14 November 2021: Clinical Research
Clinical Features and Temporal Lung Radiographic Changes in 25 Patients Recovering from COVID-19 Pneumonia: A Retrospective Case-Control Study
Chao Hu1ABCDEG, Jian Ping Zeng2ACDFG, Ke Peng3ABCDF, Hong Xia4BCEF, Huan Ming Zhang5BCDEF, Zhi Zhong5BCDE, Ming Yan Jiang1ABDFG*DOI: 10.12659/MSM.933381
Med Sci Monit 2021; 27:e933381
Abstract
BACKGROUND: Little is known of the changes in lung radiographic characteristics over time in patients recovering from COVID-19. This study analyzed the clinical features and temporal lung radiographic changes in patients with moderate and severe COVID-19 pneumonia who did not require invasive mechanical ventilation during the acute and convalescent periods.
MATERIAL AND METHODS: The data of 25 patients with COVID-19 pneumonia from January 29, 2020, to November 24, 2020, who did not require invasive mechanical ventilation and who were followed up were retrospectively collected. The 25 patients were divided into severe and moderate groups. Clinical characteristics and computed tomography (CT) manifestations were compared. A total of 121 consecutive thin-slice CT scans were collected at 4 weeks, 2 months, and 5 months after admission to evaluate lung abnormalities in the patients. The CT score was used to assess disease severity.
RESULTS: The severe group had a lower rate of nucleic acid conversion within 10 days of admission and higher D-dimer, creatine kinase, and lactate dehydrogenase values. In the severe group, hospital stay was longer and hospitalization costs were higher. The average CT score of the severe group peaked in the second week, while the moderate group peaked in the first week and then decreased over time. There were no statistically significant differences in the average CT score between the 2 groups at the 5-month follow-up.
CONCLUSIONS: The pulmonary lesions of patients recovering from COVID-19 and who do not require invasive mechanical ventilation were gradually absorbed and resolved over time.
Keywords: bronchopneumonia, COVID-19, Tomography, X-Ray Computed, COVID-19, Case-Control Studies, Female, Humans, Longitudinal Studies, Lung, Male, SARS-CoV-2
Background
COVID-19, which is caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), is reported to have led to 211 288 358 infections and 4 422 666 deaths worldwide as of August 22, 2021 according to the data of the World Health Organization [1]. COVID-19 mainly causes pneumonia but it also affects other organs, such as the gastrointestinal, hepatobiliary, cardiovascular, blood, nervous, and urinary systems [2–5].
Pneumonia caused by a viral infection usually shows lung abnormalities after inflammation. Among the coronavirus family, SARS-CoV and Middle East respiratory syndrome coronavirus (MERS-CoV) cause not only SARS and MERS but also lung abnormalities, especially fibrosis, which is most common in patients with severe SARS-CoV and MERS-CoV [6,7]. Zhou et al reported that 60% of patients discharged from the hospital after SARS-CoV-2 infection showed fibrosis-related changes [8]. At present, we know little about the pathophysiological outcomes of fibrosis-related changes after COVID-19.
It is unclear whether, over time, lung abnormalities can be gradually absorbed and lung function can be gradually restored after a patient has COVID-19. Studies have mainly focused on severe patients who required mechanical ventilation, and there are few studies on patients with severe disease who did not require mechanical ventilation. Because the current SARS-CoV-2 nucleic acid test result can turn positive for survivors of COVID-19, there are high risks associated with administering pulmonary function tests among these patients [9]. Therefore, chest computed tomography (CT) scans are more suitable than pulmonary function tests for assessing a patient’s lung condition during the recovery period, although the patients can be exposed to higher levels of radiation with CT scanning. We conducted a longitudinal study to analyze the CT findings of patients with COVID-19 pneumonia with moderate and severe disease who did not require invasive mechanical ventilation during the acute and convalescent periods.
Material and Methods
STUDY PARTICIPANTS:
The data of 25 patients diagnosed with COVID-19 pneumonia from January 29, 2020, to November 24, 2020, and who were followed up until the end of the study were retrospectively collected on December 8, 2020. In the process of data collection, patient information was anonymized. By November 24, 2020, the public health clinical center of a 3A hospital, the designated hospital of a city in South China, had 25 confirmed cases of COVID-19 pneumonia. The inclusion criteria were (1) patients who tested positive for SARS-CoV-2 by nucleic acid polymerase chain reaction (PCR); (2) patients with chest CT findings confirming that there were new lung abnormalities within 1 week before and after the positive nucleic acid test; (3) patients who do not require mechanical ventilation; and (4) patients who underwent at least 2 chest CT examinations during the entire study period. The criteria for severe patients and discharge standards were based on the “COVID-19 Pneumonia Diagnosis and Treatment Plan (Trial Version 8)” released by the National Health Commission of China [10]. The criteria were as follows: (1) shortness of breath, respiratory rate ≥30 breaths/min and (2) at rest, percutaneous oxygen saturation less than 93% or ratio of arterial oxygen to fractional inspired oxygen concentration (PaO2/FiO2) (sea level) of 300 mmHg or lower (1 mmHg=0.133 kPa). The PaO2/FiO2 ratio was corrected according to the following formula at high altitudes (over 1000 m): PaO2/FiO2×(atmospheric pressure [mmHg]/760). The pulmonary imaging findings showed significant progression, and 50% of the lesions were considered severe within 24 to 48 h. The discharge criteria were (1) the patient’s body temperature was normal for more than 3 days; (2) respiratory symptoms improved significantly; (3) pulmonary imaging findings showed significant improvement in acute exudative lesions; and (4) 2 consecutive respiratory tract specimens showed negative nucleic acid test results (at least 24 h apart). The patients who met the above conditions were discharged. All patients were discharged from the hospital before March 2020. We continued to perform follow-up examinations after the patients were discharged from the hospital. This retrospective study was approved by the Institutional Review Board of Xiangtan Central Hospital, and the requirement for informed consent was waived.
CLINICAL DATA COLLECTION:
The clinical laboratory of the hospital was approved by the Chinese Center for Disease Control (CDC) to conduct this study, and the PCR tests were performed by another laboratory. Nasopharyngeal swabs and blood samples were collected from the patients, and SARS-CoV-2 was detected by PCR testing using a kit that was developed by the Chinese CDC. Blood cell counts, clotting function, blood biochemistry parameters, and infection indicators, including renal and liver function, creatine kinase, lactate dehydrogenase, electrolytes, lactic acid, and ferritin, were assessed in all patients upon admission. Routine bacterial and fungal tests were also performed. The antiviral drugs and corticosteroids used were lopinavir/ritonavir (400 mg/100 mg, twice per day), arbidol (200 mg, 3 times per day), and methylprednisolone (40 mg, once per day), as appropriate, in the patients who presented significant pulmonary exudation. Oxygen support techniques, including nasal catheter oxygen, high-flow oxygen, and noninvasive/invasive mechanical ventilation, were performed, depending on the severity of hypoxemia in each patient. Repeated tests for SARS-CoV-2 were performed in patients confirmed to be infected with SARS-CoV-2 to show virus clearance before discharge or the termination of isolation. The clinical records, laboratory examination results, and chest CT results of all patients with COVID-19 confirmed by the laboratory in the public health clinical center of the hospital were reviewed.
CT IMAGE ACQUISITION:
For CT imaging, the patients were placed in a supine position, and a thin-slice CT scan was performed at the end of inhalation. The scan range was from the entrance of the thorax to under the lateral costophrenic angle. All chest CT scans were performed with the same scanner: a 16-slice spiral CT scanner (Mx 16, Philips). The tube voltage was 120 kV, the tube current was 150–250 mA, wheelbase scans were performed, slice thickness was 1 mm, slice distance was 10 mm, and the matrix size was 512×512. A total of 121 scans were performed in the 25 patients. The images were photographed at mediastinal settings (window width, 360 Hounsfield units [HU]; window level, 60 HU) and lung settings (window width, 1600 HU; window level, 600 HU).
CT IMAGE EVALUATION:
Two experienced chest radiologists independently evaluated all the chest images. The conclusions of the assessment were discussed, and a consensus was reached. The patients were divided into severe and moderate groups according to the criteria discussed by the clinicians and radiologists. The main CT classification modes used were the same as those defined by the Fleischer Society and other scholars: ground-glass opacity (GGO) (increased attenuation of the fuzzy area not covering the underlying blood vessels), consolidation (homogeneous turbid and dark parenchyma with potential blood vessels), mixed (combining integration, frosted-glass transparency, and net-like transparency of architectural deformation), reticular (large linear or curved opaque or fine subpleural reticular structure, without a large amount of ground-glass-like opacity), and honeycomb patterns. GGO could be exhibited by GGO alone, GGO+intralobular, and GGO+linear. The distribution of the lesions was mainly peripheral (mainly involving the surrounding one-third of the lungs), central (mainly involving the central two-thirds of the lungs), or both central and peripheral (continuous involvement of lung segments). In addition, air bronchogram (the bronchi containing gas were highly attenuated in consolidation and GGO), crazy-paving pattern (the thickening of the interlobular septum and the inner line of the lobules were superimposed on the GGO), pleural effusion, pneumothorax, and pleural hyperplasia thickening could be observed. The CT semiquantitative scoring method was used to assess the severity of the lesions [11]: the lungs were divided into 3 lung areas: the upper lung area (above the carina), middle lung area (below the carina to the inferior pulmonary vein), and lower lung area (below the pulmonary vein). Each lung area was scored according to the involvement of the lesion, as follows: 0% involvement, score of 0; involvement of less than 25%, score of 1; involvement of 25% to 50% or less, score of 2; involvement of 50% to 75% or less, score of 3; involvement of more than 75%, score of 4. The total score corresponded to the degree of lung involvement, assessing a total of 6 lung regions in both lungs, with the maximum CT score of 24. All scans were classified according to whether the scan was performed during the first week, second week, third week, fourth week, second month, or fifth month after admission.
STATISTICAL ANALYSIS:
The data were expressed as medians and interquartile ranges for the continuous variables and as numbers (%) for the categorical variables. The continuous and categorical variables were compared using a 2-tailed independent sample
The study was approved by the Institutional Review Board of Xiangtan Central Hospital (2020-11-03), and individual consent for this retrospective analysis was waived.
Results
CLINICAL FEATURES AND TREATMENT OF PATIENTS IN THE SEVERE AND MODERATE GROUPS:
As of November 24, 2020, a total of 25 patients were included in the study, including 13 men and 12 women. There were 8 patients in the severe group and 17 patients in the moderate group. The average time from onset to the aggravation of disease in severe cases was 10.2±3.7 days. The demographic data, clinical symptoms, and laboratory test results for the patients are summarized in Tables 1 and 2.
Three patients had a history of smoking, 2 (25%) of whom were severely ill. Ten patients (40%) had underlying diseases; the most common were a history of surgery, hypertension, and diabetes. The most common pneumonia symptom was cough (80%), and the incidence of fever was 65%. As indicated by urea nitrogen and creatinine levels, abnormalities in renal function were more common in the clinically severe group (2.8 vs 4.4 and 65 vs 80;
All patients enrolled were treated with the antiviral therapies lopinavir/ritonavir and arbidol. Nine patients (34.62%) underwent glucocorticoid therapy; 1 (5.6%) was moderate and 8 (100%) were severe. Noninvasive ventilation was used in 3 patients in the severe group. For the moderate group, the average length of hospital stay was 12.5 days, and the average hospital cost was 7663.27 RMB. The average hospitalization time was 18.5 days for the severe group, and the average hospitalization cost was 42 401.85 RMB. Thus, hospitalization costs were significantly different between the 2 groups, while the average hospitalization time was not (Table 3).
THIN-SECTION CT FINDINGS:
Figure 1 compares the longitudinal average CT scores of the severe and moderate groups. The average CT score of the severe group was higher than the average CT score of the moderate group. The average score of the severe group was higher for the first 4 scans, indicating the scope of the lesion. After the fifth scan, the average CT score of the clinically severe group decreased, indicating that the condition improved. The average CT score of the moderate group was the highest for the initial scan. Over time, the score decreased. The average CT score differed significantly between the 2 groups for the first 5 scans. At the last scan, there were no significant differences in the CT score between the severe and moderate groups, suggesting that the residual lesions of the 2 groups improved (2.00 vs 0.73; P=0.085).
