30 May 2022: Clinical Research
Effects of Wearing Face Masks on Exercise Capacity and Ventilatory Anaerobic Threshold in Healthy Subjects During the COVID-19 Epidemic
Qiang LinDOI: 10.12659/MSM.936069
Med Sci Monit 2022; 28:e936069
Abstract
BACKGROUND: Face masks have become an important part of the COVID-19 prevention approach. This study aimed to explore the effect of wearing masks on exercise ability and ventilatory anaerobic threshold (VAT).
MATERIAL AND METHODS: Thirty-four young, healthy volunteers were included in this study, consisting of 18 men and 16 women. The subjects were randomized to perform 2 cardiopulmonary exercise tests (CPET) on a cycle ergometer with gas exchange analysis, one with and another without wearing a face mask (cross-over design). The general data for all subjects and indicators from the 2 exercise tests performed with and without wearing a face mask were collected.
RESULTS: In cardiopulmonary exercise tests, wearing a mask significantly (P<0.05) decreased peak indexes (eg, work rate (WR), oxygen consumption per kg body weight (VO₂/kg), heart rate (HR), ventilation per minute (VE) and carbon dioxide ventilation equivalent (VE/VCO₂)) and anaerobic threshold indexes (eg, WR, HR, VE, breath frequency (BF), dead space ratio (VD/VT), and VE/VCO₂). However, the PETCO₂ at peak was significantly higher. There was a positive linear correlation between WR difference and VO₂ difference at VAT (abbreviated as δWR@VAT and δVO₂@VAT, respectively) (r=0.495, P=0.003). Subgroup analysis of the VAT indexes showed that WR, VO₂/kg, and VE were significantly decreased in the advanced VAT group with mask compared with the stable VAT group with mask (P<0.05). Logistic regression showed that δVE, δBF, and δVE/VCO₂ had independent influences on VAT.
CONCLUSIONS: Wearing masks advances VAT in healthy young subjects during CPET. The advanced VAT was associated with changes in VE, BF, and VE/VCO₂ while wearing masks.
Keywords: Anaerobic Threshold, COVID-19, Exercise Test, COVID-19, Exercise Tolerance, Female, healthy volunteers, Humans, Male, Masks
Background
The coronavirus-19 (COVID-19) pandemic has had a long-term and profound effect on people’s lives, studies, work, and social activities around the world. Wearing face masks, which prevent the transmission of infectious respiratory pathogens, has become a major strategy to prevent its spread [1,2].
Some clinical trials have investigated the effects of wearing face masks on subjects’ performance during exercise. Fikenzer et al conducted repetitive cardiopulmonary exercise tests on 12 healthy male subjects in a randomized order: no mask, surgical mask, and an FFP2/N95 mask; the forced expiratory volume and peak expiratory flow of the subjects decreased during the lung function tests, while peak power and ventilation also decreased during the cardiopulmonary exercise test [3]. Shaw et al showed that wearing a face mask during vigorous exercise had no discernable detrimental effect on blood or muscle oxygenation or exercise performance in young, healthy participants [4]. The conclusions of these studies were based on comparisons of maximum exercise capacity, which does not necessarily represent the actual exercise conditions during a routine exercise.
However, there is a lack of studies on continuous exercise capability (anaerobic threshold), which we believe is the crux of the issue. Any physical activity that exceeds the anaerobic threshold can lead to anaerobic metabolism and unsustainable exercise. Continuous physical activity is only possible if the exercise intensity does not exceed the anaerobic threshold. According to previous studies, the endurance threshold for an 8-h shift of heavy manual occupational labor is 33%–40% of an individual’s maximum oxygen uptake [5]. Even in physically highly demanding occupational tasks, the ventilatory threshold of an individual was only exceeded for short periods at 35–69% of maximal oxygen uptake [6]. To study the harm caused by wearing a mask during exercise, it is important to determine an individual’s ventilatory threshold. However, there are limited studies on the effect of exercising with a mask on the ventilatory anaerobic threshold.
Two separate incidents of the sudden death of students wearing face masks in China have raised concerns about whether wearing face masks during exercise results in physiological changes that endanger human life. Considering that wearing masks is thought to prevent oxygen inhalation, increase repetitive inhalation of carbon dioxide, and increase work of breathing [7], we hypothesized that wearing face masks might advance both the peak and ventilatory anaerobic threshold (VAT) during cardiopulmonary exercise testing. This study aimed to investigate the effect of wearing face masks on exercise performance and the VAT in healthy young subjects through a cardiopulmonary exercise test (CPET), as well as the mechanisms involved.
Material and Methods
SUBJECTS:
A total of 34 young, healthy volunteers were recruited from the medical staff of our Rehabilitation Department. The inclusion criteria were: 1) 18–30 years of age, 2) healthy and without cardiopulmonary diseases, 3) not using drugs that affect heart rate, and 4) signed the informed consent form. The exclusion criteria were: 1) any signs of hemodynamic instability during exercise, such as pale complexion and decreased blood pressure, or 2) unable to complete the cycling task for any reason.
STUDY DESIGN:
This study was registered at
CARDIOPULMONARY EXERCISE TEST (CPET) PROTOCOL:
All CPETs were performed by the same operator, who has been a CPET operator at the Rehabilitation Department for >10 years. The fit of the surgical face mask beneath the Schiller mask was standardized; the correct fit was confirmed by exhaling with maximal force before each test to identify air leakage. At the beginning of each exercise test, subjects rested for 3 minutes, then performed warm-up exercise for 3 minutes (unload cycling), followed by a ramp incremental exercise stage until voluntary exhaustion occurred. Each subject continued an additional 5-min recovery period at a work rate of 20 W. The increase in the work rate varied from 10 to 25 W/min according to the estimated exercise capability of each subject and ensured that the subject reached the peak within 10 minutes. The power increasing scheme for each subject’s 2 exercise tests was the same so that the detection of exercise peak and the anaerobic threshold were not affected. Gas exchange was measured using a breath-by-breath instrument (Schiller AT-104) with a mask with 80 to 100 mL of dead space. All values were averaged across 10-second epochs. At the end of each CPET test, the physician estimated the location of the subject’s VAT. At the end of all tests, the location of the VAT for each exercise test was re-verified by another physician. The VAT point of each test was determined using the V-slope method [8] and other ventilatory parameters, including the VE/VCO2 nadir, PETCO2 response, and RER transition point.
COLLECTED INDICATORS:
General information about each subject was collected, and all indicators from the 2 exercise tests were recorded, with or without wearing a face mask, including work rate (WR), oxygen uptake (VO2), heart rate (HR), ventilation per minute (VE), tidal volume (VT), breath frequency (BF), dead space ratio (VD/VT), carbon dioxide ventilation equivalent (VE/VCO2), and end-tidal CO2 pressure (PETCO2). The VAT was denoted by work rates and oxygen uptake, abbreviated as WR@VAT and VO2@VAT, respectively.
STATISTICAL ANALYSIS:
R version 4.0.3 (R version 4.0.3 (2020-10-10) – “Bunny-Wunnies Freak Out” Copyright (C) 2020 The R Foundation for Statistical Computing Platform:
Results
DEMOGRAPHIC AND BASELINE DATA:
A total of 34 young, healthy volunteers were enrolled, consisting of 18 men and 16 women (Figure 1). All 34 participants completed the 2 CPETs. The main characteristics were an age of 23.4±3.6 years, a height of 170.3±9.7 cm, a weight of 63.3±13.5 kg, and a BMI of 21.7±3.7 kg·m−2. The physiological indexes at rest included heart rate of 87.7±12.5 bpm, systolic blood pressure of 114.8±17.8 mmHg, and diastolic blood pressure of 77.0±9.6 mmHg. All pulmonary function test indexes were good (Table 1).
