12 December 2021: Clinical Research
Influenza and Influenza-Like Respiratory Virus Infections in Children During the 2019/20 Influenza Season and the COVID-19 Pandemic in Poland: Data from the National Influenza Centre, the Department of Influenza Research at the National Institute of Public Health, and 16 Voivodeship Sanitary and Epidemiological Stations
Katarzyna Kondratiuk1ACDEF*, Ewelina Hallmann1CDEF, Katarzyna Łuniewska1CDEF, Karol SzymańskiDOI: 10.12659/MSM.934862
Med Sci Monit 2021; 27:e934862
Abstract
BACKGROUND: This population study aimed to investigate influenza and influenza-like respiratory virus infections in children during the 2019/20 influenza season and the coronavirus disease 2019 (COVID-19) pandemic in Poland.
MATERIAL AND METHODS: This study analyzed data from the National Influenza Centre, the Department of Influenza Research at the National Institute of Public Health, and 16 Voivodeship Sanitary and Epidemiological Stations in Poland. Nose and throat swabs were obtained from children during the 2019/20 influenza season and the COVID-19 pandemic. Viral RNA detection was performed using quantitative reverse transcription-polymerase chain reaction (qRT-PCR) to diagnose influenza virus infection and viral subtypes.
RESULTS: In the analyzed group, both cases of influenza A and B and infections with influenza-like viruses were confirmed. Among all cases caused by influenza viruses, influenza A was more frequent than B, with predominance of the A/H1N1/pdm09 subtype. The flu-like virus which infected most children was the human respiratory syncytial virus (RSV). The greatest number of cases with RSV was registered in the group of the youngest children (0-4 years).
CONCLUSIONS: This population study from Poland showed that during the COVID-19 pandemic, and during the winter influenza season of 2019/20, influenza and influenza-like viral infections in children showed some differences from previous influenza seasons. The findings highlight the importance of viral infection surveillance and influenza vaccination in the pediatric population.
Keywords: Epidemiology, Influenza A virus, Influenza B virus, Influenza, Human, Respiratory Syncytial Virus, Human, Academies and Institutes, Age Distribution, COVID-19, Child, Child, Preschool, Humans, Infant, Male, Pandemics, Poland, Polymerase Chain Reaction, SARS-CoV-2
Background
Every epidemic season, infections due to influenza viruses are a common cause of illnesses among children. Both healthy and chronically ill children can be affected by complications from the virus itself or from a secondary bacterial infection.
Influenza is an acute infectious disease caused by a flu virus that affects the respiratory tract. Humans are vulnerable to A, B, and C subtypes, which most often spread by airborne droplets. Influenza A virus additionally exists in the form of different subtypes, eg, A/H1N1, A/H3N2. Influenza A is the most severe one, while influenza B has milder symptoms. Children are most often infected with the influenza C virus, in which case the course of the disease is usually mild. The duration of influenza and its course depend not only on the properties of the pathogen, but also on the physical condition and response of a person’s immune system.
The influenza virus is spread from person to person by airborne droplets, by transmission of large particles (contamination by contact with contaminated objects or hands is also possible). The incubation period is on average 1–2 days (1–4 days). The period of infectivity depends mainly on the immune status of the organism and the age of the patient. Healthy adults without comorbidities can become infected even a day before and 5–7 days after the first symptoms of the disease appear. Children and people with impaired immune systems may shed the virus a few days before the symptoms appear, up to more than 10 days after the symptoms of the infection have ceased [1]. Characteristic to influenza is a sudden onset of symptoms, which notably include high fever, even up to 40°C. Among the most common symptoms of influenza in adults, we also observe muscle aches, headaches, chills, general weakness, or breakdown. Also, there may be dry cough, obstruction of the upper respiratory tract, and runny nose. In children, symptoms can often be non-specific. However, according to observations of pediatricians, influenza in children most often manifests itself in the form of an acute infection of the upper respiratory tract. Otitis media is often associated with influenza symptoms in children [2]. Seizures are found in 10–20% of children [3]. Gastrointestinal symptoms (eg, nausea and vomiting) are more common with influenza B, and 40–80% of children have changes in the radiographic image (X-ray) of the lungs [1]. Less common symptoms include runny nose, chest pain, eye pain, and sensitivity to light.
Influenza causes diseases of an epidemic character, occurring every season or pandemics, recurring every several to several dozen years, which are worldwide in scope. Pandemics occur about 3 times in a century and can kill tens of millions of people. The most tragic pandemic was Spanish flu. According to current estimates, 50–100 million people died because of it [4]. The most effective preventive measures against influenza infections are vaccinations. They alleviate the course of the disease and prevent complications from influenza, which can be very serious, especially in children. It should be remembered that children are outposts that spread influenza infections, so remember to vaccinate children in nurseries and kindergartens as well as teachers against flu seasonally. The Advisory Committee on Vaccinations (ACIP) recommends influenza vaccination for all healthy people from the age of 6 months (depending on the type of vaccine), unless there are medical contraindications. Since November 2019, the live attenuated intranasal flu vaccine is available for both children (older than 24 months) and adolescents [5,6]. Influenza vaccines are safe, effective, and well tolerated. They are characterized by the lowest number of adverse post-vaccination reactions recorded. After vaccination, local reactions may occur, such as redness, soreness, and swelling at the injection site, and, less frequently, general reactions (a slight increase in body temperature, pain in muscles, joints and head) that disappear after a few days may occur.
If left untreated, influenza can sometimes cause serious complications, which can even be fatal. Children are an important risk group for developing post-flu complications because their immune systems are still poorly developed. These complications include pneumonia and bronchitis, secondary bacterial pneumonia and bronchiolitis (especially in infants and children), otitis media, and others. Respiratory failure, encephalopathy, streptococcal angina, exacerbation of chronic diseases (eg, asthma, diabetes, chronic kidney failure), myositis, myocarditis and pericarditis, meningitis, or encephalitis may occur as well as partial hearing loss and even deafness, neurological complications, including Guillain-Barré syndrome, convulsions, severe seizures, and transplant rejection [7].
In the 2020/2021 epidemic season, in addition to influenza and other widespread flu-like infections, a new virus appeared, which was the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). It is responsible for the ongoing COVID-19 pandemic. This disease affects the respiratory system of patients of all ages, in extreme cases leading to severe respiratory and multi-organ failure, which can lead to the death of the patient. Both the influenza and SARS-CoV-2 viruses primarily attack the patient’s respiratory system, and in both, pneumonia may be a complication. For infants and sick children, the risk of getting infected with influenza and SARS-CoV-2 is similar. Doctors warn that with the advent of the influenza season, many people may become infected with the SARS-CoV-2 and influenza virus simultaneously. In Poland, infections caused by this new pathogen coincided with the 2019/2020 influenza season, because the peak of influenza incidence was recorded in the 9th week of the season, ie, February 24-March 1, 2020 [8]. The World Health Organization (WHO) emphasizes the need of increased monitoring of influenza virus infections, noting that the influenza virus can quickly mutate, and that the recent pandemic of the influenza virus, so-called The Hong Kong era of 1968–1969, caused by the A/H3N2/ subtype, caused 1–4 million deaths all over the world. It is crucial not to overlook a new subtype of influenza A virus, with potentially highly pathogenic features. The WHO states that we should not forget about influenza not only in terms of the Global Influenza Surveillance and Response System (GISRS), but also in vaccinations, which are reported in Flu News Europe and FluNet [9–11]. We should also be aware that influenza virus co-infection with SARS-CoV-2 may occur.