Table 4 describes the main CT types and CT scores of the 25 patients. The patients underwent a total of 121 scans. The scans were performed upon admission and at 2 and 3 to 4 weeks after admission. Follow-up scans were conducted after discharge. The follow-up scans and final scans were performed at least 2 and 5 months after admission. The abnormal patterns of patients differed between the severe and moderate groups. In the initial scan, the main type was GGO (5 [5/8]) in the severe group and mixed (10 [10/17]) in the moderate group. As shown in Figure 2A, the main lesion types in the CT scans varied and exhibited changes over time. In the second week, the main type changed to the mixed type in the severe group, increasing the average CT score (10) (Figure 1). The main type of lesion in the moderate group also changed to the mixed type. In the second month of follow-up, the moderate group showed CT imaging absorption (5) and irregular striped shadows (3); the severe group mainly showed mixed (6) and GGO patterns (3). At the last follow-up, most of the patients in the severe and moderate groups showed imaging absorption and irregular grid-like shadows.
Tables 5 and 6 summarize the longitudinal changes in the 2 groups of patients. According to the initial scans, the lesions were mainly bilateral and multicenter. In the moderate group, there were 14 cases of GGO and 3 cases of paving stone signs in the initial lesions, and in the severe group, there were 8 cases of GGOs and 7 cases of paving stone signs. GGO in the patients in the severe group mainly manifested as thickening of the GGO+lobular septum (Figure 3). As shown in Figure 2B, the main type of GGO in the severe group was GGO+lobular septal thickening in the first scan, which appeared as GGO+irregular strips in the final scan. The paving stone sign was reversed at 2 months. In the moderate group, the lesions were concentrated in the periphery. In the severe group, 1 patient showed peripheral and central lesions. In the third scan, some patients in the severe group had pleural effusion (in the first scan, 1 patient; in the second scan, 2 patients; and in the third scan, 1 patient). In the subsequent scans, the cases of pleural effusion were absorbed. In the follow-up and final scans, 9 patients in the moderate group showed negative, while only 2 patients in the severe group showed negative. A total of 9 patients showed residual lesions, with an average score of 1.06, with 6 having irregular striped shadows, 2 having mixed-type lesions, and 1 having GGO. Figures 3–6 show 4 CT patterns of GGO, consolidation, GGO combined with part consolidation, and mixed, respectively.
Discussion
This study described the clinical features and lung abnormality changes of 25 patients with COVID-19 pneumonia who did not require invasive mechanical ventilation from admission to the 5-month follow-up. Clinically severe patients had more test abnormalities than did the moderate group on admission.
In the first 2 months, the clinical pulmonary disease in the severe patients without mechanical ventilation was more serious than that in the moderate group. However, at the 5-month follow-up, there was no statistically significant difference in the average CT scores of pulmonary lesions between the 2 groups, suggesting that pulmonary lesions in severe patients who did not require invasive mechanical ventilation were similar to those in the moderate group at the fifth month after onset.
There were fewer negative nucleic acid test results with the throat swabs in the severe group than in the moderate group within 10 days, which might have been related to the severe group’s decreased ability to clear the virus but might also have been related to the use of glucocorticoids in the severe group. Previous studies on SARS showed that glucocorticoids could delay virus clearance [12]. Moreover, an influenza study showed that the virus clearance rate was weaker in severe cases than in moderate cases [13]. Consistent with previous studies [14,15], in the present study we found that patients with severe disease showed hypercoagulability and creatine kinase abnormalities, which might have been related to the expression of the angiotensin-converting enzyme 2 receptor of SARS-CoV-2 in the vascular endothelium and heart, endothelial dysfunction, and infection damage [4,16]. In addition, in the present study, all severe patients were administered glucocorticoids. In the RECOVERY trial, glucocorticoids improved the survival rate among severe cases [17]. In the present study, the severe group showed longer hospital stays and higher hospital costs.
GGO was more commonly observed on initial thin-slice CT scans in severe cases, as supported by the study by Han et al [18], but mixed GGO was more commonly observed in moderate cases. Three patients presented with consolidation. In the second week, the main CT type in the severe group changed to mixed.
Both the severe and moderate groups’ lung CT lesions mainly manifested as bilateral lesions. Those in the moderate group mostly manifested as peripheral lesions near the subpleural. Those in the severe group manifested as multicentric lesions. These results are somewhat inconsistent with those of Wei et al, which might be related to those authors’ not conducting a subgroup analysis of patients with severe illnesses [19]. Interestingly, in the present study, the CT scores declined gradually over time in the moderate group, while in the severe group, the CT scores were the highest in the second week and then gradually decreased, consistent with the time of exacerbation of pneumonia reported previously [8,18,20]. Moreover, the severe group had more cases with air bronchogram and pleural effusion that persisted longer than in the moderate group, which often indicates worsening of the disease in patients with pneumonia [21,22].
Through regular thin-slice CT examinations of the patients, we found that the lung lesions of the patients with pneumonia could gradually absorb and improve, and moderate cases showed irregular reticular patterns earlier than did those with severe cases, suggesting that the lesions entered the recovery stage or possible stages of fibrosis. In the subsequent stage of recovery, the CT score was higher in the severe group than in the moderate group in the first 2 months. However, after 5 months of follow-up, the patients with and without severe lung disease did not show statistically significantly different scores, suggesting that lung lesions after COVID-19 pneumonia infection could absorb over time and that the degree of absorption of the remaining lesions might not be consistent with the severity of the initial condition. Regarding patients with SARS pneumonia, studies including follow-up examinations have also shown that pulmonary fibrosis can heal on its own and the mechanism of fibrosis after viral infection might be inconsistent with that of idiopathic pulmonary fibrosis [23]. Therefore, further exploration of the pathophysiological mechanisms is still necessary.
There are limitations to our study. It should be noted that the patients in our study were mainly from 1 city. Due to the control of the epidemic in China, the sample size was only 25 cases, potentially leading to selection bias. Moreover, due to the infectivity of SARS-CoV-2, we did not conduct a lung function test, which might have prevented us from revealing a trend in the changes in lung function in the recovered patients.
Conclusions
The early imaging recovery of patients with severe COVID-19 without endotracheal intubation was slower than that of moderate patients, and the residual lesions were more pronounced. However, after 5 months of follow-up, there was no significant difference in image scores between severe patients without endotracheal intubation and moderate patients. The absorption of residual pulmonary lesions after SARS-CoV-2 infection was gradual. The lesions from SARS-CoV-2 infection might be inconsistent with the pulmonary lesions of SARS and MERS; therefore, a longer follow-up period for thin-slice CT and accompanying functional studies is needed to determine the long-term pulmonary sequelae of SARS-CoV-2.
Figures
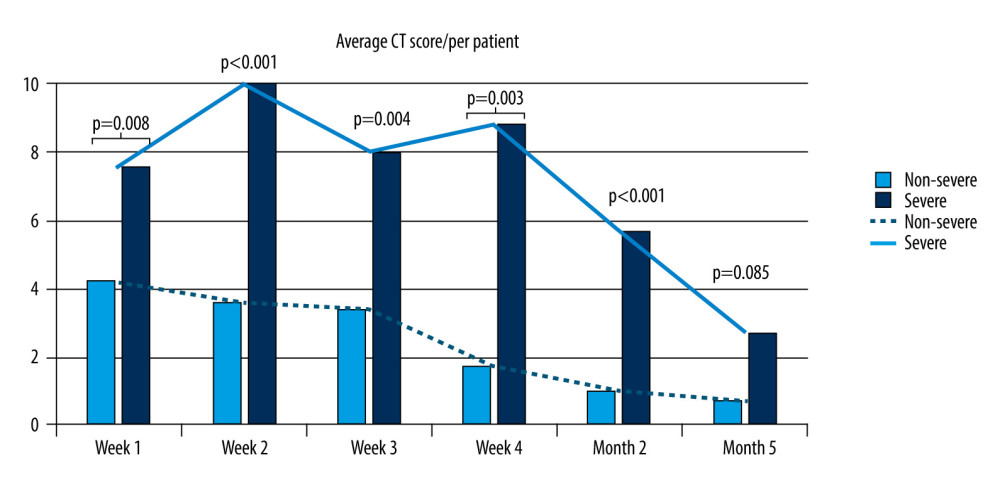 Figure 1. Temporal change in average computed tomography score in moderate and clinically severe groups. Microsoft Excel, Office 365.
Figure 1. Temporal change in average computed tomography score in moderate and clinically severe groups. Microsoft Excel, Office 365. 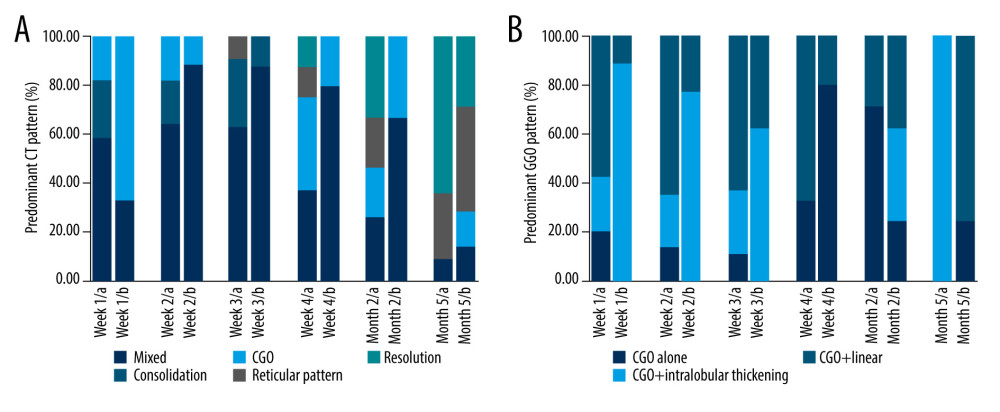 Figure 2. (A, B) Temporal change in the main patterns of computed tomography and ground-glass opacity in moderate and clinically severe groups. Microsoft Excel, Office 365.
Figure 2. (A, B) Temporal change in the main patterns of computed tomography and ground-glass opacity in moderate and clinically severe groups. Microsoft Excel, Office 365. 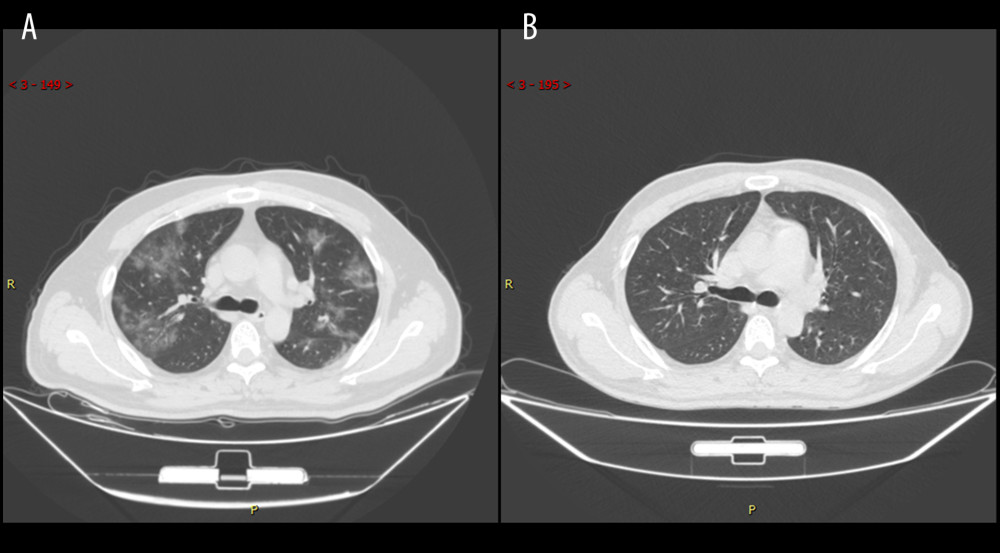 Figure 3. Series computed tomography (CT) scans in 39-year-old man with COVID-19 pneumonia. (A) CT scan obtained on illness day 7 shows diffuse ground-glass opacity. (B) CT scan obtained of illness at month 5 shows that the lesion had been absorbed.