COMPARISON OF PEAK INDEXES AND VAT INDEXES BETWEEN 2 EXERCISE TESTS WITH AND WITHOUT A MASK:
As shown in Table 2, the peak indexes of the cardiopulmonary exercise test while wearing face masks, such as WR, VO2/kg, HR, VE, and VE/VCO2, were significantly lower than those in the cardiopulmonary exercise test without a face mask (all P<0.05). However, the PETCO2 was significantly higher than those in the cardiopulmonary exercise test without a face mask (P=0.004). The VAT indexes of the cardiopulmonary exercise test while wearing face masks, such as WR, HR, VE, BF, VD/VT, and VE/VCO2, were significantly lower than those in the cardiopulmonary exercise test without a face mask (all P<0.05).
:
There was a positive linear correlation between δWR@VAT and δVO2@VAT (r=0.495, P=0.003, Figure 2).
SUBGROUP ANALYSIS:
According to the aggregation characteristics of scattered points, δWR@VAT=−6 watts at the X-axis position was selected as the vertical dividing line, and the 34 subjects were divided into 2 groups: the stable VAT group (VS group) and the advanced VAT group (VA group). The subgroup analysis of the VAT indicators showed that all subjects in the VS group and VA group had similar VAT indicators in the exercise test without a mask. Compared with the VS group, WR, VO2/kg, and VE were significantly decreased in the VA group after wearing masks (all P<0.05) (Table 3).
As shown in Table 4, subjects in the VA group demonstrated a significant difference in δHR, δVE, δVT, δVE/VCO2, and δPETCO2 compared with subjects in the VS group (all P<0.05). All demographics and physiological characteristics were not significantly different between the 2 groups. Multivariable logistic regression analysis revealed that the factors independently associated with decreased VAT were δVE, δBF, and δVE/VCO2 (Table 5).
Discussion
LIMITATIONS:
Although the tightness test of the mask was assessed in a calm state, we could not guarantee the absence of gas leakage during the exercise test. Due to many missing values, systolic blood pressure data could not be provided, which is important because it may be closely related to the risk of wearing masks. However, we did detect a decrease in systolic blood pressure in many subjects, whether at peak or VAT. When portable finger pulse oximetry was added, SpO2 did not significantly decrease during the exercise test while wearing a mask, and in some cases, it even increased. Since SpO2 values cannot be recorded synchronously in real-time, we could not provide SpO2 values at each observation time point. Blinding was not possible for the participant nor any study personnel in the same room as the participant. Finally, no body composition tests were performed, and follow-up studies will be conducted.
Conclusions
Our data show that wearing surgical masks causes ventilatory anaerobic threshold to occur earlier in some healthy young subjects during cardiopulmonary exercise test. Whether VAT occurs in advance is related to the changes in VE, BF, and VE/VCO2.
Figures
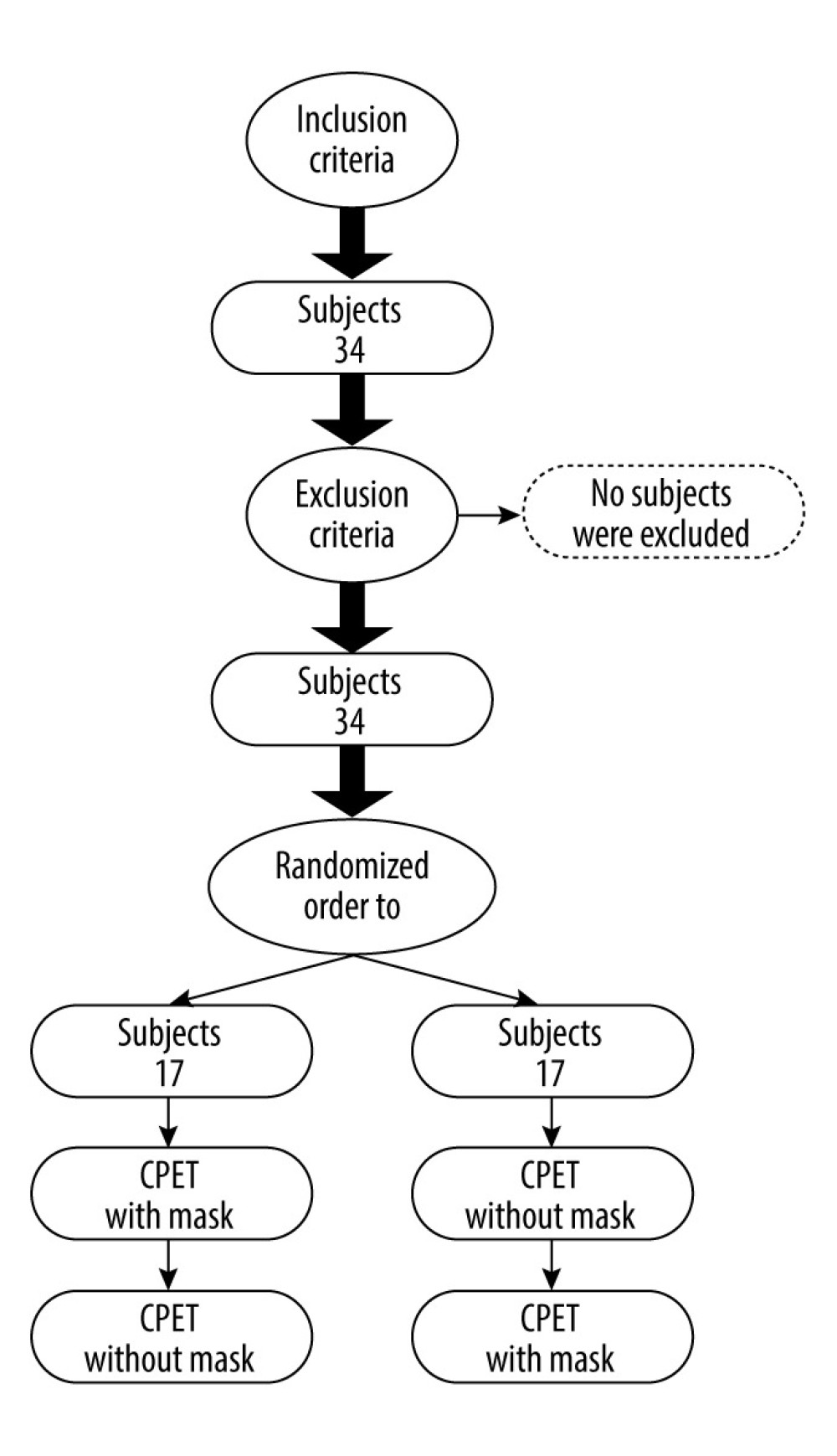 Figure 1. Patient flowchart.
Figure 1. Patient flowchart. 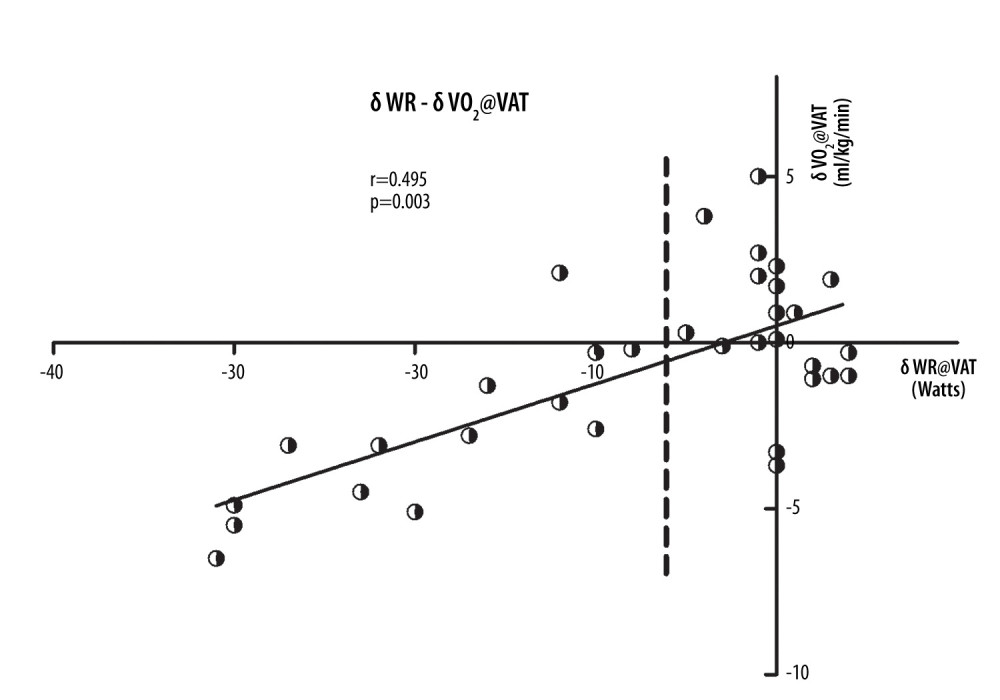 Figure 2. Scatter plots of the δWR and δVO2 at the VAT point. The scatter plot shows a positive linear correlation between δWR@VAT and δVO2@VAT (r=0.495, P=0.003). VAT – ventilatory anaerobic threshold; δWR – work rate difference between 2 exercise tests with and without a mask; δVO2 – oxygen consumption difference between 2 exercise tests with and without a mask.
