24 November 2023: Clinical Research
Prosthodontic Rehabilitation’s Role in Alleviating Anxiety and Depression in Mucormycosis-Induced Maxillectomy Patients Post-COVID-19
Abdulelah Sameer SindiDOI: 10.12659/MSM.941488
Med Sci Monit 2023; 29:e941488
Abstract
BACKGROUND: The aim of this study was to assess the influence of maxillofacial prosthodontic rehabilitation on anxiety/depression severity in patients with rhino-orbital cerebral mucormycosis (ROCM) after maxillectomy.
MATERIAL AND METHODS: Sixty post-mucormycotic patients treated with maxillectomy (33 males, 27 females) were divided into 5 groups based on maxillectomy types (unilateral/bilateral, subtotal/total) and treatment given (psychotherapy/obturator/implant/orbital/ocular prosthesis). Anxiety and depression symptoms were assessed using appearance anxiety inventory (AAI) and patient health questionnaire (PHQ9). Data were collected at 4 time intervals [T0 (before prosthesis), T1 (2 weeks after prosthesis), T2 (6 months) and T3 (1 year). Frequency distribution and mean values were determined for individual group/subgroups/total cohort. Differences between groups were determined using one-way ANOVA (single-factor/Friedman’s) followed by post hoc correction (Bonferroni) and t test for unequal variance with probability P value being statistically significant at <0.05.
RESULTS: The mean scores for appearance anxiety were 29.13±4.72 (diagnostic for existing body dysmorphic disorder) at T0, which decreased to 16.88±3.02 at T3 for the total cohort. The differences for the gender-based cohort, its various groups, and respective subgroups were significant (P<0.05) at various time intervals. The mean scores in the total cohort for depression symptom severity were 16.81±4.89 (moderately severe) at T0, which increased to 18.5±4.94 at T1, followed by reduction at T2 (12.0±4.43; moderate) and T3 (7.38±3.37; mild). Gender differences for both variables were found to be statistically significant (P<0.05).
CONCLUSIONS: Comprehensive rehabilitation that included a diagnosis of psychological symptoms followed by psychotherapeutic/pharmacotherapeutic/prosthodontic intervention reduced the anxiety/depression symptom levels to normal at 1 year.
Keywords: COVID-19, Diabetes Mellitus, mucormycosis, Prostheses and Implants, Psychotherapy
Background
On May 23, 2023, the world received an auxiliary warning by the World Health Organization director, stating that pathogens of the future will have more fatal potential than COVID-19 [1]. Fear of death was the feature of the first COVID-19 pandemic phase, which involved social distancing and quarantine, irrespective of age or gender. Preventive social measures (eg, social distancing, quarantines, work from home) created distress, which has been associated with the development of chronic disease and premature mortality [2,3]. After COVID-19, stress-related disorders like anxiety and depression affected otherwise healthy populations, including the elderly [4]. Vaccination imparted initial immunity, but then there was a second wave of the COVID-19 pandemic. The second wave of the COVID-19 pandemic in India (March 13, 2021, to June 19, 2021), due to delta variant (B.1.617.2), not only increased COVID-19 cases (by 2.4 times) and mortality (by 2.7 times), [5] but also triggered a dormant, rare, life-threatening, and disfiguring fungus (angioinvasive), termed mucormycosis (MM) (Order, Mucorales). The flesh-eating fungus was reported to affect 45 374 people, killing more than 4300 individuals, during the second Indian COVID-19 wave [6]. MM is an opportunistic superinfection in immune-compromised people, and takes different forms (pulmonary, gastrointestinal, cutaneous, disseminated, and sinus-orbit-brain) based on the site of occurrence. Rhino-orbital-cerebral mucormycosis (ROCM) during the second wave was the most prevalent form in India (90% of cases) [7], chiefly because of climatic condition favoring the spread of
For a COVID-19-associated ROCM patient, developing a life-threatening fungal infection within the face, followed by its resection that results in a disfigured face, inflicts additional, different, and extreme mental distress that needs to be diagnosed and treated during or after the course of post-maxillectomy rehabilitation. Anxiety reduces an individual’s coping strategies while depression diminishes self-esteem, causing apathy and anhedonia, and are known to impact treatment outcomes [18]. Both being complexly interwoven, anxiety and depression share symptoms (non-specific and similar), which favors evolving of one condition into another, over time, if unchecked or left untreated [19]. The severity of the condition will increase if both occur simultaneously, since both are interrelated. Recent evidence reveals pre-infection distress (symptoms of depression and anxiety) strongly associated with risk of post-COVID-19 conditions (long COVID) [20]. Disturbingly, anxiety was triggered by events like physical activity (50% of study subjects), which contrarily protects against psychological illness [21]. The severity (degree) of anxiety/depression in COVID-19-associated ROCM have also been reported to increase – anxiety: extremely severe (26%), severe (17%), moderate (5%), depression: extremely severe (6%), severe (28%), moderate (12%) [22]. Studies have also investigated the psychological construct “demoralization” with subcomponents of existential despair, hopelessness, helplessness, and loss of purpose and meaning in life. The consequences of demoralization have been reported to be associated with suicide risk and suboptimal recovery [23].
Higher levels of these psychological parameters can be detrimental during complex maxillofacial rehabilitation, can lead to negative outcomes, and can be a possible source of patient dissatisfaction with planned treatment [24]. Significantly, during the course of maxillofacial rehabilitation, the influence of such psychological variables needs to be controlled through correct diagnosis/intervention (psychotherapy/pharmacotherapy). Alternately, successful rehabilitation compounded with psychotherapeutic intervention can reduce anxiety and/or depression levels and improve final treatment outcome. Maxillofacial prosthetic/prosthodontic rehabilitation in ROCM patients who have undergone maxillectomy (total or subtotal; unilateral or bilateral) may require either an obturator prosthesis (unilateral cases) or zygomatic implant-supported complete denture prosthesis (bilateral maxillectomy), both of which require patients to learn new functional patterns. Occlusal rehabilitation that restores masticatory functions improve patient neuro-cognition [22]. Therefore, this study was intended to fulfill the following aims and objectives: (a) to assess the severity of symptoms of anxiety and depression in ROCM maxillectomy patients scheduled for maxillofacial prosthodontic rehabilitation; and (b) to evaluate the influence of comprehensive prosthodontic/psychotherapeutic rehabilitation using definitive obturator and zygomatic implant-supported prosthesis on the levels of anxiety and depression before/after rehabilitation. We hypothesized that prosthodontic rehabilitation would reduce the levels of anxiety and depression in ROCM maxillectomy patients. The null hypothesis was that there would be no differences in the levels of anxiety or depression after comprehensive interventions.
Material and Methods
ETHICS:
This clinical study was conducted from 2021 to 2022, in collaboration with the Department of General Surgery, Ear, Nose, and Throat (ENT) and Maxillofacial Prosthodontics at a postgraduate institute of north India, which adheres to the principles of human and animal experimentation according to national and international guidelines (Helsinki Declaration). The study was duly registered and approved by the King George Medical University Ethics Committee (No. 744/Ethics/21; Ref code – 99 ECM IIB/P 53). All patients who were involved in this study provided written informed consent after being educated about the purpose/benefit/confidentiality while conducting or reporting the results of the study. All participants also gave written consent to display their images for education or publishing purpose.
STUDY DESIGN:
This clinical study presents a double-blinded (investigation and data collection) prospective cohort study that was conducted in 3 phases: sampling, intervention, and follow-up. The sample (purposive) of patients was derived from the outpatient department, who reported for maxillofacial prosthetic/prosthodontic rehabilitation after undergoing surgery (maxillectomy) for post-COVID-19-related mucormycosis-associated ROCM. The study utilized both quantitative and qualitative data collection measure and analysis.
OPERATIONAL DEFINITION:
Subtotal maxillectomy (STM) is maxillary resection involving removal of a minimum of 2 walls, including the hard palate (antrum floor), except for the posterior wall. Total maxillectomy (TM) is specific resection of the entire maxilla (including 4 processes, hard palate, and involved sinuses) with/without resection of the floor of the orbit. When total maxillectomy was extended to include exenteration of the orbital contents and sphenoidectomy and/or pterygoid plates, it was termed total maxillectomy with orbital exenteration (TMOE). Body dysmorphic disorder is a mental health condition in which an individual is preoccupied with perceived defects/imperfections in physical appearance that may not necessarily be observed by others.
SAMPLE SELECTION, PREPARATION, AND GROUPING:
ROCM patients previously diagnosed and/or treated at the Medical College, either through a referral or direct outpatient approach, formed the patient pool from which the study sample was gathered. Definitive diagnosis of ROCM associated with COVID-19 was based on and verified (medical records) by clinical history (history of COVID-19, vaccination, and systemic history), clinical manifestations (signs and symptoms) specific to mucormycosis, tissue biopsy with blood and fungal culture (Sabouraud dextrose agar and potato dextrose agar), computed tomography (CT) scan, and magnetic resonance imaging (MRI). General selection criteria included adult patients, any gender, systemic health compromised but limited to controlled diabetes, hypertension, and/or both, no history of previous diagnosis of depressive disorders, manic episodes, drug abuse, bereavement due to loss of family member, complications after/during maxillectomy postoperative healing, complete healing from previous surgery, willing to undergo further surgery (for placement of zygomatic implants), had completed full course of anti-fungal medication, vaccinated for corona virus, and gave written informed consent for the treatment/study. Additional eligibility criteria for bilateral subtotal and total maxillectomy patients were additional minimum 1-month postoperative healing period (total minimum of 3–4 months after maxillectomy), intact zygomatic bone and its processes on both sides, and vertical and horizontal component within guidelines for modified maxillectomy defects (with/without local soft-tissue flap closure) [25]. Any patient with poor Mini-Mental State Examination (MMSE) scores, histopathologic or radiographic evidence of MM recurrence, symptoms/signs of ROCM, existing uncontrolled systemic diseases, drug/smoking/alcohol/chewing tobacco use, or who did not consent for intervention were excluded from the study protocol. After screening of each patient using CBCT, the study sample included 60 patients from a total of 108 patients, whose characteristics regarding the defect and the treatment planned are presented in Figure 1 (Flowchart). The study sample was derived from a large sample (purposive sampling) categorized into subgroups (convenience sampling) based on the type of maxillectomy and the required treatment protocol (critical case sampling). Based on the previously published prosthodontic guidelines [26], the participants were categorized into 5 different groups (Gp) of maxillectomy (treatment) type: subtotal maxillectomy (STM) – unilateral (U), STM – bilateral (B) (Figure 2A), Total maxillectomy (TM) – unilateral (Figure 2B), TM – bilateral (Figure 2C) and total maxillectomy (unilateral) with orbital exenteration (TMOE) (Figure 2D). The treatment (maxillectomy) rendered to these subjects was determined based on the severity and extent of RCOM mucormycosis at the time of diagnosis of post-COVID-19 mucormycosis. All groups were further subdivided based on gender as male (M) and female (F) to minimize variability in responses for variable measurements between groups.
CLINICAL INTERVENTION/TREATMENT:
A case history sheet was specifically developed for the study that recorded the demographic details (personal, social, medical, drug, dental histories), current chief concerns, and history of present illness. The case sheet was also customized to include the treatment plan, treatment delivered (including all clinical and laboratory steps), and measurement tools for anxiety (appearance anxiety inventory – AAI) and severity of depression symptoms (PHQ-9). All patients had chief concerns of abnormal eating and swallowing, nasal regurgitation of food and drinks (patients with oral-nasal communication), speech defects, and difficult oral hygiene maintenance. For all patients, extra-oral and intra-oral photographs (exemplary Figure 2A–2D), orthopantomograph (Gendex GXDP-700 Series OPG System, KaVo, Germany) and a preoperative computed tomography scan (CT) (Figure 3A–3D) (CS9300 Carestream, Atlanta, GA) were taken and assessed. The analysis showed the level of tissue removal, the areas of non-healing or unhealed tissues, bone mineralization, and the possibility of reinfection with MM. For bilateral maxillectomy cases (subtotal and total), the treatment planned was a zygomatic implant-supported maxillary complete denture prosthesis, and for unilateral maxillectomy cases (subtotal and total) the treatment planned was obturator prosthesis retained and supported by a removable cast partial denture. For unilateral TMOE, the treatment included an obturator and ocular and orbital prostheses. The latter 2 were either fabricated together or separately, depending on the individual case.
STM (B) AND TM (B) GROUPS (BILATERAL ZYGOMATIC IMPLANT PLACEMENT):
Routine diagnostic investigations (blood glucose, hypertension, blood cell count, and kidney and liver function tests) were performed for all patients in all groups. CBCT evaluation added with the aid of DICOM (Digital Imaging and Communications in Medicine) and 3D printed acrylic models were used to determine the correct placement of long isoelastic implants with a smooth surface (lag screw designs for immediate functional loading protocol) (exemplary Figures 4A–4D, 5A–5G). Ideal location for 9 different lengths long and intermediate implants was first visualized on the CT scan (Figures 4, 5) followed by mock implant placement on 3D printed acrylic models derived from the data obtained from the scan. This enabled evaluation of angulation of each implant and their respective anteroposterior spread to enable a successful prosthetic outcome. Surgical planning was achieved by running virtual software (Die EXOCAD, Dental CAD, Darmstadt, Germany), which enabled maximum prosthetic efficiency in terms of function and durability. The final prosthesis design included 3 sections: a soldered intra-oral framework base, orbital wall extension laterally using bi-cortical screws, long bar (short connector) that minimizes tissue impingement and does not obliterate restorative space), cylinder threads (to attach equator bridge), natural canine and molar abutment placements, and bar-supported cement-retained prosthesis (self-cleansing and manual cleansing by the patient). Surgical procedures were performed under a combination of topical and local anesthesia following strict infection control [27] and COVID-19 guidelines [28] were performed by a multidisciplinary team (oral maxillofacial surgeon, ENT specialist, general surgeon, and prosthodontist). Bilateral full-thickness flaps raised over the zygoma body with a surgical blade (15 c) (Hu-Friday, Rockwell, St. Chicago) were raised while identifying and retracting significant anatomical structures. Bony sutures (zygomatic arch root, frontozygomatic) were accessed through sub-periosteal undermining. Osteotomy for implant placements was done with zygomatic implant drills under copious irrigation of normal saline. Four long, smooth-surface implants (apical thread 4.6 mm length and 2 mm diameter, overall length 45 mm/47.5 mm) for zygoma body, 4 intermediate-length implants for posterior placement (26 mm/29 mm), and 1 extra-long (52.5 mm or longer) for frontal bone were placed at respective implant sites with high initial stability [ISQ (implant stability quotient) >70 Ncm]. All patients were prescribed post-surgical analgesics and antibiotics, depending upon the clinical indication for each patient.
A zygomatic implant-supported prosthesis was fabricated and delivered to each patient within 1 week of surgery (immediate loading protocol). Standard cylindrical titanium bar protruding implants were splinted together into a single unit using an intra-oral welding procedure (International Implant Company, Verona, Italy) [29]. Definitive impressions using elastomers (addition silicone) were made over impression caps followed by laboratory fabrication of superstructure using laser sintering. An alloy framework was tried for each individual patient and verified using radiographs followed by cementation with resin modified glass ionomer cement (GC Fuji plus). The outstanding prosthodontic procedure included standard clinical/laboratory procedures for an implant-supported prosthesis. A permanent silicon-based soft liner (Molloplast B, Detax GmbH & Co, KG Ettlingen, Germany) provided retention of the acrylic prosthesis over the bar (Figure 6A). All patients received written post-insertion instructions along with a chairside verbal explanation of each instruction for long-term maintenance, use, and care. Post-prosthetic rehabilitation using zygomatic implants improved the facial aesthetics of patients (exemplary Figure 7A, 7B) and also improved speech (Video 1 – pre-prosthetic and Video 2 – post-prosthetic). A 6-month and 1-year follow-up showed the implants functioning normally with good bone and soft-tissue response (Figure 7C).
STM (U) AND TM (U) GROUPS (INTERIM/DEFINITIVE OBTURATOR):
The patients in these groups were initially treated with an interim obturator (Figure 6B, 6C) that was customized for each patient depending upon the defect. The interim obturator was worn by the patient for 3–6 months until the definitive obturator (Figure 6D) together with a cast partial denture framework was fabricated. For larger defects, the obturators were hollowed out to reduce the weight of the prosthesis [30]. All obturators followed standard recommended clinical/laboratory procedures for fabrication.
