits, disadvantages, challenges, and recommendations) framework supports authors in formulating a focused, clear, and manageable research question for qualitative reviews [29]. Therefore, we performed a systematic review of qualitative research addressing primary healthcare professionals’ perceptions and experiences regarding management of chronic illnesses, identifying the benefits, risks, and barriers associated with synchronous telemedicine during and beyond the COVID-19 pandemic.
Keys Terms
The following words and associated synonyms were used alone or in various combinations and keyed in the databases: “telehealth” OR “telemedicine” OR virtual health” OR “remote health” AND “Chronic condition” OR “Long-term diseases” AND “primary care” OR “general practitioner” “perceptions” OR “experience” AND “benefits” OR “advantages” AND “barriers” OR “challenges” AND “covid” OR coronavirus” OR “Pandemic” to help narrow down the searches and extract only focused data to address the research question. Boolean operators “AND”, “OR”, and “NOT” were used to connect and combine relationships between search terms and exclude irrelevant data, resulting in more focused and productive results. Each database consists of their unique symbols and strings such as (“$#*) and restrictions, including language, year, and whether the full text is available online or in journal articles; therefore, the search in each database was adapted accordingly to effectively retrieve results [30]. Restrictions were applied to the “English” language as it is more accessible and easier to interpret, but this may impose a language publication bias due to cultural differences, which may subsequently impact interpretation of the results. Data available from April 2020 to March 2022 were included, extracting only relevant data on COVID-19. Other sources such as Cochrane Database of Systematic Reviews, National Institute for Health and Clinical Excellence (NICE), Joanne and Briggs Institute Database were used to check for relevant data and reviews on the research question.
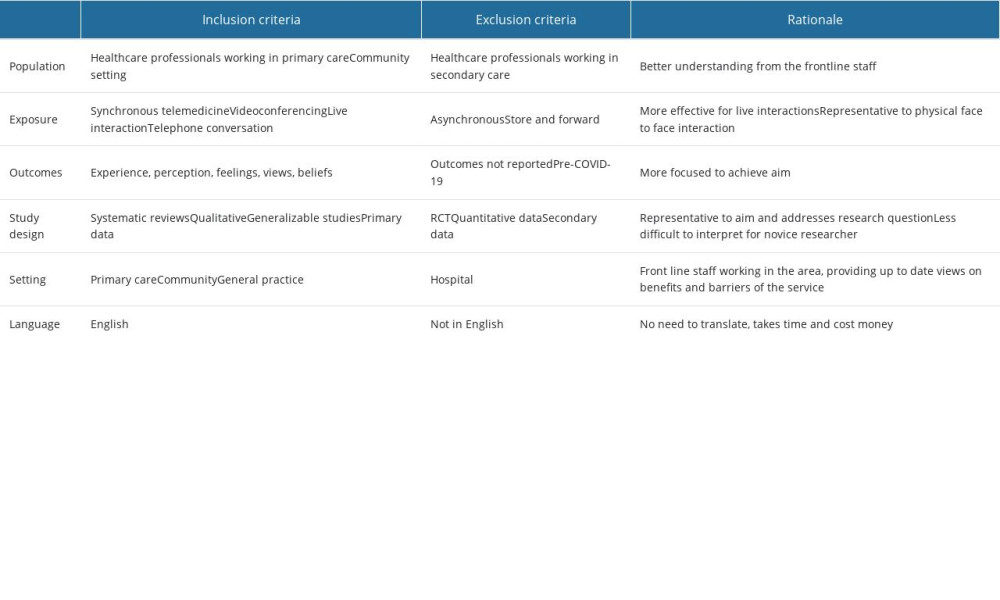
Inclusion and Exclusion Criteria
Inclusion and exclusion criteria for this systematic review were developed based on the Population, Exposure, and Outcome (PEO) scoping framework, in which Population was healthcare professionals working in primary care services managing chronic conditions, Exposure was synchronous telemedicine, and Outcome was benefits, disadvantages, challenges, and recommendations [25,31,32]. However, we intentionally used broad criteria for inclusion, which was based on a scoping review. Because of the research question and the ongoing nature of the pandemic at the time of the study, it was unlikely that a substantial number of empirical studies would be identified, so descriptive papers were also included in the study [33]. Healthcare professionals who were actively working in primary healthcare services, such as doctors, nurses, physiotherapists, and pharmacists, were the target population for this study. The reason this population was chosen is because they served as the primary source of assistance for patients who were greatly affected by the COVID-19 pandemic. Therefore, the population is focused, well-defined, and relevant to current practice. Table 1 shows the inclusion and exclusion criteria and their rational in this review.
The studies encompassed various types of telemedicine that are currently being used in combination and have been proven effective in enabling primary healthcare professionals to conduct remote consultations as a substitute for in-person visits [34]. These types include:
In the systematic review, various qualitative studies were included. These studies focused on exploring the emotions, perspectives, and encounters of primary healthcare professionals in relation to the utilization of synchronous telemedicine to manage patients’ chronic health conditions during the COVID-19 pandemic and beyond. Common qualitative research philosophies and analysis methodologies, such as phenomenological studies, ethnographic studies, grounded theory studies, action studies, and disclosure studies, were included. Qualitative studies that collected data using methods such as interviews, open-ended questionnaires, observations, diaries, and document analysis were also included. Mixed analysis approaches were used in this systematic review, allowing for comprehensive qualitative data analysis [29,35].
Databases Selection and Studies Searching
PRISMA guidelines were followed to structure and report this systematic review, ensuring the avoidance of bias and duplication of included studies. The research question and objectives guided the selection of electronic databases to extract qualitative studies that were relevant and met the eligibility criteria. A brief search was conducted based on titles and abstracts in September 2020 that broadly identified a range of available evidence on telemedicine. Subsequently, a more comprehensive search was conducted in November 2020 for updated results. Based on the research question and objectives, the following electronic databases were used to extract relevant and published and eligible qualitative studies: Cinhal, PubMed, Science Direct, ProQuest, and Summon. According to Boland et al, qualitative research is more comprehensive, thus these databases will facilitate their index to be former than other databases [36]. This was devised using the PEO framework to tailor the searches to the objectives of the research questions [37] and identify studies that met the relevant inclusion and exclusion criteria.
