28 November 2021: Clinical Research
Diagnostic Accuracy of Intraoperative Intact Parathyroid Hormone Monitoring for Surgical Outcomes of Secondary Hyperparathyroidism
Yuanyuan Chen1ABCDEF, Bin Liang1ABCDEF, Xiaofeng Dong1F, Tao Huang1B, Tian-qi Liu1AG*DOI: 10.12659/MSM.932556
Med Sci Monit 2021; 27:e932556
Abstract
BACKGROUND: Intraoperative intact parathyroid hormone (IO-iPTH) monitoring has not reached a consensus in predicting surgical outcomes of secondary hyperparathyroidism. Here, we explore the predictive effect of IO-iPTH monitoring on surgical outcomes of secondary hyperparathyroidism as a potentially effective standard.
MATERIAL AND METHODS: We enrolled 119 patients who underwent total parathyroidectomy with autotransplantation from January 2016 to August 2019. Intact parathyroid hormone (iPTH) levels were tested 1 day before surgery (iPTHpre), 10 min after glands resection (iPTH10min), and 1 and 7 days after the operation (iPTHd1, iPTHd7). According to iPTHpre levels, patients were divided into a <2000 pg/ml group and a ≥2000 pg/ml group, and the cutoff values were compared. In patients with successful parathyroidectomy, the value of iPTHpre minus iPTH10min (iPTHdec) and relative-iPTH10min were compared between groups.
RESULTS: Using cutoff values, the predictive criterion was defined as iPTH10min ≤314.5 pg/ml or relative-iPTH10min ≤12.4%. In the iPTHpre ≥2000 pg/ml group, iPTH10min had a higher predictive value (318 pg/ml vs 218 pg/ml) whereas relative-iPTH10min had a lower predictive value (12.1% vs 20.3%). In patients with successful PTX, the iPTHdec value of the iPTHpre ≥2000 pg/ml group was significantly higher than that of the <2000 pg/ml group. Additionally, the relative-iPTH10min was significantly lower in the ≥2000 pg/ml group than in the <2000 pg/ml group.
CONCLUSIONS: An intraoperative predictive criterion of iPTH10min ≤314.5 pg/ml or relative-iPTH10min ≤12.4% is associated with effectively predicting surgical success of secondary hyperparathyroidism. The predictive value is affected by iPTHpre level; therefore, a variable prediction standard based on iPTHpre levels shall be established.
Keywords: Hyperparathyroidism 1, Parathyroid Hormone (1-28), Parathyroidectomy, Predictive Value of Tests, Female, Humans, Hyperparathyroidism, Secondary, Male, Monitoring, Intraoperative, Parathyroid Hormone, Reproducibility of Results
Background
Secondary hyperparathyroidism (SHPT) is a common consequence of chronic kidney disease that requires surgical intervention in patients who do not respond to medical therapy [1]. Surgery in SHPT patients requires parathyroidectomy (PTX), which can be classified into subtotal parathyroidectomy (sPTX) and total parathyroidectomy (tPTX) with or without autotransplantation (AT) [2]. Successful total parathyroidectomy depends on the complete removal of all parathyroid glands; however, complications can occur from uncertainty regarding the number of glands, the existence of ectopic glands, and limitations in preoperative positioning methods. Therefore, an effective intraoperative prediction index is needed to determine when exploratory surgery should be terminated. For the surgical treatment of primary hyperparathyroidism, intraoperative intact parathyroid hormone (IO-iPTH) monitoring has been successfully used to predict surgical efficacy, with several prediction criteria having been established [3–5]. The most commonly used index for the prediction of primary hyperparathyroidism operative success is the Miami criterion [6], a protocol that uses a ≥50% drop in intact parathyroid hormone (iPTH) level from either the highest pre-incision or pre-excision measurement at 10 min after gland excision. However, prediction criteria for SHPT have not yet reached a consensus. The purpose of this retrospective study was to explore the predictive effect of IO-iPTH monitoring on surgical outcomes of SHPT as a potentially effective standard. This study was based on the Standard Reporting for Diagnostic (STARD) studies.
Material and Methods
PATIENTS:
A total of 119 patients (56 males and 63 females) with uremic SHPT who underwent tPTX+AT in our hospital from January 2016 to August 2019 were enrolled in this study. All patients were treated by surgery for the first time. All data were collected retrospectively. This study was approved by the Ethics Committee of the People’s Hospital of Guangxi Zhuang Autonomous Region (ethics approval no. KY-LW-2019-3).
SURGICAL INDICATIONS:
The surgical indications include: (1) serum iPTH >800 pg/ml; (2) with hypercalcemia and/or hyperphosphatemia, medical treatment was tolerated or ineffective; (3) with obvious clinical symptoms such as severe bone pain, itchy skin, or restless legs syndrome; (4) imaging examination revealed at least 1 significantly enlarged parathyroid gland; and (5) had no serious diseases of other important organs.
OPERATIVE PROCEDURE:
Ultrasound and parathyroid scintigraphy (99mTc-MIBI) were used to locate parathyroid glands before the operation. All patients underwent tPTX+AT by open surgery under general anesthesia. All the parathyroid glands explored were completely removed during the operation. The thymus was not removed based on the following considerations: 1) For most patients, removal of the thymus may prolong operative duration and expand the area of surgical resection, which can greatly increase the risk of surgery. Previous reports show that the incidence of ectopic parathyroid glands in the thymus is 10.0~33.0% [7,8], which is relatively low; 2) Each patient was screened with B-ultrasound and parathyroid ECT before surgery, and ectopic parathyroid hyperplasia was not found in the thymus of the patients enrolled in this study; therefore, the thymus is not considered as a routine resection site; 3) For patients whose PTH did not decrease to an ideal level during surgery, an observation time window would be given instead of removing the thymus directly. When the residual or ectopic parathyroid hyperplasia became obvious after surgery, imaging examination was used to position the hyperplasia and then the treatment was performed as needed. According to the intraoperative frozen section results, the parathyroid gland tissue that was closest to normal and pathologically confirmed as diffuse hyperplasia was cut into pieces with a size of l×l×l mm, and 5–20 pieces were transplanted into the forearm between the muscles and sarcolemma. The number of parathyroid glands removed during the operation was confirmed by the postoperative pathological results. All operations were performed by 4 experienced surgeons.
IPTH MONITOR:
As a baseline value, iPTH level was measured in patients 1 day prior to surgery (iPTHpre). The IO-iPTH level was tested at 10 min after the last explored parathyroid gland was removed (iPTH10min). The value of iPTH10min/iPTHpre (relative-iPTH10min) was then calculated and recorded. Postoperative iPTH level was finally determined on the 1st and 7th day after surgery (iPTHd1, iPTHd7). Blood samples were drawn from the peripheral vein, and testing of serum iPTH levels was performed using a Beckman-Coulter UniCel Dxl 800 system with a normal range of 12–88 pg/ml. Generally, quality control in the laboratory was daily performed by using the control sample, and the patient samples were tested only when indoor quality control was completed. In addition, inter-room quality assessments and quality control comparisons between laboratories were conducted annually 2 to 3 times to ensure the accuracy and comparability of the test results.
DEFINITION OF SUCCESSFUL PTX:
Previous studies have shown that an iPTH level <60 pg/ml (as a normal upper value) on the first postoperative day is a good predictor of surgical success [9,10]. We extended the observation period to 1 week after the operation, and we then used iPTHd1 and iPTHd7 levels as predictors associated with successful PTX. After considering the normal value range of our iPTH detection method, we adopted the following criterion for prediction of successful PTX: if both iPTHd1 and iPTHd7 levels were <88 pg/ml, the operation was considered successful; patients whose iPTHd1 or iPTHd7 levels were 88 pg/ml were followed up for half a year. Persistent SHPT was then determined if iPTH was 300 pg/ml, otherwise, the operation was deemed successful.
HIERARCHICAL ANALYSIS:
All patients were divided into 3 groups based on the number of parathyroid glands removed during the operation: those with <4 glands, 4 glands, and >4 glands. The successful PTX rate was recorded and compared. For analysis, patients were split into 2 groups based on iPTHpre level: <2000 pg/ml and ≥2000 pg/ml. iPTH10min and relative-iPTH10min levels in the 2 groups were then measured and compared for their association with successful PTX. In patients with successful PTX, relative-iPTH10min and the decrease in iPTH level from iPTHpre to iPTH10min (iPTHdec) were also compared between groups.
STATISTICAL ANALYSIS:
All statistical analyses were performed with SPSS software version 26.0 (SPSS, Inc., Chicago, IL). Continuous variables are expressed as mean±SD or median (interquartile range), and were analyzed with an independent samples
Results
PARTICIPANT CHARACTERISTICS:
We included 119 patients (56 males and 63 females) in this retrospective study. The average age was 46.1±10.5 years, and the average time from the first hemodialysis to surgery was 6.0 (4.0 to 9.0) years. The laboratory data before and after the operation are shown in Table 1. The number of patients for whom 2, 3, 4, 5, and 6 parathyroid glands were removed during the operation was 5, 21, 81, 10 and 2, respectively. According to the definition of successful PTX, 97 patients with iPTHd1 and iPTHd7 levels <88 pg/ml were judged to have had a successful operation. Twenty-two patients with iPTHd1 or iPTHd7 levels ≥88 pg/ml were followed up for half a year; 20 of them ultimately exceeded 300 pg/ml during the follow-up period and were judged to have persistent SHPT. The other 2 patients were maintained below 300 pg/ml, and the operation was judged to be successful (Figure 1).
DEFINITION OF IO-IPTH PREDICTIVE CRITERION:
By ROC analysis, the best predictive value of iPTH10min for determining persistent SHPT was 314.5 pg/ml (sensitivity 93.9%, specificity 75.0%) with an area under the curve (AUC) of 0.880. Similarly, using a relative-iPTH10min of 12.4% (sensitivity 90.0%, specificity 90.9%) gave an AUC of 0.993 (Figure 2). Taken together, these results suggest that both iPTH10min ≤314.5 pg/ml and relative-iPTH10min ≤12.4% can effectively predict successful PTX. To improve the detection rate of successful PTX and avoid unnecessary surgical exploration, we paralleled the 2 indicators and used a predictive criterion of iPTH10min ≤314.5 pg/ml or relative iPTH10min ≤12.4%. With this paralleled criterion, 99 of the 119 patients met iPTH10min ≤314.5 pg/ml, an additional 3 of the remaining 20 patients met relative-iPTH10min ≤12.4%, and 17 patients did not meet either criterion (Figure 3).