TMOE (U) TOTAL MAXILLECTOMY (UNILATERAL) WITH ORBITAL EXENTERATION:
The patients in this group were treated with an interim obturator for 3 months, followed by definitive obturator prosthesis that was either isolated or united with the maxillofacial component (maxillary, orbital, ocular). The ocular prosthesis in all cases was separate.
PSYCHOTHERAPEUTIC/PHARMACOTHERAPY INTERVENTION:
Patients who were diagnosed with high level of anxiety/depression at T0 (before prosthesis) were referred to a psychiatrist who was also a part of the multidisciplinary team. Depending upon the severity, different forms of psychotherapies were instituted at regular time intervals – psycho-educational (to improve self-knowledge), psychotherapeutic (individual counselling to teach coping skills and problem solving), and supportive (to build family support) [31]. The number of counselling sessions was kept small for individual counselling, while to improve family support there were group sessions organized during the study. Pharmacotherapy (benzodiazepine) was instituted only in severe cases of anxiety, monitored depending upon the case. No pharmacotherapy was instituted in cases of depression.
MEASURES, DATA EVALUATION, COLLECTION, AND ANALYSIS:
Demographic variables were collected in the form of categorical and numerical data. The anxiety associated with maxillectomy was assessed using the appearance anxiety inventory scale (AAI), a 10-question scale (self-reported) measuring body image anxiety (BIA) (cognitive and behavioral aspects) and body deformity disorder (BDD) [32]. The questionnaire was translated and back-translated into the local language (Hindi) followed by pilot testing and retesting on a validation sample (n=101) on a population (average age 43 years, male 58.2% and female 41.8%) that had been diagnosed with clinical BDD against a non-clinical community sample. Its convergent validity was good (0.62) with other clinical scales (0.59 with PHQ9). The internal consistency (Cronbach alpha 0.83) of the scale was also high upon retesting. Since the scale uses the patient’s own individual cognitive ability, the subjective opinion of others is eliminated. Assessment for BDD and the BIA is done under 2 subscales: avoidance (items 1, 3, 4, 7, 9, 10) and threat monitoring (items 2, 4, 6,8). For each item, the individual rates a frequency from 0 to 4 (score 0 – not at all; score 1 – Rarely; score 2 – Sometimes; score 3 – Often; score 4 – All the time), thus giving a possible range of summed scores from 0 to 40. Studies have shown that a mean score of 20 indicates high risk (diagnostic for BIA), and a score of 27 is confirmed for BDD [33]. Pilot test results (BIA – 20 to 26, BDD – 27 and above, post-therapy – 11 to 13, non-community sample 13.44] showed similar cut-off point values, which were retained in the study. All patients filled out the AAI at 4 different time intervals – T0: before prosthesis; T1: 2 weeks after delivery of respective prosthesis (obturator or zygomatic implant-supported prosthesis); T2: 6 months; and T3: 12 months.
Depression symptom severity was measured using the PHQ9 patient health questionnaire, which is a 9-item instrument (each item scored from 0 to 3, total possible severity score 0–27). The main feature of the scale is that it specifically assesses and monitors the severity of depression symptoms. For each item the score is given in ascending frequency: 0 – not at all, 1 – several days, 2 – more than half of days, and 3 – nearly every day (week). The degree of severity is assessed from the total scores of 5 (mild), 10 (moderate), 15 (moderately severe), and above 20 (severe), representing symptom grades [34]. PHQ9 is sensitive to change of condition severity (in this case, depressive symptoms) over treatment intervals, in addition to being used as an outcome-measuring tool to determine the need for treatment [35]. The severity level, thus allows a clinician to take prompt action in terms of whether additional psychotherapy (e.g., counselling) or pharmacotherapy is needed. Patients with mild and moderate levels generally need counselling and follow-up, while moderately severe and severe levels require active treatment with pharmacotherapy/psychotherapy. Pharmacotherapy is instituted only when there is a diagnosis of depressive disorder not associated with recent life experiences. This study protocol did not require to establish a depressive disorder/syndrome and the tool was used only to monitor depressive symptom severity.
STATISTICAL ANALYSIS:
All data were coded, corrected, and refined using Microsoft Excel spreadsheets, then the data were entered into SPSS version 24.0 (SPSS 24.0; SPSS, Inc., Chicago, Illinois, USA) for statistical analysis and testing. Demographic characteristics of the cohort were calculated in terms of quantitative frequencies, while interval ratio data were expressed as means and standard deviations. For AAI and PHQ9 scores, the mean values were calculated for each group, subgroups (males and females), and total cohort. Data for each group was first tested for distribution (normality) using the Kolmogorov-Smirnov test. The quantitative differences in means between the groups, subgroups, and total cohort for anxiety and depression were analyzed using one-way analysis of variance (ANOVA) (single-factor and Friedman), which were further corrected for probability distribution (unequal variance). A chi-square value (Friedman) was also derived that indicated how far the mean ranks lie apart in the data obtained. To assess statistically significant differences within the groups, post hoc tests (independent-sample
Results
DEMOGRAPHIC VARIABLES:
The demographic characteristics of the MM affected post-maxillectomy maxillofacial rehabilitation using either an obturator prosthesis or zygomatic implant-supported prosthesis are shown in Table 1. A total of 60 MM treated with maxillectomy/orbital exenteration represented the cohort with almost equal gender distribution (males 33, females 27). The mean age of the total cohort was 55.96±14.41 years, with 96% married and 66.6% living in rural areas, 78.3% were illiterate (Census of India, 2011), and 56.6% had low economic rank (Atlas method). Nine out of 60 patients did not have any underlying systemic condition. The mean duration of diabetics was 3.79 years, and 53.3% of the total cases were diagnosed as having Rhizopus arrhizus as the causative agent of ROCM.
ANXIETY (BIA, BDD) (INTER-GROUP/INTRA-GROUP):
The results show that patients who underwent unilateral maxillectomy and received obturator as treatment prosthesis had lower anxiety scores (range=22.17±1.16 to 27±1.58) than patients with bilateral maxillectomy (range=30.56±1.33 to 33.78±1.39) before rehabilitation treatment was initiated (T0) (Table 2). The highest anxiety scores at T0 (35.33±2.08) were among patients in the TMOE (U) group who had undergone orbital exenteration. At T1 (2 weeks), all groups showed a decline in anxiety scores, with the greatest decline observed in the TM(B) group. In the STM (B) and TM (B) groups, the mean anxiety scores were higher than in the STM (U) and TM (U) groups at time T0. In the STM (B) and TM (B) groups, the mean anxiety scores were higher than in the STM (U) and TM (U) groups at time T0. At 6 months (T2), nearly normal anxiety scores (0–19) were observed in all groups except for patients in TM(B) [M-20.6±1.57, F-22.67±2.06] and TMOE (U) [M-26.33±2.08] Gp. At the 1-year follow-up, all groups treated with either an obturator or zygomatic implants had achieved normal anxiety levels, except those in TMOE (U) [M-22.33±1.15] Gp, who still had scores that indicated high risk (BIA). For all the groups and their respective subgroups, the differences at various time intervals were found to be statistically significant (P≤0.05) (Table 2). Post hoc test results after multiple comparisons between groups and subgroups are shown in Table 3. The results show where the differences between various time intervals occurred. The anxiety scores when compared between T0 and T1 showed significant differences for Gp STM(U) (both subgroups), STM(B) (both subgroups), and TM(U) (subgroup male only). Significant differences in Gp TM(U) were observed in comparisons at all time intervals except comparison at T2–T3 (male subgroup) and T0–T1(female subgroup).
DEPRESSION SEVERITY SYMPTOMS) (INTER-GROUP/INTRA-GROUP):
This instrument indicates depression severity that is diagnostic for either initiating psychotherapy and/or pharmacotherapy, depending on the level of depression of an individual. The results of this study show that at T0 the patients in STM (U) and TM (U) groups had moderate depression levels (range 10.5±1.60 to 12.8±1.63), as compared to severe depression of patients in the bilateral maxillectomy groups (range 20.11±2.14 to 21.33±1.80) (Table 2). At T1 (2 weeks) the mean levels of depression were higher than at T0 among all the groups and subgroups, with 3 of the groups [STM(B), TM (B) and TMOE (U)] having mean scores above 20 (severe depression). At T2 (6 months), however, there was a decline in the severity of depression symptoms, which had shifted from severe to moderate [STM(B) males (22.11±1.61 to 13.88±1.26), or moderately severe [STM(B) females (21.6±1.67 to 16.8±1.48); TM(B) both males (21.9±1.44 to 14.7±2.05) and females (23.0±1.32 to 14.22±1.78)]. At a similar stage of treatment, the patients in the TMOE (U) group still had severe depression (20.0±1.73) (males). Lower mean scores for depression severity were observed in STM(U) and TM(U) groups/subgroups at all time intervals as compared to STM(B) and TM(B) Groups/subgroups. At T3 (1 year) the overall mean score levels of depression had further reduced to mild (5 to 9), while the patients in TMOE (U) continued to have moderately severe depression (20.0±1.73 to 17.33±2.08) (Table 2). For all the groups and their respective subgroups, the differences at various time intervals were found to be statistically significant (P≤0.05). Post hoc tests showed the differences to be significant across various time intervals (Table 3).
ANXIETY (BIA, BDD) AND DEPRESSION SEVERITY SYMPTOMS OF TOTAL COHORT:
The comparative differences in means for anxiety and depression severity scores at various time intervals and between males and females are shown in Table 3 (post hoc test results). The total cohort results showed a decline in anxiety levels after maxillofacial rehabilitation. The mean anxiety of the total cohort was highest at T0 (29.13±4.72), which reduced at T1 (24.81±3.86) and T2 (19.88±3.36) at various treatment stages. The differences at various time intervals were statistically significant, with differences being observed across all comparisons (Table 3). For the total cohort, the differences in the mean anxiety scores were lower at T0–T1 and T2–T3 than at other time intervals, and the same observation was also seen in both genders. The mean scores for depression severity in the total cohort was higher at T1 than at other time intervals. The overall depression level at the beginning of the treatment was moderately severe (16.81±4.89), while at T2 and T3, it reduced to 12.0±4.43 and 7.38±3.37, respectively. The differences between time intervals for the total cohort were also statistically significant (P≤0.05). Multiple comparison testing (Table 3) showed less difference in initial treatment stages (T0–T1), and showed a significant increase at other comparisons. The overall differences in mean anxiety scores and depression severity among various treatment groups between males and females are presented in Figures 8 and 9, respectively. The reduction in anxiety levels among both genders followed a uniform pattern with all subgroups, except for TM(B), which returned to normal level within 6 months in males and 1 year in females. For depression severity, there is an initial increase in depression levels at T1 in both genders, followed by reduction at T2 and T3. Males in both unilateral maxillectomy groups (TM and STM) achieved normal levels earlier than females.
Discussion
COVID-19-ASSOCIATED MUCORMYCOSIS COHORT (DEMOGRAPHIC CHARACTERISTICS):
The 60 ROCM maxillectomy patients in this study included 33 males and 27 females with an average age 55.96 years, which validates previous independent studies [10]. The higher percentage of the patients in this cohort were married (96%), illiterate (78%), low economic rank (56%), and from rural areas (66%), which fall within the ranges for previous epidemiologic and intervention studies [7,8,10]. We found that 15% of the patients did not have any underlying systemic condition, indicating that MM can also affect immunocompetent individuals, which agrees with the results reported by Sridhara et al [36]. Patient records revealed Rhizopus arrhizus caused 53% of the ROCM cases, and Apophysomyces variabilis caused 25%. Earlier reports have specified these 2 pathogens as most common and in the same order [7,10,36]. These species are not dematiaceous fungi, which actually cause black fungus; therefore, the term black fungus is incorrect as it only depicts the clinical picture [37]. Post-COVID-19 ROCM in the Indian subcontinent was found to be strongly associated with systemic corticosteroid therapy in untreated and diabetes (de novo) patients [10]. The patient’s previous medical records in this study also pointed to the use of systemic corticosteroids during their routine treatment of COVID-19. The distressing surge of COVID-19-associated ROCM in India as compared to rest of the world, despite the same treatment protocols, has been attributed to patients not being tested for blood glucose (due to overcrowding of hospital out-patients) [10], increased dexamethasone dose (6.0 mg/day for 5–10 days) to control cytokine storm [7,37], higher outdoor ubiquitous spore load in the air, and patients developing diabetes after contracting COVID-19 (damage to pancreatic beta cells by coronavirus) [37]. ROCM is the most common form of COVID-19-associated MM and has better treatment outcomes than CAM of other sites if early diagnosis and prompt correct treatment occur [13]. Radiographic investigation that reveals mucosal thickening (sinus lining), opaque sinus, brain edema, or inflammation are highly predictive of ROCM [5,11]. The rapid spread of MM is the direct result of endothelial cell adhesion and penetration of the vascular system [11,37]. Evaluation of maxillary bone using either a CT scan or, preferably, an MRI in the early stage has been found to limit the spread [38]. Routine treatment for ROCM has been to first treat any emergency (reduce risk factors), followed by surgical intervention removing all damaged organ/tissue, and anti-fungal pharmacotherapy [13,37].
TREATMENT INTERVENTIONS IN THE COHORT:
All patients in this study had undergone maxillectomy, and depending upon the extent, interventions were initiated. Subtotal and total maxillectomy that is unilateral create oro-nasal communication, for which the treatment of choice is an obturator (implant or natural teeth retained). In total, 27 patients [14 males, 15 females] were treated using an interim and definitive obturator according to the individual requirements of each case. The remaining 33 patients [19 males, 14 females] were treated using a zygomatic implant-supported prosthesis. Zygomatic implants for maxillary defects have high survival rates (77–100% at 10-year follow-up) [39], irrespective of their timing of placement (primary or secondary) [40]. The use of conventional endosseous implants in maxillectomy requires maxillary reconstruction using bone grafts, which have disadvantages like donor site morbidity, graft resorption, high cost, and additional surgery [39]. Occlusal forces generated in the zygomatic implant-supported prosthesis have better and wider distribution than conventional implants. The wide and long threads at the apex of zygomatic implants further enhance wider distribution in addition to the splinting (Toulouse leg screw) with diverse thread and core diameters [41]. Biocompatibility of implants with acceptable biological seal due to the smooth surface (with less chances of developing peri- implantitis) makes them ideal for long-term maxillofacial rehabilitation.
ANXIETY (BIA AND BDD):
The results show that for unilateral maxillectomy cases (total and subtotal), the mean anxiety scores were lower than for bilateral maxillectomy cases at baseline T0. The results can be explained by the different characteristics of disfigurement and different treatment plans required. Patients with unilateral maxillectomy had less facial disfigurement while those with bilateral maxillectomy had obvious, distressing facial disfigurements. Visible disfigurement has a more consistent relationship between severity and degree of body image dissatisfaction [42] and higher levels of anxiety and depression [43]. Since our study evaluated the 2 psychological variables at T0 (before prosthesis), the additional surgery for zygomatic implants could also cause higher anxiety in the TM (B) and STM (B) groups. Additionally, at the stage of anxiety measurement of this study, the surgical impairment had already healed, and the bilateral maxillectomy patient’s high anxiety could also be due to social detachment, which is inherent in such cases [44], dysfunctional mastication, and impaired speech [45]. Generally, patients who require dental treatment have also been found to be highly anxious. The results of this study demonstrate reduction in anxiety levels between T0 and T1 for the total cohort and within groups and subgroups. Between time intervals, post hoc testing showed that the reduction in anxiety from T0 to T1 was lower in all groups as compared to other comparisons (Table 3). Among other comparisons, the differences were significant between various time intervals (Table 3). Anxiety was further reduced from T1 to T2 and to T3 for the total cohort. A study by Srivastava et al, investigating suspect and confirmed COVID-19-associated mucormycosis reported significant anxiety levels in all subjects [46], which was also related to surgical intervention.
