17 August 2021: Clinical Research
Effects of Temperature and Volume of Intraoperative Normal Saline Irrigation on Postoperative Pain, Swelling, and Serum Markers of Inflammation in Patients After Elective, Arthroscopic, Single-Bundle Surgical Reconstruction of the Anterior Cruciate Ligament: A Retrospective, Single-Center Study
Chen Wang1AE, Pu Yang1BCD, Dongfang Zhang1BCD, In-Ho Jeon2F, Tengbo Yu1F, Yingze Zhang1F, Chao Qi1AF*DOI: 10.12659/MSM.930954
Med Sci Monit 2021; 27:e930954
Abstract
BACKGROUND: Arthroscopic single-bundle surgical reconstruction of the anterior cruciate ligament (ACL) is often performed electively after 3 weeks of mobilization therapy. The present single-center retrospective study aimed to investigate the effects of temperature and volume of intraoperative normal saline irrigation on postoperative pain and swelling and on serum markers of inflammation following elective, arthroscopic, single-bundle surgical reconstruction of the ACL.
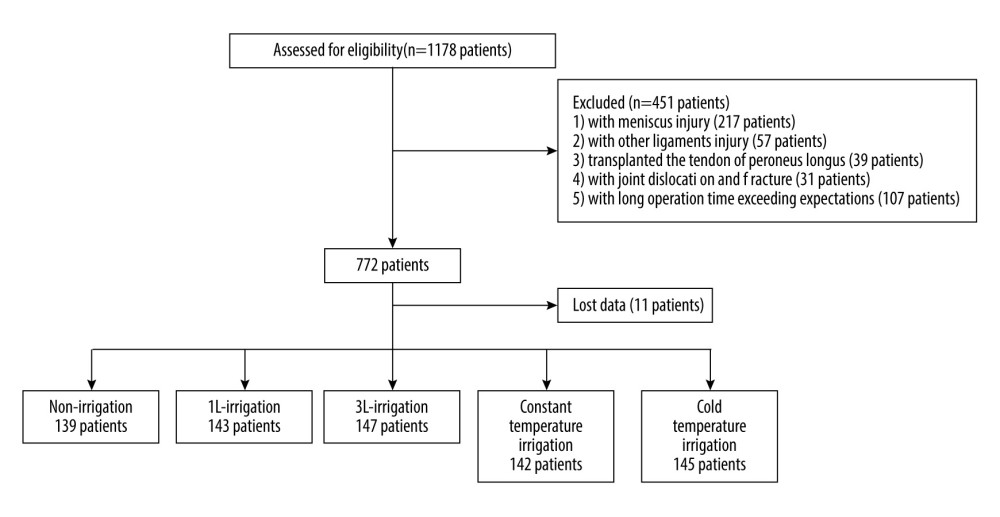
MATERIAL AND METHODS: Clinical data from 716 patients with non-acute ACL injuries who met the criteria between March 2015 and May 2020 were retrospectively analyzed. The patients were broken into 5 groups, depending on the volume or temperature of intraoperative irrigation with normal saline. At specific times after surgery, pain, knee swelling, and skin temperature were assessed. Postoperative levels of serum C-reactive protein (CRP), interleukin (IL)-1, IL-6, and IL-10 also were measured.
RESULTS: Visual analog scale (VAS) scores for pain, rates of swelling, and skin temperature differed significantly among the 5 groups at all postoperative time points (P<0.001). The VAS scores(P=0.322) and ratings for swelling (P=0.245), and skin temperature (P=0.093) were not significantly different among the volume groups. There were no significant differences in the VAS scores (P=0.055), swelling ratings (P=0.570), or skin temperatures (P=0.321) among the groups that received irrigation with normal saline at different temperatures. There were no significant differences in postoperative serum levels of CRP, IL-1, IL-6, or IL-10 among the groups (P>0.05).
CONCLUSIONS: Irrigation with different volumes and temperatures of normal saline did not have a significant effect on postoperative pain, swelling, or serum markers of inflammation.
Keywords: Arthroscopy, Knee, Pain, Postoperative, Therapeutic Irrigation, Anterior Cruciate Ligament, Anterior Cruciate Ligament Injuries, anterior cruciate ligament reconstruction, C-Reactive Protein, Edema, Knee Joint, Postoperative Complications, saline solution, Temperature
Background
Injuries to the anterior cruciate ligament (ACL) are common and arthroscopic reconstruction is a routine procedure in Sports Medicine [1,2]. The ACL plays a major role in maintaining knee stability and function [2–4]; therefore, most patients require treatment after an ACL injury. Eighty-one percent of patients are able to return to exercise after ACL reconstruction [4]. After surgery, patients need to undertake rigorous postoperative rehabilitation exercise, but postoperative swelling and pain in the knee can affect movement of the joint and cause difficulties [4–8]. Intraoperative intervention and postoperative management are routinely used to reduce postoperative pain and swelling [9–12].
