23 July 2023: Clinical Research
Assessing the Impact of the Zero Mother Mortality Preeclampsia Program on Maternal Mortality Rates at a Single Center in Bandung, West Java (2015–2022): A Retrospective Study
Adhi PribadiDOI: 10.12659/MSM.941097
Med Sci Monit 2023; 29:e941097
Abstract
BACKGROUND: The Zero Mother Mortality Preeclampsia (ZOOM) program was adopted as an accelerated initiative to curb mortality related to hypertensive disorders in pregnancy, including preeclampsia. This single-center, retrospective study in Bandung, West Java, aims to evaluate the impact of the ZOOM program implemented from 2015 to 2022.
MATERIAL AND METHODS: We analyzed 19,176 childbirths and associated maternal deaths due to hypertension in pregnancy. Diagnoses were validated using blood pressure measures, lab tests including urine protein, liver function, blood profiles, platelets, X-ray, echocardiography, and COVID-19 testing. The case fatality rate (CFR) was assessed to evaluate the impact of the ZOOM program.
RESULTS: Hypertension in pregnancy was identified in 25.1% of cases, with 9.8% and 1.4% attributed to preeclampsia and eclampsia, respectively. Maternal deaths associated with hypertension accounted for 36.6%, with the majority linked to eclampsia. Heart failure (45.5%) and Hemolysis, Elevated Liver enzymes, and Low Platelets (HELLP) syndrome (22%) were the most common complications. The CFR decreased from 61% in 2018 to 10% in 2022. The overall CFR from 2015 to 2022 was 1.3%, with the highest fatality rate observed in eclampsia cases (9.4%). However, a declining trend was seen since 2018, reaching a low of 0.2% in 2021.
CONCLUSIONS: The implementation of the ZOOM program, which includes preeclampsia re-education, early detection, prompt intervention, protocol adjustments, and a refined referral system, led to a marked reduction in maternal deaths from hypertensive pregnancy disorders.
Keywords: Eclampsia, Maternal Mortality, Mortality, Pre-Eclampsia, Pregnancy, Female, Humans, Retrospective Studies, Maternal Death, COVID-19 Testing, Indonesia, Mothers, COVID-19, Hypertension, HELLP Syndrome
Background
The Zero Mother Mortality Preeclampsia (ZOOM) program has been implemented since the end of 2017 by implementing both types of early detection re-education approaches, prevention and referral criteria, as well as changes to preeclampsia management protocols [1]. This breakthrough program has a target of reducing maternal mortality associated with preeclampsia to zero percent.
The maternal mortality rate in Indonesia in 2015 was 305 per 100 000 live births [2]. Hypertension in pregnancy globally is the second most frequent cause of maternal death after postpartum hemorrhage (PPH) [3]. Based on Indonesian statistics in 2018, the population was 265 015 313 and there were 5 291 143 pregnant women [4]. Hypertension in pregnancy affects 2–3% of all pregnancies in a year, so based on calculations, there will be very many maternal deaths due to hypertension in pregnancy [5].
This certainly requires a breakthrough program to reduce the death rate, so programs like ZOOM are needed. The ZOOM program was originally intended to reduce preeclampsia because there were recommendations for preventive methods, low-dose aspirin, and calcium, but in practice provided re-education of all types of hypertension in pregnancy, including changes in protocols and referral systems. The target is to reduce preeclampsia and the number of deaths due to hypertension in pregnancy.
Hypertension in pregnancy includes 4 categories, as recommended by the Working Group of the National High Blood Pressure Education Program on High Blood Pressure: 1) chronic hypertension, 2) preeclampsia-eclampsia, 3) chronic hypertension accompanied by preeclampsia or superimposed, and 4) gestational hypertension [5]. The effects of high blood pressure vary from mild to severe and are often accompanied by complications of the kidneys, heart, liver, and seizures or eclampsia. In addition, it can harm the fetus, which can lead to low birth weight and preterm labor [6]. However, when treated appropriately, many pregnant women with high blood pressure can give birth safely and have healthy babies without serious problems, so it can be concluded that high blood pressure can be harmful to the mother and fetus [7,8].
