03 January 2022: Database Analysis
Relationships Between Obstructive Sleep Apnea and Cardiovascular Disease: A Bibliometric Analysis (2010–2021)
Yumeng Wang1AE, Xintian Shou12AC, Yang Wu3AG*, Zongjing Fan2BC, Jie Cui2DF, Rui Zhuang1CD, Ruixiang Luo1BFDOI: 10.12659/MSM.933448
Med Sci Monit 2022; 28:e933448
Abstract
BACKGROUND: Obstructive sleep apnea (OSA) is a common disease that can lead to intermittent hypoxia, increased sympathetic overdrive, and excessive oxidative stress, and eventually lead to cardiovascular/cerebrovascular diseases and metabolic disorders. The prevalence of OSA is reported to be higher in people with certain cardiovascular diseases (CVD). Therefore, the relationship between OSA and CVD has been gradually favored by researchers.
MATERIAL AND METHODS: Data were downloaded from the Web of Science Core Collection database. Citespace was used to remove duplicated data and construct knowledge visual maps.
RESULTS: A total of 7047 publications were obtained. The USA was the largest contributor as well as an important player in the cooperation network between nations. The leading institution was the Mayo Clinic. Our study ultimately identified the top 5 hotspots and 4 research frontiers in this field. Top 5 hotspots were: the specific types of obstructive sleep apnea-related cardiovascular and metabolic co-morbidities, the curative effects of CPAP on these co-morbidities, the specific mechanisms of co-morbidities, the importance of polysomnography on OSA and its co-morbidities with CVD, and the prevalence of OSA and its co-morbidities with CVD in particular populations. The top 4 frontiers were: the relationship between OSA and resistant hypertension, the molecular mechanisms of OSA and its co-morbidities with CVD, specific medications and treatment guidelines for the co-morbidities, and the mainstream research methods in this field.
CONCLUSIONS: This study provides insight and valuable information for researchers and helps to identify new perspectives concerning potential collaborators and cooperative institutions, hot topics, and research frontiers in this field.
Keywords: Bibliometrics, Cardiovascular Diseases, Sleep Apnea Syndromes, Sleep apnea, obstructive, Comorbidity, Continuous Positive Airway Pressure, Disease Management, Humans, International Cooperation, Metabolic Networks and Pathways, Polysomnography, Prevalence, Research, Risk Factors
Background
Obstructive sleep apnea (OSA) is a disease characterized by repeated episodes of upper airway closure during sleep, which results in recurrent oxyhemoglobin desaturation and sleep fragmentation. OSA can lead to intermittent hypoxia, increased sympathetic overdrive, and excessive oxidative stress, and can eventually lead to cardiovascular/cerebrovascular diseases and metabolic disorders. Recent epidemiological studies have shown that the prevalence of OSA is about 14% in men and 5% in women [1]. OSA is an independent risk factor for many cardiovascular diseases (CVD), and is also associated with obesity [2], insulin resistance [3], hypertension [4], arrhythmias [5], stroke [6], coronary artery disease [7,8], heart failure [9], and atherosclerosis [10]. Patients with CVD are susceptible to OSA-related stress factors and their associated adverse cardiovascular outcomes. The prevalence of OSA is reported to be higher in people with certain cardiovascular diseases. For example, the prevalence of OSA is 40% in patients with hypertension and rises to 90% in patients with refractory hypertension [11]. About 30~60% of OSA patients have a complicated arrhythmia, including sinus arrest, second-degree atrioventricular block, atrial flutter, atrial fibrillation, premature atrial (ventricular) contraction, ventricular (supraventricular) tachycardia, and even sudden cardiac death [12,13]. Likewise, the prevalence of OSA is conservatively estimated to be 12% to 53% in patients with HFrEF and 40% in patients with HFpEF [14]. Despite the high incidence of OSA in patients with various types of CVD, OSA is often underrecognized and undertreated in the treatment of CVD. The relationship between OSA and CVD has been gradually favored by researchers.
Bibliometric analysis contains co-word analysis and cluster analysis. It is used to present the knowledge structure, identify international collaborations and geographic distributions, as well as explore development tendency via quantitative analysis [15,16]. Citespace is a Java-based bibliometric visualization tool created by Chaomei Chen (University of Dressel). It uses programming methods to help visualize the research countries, institutions, and authors [17]. The most notable feature is that Citespace can identify research hotspots and frontiers by analyzing co-cited references and burst terms. In this review, we used Citespace to present the current research situation and future trends of OSA and CVD in a visual way, aiming to provide direction for related researchers.
Material and Methods
SEARCH STRATEGIES:
We collected the data from the Web of Science Core Collection (WoSCC) database. These data were download on Apr 26th (2021). We used the following topics for retrieval: (heart OR *cardi* OR “blood pressure” OR hypertension OR coronary OR “atrioventricular block”) AND (“obstructive sleep apnea” OR “obstructive sleep apnea hypopnea syndrome” OR OSAHS). Indexes: SCI-expanded, CCR-expanded, IC. Timespan: 2010–2021. Only articles and reviews were included, while other types of publications were excluded.
DATA COLLECTION AND ANALYSIS:
The full record and cited references were exported from WoSCC in plain text format. First, we imported the data into Citespace (Version 5.7 R5, University of Dressel, Chaomei Chen) to remove duplication. After that, we constructed knowledge visual maps by using Citespace [17,18].
PARAMETERS SETTING:
Timespan: 2005–2021 (Slice Length=1). Selection Criteria: Top 50. Term source: all selected. Node type: check one at a time. Selection criteria: 50. Pruning: pathfinder. Visualization: cluster view static, display merged network.
ANALYTICAL METHOD:
The nodes in the map represent the countries, authors, institutions, or keywords. The link lines between the nodes indicate the collaboration relationship. The wider the line, the stronger the relationship between the 2 nodes. The size of the node represents the number of studies published. The purple ring represents centrality of more than 0.1, which means the element is considered relatively important.
Results
SEARCH RESULTS:
The initial search resulted in 8226 publications after duplicates had been removed. These publications included articles (5678), reviews (1369), editorial materials (224), proceedings papers (89), news item (1), letters (152), book chapters (48), retracted publications (2), meeting abstracts (790), early access (86), correction (11), and retraction (1). A total of 7047 publications met the inclusion criteria – 5678 articles and 1369 reviews.
ANNUAL PUBLICATION OUTPUT:
A total of 382 papers were published in 2010. The annual publication output increased sharply from 2010 to 2014 and showed a fluctuating upward trend from 2015 to 2019. A total of 747 papers were published in 2020, which is the year with the highest number of papers. To date, a total of 178 papers have been published in 2021, and the number is expected to grow (Figure 1). The results showed that the field of the relationship between OSA and CVD had gradually developed in the past decade.
ANALYSIS OF JOURNALS:
The top 10 most productive journals are listed in Table 1. According to the results, the journal Sleep and Breathing published the most articles and came in first place. This journal focuses on different pathological respiratory states during sleep and covers a wide range of sub-topics. The journal has published worldwide studies of OSA on prevalence, etiology, pathogenesis, and treatment. The American Journal of Respiratory and Critical Care Medicine, with the highest impact factor of 21.405, paid special attention to cardiovascular consequences of OSA and published many relevant articles. The majority of these journals are in the field of sleep, with the rest distributed among journals related to cardiothoracic, respiratory, nervous and metabolic diseases. There is still currently no specific journal on OSA and cardiovascular co-morbidities.
ANALYSIS OF COUNTRIES, INSTITUTIONS, AND AUTHORS:
The co-occurrence map provides valuable information and helps researchers to identify the cooperative relationship. A total of 595 researchers from more than 97 countries and 265 institutions contributed to the 7047 articles on the research of the relationship between OSA and CVD. The top 10 countries and institutions in terms of frequency and centrality are shown in Tables 2 and 3, respectively. The USA (2223) and China (707) were the leading countries. The Mayo Clinic (154) and Harvard Medical School (142) were the leading institutions. Australia, Singapore, Denmark, the University of Melbourne, and Boston University have high centrality, which means active cooperation has already developed (Figures 2, 3). Susan Redline, David Gozal, and Jeanlouis Pepin were the most productive authors (Table 4). We can draw a conclusion from Figure 4 that many authors prefer to cooperate with a relatively stable group of authors to generate several major author clusters, and each of these clusters contains more than 2 core authors.
ANALYSIS OF CO-CITED REFERENCES:
Analysis of co-cited references can help identify the influential publications and authors, as well as development tendency in this field. A total of 420 papers were obtained. The top 10 most co-cited references are listed in Table 5. Three of them reported the epidemiological information of OSA. Specifically speaking, Heinzer and Peppard found a sharp increase in the prevalence of OSA in adults from Wisconsin (USA) and Lausanne (Switzerland) over the past 20 years, and pointed out the independent associations between severity of sleep-disordered breathing and hypertension [19,20]. Senaratna made a systematic review to determine the prevalence of OSA in the general population, and mentioned that the diagnostic apnea hypopnea index (AHI) level where the treatment needs to begin can be determined based on the related morbidity/mortality profile, as in the case of hypertension and hyperlipidemia [21]. Three other studies emphasized the relationship between OSA and CVD. Gottlieb carried out a prospective study and found that OSA is associated with an increased risk of incident heart failure in community-dwelling middle-aged and older men [22]. Javaheri made a review to generalize the clinical cardiovascular consequences and molecular signatures of OSA concerning cardiocerebrovascular disorders [23]. The paper “Adult obstructive sleep apnea”, published in the Lancet, was considered to be the first comprehensive review in this field. The authors highly summarized the diagnosis, definitions, pathophysiology, risk factors, consequences, and management of OSA. Then they cited a large number of examples to illustrate the relationship between OSA and other CVD, such as hypertension, and pointed out that the effect of continuous positive airway pressure (CPAP) on CVD in OSA patients is equivocal [24]. Similarly, the SAVE study, a large international multi-center randomized controlled study conducted by McEvoy, showed that CPAP did not prevent cardiovascular events in patients with moderate-to-severe OSA and established cardiovascular disease [25]. Another study showed a significant positive association between ischemic stroke and AHI in men, in which each 1-unit increase in OAHI in men was estimated to increase stroke risk by 6% in the mild-to-moderate range [26]. In addition, 2 important guidelines were also obtained through our analysis: one is an update of the “2007 AASM Manual for the Scoring of Sleep and Associated Events” by the American Academy of Sleep Medicine (AASM), and the other is a clinical practice guideline for diagnostic testing for adult OSA [27,28]. These findings suggest that we still need to deepen clinical understanding of the relationship between OSA and CVD, and also emphasized the importance of treatment of OSA, especially in patients with complicated CVD. Clinical practice urgently needs therapeutic measures that have definite and significant positive effects on cardiovascular events.
A document co-citation analysis produced 10 co-citation clusters, which were marked by indexed terms from their citations. The results showed Modularity Q=0.8333 >0.3 and Silhouette=0.9504 >0.7, which demonstrated that the cluster structure was significant, and the results were accurate, reasonable, and reliable (Figure 5). Cluster #0, labeling “hypertension”, was the largest cluster, consisting of 36 references, followed by “mandibular advancement device” (cluster #1), “atrial fibrillation” (cluster #2), and “acute coronary syndrome” (cluster #3).
ANALYSIS OF KEYWORDS AND BURST TERMS:
Keywords represent the main content of research. Keyword co-occurrence analysis provides a reasonable description of research hotspots (Figure 6). The top keywords were “obstructive sleep apnea”, “positive airway pressure”, “hypertension”, “association”, “blood pressure”, “cardiovascular disease”, “risk factor”, “prevalence”, “risk”, and “obesity” (Table 6).