A significant reduction from T0 to T1 (total cohort and groups) indicates that anxiety could be associated with loss of functions (mastication and speech) and facial esthetics. Impaired speech has psychosocial consequences which directly and indirectly affect one’s social life [46]. The change associated with speech improvement can be appreciated from the exemplary video (Video 1 – pre-prosthetic and Video 2 – post-prosthesis). The significant differences between various time intervals show that improvements in anxiety control take place over time after maxillofacial rehabilitation, thus agreeing with previous research results [47]. The patient’s facial features, especially lips support improvement, was observed in all the cases except selected cases of unilateral subtotal maxillectomy in which the soft-tissue changes were minimal. Maxillary defects have been reconstructed using various approaches (surgical, prosthetic, implants), and among various approaches studies have reported that zygomatic implant-supported prosthesis increased patients’ ability to engage in recreation and activities [48]. Anxiety levels in individuals fluctuate and are dependent on multiple factors, including the type (generalized anxiety disorder, post-traumatic stress disorder, panic disorder) and are time-dependent [49]. Likewise, treatment-related anxieties also differ, especially in ROCM patients, who have a higher anxiety level before ROCM surgery due to the condition being life-threatening [48]. Cancer studies have reported similar anxiety patterns before and after surgery [39,44]. At the time of maxillofacial rehabilitation, the anxiety about survival is substituted by anxiety about being disfigured. Improved self-esteem and confidence levels after prosthetic rehabilitation with orbital prosthesis are well known [50]. Our results show that anxiety levels were time-dependent and decreased as the treatment proceeded, irrespective of the type of the prosthesis. Similar results have been obtained in a wide array of studies in various medical and dental specialties [44,48]. Diagnosis in such cases is important because the treatment to control such anxiety is different. Even if the anxiety levels may indicate the anxiety represents diagnosis of a disorder, the management is through behavior therapy rather than pharmacotherapy [51]. The results of the total cohort subgroups (males and females) show that although both genders had similar anxiety levels at baseline T0 (M-29.63±4.66; F-29.22±4.87), the decrease in levels differed after time interval T2 (6 months). The anxiety level in males (18.63±3.63) had normalized by 6 months, while it was still high in females (20.66±2.64). This indicates that males overcome treatment anxiety faster than females. These results further validate previous studies done on gender differences in anxiety prevalence and ability to overcome them [52].
DEPRESSION SEVERITY:
The results of the total cohort/groups/subgroups indicate that patients at baseline T0 had moderately severe depression levels [16.81±4.89], with increased value at T1 without any change in severity. The increased values can be due to the fact that the patients were still in the adaptation phase for prosthesis, which itself is a difficult process. Our results support the findings obtained in patients wearing a prosthetic limb after amputation, who also reported higher depression levels during adaptation [53]. For all groups in the cohort, the patients had to learn a new way of performing routine functions (mastication, speech). Patients may not realize the level of loss until they start performing these functions with the prosthesis. Adaptation to any type of dental prosthesis is complex and cumbersome, more so for those who neglect post-insertion instructions given to them when they received the prosthesis [54]. The depression severity levels at T2 (6 months) for the total cohort/group/subgroups had decreased in mean values and severity level (moderately severe to moderate). Within the groups, the depression levels were higher in both bilateral maxillectomy groups as compared to the unilateral maxillectomy group. These results agree with studies comparing depression level differences between radical and conservative maxillectomy, which concluded that radical maxillectomy had greater impacts on depression at 18 months [55]. In both bilateral maxillectomy groups, the normal levels of depression (none 0 to 4 or mild 5 to 9) were observed at 1-year intervals as compared to 6-month intervals for the unilateral maxillectomy group. The recovery is subjective and depends on many factors that are interrelated. Generally, the patients who have suffered from COVID-19 have been observed to recover after a minimum period of 1 year (26%) [55]. Reduction in depression levels and improvement in life quality have also been attributed to the kind of treatment prosthesis that is chosen for maxillectomy patients [56]. Patients in both bilateral maxillectomy groups were treated using a zygomatic implant-supported prosthesis, which was rated betterer than treatment with reconstruction flaps [57]. Reconstruction flaps are generally associated with scar tissue formation, which constantly reminds the individual of the related ordeal [56]. The results of our study also show that between 2 treatment modalities of the obturator and zygomatic implants, the reduction of depression severity from T0 (20.48±1.87) to T3 (8.01±2.33) (n=33) was observed in patients treated with zygomatic implants as compared to T0 (11.33±1.97) to T3 (5.29±1.80) (n=24) in patients with the obturator. These results indicate that zygomatic implants have better compliance than obturators, but the deformities were characteristically different with different individual challenges. When comparing implant-supported obturators to implant-supported fixed prosthesis, Wang et al found no difference between the 2, but concluded obturator patients had poorer mental health than those who had fixed prosthesis [58]. Differences between males and females in depression severity shows similar mean values and clinical grades of depression, which are contradictory to the general opinion of gender differences for depression [59]. However, the difference is due to 4 different subgroups in the gender-based cohort, which show different mean levels of depression at baseline that were dependent upon the extent of facial deformity.
STRENGTH AND LIMITATIONS OF THE STUDY:
The cohort studied represents a distinguished presentation of different groups and subgroups with the limitation being the small sample size in each group. Modern digital technology used in intervention for zygomatic implants reduces the clinical- and laboratory-associated errors during implant placement and prosthesis fabrication. The strength of the study also includes the psychotherapeutic intervention done with high levels of anxiety and depression, while the limitation of the intervention is that one cannot isolate the influence of such an intervention. Other limitations include that the study was short-term, and long-term results will be necessary to conclude the overall influence of both interventions. Limitations that are associated with selecting a cross-sectional sample are inherent for this study.
CLINICAL IMPLICATIONS:
Maxillofacial rehabilitation using treatment modalities of the obturator and zygomatic implants reduces anxiety levels and severity of depression over a period of time. During the rehabilitation process, the clinical diagnosis of both anxiety and depression levels is mandatory to initiate psychotherapy or pharmacotherapy to minimize the influence of anxiety and depression upon the long-term treatment outcome.
Conclusions
COVID-19-associated ROCM is a life-threatening fungal infection with high mortality if treated late. The standard proven treatment is surgical intervention (FESS) that requires removal of maxillary bone on one or both sides. After maxillectomy, the facial disfigurement is associated with high levels of anxiety and depression. Prosthodontic rehabilitation using an obturator for unilateral maxillectomy and zygomatic implants for bilateral maxillectomy is associated with reduction of anxiety and depression levels, irrespective of gender.
Figures
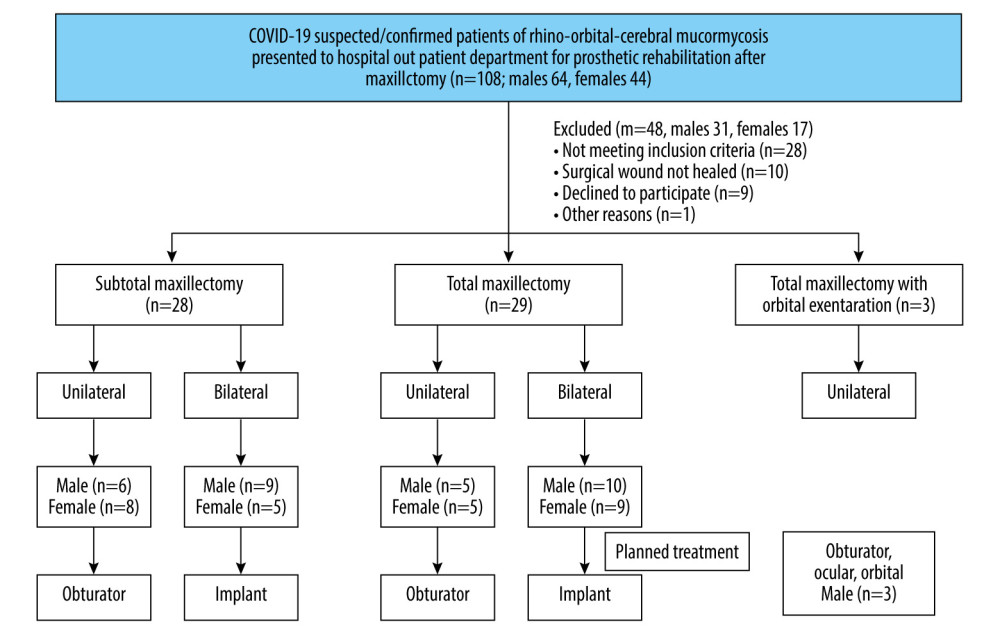 Figure 1. Flow chart showing the sample selection and distribution process. Compiled Figure created using MS PowerPoint, version 20H2 (OS build 19042,1466), Windows 11 Pro, Microsoft Corporation).
Figure 1. Flow chart showing the sample selection and distribution process. Compiled Figure created using MS PowerPoint, version 20H2 (OS build 19042,1466), Windows 11 Pro, Microsoft Corporation). 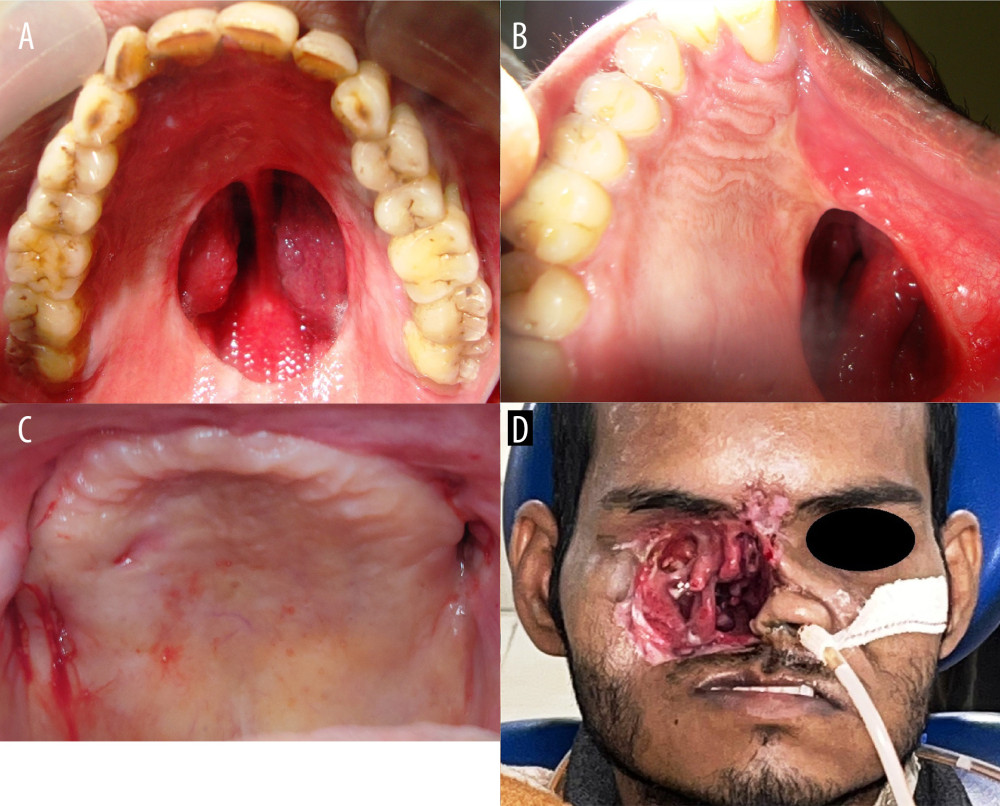 Figure 2. Exemplary cases involved in the study. (A) Subtotal maxillectomy bilateral (STM-B); (B) Total maxillectomy unilateral (STM-U) (note the depressed face on that side); (C) Total maxillectomy bilateral (TM-B) (note there is no hard palate on either side, the flap raised and then put back to prevent oro-nasal communication); (D) total maxillectomy with orbital exenteration unilateral (TMOE-U). Photographs taken using digital single-lens reflex (DSLR) camera (Canon EOS 700D) with 100 mm macro lens) with/without ring flash. Compiled Figure created using MS PowerPoint, version 20H2 (OS build 19042,1466), windows 11 Pro, Microsoft Corporation).
Figure 2. Exemplary cases involved in the study. (A) Subtotal maxillectomy bilateral (STM-B); (B) Total maxillectomy unilateral (STM-U) (note the depressed face on that side); (C) Total maxillectomy bilateral (TM-B) (note there is no hard palate on either side, the flap raised and then put back to prevent oro-nasal communication); (D) total maxillectomy with orbital exenteration unilateral (TMOE-U). Photographs taken using digital single-lens reflex (DSLR) camera (Canon EOS 700D) with 100 mm macro lens) with/without ring flash. Compiled Figure created using MS PowerPoint, version 20H2 (OS build 19042,1466), windows 11 Pro, Microsoft Corporation). 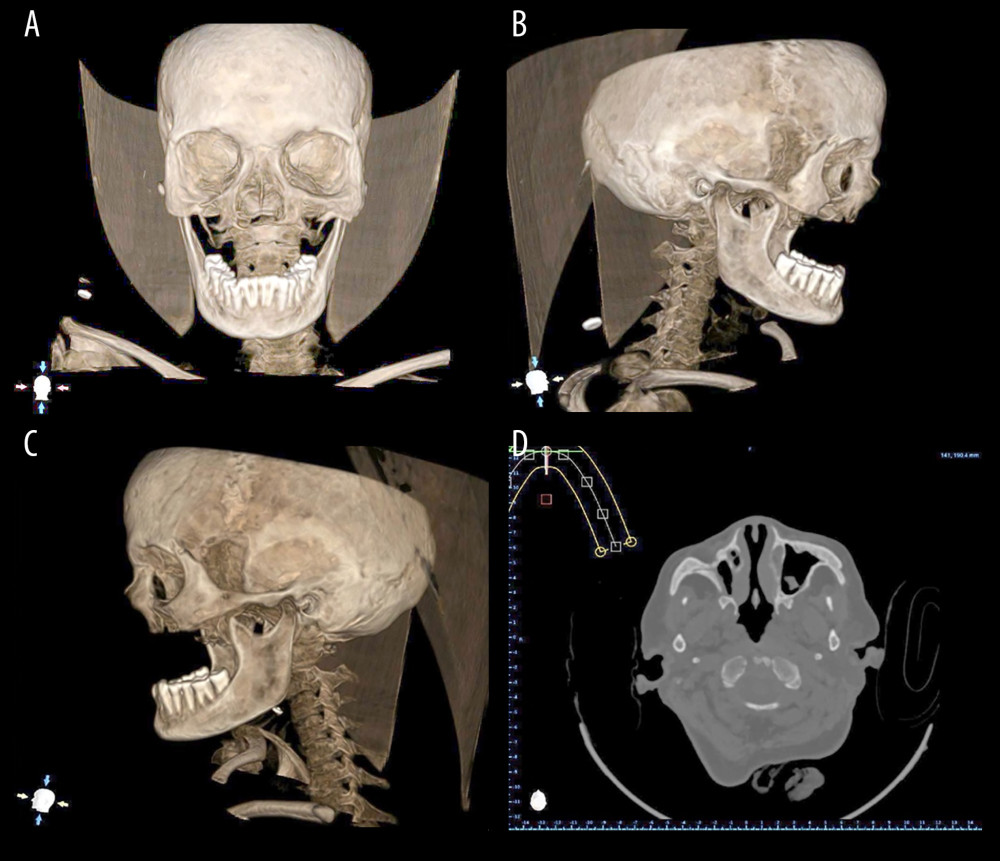 Figure 3. Diagnostic computed tomographic (CT scan) images of exemplary patient with bilateral maxillectomy. (A) Frontal view (note the maxillectomy extent); (B) Left lateral view; (C) Right lateral view; (D) Radiographic image during analysis. Photographs taken using digital single-lens reflex (DSLR) camera (Canon EOS 700D) with 100 mm macro lens) with/without ring flash. Compiled Figure created using MS PowerPoint, version 20H2 (OS build 19042,1466), windows 11 Pro, Microsoft Corporation).