Preeclampsia-related deaths are secondary, mainly as a result of severe instances like the development of eclampsia, or the advent of aggravating comorbidities including heart failure and pulmonary edema, or stroke [9,10]. Efforts are being made to prevent maternal death due to hypertension in pregnancy by early detection, and prevention programs [11,12]. Another effort is to try to make modifications to the protocol for handling hypertension in pregnancy, which can be a win-win solution for both mother and fetus and ensures that both have healthy outcomes [13]. The ZOOM program is a collaboration between the Department of Obstetrics & Gynecology, Faculty of Medicine, University of Padjadjaran – Dr. Hasan Sadikin, General Hospital and the Indonesian Society of Obstetrics and Gynecology (POGI) branch of West Java. In 2020, this program received assistance from the JALIN program, part of the U.S. Agency for International Development (USAIDS) project in Indonesia, which aims to help reduce maternal and infant mortality in Indonesia. Therefore, this retrospective study from a single center in Bandung, West Java aimed to evaluate reduction in maternal mortality rates from hypertensive pregnancy disorders between 2015 and 2022, and the Zero Mother Mortality Preeclampsia program.
Material and Methods
ETHICAL CONSIDERATION:
The study was approved from the Medical Research Ethics Committee of Hasan Sadikin General Hospital (approval number LB.02.01/X.6.5/185/2023).
STUDY DESIGN AND SUBJECTS:
This study was a retrospective observational study aimed to assess maternal deaths due to preeclampsia-eclampsia or hypertension in pregnancy. The study population was based on available hospital admission records. Data were retrieved from 2015 to 2022 from a single center (Dr. Hasan Sadikin General Hospital Bandung, West Java, Indonesia). For this purpose, all admissions including International Classification of Disease, tenth revision (ICD-10) codes related to preeclampsia, eclampsia, and hypertensive-pregnancy disorders were identified and included, becoming our study population. Details on all patients were recorded by Department of Obstetrics and Gynecology. The accuracy and completeness of all included patient records were checked. Patients without complete medical records or those whose results were unknown were excluded. The present report follows the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines.
DATA COLLECTION:
Collected information included data on the number of deliveries, records of maternal deaths due to causes related to hypertension in pregnancy (gestational hypertension, preeclampsia, chronic hypertension, chronic hypertension superimposed), eclampsia, and related complications and diseases, including HELLP syndrome, heart complications/lung edema, acute kidney injury, stroke, thyroid disease, autoimmune diseases, and COVID-19. These data were taken secondarily from Hasan Sadikin Hospital information system and medical records of the Obstetrics and Gynecology Department. As a comparison to describe the situation before the program was implemented, secondary data were taken from 2015 to 2022.
STATISTICAL ANALYSIS:
Data were checked, coded, and analyzed using the International Business Machines Statistical Package for Social Science version 28.00 (IBM SPSS) statistical software. Frequencies, proportions, and standard deviations were calculated in descriptive statistics. Considering the date of admission as a reference point, the CFR was estimated for each epidemiological year based on the proportion (%) between the number of total maternal mortality due to hypertension per total hypertensive cases.
LIMITATION:
The limitation of this study is that it was retrospective and mostly a referral cases, so there could be no tracing of health services provided and what actions were taken before arriving at the tertiary health center.
Results
HYPERTENSIVE GROUP MATERNAL DEATH ANALYSIS:
Based on data obtained from medical records from 2015 to 2022, there were 19 176 deliveries, with 4819 (25.1%) hypertension cases in pregnancy. There were 172 maternal deaths over that time for a variety of reasons, and the rate of maternal deaths attributable to pregnancy-associated hypertension was 36.6%. The main causes of death in the hypertensive group were eclampsia (39.6%) and severe preeclampsia (27%). The most common complication was heart failure and lung edema (45.5%), and the second most common complication was HELLP syndrome (22%). Some patients had multiple complications (Table 1).