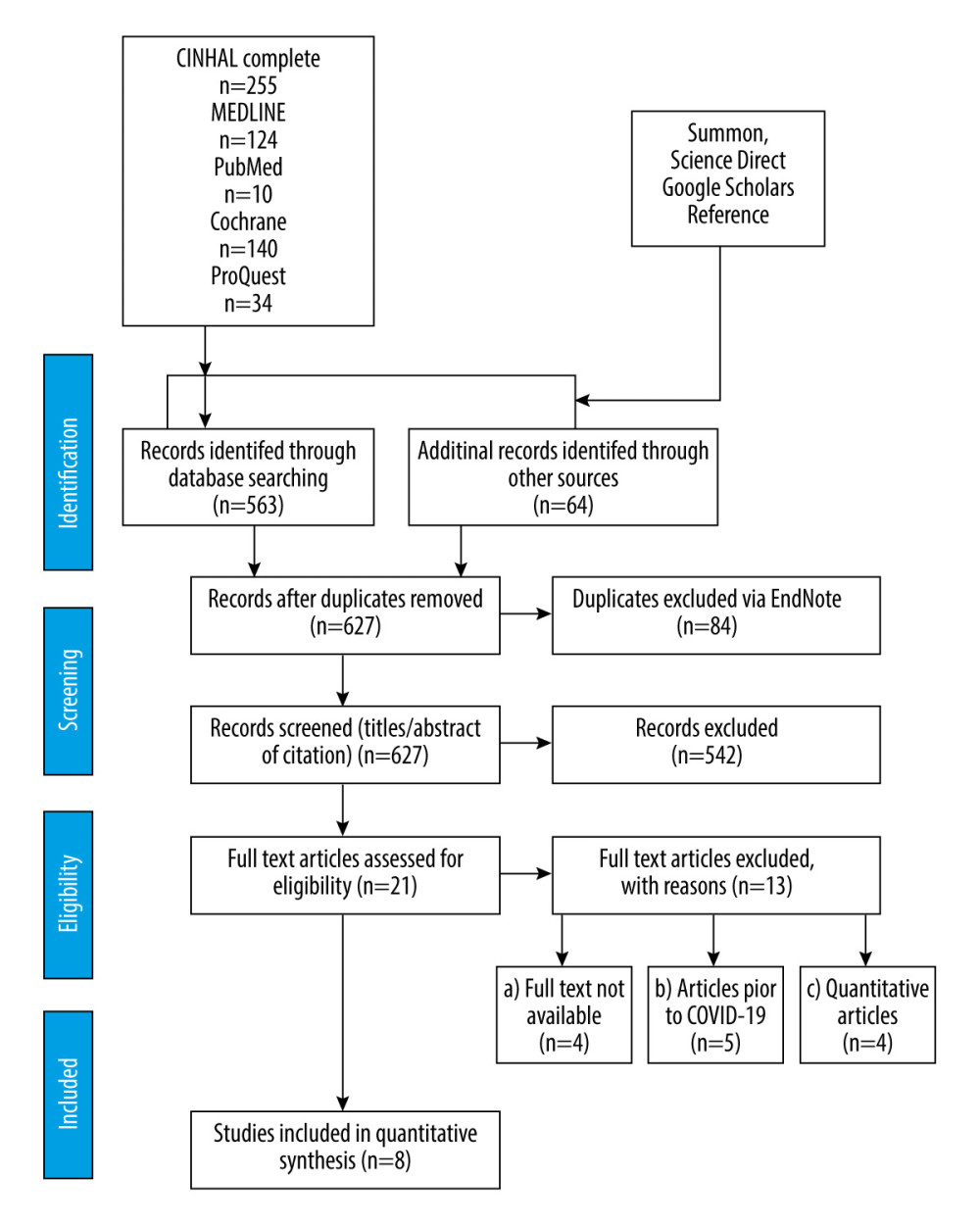
As seen in Figure 1 and from a comprehensive search across 6 databases and online platforms, a total of 627 articles were retrieved. Once duplicates were removed, 563 papers remained, from which 21 articles that met the criteria were successfully retrieved and read in their entirety. A total of 542 submissions were excluded from the screening stage due to problems with the abstract and title. Out of the total of 21 papers, 13 papers had to be excluded due to various reasons, including unavailability of the full text, articles published before the COVID-19 pandemic, and the use of an unsuitable method of data analysis. We finally included 8 papers that met the eligibility criteria. Figure 1 show data extraction process.
Quality Assessment
In qualitative literature, several methods are used to assess the rigor of potential studies and address any methodological issues that may impact the consistency of the study results, including the JBI-QARI and the Critical Appraisal Skills Programme (CASP., 2018) [38]. The tools that are included in this set consist of various components such as techniques, research rigor, sample selection, data collection, and analysis.
In relation to the quality of the studies that were included, the CASP tool has identified significant aspects. The ability to apply these results to a broader population is limited due to the specific characteristics of the participants involved. It is important to note that the research included both male and female primary healthcare professionals. However, in some studies, the participants’ titles were not included, which makes it difficult to determine if they were in their training as senior general practitioners. It is crucial to consider this factor, as the knowledge and training of participants can vary significantly.
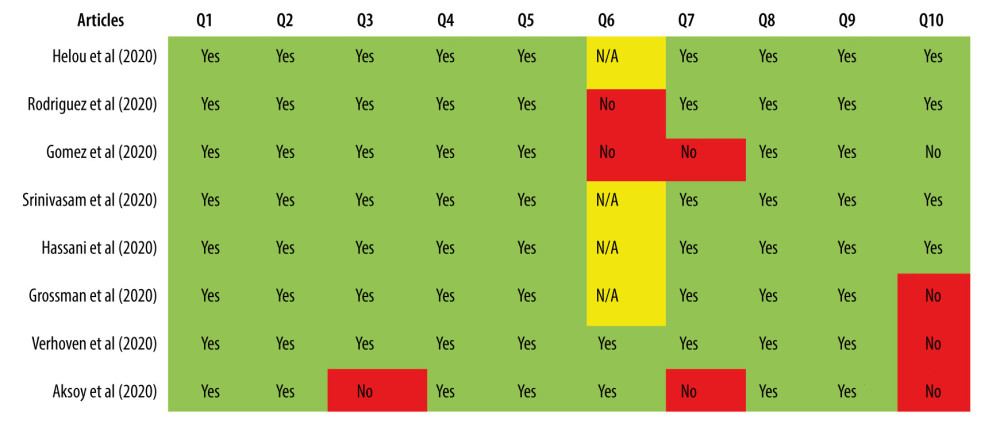
Given that the age group included individuals who were 18 years or older, it could be argued that the findings can be extrapolated to primary healthcare professionals, assuming a large and diverse sample size [39]. The validity of the study also plays a significant role in influencing the outcome. To achieve an outcome that aligns with its intended purpose, it is of utmost importance to comprehend the connection between reliability and validity. Although the assessments of the interviews were based on qualitative responses, participants were given the opportunity to openly share their perceptions about synchronous telemedicine [40]. Figure 2 show the quality assessment of the studies included in the current review.