Figure 2. Scatter plots of the δWR and δVO2 at the VAT point. The scatter plot shows a positive linear correlation between δWR@VAT and δVO2@VAT (r=0.495, P=0.003). VAT – ventilatory anaerobic threshold; δWR – work rate difference between 2 exercise tests with and without a mask; δVO2 – oxygen consumption difference between 2 exercise tests with and without a mask. Tables
Table 1. Baseline characteristics and physiological indexes of participants.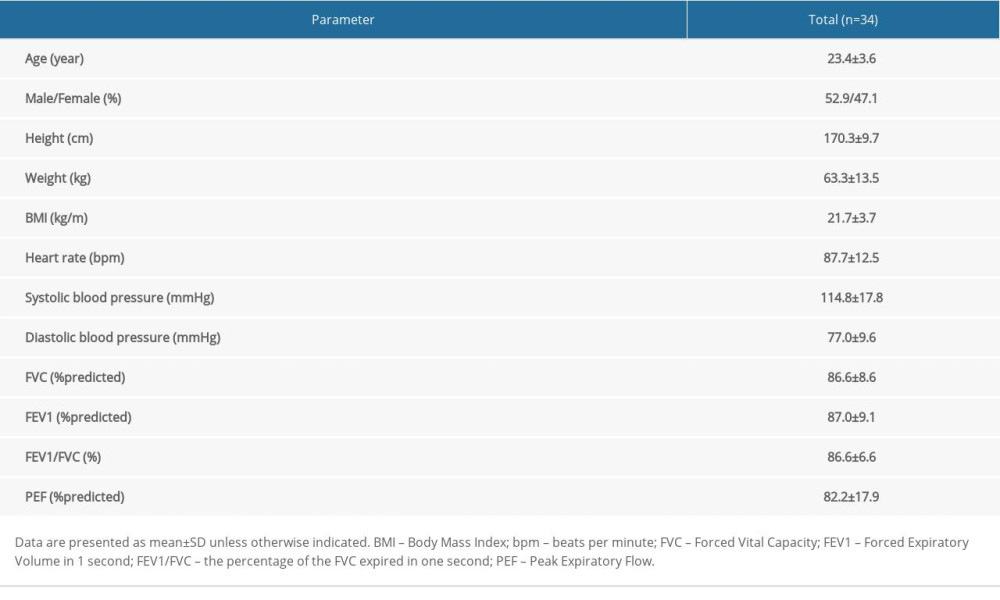 Table 2. Comparison of peak indexes and VAT indexes between 2 exercise tests with and without a mask.
Table 2. Comparison of peak indexes and VAT indexes between 2 exercise tests with and without a mask.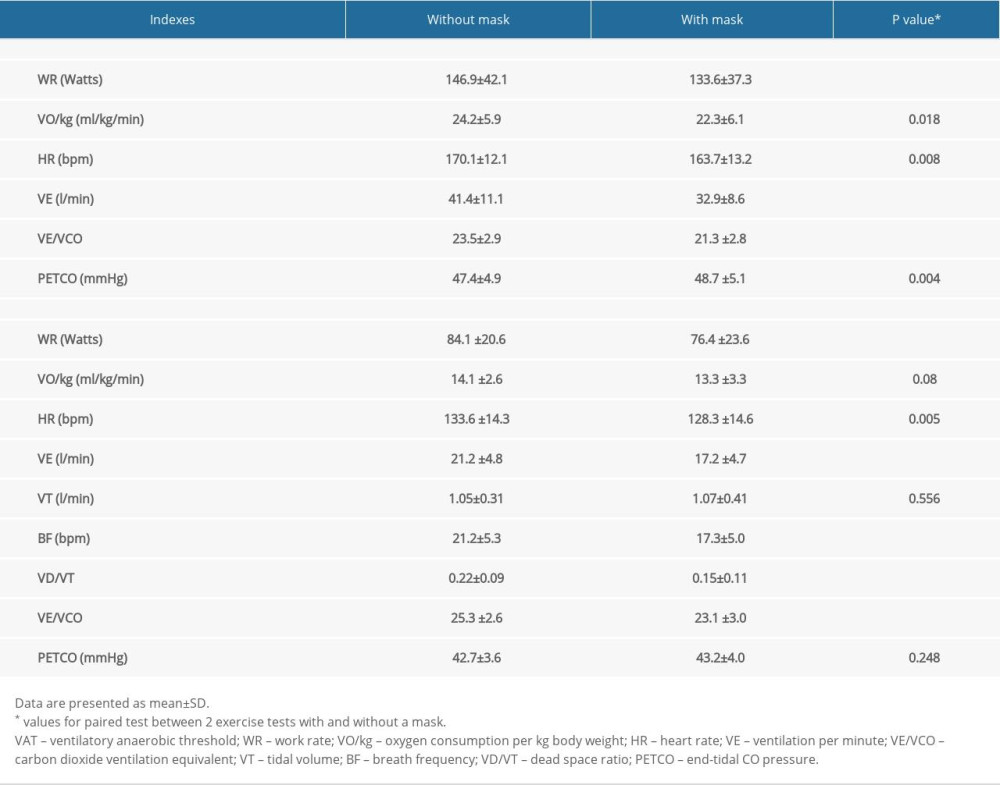 Table 3. Comparison of VAT indexes of 2 exercise tests between the 2 groups.
Table 3. Comparison of VAT indexes of 2 exercise tests between the 2 groups.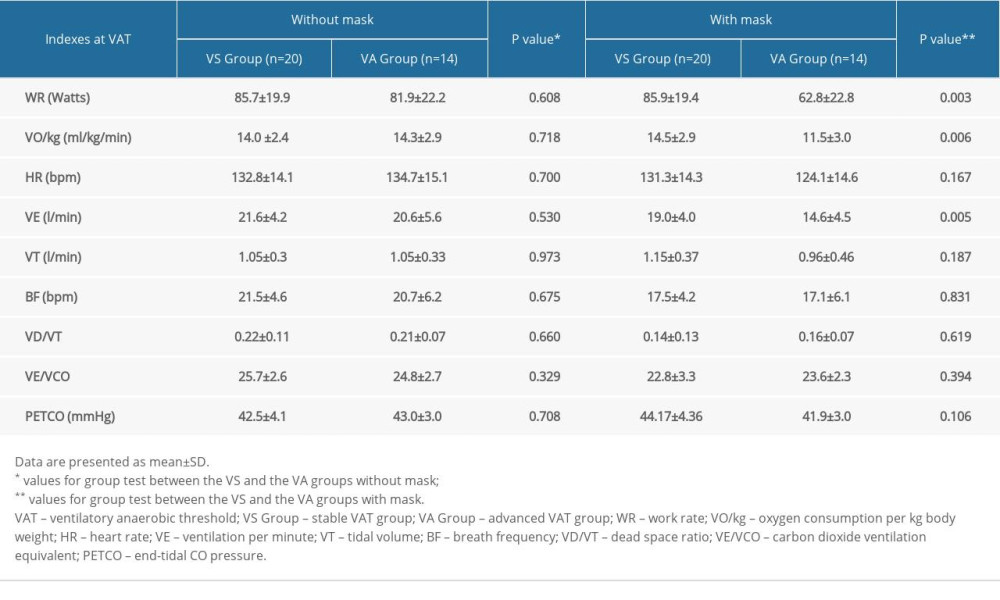 Table 4. Comparison of demographic and physiological characteristics, and delta indicators at VAT after subgrouping.