Figure 3. Series computed tomography (CT) scans in 39-year-old man with COVID-19 pneumonia. (A) CT scan obtained on illness day 7 shows diffuse ground-glass opacity. (B) CT scan obtained of illness at month 5 shows that the lesion had been absorbed. 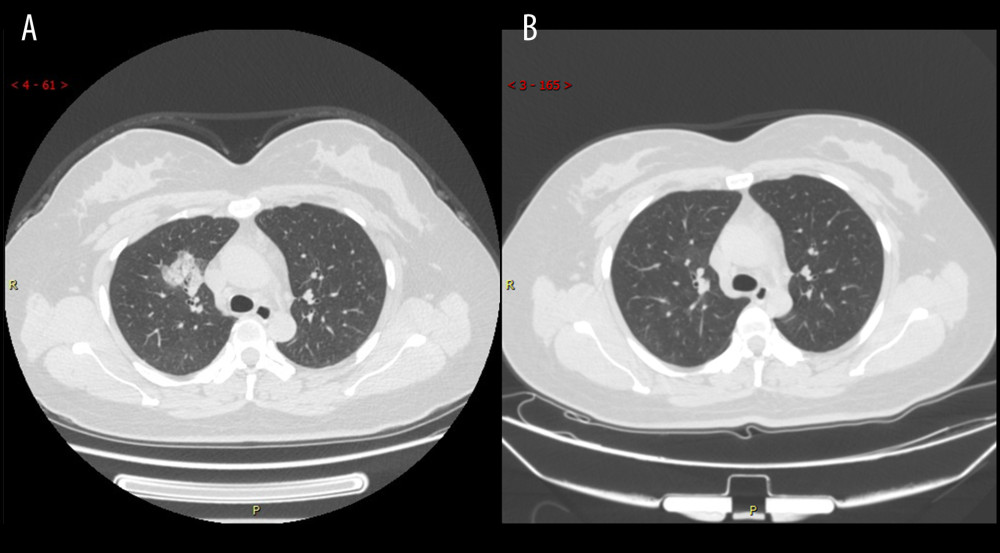 Figure 4. Series computed tomography (CT) scans in a 34-year-old woman with COVID-19 pneumonia. (A) CT scan obtained on illness day 10 shows consolidation in right lung. (B) CT scan obtained at month 2 shows the obvious absorption of abnormalities.
Figure 4. Series computed tomography (CT) scans in a 34-year-old woman with COVID-19 pneumonia. (A) CT scan obtained on illness day 10 shows consolidation in right lung. (B) CT scan obtained at month 2 shows the obvious absorption of abnormalities. 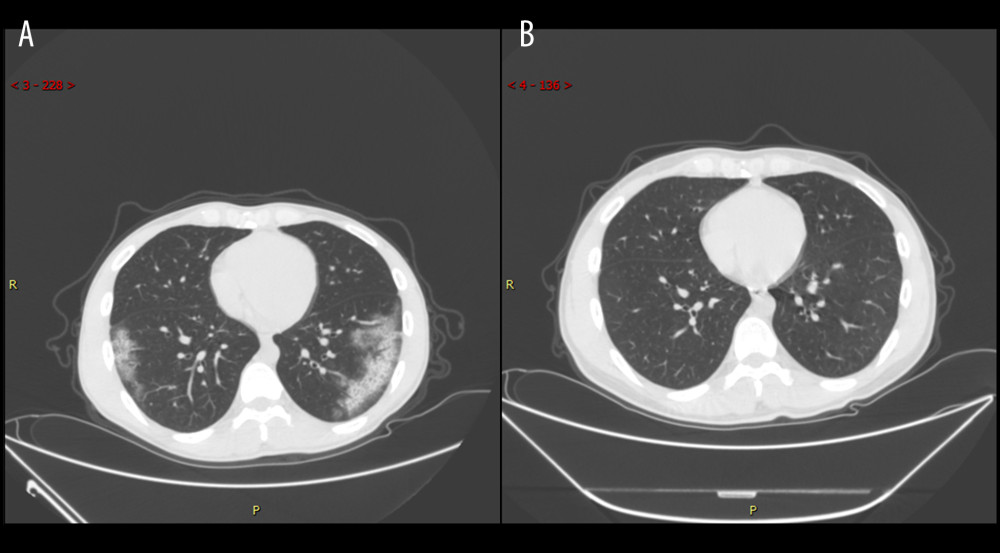 Figure 5. Series computed tomography (CT) scans in 29-year-old man with COVID-19 pneumonia. (A) CT scan obtained on illness day 17 shows ground-glass opacity combined with partial consolidation. (B) CT scan obtained at month 2 shows that the lesion had been absorbed.
Figure 5. Series computed tomography (CT) scans in 29-year-old man with COVID-19 pneumonia. (A) CT scan obtained on illness day 17 shows ground-glass opacity combined with partial consolidation. (B) CT scan obtained at month 2 shows that the lesion had been absorbed. 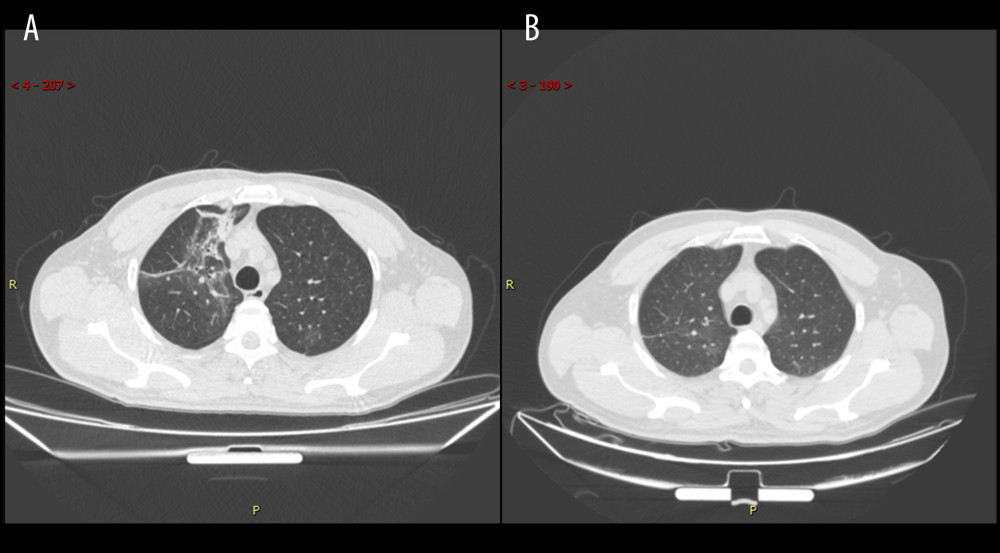 Figure 6. Series computed tomography (CT) scans in 48-year-old man with COVID-19 pneumonia. (A) CT scan obtained on illness day 3 shows mixed pattern (with ground-glass opacity, reticular pattern, and consolidation. (B) CT scan obtained at month 2 shows the obvious absorption of abnormalities.
Figure 6. Series computed tomography (CT) scans in 48-year-old man with COVID-19 pneumonia. (A) CT scan obtained on illness day 3 shows mixed pattern (with ground-glass opacity, reticular pattern, and consolidation. (B) CT scan obtained at month 2 shows the obvious absorption of abnormalities. Tables
Table 1. Comparison of demographic and clinical characteristics between patients with moderate and severe COVID-19 pneumonia.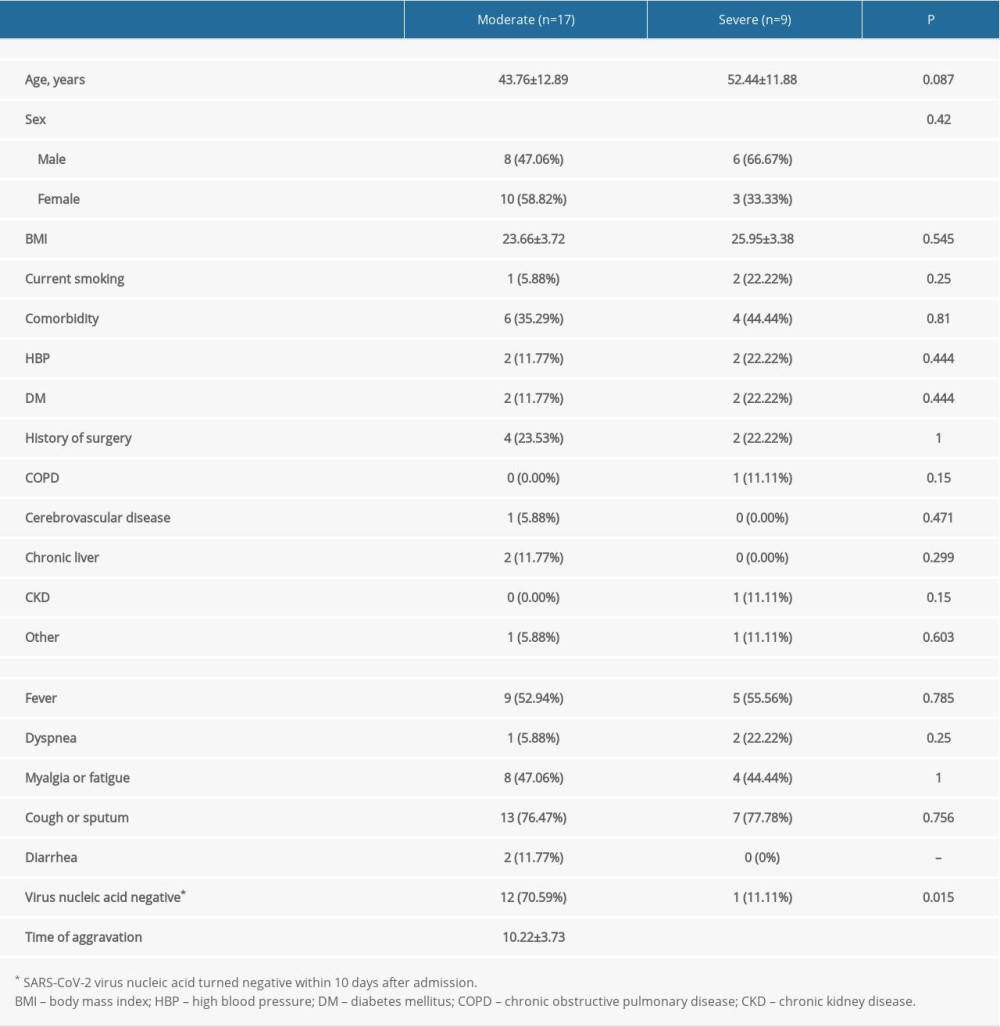 Table 2. Comparison of laboratory findings between patients with moderate and severe COVID-19 pneumonia.