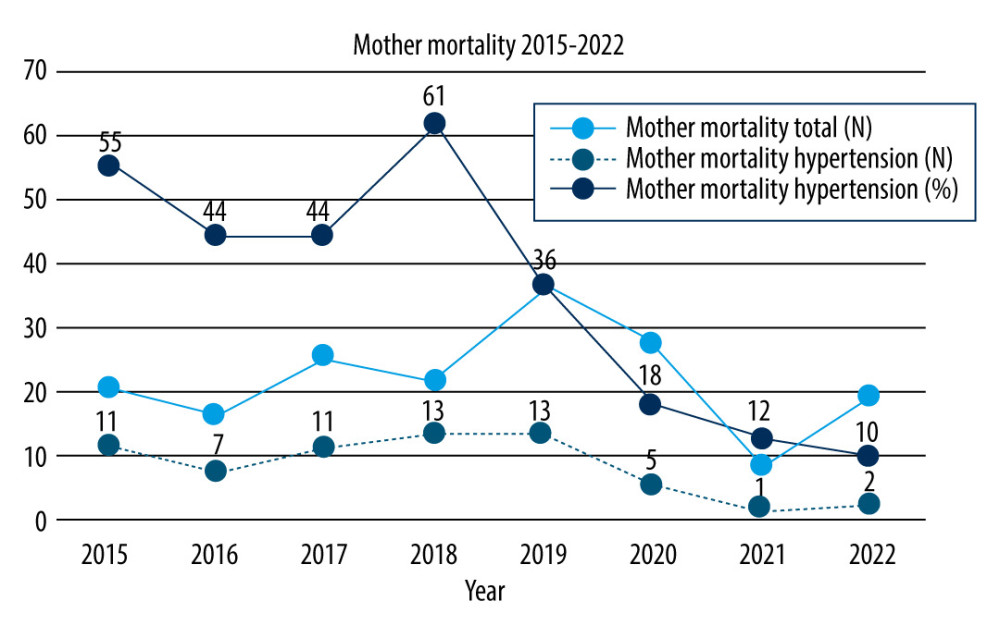
Our study reports that there was a fluctuating downward trend in the number of deaths since 2018. The number of maternal deaths peaked in 2018 and accounted for 61% of all maternal deaths due to hypertension in pregnancy compared to the total number of maternal deaths. After 2018, there was a downward trend until only 10% remained in 2022. It still did not meet the target of zero mortality according to the title and goals of the program, but this condition had significantly decreased maternal mortality due to preeclampsia-eclampsia or hypertension in pregnancy in general (Figure 1).
CASE FATALITY RATE ANALYSIS:
Based on the results of the study in Table 2, the incidence of preeclampsia was 9.8% of all deliveries. The incidence of chronic hypertension aggravated by preeclampsia or superimposed had an incidence percentage of 6.7%. The CFR of hypertension in pregnancy from 2015 to 2022 was 1.3%, with the highest fatality rate being eclampsia, at 9.4%. The CFR rate since 2018 (2.6%) tended to decline slowly and gradually, until it reached its lowest point in 2021, at just 0.2%.
Discussion
In this study, the prevalence of pregnancy with hypertension for 2015–2022 was 25.1%, which is higher than the 13.9% rate found by Nath et al in southern India [14]. In the present study, the mortality rate due to hypertension in pregnancy was 36.6% of all cases. This is in contrast to the study in India by Meh, which showed only 7% of all maternal deaths, and which ranks as the third cause of death after bleeding and infection [15].