Finally, we used Citespace to obtain burst terms that can represent research frontiers by counting the frequency and growth rate of keywords in this field. The larger the burst value, the greater the innovation of the research outcomes. Of the top 20 burst terms with the strongest citation bursts in this field (Figure 7), we were particularly interested in those keywords that related to cardiovascular health, including “coronary heart diseases”, “myocardial infarction”, “cardiovascular risk factor”, “heart health”, “resistant hypertension”, and “cardiovascular event”.
TOP 5 HOTPOTS AND 4 FRONTIERS:
The analyses of keywords and clusters reflect the core themes and hot contents in this field. Burst terms represent the indicators of frontier or emerging trends. We summarize the top 5 research hotspots as follows: the specific types of obstructive sleep apnea-related cardiovascular and metabolic co-morbidities, the curative effects of CPAP on these co-morbidities, the specific mechanisms of co-morbidities, the importance of polysomnography on OSA and its co-morbidities with CVD, and the prevalence of OSA and its co-morbidities with CVD in particular populations. The top 4 frontiers were: the relationship between OSA and resistant hypertension, the molecular mechanisms of OSA and its co-morbidities with CVD, specific medications and treatment guidelines for the co-morbidities, and the mainstream research methods in this field.
Discussion
RESEARCH PROGRESS IN OSA AND CVD:
Gastaut [29] and Jung [30] found the existence of sleep apnea in 1965. Christian Guilleminault, the founding editor of the journal SLEEP, proposed the concept of OSAHS in 1978. Since 2000, many relevant guidelines have been developed by different countries and different associations. In 2017, the American Academy of Sleep Medicine (AASM) issued a guideline which defined OSA as a single disease for the first time, that can coexist with CVD, rather than a syndrome [31]. In June 2021, the American Heart Association (AHA) issued a new scientific statement published in the journal Circulation. It detailed the strong link between OSA and CVD in terms of risk factors, pathophysiology, and clinical manifestations [32]. Today, OSA-related cardiovascular co-morbidities are very common but are still frequently undiagnosed.
Our research results shows that a growing number of studies from 2010 to 2021 have been conducted to confirm a strong association between OSA and CVD, which indicated that this field has aroused heated discussion and wide concern in recent years. The results also show that the USA was the largest contributor and an important player in the cooperation network between nations. However, the journals related to research in this field had lower impact factors which indicated that researchers should focus on improving the content of their studies and conducting high-quality studies. To sum up, it is urgent for countries to strengthen cooperation, carry out relevant research in related fields, and publish high-quality articles.
STRENGTHS AND LIMITATIONS:
To the best of our knowledge, this study is the first bibliometric analysis of publications focused on the relationship between OSA and CVD to provide direction concerning potential collaborators, hotspots, and frontiers. However, this study still has some limitations. The publications were all written in English and were retrieved only from WOSCC, which may not be comprehensive. Some authors’ names in the literature are given by using the same abbreviation, which may cause misidentification by Citespace.
Conclusions
Our study ultimately identified 5 hotspots and 4 research fron2in this field through the analysis of co-cited references, clusters, keywords, and burst terms.
Figures
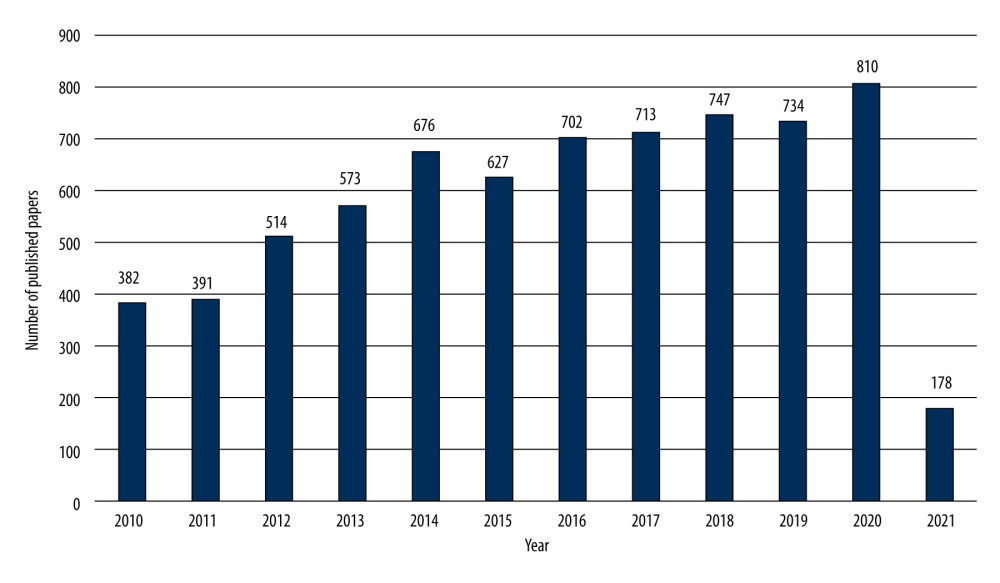 Figure 1. The number and linear growth trends of publications (Citespace, Version 5.7 R5, University of Dressel, Chaomei Chen).
Figure 1. The number and linear growth trends of publications (Citespace, Version 5.7 R5, University of Dressel, Chaomei Chen). 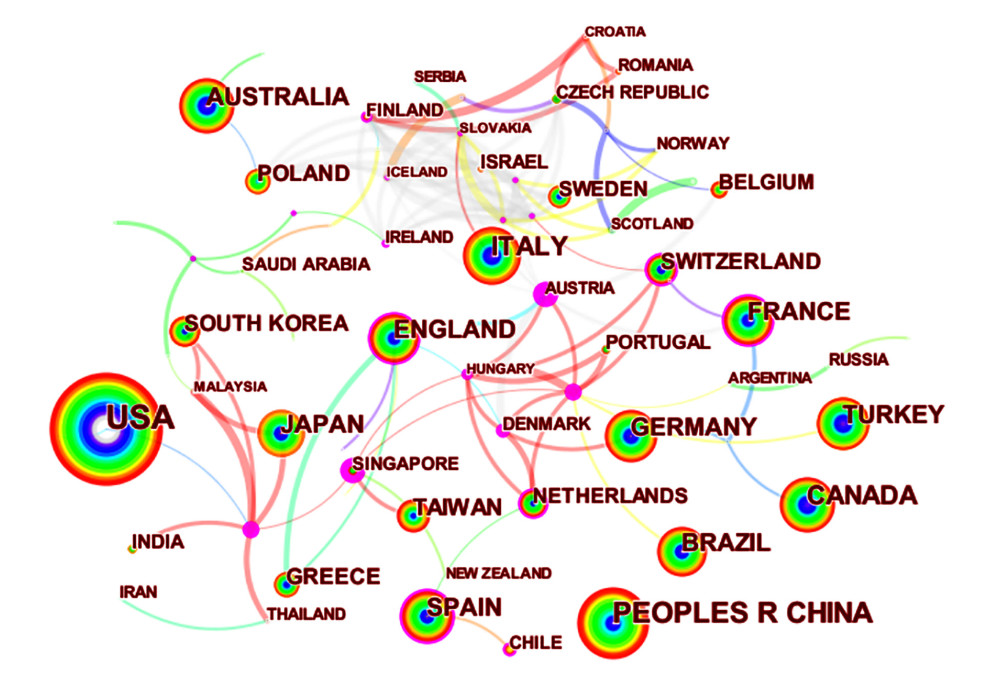 Figure 2. Co-occurrence map of countries (N97=, E=157) (Citespace, Version 5.7 R5, University of Dressel, Chaomei Chen).
Figure 2. Co-occurrence map of countries (N97=, E=157) (Citespace, Version 5.7 R5, University of Dressel, Chaomei Chen). 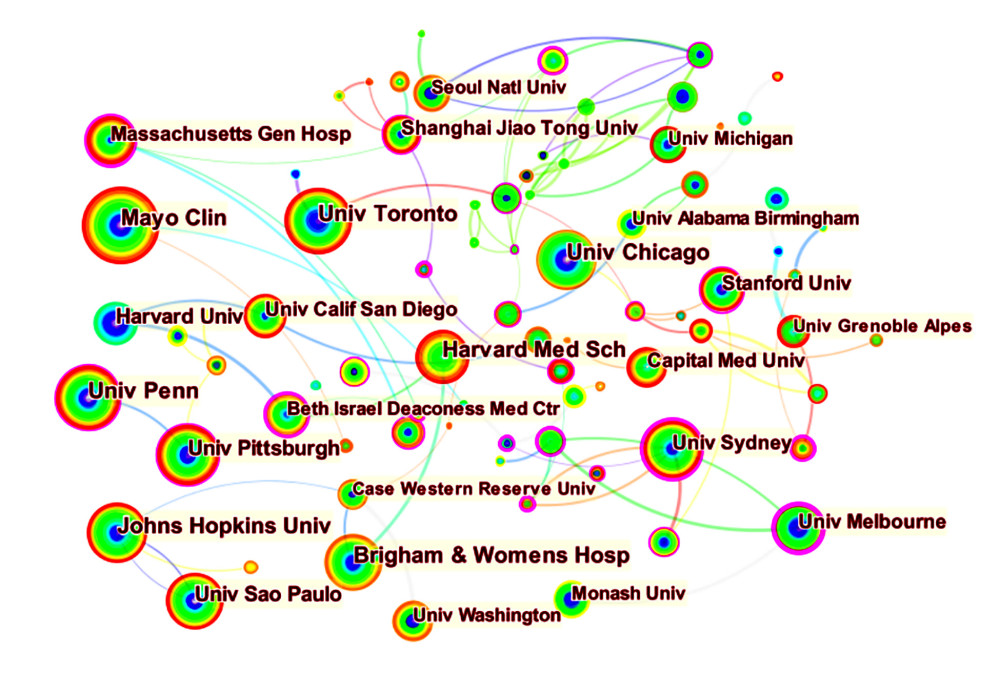 Figure 3. Co-occurrence map of institutions (N=265, E=369) (Citespace, Version 5.7 R5, University of Dressel, Chaomei Chen).
Figure 3. Co-occurrence map of institutions (N=265, E=369) (Citespace, Version 5.7 R5, University of Dressel, Chaomei Chen). 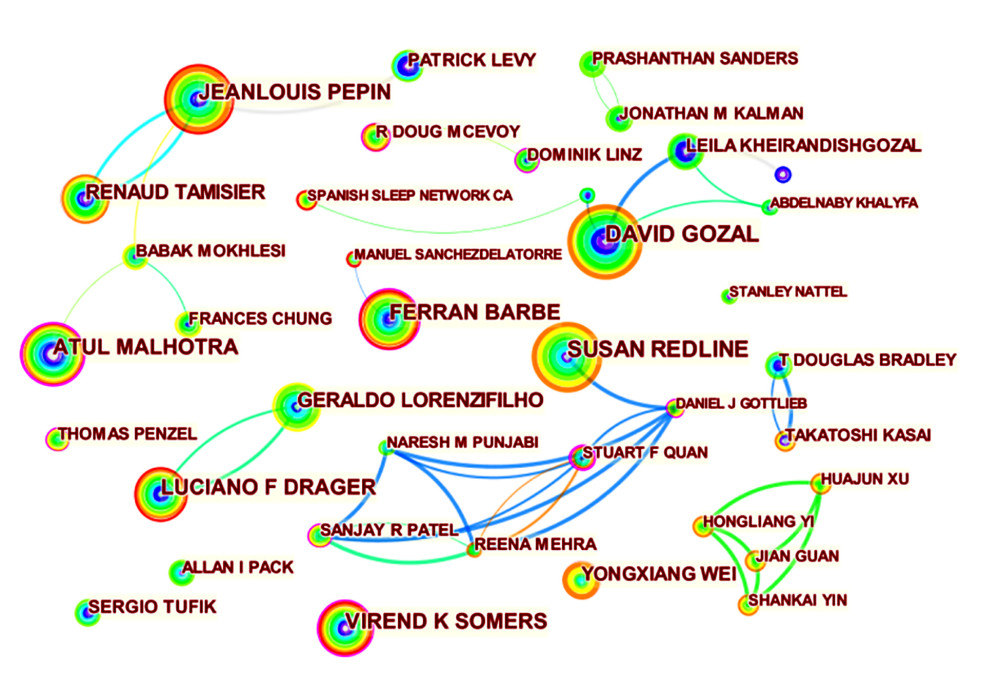 Figure 4. Co-occurrence map of authors (N=596, E=1514) (Citespace, Version 5.7 R5, University of Dressel, Chaomei Chen).