Table 4. Comparison of demographic and physiological characteristics, and delta indicators at VAT after subgrouping.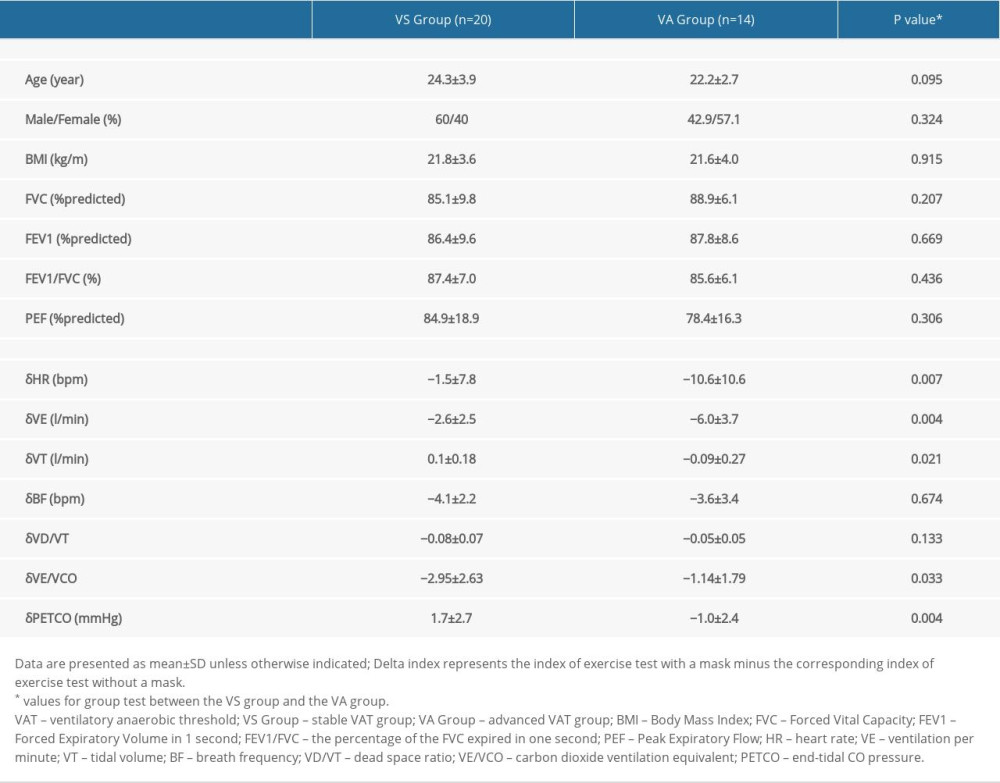 Table 5. Factors associated with being in the advanced VAT group rather than the stable VAT group via multivariable logistic regression analysis.
Table 5. Factors associated with being in the advanced VAT group rather than the stable VAT group via multivariable logistic regression analysis.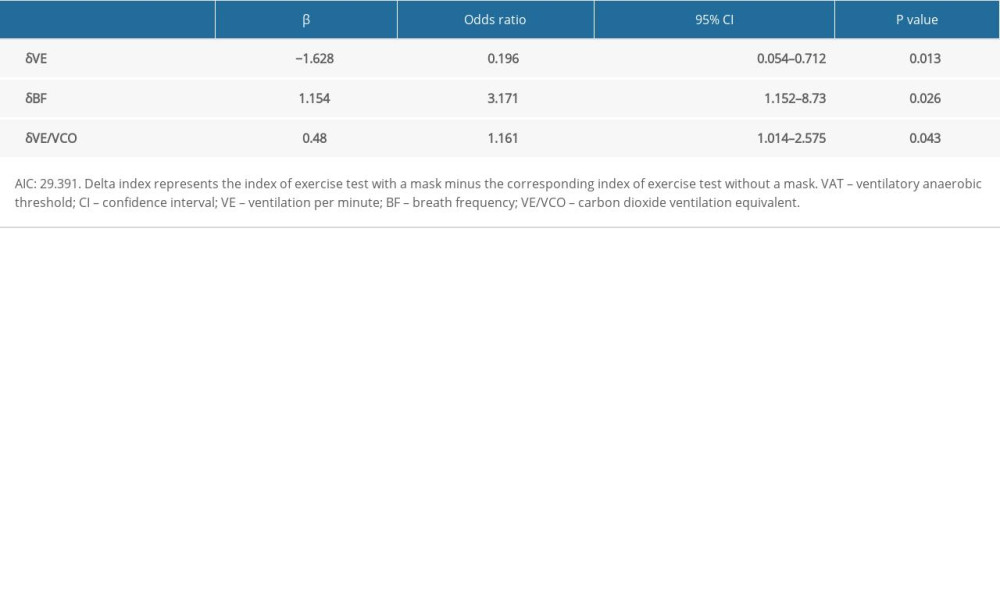
References
1. Chu DK, Akl EA, Duda S, Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: A systematic review and meta-analysis: Lancet, 2020; 395(10242); 1973-87
2. Esposito S, Principi N, Leung CC, Universal use of face masks for success against COVID-19: Evidence and implications for prevention policies: Eur Respir J, 2020; 55(6); 2001260
3. Fikenzer S, Uhe T, Lavall D, Effects of surgical and FFP2/N95 face masks on cardiopulmonary exercise capacity: Clin Res Cardiol, 2020; 109(12); 1522-30
4. Shaw K, Butcher S, Ko J, Wearing of cloth or disposable surgical face masks has no effect on vigorous exercise performance in healthy individuals: Int J Environ Res Public Health, 2020; 17(21); 8110
5. Petru R, Ochmann U, Nowak D, Letter to the editors referring to Fikenzer, S., Uhe, T., Lavall, D., Rudolph, U., Falz, R., Busse, M., Hepp, P., & Laufs, U. (2020). Effects of surgical and FFP2/N95 face masks on cardiopulmonary exercise capacity. Clinical Research in Cardiology: Clin Res Cardiol, 2020; 109(12); 1598-99
6. Fröhlich MJ, Kroidl RF, Welte T, Oxygen Consumption (V’O2) and physical Strainas measured by the occupational activity of cleaning personnel: J Occup Med Toxicol, 2018; 13; 4
7. Chandrasekaran B, Fernandes S, “Exercise with facemask: Are we handling a devil’s sword?” – a physiological hypothesis: Med Hypotheses, 2020; 144; 110002
8. Driver S, Reynolds M, Brown K, Effects of wearing a cloth face mask on performance, physiological and perceptual responses during a graded treadmill running exercise test: Br J Sports Med, 2022; 56(2); 107-13
