25 May 2022: Meta-Analysis
Effect of the COVID-19 Pandemic on Serum Vitamin D Levels in People Under Age 18 Years: A Systematic Review and Meta-Analysis
Xian Cui1ABCDEF*, Yuhang Zhai2CE, Shuai Wang1BF, Ke Ding1E, Zhenya Yang1E, Yan Tian1D, Tingting Huo1DDOI: 10.12659/MSM.935823
Med Sci Monit 2022; 28:e935823
Abstract
BACKGROUND: During the COVID-19 pandemic the implementation of a range of measures to suppress transmission, such as social distancing and home confinement resulted in limited sunlight exposure and physical inactivity in people under age 18 years, which can elevate the risk of vitamin D deficiency and insufficiency. The aim of this study was to systemically evaluate the effect of the COVID-19 pandemic on serum vitamin D levels in people under age 18 years.
MATERIAL AND METHODS: Following the PRISMA recommendations, we searched PubMed, Embase, and the Cochrane Database for trials from inception to November 3, 2021. All trials assessing the effects of the COVID-19 pandemic on serum vitamin D levels in people under age 18 years were included and analyzed. Mean differences (MDs) of serum 25-hydroxyvitamin D (25[OH] D) levels before and during the COVID-19 pandemic were calculated and pooled using a random-effects model. Risk differences were used to assess changes in the proportions of people under age 18 years with vitamin D deficiency.
RESULTS: Our analysis included 5 studies comprising 4141 people under age 18 years. The combined result MD of serum 25(OH)D levels before and during the COVID-19 pandemic as 3.28 ng/mL, 95% CI=0.95-5.62 ng/mL, P<0.01] indicated serum 25(OH)D levels were significantly lower during the COVID-19 pandemic. The decreased serum 25(OH)D level was not observed among infants (age under 1 year) (P=0.28).
CONCLUSIONS: During the COVID-19 pandemic, the serum vitamin D levels of people under age 18 years were significantly lower and vitamin D supplementation for people under age 18 years might reduce the risk of COVID-19. More research is needed to validate the present findings.
Keywords: Vitamin D Deficiency, Meta-Analysis, COVID-19, Adolescent, Calcifediol, Humans, Infant, Pandemics, Vitamin D
Background
The epidemic of coronavirus disease 2019 (COVID-19) is currently having a damaging impact on almost all countries around the world. Characterized by an approximately 2% mortality rate and the absence of medical countermeasures, COVID-19 remains a major public health threat globally [1,2]. Vitamin D is a steroid hormone essential in regulating body levels of calcium and phosphorus and mineralization of bones [3,4]. Insufficient levels of serum vitamin D are strongly associated with various diseases, including total cancer incidence, diabetes, and infectious diseases [5,6].
A growing body of circumstantial evidence shows an association of COVID-19 with serum vitamin D levels [7,8]. COVID-19 incidence and mortality were found to be strongly associated with vitamin D status in various populations [9]. Similar associations were also seen in children [10]. Since late December 2019, governments from various countries have implemented a series of measures to control the COVID-19 pandemic, such as social distancing and home confinement, which potentially limit sunlight exposure or physical activity of children. A main source of acquiring vitamin D is sunlight exposure. Several studies reported an elevated risk of vitamin D deficiency among COVID-19-negative children [12,13]. Although the COVID-19 pandemic has been reported to significantly affect serum vitamin D levels in children, it has not been systemically summarized.
In this study, we aimed to systemically evaluate the effect of the COVID-19 pandemic on serum vitamin D levels in people under age 18 years.
Material and Methods
LITERATURE SEARCH:
This study was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) [14] guidelines for the trial identification, data extraction and integrity, assessment of bias, and sensitivity analyses. We searched PubMed, Embase, and the Cochrane Database for eligible publications from inception to November 3, 2021. We used the following keywords and phrases: “COVID-19”, “coronavirus disease 2019”, “SARS-CoV-2”, “severe acute respiratory syndrome coronavirus 2”, “vitamin D”, “25-Hydroxyvitamin D 2”, “child”, “infants”, and “pediatric”. Detailed search strategies for each database can be found in the Supplementary Material. To include more studies, we also examined the reference lists of relevant studies.
ELIGIBILITY CRITERIA:
The inclusion criteria were: (1) studies investigating the serum vitamin D levels of participants before and during the COVID-19 pandemic; (2) study population aged <18 years and did not receive vitamin D supplementations or any other medications; (3) study population was COVID-19-negative; (4) studies published in English.
Exclusion criteria were: (1) letters, case reports, reviews, animal experiments, and expert opinions; (2) studies that included outpatients or asymptomatic COVID-19 patients; (3) studies published in languages other than English; (4) duplicate publications.