Figure 4. Co-occurrence map of authors (N=596, E=1514) (Citespace, Version 5.7 R5, University of Dressel, Chaomei Chen). 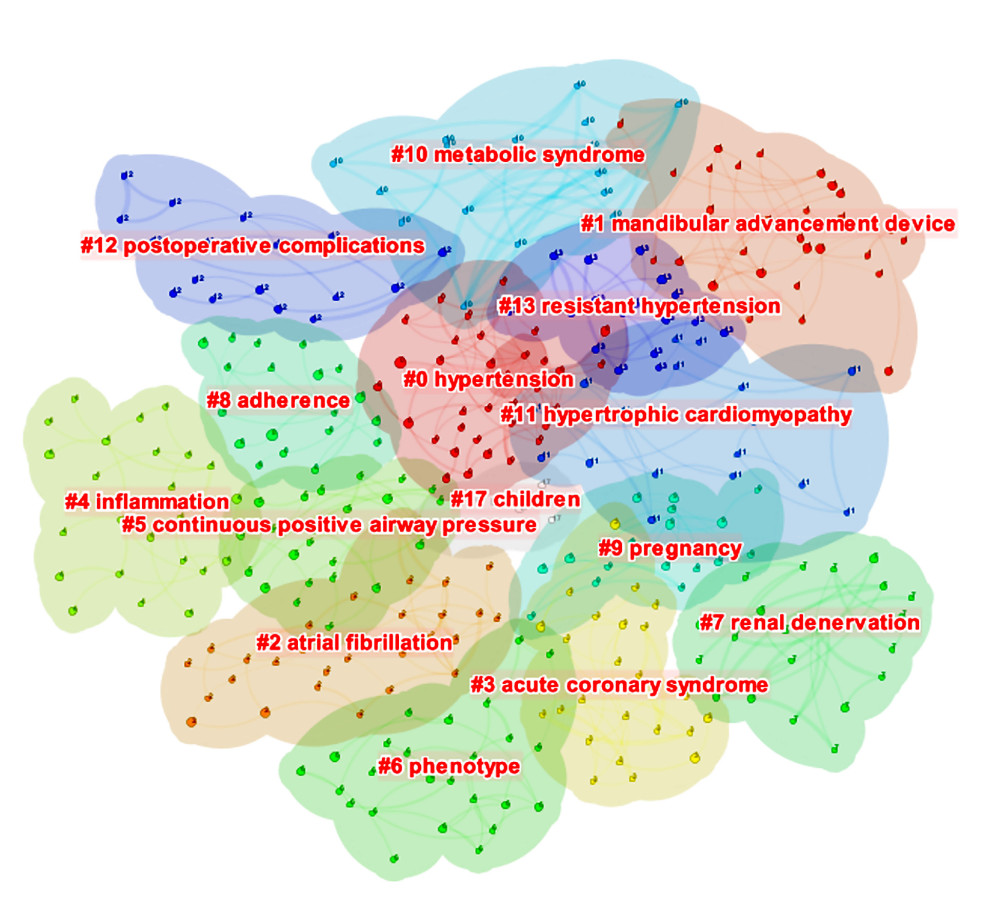 Figure 5. The clustered network map of co-cited references (N=420, E=579, Modularity Q=0.8333, Silhouette=0.9504) (Citespace, Version 5.7 R5, University of Dressel, Chaomei Chen).
Figure 5. The clustered network map of co-cited references (N=420, E=579, Modularity Q=0.8333, Silhouette=0.9504) (Citespace, Version 5.7 R5, University of Dressel, Chaomei Chen). 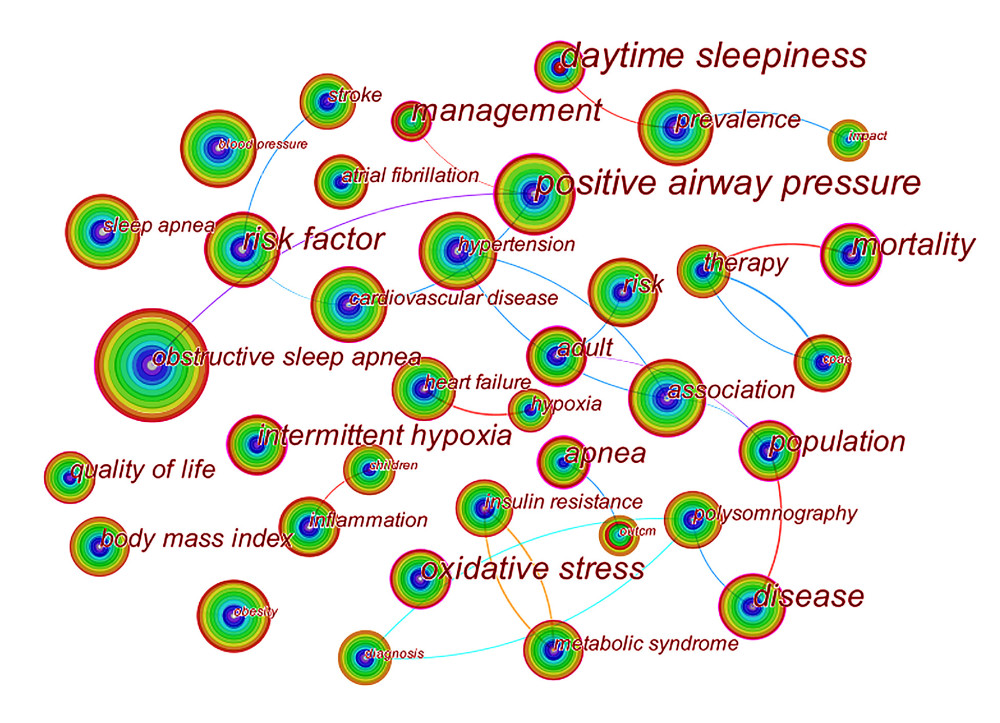 Figure 6. Co-occurrence map of keywords (N=111, E=137) (Citespace, Version 5.7 R5, University of Dressel, Chaomei Chen).
Figure 6. Co-occurrence map of keywords (N=111, E=137) (Citespace, Version 5.7 R5, University of Dressel, Chaomei Chen). 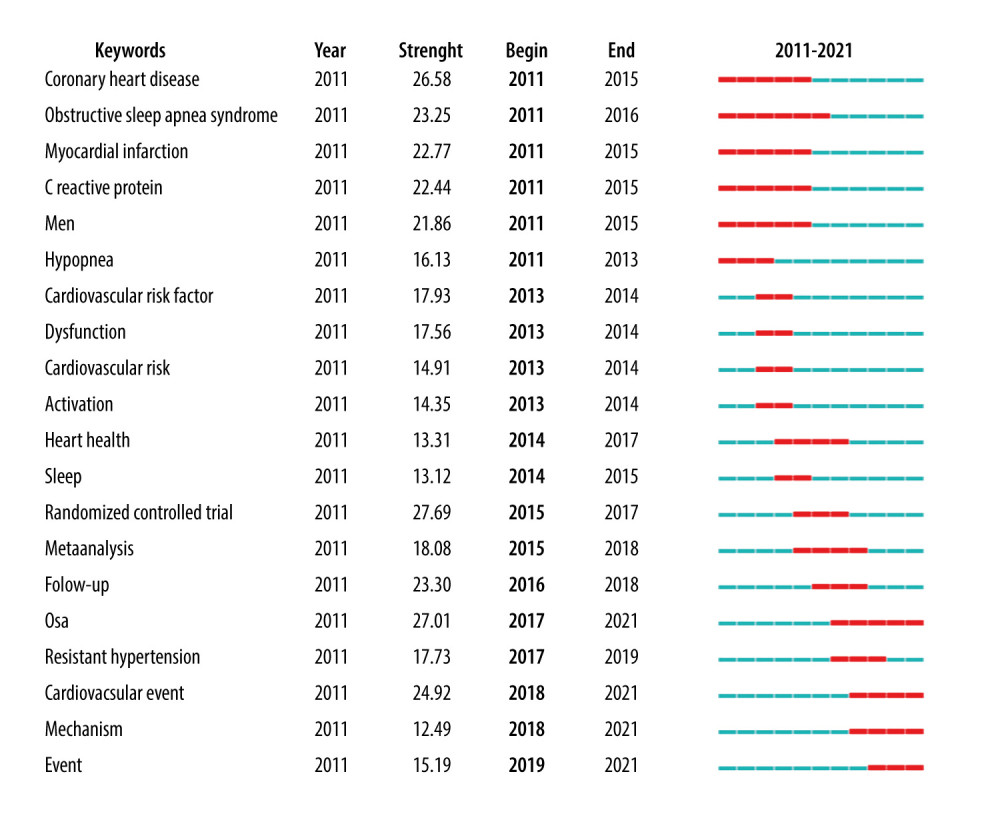 Figure 7. Top 20 keywords with the strongest citation bursts in original articles (Citespace, Version 5.7 R5, University of Dressel, Chaomei Chen).
Figure 7. Top 20 keywords with the strongest citation bursts in original articles (Citespace, Version 5.7 R5, University of Dressel, Chaomei Chen). Tables
Table 1. The top 10 productive journals.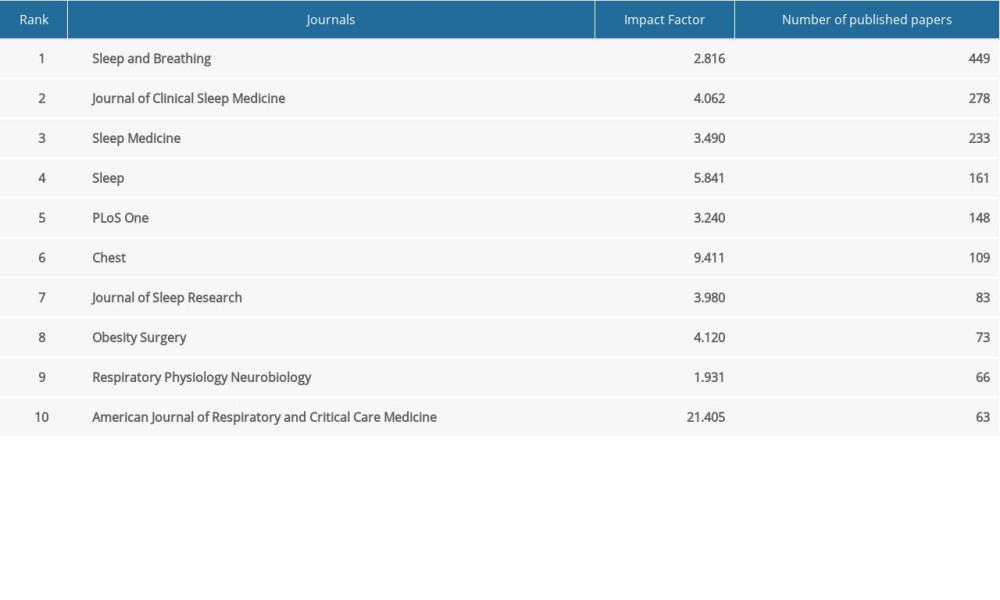 Table 2. Top 10 countries and institutions in terms of frequency.