9. Mapelli M, Salvioni E, De Martino F, “You can leave your mask on”: Effects on cardiopulmonary parameters of different airway protective masks at rest and during maximal exercise: Eur Respir J, 2021; 58(3); 2004473
10. Epstein D, Korytny A, Isenberg Y, Return to training in the COVID-19 era: The physiological effects of face masks during exercise: Scand J Med Sci Sports, 2021; 31(1); 70-75
11. Wasserman K, Whipp BJ, Koyl SN, Anaerobic threshold and respiratory gas exchange during exercise: J Appl Physiol, 1973; 35(2); 236-43
12. Beaver WL, Wasserman K, Whipp BJ, A new method for detecting anaerobic threshold by gas exchange: J Appl Physiol (1985), 1986; 60(6); 2020-27
13. Hopker JG, Jobson SA, Pandit JJ, Controversies in the physiological basis of the ‘anaerobic threshold’ and their implications for clinical cardiopulmonary exercise testing: Anaesthesia, 2011; 66(2); 111-23
14. Ntima NO, Lumb AB, Physiology and conduct of pulmonary function tests: BJA Educ, 2019; 19(6); 198-204
15. Succi PJ, Dinyer TK, Byrd MT, Comparisons of the metabolic intensities at heart rate, gas exchange, and ventilatory thresholds: Int J Exerc Sci, 2020; 13(2); 455-69
16. Sales MM, Sousa CV, da Silva Aguiar S, An integrative perspective of the anaerobic threshold: Physiol Behav, 2019; 205; 29-32
17. Vasconcelos G, Canestri R, Prado R, A comprehensive integrative perspective of the anaerobic threshold engine: Physiol Behav, 2019; 210; 112435
Figures
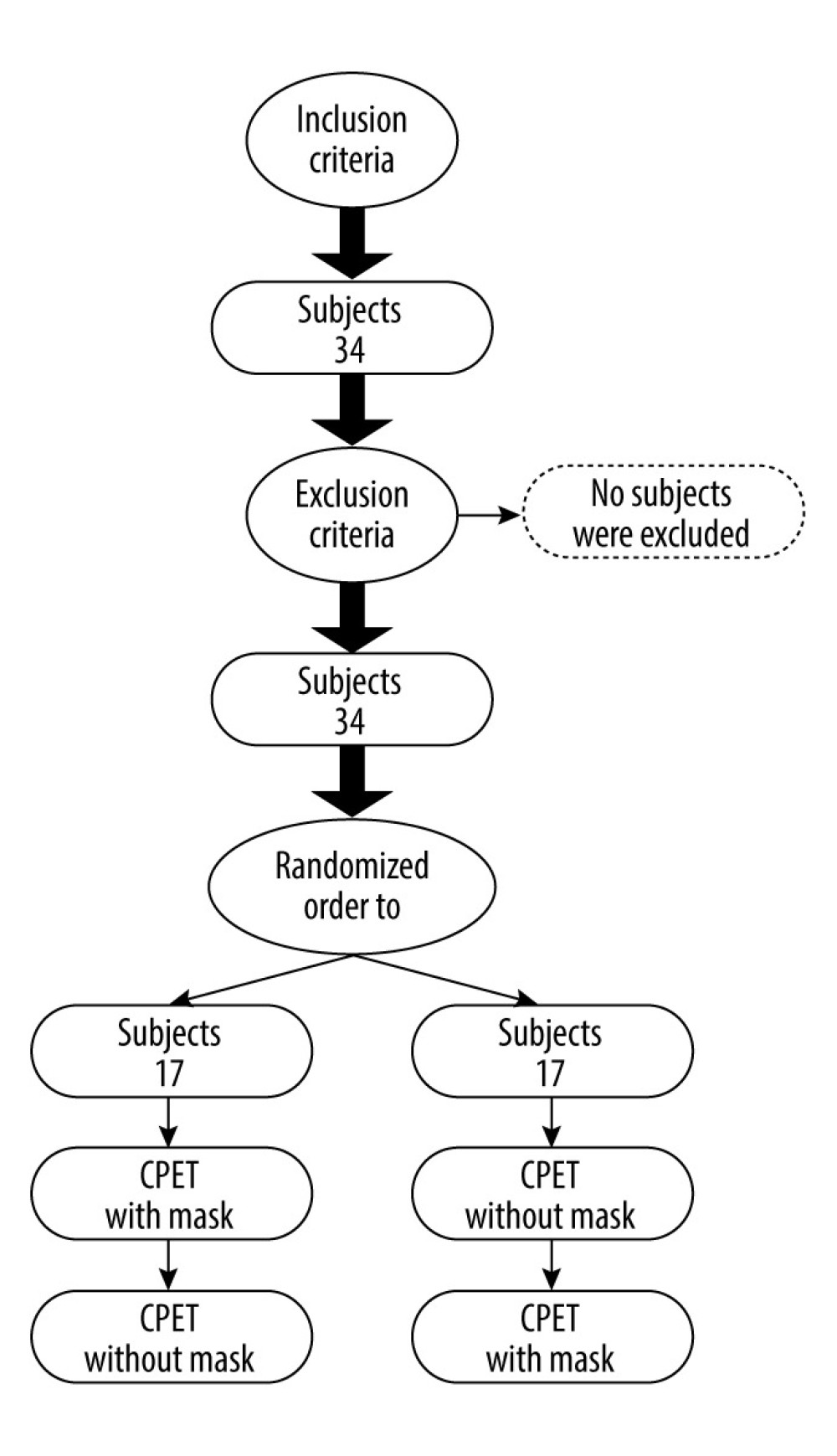 Figure 1. Patient flowchart.
Figure 1. Patient flowchart.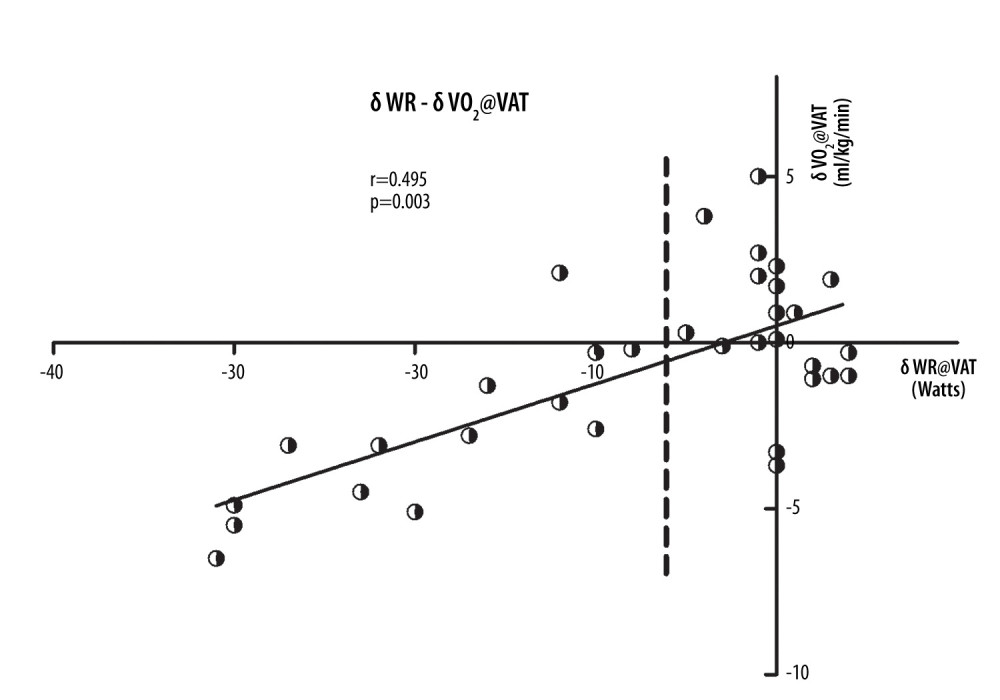 Figure 2. Scatter plots of the δWR and δVO2 at the VAT point. The scatter plot shows a positive linear correlation between δWR@VAT and δVO2@VAT (r=0.495, P=0.003). VAT – ventilatory anaerobic threshold; δWR – work rate difference between 2 exercise tests with and without a mask; δVO2 – oxygen consumption difference between 2 exercise tests with and without a mask.