Data Extraction
Extracting relevant information about studies and maintaining consistency in data extraction across all reviews is essential to effectively evaluate methodological problems and prevent bias. This includes considering factors such as the characteristics of the population and intervention being studied [41].
Using the structured data extraction tool JBI-QARI Joanna and Briggs Institute, 2011, the data were extracted independently in this review. The tool allows for a thorough extraction process, covering various aspects such as PEO specifiers, methodology, sample, environment, geography, culture, and data analysis of significance [42]. The main objective of this review was to assess the perceptions of healthcare professionals regarding this intervention.
The primary objective of all the included studies was to investigate the experiences of using telemedicine in primary healthcare. In all of the studies, the primary choice for study design was qualitative, with semi-structured interviews conducted for durations ranging from 15 to 60 minutes. This was also the primary method of data collection in most studies.
Data Synthesis
This systematic review identified healthcare professionals’ perceptions, experiences, and observations, and narrative synthesis was determined to be the best method for synthesizing the findings of the studies. Narrative synthesis focuses on techniques to improve the accountability and trustworthiness of studies [43]. Narrative synthesis aims to articulate and synthesize the findings of the included studies by comparing and contrasting the data. Therefore, synthesizing qualitative empirical data is like synthesizing quantitative evidence in the sense that where is a general interest in synthesizing empirical studies [44,45]. However qualitative synthesis seeks to synthesize qualitative data, which is usually text-based, unlike quantitative synthesis that translates knowledge into standard metrics and synthesizes these data to test a hypothesis using statistical meta-analysis [46].
Three stages of narrative synthesis were adopted to explore the relationship between the studies and assess the robustness of the synthesis [47]. Data for the included studies were qualitatively presented to reach a consensus on the conclusions [48]. A documented weakness of narrative synthesis is the transparency and the lack of clarity [49]. However, Toye et al and Barnett-Page and Thomas provide guidance on utilizing narrative synthesis systematically and present it in a more transparent way, concentrating on the synthesis and effectiveness after the intervention, and implementation factors [50,51].
Results of the Selection and Search Criteria
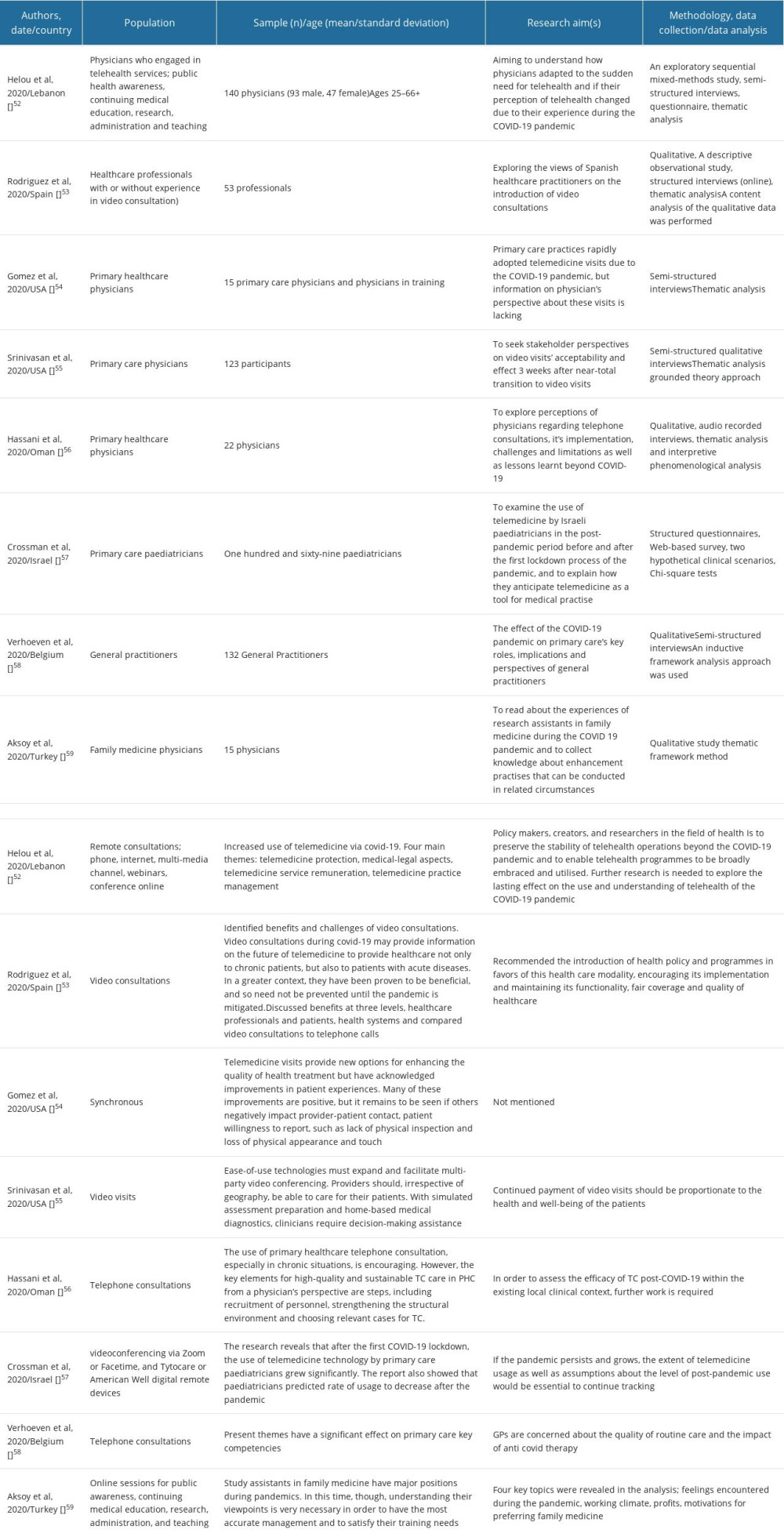
We found 627 articles from 6 databases and online searches; including Cinhal, Medline (EBSCO Host), ProQuest, PubMed, Cochrane, Summon, and Google Scholar. After duplicates were removed, 563 papers remained, and from these, 21 eligible articles were read in full text. During the screening stage, 542 were omitted based on abstract and title. Of the 21 papers, 13 papers were excluded because the full text was not available, the articles were written before the COVID-19 pandemic, or unsuitable data collection methods were used. Finally, 8 papers were included in this systematic review that met the eligibility criteria: Helou et al (2020, Lebanon); Rodriguez et al (2020, Spain); Gomez et al (2020, USA); Srinivasan et al (2020, USA); Hassani et al (2020, Oman); Crossman et al (2020, Israel); Verhoeven et al (2020, Belgium); and Aksoy et al (2020, Turkey) [52–59].