Figure 3. Diagnostic computed tomographic (CT scan) images of exemplary patient with bilateral maxillectomy. (A) Frontal view (note the maxillectomy extent); (B) Left lateral view; (C) Right lateral view; (D) Radiographic image during analysis. Photographs taken using digital single-lens reflex (DSLR) camera (Canon EOS 700D) with 100 mm macro lens) with/without ring flash. Compiled Figure created using MS PowerPoint, version 20H2 (OS build 19042,1466), windows 11 Pro, Microsoft Corporation). 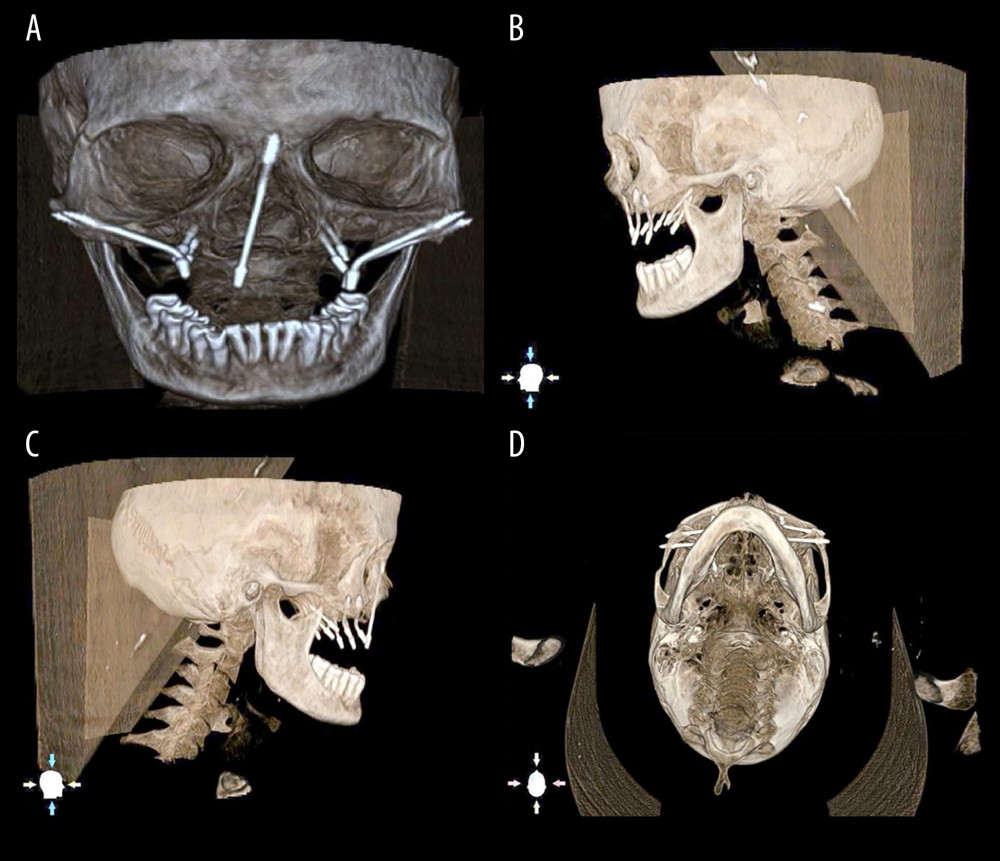 Figure 4. Different length zygomatic implant determination and placement on virtual DICOM (Digital Imaging and Communications in Medicine). (A) Frontal view; (B) Left lateral view; (C) right lateral view; (D) basal view. Note the length of the screw heads at the bone – implant interface level. Photographs taken using digital single-lens reflex (DSLR) camera (Canon EOS 700D) with 100 mm macro lens) with/without ring flash. Compiled Figure created using MS PowerPoint, version 20H2 (OS build 19042,1466), Windows 11 Pro, Microsoft Corporation).
Figure 4. Different length zygomatic implant determination and placement on virtual DICOM (Digital Imaging and Communications in Medicine). (A) Frontal view; (B) Left lateral view; (C) right lateral view; (D) basal view. Note the length of the screw heads at the bone – implant interface level. Photographs taken using digital single-lens reflex (DSLR) camera (Canon EOS 700D) with 100 mm macro lens) with/without ring flash. Compiled Figure created using MS PowerPoint, version 20H2 (OS build 19042,1466), Windows 11 Pro, Microsoft Corporation). 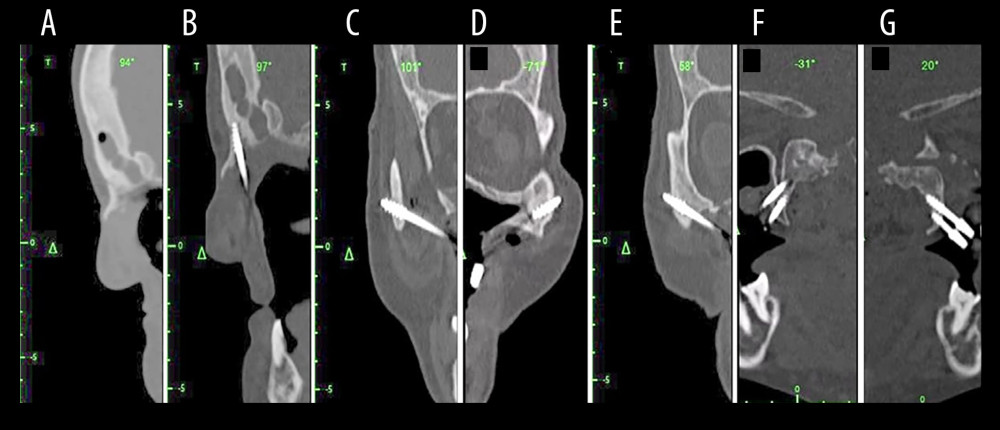 Figure 5. Preoperative display of the surgical planning for an exemplary maxillectomy patient planned to receive zygomatic implant on the navigation monitor. (A, B) Sagittal view before and after implant placement (C, D) on the left and right zygomatic bones (E–G) other views of planned areas. Photographs taken using a digital single-lens reflex (DSLR) camera (Canon EOS 700D) with 100 mm macro lens) with/without ring flash. Compiled Figure created using MS PowerPoint, version 20H2 (OS build 19042,1466), Windows 11 Pro, Microsoft Corporation).
Figure 5. Preoperative display of the surgical planning for an exemplary maxillectomy patient planned to receive zygomatic implant on the navigation monitor. (A, B) Sagittal view before and after implant placement (C, D) on the left and right zygomatic bones (E–G) other views of planned areas. Photographs taken using a digital single-lens reflex (DSLR) camera (Canon EOS 700D) with 100 mm macro lens) with/without ring flash. Compiled Figure created using MS PowerPoint, version 20H2 (OS build 19042,1466), Windows 11 Pro, Microsoft Corporation). 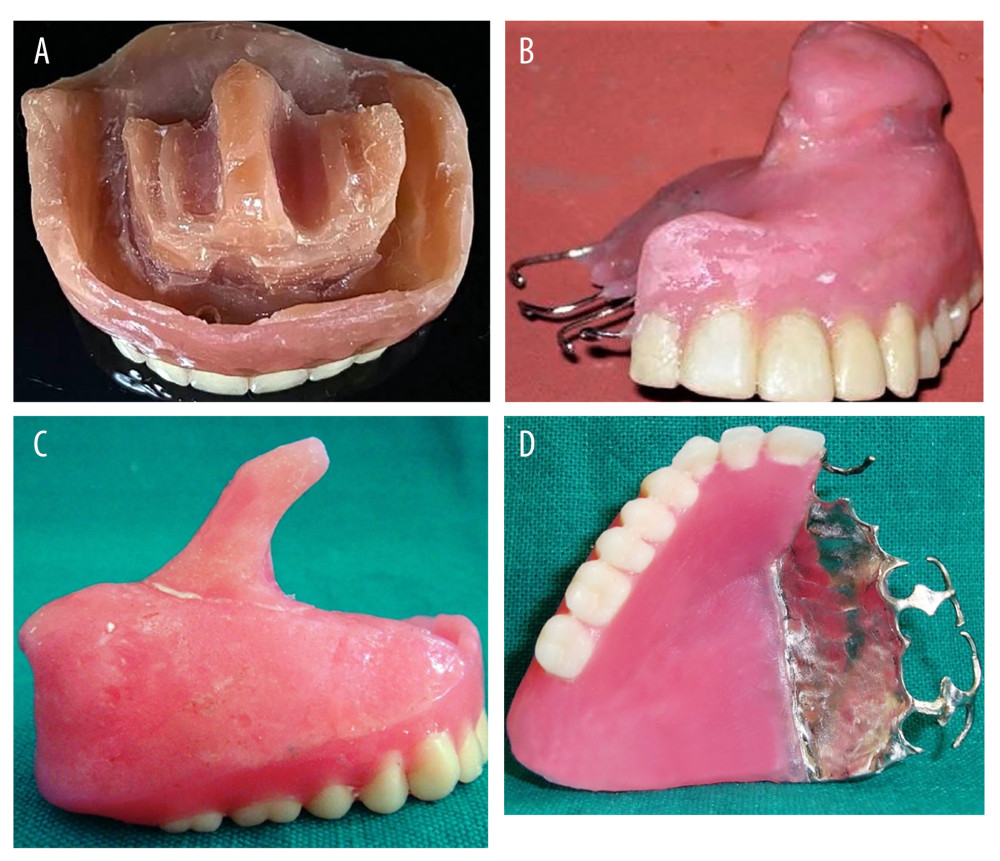 Figure 6. Types of prosthesis used in the total cohort. (A) Zygomatic implant-supported fixed complete denture prosthesis; (B) Interim obturator for unilateral total maxillectomy; (C) Interim obturator for subtotal maxillectomy; (D) Definitive prosthesis for total and subtotal maxillectomy cases. Photographs taken using a digital single-lens reflex (DSLR) camera (Canon EOS 700D) with 100 mm macro lens) with/without ring flash. Compiled Figure created using MS PowerPoint, version 20H2 (OS build 19042,1466), Windows 11 Pro, Microsoft Corporation).
Figure 6. Types of prosthesis used in the total cohort. (A) Zygomatic implant-supported fixed complete denture prosthesis; (B) Interim obturator for unilateral total maxillectomy; (C) Interim obturator for subtotal maxillectomy; (D) Definitive prosthesis for total and subtotal maxillectomy cases. Photographs taken using a digital single-lens reflex (DSLR) camera (Canon EOS 700D) with 100 mm macro lens) with/without ring flash. Compiled Figure created using MS PowerPoint, version 20H2 (OS build 19042,1466), Windows 11 Pro, Microsoft Corporation).  Figure 7. (A) Preoperative facial appearance of an exemplary patient showing facial aesthetics before prosthodontic rehabilitation; (B) Postoperative facial aesthetics with patient smiling; (C) 1 year follow-up orthopantomogram showing the zygomatic implant well received by the bone. Photographs taken using a digital single-lens reflex (DSLR) camera (Canon EOS 700D) with 100 mm macro lens) with/without ring flash. Compiled Figure created using MS PowerPoint, version 20H2 (OS build 19042,1466), Windows 11 Pro, Microsoft Corporation).
Figure 7. (A) Preoperative facial appearance of an exemplary patient showing facial aesthetics before prosthodontic rehabilitation; (B) Postoperative facial aesthetics with patient smiling; (C) 1 year follow-up orthopantomogram showing the zygomatic implant well received by the bone. Photographs taken using a digital single-lens reflex (DSLR) camera (Canon EOS 700D) with 100 mm macro lens) with/without ring flash. Compiled Figure created using MS PowerPoint, version 20H2 (OS build 19042,1466), Windows 11 Pro, Microsoft Corporation). 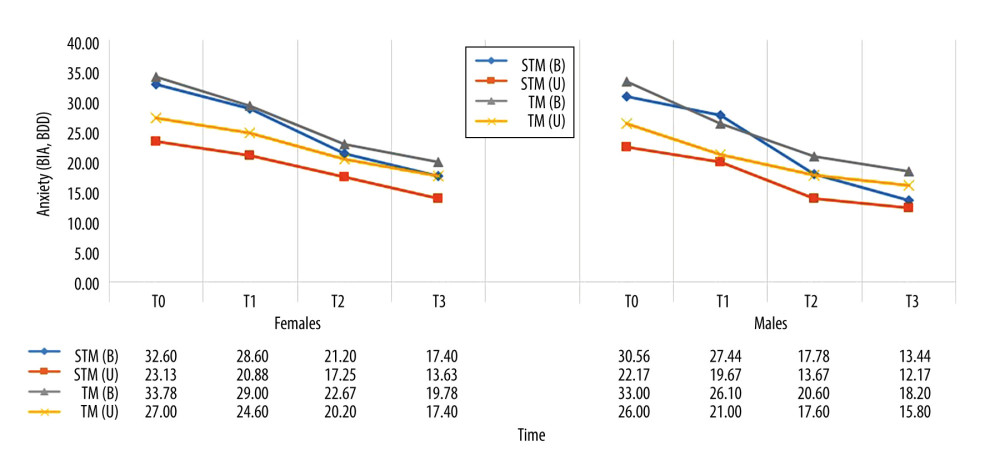 Figure 8. Comparative gender differences in mean values of appearance anxiety score among different maxillectomy types at different time intervals. Figure created using MS Excel spreadsheet, version 20H2 (OS build 19042,1466), Windows 11 Pro, Microsoft Corporation).
Figure 8. Comparative gender differences in mean values of appearance anxiety score among different maxillectomy types at different time intervals. Figure created using MS Excel spreadsheet, version 20H2 (OS build 19042,1466), Windows 11 Pro, Microsoft Corporation). 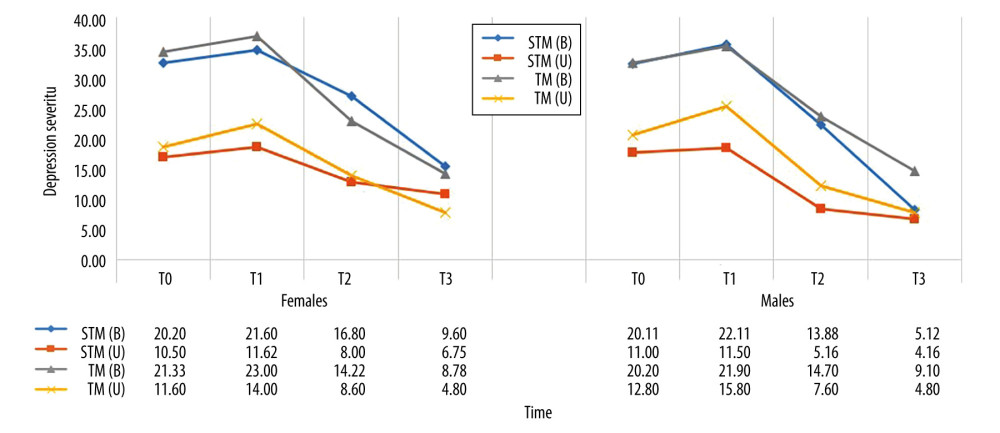 Figure 9. Comparative gender differences in mean values of severity of depression symptoms score among different maxillectomy types at different time intervals. Figure created using MS Excel spreadsheet, version 20H2 (OS build 19042,1466), Windows 11 Pro, Microsoft Corporation).
Figure 9. Comparative gender differences in mean values of severity of depression symptoms score among different maxillectomy types at different time intervals. Figure created using MS Excel spreadsheet, version 20H2 (OS build 19042,1466), Windows 11 Pro, Microsoft Corporation).  Video 1. Pre-rehabilitation speech. Video recorded using a digital single-lens reflex (DSLR) camera (Canon EOS 700D).
Video 1. Pre-rehabilitation speech. Video recorded using a digital single-lens reflex (DSLR) camera (Canon EOS 700D).  Video 2. Post-rehabilitation speech. Video recorded using a digital single-lens reflex (DSLR) camera (Canon EOS 700D).
Video 2. Post-rehabilitation speech. Video recorded using a digital single-lens reflex (DSLR) camera (Canon EOS 700D). Tables
Table 1. Demographic characteristics of the mucormycosis affected subjects seeking prosthodontic and maxillofacial rehabilitation post functional endoscopic sinus surgery with maxillectomy/exenteration of the eye.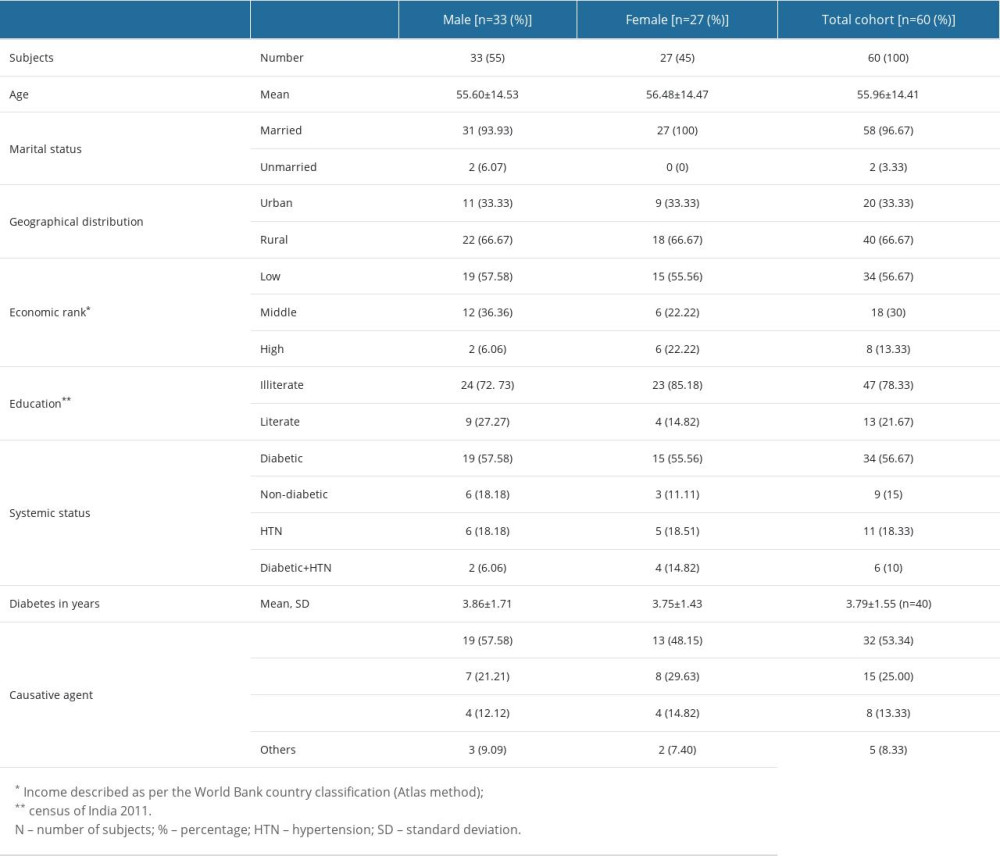 Table 2. Comparative differences in mean values of Appearance Anxiety (AAI) and Depression Scale (PHQ-9) between various maxillectomy/treatment groups/subgroups at 4 treatment time intervals.