Figure 2. Scatter plots of the δWR and δVO2 at the VAT point. The scatter plot shows a positive linear correlation between δWR@VAT and δVO2@VAT (r=0.495, P=0.003). VAT – ventilatory anaerobic threshold; δWR – work rate difference between 2 exercise tests with and without a mask; δVO2 – oxygen consumption difference between 2 exercise tests with and without a mask. Tables
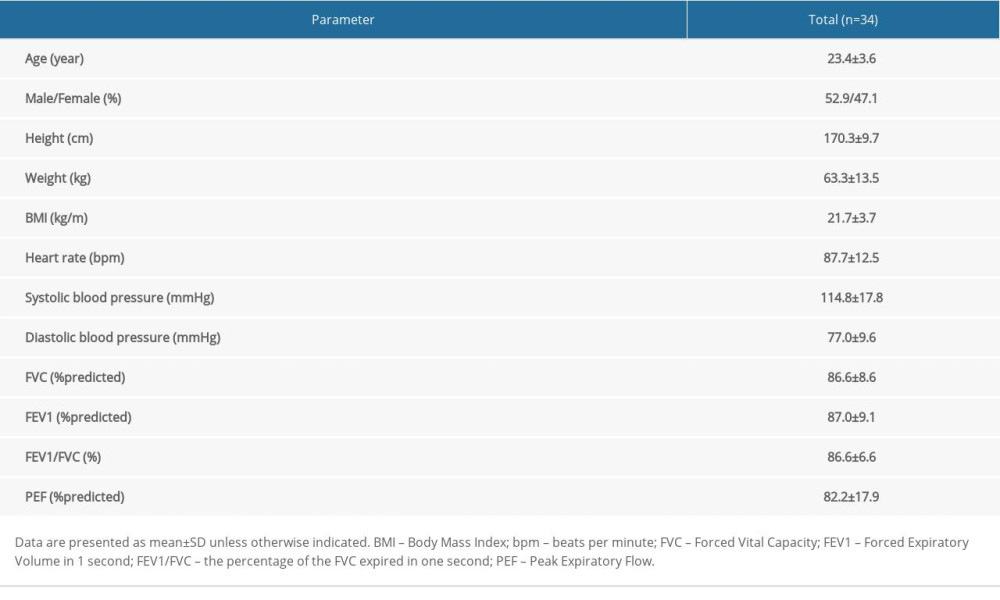 Table 1. Baseline characteristics and physiological indexes of participants.
Table 1. Baseline characteristics and physiological indexes of participants.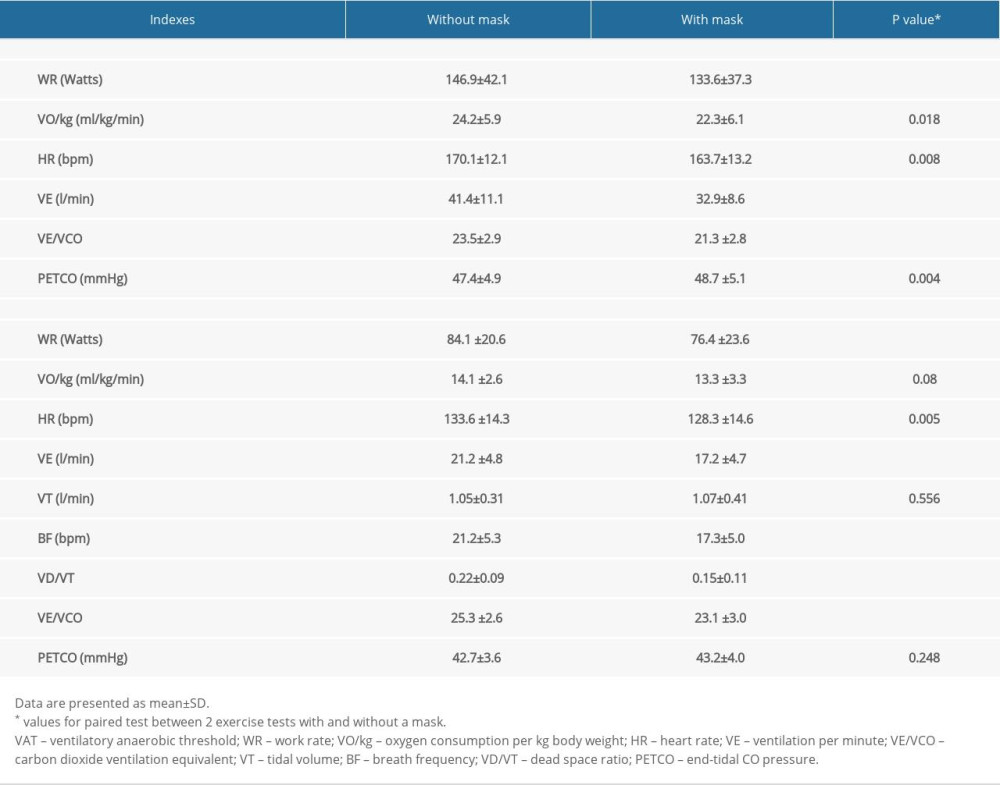 Table 2. Comparison of peak indexes and VAT indexes between 2 exercise tests with and without a mask.
Table 2. Comparison of peak indexes and VAT indexes between 2 exercise tests with and without a mask.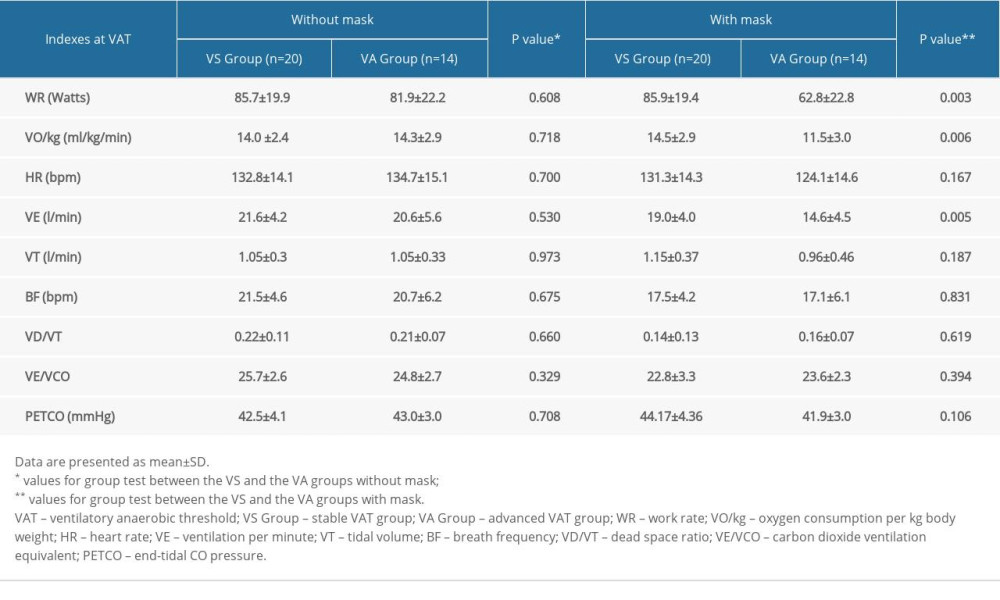 Table 3. Comparison of VAT indexes of 2 exercise tests between the 2 groups.
Table 3. Comparison of VAT indexes of 2 exercise tests between the 2 groups.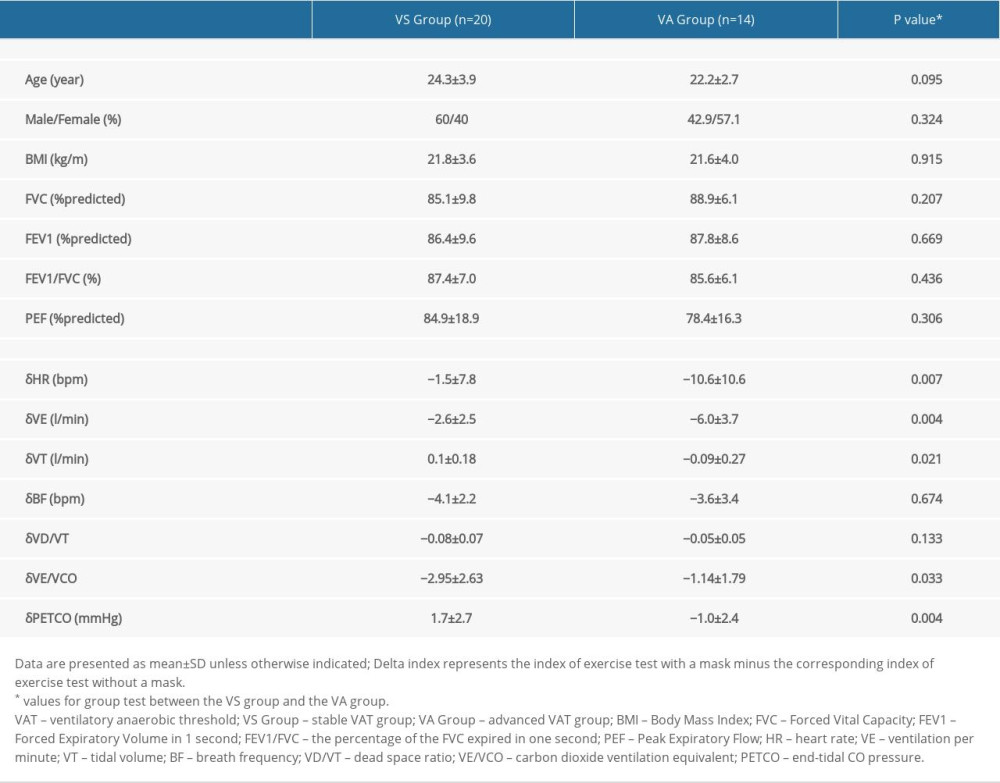 Table 4. Comparison of demographic and physiological characteristics, and delta indicators at VAT after subgrouping.