Therefore, the present population study aimed to investigate influenza and influenza-like respiratory virus infections in children during the 2019/20 influenza season and the COVID-19 pandemic in Poland using data from the National Influenza Centre, the Department of Influenza Research at the National Institute of Public Health, and 16 Voivodeship Sanitary and Epidemiological Stations.
Material and Methods
ISOLATION OF RNA:
RNA isolation was performed from nasal and throat swabs suspended in 1 ml of saline. For this isolation, the Maxwell 16 Viral Total Nucleic Acid Purification Kit (Promega Corporation, Madison, WI, USA) was used in accordance with the instructions provided by the manufacturer. From 200 μl of a clinical sample suspended in 1 ml of physiological saline, 50 μl of RNA suspended in RNAse-free water was obtained.
REAL-TIME POLYMERASE CHAIN REACTION:
Quantitative polymerase chain reaction (qRT-PCR) was used to determine the influenza virus type and subtype (for positive samples). In the Department of Influenza Research, National Influenza Centre, the reaction is performed with the SuperScript Platinum III kit (Invitrogen) and the Rotor-Gene Q thermal cycler (Qiagen). We used primer and probe kits (influenza A, influenza A/H3N2/, influenza A/H1N1/pdm09, and influenza B) obtained from the International Reagent Resource (IRR) of the Centers for Disease Control and Prevention. The sequences of the primers and probes from IRR were not publicly available. RNA was subjected to reverse transcription (50°C for 30 min). After initiation (1 cycle at 95°C for 2 min), the DNA was subjected to 45 cycles of amplification: denaturation (95°C for 15 s), annealing (55°C for 30 s), and elongation (72°C for 20 s). The positive controls of the reactions were viruses derived from the vaccine for the 2019–2020 epidemic season (A/Brisbane/02/2018 (H1N1)pdm09, A/Kansas/14/2017/ (H3N2), B/Colorado/06/2017 (B/Victoria/2/87 lineage), and B/Phuket/3073/2013 (B/Yamagata/16/88 lineage)). The negative control was the RNase-free water provided in the kit. RNA of vaccine viruses selected by the World Health Organization were used as positive controls. Similar analysis was conducted in the VSESs. See Table 1 for the details of the methodology.
STATISTICAL ANALYSIS:
We attempted to assess whether there were statistically significant differences between age groups with respect to their vulnerability to viruses, performing a number of 2-sample Z-tests. For this purpose, appropriately grouped data were treated as drawn from binomial distributions, whose parameters (success rates) were to be compared with each other.
LIMITATIONS OF THE STUDY:
This work is based on the analyses of samples that were reported to the sentinel influenza surveillance system. Not every tested sample is reported to this system. Consequently, the number of patients and samples in the given seasons could be much higher.
Results
In the 2019/2020 epidemic season, 999 samples taken from children up to 14 years of age were analyzed. As part of the SENTINEL program, 305 samples were tested (they constituted 30.5% of all samples analyzed within this age group). From outside the SENTINEL program, 694 samples were analyzed (ie, 69.5% of the total number of samples analyzed in this age group). Out of all the samples tested, 53.9% of cases of infection with influenza viruses and influenza-like viruses (538 samples) were confirmed. The percentage of positive samples is presented in Figure 1.
As one can see in Figure 1, the majority of positive cases were influenza infections, and the ratio of influenza infections to all positive cases seems to increase with age: 84.1% for 0–4 years, 92.9% for 5–9 years, and 97.8% for 10–14 years. A more rigorous statistical analysis allows us to state that the youngest population is different in this respect from the 2 older populations (
Similar to the previous epidemic season, infections caused by influenza A definitely dominated (460 cases) over influenza B (22 cases). Influenza A/H1N1/pdm09 viruses dominated among the types of influenza A viruses (64 cases, which accounted for 13.9% of all cases caused by influenza A virus). Thirty-three infections with influenza A/H3N2/ were confirmed (7.2% of influenza A infections). The remaining infections with influenza A were non-selected cases (363 positive samples, accounting for 79% of influenza A confirmations). The percentage share of influenza viruses and their subtypes is presented in Figure 2.
The results obtained were also analyzed in 3 more detailed age groups, according to the National Influenza Centre for Innovation Influenza Surveillance [12]. The highest number of influenza A infections was confirmed in the group of the youngest children (0–4 years) (204 confirmed cases); 172 cases of influenza A were confirmed in the 5–9 age group and 84 cases in the group of the oldest children (ie, 10–14 years of age). As for the confirmation of influenza B, there were 7 in the 0–4 age group, 10 in the 5–9 age group, and 5 in the 10–14 age group. The number of confirmed cases of the influenza virus in the 0–4, 5–9, and 10–14 age groups in the 2019/2020 epidemic season in Poland is presented in Figure 3. We aimed to test whether there were statistically significant differences in influenza A to B infection ratio between the age groups. With 95% certainty, we were not able to reject the hypothesis that these populations were the same in this respect (
Influenza-like virus infections are also quite common in children up to the age of 14 years, which is confirmed by the analyzed research results. An additional analysis was also carried out in 3 more detailed age groups (0–4 years, 5–9 years, and 10–14 years). The obtained results show that the highest number of infections with influenza viruses was confirmed in the age group of the youngest children up to 4 years of age, accounting for 77.4% of influenza-like virus infections in children aged 0–4 years (41 patients). In the 5–9 age group, 9 cases were confirmed (1.7% of all infections with influenza viruses), while in the age group of the oldest children aged 10–14 years, there were only 3 cases (5.7%). Among influenza-like viruses, RSV was the dominant virus, with 28 confirmed cases; the largest number was found in the age group of the youngest children aged 0–4 years (23 infections). In the analyzed samples from children aged 0–14 years, infections with other influenza viruses were also confirmed: 13 cases of Rhinovirus, 4 cases of including parainfluenza 3 (PIV3), 3 cases of including parainfluenza 1 (PIV1) infections, 2 cases of human adenovirus (ADV) and 1 case of including parainfluenza 2 (PIV2), human corona viruses 229E/NL63 (Coronavirus 229E/NL63) and human metapneumovirus (hMPV) infections each. The percentage share of influenza-like viruses is presented in Figure 4.
In the 2019/2020 epidemic season, co-infections were also confirmed in the analyzed samples from children aged 0–14 years, ie, infection with 2 or more respiratory viruses: influenza or influenza-like viruses. Confirmed co-infections are presented in Table 2.