Table 2. Comparative differences in mean values of Appearance Anxiety (AAI) and Depression Scale (PHQ-9) between various maxillectomy/treatment groups/subgroups at 4 treatment time intervals.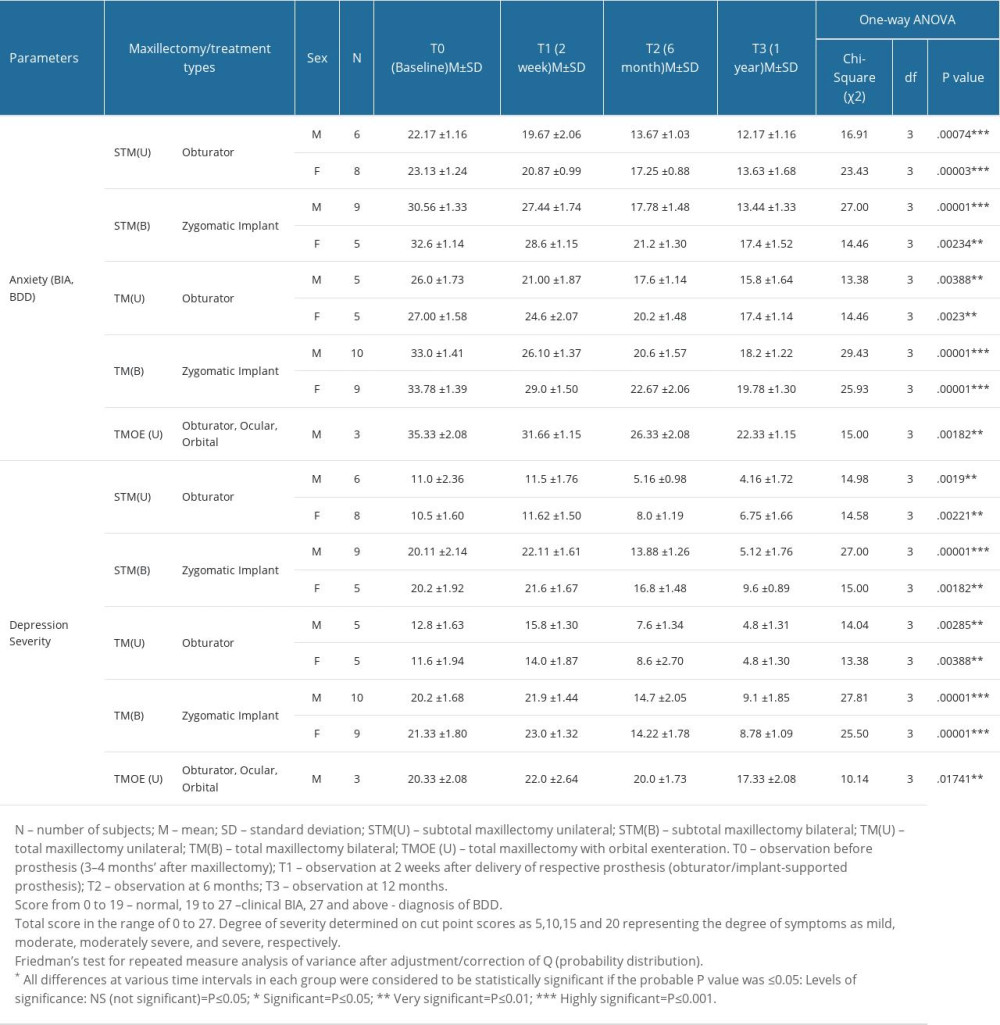 Table 3. Post hoc test showing comparative differences at various treatment time intervals among groups/subgroups for Appearance Anxiety (AAI) and Depression Scale (PHQ-9).
Table 3. Post hoc test showing comparative differences at various treatment time intervals among groups/subgroups for Appearance Anxiety (AAI) and Depression Scale (PHQ-9).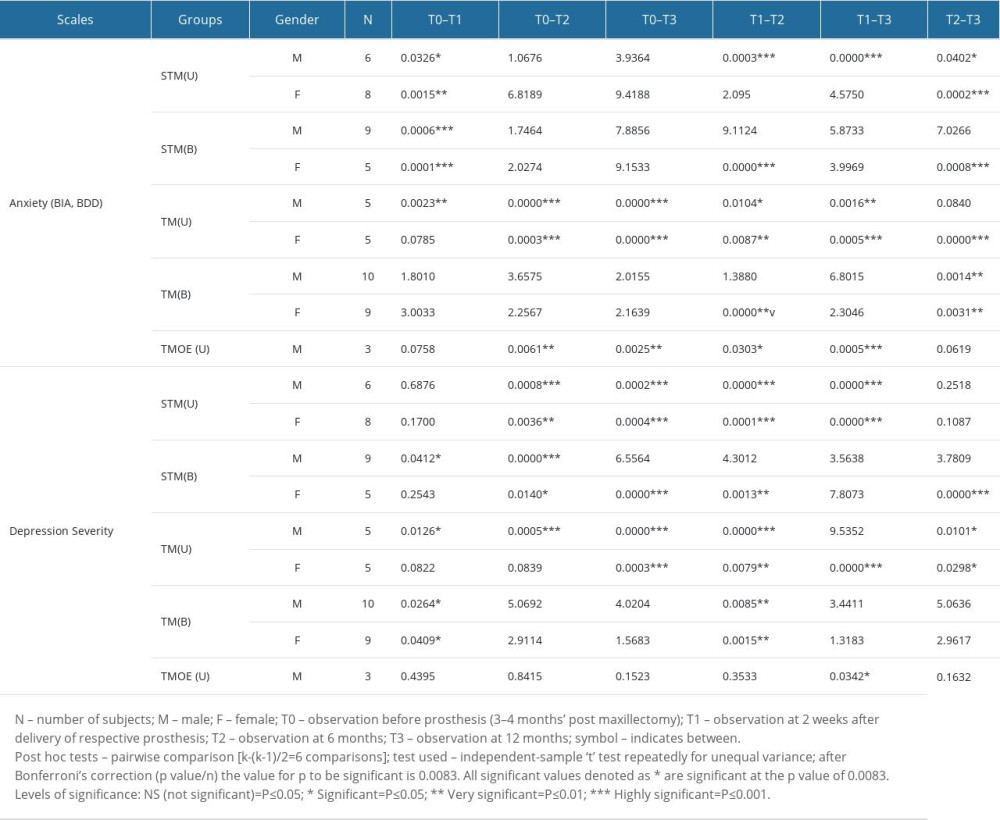
References
1. , WHO chief warns of future pathogens with ‘even deadlier potential; than COVID-19: CBS news Available at https://www.foxnews.com/health/who-chief-future-pathogens-deadlier-potential-covid
2. Charles NE, Strong SJ, Burns LC, Increased mood disorder symptoms, perceived stress, and alcohol use among college students during the COVID-19 pandemic: Psychiatry Res, 2021; 296; 113706
3. Christiansen J, Lund R, Qualter P, Loneliness, social isolation, and chronic disease outcomes: Ann Behav Med, 2021; 55(3); 203-15
4. Meng H, Xu Y, Dai J, Analyze the psychological impact of COVID-19 among the elderly population in China and make corresponding suggestions: Psychiatry Res, 2020; 289; 112983
5. Agarwala P, Bhargava A, Gahwai DK, Epidemiological characteristics of the COVID-19 Pandemic during the first and second waves in Chhattisgarh, Central India: A comparative analysis: Cureus, 2022; 14(4); e24131
6. , Mucormycosis: India records more than 4,300 “black fungus” deaths: BBC News Published July 21, 2021https://www.bbc.com/news/world-asia-india-57897682
7. Patel A, Kaur H, Xess I, A multicentre observational study on the epidemiology, predisposing factor, management and outcomes of mucormycosis in India: Clin Microbiol Infect, 2020; 26; 944e9-944.e15
8. Muthu V, Rudramurthy SM, Chakrabarti A, Agarwal R, Epidemiology and pathophysiology of COVID-19-associated mucormycosis: India versus the rest of the world: Mycopathologia, 2021; 186(6); 739-54
9. Maini A, Tomar G, Khanna D, Sino-orbital mucormycosis in a COVID-19 patient: A case report: Int J Surg Case Rep, 2021; 82; 105957
10. Sen M, Honavar SG, Bansal R, Epidemiology, clinical profile, management, and outcome of COVID-19-associated rhino-orbital-cerebral mucormycosis in 2826 patients in India – Collaborative OPAI-IJO Study on Mucormycosis in COVID-19 (COSMIC), Report 1: Ind J Ophthalmol, 2021; 69(7); 1670
11. Jose A, Singh S, RoyChoudhury A, Current understanding in the pathophysiology of SARS-CoV-2-associated rhino-orbito-cerebral mucormycosis: A comprehensive review: J Maxillofac Oral Surg, 2021; 20(3); 373-80
12. Oh WS, Roumanas E, Dental implant-assisted prosthetic rehabilitation of a patient with a bilateral maxillectomy defect secondary to mucormycosis: J Prosthet Dent, 2006; 96; 88-95
13. Groll AH, Pana D, Lanternier F: Lancet Oncol, 2021; 22(6); e254-69
14. Mahalaxmi I, Jayaramayya K, Venkatesan D, Mucormycosis: An opportunistic pathogen during COVID-19: Environ Res, 2021; 201; 111643
15. Mattoo K, Singh M, Rahman S, Rehabilitation of disfigurement associated with maxillectomy by a cheek plumper prosthesis: Am J Med Case Rep, 2014; 2(10); 200-3
16. Kumari A, Rao NP, Patnaik U, Management outcomes of mucormycosis in COVID-19 patients: A preliminary report from a tertiary care hospital: Med J Armed Forces India, 2021; 77; S289-95
17. Diwakar J, Samaddar A, Konar SK, First report of COVID-19-associated rhino-orbito-cerebral mucormycosis in pediatric patients with type 1 diabetes mellitus: Med Mycol J, 2021; 31(4); 101203
18. Fava M, Rush AJ, Alpert JE, Difference in treatment outcome in outpatients with anxious versus non-anxious depression: A STAR* D report: Am J Psychiatry, 2008; 165(3); 342-51
19. Kotov R, Krueger RF, Watson D, The Hierarchical Taxonomy of Psychopathology (HiTOP): A dimensional alternative to traditional nosologies: J Abnorm Psychol, 2017; 126(4); 454
20. Garjani A, Middleton RM, Nicholas R, Evangelou N, Recovery from COVID-19 in multiple sclerosis: A prospective and longitudinal cohort study of the United Kingdom Multiple Sclerosis Register: Neurol Neuroimmunol Neuroinflamm, 2021; 9(1); e1118
21. Wolf S, Seiffer B, Zeibig JM, Is physical activity associated with less depression and anxiety during the COVID-19 pandemic? A rapid systematic review: Sports Med, 2021; 51(8); 1771-83
22. Srivastava S, Beri N, Das GK, the psychological impact of rhino-orbital mucormycosis during the second wave of COVID-19 pandemic from South East Asian country: Cureus, 2023; 15(2); e35349
23. Costanza A, Vasileios C, Ambrosetti J, Demoralization in suicide: A systematic review: J Psychosom Res, 2022; 157; 110788
24. Hedberg L, Ekman U, Nordin LE, Cognitive changes and neural correlates after oral rehabilitation procedures in older adults: A protocol for an interventional study: BMC Oral Health, 2021; 21(1); 297
25. Brown JS, Rogers SN, McNally DN, Boyle M, A modified classification for the maxillectomy defect: Head Neck, 2000; 22(1); 17-26
26. Okay DJ, Genden E, Buchbinder D, Urken M, Prosthodontic guidelines for surgical reconstruction of the maxilla: A classification system of defects: J Prosthet Dent, 2001; 86(4); 352-63
27. Al Makramani BMA, Al Sanabani F, Mattoo KA, Reviewing infection control in prosthodontic practice with a case of herpes simplex in the times of a coronavirus pandemic: Ann Rom Soc Cell Biol, 2021; 25(6); 10898-904
28. Mattoo KA, Jain S, Managing prosthodontic (geriatric) patients during the SARS-CoV-2 pandemic: J Int Oral Health, 2020; 12; S69-75
29. Degidi M, Nardi D, Piattelli A, Immediate loading of the edentulous maxilla with a definitive restoration supported by an intraorally welded titanium bar and tilted implants: Int J Oral Maxillofac Implants, 2010; 25; 1175-82
30. Mattoo K, Brar A, Jain P, A novel approach to manage drug associated xerostomia in geriatric edentulous patients utilizing salivary reservoir in complete denture prosthesis: Eur J Pharm Med Res, 2014; 1(1); 41-48
31. Garg R, Mattoo K, Kumar L, Impact of sensitization of family caregivers upon treatment compliance among geriatric patients suffering from elder abuse and neglect: Healthcare (Basel), 2021; 9(2); 226
32. Veale D, Eshkevari E, Kanakam N, The appearance anxiety inventory: Validation of a process measure in the treatment of body dysmorphic disorder: Behav Cogn Psychother, 2014; 42; 605-16
33. Mastro S, Zimmer-Gembeck MJ, Webb HJ, Young adolescents’ appearance anxiety and body dysmorphic symptoms: Social problems, self-perceptions and comorbidities: J Obsessive Compuls Relat Disord, 2016; 8; 50-55
34. Kroenke K, Spitzer RL, The PHQ-9: A new depression diagnostic and severity measure: Psychiatr Ann, 2002; 32; 509-21
35. Löwe B, Unutzer J, Callahan CM, Monitoring depression treatment outcomes with the Patient Health Questionnaire-9: Med Care, 2004; 42; 1194-201
36. Sridhara SR, Paragache G, Panda NK, Chakrabarti A, Mucormycosis in immunocompetent individuals: An increasing trend: J Otolaryngol, 2005; 34; 402-6
37. Gupta A, Sharma A, Chakrabarti A, The emergence of post-COVID-19 mucormycosis in India: Can we prevent it?: Ind J Ophthalmol, 2021; 69(7); 1645