Table 4. Comparison of demographic and physiological characteristics, and delta indicators at VAT after subgrouping.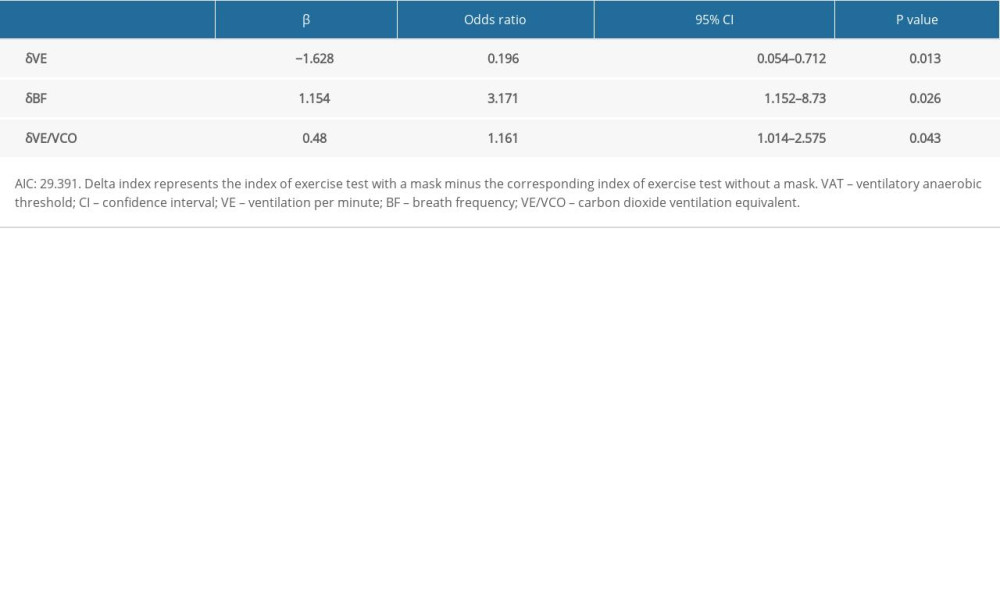 Table 5. Factors associated with being in the advanced VAT group rather than the stable VAT group via multivariable logistic regression analysis.
Table 5. Factors associated with being in the advanced VAT group rather than the stable VAT group via multivariable logistic regression analysis.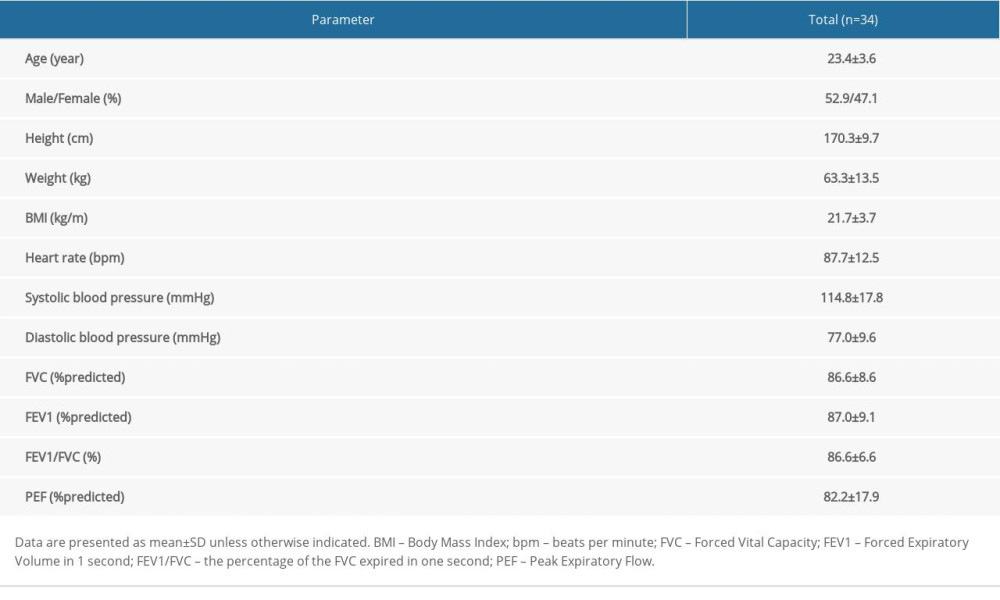 Table 1. Baseline characteristics and physiological indexes of participants.
Table 1. Baseline characteristics and physiological indexes of participants.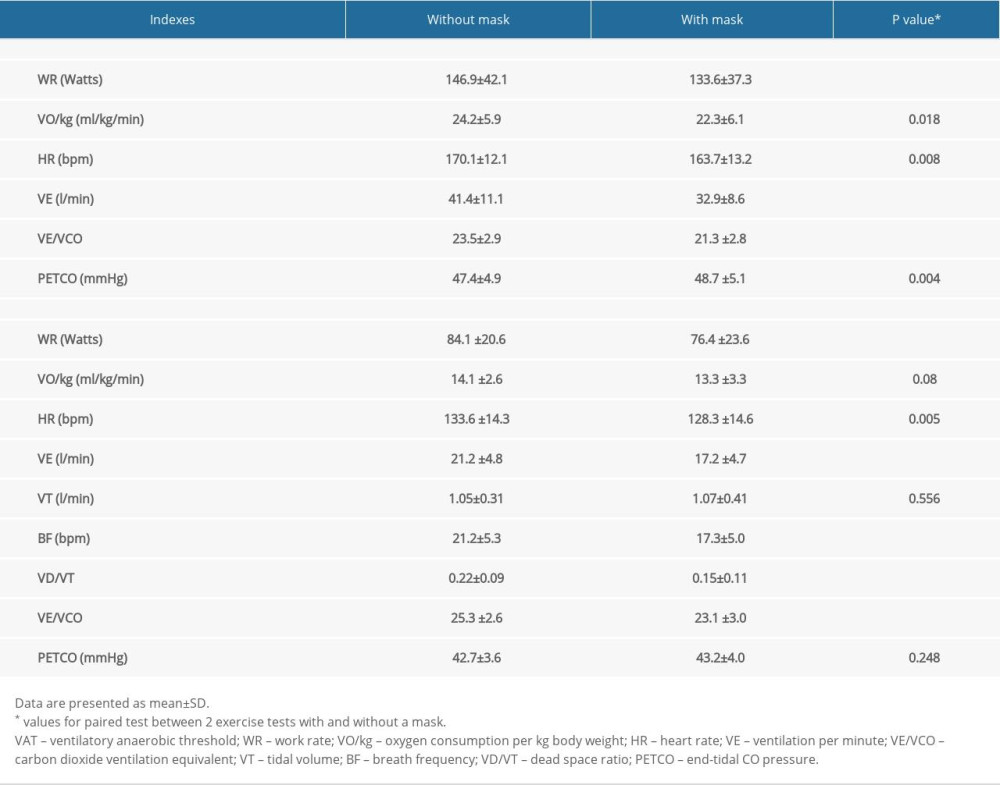 Table 2. Comparison of peak indexes and VAT indexes between 2 exercise tests with and without a mask.