After ACL reconstruction surgery, it is necessary to continue irrigation with saline under arthroscopy for a period of time to clean the dissociative tissue in the joint cavity [13,14]. One study [15] reported that the temperature of the saline solution used for irrigation during arthroscopic meniscus resection did not affect postoperative pain in and swelling of the knee. Another study [16] indicated out that a difference in volume of saline solution did not affect postoperative pain and swelling in the knee. Because of fear about serious infection and joint fibrosis, surgeons are cautious in attempting surgery soon after an ACL injury [17,18]. ACL reconstruction at 3 weeks results in good functional outcomes without increasing risk of complications such as arthrofibrosis and limitation in range of motion [19].
Studies of postoperative pain and swelling in patients with ACL injuries that happened >3 weeks previously (non-acute) who have undergone arthroscopic ACL reconstruction with irrigation using different temperatures and volumes of saline are rare. Arthroscopic single-bundle surgical reconstruction of the ACL is commonly performed electively using general anesthesia, after 3 weeks of mobilization therapy. Therefore, the present single-center, retrospective study aimed to investigate the effects of irrigation with normal saline at different temperatures and volumes on pain, swelling, and serum markers of inflammation after elective, arthroscopic, single-bundle surgical reconstruction of the ACL.
Material and Methods
SURGICAL TECHNIQUE:
Patients underwent arthroscopic, single-bundle ACL reconstruction under general anesthesia. Arthroscopic channel incisions were made and routine exploration was performed to confirm injury to the ACL. The ipsilateral hamstring tendons (the half and gracilis tendons) were stripped as spare tendons. The surgeons drilled femoral and tibial tunnels and then pulled the spare tendons into the tunnels. An Endo-Button (Smith & Nephew) was used to fix the femoral end and then tibial end was fixed with an absorbable squeeze screw (Smith & Nephew). Saline bags were hung on a bedside infusion stand and the pressure was set at approximately 80 mmHg. An arthroscope connected to the saline bags was used as the water inlet and a planer connected to the suction device was used as the water outlet. No more than 3 bags containing 3 L of saline were used during arthroscopic ACL reconstruction. After that step was complete, normal saline irrigation was performed in the irrigation groups but withheld from the non-irrigation group. Finally, sodium hyaluronate was injected into the joint cavity and the leg was bandaged with an elastic bandage.
Non-steroidal anti-inflammatory analgesics were routinely given and cold compresses applied after the procedure. To foster restoration of muscle function and joint activity, gradual rehabilitation exercises were performed beginning on day 2 after surgery, in keeping with the plan for rehabilitation after ACL reconstruction. All of the surgeries were completed by the same doctor, who had 20 years of clinical experience. He was blinded to the different patient groups.
CLINICAL EVALUATION:
A visual analog scale (VAS) was used to determine pain at 6, 12, 24, 48, and 72 h after surgery. To assess swelling, knee circumference was measured at 2 cm above the superior border of the patella at 6, 12, 24, 48, and 72 h after surgery. The postoperative knee swelling rating on the injured side was defined as the knee circumference on the injured side minus the knee circumference on the uninjured side, both measured in centimeters [15]. Skin temperature of the knee was measured at the center of the anterior patella on postoperative days 1, 3, and 5. Limbs were exposed to room temperature for 5 minutes bilaterally and then the skin temperature was measured with a skin temperature gun. The skin temperature on the injured side was defined as the skin temperature on the injured side minus the skin temperature on the uninjured side, both measured in degrees centigrade (°C) [20]. Serum levels of C-reactive protein (CRP) were measured on postoperative days 1 and 3. Serum levels of interleukin (IL)-1, IL-6, and IL-10 were measured 6, 12, and 24 h after surgery. All VAS scores and data measurements were completed by the same doctor, who had 7 years of clinical experience.
STATISTICAL ANALYSIS:
All data analyses were performed using SPSS software, version 26.0. A chi-square test was used for categorical variables. Measurements of data such as VAS scores, knee swelling ratings, skin temperatures, and serum levels of CRP, IL-1, IL-6, and IL-10 were expressed as means±standard deviations. Comparisons at different time points were performed using analysis of variance.