Discussion
The presented data indicate a very common occurrence of respiratory virus infections among children. Analysis of samples taken from children in the 0–14 age group in the 2019/2020 epidemic season shows that the influenza A virus dominated in the pediatric population in Poland. The A/H1N1/pdm09 virus was the dominant subtype. Similar tendencies can be noticed both in other European countries, as well as in the rest of the world [13]. In the season 2019/2020, activity of influenza A/H3N2/ and B were increased in relation to the influenza season 2018/2019 [14]. The highest number of infections with both influenza viruses and influenza-like viruses was recorded among the youngest children aged 0–4 years. [14]. This confirms that younger age is associated with a less mature immune system and greater vulnerability to viruses. Babies still lack protective antibodies, and the antibodies obtained from the mother only protect the baby during the first months of life [15,16]. It has been shown that in older children, subtype A/H3N2 causes the most severe course of disease. Subtype A/H1N1 causes milder disease, and subtype B causes the mildest course of disease [17].
Children staying in same-age groups (eg, nurseries, kindergartens, schools) develop such infections much more often. The data of the NIPH PZH-PIB shows that in Poland, an average of 30–40% of infections with influenza viruses and influenza-like viruses are registered among children [18–21].
In agreement with the recommendation of the Advisory Committee on Immunization Practices (ACIP), the American Academy of Pediatrics (AAP), and the Council of the European Union, EU member states should take coordinated action to mitigate the impact of seasonal influenza by promoting vaccinations, especially for people from risk groups. However, despite the recommendations, in 2019, only 0.96% of children aged 0–14 years were vaccinated against influenza (0.53% of children aged 0–4, 0.43% of children aged 5–14) [8]. It should be realized that the more people are vaccinated, the fewer people get sick; therefore, the number of people who can become infected decreases. It is worth being vaccinated before of the epidemic season. In 2003, some regions of the United States recorded a large spike in influenza as early as October, especially among young children. This means, that the flu epidemic broke out at the height of the flu vaccination period, which is luckily rare [17]. Younger children have higher risk of being hospitalized due to flu, especially those under 2 years of age. In fact, most children with the influenza virus under age 6 months are hospitalized due to infection [17]. Research by Antonova et al showed that children with laboratory-confirmed influenza infection were often hospitalized (0.3–20%), needed medical visits (1.7–2.8 visits per case), and had to take antibiotics (7–55%), antipyretic drugs and other medications to alleviate the symptoms of the disease (76–99%) [22].
In Poland, several cases of child deaths due to flu complications are registered every season. In the 2019/2020 season, 5 deaths of children in the 5–14 age group were registered, while in the 2018/2019 season 1 child from the 0–4 age group died [8]. These deaths are recorded as deaths caused by concomitant chronic diseases, especially cardiovascular and respiratory diseases, and complications of influenza, especially pneumonia.
Analyzing the course of both diseases in children, due to infection with the influenza virus and caused by the SARS-CoV-2 virus, influenza seems to be a more dangerous threat to children. Children usually go through COVID-19 asymptomatically or with mild symptoms, but are exposed to a more severe course of flu and a greater risk of complications.
The burden of influenza in children is substantial and has a significant direct impact on the ill children and an indirect impact on their families. The research results presented by Taghioff et al support vaccination against influenza, reducing the risk of sepsis, stroke, and venous thrombosis. They suggest a potential protective effect, reducing the need for patients to stay in the hospital emergency department and the hospital intensive care unit, which may benefit populations during the SARS-CoV-2 pandemic [15].
Research shows that COVID-19 can be more contagious than flu [23]. However, due to the very similar clinical symptoms when infected with these viruses, it is important that patients with flu-like infections be tested for both SARS-CoV-2 and influenza.
Conclusions
Influenza is a viral infection that can lead to serious, even life-threatening complications in children. Children are an important group at risk from flu complications and are the main group for the spread of viral infections. The presented data indicates a very common occurrence of respiratory virus infections among children. This population study from Poland showed that during the COVID-19 pandemic and during the winter influenza season of 2019/20, influenza and influenza-like viral infections in children showed some differences from previous influenza seasons. For this reason, the percentage of influenza vaccination in the pediatric population should be significantly increased, especially now, due to the current epidemiological situation related to the ongoing SARS-CoV-2 pandemic. The flu vaccine can boost our immune system. We should also be aware that influenza virus co-infection with SARS-CoV-2 may occur. An efficiently functioning epidemiological and virological surveillance system, representative for the country as a whole, is essential to observe and control influenza outbreaks, which otherwise might lead to epidemics or even pandemics. These findings highlight the importance of viral infection surveillance and influenza vaccination in the pediatric population.
Figures
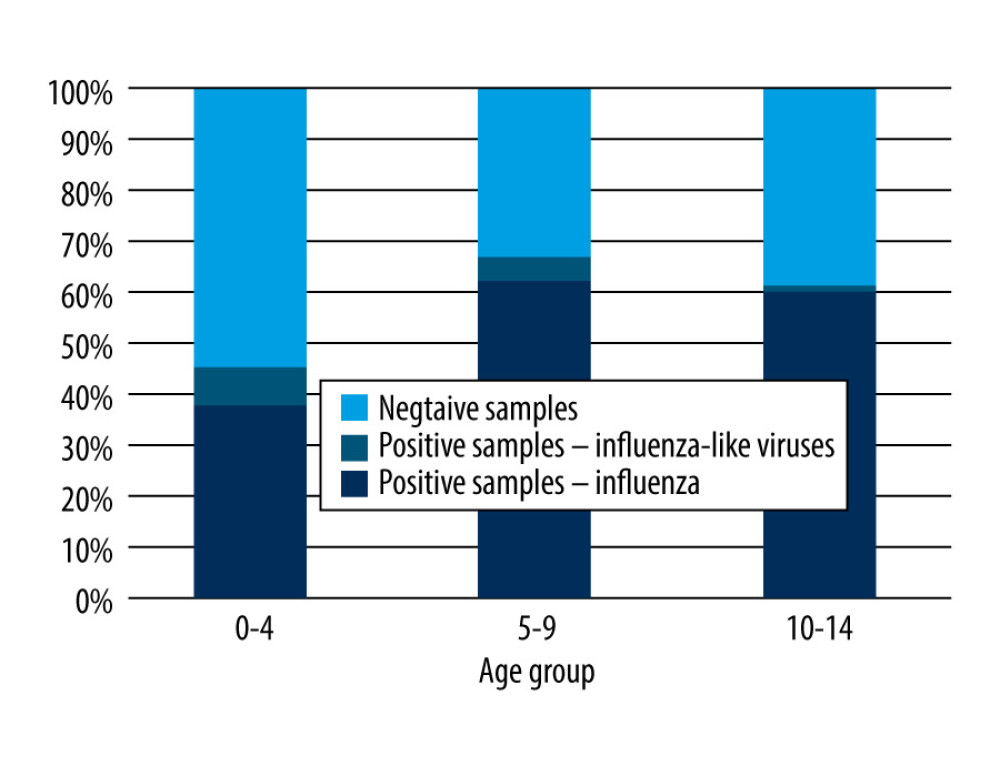 Figure 1. The percentage of positive samples in relation to all the tested samples in the 0–14 years age group in the 2019–2020 epidemic season in Poland.