Table 2. Top 10 countries and institutions in terms of frequency. Table 3. Top 10 countries and institutions in terms of centrality.
Table 3. Top 10 countries and institutions in terms of centrality. Table 4. Top 10 most productive authors.
Table 4. Top 10 most productive authors.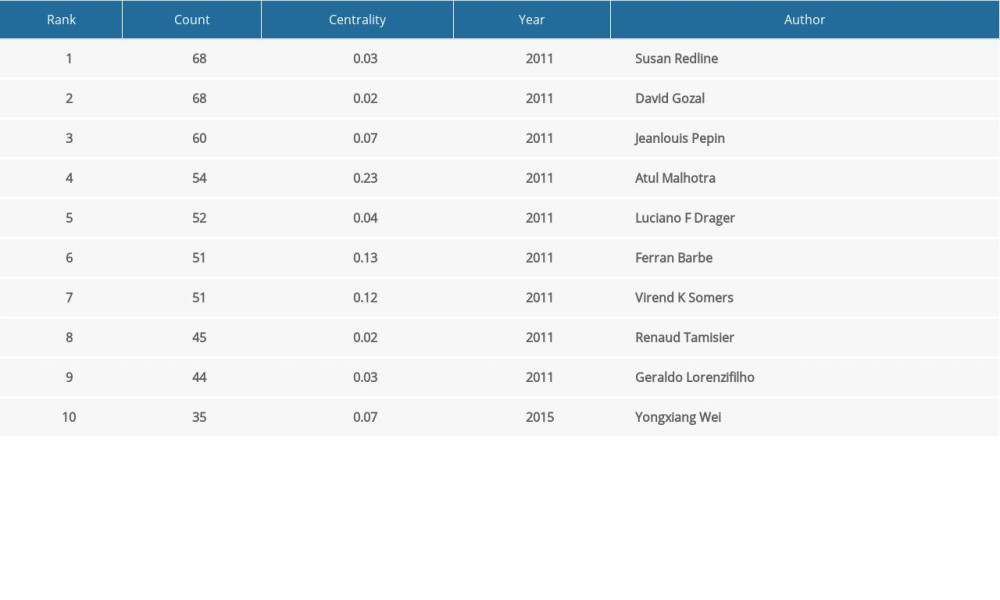 Table 5. Top 10 co-cited references in terms of frequency.
Table 5. Top 10 co-cited references in terms of frequency.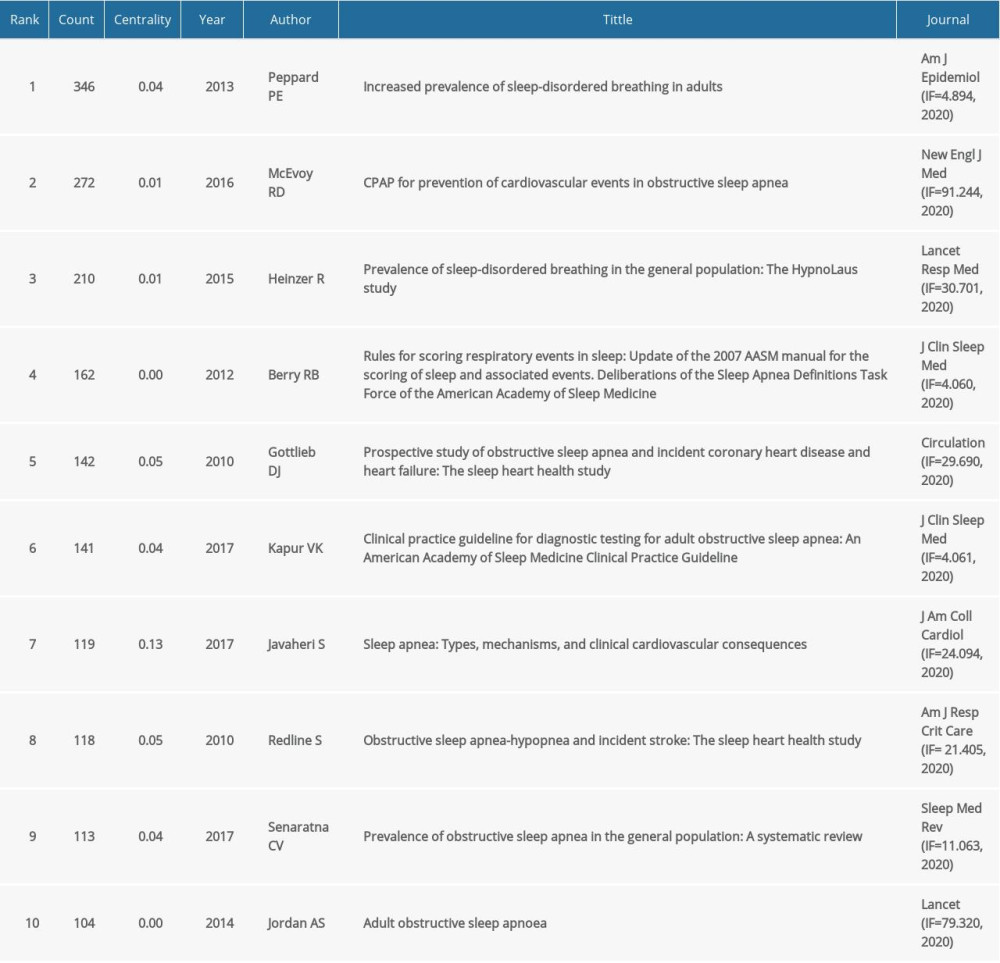 Table 6. Top 10 keywords in terms of frequency.
Table 6. Top 10 keywords in terms of frequency.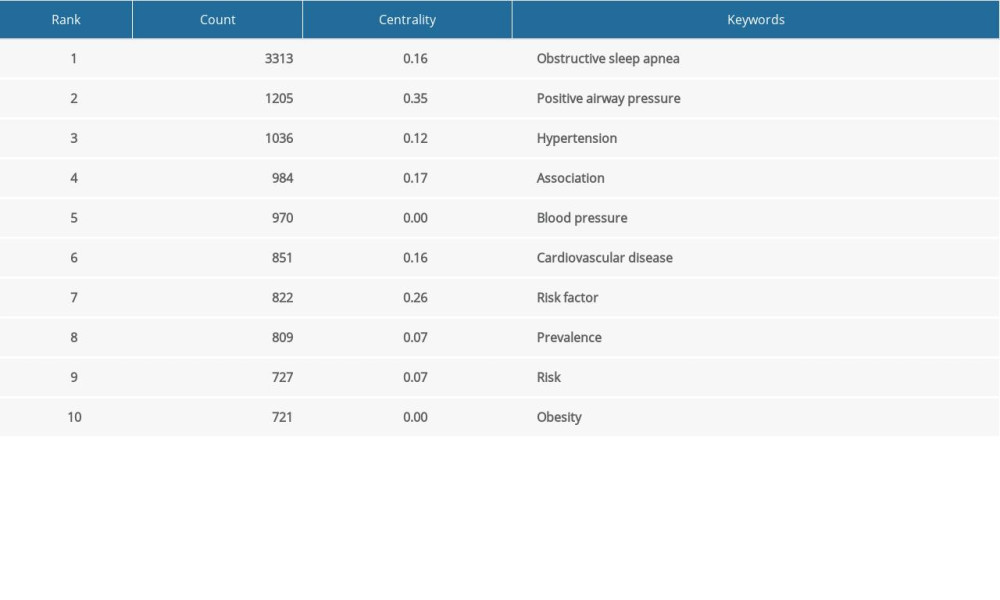
References
1. Peppard PE, Young T, Barnet JH, Increased prevalence of sleep-disordered breathing in adults: Am J Epidemiol, 2013; 177(9); 1006-14
2. Kuvat N, Tanriverdi H, Armutcu F, The relationship between obstructive sleep apnea syndrome and obesity: A new perspective on the pathogenesis in terms of organ crosstalk: Clin Respir J, 2020; 14(7); 595-604
3. Isobe Y, Nakatsumi Y, Sugiyama Y, Severity indices for obstructive sleep apnea syndrome reflecting glycemic control or insulin resistance: Intern Med, 2019; 58(22); 3227-34
4. Salman LA, Shulman R, Cohen JB, Obstructive sleep apnea, hypertension, and cardiovascular risk: Epidemiology, pathophysiology, and management: Curr Cardiol Rep, 2020; 22(2); 6
5. Patel N, Donahue C, Shenoy A, Obstructive sleep apnea and arrhythmia: A systemic review: Int J Cardiol, 2017; 228; 967-70
6. McKee Z, Auckley DH, A sleeping beast: Obstructive sleep apnea and stroke: Cleve Clin J Med, 2019; 86(6); 407-15
7. Wang X, Zhang Y, Dong Z, Effect of continuous positive airway pressure on long-term cardiovascular outcomes in patients with coronary artery disease and obstructive sleep apnea: A systematic review and meta-analysis: Respir Res, 2018; 19(1); 61
8. He CJ, Cao LF, Zhu CY, Association between obstructive sleep apnea-hypopnea syndrome and outcomes in patients with myocardial infarction in the absence of obstructive coronary artery disease: Front Cardiovasc Med, 2020; 7; 573819
9. Khattak HK, Hayat F, Pamboukian SV, Obstructive sleep apnea in heart failure: Review of prevalence, treatment with continuous positive airway pressure, and prognosis: Tex Heart Inst J, 2018; 45(3); 151-61
10. Chen J, Lin S, Zeng Y, An update on obstructive sleep apnea for atherosclerosis: Mechanism, diagnosis, and treatment: Front Cardiovasc Med, 2021; 8; 647071
11. Wang Q, Yang Z, Yang Y, Long C, Li H, A bibliometric analysis of research on the risk of engineering nanomaterials during 1999–2012: Sci Total Environ, 2014; 473–74; 483-89
12. Lombardi C, Pengo MF, Parati G, Systemic hypertension in obstructive sleep apnea: J Thorac Dis, 2018; 10(Suppl 34); S4231-43
13. Marinheiro R, Parreira L, Amador P, Ventricular arrhythmias in patients with obstructive sleep apnea: Curr Cardiol Rev, 2019; 15(1); 64-74
14. Gami AS, Hodge DO, Herges RM, Obstructive sleep apnea, obesity, and the risk of incident atrial fibrillation: J Am Coll Cardiol, 2007; 49(5); 565-71
15. Khattak HK, Hayat F, Pamboukian SV, Obstructive sleep apnea in heart failure: Review of prevalence, treatment with continuous positive airway pressure, and prognosis: Tex Heart Inst J, 2018; 45(3); 151-61
16. Chen C, Dubin R, Kim MC, Emerging trends and new developments in regenerative medicine: A scientometric update (2000–2014): Expert Opin Biol Ther, 2014; 14(9); 1295-317
17. Chen C, Searching for intellectual turning points: Progressive knowledge domain visualization: Proc Natl Acad Sci USA, 2004; 101(Suppl 1); 5303-10
18. Synnestvedt MB, Chen C, Holmes JH, CiteSpace II: Visualization and knowledge discovery in bibliographic databases: AMIA Annu Symp Proc, 2005; 2005; 724-28
19. Heinzer R, Vat S, Marques-Vidal P, Prevalence of sleep-disordered breathing in the general population: the HypnoLaus study: Lancet Respir Med, 2015; 3(4); 310-18
20. Peppard PE, Young T, Barnet JH, Increased prevalence of sleep-disordered breathing in adults: Am J Epidemiol, 2013; 177(9); 1006-14
21. Senaratna CV, Perret JL, Lodge CJ, Prevalence of obstructive sleep apnea in the general population: A systematic review: Sleep Med Rev, 2017; 34; 70-81
22. Gottlieb DJ, Yenokyan G, Newman AB, Prospective study of obstructive sleep apnea and incident coronary heart disease and heart failure: The sleep heart health study: Circulation, 2010; 122(4); 352-60
23. Javaheri S, Barbe F, Campos-Rodriguez F, Sleep apnea: Types, mechanisms, and clinical cardiovascular consequences: J Am Coll Cardiol, 2017; 69(7); 841-58
24. Jordan AS, McSharry DG, Malhotra A, Adult obstructive sleep apnoea: Lancet, 2014; 383(9918); 736-47
25. McEvoy RD, Antic NA, Heeley E, CPAP for prevention of cardiovascular events in obstructive sleep apnea: N Engl J Med, 2016; 375(10); 919-31
26. Redline S, Yenokyan G, Gottlieb DJ, Obstructive sleep apnea-hypopnea and incident stroke: The sleep heart health study: Am J Respir Crit Care Med, 2010; 182(2); 269-77
27. Berry RB, Budhiraja R, Gottlieb DJ, Rules for scoring respiratory events in sleep: Update of the 2007 AASM Manual for the Scoring of Sleep and Associated Events. Deliberations of the Sleep Apnea Definitions Task Force of the American Academy of Sleep Medicine: J Clin Sleep Med, 2012; 8(5); 597-619