Characteristics of the Included Studies
The 8 studies included in the review were conducted between April 2020 and December 2020 due to the COVID-19 pandemic rising in December 2019. Due to the recent existence of COVID-19 and scarce data, the studies retrieved were conducted worldwide: USA (n=2), Israeli (n=1), Spain (n=1), Belgium (n=1), Turkey (n=1), Lebanon (n=1), and Oman (n=1). The population included in the studies were men and women aged >18, predominately primary and family medicine healthcare professionals. Table 2 show a description of included studies in this review.
All the studies included shared the same aim of exploring primary healthcare experiences with using telemedicine, particularly synchronous during the COVID-19 pandemic and beyond to continue care and treatment for patients with chronic conditions. The qualitative study design was predominately used in all the studies and semi-structured interviews, lasting 15–60 minutes. This was also the primary method of data collection among most studies.
Heterogenicity of the Studies
The method of analysis was varied among studies, with 4 of the studies using the thematic framework method [52–54,59], and combined content analysis of the qualitative data was also performed. Hassani et al also used thematic analysis collective with descriptive-interpretative phenomenological method analysis [56], the thematic analysis-grounded theory approach was used by Srinivasan et al [55], an inductive framework analysis approach was used by another study [58], and the chi-square test was used for a mixed-method study [57].
Synchronous (video conferencing or live telephone) interactions were the principal methods of telemedicine technology used in the studies, with some studies using a combination of synchronous telemedicine. Helou et used remote consultations using phone, internet, multimedia channel, and a webinar using online conferences [52]. Video consultations were used in studies carried by Rodriguez et al, Srinivasan et al, and Gomez et al [53–55], and video conferencing through Zoom was used by Crossman et al [57], while Hassani et al and Verhoeven et al performed telephone consultations [56–58]. On contrary, Aksoy et al focused on online sessions for public awareness, continuing medical education, research, administration, and teaching [59].
Quality Appraisal of the Included Studies
The quality of the 8 studies include was diverse. Methodology flaws in some studies were noted. Two studies, despite using a qualitative methodology, did not disclose the study design [54–57], whereas some studies noted the design, but they did not report the qualitative method, including phenomenological or ethnographic study [52,58,59]. The 3 remaining studies used grounded theory or a phenomenological approach [53,55,56]. Gomez et al and Helou et al used designs that were not robust enough for their aims and research question, raising the issues of validity and credibility [52,54]. Due to the difference in interview timing, some responses were less comprehensive than others [57–59], hindering the analysis and identification of the studies. The methodological choices were constrained by scarce data on telemedicine during the COVID-19 pandemic. Qualitative research predominately assesses participants’ feelings, emotions, and experiences, and this may affect interpretations of the results [44]. Akosy et al and Gomez et al [54,59] did not disclose ethical consideration; therefore, this should be addressed more carefully in qualitative research, as it focuses on exploring, identifying, and explaining human beings and their living environment [60].
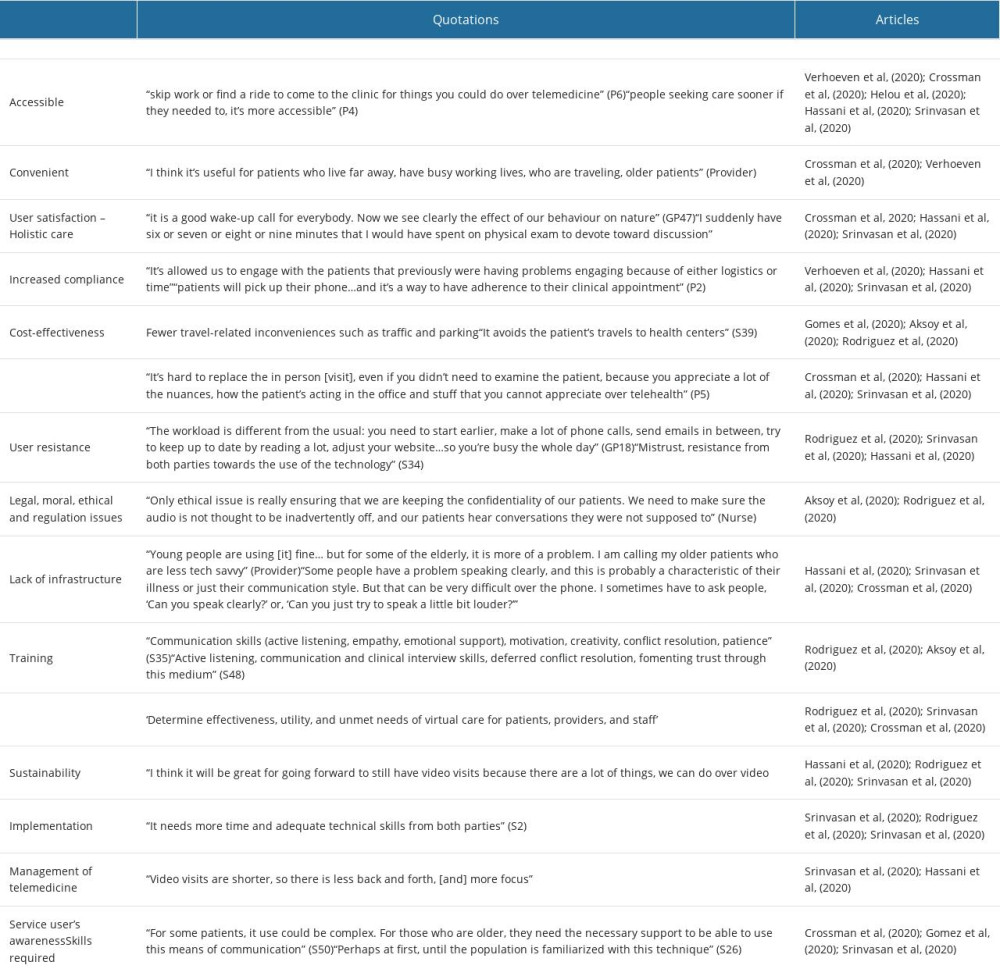
Emerging Themes
Four themes emerged and additional subthemes were also identified after reviewing the studies. The key themes were:
Discussion
The studies presented comprehensive qualitative data generated by narrative synthesis of experiences and perceptions of primary healthcare professionals on using synchronous telemedicine during the COVID-19 pandemic, which were mainly positive. Increased patient engagement, convenience, cost-effectiveness, and the ability to provide access to wider specialties were also identified as benefits of telemedicine. Nevertheless, the challenges, including technological issues, staff training, and user resistance, need to be investigated to ensure the successful implementation and sustainability of the service. Moreover, the shortcomings regarding patient safety and privacy also need to be urgently considered, as telemedicine is deemed to be key in managing the COVID-19 pandemic.