38. Cornely OA, Alastruey-Izquierdo A, Arenz D, Global guideline for the diagnosis and management of mucormycosis: An initiative of the European Confederation of Medical Mycology in cooperation with the Mycoses Study Group Education and Research Consortium: Lancet Infect Dis, 2019; 19(12); e405-21
39. Butterworth CJ, Primary vs. secondary zygomatic implant placement in patients with head and neck cancer – a 10-year prospective study: Head Neck, 2019; 41(6); 1687-95
40. Boyes-Varley JG, Howes DG, Davidge-Pitts KD, A protocol for maxillary reconstruction following oncology resection using zygomatic implants: Int J Prosthodont, 2007; 20(5); 521-31
41. Lacroix T, Jaby P, Nokovitch L, Chaux-Bodard AG, Prosthetic rehabilitation with zygomatic implants after maxillectomy: A systematic review: J Dent Oral Disord, 2020; 6; 1132
42. Crerand CE, Sarwer DB, Kazak AE, Body image and quality of life in adolescents with craniofacial conditions: Cleft Palate Craniofac J, 2017; 54; 2-12
43. Bryant RA, Disentangling mild traumatic brain injury and stress reactions: N Engl J Med, 2008; 358; 525-27
44. Lebel S, Castonguay M, Mackness G, The psychosocial impact of stigma in people with head and neck or lung cancer: Psychooncology, 2013; 22(1); 140-52
45. Elisabeta CL, Ovidiu S, Aminov L, Elena LD, Parafunctions in dysfunctional syndrome of the stomatognathic system-literature review: Romanian Journal of Medical and Dental Education, 2020; 9(1); 53-61
46. Sahoo JP, Panda B, Mishra AP, Samal KC, The unseen “Fungal Infections” – an extra thrust aggravating COVID second wave in India: Biot Res Today, 2021; 3(5); 354-56
47. Sen P, Ross N, Rogers S, Recovering maxillofacial trauma patients: The hidden problems: J Wound Care, 2001; 10(3); 53-57
48. Ahuja A, Samudra M, Prasad SP, Correlates of depression, anxiety, self-esteem, and suicidal ideas in COVID-associated mucormycosis patients and the effects of treatment: Ind Psychiatry J, 2021; 30; S75-82
49. Hou Y, Zhang S, Li N, Neurofeedback training improves anxiety trait and depressive symptom in GAD: Brain Behav, 2021; 11(3); e02024
50. Martel A, Baillif S, Nahon-Esteve S, Orbital exenteration: An updated review with perspectives: Surv Ophthalmol, 2021; 66(5); 856-76
51. Hirsch CR, Beale S, Grey N, Liness S, Approaching cognitive behavior therapy for generalized anxiety disorder from a cognitive process perspective: Front Psychiatry, 2019; 10; 796
52. McLean CP, Asnaani A, Litz BT, Hofmann SG, Gender differences in anxiety disorders: Prevalence, course of illness, comorbidity and burden of illness: J Psychiatr Res, 2011; 45(8); 1027-35
53. Belon HP, Vigoda DF, Emotional adaptation to limb loss: Phys Med Rehabil, 2014; 25(1); 53-74
54. Sindi AS, Mittal R, Mattoo K, Impact of an auditory mediated Patient Health Education (PHE) program on treatment compliance and satisfaction among patients seeking prosthodontic care during COVID pandemic – a prospective interventional study: Patient Prefer Adherence, 2022; 1247-55
55. Xie Y, Xu E, Al-Aly Z, Risks of mental health outcomes in people with COVID-19: Cohort study: BMJ, 2022; 376; e068993
56. Irish J, Sandhu N, Simpson C, Quality of life in patients with maxillectomy prostheses: Head Neck, 2009; 31(6); 813-21
57. Landes CA, Zygoma implant-supported midfacial prosthetic rehabilitation: A 4-year follow-up study including assessment of quality of life: Clin Oral Implants Res, 2005; 16(3); 313-25
58. Wang F, Huang W, Zhang C, Functional outcome and quality of life after a maxillectomy: A comparison between an implant supported obturator and implant supported fixed prostheses in a free vascularized flap: Clin Oral Implants Res, 2017; 28(2); 137-43
59. Martinez-Muniz GA, Wood SK, Sex differences in the inflammatory consequences of stress: Implications for pharmacotherapy: J Pharmacol Exp Ther, 2020; 375(1); 161-74
Figures
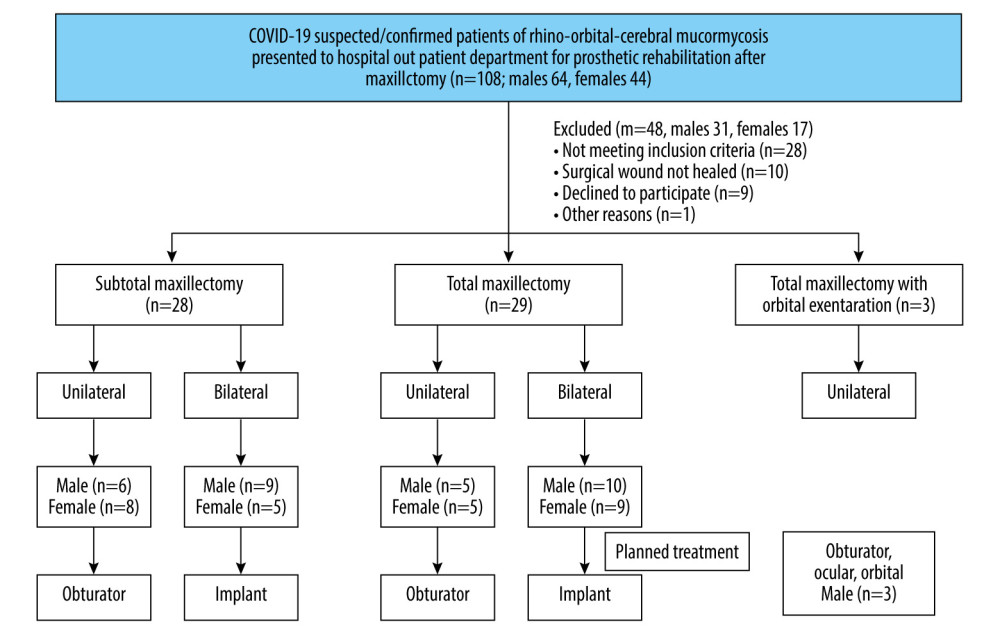 Figure 1. Flow chart showing the sample selection and distribution process. Compiled Figure created using MS PowerPoint, version 20H2 (OS build 19042,1466), Windows 11 Pro, Microsoft Corporation).
Figure 1. Flow chart showing the sample selection and distribution process. Compiled Figure created using MS PowerPoint, version 20H2 (OS build 19042,1466), Windows 11 Pro, Microsoft Corporation).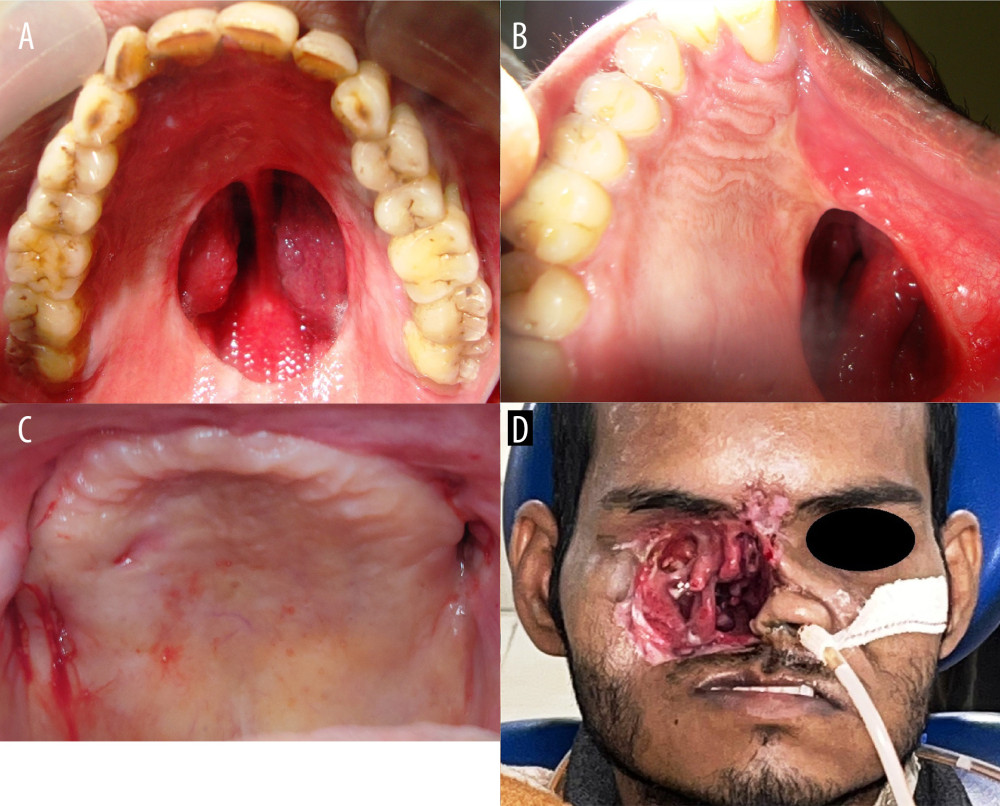 Figure 2. Exemplary cases involved in the study. (A) Subtotal maxillectomy bilateral (STM-B); (B) Total maxillectomy unilateral (STM-U) (note the depressed face on that side); (C) Total maxillectomy bilateral (TM-B) (note there is no hard palate on either side, the flap raised and then put back to prevent oro-nasal communication); (D) total maxillectomy with orbital exenteration unilateral (TMOE-U). Photographs taken using digital single-lens reflex (DSLR) camera (Canon EOS 700D) with 100 mm macro lens) with/without ring flash. Compiled Figure created using MS PowerPoint, version 20H2 (OS build 19042,1466), windows 11 Pro, Microsoft Corporation).
Figure 2. Exemplary cases involved in the study. (A) Subtotal maxillectomy bilateral (STM-B); (B) Total maxillectomy unilateral (STM-U) (note the depressed face on that side); (C) Total maxillectomy bilateral (TM-B) (note there is no hard palate on either side, the flap raised and then put back to prevent oro-nasal communication); (D) total maxillectomy with orbital exenteration unilateral (TMOE-U). Photographs taken using digital single-lens reflex (DSLR) camera (Canon EOS 700D) with 100 mm macro lens) with/without ring flash. Compiled Figure created using MS PowerPoint, version 20H2 (OS build 19042,1466), windows 11 Pro, Microsoft Corporation).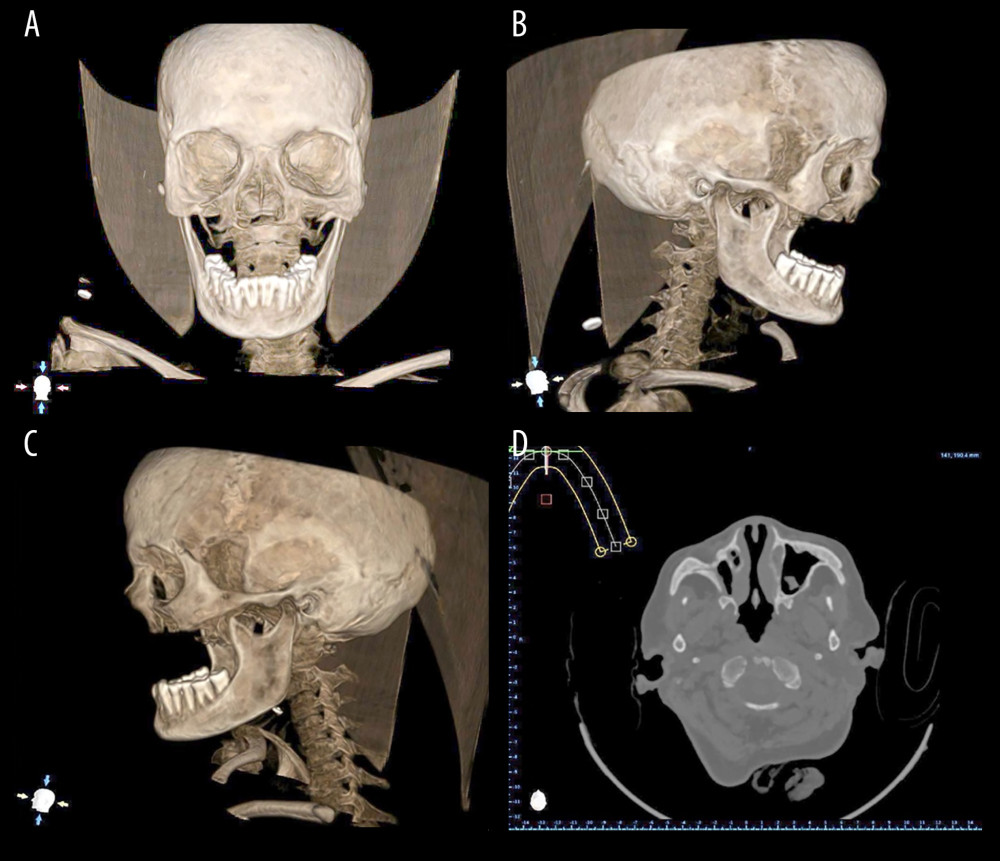 Figure 3. Diagnostic computed tomographic (CT scan) images of exemplary patient with bilateral maxillectomy. (A) Frontal view (note the maxillectomy extent); (B) Left lateral view; (C) Right lateral view; (D) Radiographic image during analysis. Photographs taken using digital single-lens reflex (DSLR) camera (Canon EOS 700D) with 100 mm macro lens) with/without ring flash. Compiled Figure created using MS PowerPoint, version 20H2 (OS build 19042,1466), windows 11 Pro, Microsoft Corporation).
Figure 3. Diagnostic computed tomographic (CT scan) images of exemplary patient with bilateral maxillectomy. (A) Frontal view (note the maxillectomy extent); (B) Left lateral view; (C) Right lateral view; (D) Radiographic image during analysis. Photographs taken using digital single-lens reflex (DSLR) camera (Canon EOS 700D) with 100 mm macro lens) with/without ring flash. Compiled Figure created using MS PowerPoint, version 20H2 (OS build 19042,1466), windows 11 Pro, Microsoft Corporation).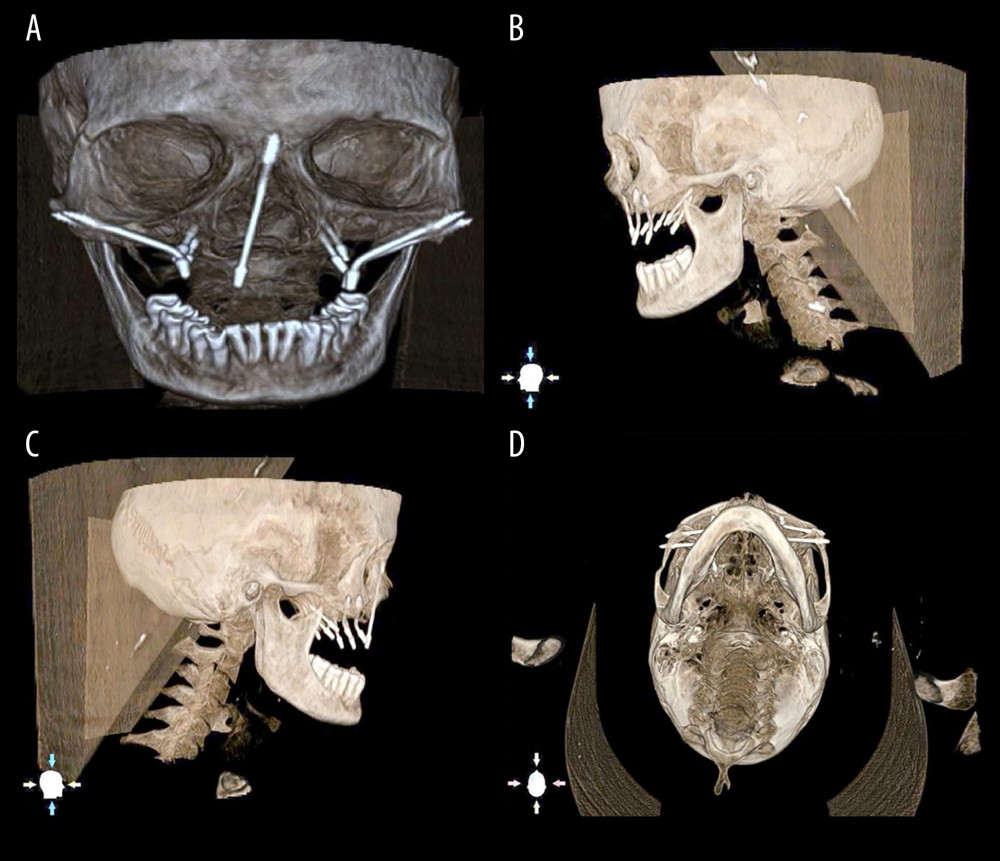 Figure 4. Different length zygomatic implant determination and placement on virtual DICOM (Digital Imaging and Communications in Medicine). (A) Frontal view; (B) Left lateral view; (C) right lateral view; (D) basal view. Note the length of the screw heads at the bone – implant interface level. Photographs taken using digital single-lens reflex (DSLR) camera (Canon EOS 700D) with 100 mm macro lens) with/without ring flash. Compiled Figure created using MS PowerPoint, version 20H2 (OS build 19042,1466), Windows 11 Pro, Microsoft Corporation).