28. Kapur VK, Auckley DH, Chowdhuri S, Clinical practice guideline for diagnostic testing for adult obstructive sleep apnea: An American Academy of Sleep Medicine Clinical Practice Guideline: J Clin Sleep Med, 2017; 13(3); 479-504
29. Gastaut H, Tassinari CA, Duron B, Polygraphic study of diurnal and nocturnal (hypnic and respiratory) episodal manifestations of Pickwick syndrome: Rev Neurol (Paris), 1965; 112(6); 568-79
30. Jung R, Kuhlo W, Neurophysiological studies of abnormal night sleep and the Pickwickian syndrome: Prog Brain Res, 1965; 18; 140-59
31. Kapur VK, Auckley DH, Chowdhuri S, Clinical practice guideline for diagnostic testing for adult obstructive sleep apnea: An American Academy of Sleep Medicine Clinical Practice Guideline: J Clin Sleep Med, 2017; 13(03); 479-504
32. He CJ, Cao LF, Zhu CY, Association between obstructive sleep apnea-hypopnea syndrome and outcomes in patients with myocardial infarction in the absence of obstructive coronary artery disease: Front Cardiovasc Med, 2020; 7; 573819
33. Patel SR, Obstructive sleep apnea: Ann Intern Med, 2019; 171(11); ITC81
34. Mansukhani MP, Kolla BP, Somers VK, Hypertension and cognitive decline: Implications of obstructive sleep apnea: Front Cardiovasc Med, 2019; 6; 96
35. Levy P, Kohler M, McNicholas WT, Obstructive sleep apnoea syndrome: Nat Rev Dis Primers, 2015; 1; 15015
36. Schwarz EI, Puhan MA, Schlatzer C, Effect of CPAP therapy on endothelial function in obstructive sleep apnoea: A systematic review and meta-analysis: Respirology, 2015; 20(6); 889-95
37. Iftikhar IH, Hoyos CM, Phillips CL, Magalang UJ, Meta-analyses of the association of sleep apnea with insulin resistance, and the effects of CPAP on HOMA-IR, adiponectin, and visceral adipose fat: J Clin Sleep Med, 2015; 11(4); 475-85
38. Prabhakar NR, Peng YJ, Nanduri J, Hypoxia-inducible factors and obstructive sleep apnea: J Clin Invest, 2020; 130(10); 5042-51
39. Wang Y, Meagher RB, Ambati S, Patients with obstructive sleep apnea have altered levels of four cytokines associated with cardiovascular and kidney disease, but near normal levels with airways therapy: Nat Sci Sleep, 2021; 13; 457-66
40. Cofta S, Winiarska HM, Plociniczak A, Oxidative stress markers and severity of obstructive sleep apnea: Adv Exp Med Biol, 2019; 1222; 27-35
41. Wu X, Gong L, Xie L, NLRP3 deficiency protects against intermittent hypoxia-induced neuroinflammation and mitochondrial ROS by promoting the PINK1-parkin pathway of mitophagy in a murine model of sleep apnea: Front Immunol, 2021; 12; 628168
42. Xu H, Liang C, Zou J, Interaction between obstructive sleep apnea and short sleep duration on insulin resistance: A large-scale study: OSA, short sleep duration and insulin resistance: Respir Res, 2020; 21(1); 151
43. Dominguez JE, Krystal AD, Habib AS, Obstructive sleep apnea in pregnant women: A review of pregnancy outcomes and an approach to management: Anesth Analg, 2018; 127(5); 1167-77
44. Dominguez JE, Street L, Louis J, Management of obstructive sleep apnea in pregnancy: Obstet Gynecol Clin North Am, 2018; 45(2); 233-47
45. Huang Y-S, Guilleminault C, Pediatric obstructive sleep apnea: Where do we stand?: Adv Otorhinolaryngol, 2017; 80; 136-44
46. Gulotta G, Iannella G, Vicini C, Risk factors for obstructive sleep apnea syndrome in children: State of the art: Int J Environ Res Public Health, 2019; 16(18); 3235
47. Ingram DG, Matthews CK, Effect of adenotonsillectomy on c-reactive protein levels in children with obstructive sleep apnea: A meta-analysis: Sleep Med, 2013; 14(2); 172-76
48. Marcus JA, Pothineni A, Marcus CZ, Bisognano JD, The role of obesity and obstructive sleep apnea in the pathogenesis and treatment of resistant hypertension: Curr Hypertens Rep, 2014; 16(1); 411
49. Carnethon MR, Johnson DA, Sleep and resistant hypertension: Curr Hypertens Rep, 2019; 21(5); 34
50. Martinez-Garcia MA, Capote F, Campos-Rodriguez F, Effect of CPAP on blood pressure in patients with obstructive sleep apnea and resistant hypertension: The HIPARCO randomized clinical trial: JAMA, 2013; 310(22); 2407-15
51. Arnaud C, Bochaton T, Pepin JL, Belaidi E, Obstructive sleep apnoea and cardiovascular consequences: Pathophysiological mechanisms: Arch Cardiovasc Dis, 2020; 113(5); 350-58
52. Belaidi E, Thomas A, Bourdier G, Endoplasmic reticulum stress as a novel inducer of hypoxia inducible factor-1 activity: Its role in the susceptibility to myocardial ischemia-reperfusion induced by chronic intermittent hypoxia: Int J Cardiol, 2016; 210; 45-53
53. Bourdier G, Flore P, Sanchez H, High-intensity training reduces intermittent hypoxia-induced ER stress and myocardial infarct size: Am J Physiol Heart Circ Physiol, 2016; 310(2); H279-89
Figures
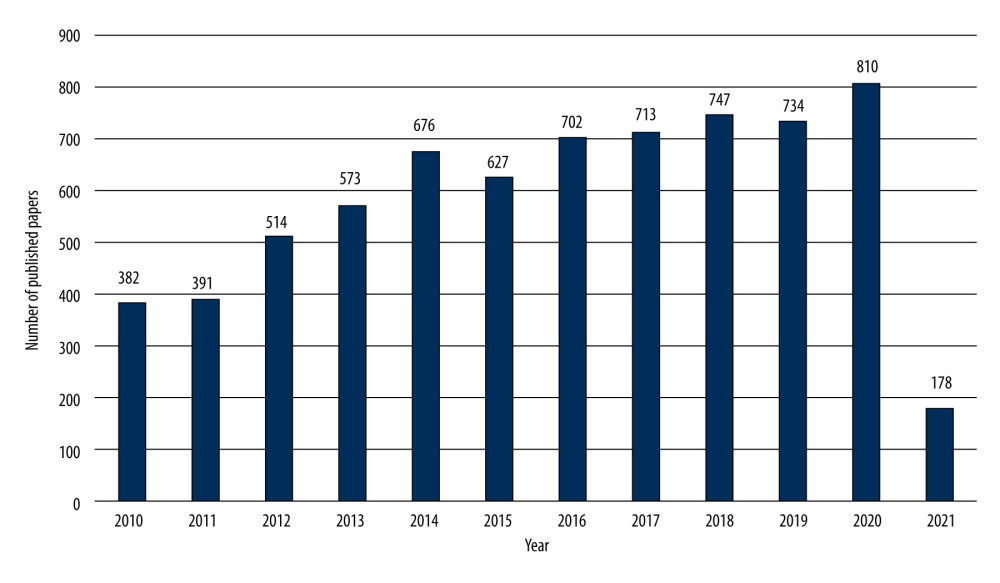 Figure 1. The number and linear growth trends of publications (Citespace, Version 5.7 R5, University of Dressel, Chaomei Chen).
Figure 1. The number and linear growth trends of publications (Citespace, Version 5.7 R5, University of Dressel, Chaomei Chen).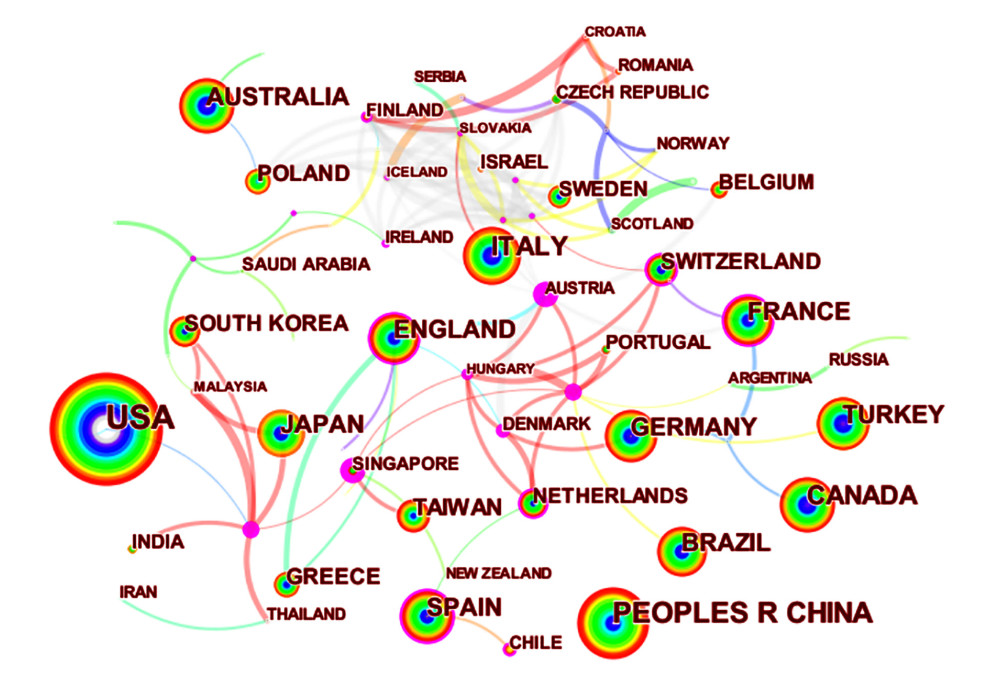 Figure 2. Co-occurrence map of countries (N97=, E=157) (Citespace, Version 5.7 R5, University of Dressel, Chaomei Chen).