In Norway from 1996 to 2014, 74 maternal deaths occurred due to hypertensive disorders (21.6%) [16]. The number of maternal deaths due to preeclampsia was 9.8% of the total 172 cases over a period of 8 years. In another study, preeclampsia accounted for 10–15% of maternal deaths [17], but in this study, mortality due to eclampsia was 1.4%, almost 3 times higher than the average percentage of other studies (0.5%) [6]. Eclampsia was the most common cause of death (39.6%) of the group of maternal deaths due to hypertension in pregnancy as well. This finding is slightly lower than in another study, which found that eclampsia accounts for 43.35% of all maternal deaths [18].
The term case fatality rates in this study refers to the proportion of people who die due to certain diseases, while maternal mortality rate (MMR) refers to maternal deaths due to complications from pregnancy or childbirth. Table 2 shows that the eclampsia fatality rate was likewise the highest, at 9.4%. This shows that CFR eclampsia is 9 times deadlier when compared to CFR preeclampsia, which is only 1%. Another study, published by Das et al, in southern India, showed CFR eclampsia was 8.0% [18]
The most frequent eclampsia complication is heart failure, which can lead to further problems like pulmonary edema [18]. Other studies have shown 12.7% of patients with severe preeclampsia had grade II diastolic dysfunction, and 9.5% had peripartum pulmonary edema [19]. This study also indicated that heart decompensation was the most frequent sequelae, which occurred in 45.5% of cases. Preeclampsia affects pregnant women’s health over time, notably the possibility of long-term cardiovascular diseases [20]. In addition to heart complications and pulmonary edema, another disorder that is quite often associated with maternal death is HELLP syndrome [21,22]. In this study, the second most common complication was HELLP syndrome; about 22% of the complications that arose were related to maternal death. In addition to cardiac decompensation and pulmonary edema, the incidence of HELLP syndrome was also consistently the second most common complication in the years prior to 2021.
The decrease in the percentage of maternal deaths in Figure 1 is followed by the decrease in CFR as shown in Table 2. It was revealed that the CFR in 2019 (1.4%) began to decline significantly when compared to 2018 (2.6%). After 2019, the decline continued until the lowest point in 2021 (0.2%). This finding showed that re-education programs and protocol changes play an important role in reducing the number of severe preeclampsia cases with complications, thus reducing the risk of death (CFR and the amount of maternal mortality directly).
Therefore, re-education of medical professionals in West Java province can reach a wider range, including government officials. This step aims strategically to further expand the coverage of re-education to specialists, general practitioners, and midwives as medical personnel in primary care. The maternal mortality reduction program in West Java is widely supported by various parties in West Java province. This could happen considering that West Java is the most populous province in Indonesia, so if one program can be successful, it may be implemented or become a role model elsewhere.
The limitation of this study is that it was retrospective and mostly included referral cases, so there could be no tracing of health services and what actions were taken before arriving at the tertiary health center, including whether to go through prevention programs. In addition, the mobility of the population in Indonesia is relatively high, without the need to report a new address to the government, making tracing to find information during pregnancy with hypertension relatively difficult because the address is not clear.
Conclusions
There was a decrease in the number of maternal deaths after preeclampsia re-education, early and prompt identification, prevention, protocol adjustments, and referrals system, all of which are included in the ZOOM program.