Table 2. Comparison of laboratory findings between patients with moderate and severe COVID-19 pneumonia.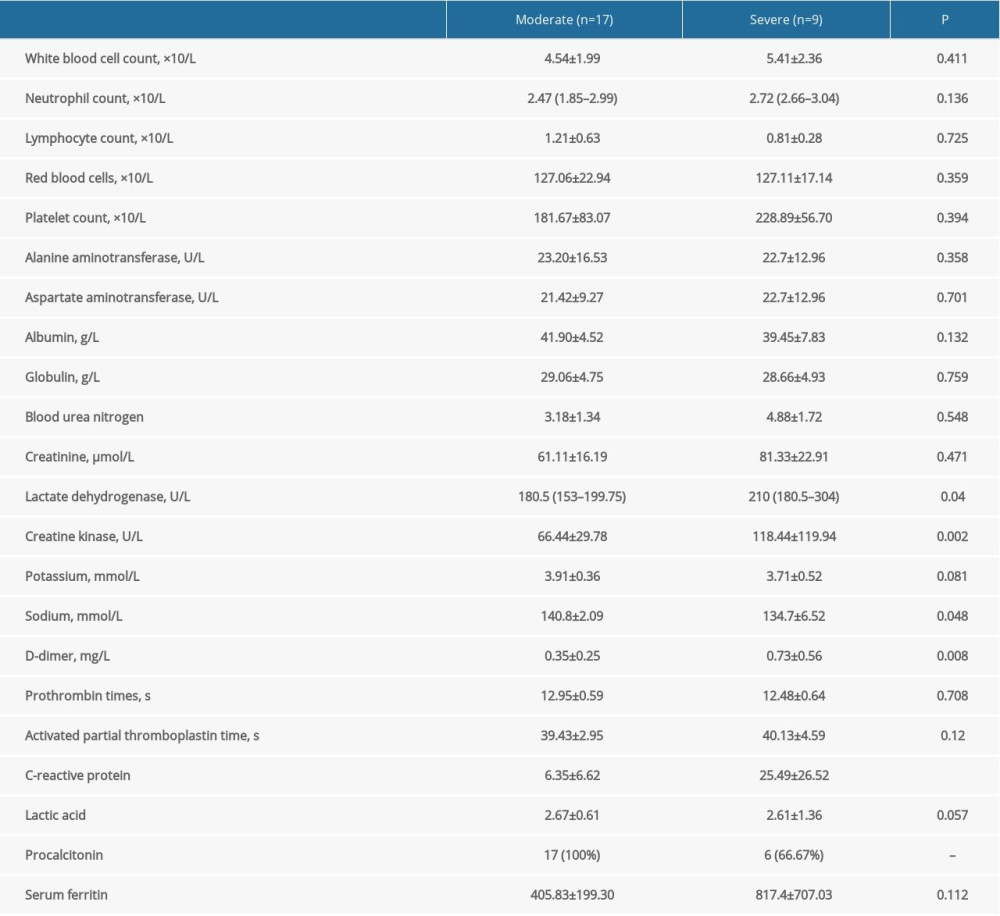 Table 3. Comparison of treatment and prognosis between patients with moderate and severe COVID-19 pneumonia.
Table 3. Comparison of treatment and prognosis between patients with moderate and severe COVID-19 pneumonia.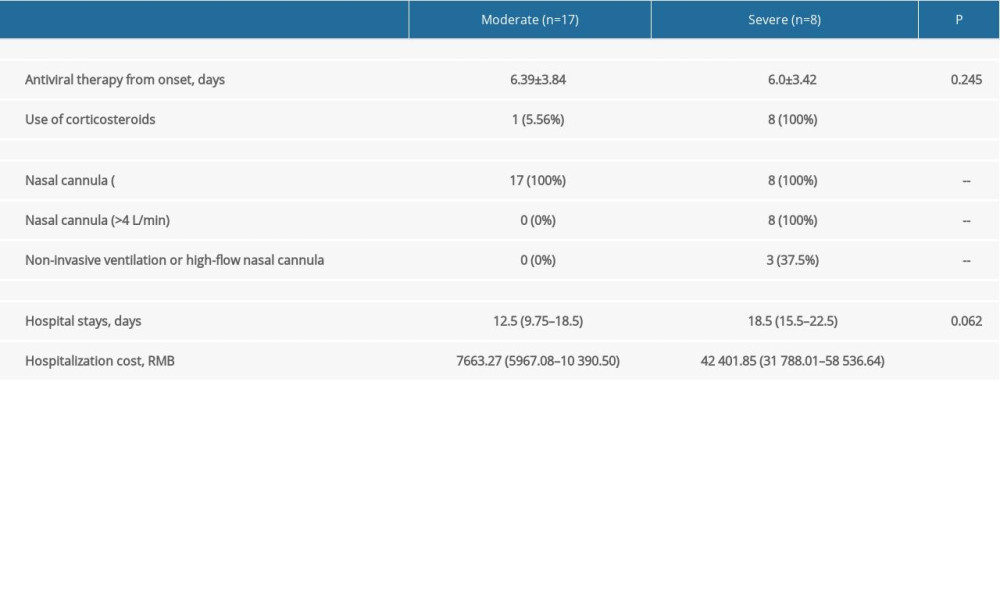 Table 4. Longitudinal lung changes in the computed tomography features in patients with moderate and severe COVID-19 pneumonia.
Table 4. Longitudinal lung changes in the computed tomography features in patients with moderate and severe COVID-19 pneumonia.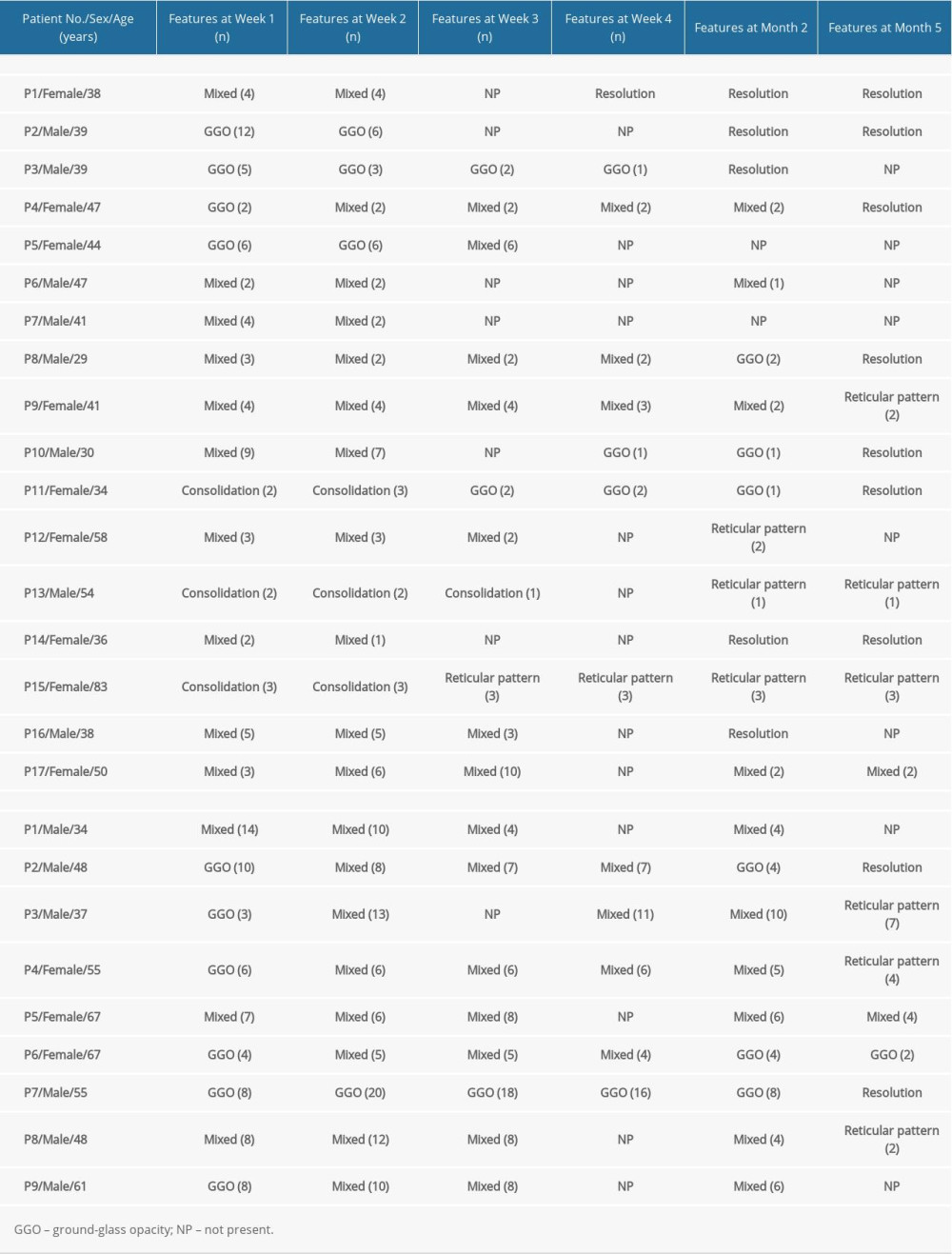 Table 5. Computed tomography characteristics and scores in patients with moderate COVID-19 pneumonia.
Table 5. Computed tomography characteristics and scores in patients with moderate COVID-19 pneumonia. Table 6. Computed tomography characteristics and scores in patients with severe COVID-19 pneumonia.