DIAGNOSTIC ACCURACY OF IO-IPTH PREDICTIVE CRITERION:
Ninety-seven (TP) of the 102 patients (TP+FP) who were predicted to have had successful PTX by our paralleled IO-iPTH criterion were confirmed to have had a successful surgery. Furthermore, persistent SHPT was confirmed in 15 (TN) of the 17 patients (TN+FN) who were predicted to not benefit from excessive exploratory surgery. Sensitivity, specificity, PPV, NPV, and accuracy were 97.8%, 75%, 95.1%, 88.2%, and 94.1%, respectively, using our paralleled criterion (Table 2). In contrast, using a relative-iPTH10min ≤30% as the standard to evaluate the data in our study, the sensitivity, specificity, PPV, NPV, and accuracy were 100%, 30%, 87.6%, 100%, and 88.2%, respectively (Table 2). These results demonstrate that our paralleled predictive criterion has higher accuracy and specificity in predicting successful PTX.
According to the number of parathyroid glands removed during the operation, patients were divided into a <4-glands group, a 4-glands group, and a >4-glands group. The rate of successful PTX in each group was 57.7% (15/26), 90.1% (73/81), and 75% (9/12), respectively. By chi-squared analysis, the success rate in the <4-glands group was significantly lower than the 4-glands group (χ2=14.175, P<0.001). The success rate in the >4-glands group was also lower than in the 4-glands group, but the difference was not statistically significant (χ2=1.071, P>0.05) (Table 3). Using our predictive criterion to evaluate the non-4-glands group data, 23 of 26 patients who met the criterion were confirmed to have had successful surgery. Moreover, 11 of 12 patients who did not meet the criterion were confirmed to have persistent SHPT after surgery. Sensitivity, specificity, PPV, NPV, and accuracy using our predictive criterion on the non-4-glands group data were 95.8%, 78.6%, 88.5%, 91.7%, 89.5%, respectively (Table 2).
:
Patients were divided into a ≥2000 pg/ml group (67 patients) and a <2000 pg/ml group (52 patients) based on their iPTHpre levels. By ROC analysis, iPTH10min and relative-iPTH10min effectively predicted surgical outcomes in both the ≥2000 pg/ml group (AUC 0.869 and 0.923) and <2000 pg/ml group (AUC 0.910 and 0.932). However, we observed a higher predictive value of iPTH10min and a lower predictive value of relative-iPTH10min in the ≥2000 pg/ml group. Specifically, in the ≥2000 pg/ml group, the best predictive values of iPTH10min and relative-iPTH10min were 318 pg/ml (sensitivity 83.3%, specificity 91.8%) and 12.1% (sensitivity 83.3%, specificity 96.7%), respectively. In contrast, the best predictive values in the <2000 pg/ml group were 218 pg/ml using iPTH10min (sensitivity 85.7%, specificity 92.1%) and 20.3% using relative-iPTH10min (sensitivity 78.6%, specificity 97.4%) (Figure 4). Finally, we found that for patients with successful PTX, the iPTHdec value in the ≥2000 pg/ml group was significantly higher than that of the <2000 pg/ml group (2515.6±461.9 pg/ml vs 1346.9±319.5 pg/ml, P<0.001). The relative-iPTH10min was also significantly lower in the ≥2000 pg/ml group than in the <2000 pg/ml group (6.8% vs 8.0%, P=0.007) (Table 4).
Discussion
The success of PTX for the treatment of SHPT depends on accurately locating and completely removing all parathyroid tissue, but there is often uncertainty in the number and location of the parathyroid glands. The results of 503 autopsies by Akerström et al [11] showed that while 84% of people had 4 parathyroid glands, 3% had only 3 parathyroid glands and 13% had 5 parathyroid glands. Moreover, ectopic parathyroid was reported to be found in 13.6% to 43.0% of PTX patients with locations in the thymus, tracheoesophageal groove, mediastinum, thyroid parenchyma, retroesophageal, carotid sheath, prevertebral, thyrothymic ligament, and submandibular [7,12,13]. At present, the main methods of parathyroid gland localization before surgery include ultrasound, 99mTc-MIBI, and CT examination, with detection sensitivities of 91.5%, 56.1%, and 84.8%, respectively [14]. While advantages and disadvantages exist for each examination method, no procedure is able to locate all the parathyroid glands very accurately. A prior study found that among 134 patients with PTX, the coincidence rate between the number of parathyroid glands confirmed by preoperative ultrasound and 99mTc-MIBI examination, and postoperative pathology was only 78.9% and 89.3%, respectively [15]. The true coincidence rate is likely lower given situations of intraoperative omission. In our study, 4 parathyroid glands were found during the operation in 68.1% of patients (81), but 21.8% of patients (26) had less and 10.1% of patients (12) had more than 4 parathyroid glands. The PTX success rate for the patients with fewer than 4 glands was 57.7%, significantly lower than the 90.1% success rate of patients with 4 glands. Therefore, there was likely residual parathyroid tissue in the <4-glands group. Interestingly, however, the PTX success rate of the >4-glands group (75%) was also lower than that of 4-glands group (90.1%). We speculate that the reason for this discrepancy is that finding more than 4 parathyroid glands during an operation increases the likelihood of a patient having even more undetected parathyroid tissue. Thus, to shorten operation time and reduce surgical complications for patients with PTX, it is necessary to find an intraoperative predictive index to guide the termination of surgical exploration, particularly for those patients in which fewer than or more than 4 parathyroid glands are found.
Our study showed that the success of PTX is associated with all 3 of our prediction criteria: an iPTH10min level ≤314.5 pg/ml (sensitivity 93.9%, specificity 75.0%, and accuracy 90.8%), a relative-iPTH10min level ≤12.4% (sensitivity 90.9%, specificity 90.0%, and accuracy 90.8%), and the paralleled standard (sensitivity 97.8%, specificity 75%, and accuracy 94.1%). Using a standard relative-iPTH10min ≤12.4% criterion resulted in the highest specificity, while the paralleled standard resulted in the highest sensitivity. By using a standard relative-iPTH10min ≤12.4% criterion, 9 successful PTX patients were predicted to have persistent SHPT and would therefore undergo excessive surgical exploration. However, by using the paralleled standard that combines the 2 indicators, an additional 7 PTX patients were predicted to have persistent PTH and therefore would not benefit from additional exploration. While persistent SHPT still went undetected in 3 additional patients, the paralleled standard would benefit the most patients; therefore, we defined the predictive criterion as iPTH10min ≤314.5 pg/ml or relative-iPTH10min ≤12.4%. In the subgroup analysis, this predictive criterion also showed high prediction accuracy among PTX patients with more or fewer than 4 glands, who were considered to have a higher risk of residual parathyroid glands (sensitivity 95.8%, specificity 78.6%, and accuracy 89.5%).
Although a few studies had previously reported several prediction criteria, there was no consensus on the significance and standard of IO-iPTH monitoring in predicting SHPT surgical outcomes. The study by Ohe et al showed that an IO-iPTH20min decrease of ≥80% compared to iPTHpre predicts 100% of cure in all renal SHPT patients, while a decrease of <70% indicates a missed or hyperfunctioning supernumerary gland and is predictive of surgical failure in 66.6% [16]. In a cohort study, Seehofer et al proposed to use iPTH15min ≤150 pg/ml or iPTH15min/iPTHpre ≤30% as the intraoperative predictive index [17]. Silveira et al reported an iPTH10-15min decay ≥80% of the highest iPTHpre as a predictor of surgical success, showing an accuracy of 86%, a sensitivity of 88%, and specificity of 67% [18]. In a study by Hiramtsu et al [9] a >70% iPTH drop from the baseline to 10 min after PTX could effectively predict the surgical outcomes (sensitivity 97.5%, specificity 52.2%, accuracy 92.9%). However, when we used Hiramatsu’s criterion to evaluate the data in our study, it had low specificity of detection, and successfully detected only 6 of 20 patients who were confirmed to have persistent SHPT after surgery. The sensitivity, specificity, PPV, NPV, and accuracy of Hiramatsu’s criterion with our data were 100%, 30%, 87.6%, 100%, and 88.2%, respectively. Compared to Hiramtsu’s results, our criterion greatly improved the specificity of detection.
Importantly, the above studies reported a significant difference in iPTH levels before surgery. The mean iPTHpre level in our study was 2155.2±733.6 pg/ml, which was much higher than the levels reported in the Seehofer’s and Hiramtsu’s studies (862±46 pg/ml and 451 pg/ml, respectively). The reason for this discrepancy was that our patients usually seek surgical treatment only after unbearable clinical symptoms, and as a result, our patients’ stages were relatively advanced. In a study with a similar baseline iPTH level as ours, a closed predicted value of relative-iPTH10min was reported [19]. Stratified analysis showed that in the group of patients with iPTHpre levels ≥2000 pg/ml, we achieved a higher predictive value for iPTH10min (318 pg/ml vs 218pg/ml) and a lower predictive value for relative-iPTH10min (12.1% vs 20.3%). Taken together with Hiramtsu’s results, this suggests that higher iPTHpre levels are associated with lower predictive values of relative-iPTH10min.
Additionally, it had been previously reported that the rate of IO-iPTH decline was associated with higher baseline iPTH values: shorter half-lives were associated with high baseline iPTH and longer half-lives were associated with low baseline iPTH [20]. For patients with successful PTX in our study, both the absolute value of the decline and the percentage of decline in the iPTHpre ≥2000 pg/ml group were significantly higher than <2000 pg/ml group at 10 min after gland resection. Consequently, preoperative iPTH levels may affect the predictive value of IO-iPTH. We therefore believe that a modified criterion based on preoperative iPTH level should be established. The establishment of this criterion requires the support of a multi-center study and the collection of large amounts of data, particularly that of PTX patients with preoperative iPTH levels less than 1000 pg/ml.
There are some limitations in this study. Firstly, this was a single-center study, and the preoperative average PTH of the SHPT patients enrolled is as high as 2155.2±733.6 pg/ml. The accuracy of our predictive criteria still needs to be further confirmed by multi-center studies. Secondly, for patients with an intraoperative PTH that did not fall to an ideal level, especially when the residual glands were still not removed after re-examination, no further solutions have been proposed. Thymectomy is likely an option that can be used in this situation. Lastly, the accuracy of the predictive value of intraoperative PTH greatly depends on how surgical success is defined. In published reports, the criteria for successful PTX surgery are inconsistent, which may largely compromise the comparability and application scope of the predictive criteria we used in this study. Therefore, it is important to develop a unified criterion of surgical success before setting predictive criteria for intraoperative PTH. This also needs to be further studied and discussed.