DEFINITIONS OF VITAMIN D DEFICIENCY AND INSUFFICIENCY:
Because vitamin D is converted by 25-hydroxylase to 25-hydroxyvitamin D [25(OH)D] in the liver, serum vitamin D was defined as serum 25(OH)D concentrations. Following the Endocrine Society’s Clinical Practice Guideline [15], we defined vitamin D deficiency, insufficiency, and sufficiency according to serum concentrations of 25(OH)D <20 ng/mL (<50 nmol/L), 21–29 ng/mL (51–74 nmol/L), and 30–100 ng/mL (75–250 nmol/L), respectively.
DATA EXTRACTION:
Two authors (XC and SW) independently screened the studies retrieved form the above-mentioned databases for eligible studies following the inclusion criteria. Necessary information was independently extracted by the 2 authors using a customized and standardized form. Any discrepancy was resolved by discussion with the third author (TTH).
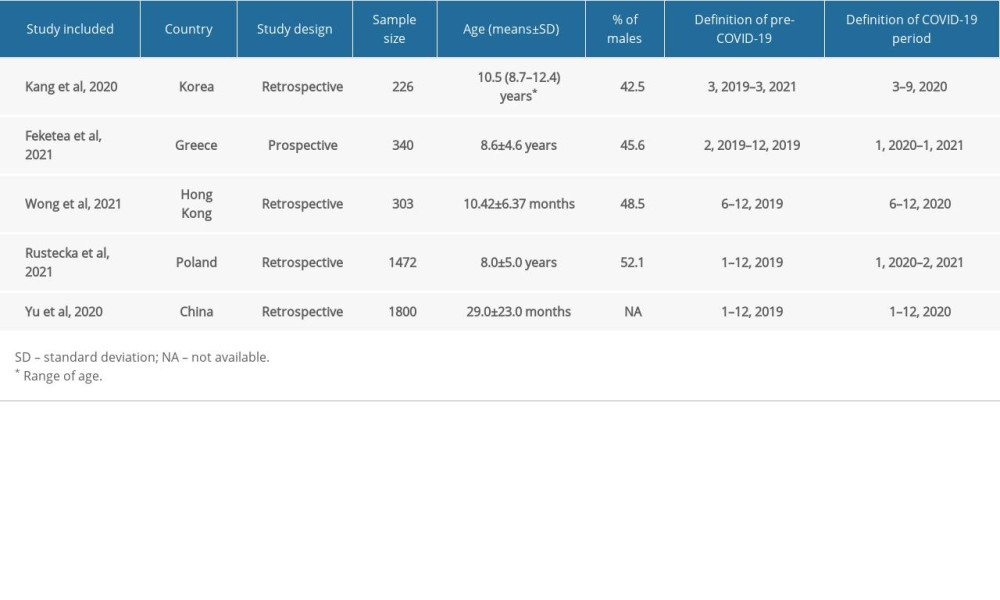
For included studies, the following information was extracted: the first author, publication year, country, mean ages and proportions of males of the study population, sample size, definition of COVID-19 pandemic period, and serum vitamin D levels before and during the COVID-19 pandemic.
QUALITY SCORING OF STUDIES:
Two reviewers (XC and SW) independently assessed study quality using the Newcastle-Ottawa Scale (NOS) [16], a risk of bias assessment tool for observational studies. Using this tool, 3 domains were assessed: (1) selection of study population (4 items); (2) comparability of groups (2 items); and (3) ascertainment of exposure and outcomes (3 items). Studies with NOS scores 7–9 were high-quality, scores 4–6 had moderate risk of bias, and scores 0–3 had very high risk of bias.
STATISTICAL ANALYSIS:
Changes of the serum vitamin D levels before and during the COVID-19 pandemic were evaluated by pooling mean differences (MDs) or risk differences. MDs or risk differences from included studies were combined using a random-effects model. Stratification analysis was done according the age of the participants as infants and children (infants were defined as <1 year old and children were defined as 1–18 years old).
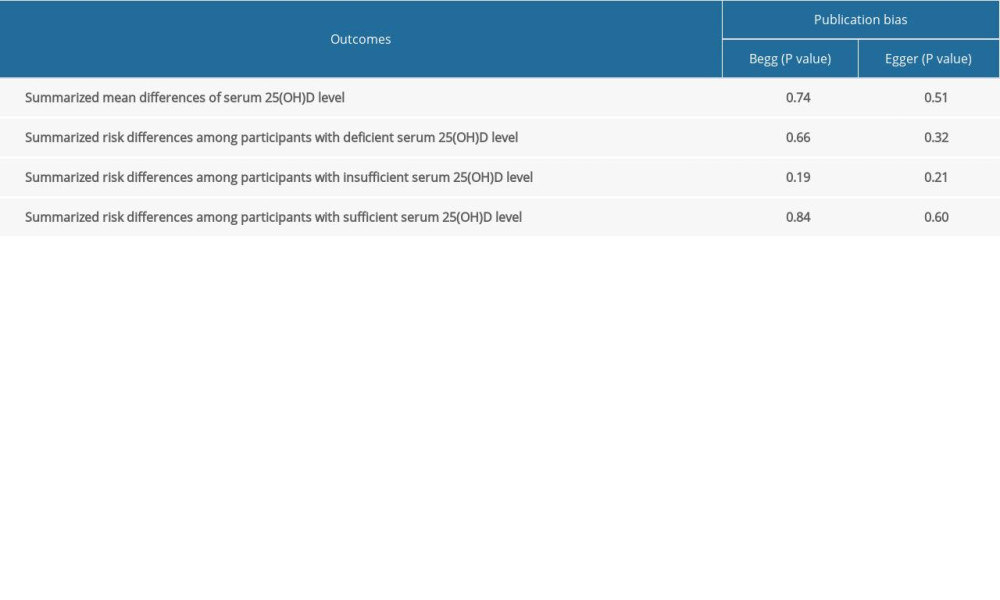
Heterogeneity was assessed using Cochran’s Q test and Higgins’s I2, with I2 >50% and a P value <0.10 suggested significant heterogeneity [17]. To explore the sources of significant heterogeneity, the enrolled studies were sequentially excluded to observe the overall impact of the individual study. Potential publication bias was evaluated using Begg’s rank correlation [18] and Egger’s weighted regression methods [19].