Figure 2. Co-occurrence map of countries (N97=, E=157) (Citespace, Version 5.7 R5, University of Dressel, Chaomei Chen).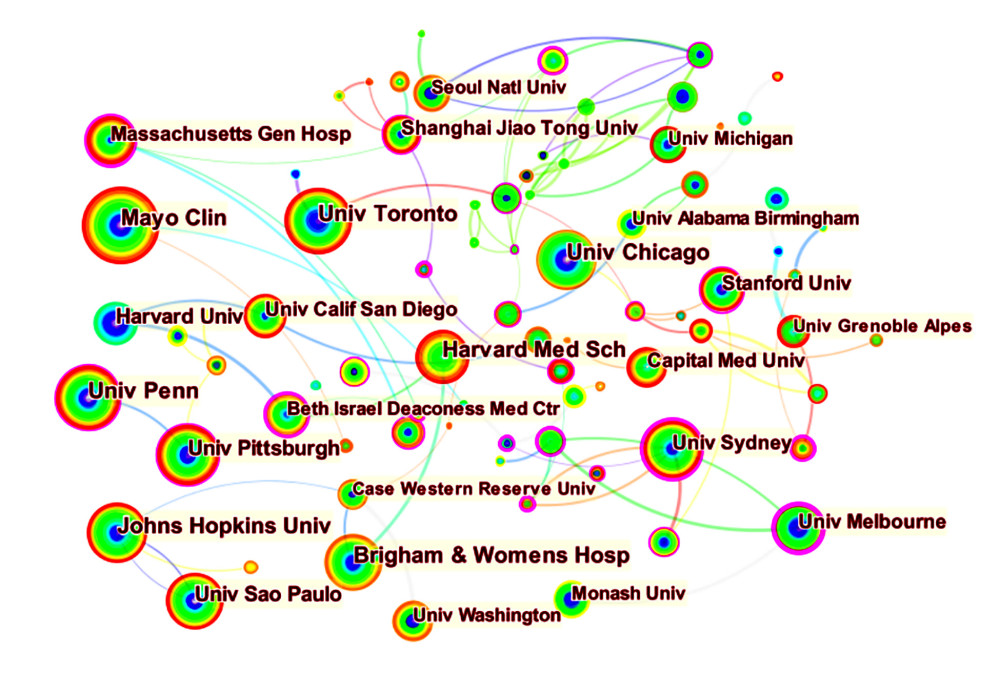 Figure 3. Co-occurrence map of institutions (N=265, E=369) (Citespace, Version 5.7 R5, University of Dressel, Chaomei Chen).
Figure 3. Co-occurrence map of institutions (N=265, E=369) (Citespace, Version 5.7 R5, University of Dressel, Chaomei Chen).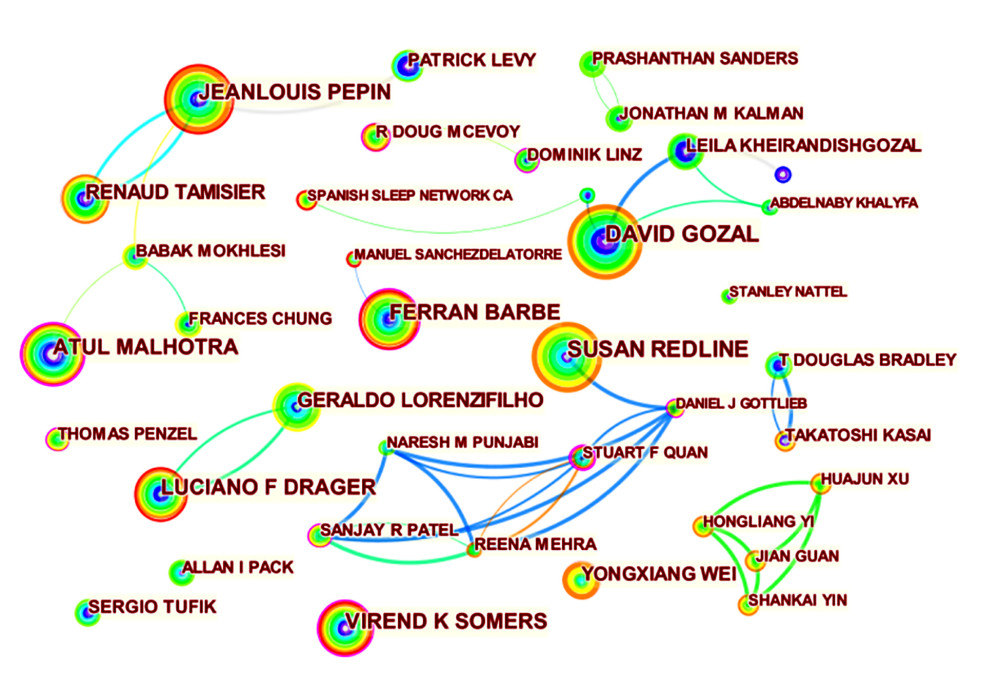 Figure 4. Co-occurrence map of authors (N=596, E=1514) (Citespace, Version 5.7 R5, University of Dressel, Chaomei Chen).
Figure 4. Co-occurrence map of authors (N=596, E=1514) (Citespace, Version 5.7 R5, University of Dressel, Chaomei Chen).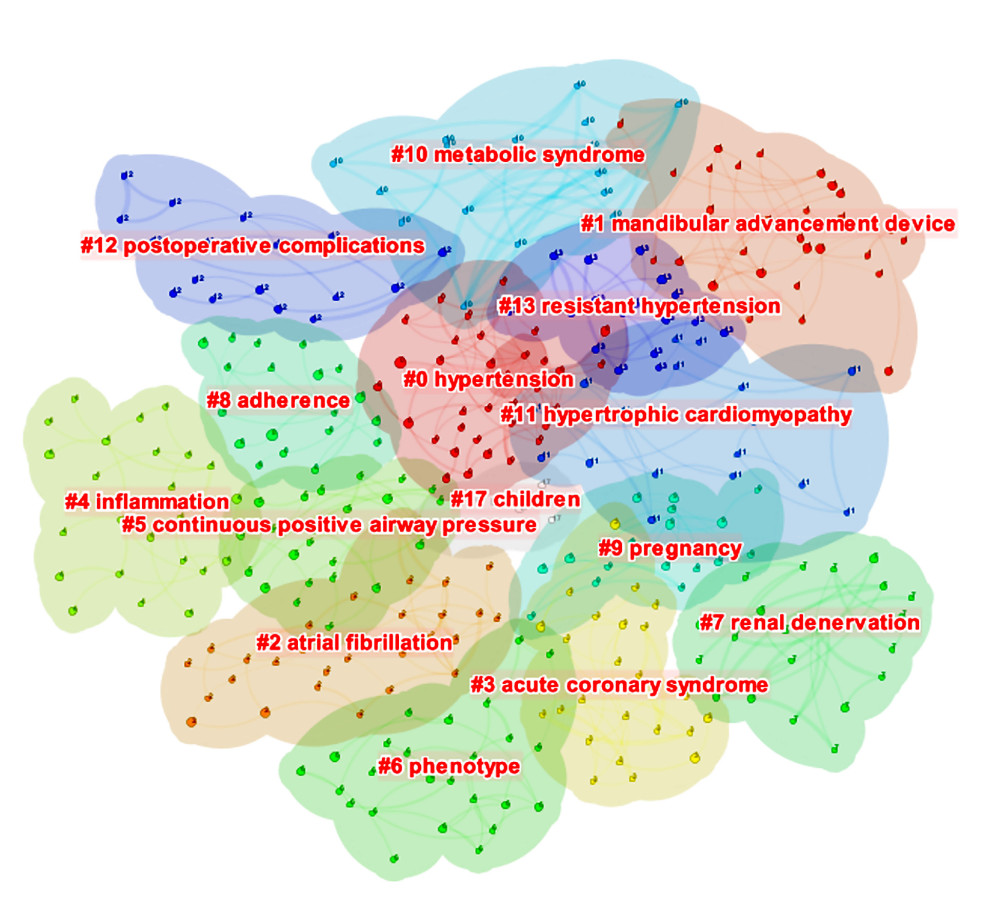 Figure 5. The clustered network map of co-cited references (N=420, E=579, Modularity Q=0.8333, Silhouette=0.9504) (Citespace, Version 5.7 R5, University of Dressel, Chaomei Chen).
Figure 5. The clustered network map of co-cited references (N=420, E=579, Modularity Q=0.8333, Silhouette=0.9504) (Citespace, Version 5.7 R5, University of Dressel, Chaomei Chen).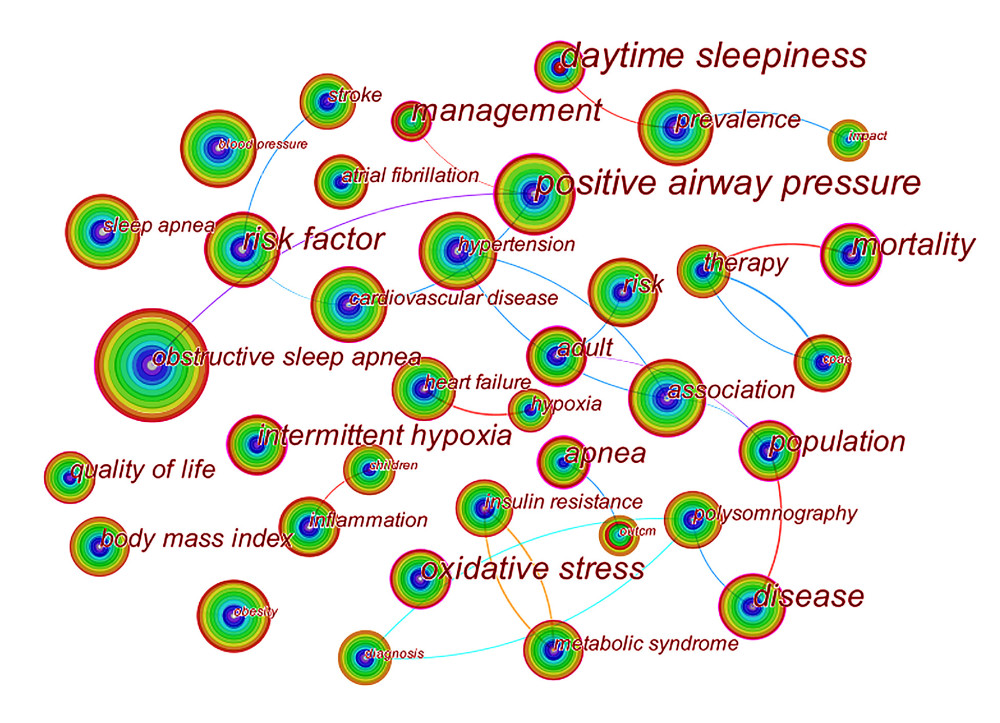 Figure 6. Co-occurrence map of keywords (N=111, E=137) (Citespace, Version 5.7 R5, University of Dressel, Chaomei Chen).