Results
There were no statistically significant differences in sex, age, body mass index (BMI), or MRI classification among the 5 groups (
Discussion
In the present study, we compared outcomes of intraoperative irrigation with different volumes of normal saline during follow-up of patients who had undergone ACL surgery. Our results showed no statistically significant differences among the volume or temperature groups in VAS scores, swelling, or skin temperature. Moreover, postoperative serum levels of CRP, IL-1, IL-6, and IL-10 were similar in the volume and temperature groups. In general, arthroscopic techniques are believed to be quicker, safer, simpler, and more effective than open surgery because they result in a smaller wound [21–23]. During arthroscopic knee surgery, flushing the site with saline irrigation often is necessary to clear the surgical field and improve visualization. Fluids such as normal saline, lactated Ringer’s solution, and carbohydrate solutions typically are used for irrigation to expand the joint and provide visibility sufficient that the procedure can continue [23,24].
Similar studies have reported that the temperature [15] and volume [16] of saline solution used in irrigation during arthroscopic meniscus resection does not affect postoperative pain and swelling in the knee. The inference is that cold saline irrigation of the joint does not change the temperature of superficial knee tissues such as the skin and muscles. In our study, we focused on ACL reconstruction. As is well known, arthroscopic ACL reconstruction requires drilling femoral and tibial tunnels, which results in bone debris that must be carefully cleared to ensure a successful procedure. Compared with a partial meniscus resection, the operative time for ACL repairs is longer while the procedure is more complicated and generates more impurities. An extended irrigation time would be more practical following ACL reconstruction than meniscus resection. In the present study, emphasis was placed on whether use of differing volumes of continuous saline for intraoperative irrigation would affect postoperative pain and swelling. We also focused on the effect on postoperative pain, swelling, and serum inflammation values of the temperature of the irrigation solution used during ACL surgery. The temperature of saline used in the operating room is generally 23°C, whereas normal body temperature is 36°C [25,26]. Here, we summarize results of previous studies similar to ours, which focused on a comprehensive assessment of the effects of different volumes and temperatures of intraoperative irrigation on postoperative pain, swelling, and serum inflammation values in patients undergoing ACL surgery.
One research paper demonstrated that normal saline supplemented with epinephrine (concentration 1 mg/L) reduced bleeding volume during arthroscopic procedures, improving visibility and reducing operative time [27]. Postoperative pain and swelling in the knee also were observed; postoperative symptoms improved substantially, which led to a quicker postoperative recovery in patients. In that study, an appropriate amount of epinephrine was added to the normal saline before the intraoperative conditions were noted and postoperative symptoms observed. In some countries, this has now become the criterion standard for practice in arthroscopic surgeries; however, it has not been adopted universally. Most hospitals use conventional saline for arthroscopic surgery. Therefore, the present study is of great significance because the aim was to identify ways to improve a practice that is widely utilized.
Recent research has indicated that use of a mechanical irrigation system is superior to gravity irrigation [28,29]. The advantages are constant flow, greater joint expansion, an improved field of vision, a reduced tourniquet requirement, and less operative bleeding. Although a mechanical irrigation system has many advantages, it comes with high usage and maintenance costs, as well as a requirement that the surgical team learn a complicated technique. For these reasons, such a system is rarely used in arthroscopic surgery; the preferred method is gravity-mediated irrigation. The present study focused on a gravity irrigation system, but the differential volumes of saline were applied in the same way as with a mechanical irrigation system. In the future, gravity-mediated irrigation may be replaced by mechanical irrigation, but our research is still of importance because it focused on improving the practice that is utilized most commonly.
The results of the present study indicate that the different saline volumes and temperatures did not aggravate or worsen postoperative pain and swelling. This was in contrast to the initial assumptions about the study. We hypothesized that enlarging the joint capacity and irrigating for a longer period of time would lead to more fluid penetration into the interstitial space and result in increased postoperative pain and swelling. That, however, was not the case; there were no significant differences in postoperative VAS scores, swelling, or temperature ratings for different volumes of irrigation. Therefore, although we used 3 different volumes of saline, the extra fluid appeared to be absorbed without issue. Arthroscopic irrigation was performed throughout the whole surgical procedure, so the total volume of saline was similar among the 3 groups. This could infer that the different volumes of saline used in this study were not large enough to have a detrimental effect on postoperative symptoms. In future research, a larger volume of saline could be used to test the effect on postoperative outcomes following arthroscopic surgery. We believed that such a volume would not beneficial; therefore, it was not incorporated into the present study.