References
1. Pribadi A, Zero Mother Mortality Preeclampsia Program: Opportunity for a rapid acceleration in the decline of maternal mortality rate in Indonesia: Int J Womens Health Reprod Sci, 2021; 9(3); 160-63
2. : BPS statistics Indonesia, 2015 Available at: https://www.bps.go.id/publication/2016/11/30/63daa471092bb2cb7c1fada6/profil-penduduk-indonesia-hasil-supas-2015.html
3. Edhi MM, Aslam HM, Naqvi Z, Hashmi H, Post partum hemorrhage: Causes and management: BMC Res Notes, 2013; 6; 236
4. : Indonesia Health Profile, 2018 Available at: https://pusdatin.kemkes.go.id/resources/download/pusdatin/profil-kesehatan-indonesia/Data-dan-Informasi_Profil-Kesehatan-Indonesia-2018.pdf
5. Mammaro A, Carrara S, Cavaliere A, Hypertensive disorders of pregnancy: J Prenat Med, 2009; 3(1); 1-5
6. , Report of the National High Blood Pressure Education Program Working Group on High Blood Pressure in Pregnancy: Am J Obstet Gynecol, 2000; 183(1); S1-S22
7. Nakimuli A, Nakubulwa S, Kakaire O, The burden of maternal morbidity and mortality attributable to hypertensive disorders in pregnancy: A prospective cohort study from Uganda: BMC Pregnancy Childbirth, 2016; 16; 205
8. Ghulmiyyah L, Sibai B, Maternal mortality from preeclampsia/eclampsia: Semin Perinatol, 2012; 36(1); 56-59
9. Ford ND, Cox S, Ko JY, Hypertensive Disorders in pregnancy and mortality at delivery hospitalization - United States, 2017–2019: MMWR Morb Mortal Wkly Rep, 2022; 71; 585-91
10. Chuang CJ, Chiou WY, Yang HJ, Impact of preeclampsia/eclampsia on hemorrhagic and ischemic stroke risk: A 17 years follow-up nationwide cohort study: PLoS One, 2022; 17(11); e0276206
11. Mikat B, Gellhaus A, Wagner N, Early detection of maternal risk for preeclampsia: Int Sch Res Notices, 2012; 2012; 172808
12. US Preventive Services Task Force, Aspirin use to prevent preeclampsia and related morbidity and mortality: US Preventive Services Task Force Recommendation Statement: JAMA, 2021; 326(12); 1186-91
13. Aziz A, Mose JC, The differences of characteristic, management, maternal and perinatal outcomes among early and late onset preeclampsia: Open Access Library Journal, 2016; 3; 1-7