Figure 1. The percentage of positive samples in relation to all the tested samples in the 0–14 years age group in the 2019–2020 epidemic season in Poland. 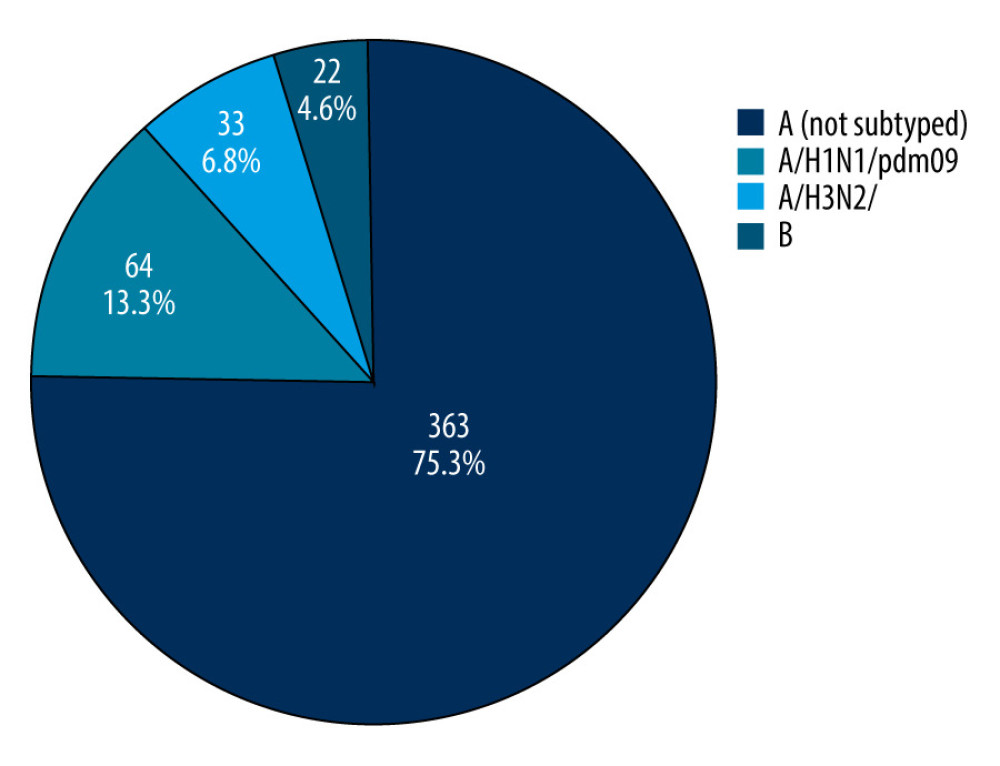 Figure 2. The percentage share of influenza viruses and their subtypes in children in the 0–14 years age group in the 2019/2020 epidemic season in Poland.
Figure 2. The percentage share of influenza viruses and their subtypes in children in the 0–14 years age group in the 2019/2020 epidemic season in Poland. 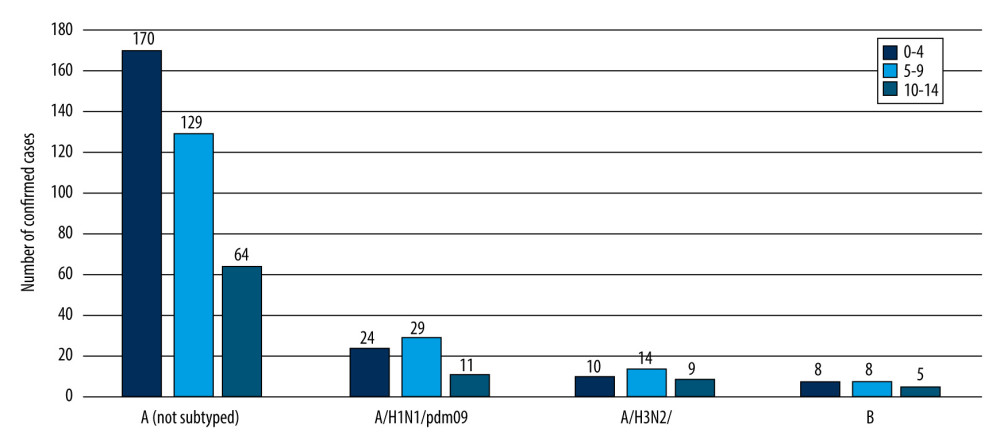 Figure 3. The number of confirmed cases of the influenza virus in the age groups 0–4, 5–9, 10–14 years in the 2019/2020 epidemic season in Poland.
Figure 3. The number of confirmed cases of the influenza virus in the age groups 0–4, 5–9, 10–14 years in the 2019/2020 epidemic season in Poland. 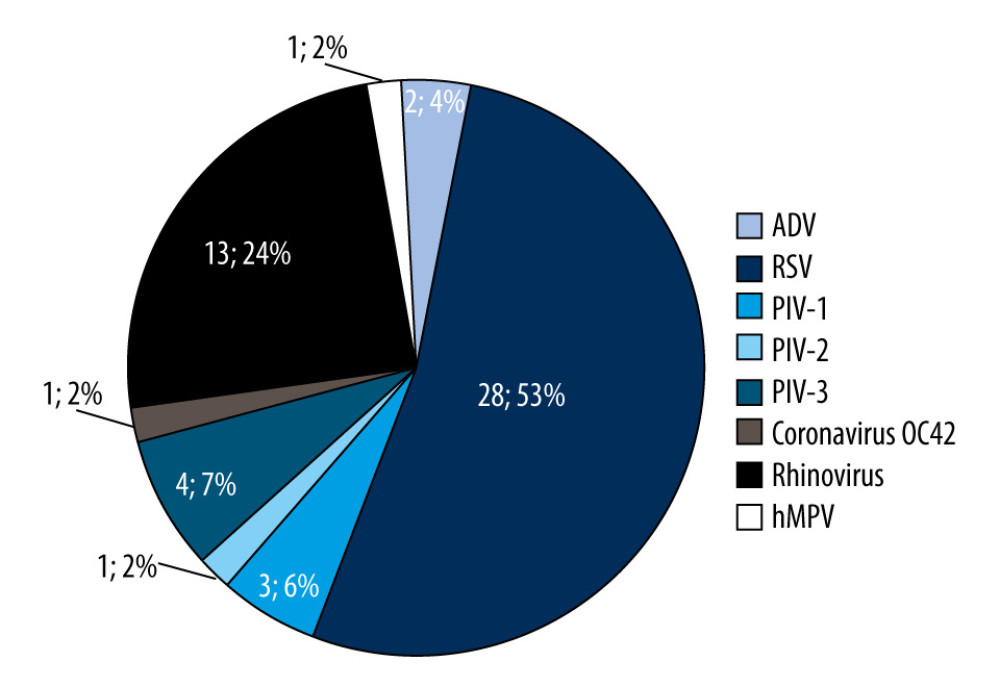 Figure 4. The percentage share of influenza-like viruses in the 0–14 age group in the 2019/2020 epidemic season in Poland.