Conclusions
IO-iPTH monitoring effectively predicted SHPT surgical outcomes. Using iPTH10min ≤314.5 pg/ml or relative-iPTH10min ≤12.4% was an effective prediction criterion, especially in patients with high baseline iPTH levels. Given that preoperative iPTH levels have an impact on IO-iPTH prediction value, a variable intraoperative prediction standard based on preoperative iPTH levels should be established.
Figures
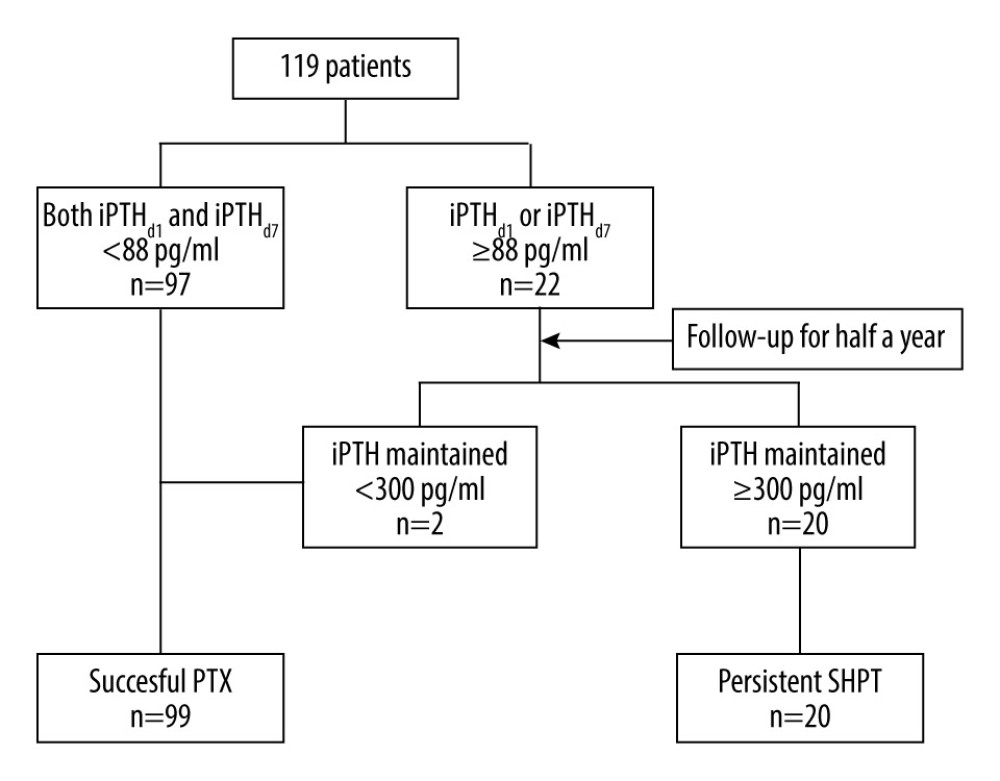 Figure 1. Flow chart for confirming successful parathyroidectomy and persistent secondary hyperparathyroidism.
Figure 1. Flow chart for confirming successful parathyroidectomy and persistent secondary hyperparathyroidism. 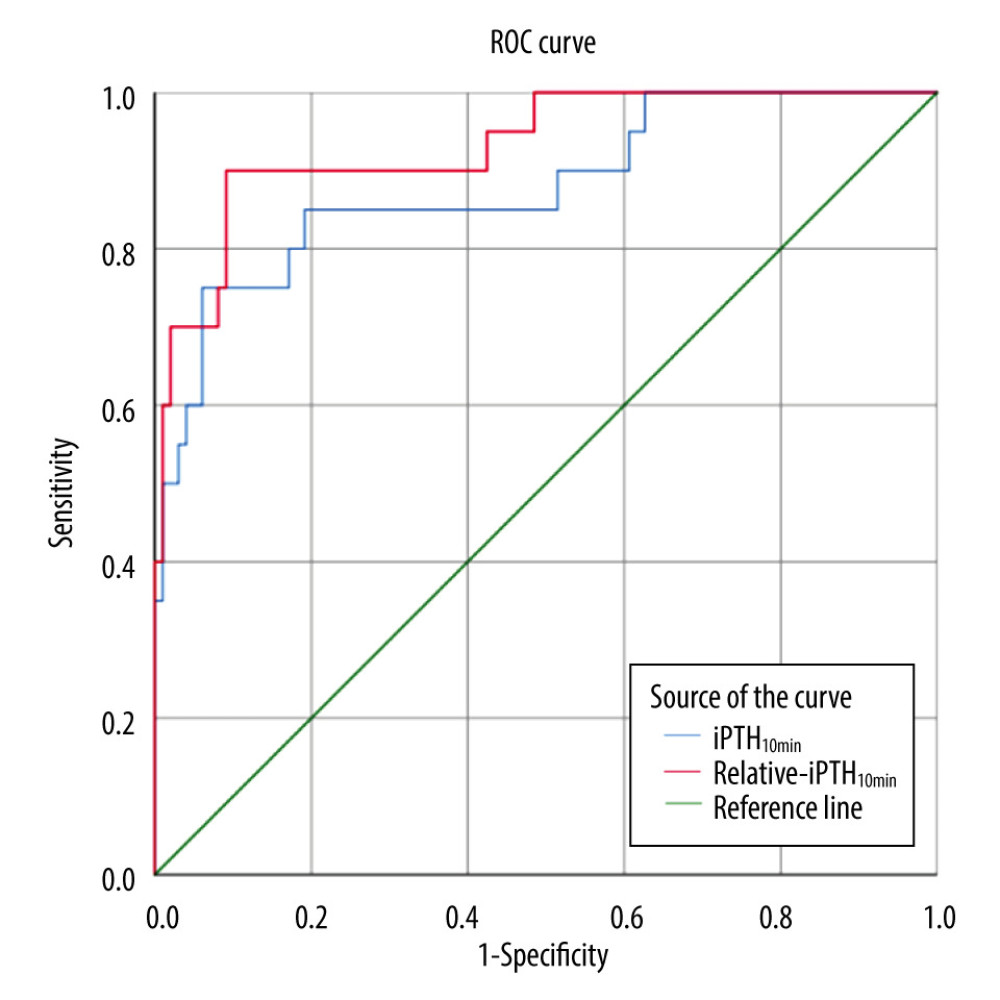 Figure 2. The ROC curves for persistent secondary hyperparathyroidism. The AUC for iPTH10min and relative-iPTH10min was 0.880 and 0.933, respectively. Cutoff values of iPTH10min and relative-iPTH10min were 314.5 pg/ml (sensitivity 75.0%, specificity 93.9%) and 12.4% (sensitivity 90.0%, specificity 90.9%).
Figure 2. The ROC curves for persistent secondary hyperparathyroidism. The AUC for iPTH10min and relative-iPTH10min was 0.880 and 0.933, respectively. Cutoff values of iPTH10min and relative-iPTH10min were 314.5 pg/ml (sensitivity 75.0%, specificity 93.9%) and 12.4% (sensitivity 90.0%, specificity 90.9%). 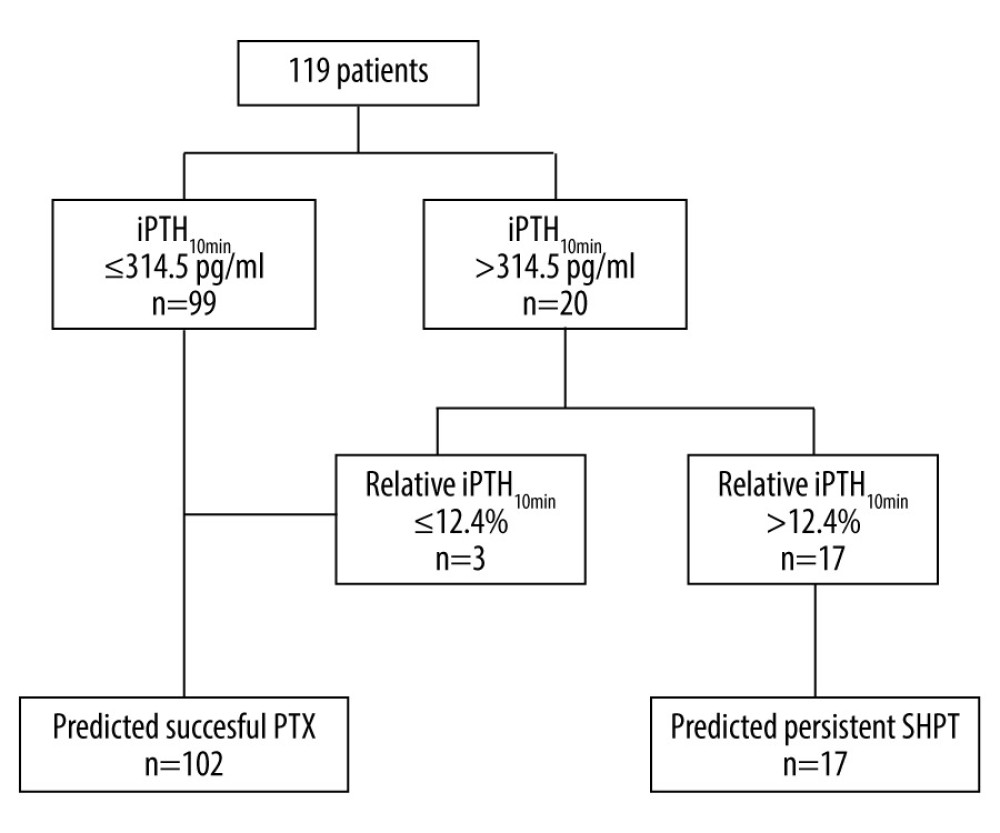 Figure 3. Flow chart using the paralleled criterion to predict surgical outcomes.