14. Nath A, Sheeba B, Sisira R, Metgud CS, Prevalence of hypertension in pregnancy and its associated factors among women attending antenatal clinics in Bengaluru: J Family Med Prim Care, 2021; 10(4); 1621-27
15. Meh C, Sharma A, Ram U, Trends in maternal mortality in India over two decades in nationally representative surveys: BJOG, 2022; 129(4); 550-61
16. Nyfløt LT, Ellingsen L, Yli BM, Maternal deaths from hypertensive disorders: Lessons learnt: Acta Obstet Gynecol Scand, 2018; 97; 976-87
17. Duley L, The global impact of pre-eclampsia and eclampsia: Semin Perinatol, 2009; 33(3); 130-37
18. Das R, Biswas S, Eclampsia: The major cause of maternal mortality in Eastern India: Ethiop J Health Sci, 2015; 25(2); 111-16
19. Vaught AJ, Kovell LC, Szymanski LM, Acute cardiac effects of severe pre-eclampsia: J Am Coll Cardiol, 2018; 72(1); 1-11
20. Garovic VD, August P, Preeclampsia and the future risk of hypertension: The pregnant evidence: Curr Hypertens Rep, 2013; 15(2); 114-21
21. Lisonkova S, Razaz N, Sabr Y, Maternal risk factors and adverse birth outcomes associated with HELLP syndrome: A population-based study: BJOG, 2020; 127; 1189-98
22. Vigil-De Gracia P, Maternal deaths due to eclampsia and HELLP syndrome: Int J Gynaecol Obstet, 2009; 104; 90-94
23. Hantoushzadeh S, Shamshirsaz AA, Aleyasin A, Maternal death due to COVID-19: Am J Obstet Gynecol, 2020; 223(1); 109e1-e16
24. Hung SK, Lee MS, Lin HY, Impact of hypertensive disorders of pregnancy on the risk of stroke stratified by subtypes and follow-up time: Stroke, 2022; 53(2); 338-44
25. Sharshar T, Lamy C, Mas JL, Incidence and causes of strokes associated with pregnancy and puerperium: A study in public hospitals of Ile de France: Stroke, 1995; 26(6); 930-36
26. Tim I, Korevaar M, Eric A, The risk of preeclampsia according to high thyroid function in pregnancy differs by hCG concentration: J Clin Endocrinol Metab, 2016; 101(12); 5037-43
27. Spinillo A, Beneventi F, Locatelli E, The impact of unrecognized autoimmune rheumatic diseases on the incidence of preeclampsia and fetal growth restriction: A longitudinal cohort study: BMC Pregnancy Childbirth, 2016; 16; 313
Tables
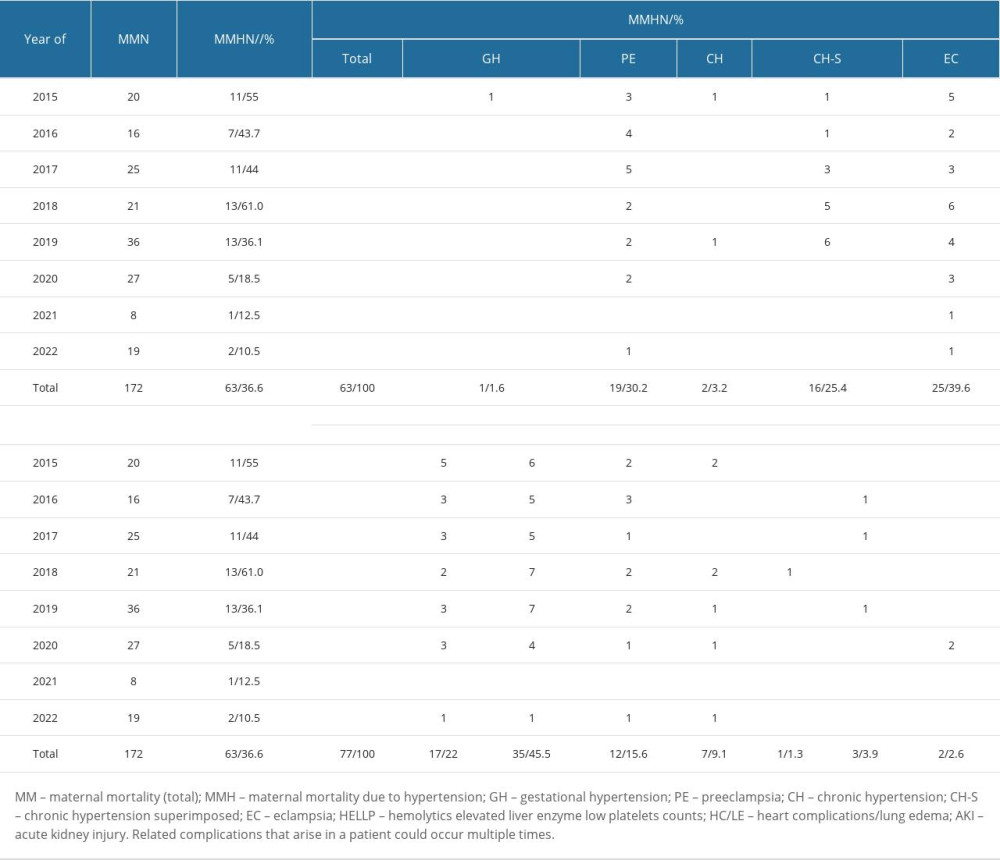 Table 1. Total maternal mortality, diagnosis characteristic, and related complications.