Review Manager Version 5.3 (Cochrane Collaboration, Oxford, United Kingdom) and STATA 15.0 (Stata Corporation, College Station, TX) were used to perform statistical analyses. A 2-side
Results
STUDY SELECTION:
As illustrated in Figure 1, a total of 748 studies were identified through the initial searches in the above-mentioned databases; 317 were excluded due duplication among various databases and 256 papers were excluded by browsing the titles or abstracts. After retrieving 33 full-length manuscripts, 5 studies [12,13,20–22] were included into the current study.
STUDY CHARACTERISTICS:
The 5 studies encompassed a total of 4141 people under age 18 years and were published between 2020 and 2021. The sample size ranged from 226 to 1800. The studies were conducted in 1 each in South Korea (21), Greece (20), Hong Kong (13), Poland (12), and China (22). Most studies (4/5) were retrospective studies. Three studies [12,20,21] focused on people age 1–18 years and 2 on infants [13,22]. Nearly half of the study population were males. All studies defined the pre-COVID-19 period as the year 2019 and the COVID-19 period as the year 2020. The demographic characteristics of the study population from the included studies are presented in Table 1.
QUALITY ASSESSMENT OF STUDIES:
NOS for included eligible studies are shown in Supplementary Table 1. All 5 included studies were evaluated as moderate or high quality, of which 2 each scored 6 points and 7 points, and 1 scored 8 points.
IMPACT OF THE COVID-19 PANDEMIC ON SERUM VITAMIN D LEVELS:
Of the 5 included studies, 4 [12,13,21,22] reported serum 25(OH)D levels before and during then COVID-19 pandemic. As shown in Figure 2, when summarizing the serum 25(OH)D levels together, a statistically significant decrease was seen with pooled MD as 3.28 ng/mL (95% confidence interval (CI)=0.95–5.62 ng/mL, P<0.01) with a significant heterogeneity (I2=85%).
To explore the potential source of the heterogeneity, we excluded included studies sequentially. As illustrated in Supplementary Figure 1, when we excluded the study conducted by Yu et al [22], the heterogeneity was significantly decreased (I2=0%)
As presented in Figure 3, 2 studies reported serum 25(OH)D level changes among infants (<1 year old). No statistically significant serum 25(OH)D level change was seen, with P value 0.28.
According to serum 25(OH)D level, 3 studies [12,20,22] categorized serum vitamin D levels into vitamin D deficiency, insufficiency, and sufficiency (Figure 4). No significantly increased vitamin D deficiency and vitamin D insufficiency risk were seen, with pooled risk differences as 0.03 (95% CI=−0.11–0.18, P=0.64, I2=96%) and −0.01 (95% CI=−0.09–0.07, P=0.81, I2=81%), respectively, which indicates the proportions of vitamin D deficiency and vitamin D insufficiency among children remained unchanged.
Similarly, to explore the potential source of the heterogeneity, we excluded the study specifically focused on infants (Supplementary Figure 2). Decreased heterogeneity was then 0%, 36%, and 0% for vitamin D deficiency, vitamin D insufficiency, and vitamin D sufficiency risk, respectively. Then we assessed the association among infants (<1 year old). Similarly, no statistically significant differences were seen (Supplementary Figure 3).
PUBLICATION BIAS:
No potential publication bias was observed (P>0.05), and the detailed results of potential publication bias can be found in Supplementary Table 2.
Discussion
To the best of our knowledge, the current study is the first systematic review and meta-analysis study to summarize the impact of the COVID-19 pandemic on serum vitamin D levels in people under age 18 years. Five studies with a total 4141 pediatric participants were included and analyzed. For the pediatric population, the serum vitamin D levels were significantly decreased during the COVID-19 pandemic.