Figure 4. The percentage share of influenza-like viruses in the 0–14 age group in the 2019/2020 epidemic season in Poland. References
1. Zawłocka E, Chwiećko J, Jackowska TFalling ill with flu in children under 2 years of age: Nowa Pediatria, 2016; 3(2016); 105-12 [in Polish]
2. Fiore AE, Fry A, Shay D, Centers for Disease Control and Prevention: Antiviral agents for the treatment and chemoprophylaxis of influenza: MMWR Recomm Rep, 2011; 60(1); 1-24
3. Aguirre E, Papenburg J, Ouakki M, Comparison of pandemic and seasonal influenza in the Pediatric Emergency Department: Ped Infect Dis J, 2011; 30(8); 633-39
4. Murray J, Lopez AD, Chin B, Estimation of potential global pandemic influenza mortality on the basis of vital registry data from the 1918–20 pandemic: A quantitative analysis: Lancet, 2006; 368(9554); 2211-18
5. Grohskopf LA, Alyanak E, Broder KR, Prevention and control of seasonal influenza with vaccines: Recommendations of the Advisory Committee on Immunization Practices – United States, 2019–20 influenza season: MMWR Recomm Rep, 2019; 68(3); 1-21
6. American Academy of Pediatrics, Committee on Infectious Diseases, Recommendations for prevention and control of influenza in children (2019–2020): Pediatrics, 2019; 44(4); e20192478
7. Brydak LB, 2008; 101-23, Warsaw, Rytm [in Polish]
8. NIZP PZH-PIB, 2021 Available from: [in Polish]http://wwwold.pzh.gov.pl/oldpage/epimeld/2019/Sz_2019pdf#page=27&zoom=auto,-274,642
9. Brydak LB, 2008; 9-34, Warsaw, Rytm [in Polish]
10. https://flunewseurope.org/
11. https://www.who.int/teams/global-influenza-programme
12. Bednarska K, Hallmann-Szelińska E, Kondratiuk KInnovations in influenza surveillance: Probl Hig Epidemiol, 2016; 97(2); 101-5 [in Polish]
13. Flu News Europe: Weekly influenza surveillance – Bulletin Archives. [serial online] [cited 2021 Sept 1]: Available from: https://flunewseurope.org/Archives
14. Kondratiuk K, Hallmann E, Łuniewska K, Epidemiology of influenza viruses and viruses causing influenza-like illness in children under 14 years old in the 2018–2019 epidemic season in Poland: Med Sci Monit, 2021; 27; e929303
15. Taghioff SM, Slavin BR, Holton T, Singh D, Examining the potential benefits of the influenza vaccine against SARS-CoV-2: Aerospective cohort analysis of 74,754 patients: PLoS ONE, 2021; 16(8); e0255541
16. Kumar V, Influenza in children: Indian J Pediatr, 2017; 84(2); 139-43
17. Monto AS, Epidemiology of influenza: Vaccine, 2008; 26(Suppl 4); D45-48
18. Hallmann-Szelińska E, Bednarska K, Kondratiuk K, Viral infections in children in the 2014/2015 epidemic season in Poland: Adv Exp Med Biol, 2016; 912; 51-56
19. Cieślak K, Szymański K, Kowalczyk D, Brydak LB, Influenza and influenza-like viruses in children in the epidemic season 2015/2016 in Poland: Adv Exp Med Biol, 2017; 968; 13-18
20. Cieślak K, Kowalczyk D, Szymański K, Influenza and influenza-like viruses: Frequent infections in children under 14 years of age during the 2016/2017 epidemic season: Adv Exp Med Biol, 2018; 1114; 83-87
21. Łuniewska K, Szymański K, Hallmann-Szelińska E, Infections caused by influenza viruses among children in Poland during the 2017/18 epidemic season: Adv Exp Med Biol, 2019; 1211; 97-102
22. Antonova EN, Rycroft CE, Ambrose CS, Burden of paediatric influenza in Western Europe: A systematic review: BMC Public Health, 2012; 12; 968
23. Petersen E, Koopmans M, Go U, Comparing SARS-CoV-2 with SARS-CoV and influenza pandemics: Lancet Infect Dis, 2020; 20(9); e238-44
Figures
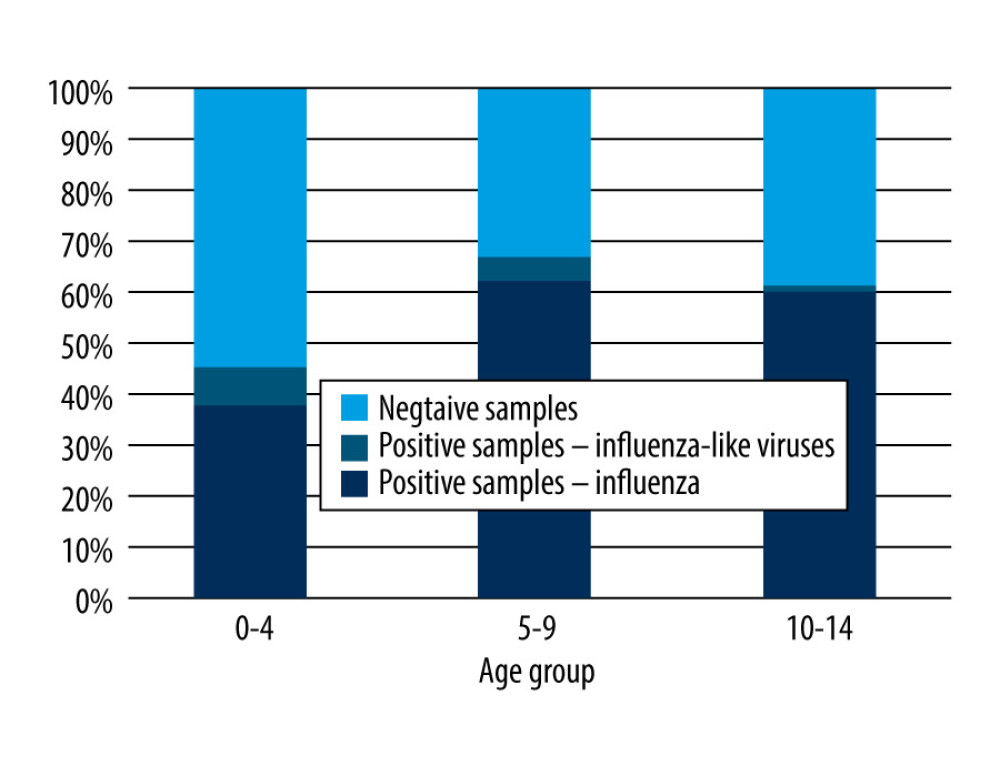 Figure 1. The percentage of positive samples in relation to all the tested samples in the 0–14 years age group in the 2019–2020 epidemic season in Poland.