Table 1. Total maternal mortality, diagnosis characteristic, and related complications.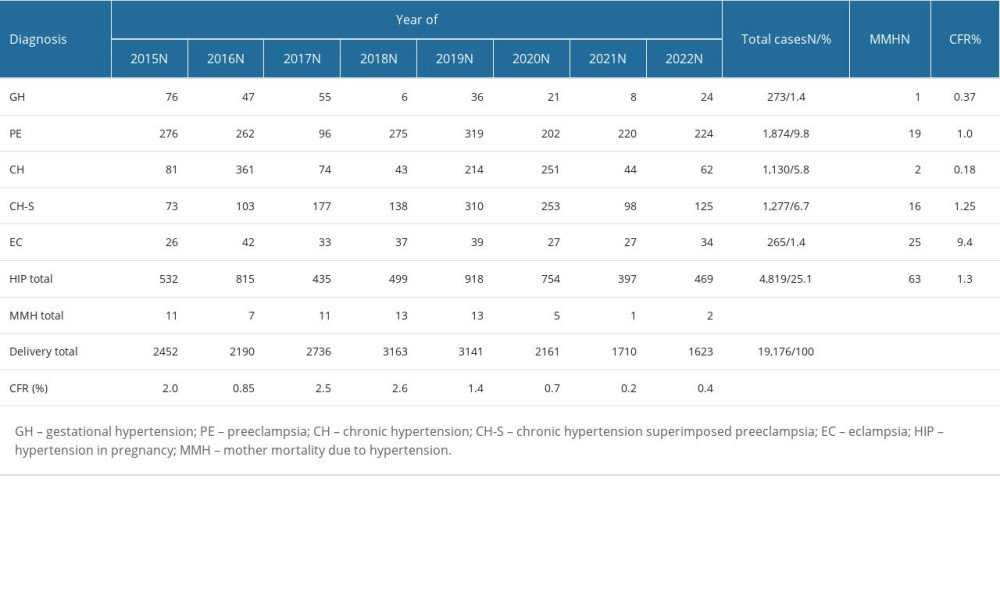 Table 2. Case fatality rate by year and type of hypertension in pregnancy.
Table 2. Case fatality rate by year and type of hypertension in pregnancy.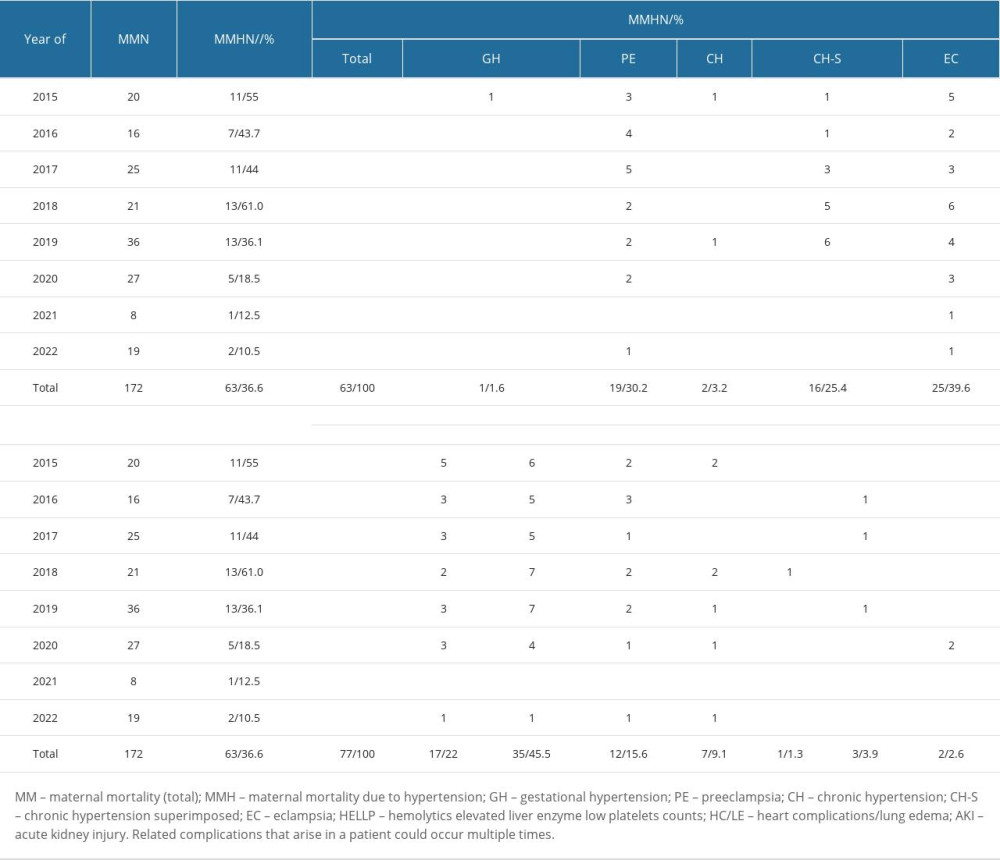 Table 1. Total maternal mortality, diagnosis characteristic, and related complications.