Table 2. Comparison of peak indexes and VAT indexes between 2 exercise tests with and without a mask.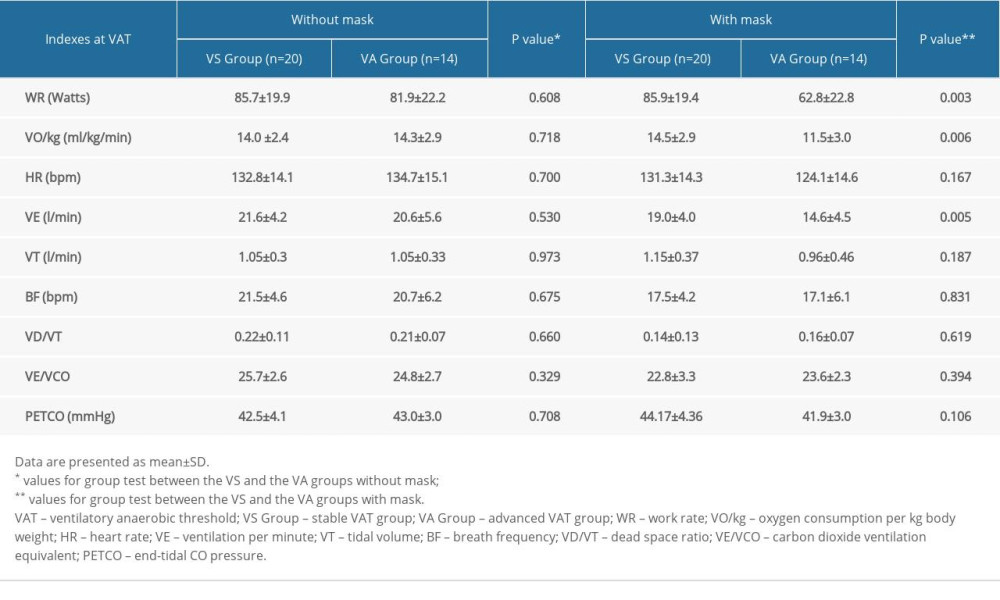 Table 3. Comparison of VAT indexes of 2 exercise tests between the 2 groups.
Table 3. Comparison of VAT indexes of 2 exercise tests between the 2 groups.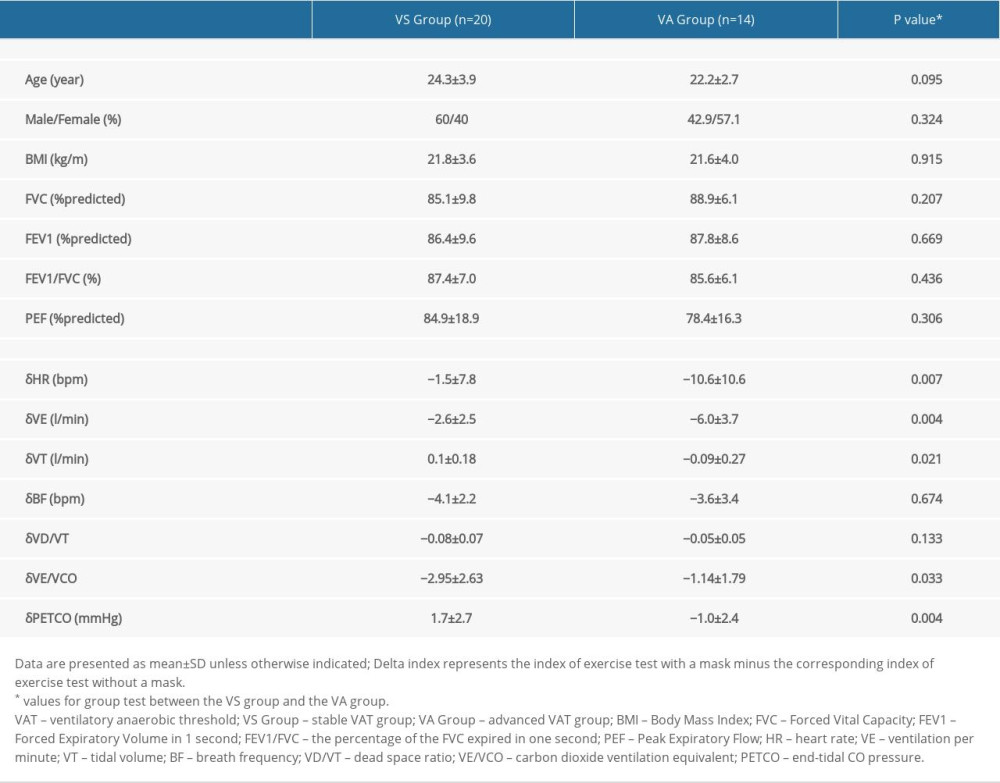 Table 4. Comparison of demographic and physiological characteristics, and delta indicators at VAT after subgrouping.
Table 4. Comparison of demographic and physiological characteristics, and delta indicators at VAT after subgrouping.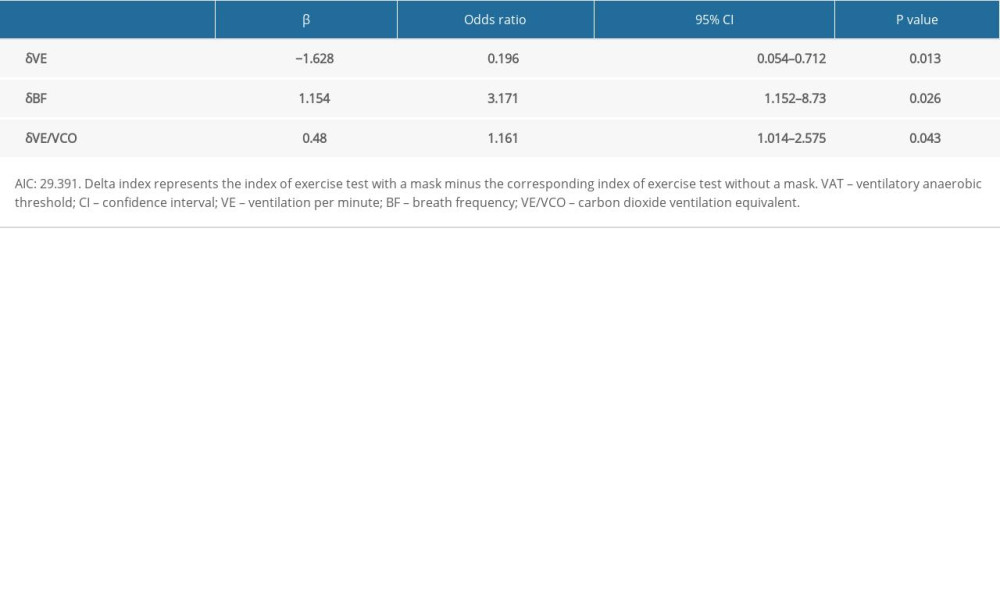 Table 5. Factors associated with being in the advanced VAT group rather than the stable VAT group via multivariable logistic regression analysis.
Table 5. Factors associated with being in the advanced VAT group rather than the stable VAT group via multivariable logistic regression analysis. In Press
18 Apr 2024 : Clinical Research
Comparative Analysis of Open and Closed Sphincterotomy for the Treatment of Chronic Anal Fissure: Safety an...Med Sci Monit In Press; DOI: 10.12659/MSM.944127
08 Mar 2024 : Laboratory Research
Evaluation of Retentive Strength of 50 Endodontically-Treated Single-Rooted Mandibular Second Premolars Res...Med Sci Monit In Press; DOI: 10.12659/MSM.944110
11 Mar 2024 : Clinical Research
Comparison of Effects of Sugammadex and Neostigmine on Postoperative Neuromuscular Blockade Recovery in Pat...Med Sci Monit In Press; DOI: 10.12659/MSM.942773
12 Mar 2024 : Clinical Research
Comparing Neuromuscular Blockade Measurement Between Upper Arm (TOF Cuff®) and Eyelid (TOF Scan®) Using Miv...Med Sci Monit In Press; DOI: 10.12659/MSM.943630
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