The purpose of this systematic review was to explore the perceptions and experiences of healthcare professionals working in primary care settings on using synchronous telemedicine to manage chronic health conditions during the COVID-19 pandemic. The review identified the benefits and effectiveness of synchronous telemedicine, risks and challenges, and the intended continuity of telemedicine interventions beyond the COVID-19 pandemic, thus reducing the morbidity and mortality during the pandemic [52,55]. The studies were conducted worldwide because of the currently limited data on COVID-19. Although differences in healthcare systems and infrastructure are recognised, the studies provided rich experiences, showing similarities and differences, thus learning from their experiences, and sharing best practices.
The main synchronous types of telemedicine that were used in the studies included video and telephone consultations or a combination of both, but video conferencing was the preferred mode of delivery by both the healthcare professionals and their patients. The ability to assess patients visually and have visual clues to make comprehensive assessments and empowering patients to take control of their treatments were reported as valuable features of video conferencing. The duration of the consultations is not clearly documented; however, in a study by Verhoeven et al, primary healthcare professionals mentioned that they have longer consultations virtually compared to the traditional 10 minutes per patient during an in-person visit [58,63], and indicated they can use the additional time to build rapport with their patients and get to know their patients more and conversely raise any social and safeguarding issues.
In a study conducted by Helou et al in 2020, the accessibility and convenience of telemedicine were extensively discussed. However, it is important to note that not all studies have the same results. Verhoeven et al found that while telemedicine may be accessible to a large group of people, there are concerns regarding the technological literacy of certain patient populations, particularly older individuals [58], which could hinder the effectiveness of telemedicine interventions, as pointed out by Akosy et al [54]. Despite the unprecedented situation caused by the COVID-19 pandemic, research suggests that utilizing telephone technology, which is less complex than video visits, could serve as a viable substitute for in-person consultations in general medical practice, as indicated by Gomez et al [54]. This is especially relevant for patients with chronic conditions, as highlighted by Hassani et al in 2020 [56], and involving families in setting up these telemedicine interventions could potentially overcome any technical barriers, as proposed by Gomez et al [54]. Another important benefit of telemedicine intervention, which is widely documented in studies, is the ability to provide continuity of care to patients, thereby offering a holistic approach. The implementation of this intervention has provided healthcare providers with a solution to the challenges they face in terms of limited time and resources during patient interactions [54]. Also, one more valuable aspect that the studies have highlighted about synchronous telemedicine is that it leads to an increase in patient compliance with their care and treatment plans, which ultimately showcases the promising benefits of telemedicine [52].
In addition, telemedicine has gained recognition for providing immediate remote access to expert medical advice, treatment, and diagnosis. This eliminates the necessity for individuals from rural areas to travel long distances to urban centers. Many medical residents have expressed a growing interest in enrolling in courses to enhance their understanding of telemedicine. More than half of the respondents in a study believed that telemedicine is a crucial component of the healthcare system, even during the COVID-19 pandemic [64,65]. Consequently, telemedicine has contributed to increased compliance among patients. In a 2020 study by Gomez et al [54], primary healthcare professionals observed that patients tend to be more engaged and compliant with their medications when they can physically show their medications and read the labels. Conversely, when patients are in the office, they often struggle to recall the names and regimens of their medications. Additionally, being able to communicate with their family members, whom they may not have had the opportunity to interact with otherwise, is another benefit of this engagement [53], possibly including them in the treatment of their patients, enhancing further compliance [55].
Concerns regarding patient privacy policies were highlighted by healthcare professionals. Therefore, it is of utmost importance to carefully consider the potential obstacles that could hinder the successful implementation of telemedicine, including but not limited to the safeguarding of patients’ sensitive data and ensuring confidentiality. Regrettably, the exploration of the legal and ethical responsibilities that come with telemedicine has not been fully realized, causing this issue to persist.
In their study, Scriviscan et al discovered that patients had concerns regarding the privacy of their transmitted medical records and other identifiable information when it came to the use of telemedicine [55]. Additionally, Gomez et al [54] and Bashshur et al [56] observed that the absence of proper legislation poses a significant constraint on implementing telemedicine. This is mainly due to the inconsistencies in establishing laws and regulations that effectively incorporate telemedicine into conventional healthcare systems [66].
Rodriguez et al, Scrinvasan et al, and Hassani et al identified barriers that could potentially impede the implementation of telemedicine and also emphasized the obstacle of acceptance of using human-computer interaction with patients for managing their clinical conditions [53,55,56]. The studies indicate that the successful implementation of telemedicine relies on individuals accepting and supporting the changes in their behavior.
One of the limiting factors in implementing the intervention is the lack of exposure to the latest technology, which affects both doctors and patients. Physicians are not only required to receive training on utilizing technological devices such as laptops, but they are also expected to maintain eye contact with their patients as a means of establishing a connection [55]. One of the challenges identified in the studies is the lack of technological infrastructure, including the absence of smart devices for elderly patients, limited bandwidth, and weak WIFI connection [55,57].
As a result of the swift expansion of telemedicine, valuable insights were gained on the implementation, maintenance, and administration of telemedicine both throughout and after the COVID-19 crisis.
According to the studies, the implementation stage is identified as a crucial factor in any telemedicine intervention. Verhoeven et al argue that it is a tremendous benefit for healthcare professionals to have their own patient list, as the challenges increase when patients are not familiar with their usual healthcare provider. Furthermore, in their video consultations, the primary healthcare professionals employ a proven technique known as Ideas, Concerns, and Expectations (ICE) to assist in the process [58]. However, even with the implementation of these innovative approaches, healthcare professionals have concerns about potentially overlooking critical diagnoses. Furthermore, Scrinivasan et al emphasized that to ensure high quality and sustainable synchronous telemedicine consultations, it is crucial to establish a proper structural framework. This framework should include defining the roles and responsibilities of primary healthcare professionals in a way that aligns with their professional objectives. In addition to these components, successful implementation of this project also necessitates staff training, enhancement of physical arrangements within the health center, and the careful selection of suitable cases for synchronous telemedicine [67].