Table 1. Total maternal mortality, diagnosis characteristic, and related complications.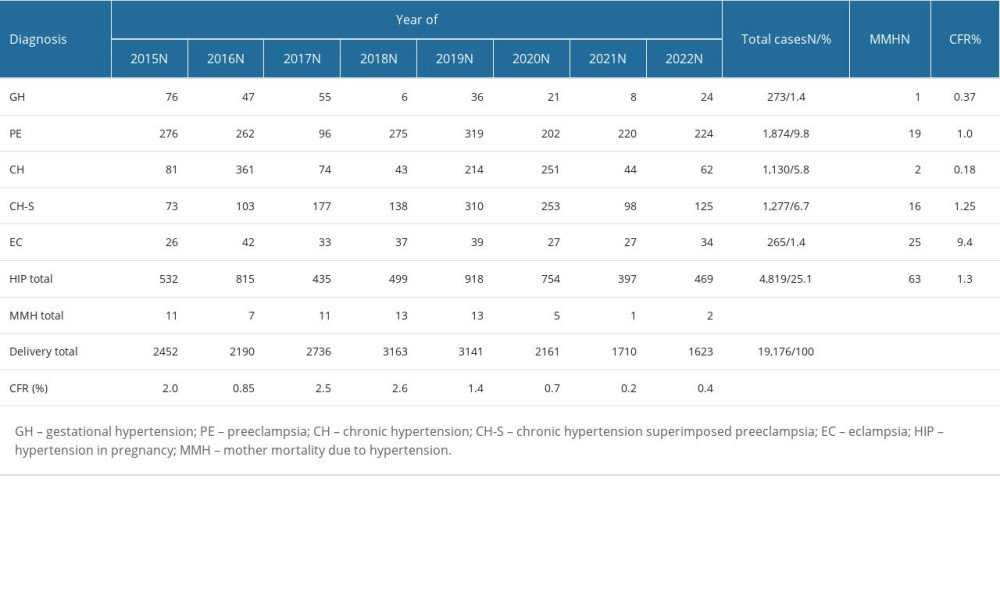 Table 2. Case fatality rate by year and type of hypertension in pregnancy.
Table 2. Case fatality rate by year and type of hypertension in pregnancy. In Press
08 Mar 2024 : Animal Research
Modification of Experimental Model of Necrotizing Enterocolitis (NEC) in Rat Pups by Single Exposure to Hyp...Med Sci Monit In Press; DOI: 10.12659/MSM.943443
18 Apr 2024 : Clinical Research
Comparative Analysis of Open and Closed Sphincterotomy for the Treatment of Chronic Anal Fissure: Safety an...Med Sci Monit In Press; DOI: 10.12659/MSM.944127
08 Mar 2024 : Laboratory Research
Evaluation of Retentive Strength of 50 Endodontically-Treated Single-Rooted Mandibular Second Premolars Res...Med Sci Monit In Press; DOI: 10.12659/MSM.944110
11 Mar 2024 : Clinical Research
Comparison of Effects of Sugammadex and Neostigmine on Postoperative Neuromuscular Blockade Recovery in Pat...Med Sci Monit In Press; DOI: 10.12659/MSM.942773
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952