Figure 6. Co-occurrence map of keywords (N=111, E=137) (Citespace, Version 5.7 R5, University of Dressel, Chaomei Chen).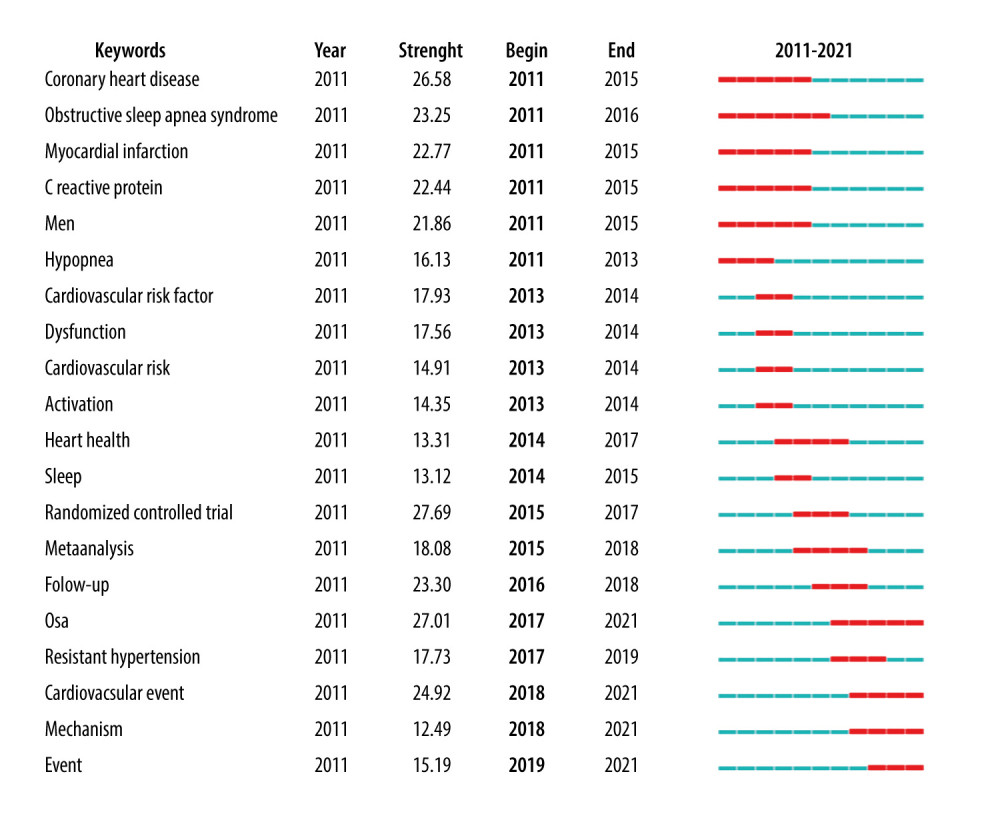 Figure 7. Top 20 keywords with the strongest citation bursts in original articles (Citespace, Version 5.7 R5, University of Dressel, Chaomei Chen).
Figure 7. Top 20 keywords with the strongest citation bursts in original articles (Citespace, Version 5.7 R5, University of Dressel, Chaomei Chen). Tables
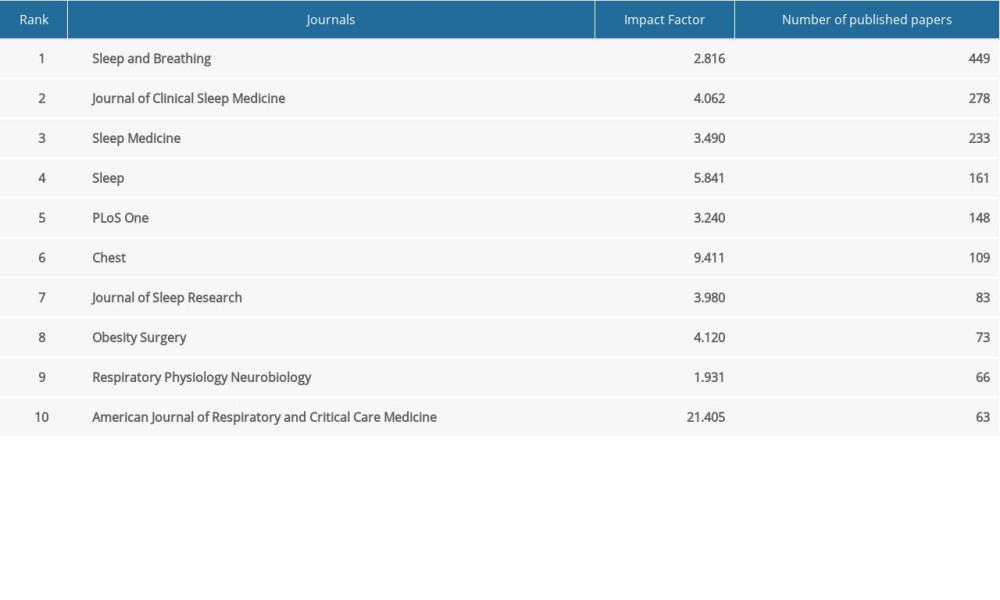 Table 1. The top 10 productive journals.
Table 1. The top 10 productive journals. Table 2. Top 10 countries and institutions in terms of frequency.
Table 2. Top 10 countries and institutions in terms of frequency. Table 3. Top 10 countries and institutions in terms of centrality.
Table 3. Top 10 countries and institutions in terms of centrality.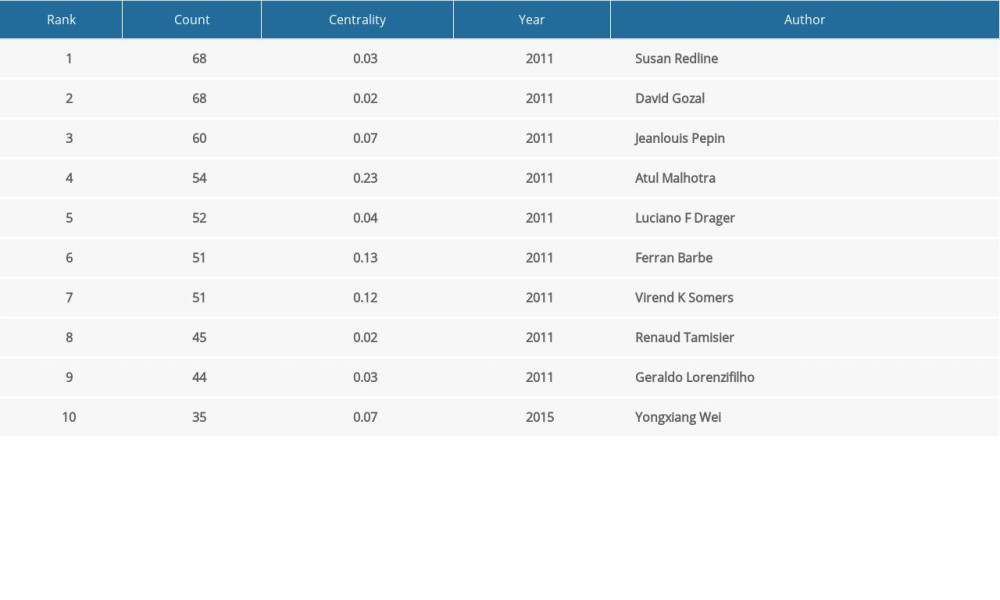 Table 4. Top 10 most productive authors.
Table 4. Top 10 most productive authors.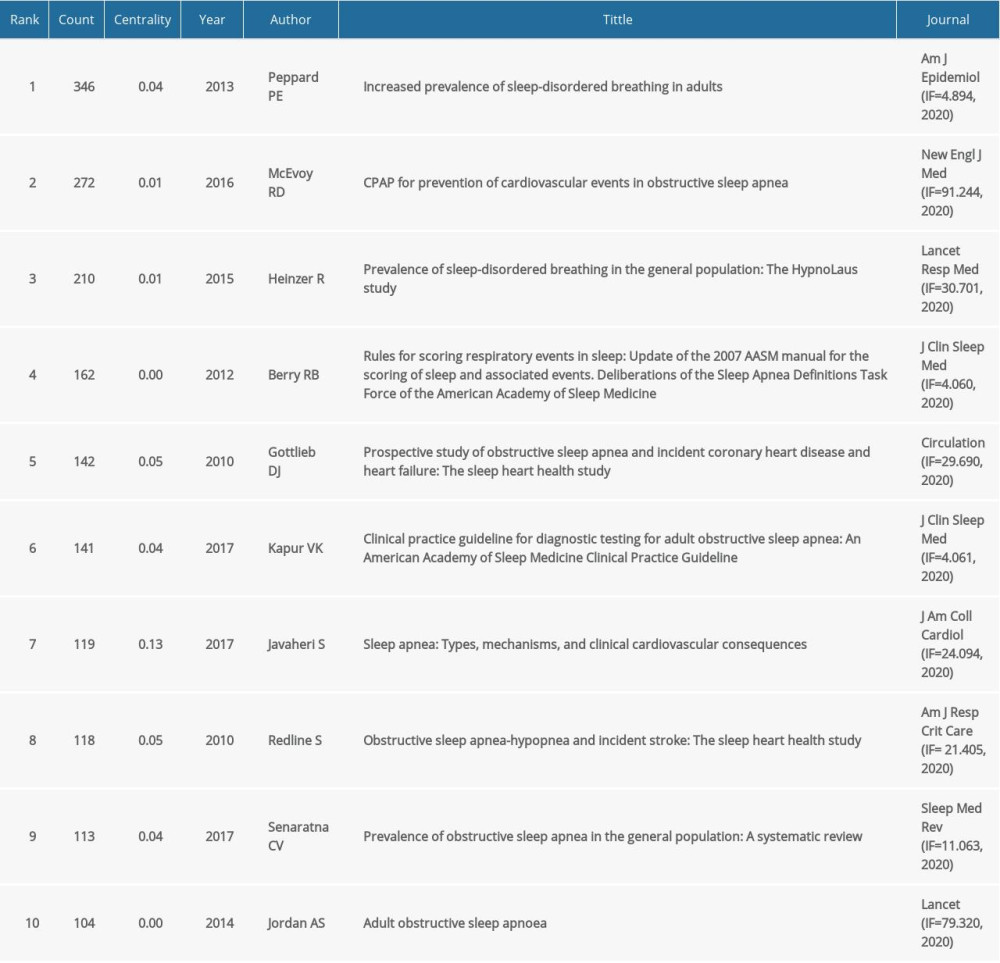 Table 5. Top 10 co-cited references in terms of frequency.
Table 5. Top 10 co-cited references in terms of frequency.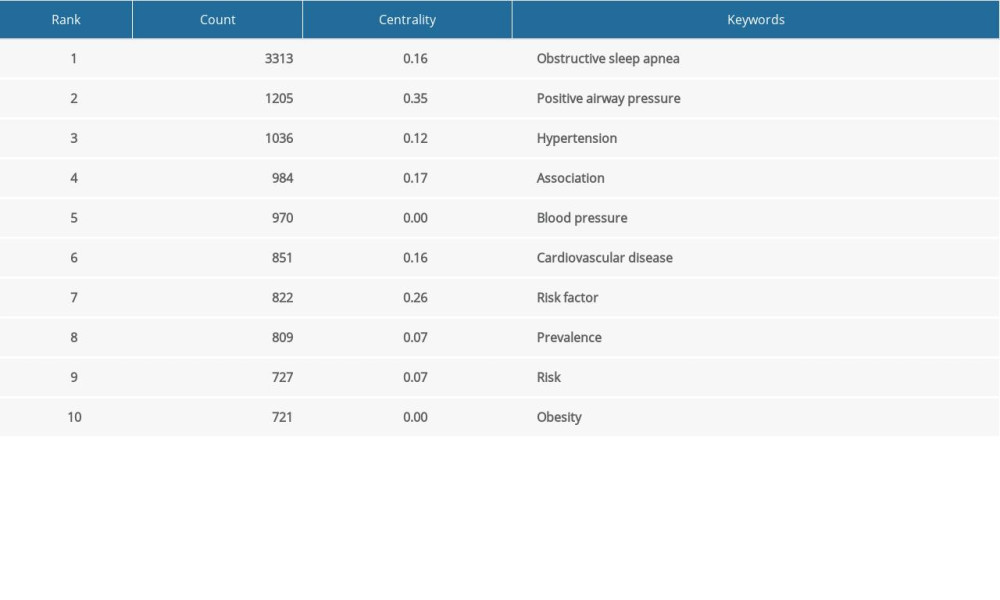 Table 6. Top 10 keywords in terms of frequency.