The results suggested that the move to video consultations unveiled new ways of practicing medicine if obstacles to expense, equity, and staffing can be overcome [55,57,58]. Thus, some primary healthcare professionals strongly agree that telemedicine practices should remain ongoing for conditions that are deemed appropriate for telemedicine interventions beyond the pandemic, as this will improve access to healthcare, particularly for patients with chronic conditions [55]. However, there have been concerns raised about the level of job satisfaction among healthcare professionals and their capacity to effectively make complex and sensitive decisions through telemedicine methods; therefore, it is crucial that these concerns are addressed to ensure the long-term viability and success of telemedicine [53].
The studies highlight the crucial importance of effectively managing telemedicine services to ensure long-term success and the ongoing delivery of telemedicine interventions. As a result, the studies emphasized the importance of providing regular and consistent feedback on telemedicine activities to maintain its continuity and make further enhancements that align with clinical requirements. Compliance with the COVID-19 government guidelines prompted primary healthcare practices to make adaptations during the implementation of synchronous telemedicine.
It is evident from the studies that the COVID-19 pandemic has led to a swift and substantial growth in the utilization of telemedicine [68]. According to the studies, under normal circumstances, it would have required several years to achieve this level of progress. However, due to the urgent demands, the timeline was compressed to just 2 to 3 weeks, resulting in immense pressure on healthcare personnel to ensure safety and optimize all essential aspects. A study conducted by Srinivasan et al in 2020 recorded a remarkable statement that caught their attention: “I have never witnessed such a rapid allocation of resources before” [55]. Therefore, the future of telemedicine as an essential component of the healthcare system relies on the permanence and approval of legislation and regulations by governmental authorities, regardless of the COVID-19 pandemic.
Due to the high number of COVID-19 cases that have been reported during the pandemic, patients have come to realize that the healthcare system is under immense pressure, making it increasingly challenging for them to schedule in-person appointments with their regular healthcare providers. Following that, the articles found in the results suggest that service users have shown their appreciation for telemedicine as it helps mitigate the risk of transmission, especially for individuals who are considered high-risk. Furthermore, both patients and healthcare professionals had to make adjustments and embrace the concept of telemedicine to fully reap its benefits [52].
However, it is important to address the limitations of telemedicine, which include concerns regarding patient privacy, confidentiality, and the need for a robust technical infrastructure, to fully maximize its potential. Firstly, the review was conducted in December 2020 when COVID-19 first appeared at the beginning of the outbreak to explore the use of synchronous telemedicine. Thus, there were many interviews conducted; therefore, there was wide variability in the sample of the primary healthcare professionals, contributing to rich results. Secondly, this systematic review was conducted with the support of the university librarians, providing advice and guidance using their expert knowledge on literature searching. The PEO framework was utilized to identify related terms, focusing on the search and using Boolean words to build on searches adapted to various databases. However, the qualitative analysis provides more precise, comprehensive, and complex search strategies compared to quantitative data [44]. Although an advantage of qualitative review is the ability to provide a comprehensive and detailed review [69], a drawback of this is that it can be time-consuming to scan a large amount of data to read the full text, particularly for an MSC student to undertake this review independently. However, the 8 included studies provided rich data, and the PRISMA flow diagram was used to visualize the process of filtering the desired studies.
Additional recent studies or systematic reviews investigated and assessed the different types of telemedicine with its various themes “effectiveness and/or challenges of telemedicine, and lessons learned with strategies moving forward, as well as service acceleration”. The different outcome of this systematic review is in parallel with the investigated studies analyzed in the telemedicine during last year’s [70–73].
Although previous research conducted on this topic might have been missed during searches, this research adds knowledge to the missing data within primary practice, particularly with the rapid changes in government polices to reflect on best practice based on current evidence, so our study followed a systematic search strategy and covered a wide spectrum of evidence worldwide. We only included studies written in English, which could be a source of bias, and we did not search the grey literature.
Conclusions
According to the narrative synthesis, synchronous telemedicine is believed to offer valuable benefits, and its features are seen as promising in terms of providing ongoing care and treatment to patients, particularly those with chronic conditions. Telemedicine also brought to light concerns such as patient privacy, confidentiality, and the need for adequate training for service users. The significance of addressing these flaws is reiterated in the review, as it is crucial for telemedicine to be implemented successfully and reach its full potential.
Given the exponential global growth of the COVID-19 pandemic, there is a pressing need for future research to delve deeper into the effectiveness of synchronous telemedicine and shed light on unmet needs within the health sector. Healthcare professionals showed great enthusiasm for the ongoing integration of telemedicine into their practices. The identified themes have significant empirical implications for future research, as they offer concrete evidence based on the experiences of primary healthcare professionals, thus contributing to a better understanding of the subject.
References
1. Barnett K, Mercer SW, Norbury M, Epidemiology of multimorbidity and implications for health care, research, and medical education: A cross-sectional study: Lancet, 2012; 380(9836); 37-43
2. Murphy M, Scott LJ, Salisbury C, Implementation of remote consulting in UK primary care following the COVID-19 pandemic: A mixed-methods longitudinal study: Br J Gen Pract, 2021; 71(704); e166-e77