Figure 4. Different length zygomatic implant determination and placement on virtual DICOM (Digital Imaging and Communications in Medicine). (A) Frontal view; (B) Left lateral view; (C) right lateral view; (D) basal view. Note the length of the screw heads at the bone – implant interface level. Photographs taken using digital single-lens reflex (DSLR) camera (Canon EOS 700D) with 100 mm macro lens) with/without ring flash. Compiled Figure created using MS PowerPoint, version 20H2 (OS build 19042,1466), Windows 11 Pro, Microsoft Corporation).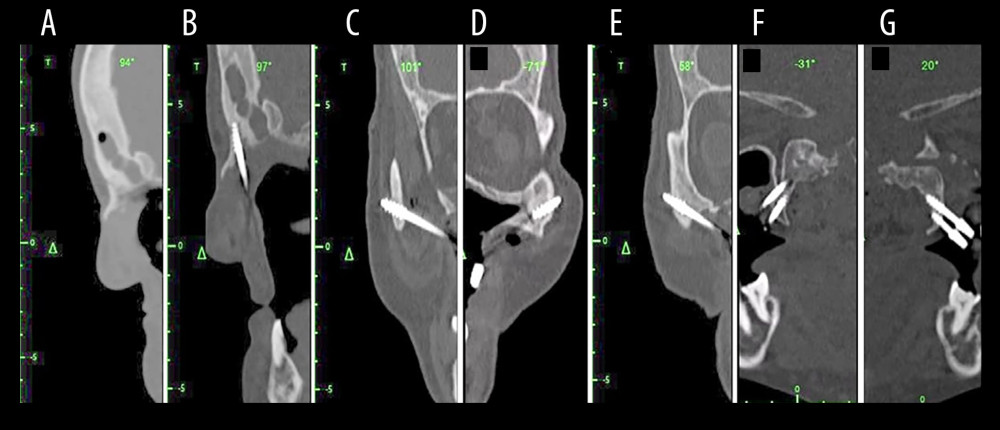 Figure 5. Preoperative display of the surgical planning for an exemplary maxillectomy patient planned to receive zygomatic implant on the navigation monitor. (A, B) Sagittal view before and after implant placement (C, D) on the left and right zygomatic bones (E–G) other views of planned areas. Photographs taken using a digital single-lens reflex (DSLR) camera (Canon EOS 700D) with 100 mm macro lens) with/without ring flash. Compiled Figure created using MS PowerPoint, version 20H2 (OS build 19042,1466), Windows 11 Pro, Microsoft Corporation).
Figure 5. Preoperative display of the surgical planning for an exemplary maxillectomy patient planned to receive zygomatic implant on the navigation monitor. (A, B) Sagittal view before and after implant placement (C, D) on the left and right zygomatic bones (E–G) other views of planned areas. Photographs taken using a digital single-lens reflex (DSLR) camera (Canon EOS 700D) with 100 mm macro lens) with/without ring flash. Compiled Figure created using MS PowerPoint, version 20H2 (OS build 19042,1466), Windows 11 Pro, Microsoft Corporation).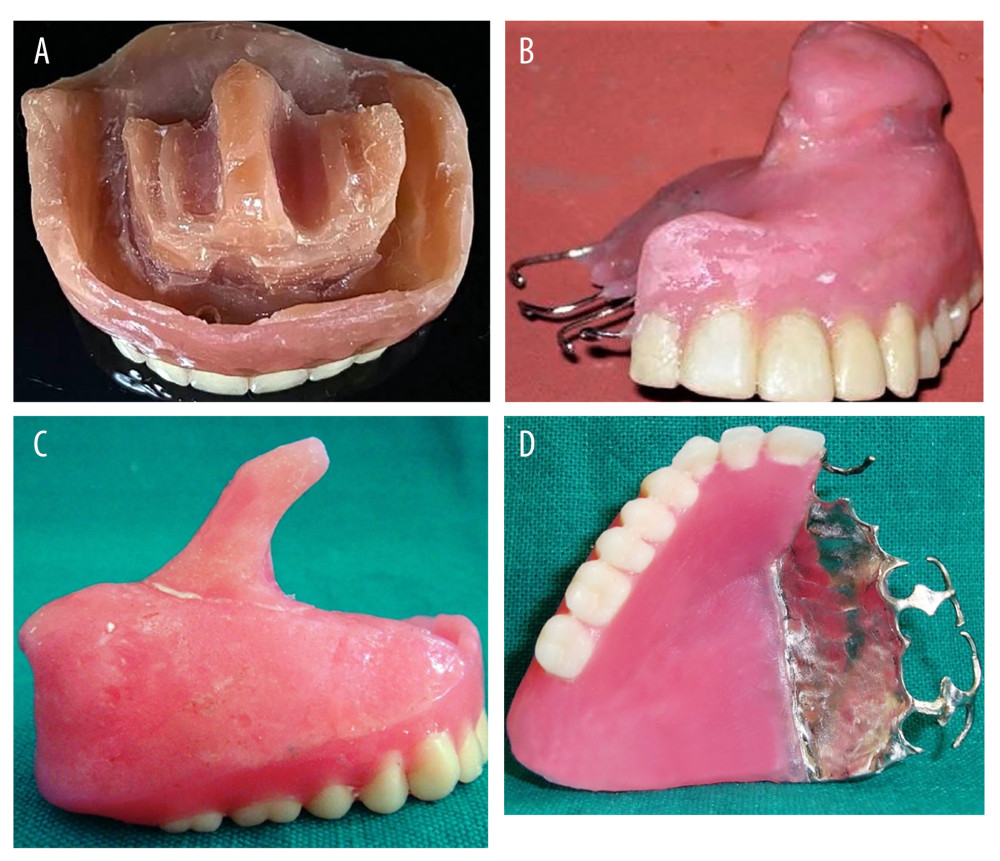 Figure 6. Types of prosthesis used in the total cohort. (A) Zygomatic implant-supported fixed complete denture prosthesis; (B) Interim obturator for unilateral total maxillectomy; (C) Interim obturator for subtotal maxillectomy; (D) Definitive prosthesis for total and subtotal maxillectomy cases. Photographs taken using a digital single-lens reflex (DSLR) camera (Canon EOS 700D) with 100 mm macro lens) with/without ring flash. Compiled Figure created using MS PowerPoint, version 20H2 (OS build 19042,1466), Windows 11 Pro, Microsoft Corporation).
Figure 6. Types of prosthesis used in the total cohort. (A) Zygomatic implant-supported fixed complete denture prosthesis; (B) Interim obturator for unilateral total maxillectomy; (C) Interim obturator for subtotal maxillectomy; (D) Definitive prosthesis for total and subtotal maxillectomy cases. Photographs taken using a digital single-lens reflex (DSLR) camera (Canon EOS 700D) with 100 mm macro lens) with/without ring flash. Compiled Figure created using MS PowerPoint, version 20H2 (OS build 19042,1466), Windows 11 Pro, Microsoft Corporation). Figure 7. (A) Preoperative facial appearance of an exemplary patient showing facial aesthetics before prosthodontic rehabilitation; (B) Postoperative facial aesthetics with patient smiling; (C) 1 year follow-up orthopantomogram showing the zygomatic implant well received by the bone. Photographs taken using a digital single-lens reflex (DSLR) camera (Canon EOS 700D) with 100 mm macro lens) with/without ring flash. Compiled Figure created using MS PowerPoint, version 20H2 (OS build 19042,1466), Windows 11 Pro, Microsoft Corporation).
Figure 7. (A) Preoperative facial appearance of an exemplary patient showing facial aesthetics before prosthodontic rehabilitation; (B) Postoperative facial aesthetics with patient smiling; (C) 1 year follow-up orthopantomogram showing the zygomatic implant well received by the bone. Photographs taken using a digital single-lens reflex (DSLR) camera (Canon EOS 700D) with 100 mm macro lens) with/without ring flash. Compiled Figure created using MS PowerPoint, version 20H2 (OS build 19042,1466), Windows 11 Pro, Microsoft Corporation).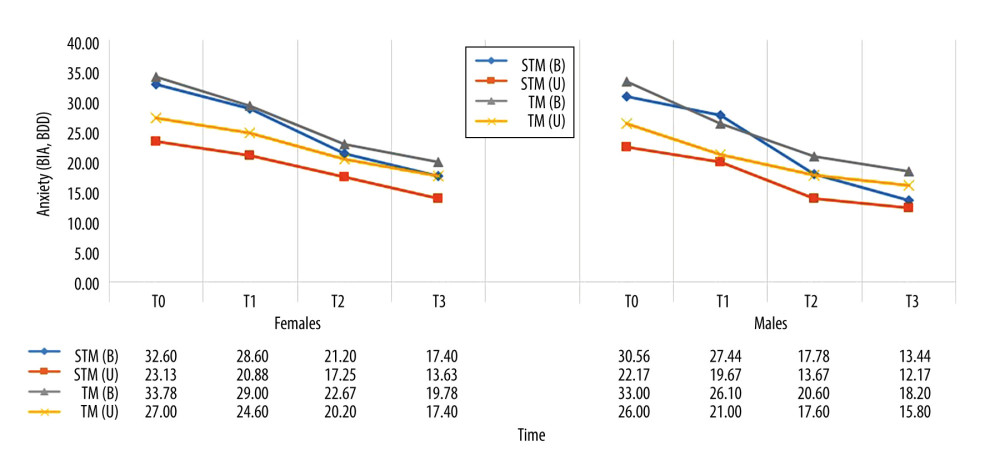 Figure 8. Comparative gender differences in mean values of appearance anxiety score among different maxillectomy types at different time intervals. Figure created using MS Excel spreadsheet, version 20H2 (OS build 19042,1466), Windows 11 Pro, Microsoft Corporation).
Figure 8. Comparative gender differences in mean values of appearance anxiety score among different maxillectomy types at different time intervals. Figure created using MS Excel spreadsheet, version 20H2 (OS build 19042,1466), Windows 11 Pro, Microsoft Corporation).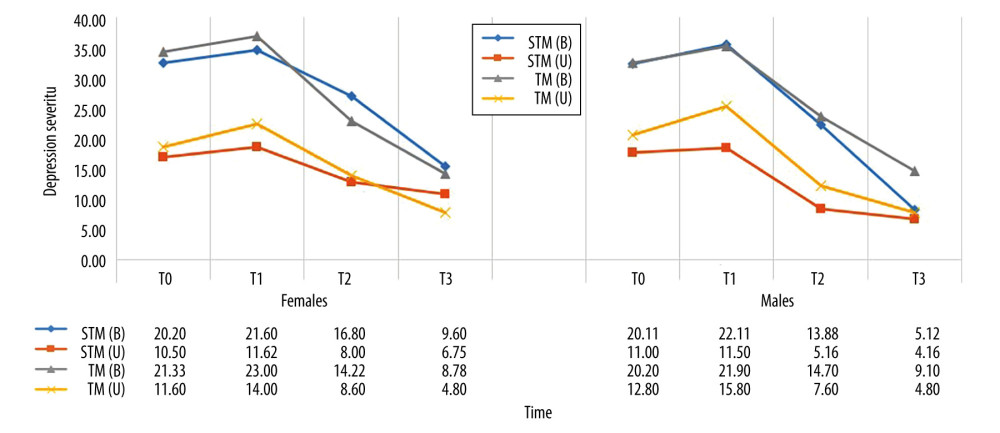 Figure 9. Comparative gender differences in mean values of severity of depression symptoms score among different maxillectomy types at different time intervals. Figure created using MS Excel spreadsheet, version 20H2 (OS build 19042,1466), Windows 11 Pro, Microsoft Corporation).
Figure 9. Comparative gender differences in mean values of severity of depression symptoms score among different maxillectomy types at different time intervals. Figure created using MS Excel spreadsheet, version 20H2 (OS build 19042,1466), Windows 11 Pro, Microsoft Corporation). Video 1. Pre-rehabilitation speech. Video recorded using a digital single-lens reflex (DSLR) camera (Canon EOS 700D).
Video 1. Pre-rehabilitation speech. Video recorded using a digital single-lens reflex (DSLR) camera (Canon EOS 700D). Video 2. Post-rehabilitation speech. Video recorded using a digital single-lens reflex (DSLR) camera (Canon EOS 700D).
Video 2. Post-rehabilitation speech. Video recorded using a digital single-lens reflex (DSLR) camera (Canon EOS 700D). Tables
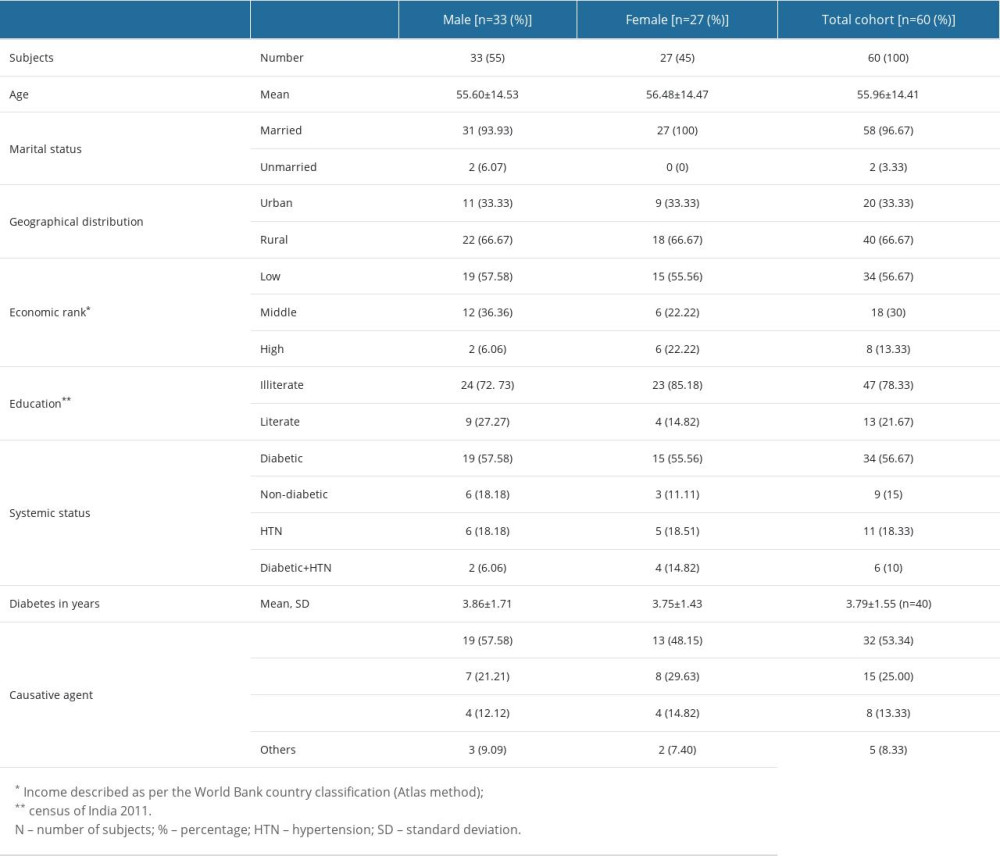 Table 1. Demographic characteristics of the mucormycosis affected subjects seeking prosthodontic and maxillofacial rehabilitation post functional endoscopic sinus surgery with maxillectomy/exenteration of the eye.