Table 6. Top 10 keywords in terms of frequency.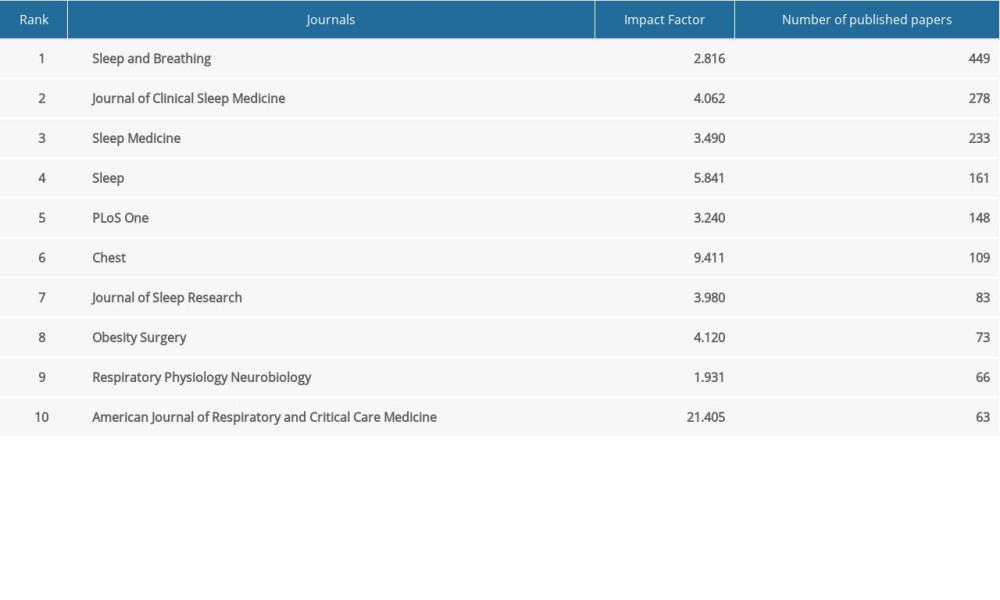 Table 1. The top 10 productive journals.
Table 1. The top 10 productive journals. Table 2. Top 10 countries and institutions in terms of frequency.
Table 2. Top 10 countries and institutions in terms of frequency. Table 3. Top 10 countries and institutions in terms of centrality.
Table 3. Top 10 countries and institutions in terms of centrality.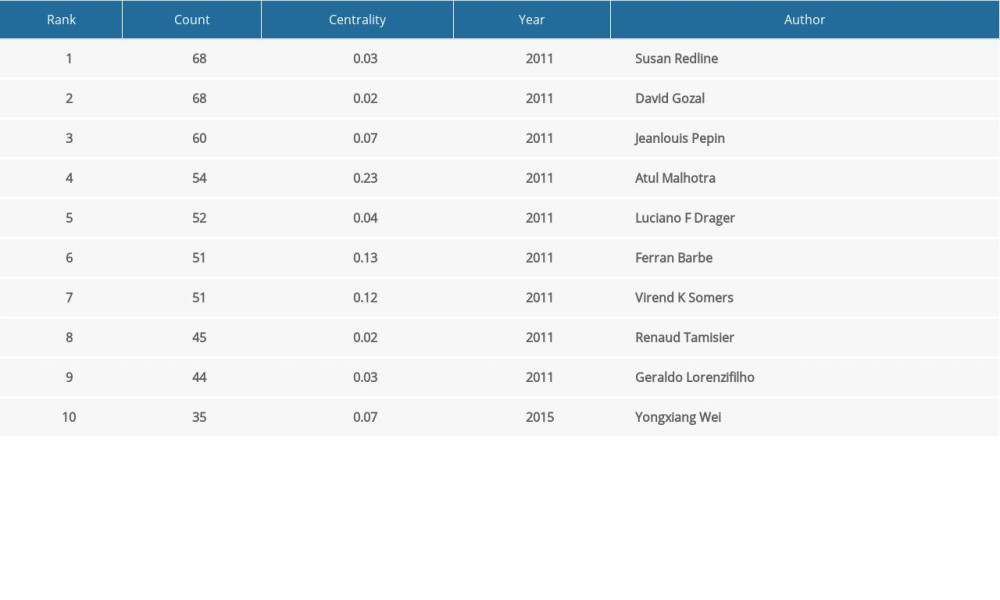 Table 4. Top 10 most productive authors.
Table 4. Top 10 most productive authors.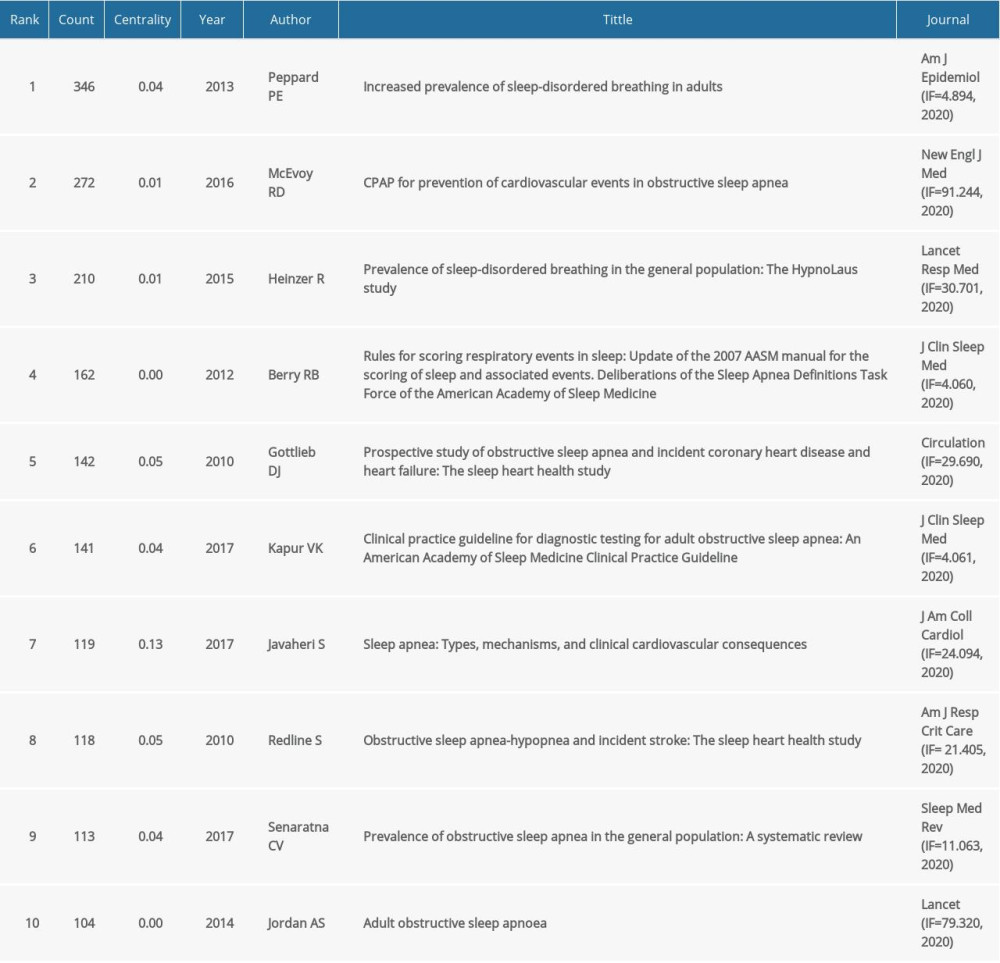 Table 5. Top 10 co-cited references in terms of frequency.
Table 5. Top 10 co-cited references in terms of frequency.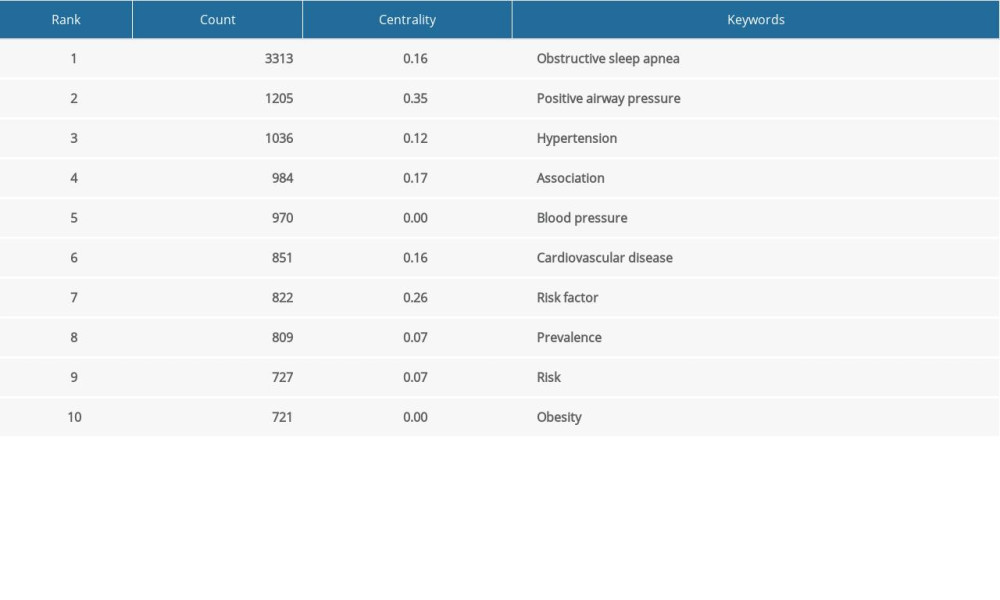 Table 6. Top 10 keywords in terms of frequency.
Table 6. Top 10 keywords in terms of frequency. In Press
08 Mar 2024 : Clinical Research
Evaluation of Foot Structure in Preschool Children Based on Body MassMed Sci Monit In Press; DOI: 10.12659/MSM.943765
15 Apr 2024 : Laboratory Research
The Role of Copper-Induced M2 Macrophage Polarization in Protecting Cartilage Matrix in OsteoarthritisMed Sci Monit In Press; DOI: 10.12659/MSM.943738
07 Mar 2024 : Clinical Research
Knowledge of and Attitudes Toward Clinical Trials: A Questionnaire-Based Study of 179 Male Third- and Fourt...Med Sci Monit In Press; DOI: 10.12659/MSM.943468
08 Mar 2024 : Animal Research
Modification of Experimental Model of Necrotizing Enterocolitis (NEC) in Rat Pups by Single Exposure to Hyp...Med Sci Monit In Press; DOI: 10.12659/MSM.943443
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