Figure 3. Flow chart using the paralleled criterion to predict surgical outcomes. 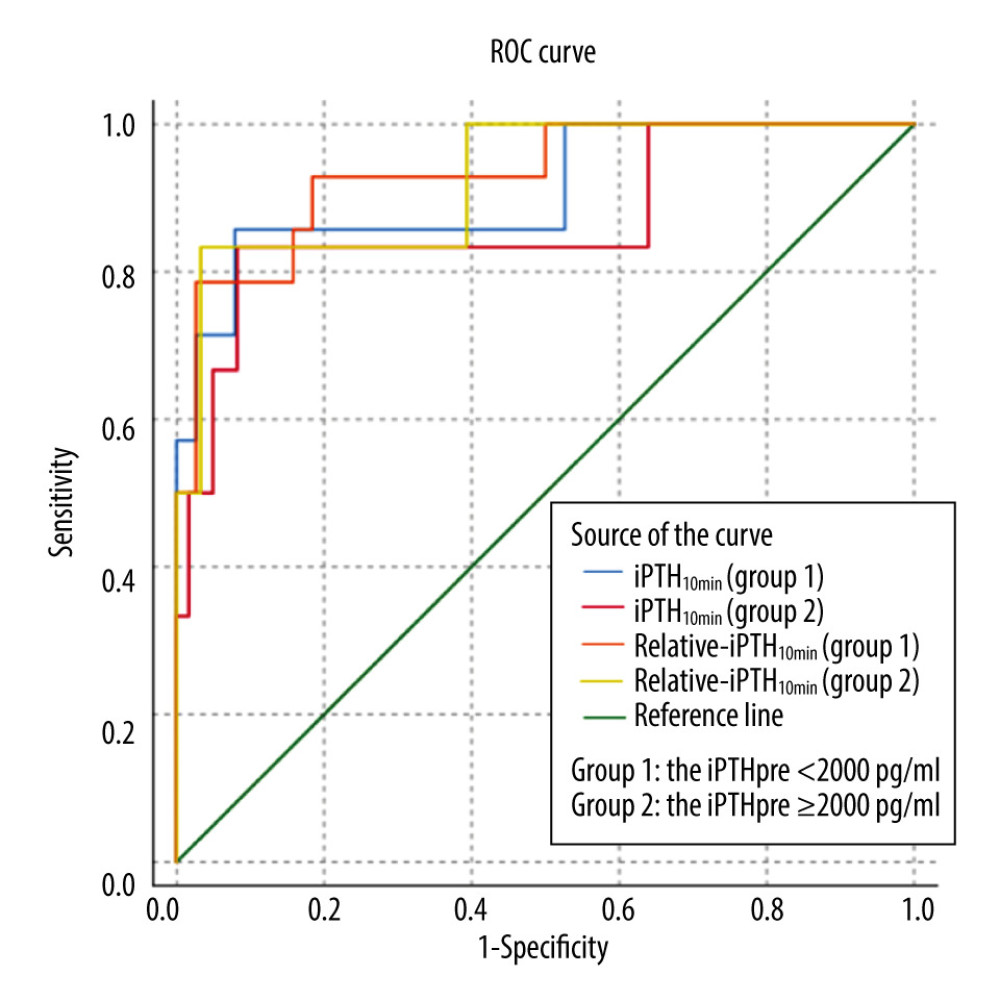 Figure 4. The ROC curves for persistent secondary hyperparathyroidism in the iPTHpre <2000 pg/ml group and the iPTHpre ≥2000 pg/ml group. In the iPTHpre <2000 pg/ml group, the AUC of iPTH10min and relative-iPTH10min were 0.910 and 0.932, respectively; cutoff values of iPTH10min and relative-iPTH10min were 218 pg/ml (sensitivity 85.7%, specificity 92.1%) and 20.3% (sensitivity 78.6%, specificity 97.4%). In the iPTHpre ≥2000 pg/ml group, the AUC of iPTH10min and relative-iPTH10min were 0.869 and 0.923, respectively; cutoff values of iPTH10min and relative-iPTH10min were 318 pg/ml (sensitivity 83.3%, specificity 91.8%) and 12.1% (sensitivity 83.3%, specificity 96.7%).
Figure 4. The ROC curves for persistent secondary hyperparathyroidism in the iPTHpre <2000 pg/ml group and the iPTHpre ≥2000 pg/ml group. In the iPTHpre <2000 pg/ml group, the AUC of iPTH10min and relative-iPTH10min were 0.910 and 0.932, respectively; cutoff values of iPTH10min and relative-iPTH10min were 218 pg/ml (sensitivity 85.7%, specificity 92.1%) and 20.3% (sensitivity 78.6%, specificity 97.4%). In the iPTHpre ≥2000 pg/ml group, the AUC of iPTH10min and relative-iPTH10min were 0.869 and 0.923, respectively; cutoff values of iPTH10min and relative-iPTH10min were 318 pg/ml (sensitivity 83.3%, specificity 91.8%) and 12.1% (sensitivity 83.3%, specificity 96.7%). Tables
Table 1. Laboratory data before and after the operation.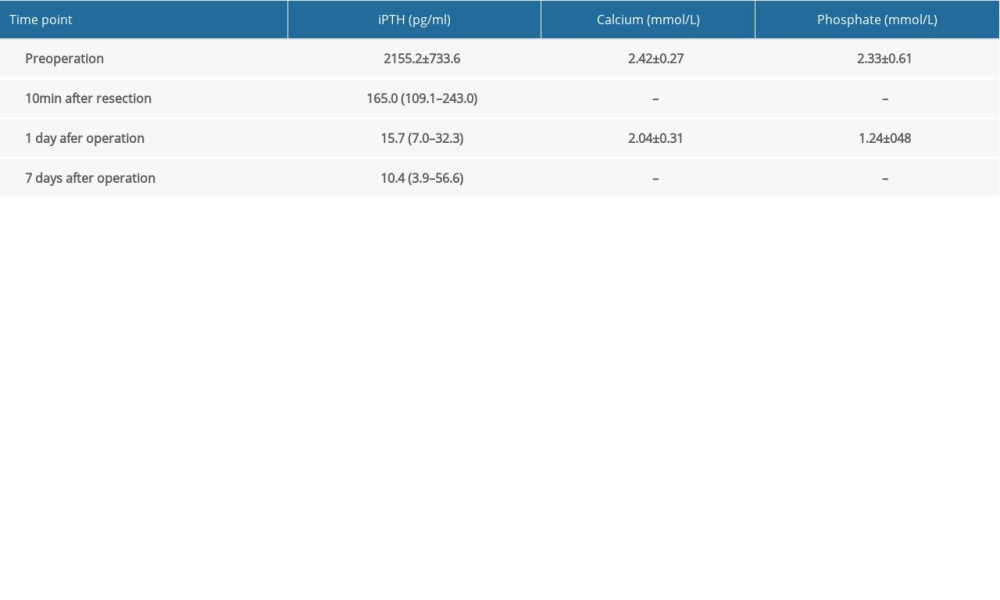 Table 2. Accuracy of different IO-iPTH prediction criteria.
Table 2. Accuracy of different IO-iPTH prediction criteria.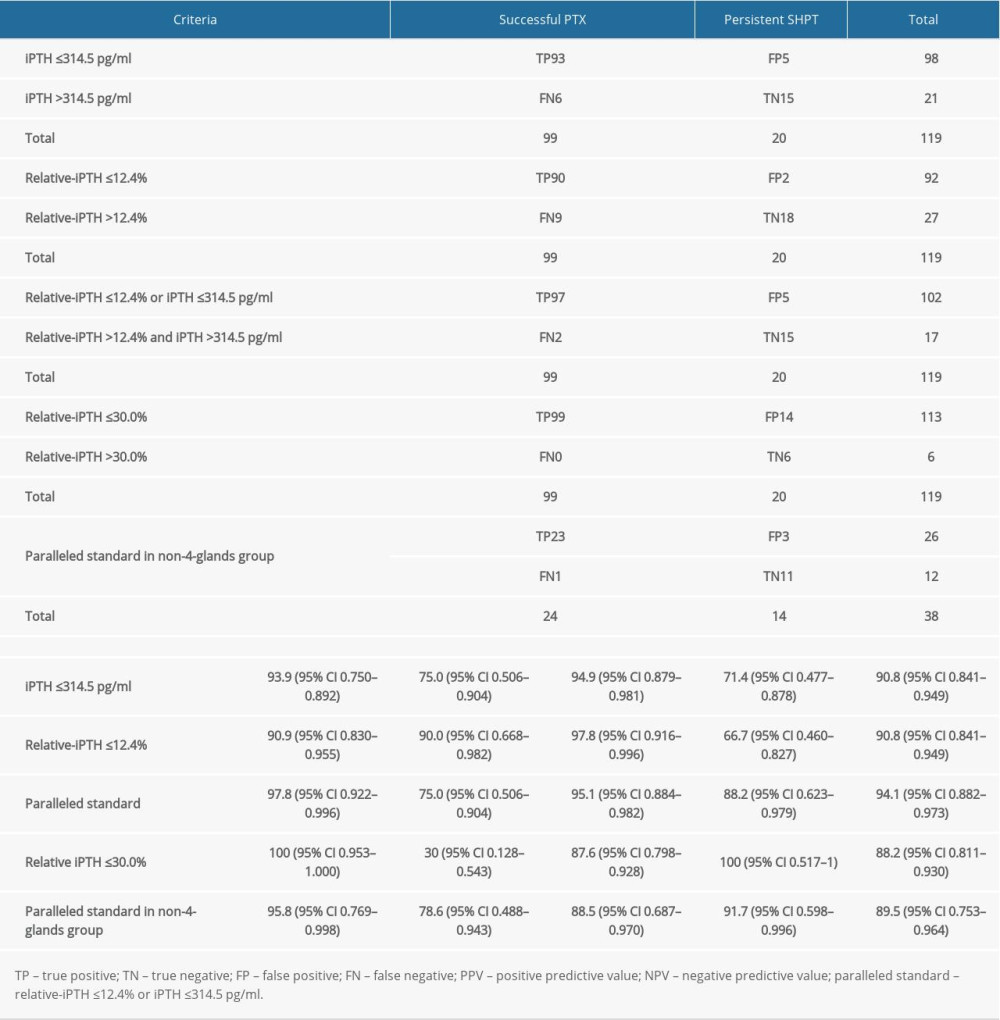 Table 3. Influence of the number of parathyroid glands removed during operation on the successful PTX rate.