The general metabolism and actions of vitamin D are well-established [23]. Vitamin D has 2 forms (D2 and D3), which differ chemically in their side chains. Vitamin D2 is obtained from daily diet such as oil-rich fish [24]. Vitamin D3 is produced in the skin from 7-dehydrocholesterol by UV irradiation. Due to the COVID-19 pandemic, many negative effects on lifestyle choices were reported [25]. A study conducted by Xiang et al [26] in 2426 children and adolescents from China reported a substantial decrease in physical activity and increase in screen time during the COVID-19 pandemic. Another study, conducted in Italy, also reported significantly less time spent in sports activities [27]. The home confinement and decreased physical activity during the COVID-19 pandemic thus resulted in inadequate exposure to sunlight, which can lead to decreased serum vitamin D levels. Moreover, studies also reported that red meat, high-sugar and high-fat diets, and sugary drink intakes increased significantly during the lockdown and school closure [25,26,28]. The daily diet changes might also promote decreased serum vitamin D levels.
The findings of our study that the serum vitamin D level was significantly decreased during COVID-19 pandemic highlight the importance of vitamin D supplementation people under age 18 years. A recent meta-analysis reported that low serum 25 (OH) vitamin D level was strongly associated with an increased risk of COVID-19 infection [29]. Another meta-analysis reported that there was about 3 times higher chance of getting infected with COVID-19 among vitamin D-deficient individuals and about 5 times increased probability of developing severe COVID-19 disease in vitamin D-deficient patients [30]. Improving serum vitamin D levels in people under age 18 years therefore has a potential benefit in reducing the risk of acquiring COVID-19. Grant et al [7] recommended that people at risk of influenza and/or COVID-19 consider taking 10 000 IU/d of vitamin D3 for a few weeks to rapidly raise 25(OH)D concentrations, followed by 5000 IU/d.
While interpreting the findings in the current study, limitations need to be considered. First, most of the studies did not compare the prior and current COVID-19 period serum vitamin D levels in the same population. Even if the sensitivity analyses and subgroup analyses were performed carefully, the heterogeneities of some comparisons remained substantial. Second, the mean ages of the participants among the 5 included studies varied greatly. Because age has an important effect on living habits, the impact of the COVID-19 pandemic on serum vitamin D levels may be significantly different, such between infants versus kindergarten or elementary school students. However, as described above, 2 studies provided data on infants <1 year and we observed they differed from the entire pediatric population. Third, the serum vitamin D levels might be affected by various factors, such as the season. However, due to the limited number of included studies and the information provided by each study, we could not perform more subgroup analyses. Fourth, potential language bias might exist because we only included articles published in English. Fifth, possible publication bias could not be assessed for all analyses, as a small number of studies were included.
Conclusions
Our meta-analysis provides pooled results based on 5 studies and reported the quantized changes in serum vitamin D levels during the COVID-19 pandemic. Vitamin D supplementation may be needed for people under age 18 years. The measures aimed to reduce the transmission of SARS-CoV-2 need to take into account the detrimental effects on people under age 18 years. Further research should focus the long-term impact of the COVID-19 pandemic on serum vitamin D levels and health outcomes.
Figures
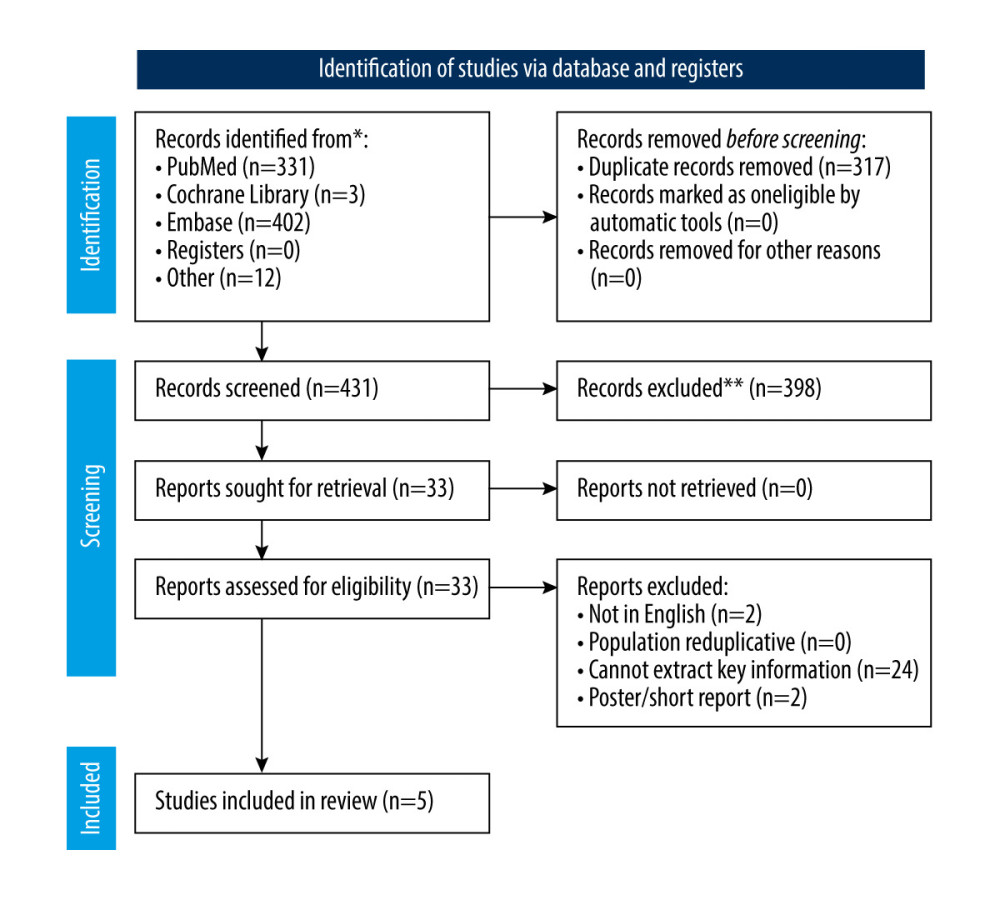 Figure 1. Flow chart of the study selection.