Figure 1. The percentage of positive samples in relation to all the tested samples in the 0–14 years age group in the 2019–2020 epidemic season in Poland.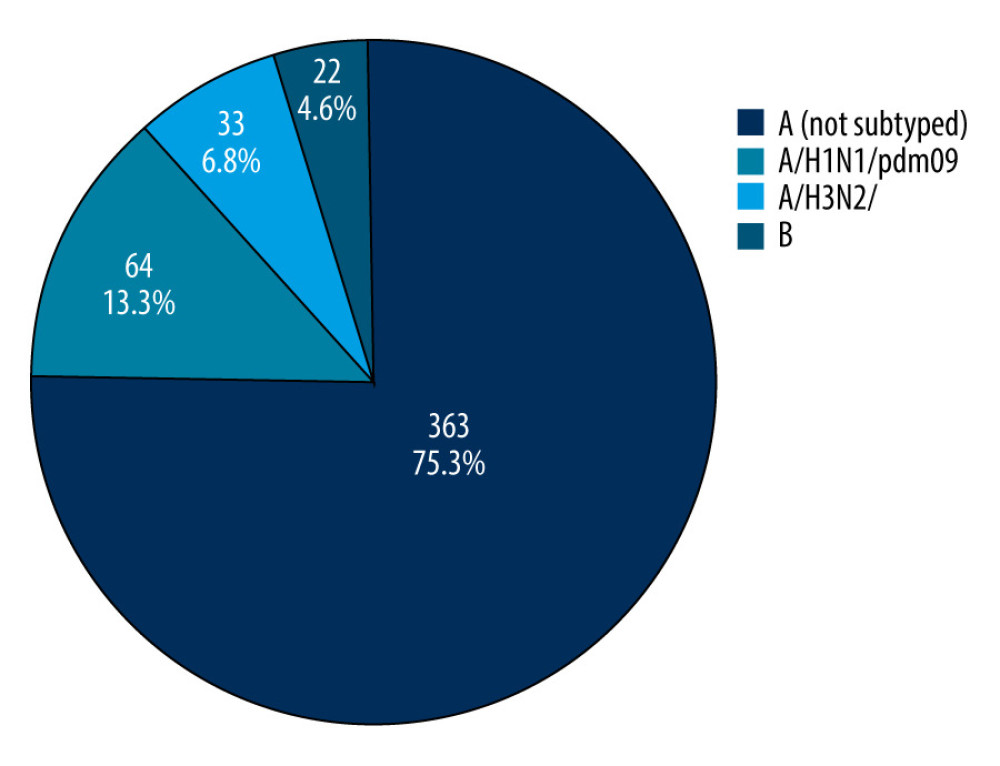 Figure 2. The percentage share of influenza viruses and their subtypes in children in the 0–14 years age group in the 2019/2020 epidemic season in Poland.
Figure 2. The percentage share of influenza viruses and their subtypes in children in the 0–14 years age group in the 2019/2020 epidemic season in Poland.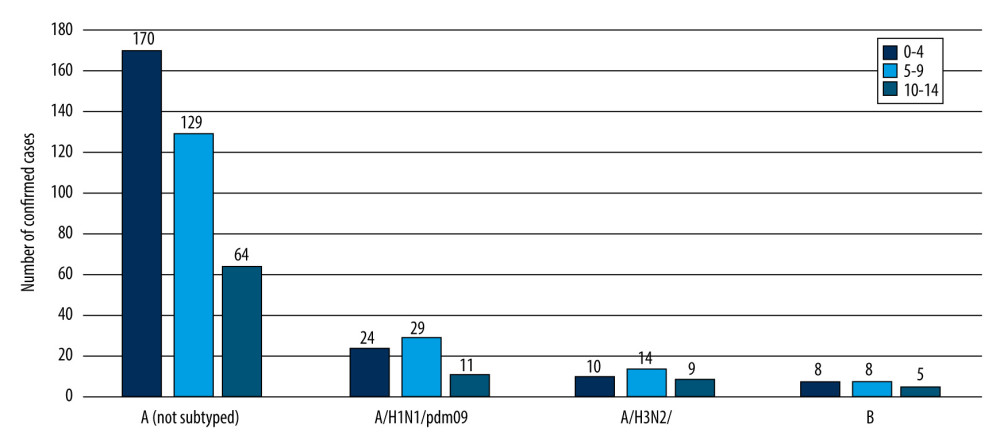 Figure 3. The number of confirmed cases of the influenza virus in the age groups 0–4, 5–9, 10–14 years in the 2019/2020 epidemic season in Poland.
Figure 3. The number of confirmed cases of the influenza virus in the age groups 0–4, 5–9, 10–14 years in the 2019/2020 epidemic season in Poland.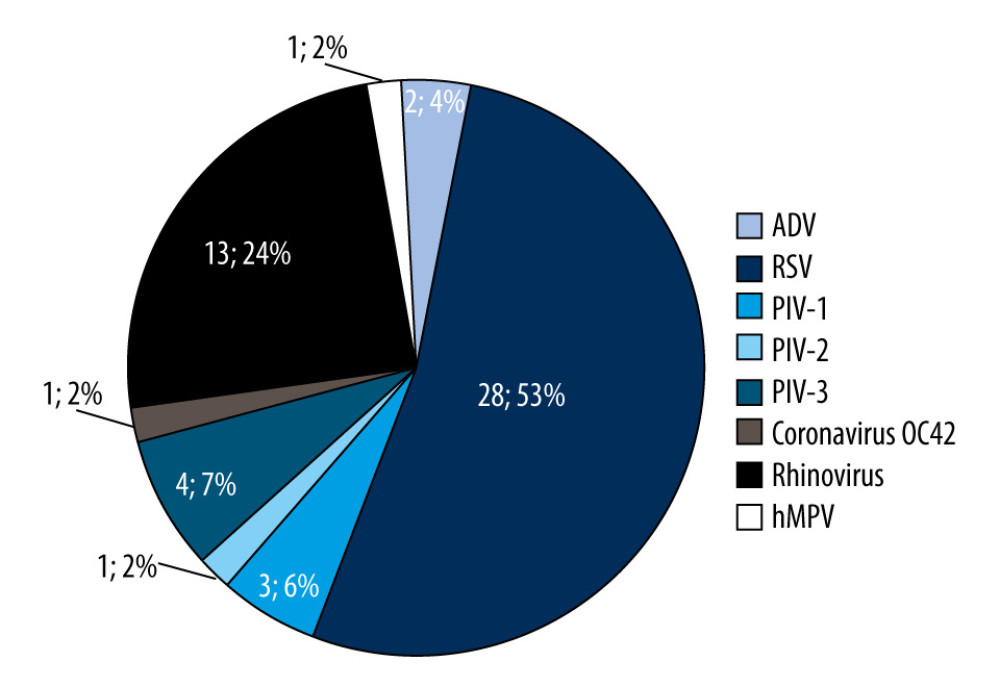 Figure 4. The percentage share of influenza-like viruses in the 0–14 age group in the 2019/2020 epidemic season in Poland.