Table 3. Influence of the number of parathyroid glands removed during operation on the successful PTX rate.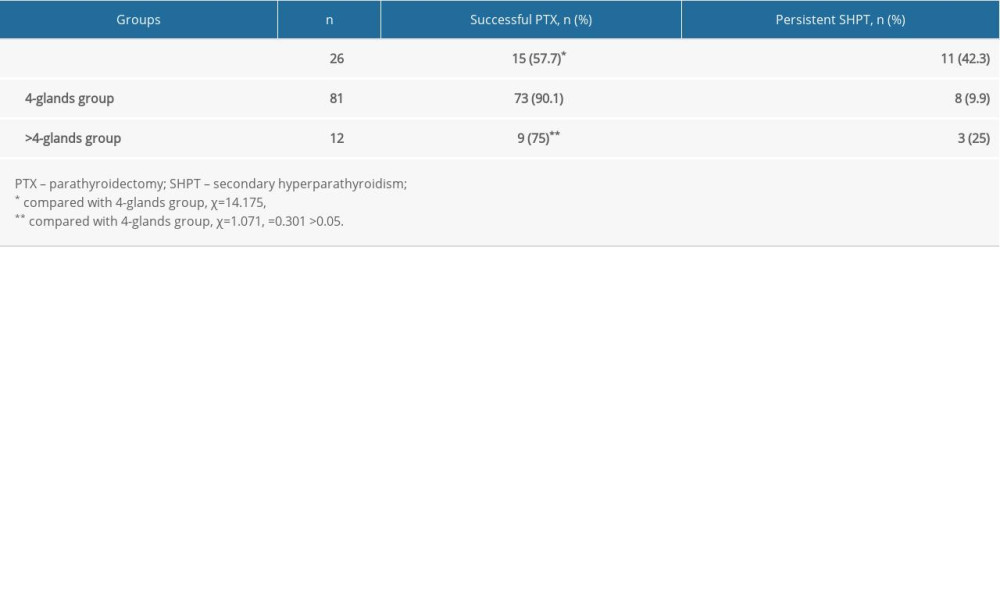 Table 4. The iPTHdec value and relative-iPTH10min in patients with successful PTX.
Table 4. The iPTHdec value and relative-iPTH10min in patients with successful PTX.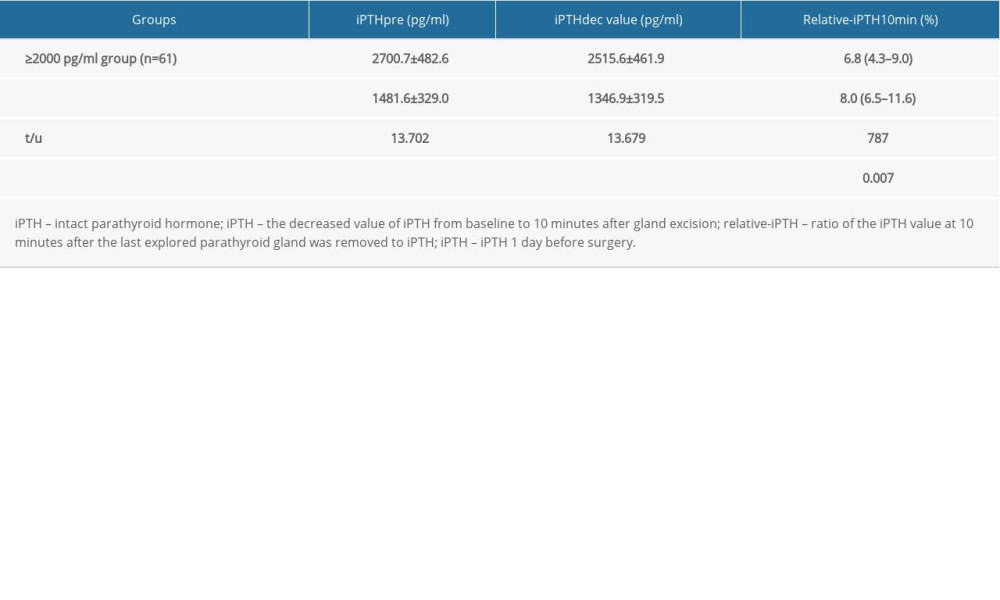
References
1. , K/DOQI clinical practice guidelines for bone metabolism and disease in chronic kidney disease: Am J Kidney Dis, 2003; 42(4 Suppl 3); S1-201
2. Isaksson E, Ivarsson K, Akaberi S, Total versus subtotal parathyroidectomy for secondary hyperparathyroidism: Surgery, 2019; 165(1); 142-50
3. Riss P, Kaczirek K, Heinz G, A “defined baseline” in PTH monitoring increases surgical success in patients with multiple gland disease: Surgery, 2007; 142(3); 398-404
4. Agarwal G, Barakate MS, Robinson B, Intraoperative quick parathyroid hormone versus same-day parathyroid hormone testing for minimally invasive parathyroidectomy: A cost-effectiveness study: Surgery, 2001; 130(6); 963-70
5. Carneiro DM, Solorzano CC, Nader MC, Comparison of intraoperative iPTH assay (QPTH) criteria in guiding parathyroidectomy: Which criterion is the most accurate?: Surgery, 2003; 134(6); 973-79 discussion 979–81
6. Barczynski M, Konturek A, Hubalewska-Dydejczyk A, Evaluation of Halle, Miami, Rome, and Vienna intraoperative iPTH assay criteria in guiding minimally invasive parathyroidectomy: Langenbecks Arch Surg, 2009; 394(5); 843-49
7. Phitayakorn R, McHenry CR, Incidence and location of ectopic abnormal parathyroid glands: Am J Surg, 2006; 191(3); 418-23
8. Welch K, McHenry CR, The role of transcervical thymectomy in patients with hyperparathyroidism: Am J Surg, 2012; 203(3); 292-95 discussion 295–96
9. Hiramitsu T, Tominaga Y, Okada M, A retrospective study of the impact of intraoperative intact parathyroid hormone monitoring during total parathyroidectomy for secondary hyperparathyroidism: STARD study: Medicine, 2015; 94(29); e1213
10. Uslu A, Okut G, Tercan IC, Anatomical distribution and number of parathyroid glands, and parathyroid function, after total parathyroidectomy and bilateral cervical thymectomy: Medicine, 2019; 98(23); e15926
11. Akerstrom G, Malmaeus J, Bergstrom R, Surgical anatomy of human parathyroid glands: Surgery, 1984; 95(1); 14-21
12. Andrade JS, Mangussi-Gomes JP, Rocha LA, Localization of ectopic and supernumerary parathyroid glands in patients with secondary and tertiary hyperparathyroidism: Surgical description and correlation with preoperative ultrasonography and Tc99m-Sestamibi scintigraphy: Braz J Otorhinolaryngol, 2014; 80(1); 29-34
13. Karipineni F, Sahli Z, Somervell H, Are preoperative sestamibi scans useful for identifying ectopic parathyroid glands in patients with expected multigland parathyroid disease?: Surgery, 2018; 163(1); 35-41
14. Lee JB, Kim WY, Lee YM, The role of preoperative ultrasonography, computed tomography, and sestamibi scintigraphy localization in secondary hyperparathyroidism: Ann Surg Treat Res, 2015; 89(6); 300-5
15. Casella C, Galani A, Totaro L, Total parathyroidectomy with subcutaneous parathyroid forearm autotransplantation in the treatment of secondary hyperparathyroidism: A single-center experience: Int J Endocrinol, 2018; 2018; 6065720
16. Ohe MN, Santos RO, Kunii IS, Intraoperative PTH cutoff definition to predict successful parathyroidectomy in secondary and tertiary hyperparathyroidism: Braz J Otorhinolaryngol, 2013; 79(4); 494-99
17. Seehofer D, Rayes N, Klupp J, Predictive value of intact parathyroid hormone measurement during surgery for renal hyperparathyroidism: Langenbecks Arch Surg, 2005; 390(3); 222-29
18. Silveira AA, Brescia MDG, do Nascimento CP, Critical analysis of the intraoperative parathyroid hormone decrease during parathyroidectomy for secondary and tertiary hyperparathyroidism: Surgery, 2020; 168(6); 1079-85
19. Zhang L, Xing C, Shen C, Diagnostic accuracy study of intraoperative and perioperative serum intact PTH level for successful parathyroidectomy in 501 secondary hyperparathyroidism patients: Sci Rep, 2016; 6; 26841
20. Libutti SK, Alexander HR, Bartlett DL, Kinetic analysis of the rapid intraoperative parathyroid hormone assay in patients during operation for hyperparathyroidism: Surgery, 1999; 126(6); 1145-50 discussion 1150–51
Figures
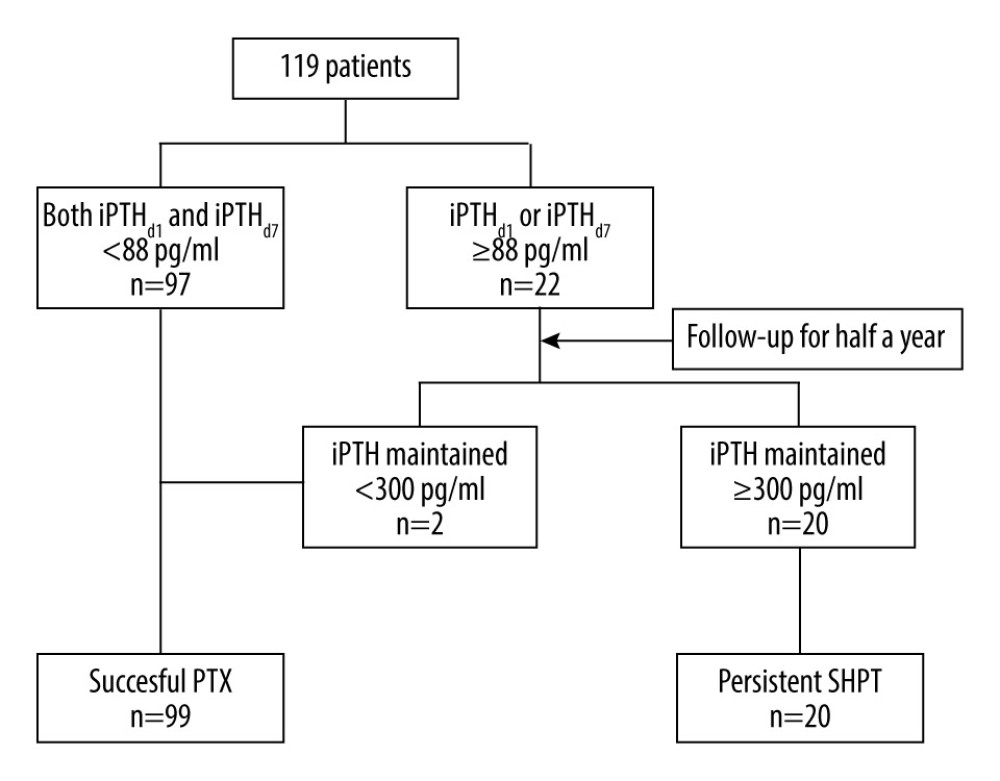 Figure 1. Flow chart for confirming successful parathyroidectomy and persistent secondary hyperparathyroidism.