Figure 1. Flow chart of the study selection. 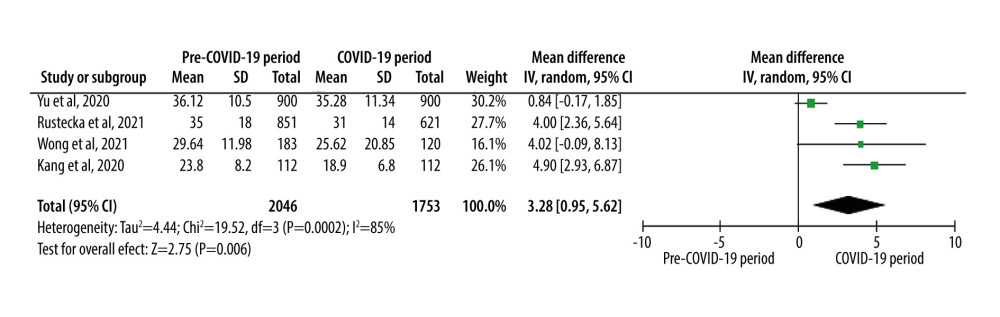 Figure 2. Summarized mean differences of serum 25(OH)D level among all participants.
Figure 2. Summarized mean differences of serum 25(OH)D level among all participants. 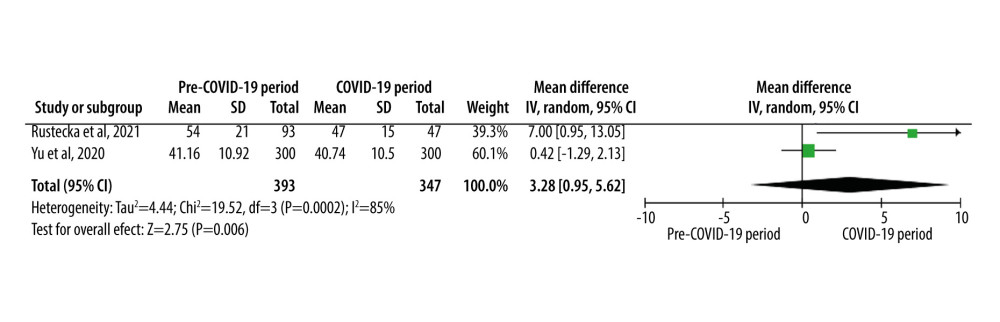 Figure 3. Summarized mean differences of serum 25(OH)D level among infants (aged <1 year).
Figure 3. Summarized mean differences of serum 25(OH)D level among infants (aged <1 year). 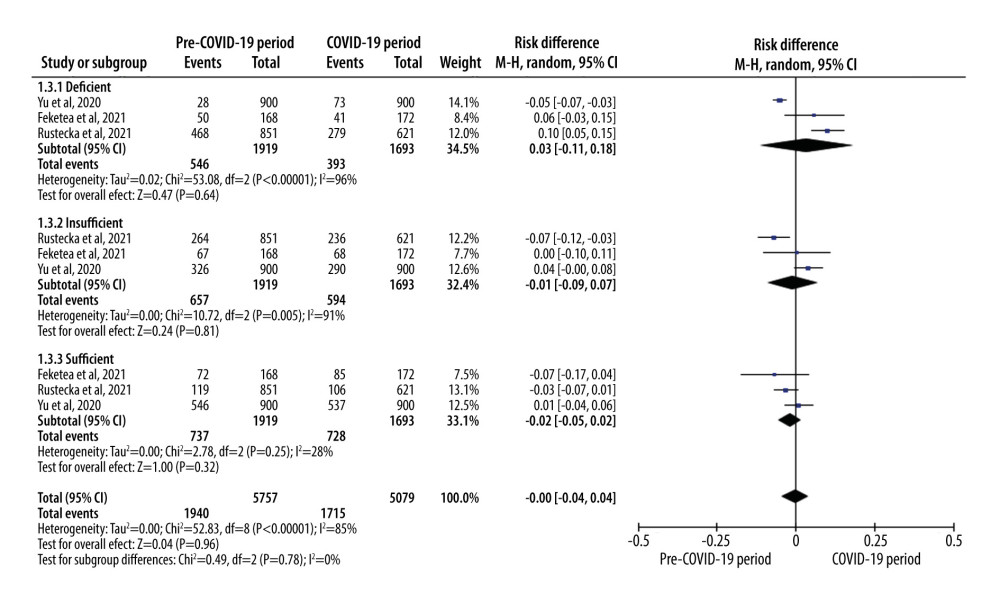 Figure 4. Summarized risk differences among participants by serum 25(OH)D level status.