3. Department of Health: Long term conditions compendium of information, 2012 https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/216528/dh_134486.pdf
4. Cutler D, Mehrotra A, Chernew M, Hatch H: The impact of the COVID-19 pandemic on outpatient visits: A rebound emerges, 2020 https://www.commonwealthfund.org/publications/2020/apr/impact-covid-19-outpatient-visits
5. Davarpanah AH, Mahdavi A, Sabri A, Novel screening and triage strategy in iran during deadly coronavirus disease 2019 (COVID-19) epidemic: Value of humanitarian teleconsultation service: J Am Coll Radiol, 2020; 17(6); 734-38
6. Jiang F, Deng L, Zhang L, Review of the clinical characteristics of coronavirus disease 2019 (COVID-19): J Gen Intern Med, 2020; 35(5); 1545-49
7. World Health Organisation: Q & A on coronaviruses (COVID-19), 2020 https://www.who.int/news-room/q-a-detail/q-a-coronaviruses
8. Department of Health and Social Care: Coronavirus: stay at home, protect the NHS save lives – web version, 2020 https://www.gov.uk/government/publications/coronavirus-covid-19-information-leaflet/coronavirusstay-at-home-protect-the-nhs-save-lives-web-version
9. Barach P, Fisher SD, Adams MJ, Disruption of healthcare: Will the COVID pandemic worsen non-COVID outcomes and disease outbreaks?: Prog Pediatr Cardiol, 2020; 59; 101254
10. World Health Organization: Telemedicine: opportunities and developments in member states. Report on the second global survey on eHealth, 2010 https://www.who.int/goe/publications/goe_telemedicine_2010.pdf
11. Smith A: Telemedicine vs. telehealth: What’s the difference?, 2018 https://chironhealth.com/blog/telemedicine-vs-telehealth-whats-the-difference/
12. Krupinski EA, Bernard J, Standards and guidelines in telemedicine and telehealth: Healthcare (Basel), 2014; 2(1); 74-93
13. Pyne JM, Fortney JC, Tripathi SP, Cost-effectiveness analysis of a rural telemedicine collaborative care intervention for depression: Arch Gen Psychiatry, 2010; 67(8); 812-21
14. Craig J, Patterson V, Introduction to the practice of telemedicine: J Telemed Telecare, 2005; 11(1); 3-9
15. Currell R, Urquhart C, Wainwright P, Lewis R, Telemedicine versus face-to-face patient care: Effects on professional practice and health care outcomes: Cochrane Database Syst Rev, 2000(2); CD002098
16. Dorsey ER, Topol EJ, State of telehealth: N Engl J Med, 2016; 375(2); 154-61
17. Chauhan V, Galwankar S, Arquilla B, Novel coronavirus (COVID-19): Leveraging telemedicine to optimize care while minimizing exposures and viral transmission: J Emerg Trauma Shock, 2020; 13(1); 20-24
18. Hollander JE, Carr BG, Virtually perfect? Telemedicine for COVID-19: N Engl J Med, 2020; 382(18); 1679-81
19. Greenhalgh T, Koh GCH, Car J, COVID-19: A remote assessment in primary care: BMJ, 2020; 368; m1182
20. Office for National Statistics: Internet access – households and individuals, 2020, Great Britain https://www.ons.gov.uk/peoplepopulationandcommunity/householdcharacteristics/homeinternetandsocialmediausage/bulletins/internetaccesshouseholdsandindividuals/2019
21. Pogorzelska K, Marcinowicz L, Chlabicz S, A qualitative study of primary care physicians’ experiences with telemedicine during the COVID-19 pandemic in North-Eastern Poland: Int J Environ Res Public Health, 2023; 20(3); 1963
22. Dwyer TF, Telepsychiatry: Psychiatric consultation by interactive television: Am J Psychiatry, 1973; 130(8); 865-69
23. Benschoter RA, Eaton MT, Smith P, Use of videotape to provide individual instruction in techniques of psychotherapy: J Med Educ, 1965; 40(12); 1159-61
24. Monaghesh E, Hajizadeh A, The role of telehealth during COVID-19 outbreak: A systematic review based on current evidence: BMC Public Health, 2020; 20(1); 1193
25. Polit DF, Beck CT, Generalization in quantitative and qualitative research: Myths and strategies: Int J Nurs Stud, 2010; 47(11); 1451-48
26. Parahoo K: Nursing research: principles, process, and issues, 2014, Basingstoke, Palgrave Macmillan https://www.scirp.org/(S(351jmbntvnsjt1aadkposzje))/reference/ReferencesPapers.aspx?ReferenceID=1982958
27. Aveyard H, Doing a literature review in health and social care: A practical guide. 2nd ed: Nurse Res, 2011; 18(4); 45
28. Stansfield C, Kavanagh J, Rees R, The selection of search sources influences the findings of a systematic review of people’s views: A case study in public health: BMC Med Res Methodol, 2012; 12; 55
29. Khan KS, Kunz R, Kleijnen J, Antes G, Five steps to conducting a systematic review: J R Soc Med, 2003; 96(3); 118-21
30. Bettany-Saltikov J, McSherry R: How to do a sytematic literature review in nursing: A step-by-step guide, 2016 https://research.tees.ac.uk/en/publications/how-to-do-a-systematic-literature-review-in-nursing-a-step-by-ste-3
31. Booth A, Searching for qualitative research for inclusion in systematic reviews: A structured methodological review: Syst Rev, 2016; 5; 74
32. Mahmoud K, Jaramillo C, Barteit S, Telemedicine in low- and middle-income countries during the COVID-19 pandemic: A scoping review: Front Public Health, 2022; 10; 914423
33. Stern C, Jordan Z, McArthur A, Developing the review question and inclusion criteria: Am J Nurs, 2014; 114(4); 53-56
34. Shaw SE, Seuren LM, Wherton J, Video consultations between patients and clinicians in diabetes, cancer, and heart failure services: Linguistic ethnographic study of video-mediated interaction: J Med Internet Res, 2020; 22(5); e18378
35. Shamseer L, Moher D, Clarke MPRISMA-P Group, Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: Elaboration and explanation: BMJ, 2015; 350; g7647
36. Boland A, Cherry MG, Dickson R: Doing a systematic review: A student’s guide, 2017, London, SAGE, Los Angeles https://study.sagepub.com/doingasystematicreview2e
37. Hart C: Doing a literature review: releasing the research imagination, 2018, Los Angeles, SAGE https://www.amazon.com/Doing-Literature-Review-Releasing-Imagination/dp/1526419211
38. : Critical Appraisal Skills Programme CASP (Qualitative) checklist, 2018 https://casp-uk.net/wp-content/uploads/2018/01/CASP-Qualitative-Checklist-2018.pdf
39. Hannes K, Lockwood C, Pearson A, A comparative analysis of three online appraisal instruments’ ability to assess validity in qualitative research: Qual Health Res, 2010; 20(12); 1736-43
40. Leung L, Validity, reliability, and generalizability in qualitative research: J Family Med Prim Care, 2015; 4(3); 324-27
41. Riesenberg LA, Justice EM, Conducting a successful systematic review of the literature, part 1: Nursing, 2014; 44(4); 13-17
42. Joanna Briggs Institute: Joanna Briggs Institute reviewers’ manual, 2011, Adelaide, Australia, The University of Adelaide https://scirp.org/reference/referencespapers.aspx?referenceid=1510926