Table 6. Computed tomography characteristics and scores in patients with severe COVID-19 pneumonia.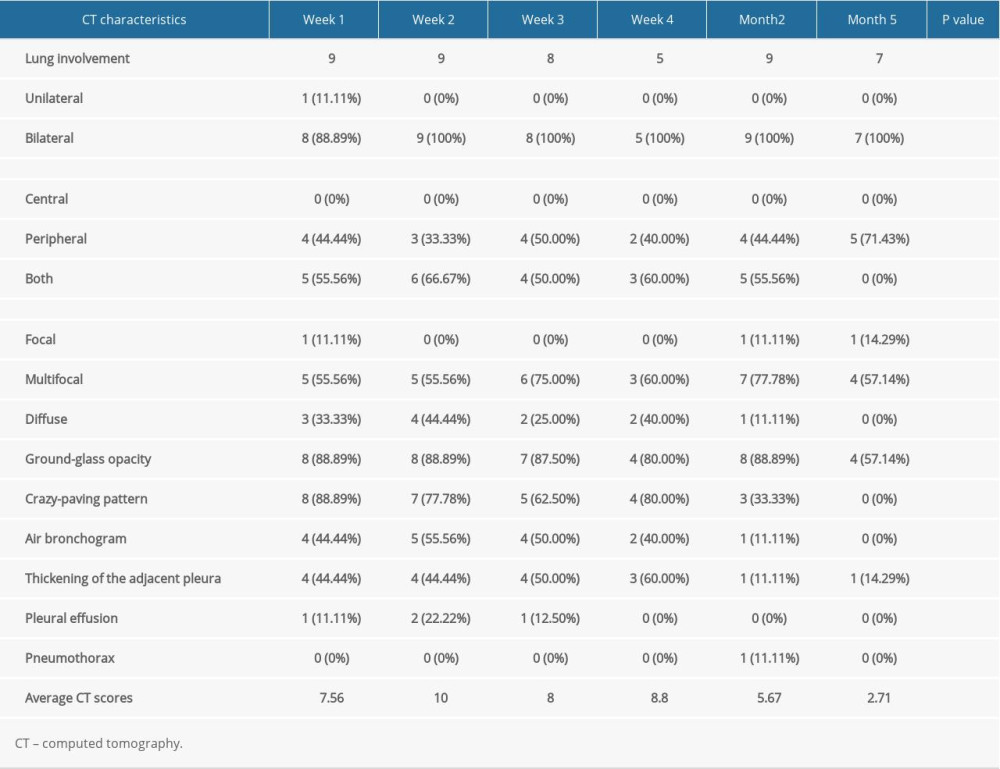
References
1. World Health Organization, 2021 Online. Available from: https://www.who.int/publications/m/item/weekly-epidemiological-update-on-covid-19---24-august-2021
2. Zhou B, Zhao W, Feng R, The pathological autopsy of coronavirus disease 2019 (COVID-2019) in China: A review: Pathog Dis, 2020; 78; ftaa026
3. Riederer P, Ter Meulen V, Coronaviruses: A challenge of today and a call for extended human postmortem brain analyses: J Neural Transm (Vienna), 2020; 127; 1217-28
4. Dhakal BP, Sweitzer NK, Indik JH, SARS-CoV-2 Infection and cardiovascular disease: COVID-19 heart: Heart Lung Circ, 2020; 29; 973-87
5. Nasr SH, Alexander MP, Cornell LD, Kidney biopsy findings in patients with COVID-19, kidney injury, and proteinuria: Am J Kidney Dis, 2021; 77; 465-68
6. Das KM, Lee EY, Singh R, Follow-up chest radiographic findings in patients with MERS-CoV after recovery: Indian J Radiol Imaging, 2017; 27; 342-49
7. Chan KS, Zheng JP, Mok YW, SARS: prognosis, outcome and sequelae: Respirology, 2003; 8(Suppl); S36-40
8. Wang Y, Dong C, Hu Y, Temporal changes of CT findings in 90 patients with COVID-19 pneumonia: A longitudinal study: Radiology, 2020; 296; E55-64
9. An J, Liao X, Xiao T, Clinical characteristics of recovered COVID-19 patients with re-detectable positive RNA test: Ann Transl Med, 2020; 8; 1084
10. The State Council of the People’s Republic of China: Notice on Printing and Distributing the New Coronavirus Pneumonia Diagnosis and Treatment Plan (Trial Version 8), 2020 Available from: http://www.gov.cn/zhengce/zhengceku/2020-08/19/content_5535757.htm
11. Ooi GC, Khong PL, Muller NL, Severe acute respiratory syndrome: Temporal lung changes at thin-section CT in 30 patients: Radiology, 2004; 230; 836-44
12. Lee N, Allen Chan KC, Hui DS, Effects of early corticosteroid treatment on plasma SARS-associated Coronavirus RNA concentrations in adult patients: J Clin Virol, 2004; 31; 304-9
13. Lee N, Chan PK, Hui DS, Viral loads and duration of viral shedding in adult patients hospitalized with influenza: J Infect Dis, 2009; 200; 492-500
14. Zhang Y, Cao W, Jiang W, Profile of natural anticoagulant, coagulant factor and anti-phospholipid antibody in critically ill COVID-19 patients: J Thromb Thrombolysis, 2020; 50; 580-86
15. Tang N, Li D, Wang X, Sun Z, Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia: J Thromb Haemost, 2020; 18; 844-47
16. Zhu H, Rhee JW, Cheng P, Cardiovascular complications in patients with COVID-19: Consequences of viral toxicities and host immune response: Curr Cardiol Rep, 2020; 22; 32
17. Group RC, Horby P, Lim WS, Dexamethasone in hospitalized patients with Covid-19: N Engl J Med, 2021; 384; 693-704
18. Han X, Cao Y, Jiang N, Novel coronavirus disease 2019 (COVID-19) pneumonia progression course in 17 discharged patients: comparison of clinical and thin-section computed tomography features during recovery: Clin Infect Dis, 2020; 71; 723-31
19. Guan CS, Wei LG, Xie RM, CT findings of COVID-19 in follow-up: Comparison between progression and recovery: Diagn Interv Radiol, 2020; 26; 301-7
20. Yang X, Yu Y, Xu J, Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: A single-centered, retrospective, observational study: Lancet Respir Med, 2020; 8; 475-81
21. Feng Y, Ling Y, Bai T, COVID-19 with different severities: A multicenter study of clinical features: Am J Respir Crit Care Med, 2020; 201; 1380-88
22. Tan D, Fu Y, Xu J, Severe adenovirus community-acquired pneumonia in immunocompetent adults: Chest radiographic and CT findings: J Thorac Dis, 2016; 8; 848-54
23. Xie L, Liu Y, Fan B, Dynamic changes of serum SARS-coronavirus IgG, pulmonary function and radiography in patients recovering from SARS after hospital discharge: Respir Res, 2005; 6; 5
Figures
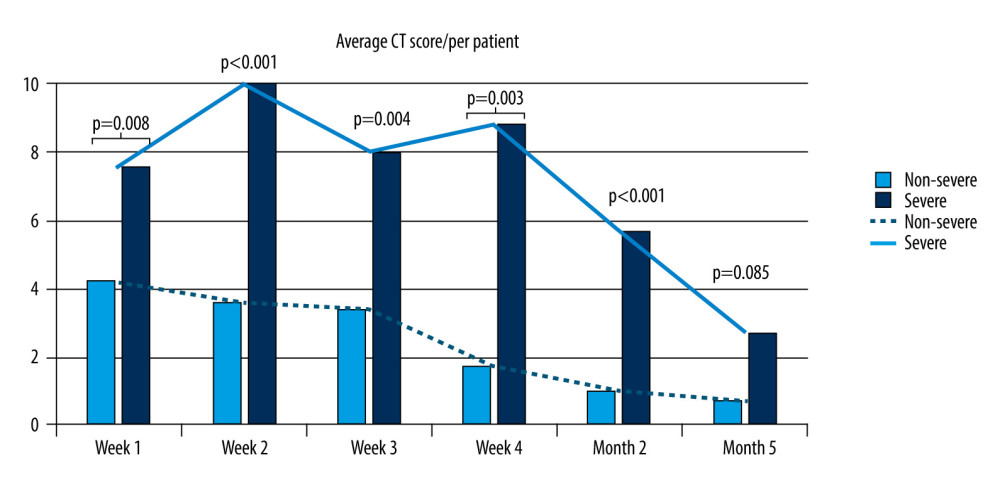 Figure 1. Temporal change in average computed tomography score in moderate and clinically severe groups. Microsoft Excel, Office 365.
Figure 1. Temporal change in average computed tomography score in moderate and clinically severe groups. Microsoft Excel, Office 365.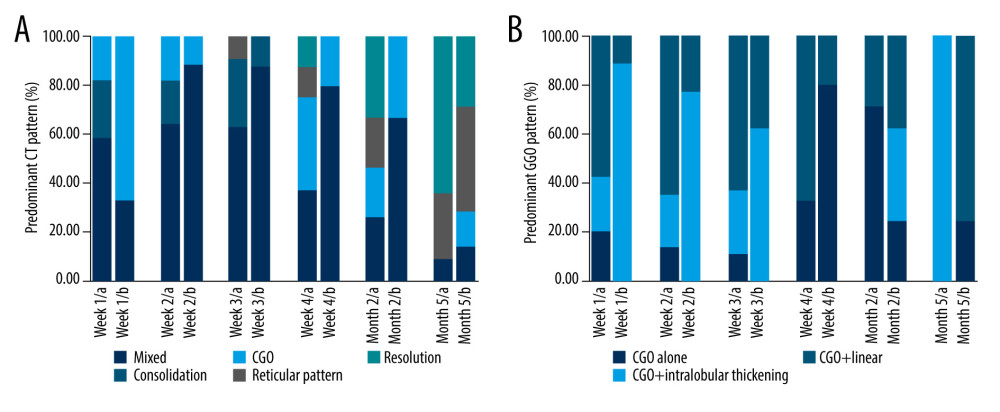 Figure 2. (A, B) Temporal change in the main patterns of computed tomography and ground-glass opacity in moderate and clinically severe groups. Microsoft Excel, Office 365.
Figure 2. (A, B) Temporal change in the main patterns of computed tomography and ground-glass opacity in moderate and clinically severe groups. Microsoft Excel, Office 365.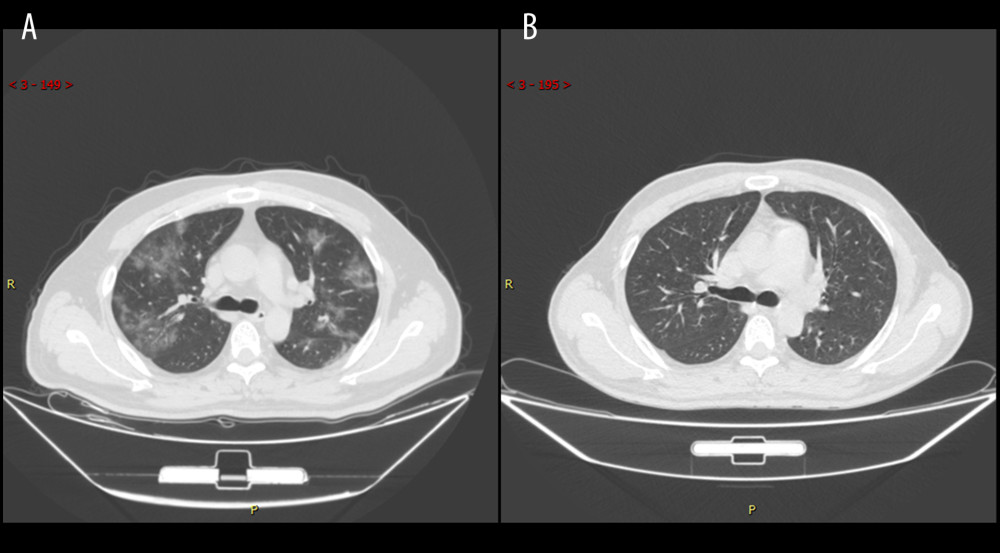 Figure 3. Series computed tomography (CT) scans in 39-year-old man with COVID-19 pneumonia. (A) CT scan obtained on illness day 7 shows diffuse ground-glass opacity. (B) CT scan obtained of illness at month 5 shows that the lesion had been absorbed.
Figure 3. Series computed tomography (CT) scans in 39-year-old man with COVID-19 pneumonia. (A) CT scan obtained on illness day 7 shows diffuse ground-glass opacity. (B) CT scan obtained of illness at month 5 shows that the lesion had been absorbed.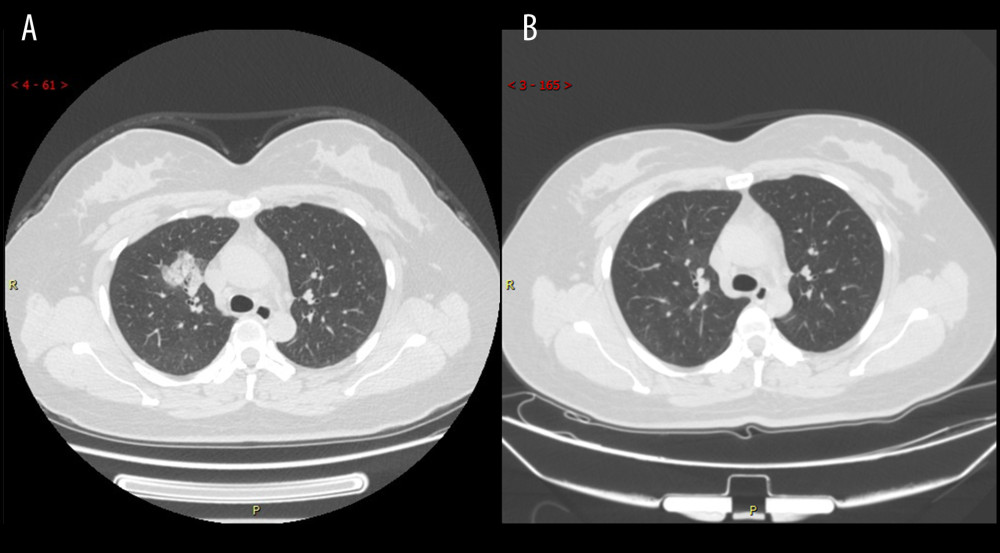 Figure 4. Series computed tomography (CT) scans in a 34-year-old woman with COVID-19 pneumonia. (A) CT scan obtained on illness day 10 shows consolidation in right lung. (B) CT scan obtained at month 2 shows the obvious absorption of abnormalities.