Figure 4. Summarized risk differences among participants by serum 25(OH)D level status. References
1. Gavriatopoulou M, Ntanasis-Stathopoulos I, Korompoki E, Emerging treatment strategies for COVID-19 infection: Clin Exp Med, 2021; 21; 167-79
2. Ita K, Coronavirus disease (COVID-19): Current status and prospects for drug and vaccine development: Arch Med Res, 2021; 52; 15-24
3. Dusso AS, Brown AJ, Slatopolsky E, Vitamin D: Am J Physiol Renal Physiol, 2005; 289; F8-28
4. Harrison HE, Vitamin D: Prog Clin Biol Res, 1981; 61; 95-108
5. Holick MF, The vitamin D deficiency pandemic: Approaches for diagnosis, treatment and prevention: Rev Endocr Metab Disord, 2017; 18; 153-65
6. Holick MF, Chen TC, Vitamin D deficiency: A worldwide problem with health consequences: Am J Clin Nutr, 2008; 87; 1080S-86S
7. Grant WB, Lahore H, McDonnell SL, Evidence that Vitamin D supplementation could reduce risk of influenza and COVID-19 infections and deaths: Nutrients, 2020; 12; 988
8. Jolliffe DA, Camargo CA, Sluyter JD, Vitamin D supplementation to prevent acute respiratory infections: A systematic review and meta-analysis of aggregate data from randomised controlled trials: Lancet Diabetes Endocrinol, 2021; 9; 276-92
9. Mitchell F, Vitamin-D and COVID-19: Do deficient risk a poorer outcome?: Lancet Diabetes Endocrinol, 2020; 8; 570
10. Yilmaz K, Sen V, Is vitamin D deficiency a risk factor for COVID-19 in children?: Pediatr Pulmonol, 2020; 55; 3595-601
11. Panfili FM, Roversi M, D’Argenio P, Possible role of vitamin D in COVID-19 infection in pediatric population: J Endocrinol Invest, 2021; 44; 27-35
12. Rustecka A, Maret J, Drab A, The impact of COVID-19 Ppandemic during 2020–2021 on the Vitamin D serum levels in the paediatric population in Warsaw, Poland: Nutrients, 2021; 13; 1990
13. Wong RS, Tung KTS, So HK, Impact of COVID-19 pandemic on serum vitamin D level among infants and toddlers: An interrupted time series analysis and before-and-after comparison: Nutrients, 2021; 13; 1270
14. Page MJ, McKenzie JE, Bossuyt PM, The PRISMA 2020 statement: An updated guideline for reporting systematic reviews: BMJ, 2021; 372; n71
15. Holick MF, Binkley NC, Bischoff-Ferrari HA, Evaluation, treatment, and prevention of vitamin D deficiency: An Endocrine Society clinical practice guideline: J Clin Endocrinol Metab, 2011; 96; 1911-30
16. Wells G, Shea B, O’Connel D, The Newcastle Ottawa Scale (NOS) for assessing the quality of non-randomised studies in meta-analysis