43. Noyes J, Booth A, Moore G: Chapter 21: Qualitative evidence, 2019 https://training.cochrane.org/handbook/current/chapter-21#section-21-10
44. Carroll C, Booth A, Quality assessment of qualitative evidence for systematic review and synthesis: Is it meaningful, and if so, how should it be performed?: Res Synth Methods, 2015; 6(2); 149-54
45. Hasson F, Nicholson E, Muldrew D, A systematic review of international palliative care research priorities and a thematic synthesis of findings: Palliative Medicine, 2019, School of Nursing, Faculty Of Life & Health Sciences (EAPC Abstracts) Available at: https://doi.org/10.1177/0269216319844405
46. Holly C, Salmond S, Saimbert M: Comprehensive systematic review for advanced practice nursing, 2016, New York, Springer Publishing, Company https://www.researchwithrutgers.com/en/publications/comprehensive-sstematic-review-for-advanced-practice-nursing-thir
47. Butler A, Hall H, Copnell B, A guide to writing a qualitative systematic review protocol to enhance evidence-based practice in nursing and health care: Worldviews Evid Based Nurs, 2016; 13(3); 241-49
48. Porritt K, Gomersall J, Lockwood C, JBI’s Systematic Reviews: Study selection and critical appraisal: Am J Nurs, 2014; 114(6); 47-52
49. Britten N, Campbell R, Pope C, Donovan J, Morgan M, Pill R, Using meta ethnography to synthesise qualitative research: A worked example: J Health Serv Res Policy, 2002; 7(4); 209-15
50. Barnett-Page E, Thomas J, Methods for the synthesis of qualitative research: A critical review: BMC Med Res Methodol, 2009; 9; 59
51. Toye F, Seers K, Allcock N, Meta-ethnography 25 years on: Challenges and insights for synthesising a large number of qualitative studies: BMC Med Res Methodol, 2014; 14; 80
52. Helou S, El Helou E, Abou-Khalil V, The effect of the COVID-19 pandemic on physicians’ use and perception of telehealth: The case of Lebanon: Int J Environ Res Public Health, 2020; 17(13); 4866
53. Jiménez-Rodríguez D, Santillán García A, Montoro Robles J, Increase in video consultations during the COVID-19 pandemic: Healthcare professionals’ perceptions about their implementation and adequate management: Int J Environ Res Public Health, 2020; 17(14); 5112
54. Gomez T, Anaya YB, Shih KJ, Tarn DM, A qualitative study of primary care physicians’ experiences with telemedicine during COVID-19: J Am Board Fam Med, 2021; 34(Suppl); S61-S70
55. Srinivasan M, Asch S, Vilendrer S, Qualitative assessment of rapid system transformation to primary care video visits at an academic medical center: Ann Intern Med, 2020; 173(7); 527-35
56. Hasani SA, Ghafri TA, Al Lawati H, The use of telephone consultation in primary health care during COVID-19 pandemic, Oman: Perceptions from physicians: J Prim Care Community Health, 2020; 11; 2150132720976480
57. Grossman Z, Chodick G, Reingold SM, The future of telemedicine visits after COVID-19: Perceptions of primary care pediatricians: Isr J Health Policy Res, 2020; 9(1); 53
58. Verhoeven V, Tsakitzidis G, Philips H, Van Royen P, Impact of the COVID-19 pandemic on the core functions of primary care: Will the cure be worse than the disease? A qualitative interview study in Flemish GPs: BMJ Open, 2020; 10(6); e039674
59. Aksoy H, Ayhan Başer D, Fidancı İ, Family medicine research assistants’ experiences during COVID-19 pandemic: A qualitative study: Int J Clin Pract, 2021; 75(5); e13975
60. Roberts LD, Ethical issues in conducting qualitative research in online communities: Qualitative Research in Psychology, 2015; 12(3); 314-25
61. Eisner E, Barrowclough C, Lobban F, Drake R, Qualitative investigation of targets for and barriers to interventions to prevent psychosis relapse: BMC Psychiatry, 2014; 14; 201
62. Davies B, Mallows L, Hoare T, “Supporting me through emotional times, all different kinds of behaviour.” Forensic mental health service users understanding of positive behavioural support: J Forensic Psychiatry Psychology, 2016; 27; 530-50
63. Daly J, Willis K, Small R, A hierarchy of evidence for assessing qualitative health research: J Clin Epidemiol, 2007; 60(1); 43-49
64. Andronic O, Petrescu GED, Artamonov AR, Healthcare professionals’ specialists’ perception of telemedicine in Romania – A quantitative study of beliefs, practices, and expectations: Healthcare (Basel), 2023; 11(11); 1552
65. Assaye BT, Belachew M, Worku A, Perception towards the implementation of telemedicine during COVID-19 pandemic: A cross-sectional study: BMC Health Serv Res, 2023; 23(1); 967
66. Bashshur R, Doarn CR, Frenk JM, Telemedicine and the COVID-19 pandemic, lessons for the future: Telemed J E Health, 2020; 26(5); 571-73
67. Kruse CS, Krowski N, Rodriguez B, Telehealth and patient satisfaction: A systematic review and narrative analysis: BMJ Open, 2017; 7(8); e016242
68. Kissi J, Annobil C, Mensah NK, Telehealth services for global emergencies: Implications for COVID-19: A scoping review based on current evidence: BMC Health Serv Res, 2023; 23(1); 567
69. Tong A, Flemming K, McInnes E, Oliver S, Craig J, Enhancing transparency in reporting the synthesis of qualitative research: ENTREQ: BMC Med Res Methodol, 2012; 12; 181
70. Lindenfeld Z, Berry C, Albert S, Synchronous home-based telemedicine for primary care: A review: Med Care Res Rev, 2023; 80(1); 3-15
71. Mabeza RMS, Maynard K, Tarn DM, Influence of synchronous primary care telemedicine versus in-person visits on diabetes, hypertension, and hyperlipidemia outcomes: A systematic review: BMC Prim Care, 2022; 23(1); 52
72. Andino JJ, Eyrich NW, Boxer RJ, Overview of telehealth in the United States since the COVID-19 public health emergency: A narrative review: Mhealth, 2023; 9; 26
73. Al-Hazmi AM, Sheerah HA, Arafa A, Perspectives on telemedicine during the era of COVID-19; What can Saudi Arabia do?: Int J Environ Res Public Health, 2021; 18(20); 10617
In Press
18 Apr 2024 : Clinical Research
Comparative Analysis of Open and Closed Sphincterotomy for the Treatment of Chronic Anal Fissure: Safety an...Med Sci Monit In Press; DOI: 10.12659/MSM.944127
08 Mar 2024 : Laboratory Research
Evaluation of Retentive Strength of 50 Endodontically-Treated Single-Rooted Mandibular Second Premolars Res...Med Sci Monit In Press; DOI: 10.12659/MSM.944110
11 Mar 2024 : Clinical Research
Comparison of Effects of Sugammadex and Neostigmine on Postoperative Neuromuscular Blockade Recovery in Pat...Med Sci Monit In Press; DOI: 10.12659/MSM.942773
12 Mar 2024 : Clinical Research
Comparing Neuromuscular Blockade Measurement Between Upper Arm (TOF Cuff®) and Eyelid (TOF Scan®) Using Miv...Med Sci Monit In Press; DOI: 10.12659/MSM.943630
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952