Figure 4. The percentage share of influenza-like viruses in the 0–14 age group in the 2019/2020 epidemic season in Poland. Tables
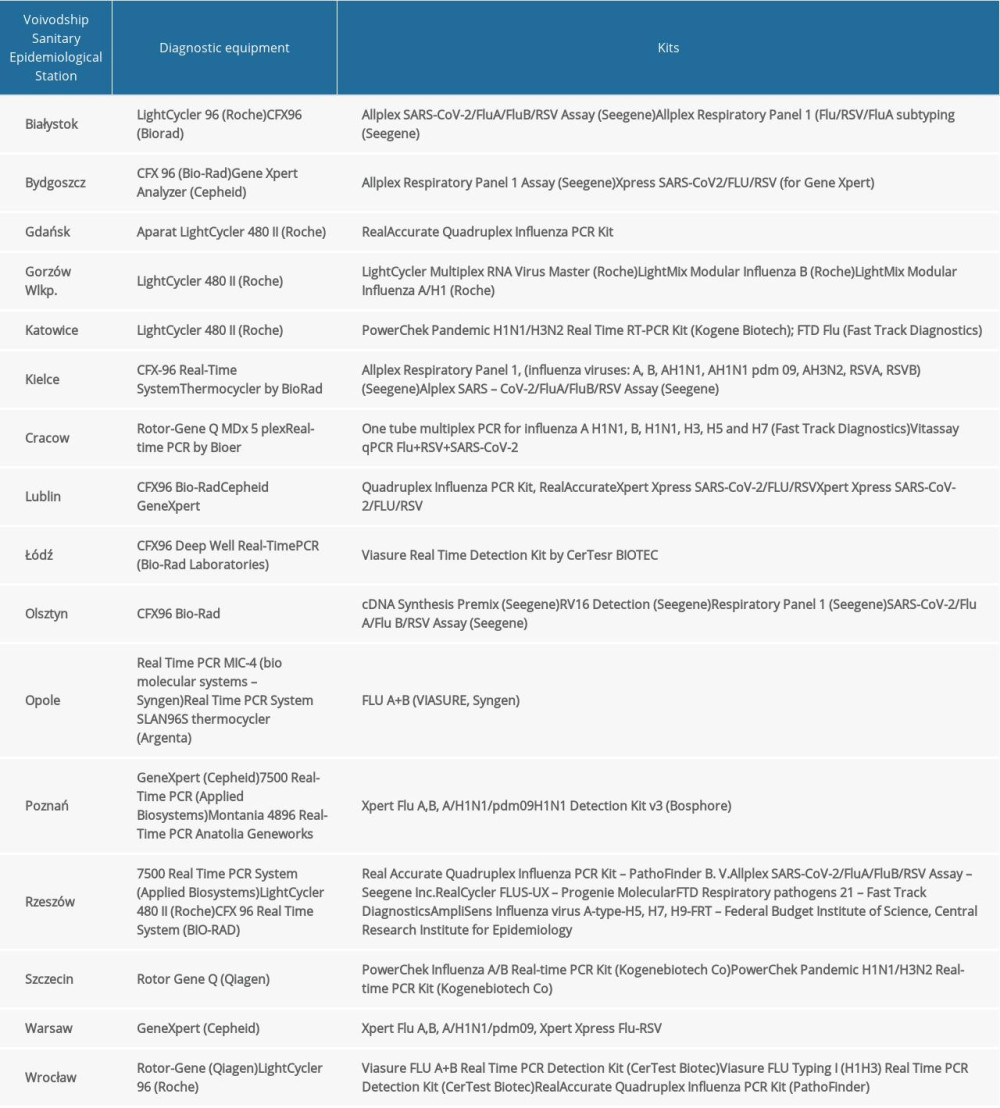 Table 1. The diagnostic methods used in 16 Voivodship Sanitary Epidemiological Stations in in the epidemic season 2018–2019 in Poland.
Table 1. The diagnostic methods used in 16 Voivodship Sanitary Epidemiological Stations in in the epidemic season 2018–2019 in Poland.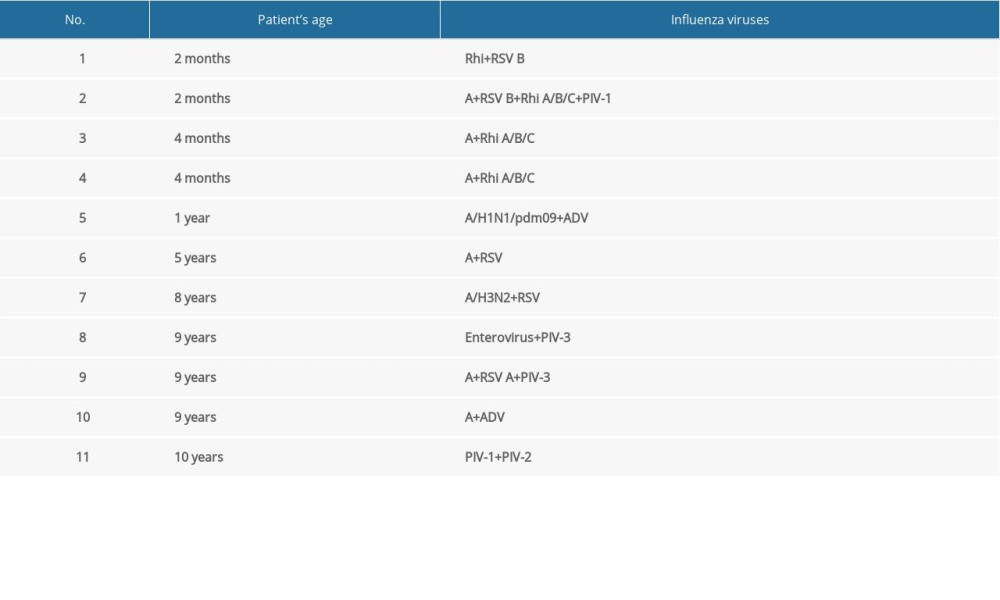 Table 2. Co-infections with respiratory viruses in children 0–14 years of age in the 2019/2020 epidemic season.