17. Higgins JP, Thompson SG, Deeks JJ, Altman DG, Measuring inconsistency in meta-analyses: BMJ, 2003; 327; 557-60
18. Begg CB, Mazumdar M, Operating characteristics of a rank correlation test for publication bias: Biometrics, 1994; 50; 1088-101
19. Egger M, Davey Smith G, Bias in meta-analysis detected by a simple, graphical test: BMJ, 1997; 315; 629-34
20. Feketea G, Vlacha V, Tsiros G, Vitamin D levels in asymptomatic children and adolescents with atopy during the COVID-19 era: J Pers Med, 2021; 11; 712
21. Kang HM, Jeong DC, Suh BK, Ahn MB, The impact of the coronavirus disease-2019 pandemic on childhood obesity and vitamin D status: J Korean Med Sci, 2021; 36; e21
22. Yu L, Ke HJ, Che D, Effect of pandemic-related confinement on vitamin D status among children aged 0–6 years in Guangzhou, China: A cross-sectional study: Risk Manag Healthc Policy, 2020; 13; 2669-75
23. Holick MF, Vitamin D deficiency: N Engl J Med, 2007; 357; 266-81
24. Nair R, Maseeh A, Vitamin D: The “sunshine” vitamin: J Pharmacol Pharmacother, 2012; 3; 118-26
25. Di Renzo L, Gualtieri P, Pivari F, Eating habits and lifestyle changes during COVID-19 lockdown: An Italian survey: J Transl Med, 2020; 18; 229
26. Xiang M, Zhang Z, Kuwahara K, Impact of COVID-19 pandemic on children and adolescents’ lifestyle behavior larger than expected: Prog Cardiovasc Dis, 2020; 63; 531-32
27. Pietrobelli A, Pecoraro L, Ferruzzi A, Effects of COVID-19 lockdown on lifestyle behaviors in children with obesity living in Verona, Italy: A longitudinal study: Obesity (Silver Spring), 2020; 28; 1382-85
28. Cancello R, Soranna D, Zambra G, Determinants of the lifestyle changes during COVID-19 pandemic in the residents of Northern Italy: Int J Environ Res Public Health, 2020; 17; 6287
29. Teshome A, Adane A, Girma B, Mekonnen ZA, The impact of vitamin D level on COVID-19 infection: Systematic review and meta-analysis: Front Public Health, 2021; 9; 624559
30. Ghasemian R, Shamshirian A, Heydari K, The role of vitamin D in the age of COVID-19: A systematic review and meta-analysis: Int J Clin Pract, 2021; 75; e14675
Figures
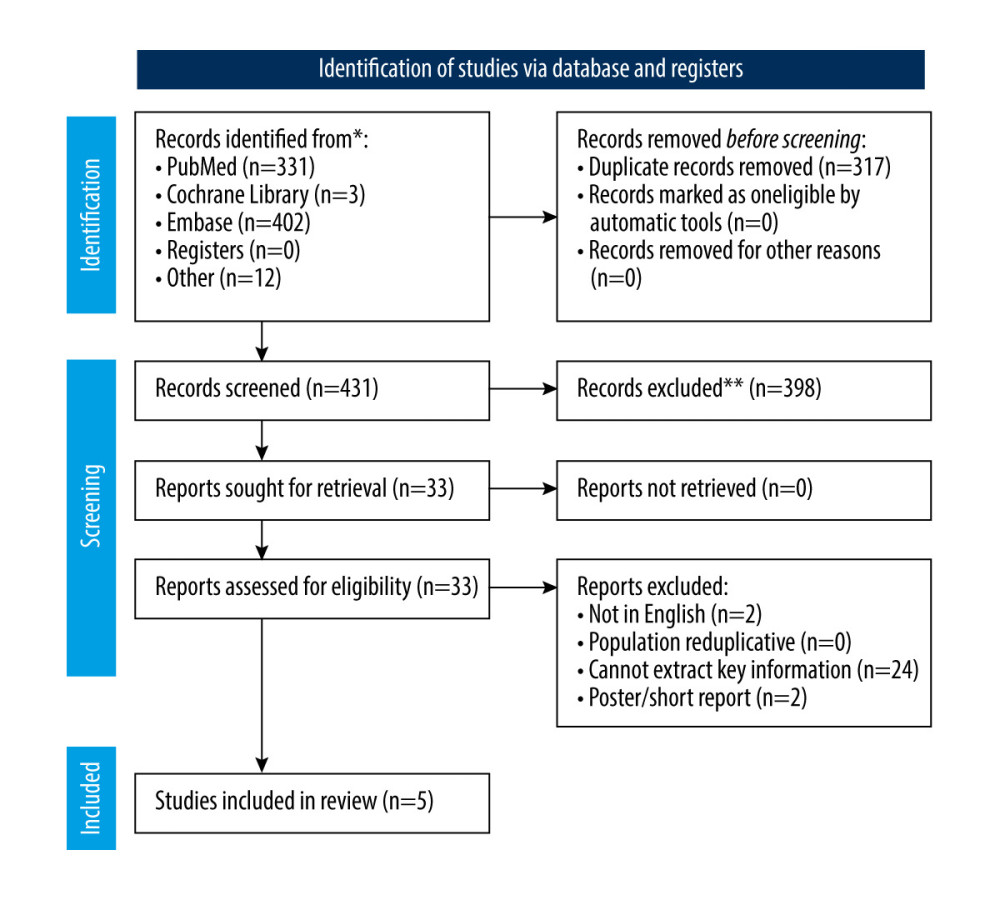 Figure 1. Flow chart of the study selection.
Figure 1. Flow chart of the study selection.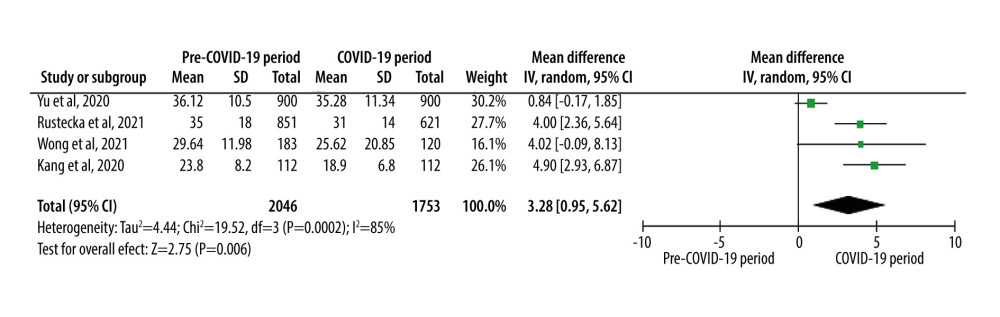 Figure 2. Summarized mean differences of serum 25(OH)D level among all participants.