Figure 1. Flow chart for confirming successful parathyroidectomy and persistent secondary hyperparathyroidism.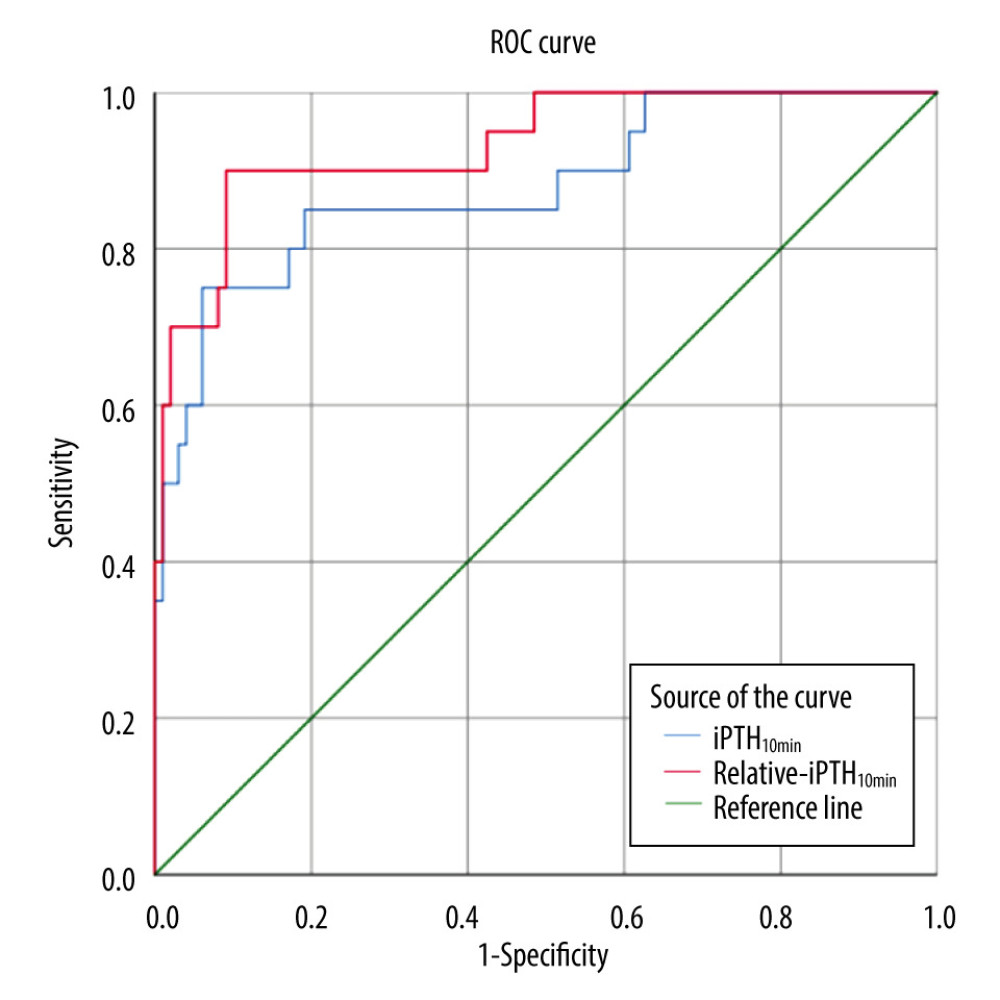 Figure 2. The ROC curves for persistent secondary hyperparathyroidism. The AUC for iPTH10min and relative-iPTH10min was 0.880 and 0.933, respectively. Cutoff values of iPTH10min and relative-iPTH10min were 314.5 pg/ml (sensitivity 75.0%, specificity 93.9%) and 12.4% (sensitivity 90.0%, specificity 90.9%).
Figure 2. The ROC curves for persistent secondary hyperparathyroidism. The AUC for iPTH10min and relative-iPTH10min was 0.880 and 0.933, respectively. Cutoff values of iPTH10min and relative-iPTH10min were 314.5 pg/ml (sensitivity 75.0%, specificity 93.9%) and 12.4% (sensitivity 90.0%, specificity 90.9%).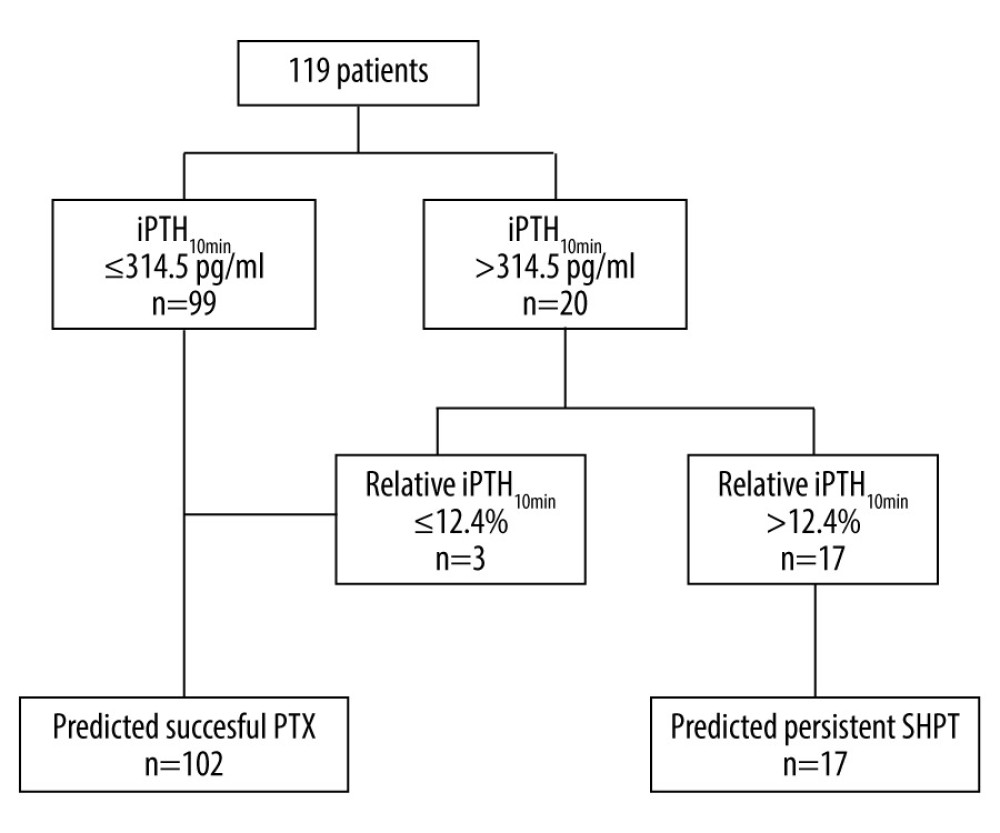 Figure 3. Flow chart using the paralleled criterion to predict surgical outcomes.
Figure 3. Flow chart using the paralleled criterion to predict surgical outcomes.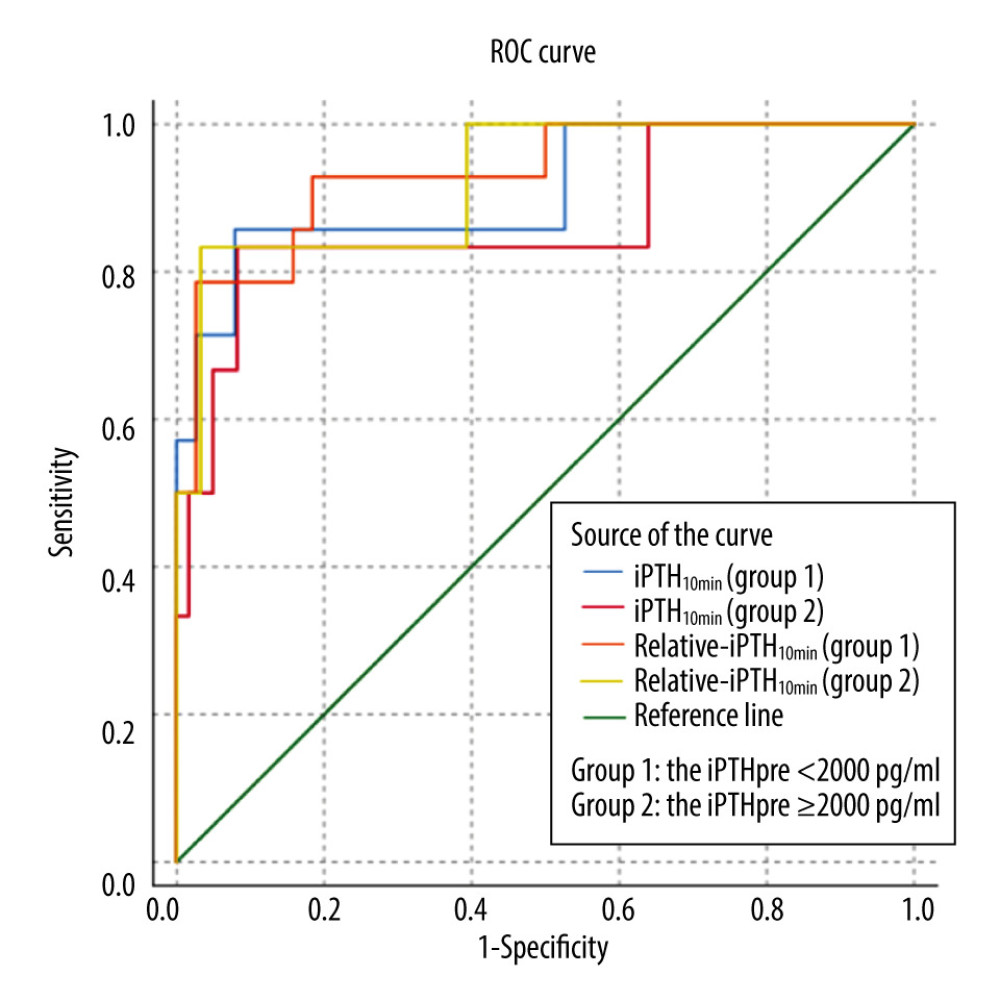 Figure 4. The ROC curves for persistent secondary hyperparathyroidism in the iPTHpre <2000 pg/ml group and the iPTHpre ≥2000 pg/ml group. In the iPTHpre <2000 pg/ml group, the AUC of iPTH10min and relative-iPTH10min were 0.910 and 0.932, respectively; cutoff values of iPTH10min and relative-iPTH10min were 218 pg/ml (sensitivity 85.7%, specificity 92.1%) and 20.3% (sensitivity 78.6%, specificity 97.4%). In the iPTHpre ≥2000 pg/ml group, the AUC of iPTH10min and relative-iPTH10min were 0.869 and 0.923, respectively; cutoff values of iPTH10min and relative-iPTH10min were 318 pg/ml (sensitivity 83.3%, specificity 91.8%) and 12.1% (sensitivity 83.3%, specificity 96.7%).