Table 1. Demographic characteristics of the mucormycosis affected subjects seeking prosthodontic and maxillofacial rehabilitation post functional endoscopic sinus surgery with maxillectomy/exenteration of the eye.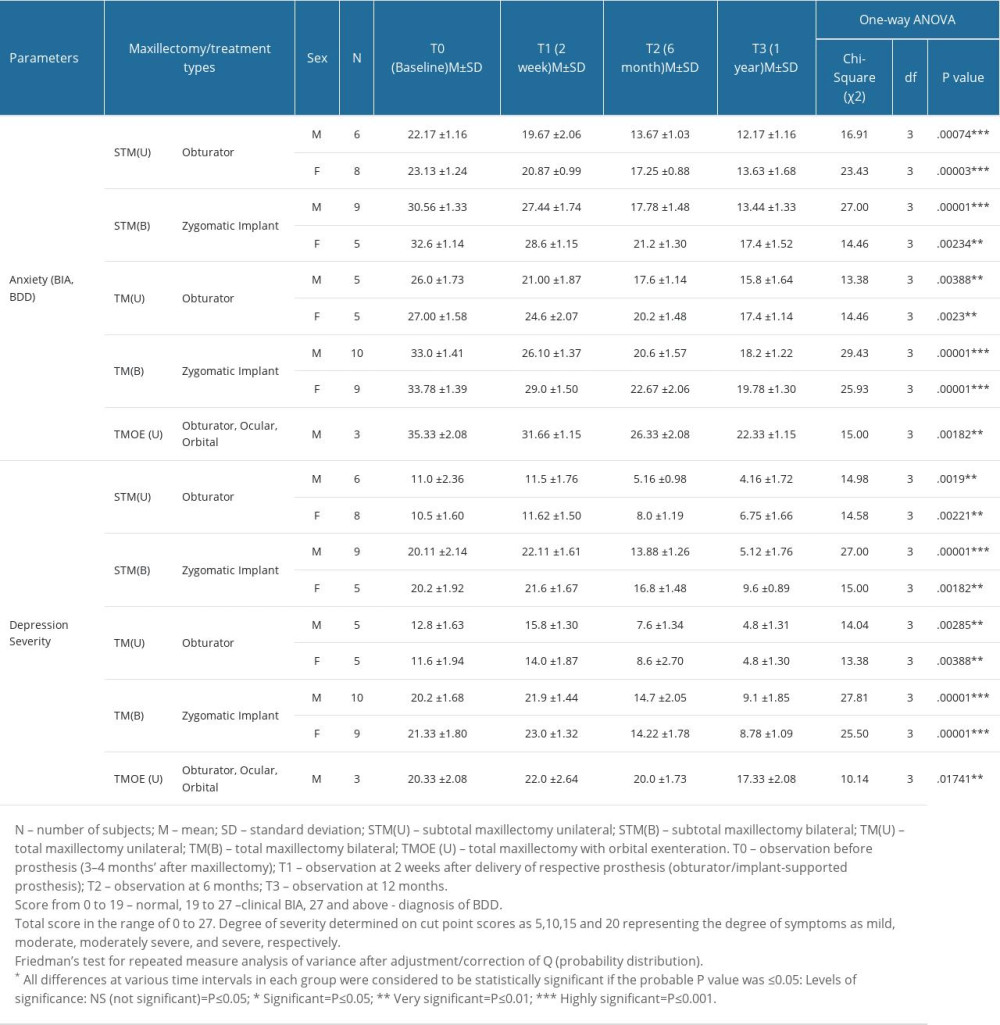 Table 2. Comparative differences in mean values of Appearance Anxiety (AAI) and Depression Scale (PHQ-9) between various maxillectomy/treatment groups/subgroups at 4 treatment time intervals.
Table 2. Comparative differences in mean values of Appearance Anxiety (AAI) and Depression Scale (PHQ-9) between various maxillectomy/treatment groups/subgroups at 4 treatment time intervals.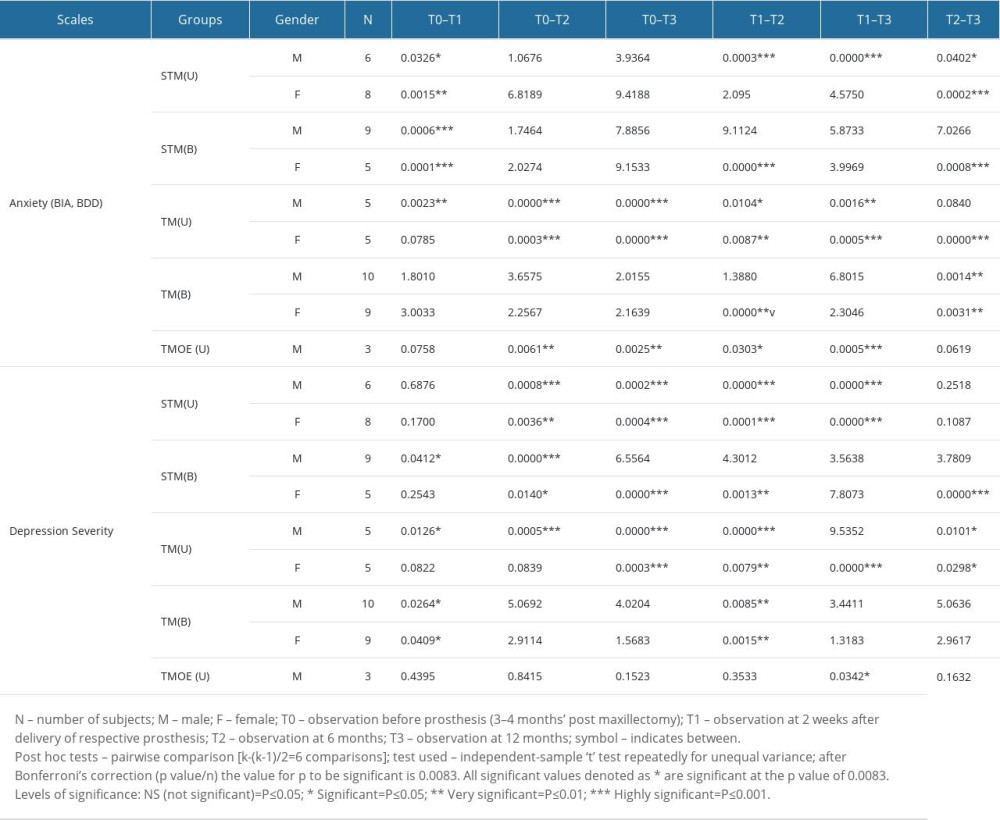 Table 3. Post hoc test showing comparative differences at various treatment time intervals among groups/subgroups for Appearance Anxiety (AAI) and Depression Scale (PHQ-9).
Table 3. Post hoc test showing comparative differences at various treatment time intervals among groups/subgroups for Appearance Anxiety (AAI) and Depression Scale (PHQ-9).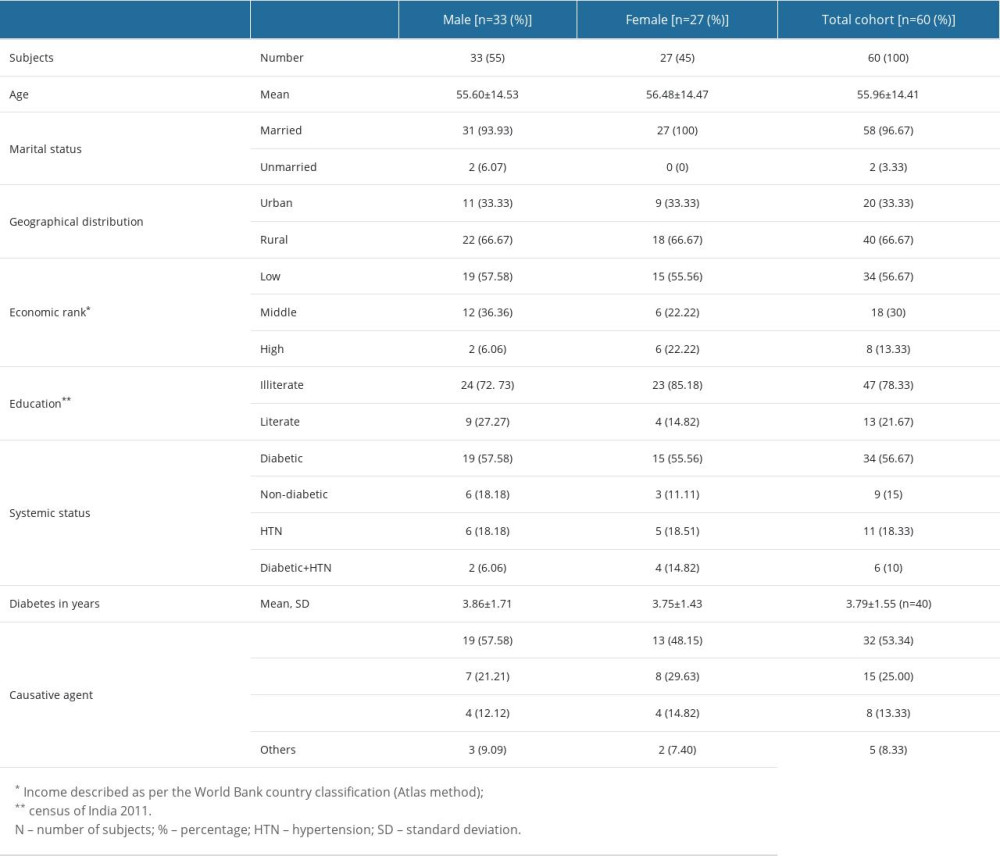 Table 1. Demographic characteristics of the mucormycosis affected subjects seeking prosthodontic and maxillofacial rehabilitation post functional endoscopic sinus surgery with maxillectomy/exenteration of the eye.
Table 1. Demographic characteristics of the mucormycosis affected subjects seeking prosthodontic and maxillofacial rehabilitation post functional endoscopic sinus surgery with maxillectomy/exenteration of the eye.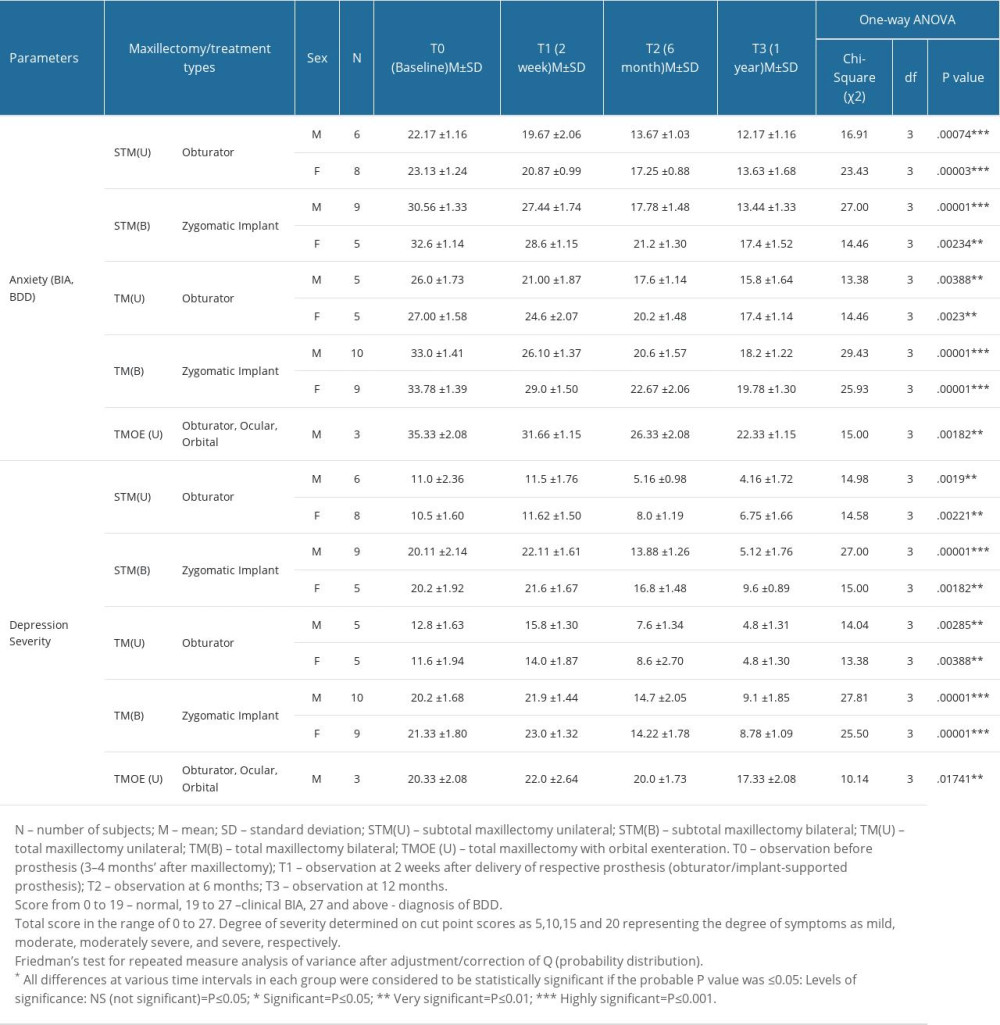 Table 2. Comparative differences in mean values of Appearance Anxiety (AAI) and Depression Scale (PHQ-9) between various maxillectomy/treatment groups/subgroups at 4 treatment time intervals.
Table 2. Comparative differences in mean values of Appearance Anxiety (AAI) and Depression Scale (PHQ-9) between various maxillectomy/treatment groups/subgroups at 4 treatment time intervals.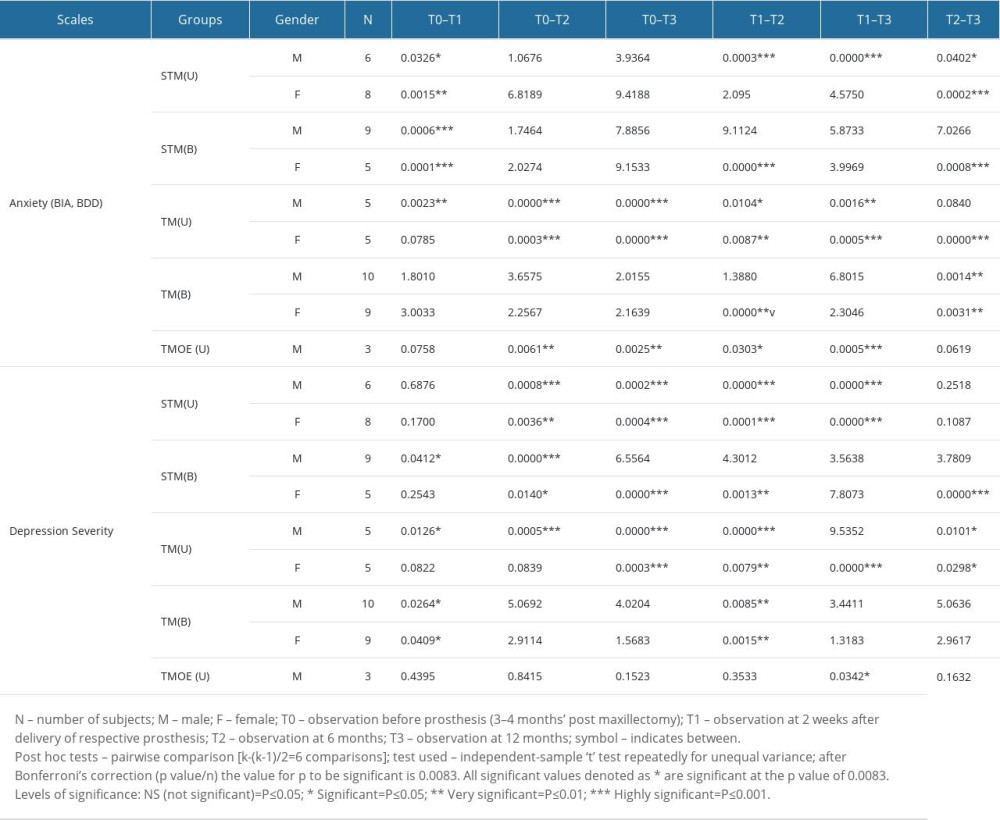 Table 3. Post hoc test showing comparative differences at various treatment time intervals among groups/subgroups for Appearance Anxiety (AAI) and Depression Scale (PHQ-9).
Table 3. Post hoc test showing comparative differences at various treatment time intervals among groups/subgroups for Appearance Anxiety (AAI) and Depression Scale (PHQ-9). In Press
08 Mar 2024 : Animal Research
Modification of Experimental Model of Necrotizing Enterocolitis (NEC) in Rat Pups by Single Exposure to Hyp...Med Sci Monit In Press; DOI: 10.12659/MSM.943443
18 Apr 2024 : Clinical Research
Comparative Analysis of Open and Closed Sphincterotomy for the Treatment of Chronic Anal Fissure: Safety an...Med Sci Monit In Press; DOI: 10.12659/MSM.944127
08 Mar 2024 : Laboratory Research
Evaluation of Retentive Strength of 50 Endodontically-Treated Single-Rooted Mandibular Second Premolars Res...Med Sci Monit In Press; DOI: 10.12659/MSM.944110
11 Mar 2024 : Clinical Research
Comparison of Effects of Sugammadex and Neostigmine on Postoperative Neuromuscular Blockade Recovery in Pat...Med Sci Monit In Press; DOI: 10.12659/MSM.942773
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