Figure 2. Summarized mean differences of serum 25(OH)D level among all participants.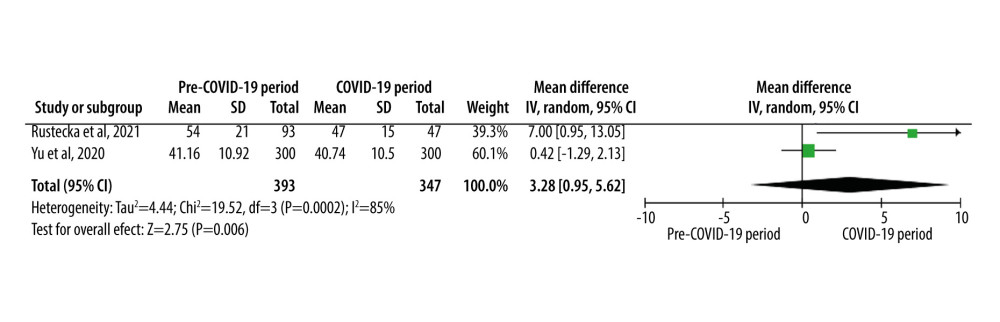 Figure 3. Summarized mean differences of serum 25(OH)D level among infants (aged <1 year).
Figure 3. Summarized mean differences of serum 25(OH)D level among infants (aged <1 year).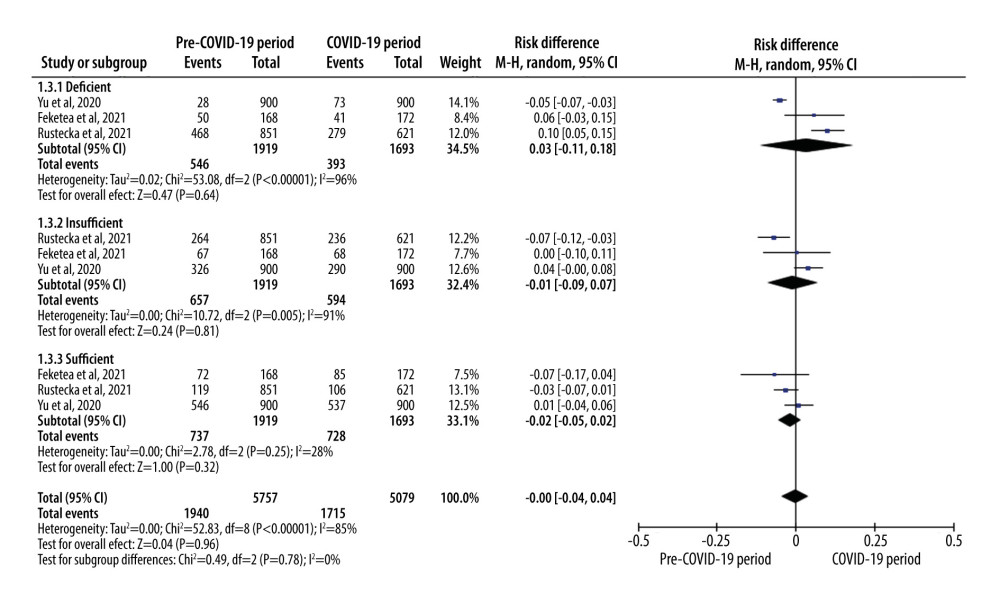 Figure 4. Summarized risk differences among participants by serum 25(OH)D level status.
Figure 4. Summarized risk differences among participants by serum 25(OH)D level status. In Press
18 Apr 2024 : Clinical Research
Comparative Analysis of Open and Closed Sphincterotomy for the Treatment of Chronic Anal Fissure: Safety an...Med Sci Monit In Press; DOI: 10.12659/MSM.944127
08 Mar 2024 : Laboratory Research
Evaluation of Retentive Strength of 50 Endodontically-Treated Single-Rooted Mandibular Second Premolars Res...Med Sci Monit In Press; DOI: 10.12659/MSM.944110
11 Mar 2024 : Clinical Research
Comparison of Effects of Sugammadex and Neostigmine on Postoperative Neuromuscular Blockade Recovery in Pat...Med Sci Monit In Press; DOI: 10.12659/MSM.942773
12 Mar 2024 : Clinical Research
Comparing Neuromuscular Blockade Measurement Between Upper Arm (TOF Cuff®) and Eyelid (TOF Scan®) Using Miv...Med Sci Monit In Press; DOI: 10.12659/MSM.943630
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952