Figure 4. The ROC curves for persistent secondary hyperparathyroidism in the iPTHpre <2000 pg/ml group and the iPTHpre ≥2000 pg/ml group. In the iPTHpre <2000 pg/ml group, the AUC of iPTH10min and relative-iPTH10min were 0.910 and 0.932, respectively; cutoff values of iPTH10min and relative-iPTH10min were 218 pg/ml (sensitivity 85.7%, specificity 92.1%) and 20.3% (sensitivity 78.6%, specificity 97.4%). In the iPTHpre ≥2000 pg/ml group, the AUC of iPTH10min and relative-iPTH10min were 0.869 and 0.923, respectively; cutoff values of iPTH10min and relative-iPTH10min were 318 pg/ml (sensitivity 83.3%, specificity 91.8%) and 12.1% (sensitivity 83.3%, specificity 96.7%). Tables
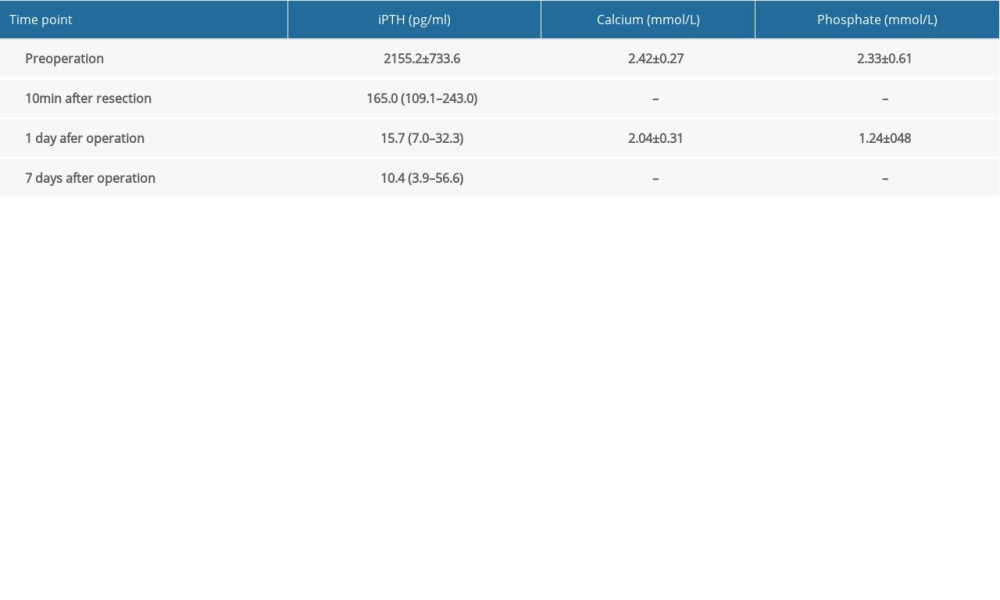 Table 1. Laboratory data before and after the operation.
Table 1. Laboratory data before and after the operation.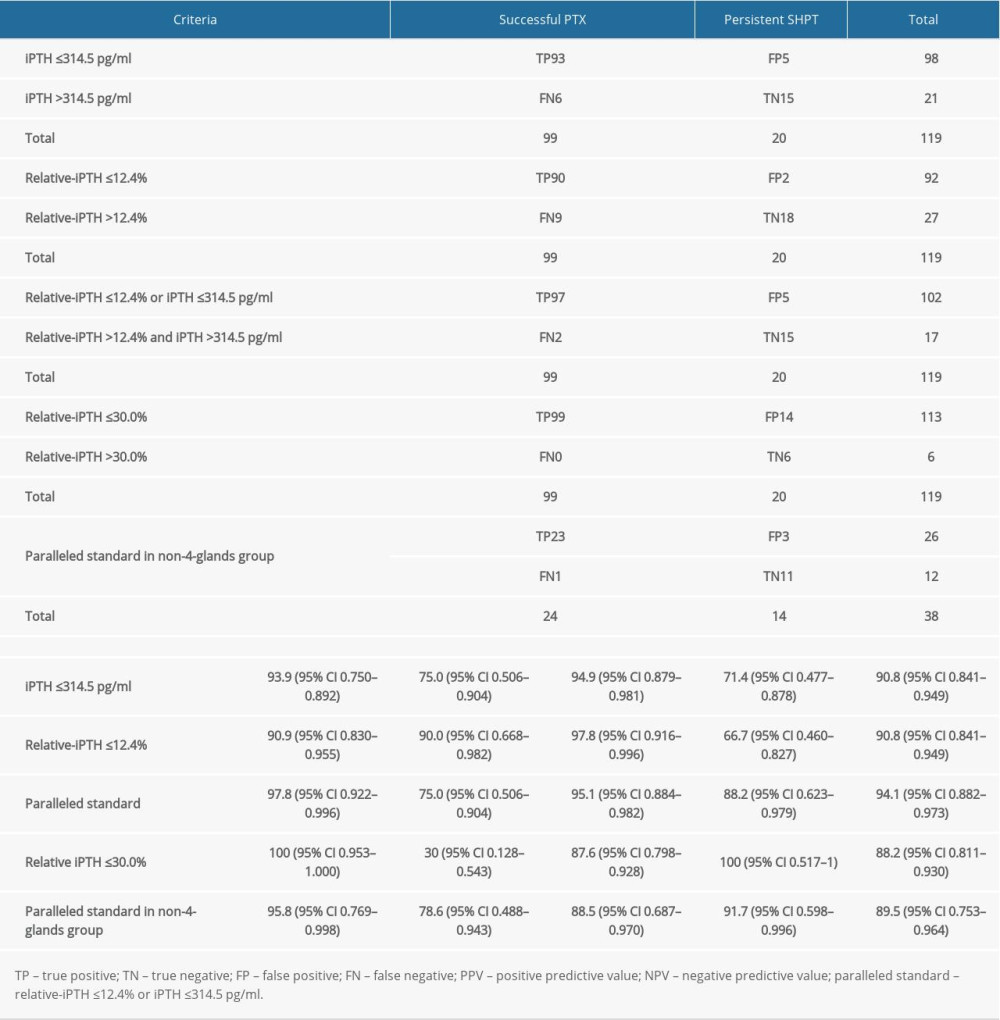 Table 2. Accuracy of different IO-iPTH prediction criteria.
Table 2. Accuracy of different IO-iPTH prediction criteria.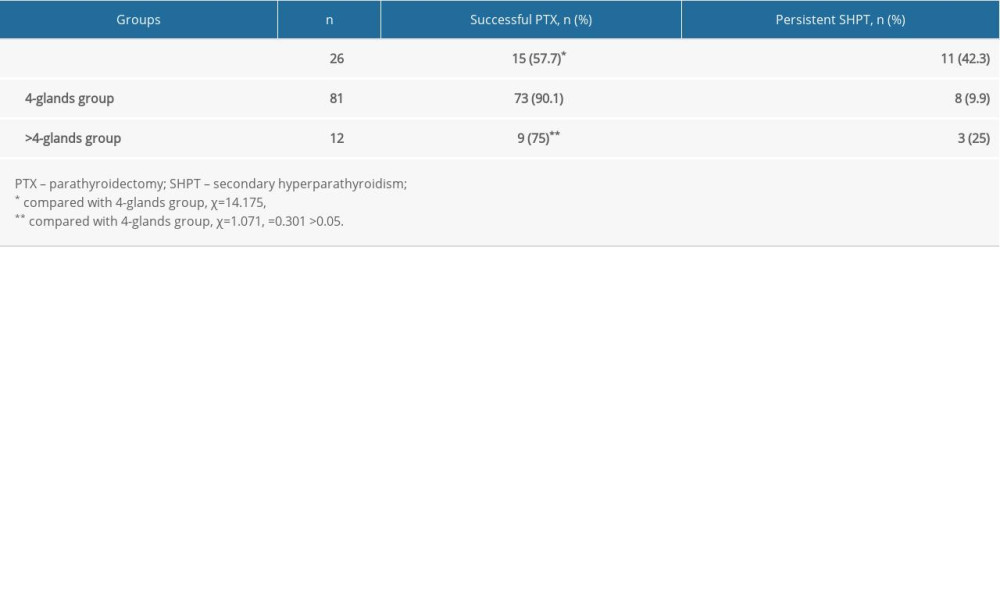 Table 3. Influence of the number of parathyroid glands removed during operation on the successful PTX rate.
Table 3. Influence of the number of parathyroid glands removed during operation on the successful PTX rate.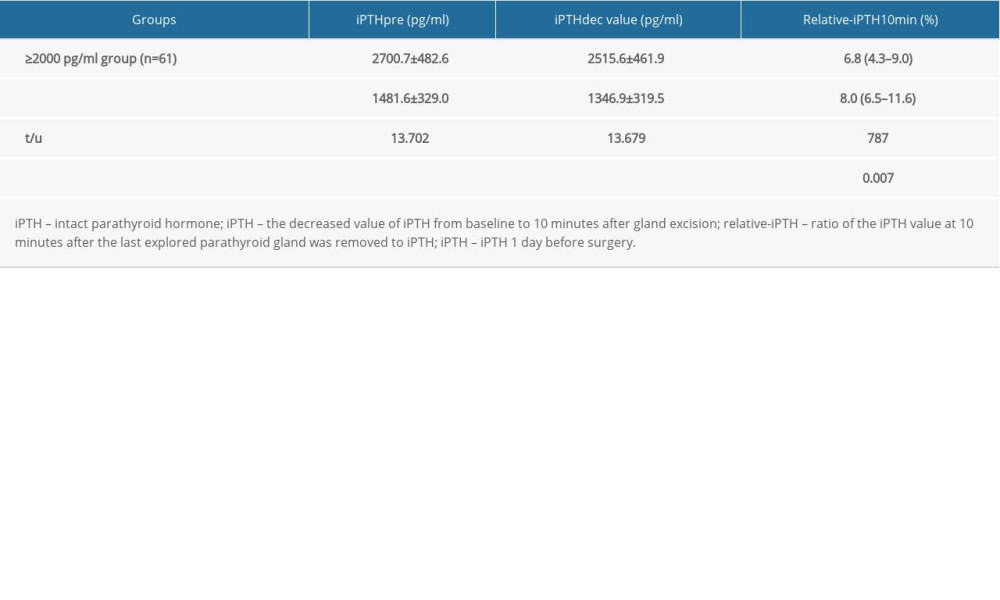 Table 4. The iPTHdec value and relative-iPTH10min in patients with successful PTX.