Figure 4. Series computed tomography (CT) scans in a 34-year-old woman with COVID-19 pneumonia. (A) CT scan obtained on illness day 10 shows consolidation in right lung. (B) CT scan obtained at month 2 shows the obvious absorption of abnormalities.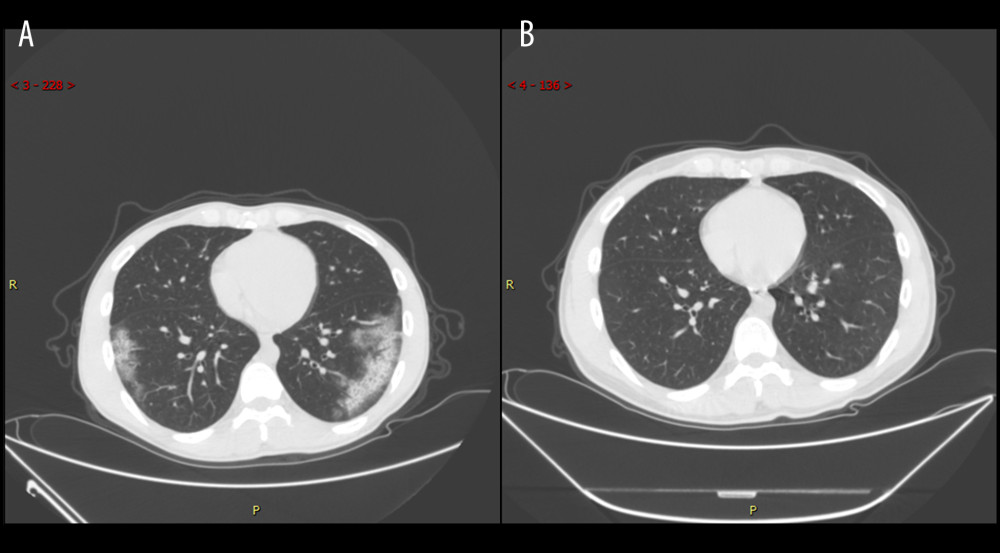 Figure 5. Series computed tomography (CT) scans in 29-year-old man with COVID-19 pneumonia. (A) CT scan obtained on illness day 17 shows ground-glass opacity combined with partial consolidation. (B) CT scan obtained at month 2 shows that the lesion had been absorbed.
Figure 5. Series computed tomography (CT) scans in 29-year-old man with COVID-19 pneumonia. (A) CT scan obtained on illness day 17 shows ground-glass opacity combined with partial consolidation. (B) CT scan obtained at month 2 shows that the lesion had been absorbed.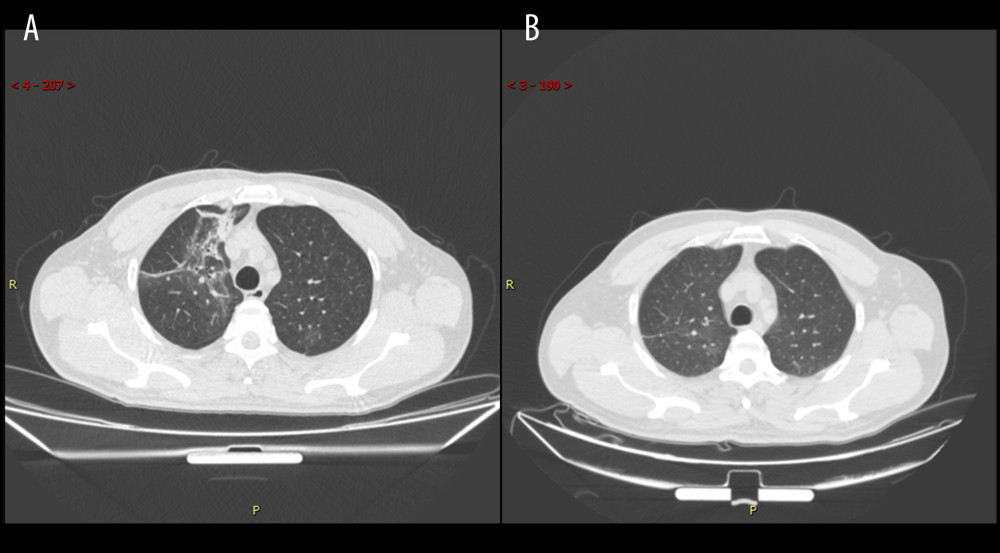 Figure 6. Series computed tomography (CT) scans in 48-year-old man with COVID-19 pneumonia. (A) CT scan obtained on illness day 3 shows mixed pattern (with ground-glass opacity, reticular pattern, and consolidation. (B) CT scan obtained at month 2 shows the obvious absorption of abnormalities.
Figure 6. Series computed tomography (CT) scans in 48-year-old man with COVID-19 pneumonia. (A) CT scan obtained on illness day 3 shows mixed pattern (with ground-glass opacity, reticular pattern, and consolidation. (B) CT scan obtained at month 2 shows the obvious absorption of abnormalities. Tables
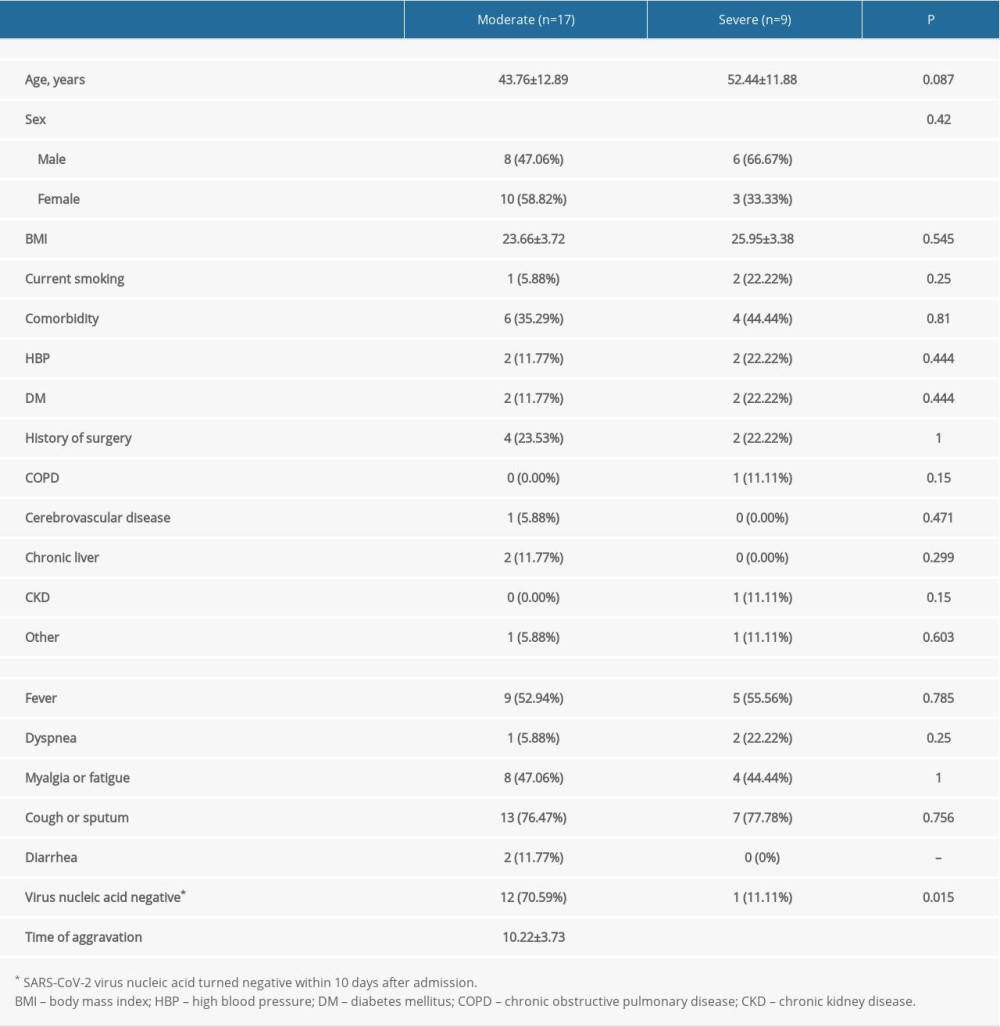 Table 1. Comparison of demographic and clinical characteristics between patients with moderate and severe COVID-19 pneumonia.
Table 1. Comparison of demographic and clinical characteristics between patients with moderate and severe COVID-19 pneumonia.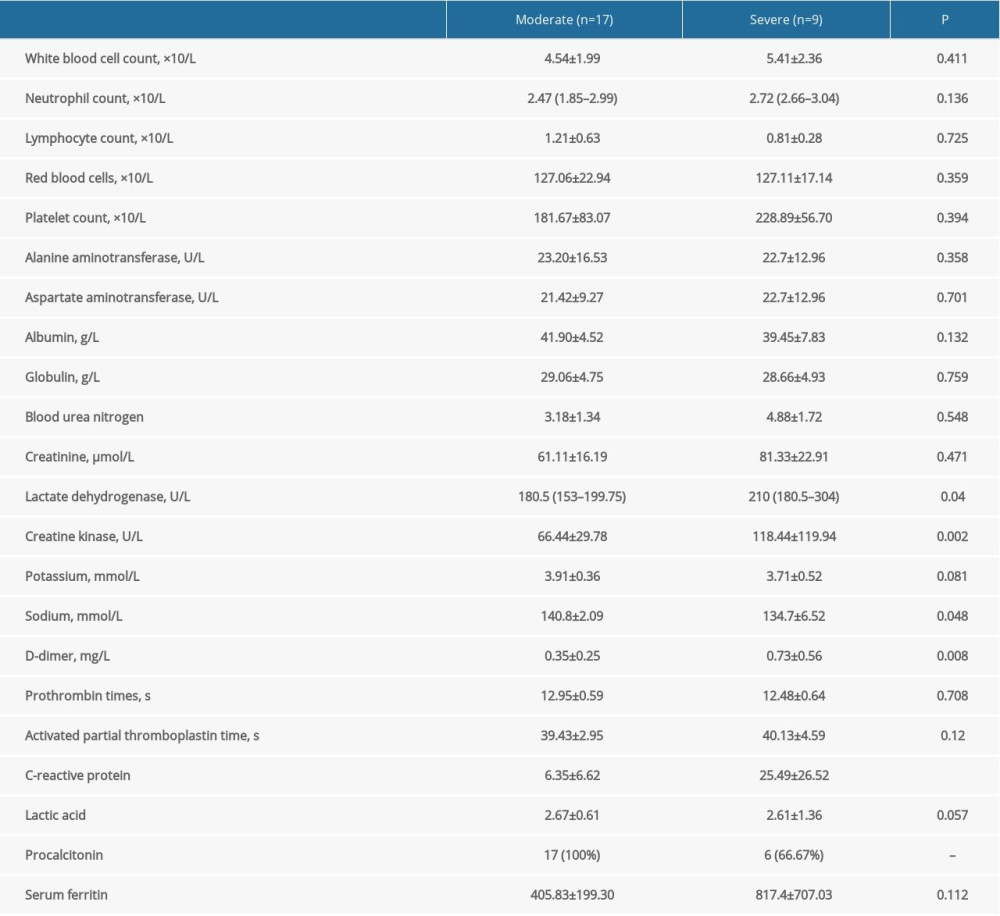 Table 2. Comparison of laboratory findings between patients with moderate and severe COVID-19 pneumonia.
Table 2. Comparison of laboratory findings between patients with moderate and severe COVID-19 pneumonia.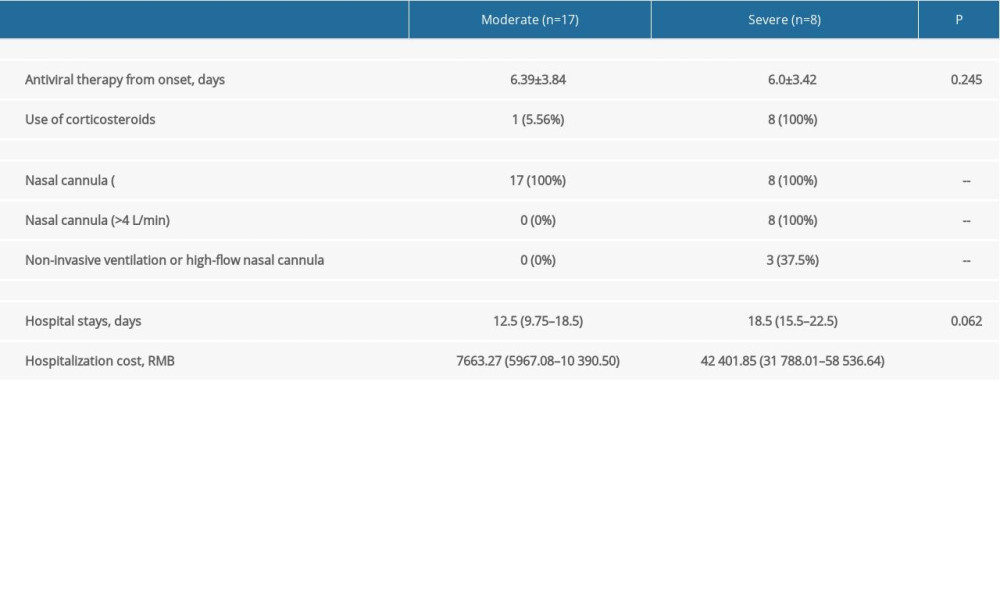 Table 3. Comparison of treatment and prognosis between patients with moderate and severe COVID-19 pneumonia.