Table 2. Co-infections with respiratory viruses in children 0–14 years of age in the 2019/2020 epidemic season.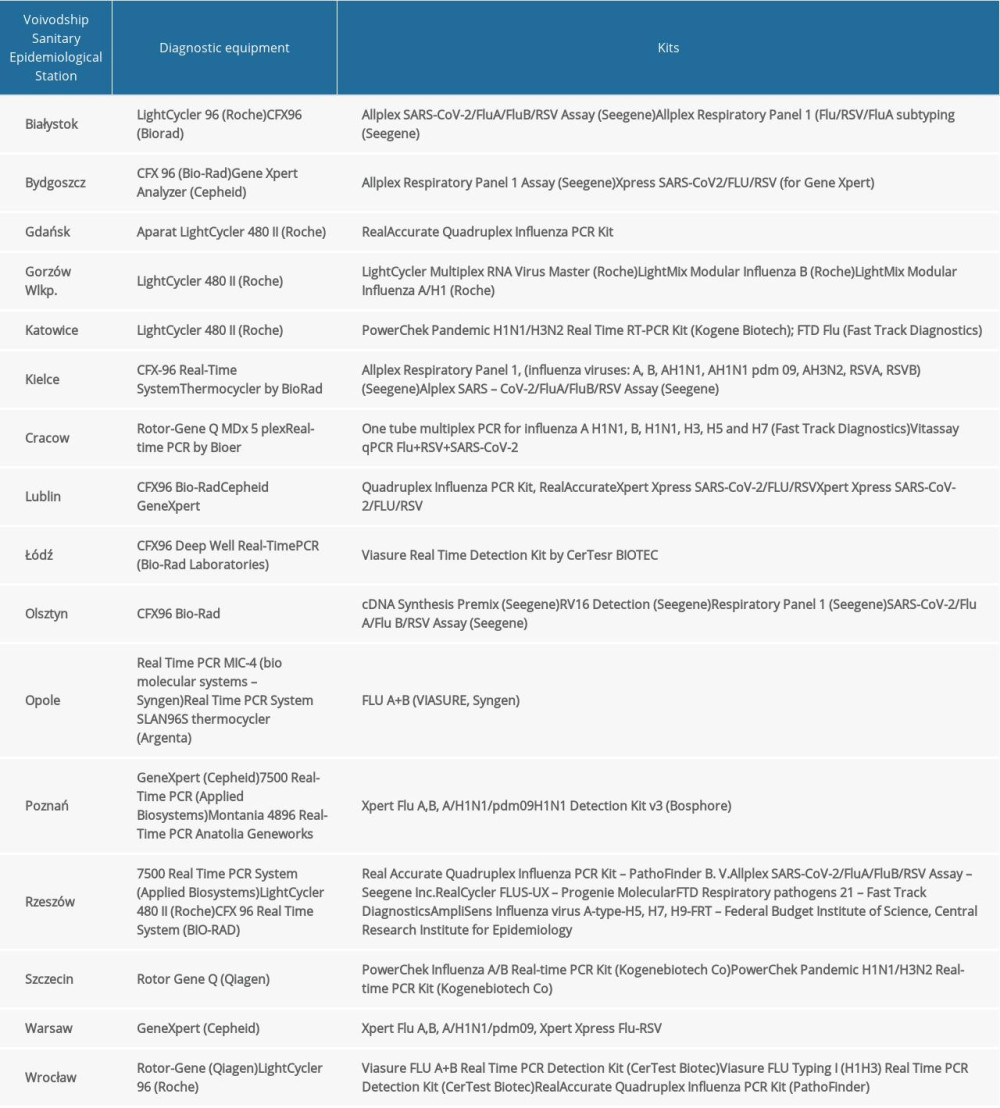 Table 1. The diagnostic methods used in 16 Voivodship Sanitary Epidemiological Stations in in the epidemic season 2018–2019 in Poland.
Table 1. The diagnostic methods used in 16 Voivodship Sanitary Epidemiological Stations in in the epidemic season 2018–2019 in Poland.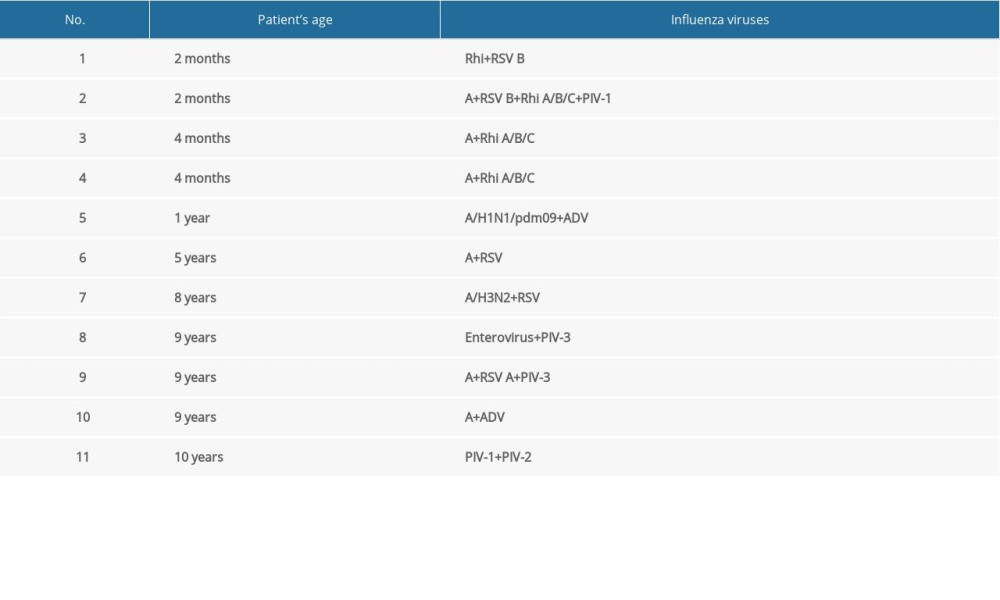 Table 2. Co-infections with respiratory viruses in children 0–14 years of age in the 2019/2020 epidemic season.
Table 2. Co-infections with respiratory viruses in children 0–14 years of age in the 2019/2020 epidemic season. In Press
18 Apr 2024 : Clinical Research
Comparative Analysis of Open and Closed Sphincterotomy for the Treatment of Chronic Anal Fissure: Safety an...Med Sci Monit In Press; DOI: 10.12659/MSM.944127
08 Mar 2024 : Laboratory Research
Evaluation of Retentive Strength of 50 Endodontically-Treated Single-Rooted Mandibular Second Premolars Res...Med Sci Monit In Press; DOI: 10.12659/MSM.944110
11 Mar 2024 : Clinical Research
Comparison of Effects of Sugammadex and Neostigmine on Postoperative Neuromuscular Blockade Recovery in Pat...Med Sci Monit In Press; DOI: 10.12659/MSM.942773
12 Mar 2024 : Clinical Research
Comparing Neuromuscular Blockade Measurement Between Upper Arm (TOF Cuff®) and Eyelid (TOF Scan®) Using Miv...Med Sci Monit In Press; DOI: 10.12659/MSM.943630
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