Table 4. The iPTHdec value and relative-iPTH10min in patients with successful PTX.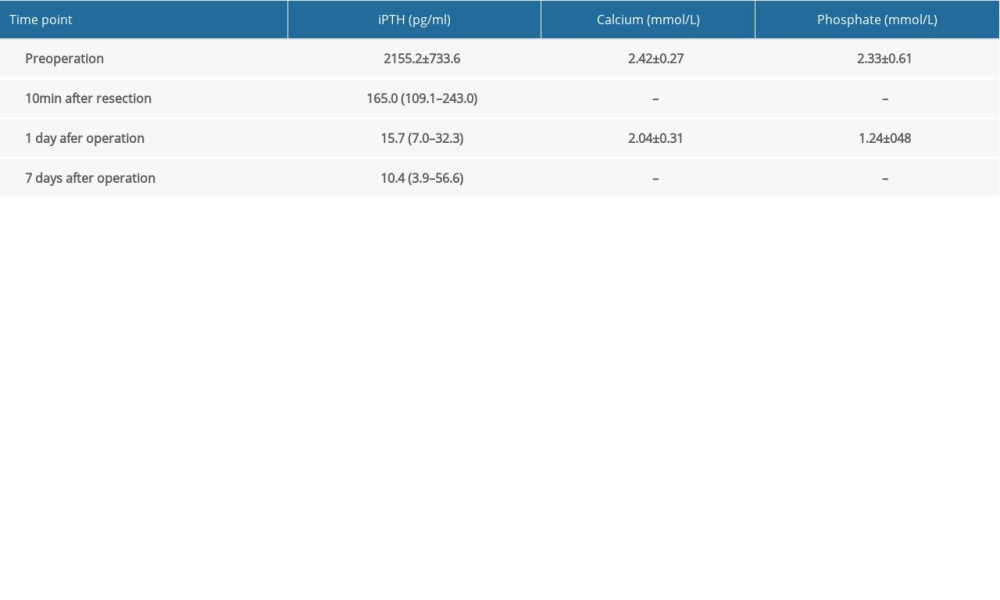 Table 1. Laboratory data before and after the operation.
Table 1. Laboratory data before and after the operation.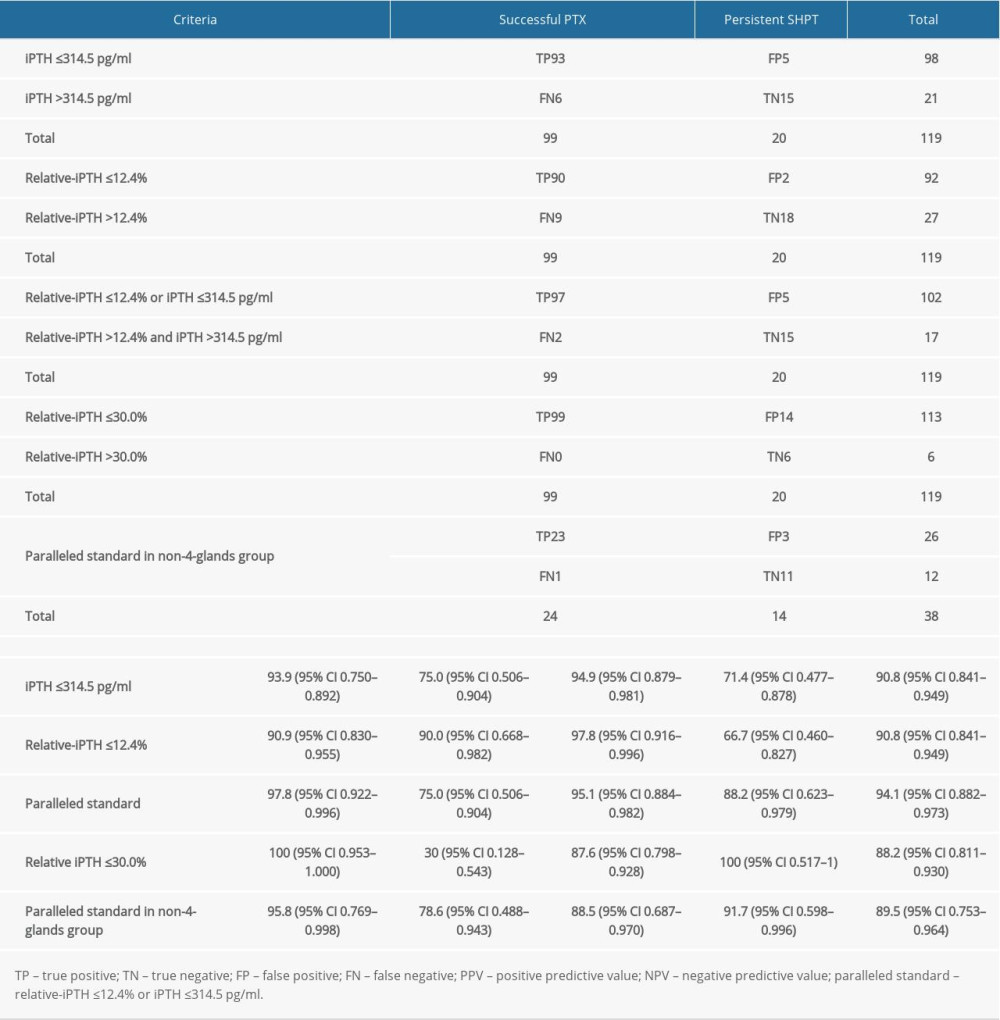 Table 2. Accuracy of different IO-iPTH prediction criteria.
Table 2. Accuracy of different IO-iPTH prediction criteria.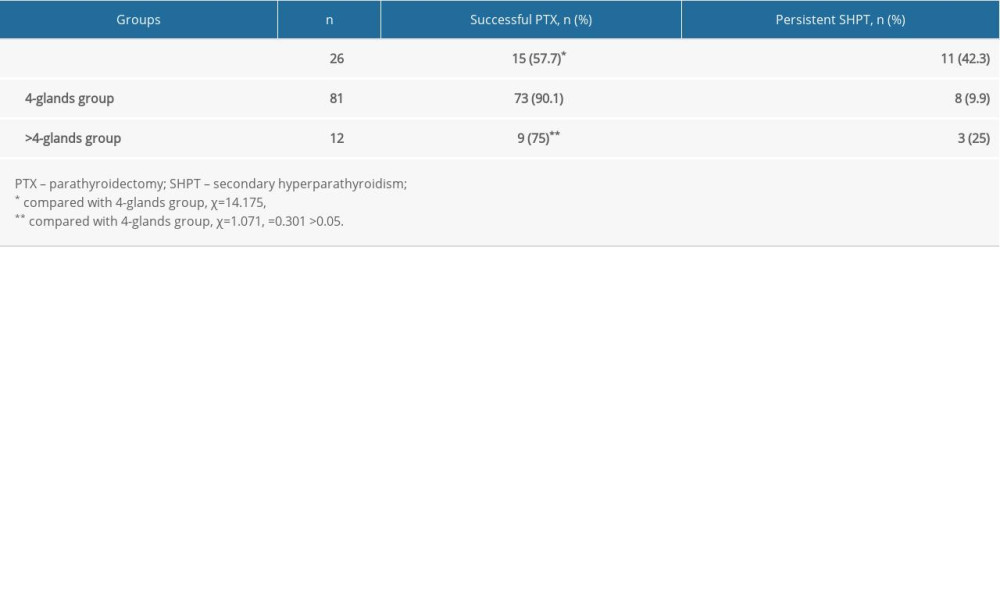 Table 3. Influence of the number of parathyroid glands removed during operation on the successful PTX rate.
Table 3. Influence of the number of parathyroid glands removed during operation on the successful PTX rate.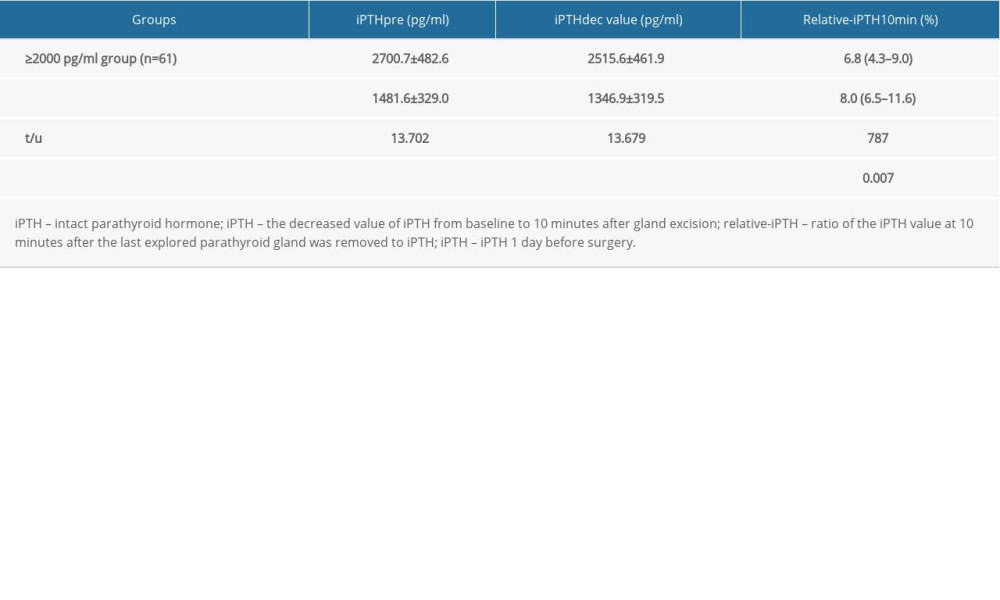 Table 4. The iPTHdec value and relative-iPTH10min in patients with successful PTX.
Table 4. The iPTHdec value and relative-iPTH10min in patients with successful PTX. In Press
05 Mar 2024 : Clinical Research
Muscular Function Recovery from General Anesthesia in 132 Patients Undergoing Surgery with Acceleromyograph...Med Sci Monit In Press; DOI: 10.12659/MSM.942780
05 Mar 2024 : Clinical Research
Effects of Thermal Insulation on Recovery and Comfort of Patients Undergoing Holmium Laser LithotripsyMed Sci Monit In Press; DOI: 10.12659/MSM.942836
05 Mar 2024 : Clinical Research
Role of Critical Shoulder Angle in Degenerative Type Rotator Cuff Tears: A Turkish Cohort StudyMed Sci Monit In Press; DOI: 10.12659/MSM.943703
06 Mar 2024 : Clinical Research
Comparison of Outcomes between Single-Level and Double-Level Corpectomy in Thoracolumbar Reconstruction: A ...Med Sci Monit In Press; DOI: 10.12659/MSM.943797
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