Table 3. Comparison of treatment and prognosis between patients with moderate and severe COVID-19 pneumonia.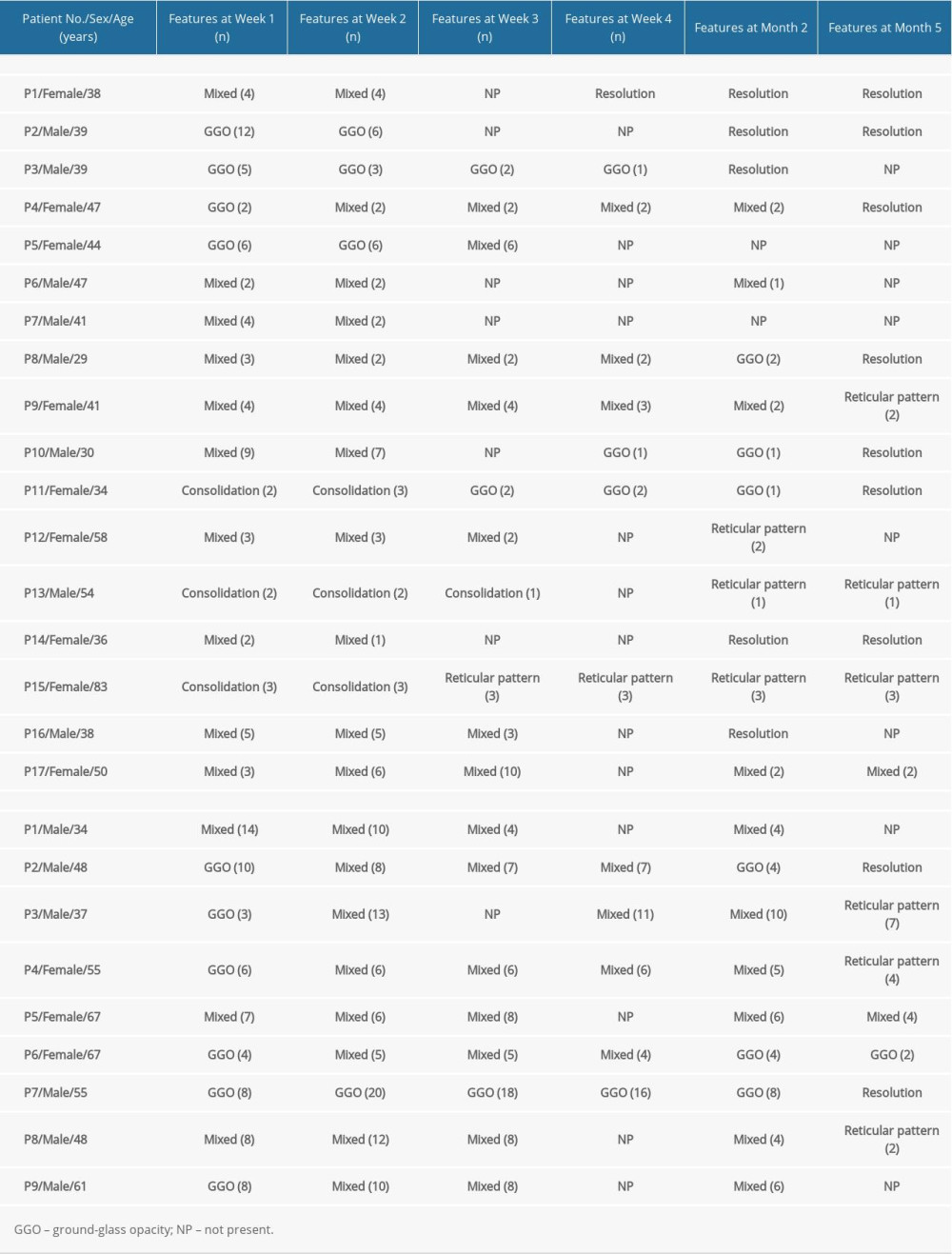 Table 4. Longitudinal lung changes in the computed tomography features in patients with moderate and severe COVID-19 pneumonia.
Table 4. Longitudinal lung changes in the computed tomography features in patients with moderate and severe COVID-19 pneumonia. Table 5. Computed tomography characteristics and scores in patients with moderate COVID-19 pneumonia.
Table 5. Computed tomography characteristics and scores in patients with moderate COVID-19 pneumonia.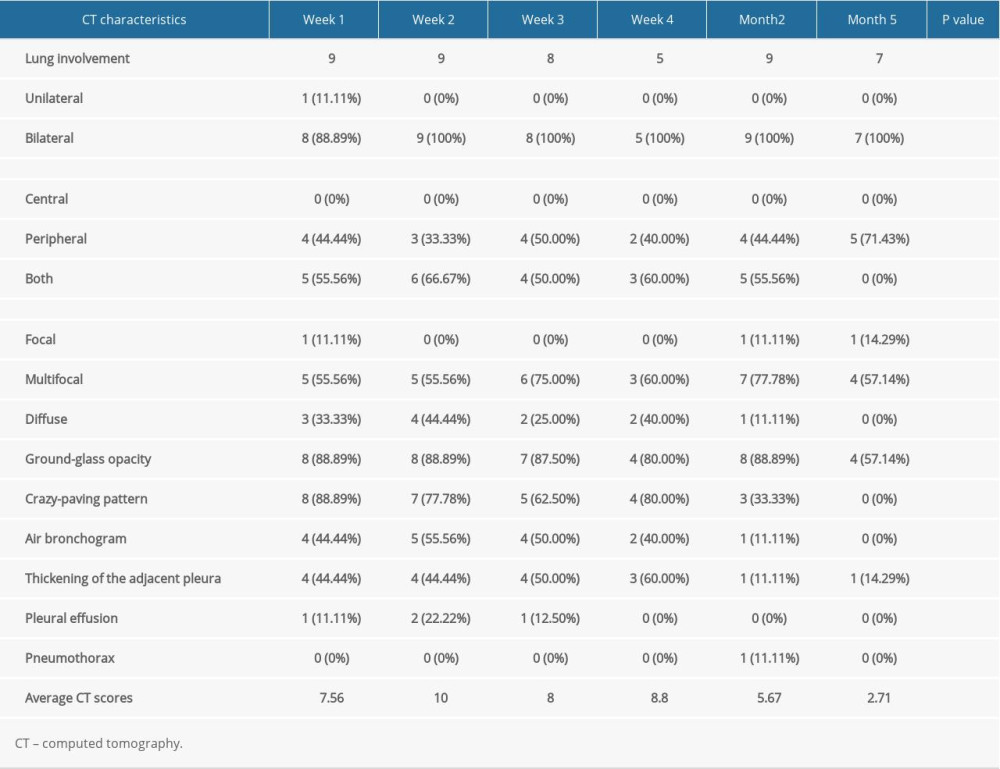 Table 6. Computed tomography characteristics and scores in patients with severe COVID-19 pneumonia.
Table 6. Computed tomography characteristics and scores in patients with severe COVID-19 pneumonia.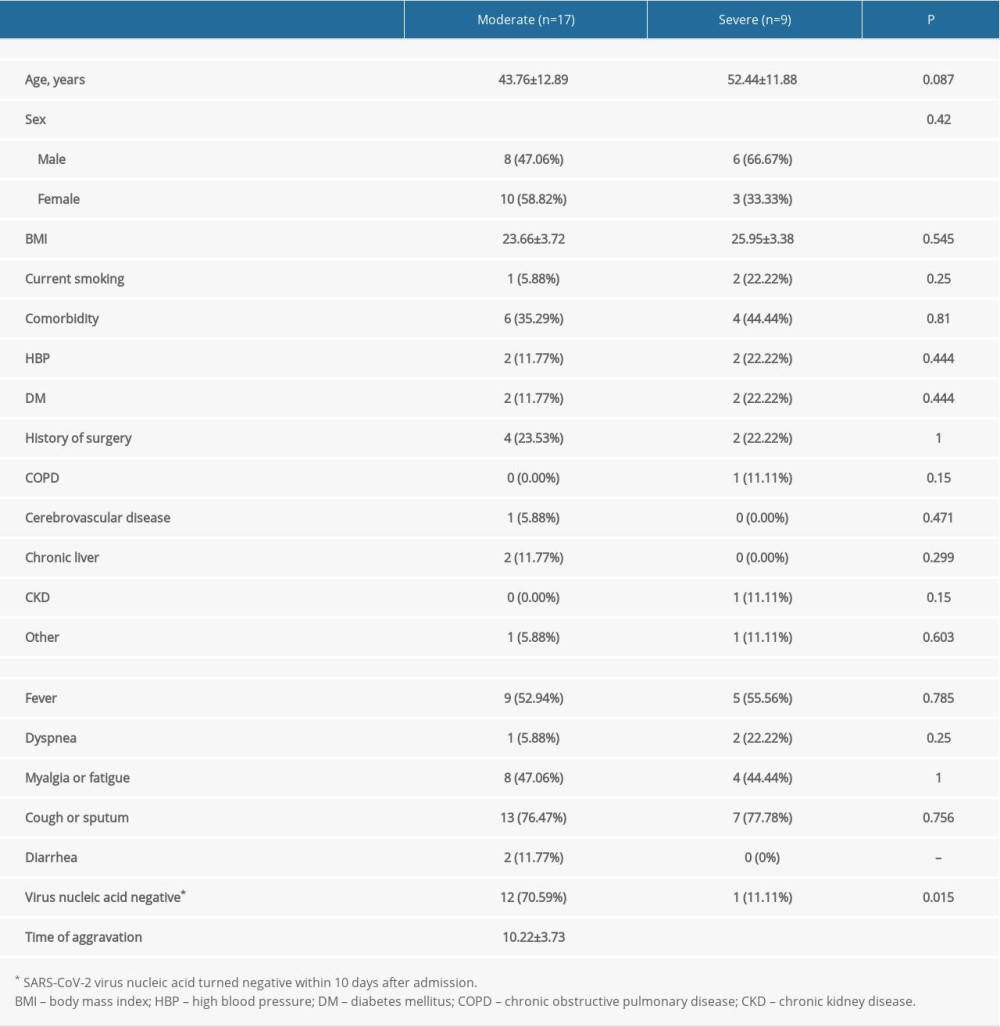 Table 1. Comparison of demographic and clinical characteristics between patients with moderate and severe COVID-19 pneumonia.
Table 1. Comparison of demographic and clinical characteristics between patients with moderate and severe COVID-19 pneumonia.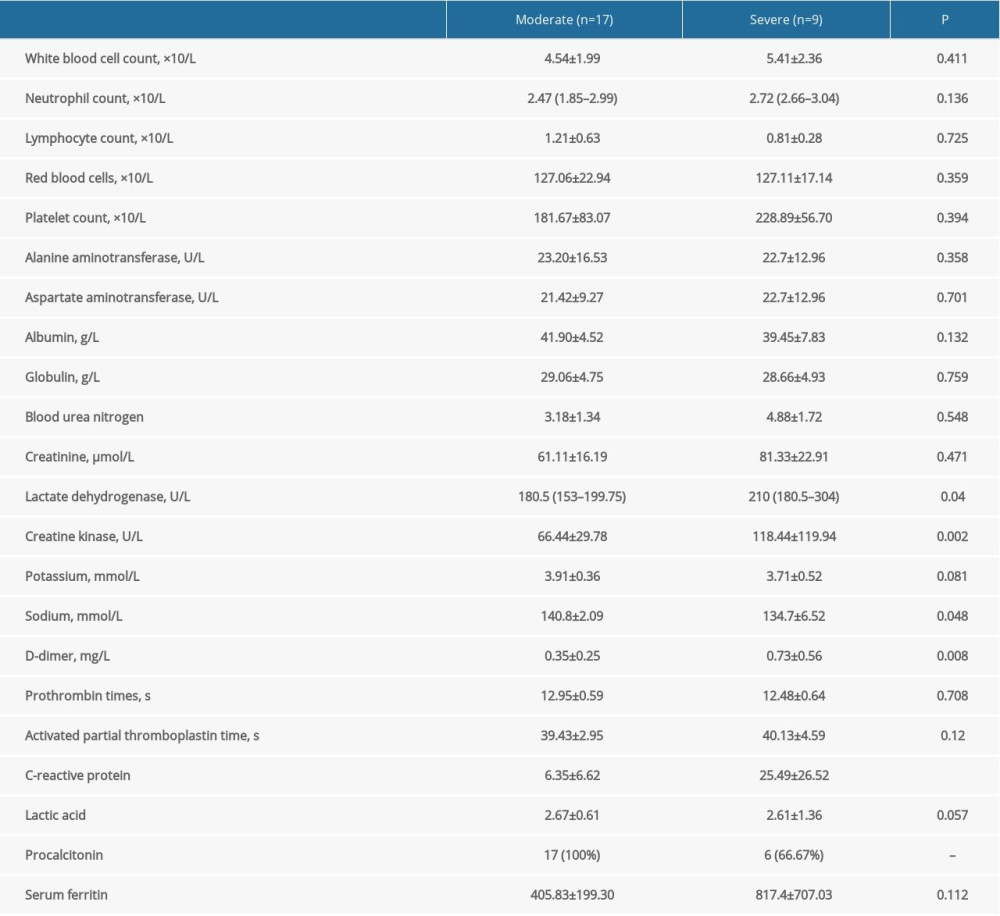 Table 2. Comparison of laboratory findings between patients with moderate and severe COVID-19 pneumonia.
Table 2. Comparison of laboratory findings between patients with moderate and severe COVID-19 pneumonia.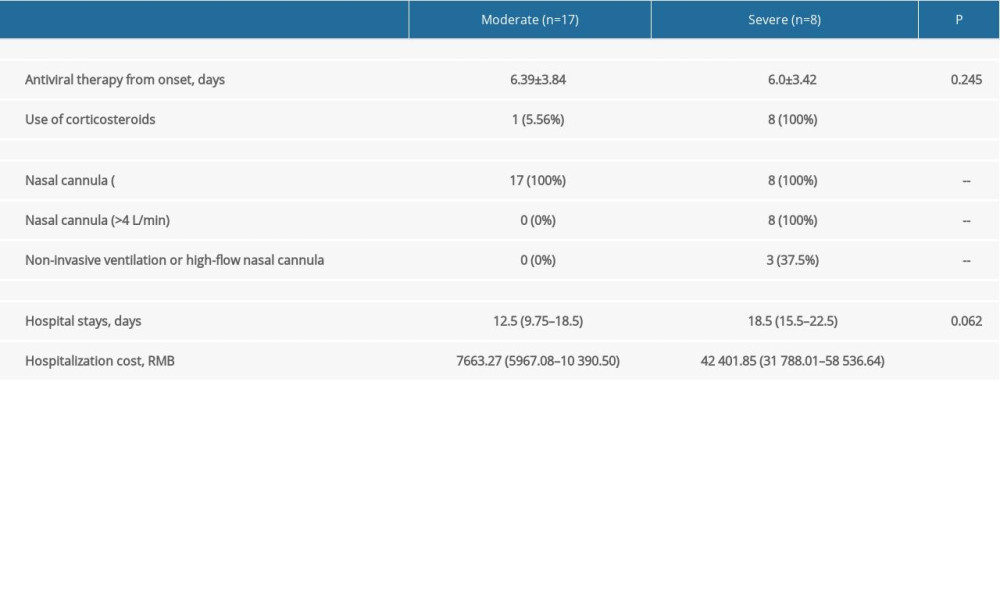 Table 3. Comparison of treatment and prognosis between patients with moderate and severe COVID-19 pneumonia.
Table 3. Comparison of treatment and prognosis between patients with moderate and severe COVID-19 pneumonia.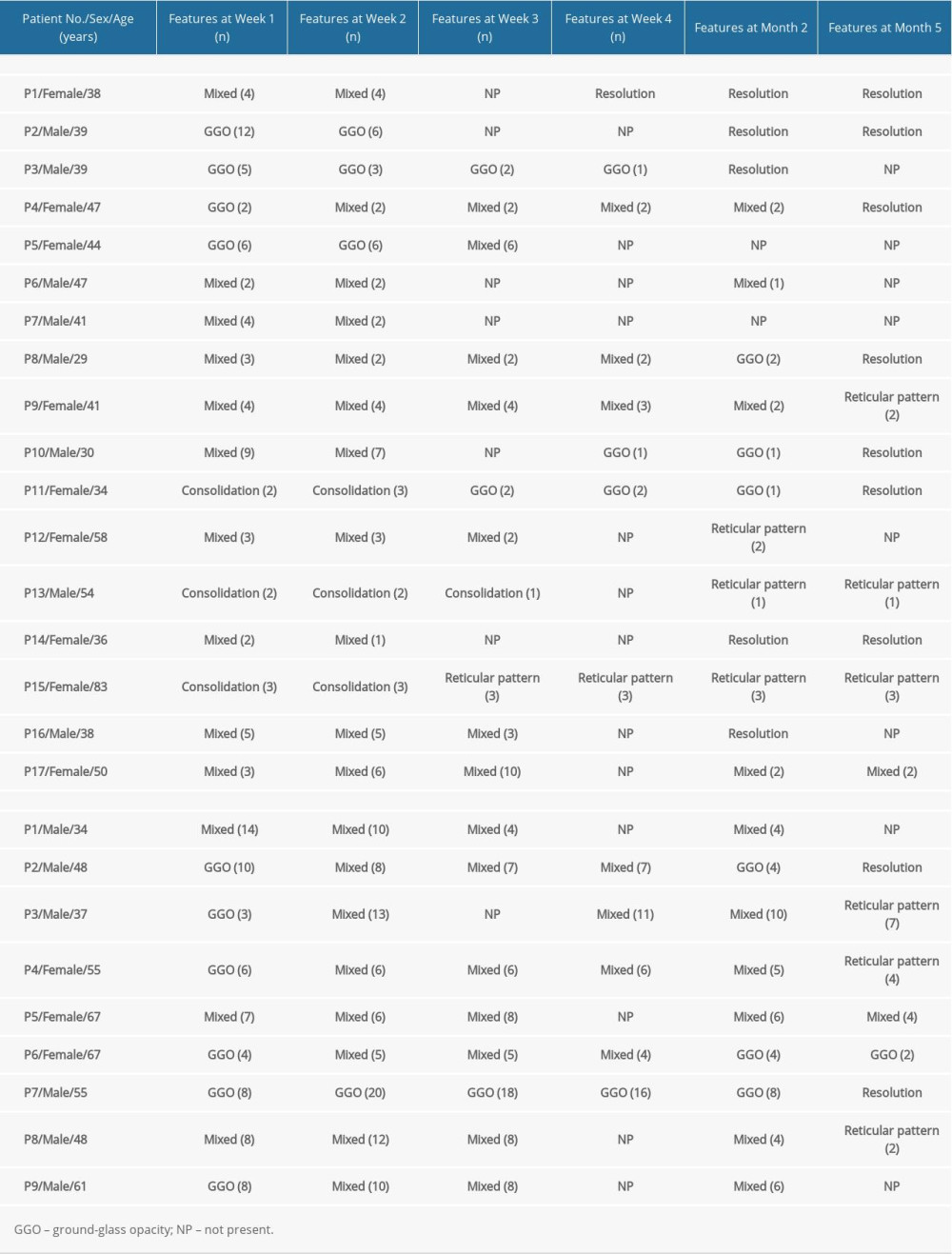 Table 4. Longitudinal lung changes in the computed tomography features in patients with moderate and severe COVID-19 pneumonia.
Table 4. Longitudinal lung changes in the computed tomography features in patients with moderate and severe COVID-19 pneumonia. Table 5. Computed tomography characteristics and scores in patients with moderate COVID-19 pneumonia.
Table 5. Computed tomography characteristics and scores in patients with moderate COVID-19 pneumonia.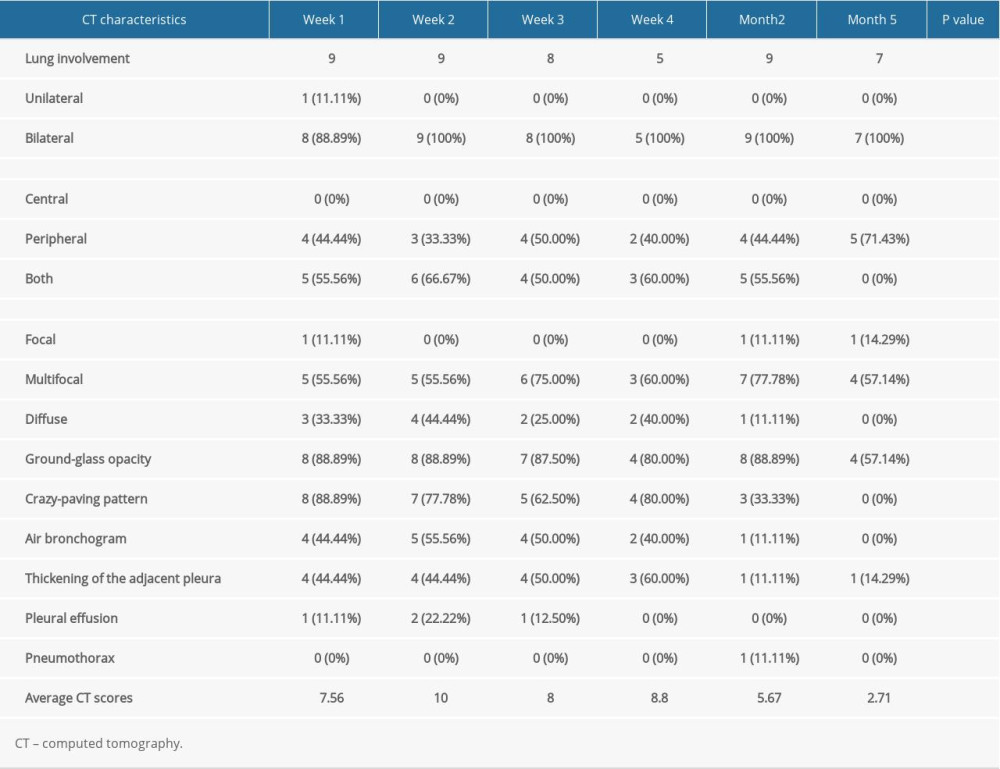 Table 6. Computed tomography characteristics and scores in patients with severe COVID-19 pneumonia.
Table 6. Computed tomography characteristics and scores in patients with severe COVID-19 pneumonia. In Press
18 Apr 2024 : Clinical Research
Comparative Analysis of Open and Closed Sphincterotomy for the Treatment of Chronic Anal Fissure: Safety an...Med Sci Monit In Press; DOI: 10.12659/MSM.944127
08 Mar 2024 : Laboratory Research
Evaluation of Retentive Strength of 50 Endodontically-Treated Single-Rooted Mandibular Second Premolars Res...Med Sci Monit In Press; DOI: 10.12659/MSM.944110
11 Mar 2024 : Clinical Research
Comparison of Effects of Sugammadex and Neostigmine on Postoperative Neuromuscular Blockade Recovery in Pat...Med Sci Monit In Press; DOI: 10.12659/MSM.942773
12 Mar 2024 : Clinical Research
Comparing Neuromuscular Blockade Measurement Between Upper Arm (TOF Cuff®) and Eyelid (TOF Scan®) Using Miv...Med Sci Monit In Press; DOI: 10.12659/MSM.943630
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