We used skin temperature to as a marker of the inflammatory reaction in local superficial tissues. In clinical practice, a temperature difference of 1°C to 2°C can be distinguished by touching the patient’s skin. In the present study, early postoperative rehabilitation was tailored according a patient’s postoperative arthritic reaction. Saline at different temperatures is known to affect the temperature of the skin over the knee joint to some extent. Some research indicates that room-temperature irrigation is a physical stimulus for the body that can cause a decrease in a patient’s core temperature [30–32]. The mechanism for the decrease in core body temperature at the beginning of irrigation is complicated and difficult to understand. Opinions about it in recent studies have differed; most research infers that the changes in body temperature are related to the continuous cold stimulation of the irrigation [31,32]. However, the present study showed that there was no significant difference among the 3 groups in which fluid at varying temperatures was used for irrigation. This suggests that, although the core temperature of the knee may have changed after surgery, the temperature differences in the irrigation fluid were not large enough to influence postoperative symptoms.
Another study suggested that cold stimulation may affect the immune system and upregulate the levels of inflammatory cytokines, including pro-inflammatory and anti-inflammatory cytokines [33]. IL-1, IL-6, IL-10, and CRP levels were considered indicators of inflammation. Brenner studied the response of the human immune system to cold and found that a cold stimulus led to elevated IL-6 levels [34]. The present study indicated that serum levels of IL-1, IL-6, IL-10, and CRP did not differ significantly after surgery, which suggests that the inflammatory response was the same even when the temperature and volume of the irrigation fluid varied. While our study is of great value to the field of arthroscopic surgery, because ACL reconstruction is limited as a surgical procedure, further research is needed regarding the volume and temperature of saline used during irrigation.
The present study had several limitations. Given the characteristics of ACL surgery, we could not do larger-volume irrigation because of the potential negative impact on patients. Using even more fluid or solutions at other temperatures could affect postoperative outcomes. Because ours was a retrospective study with all its associated biases, prospective, randomized, controlled studies are needed to validate the results.
Conclusions
The findings from the present retrospective, single-center study showed that irrigation with different volumes and temperatures of normal saline did not have a significant effect on postoperative pain, swelling, or serum markers of inflammation in patients who underwent elective, arthroscopic, single-bundle surgical reconstruction of the ACL.
Tables
Table 1. Clinical and demographic characteristics of 716 patients after arthroscopic single-bundle surgical reconstruction of the ACL performed under general anesthesia.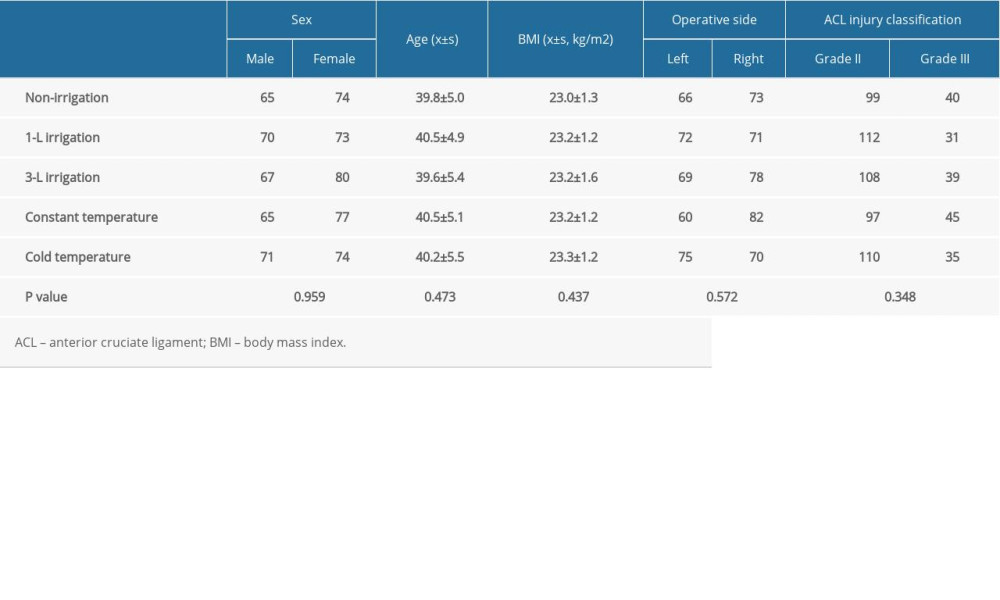 Table 2. Comparison of VAS results in 716 patients after arthroscopic single-bundle surgical reconstruction of the ACL performed under general anesthesia.
Table 2. Comparison of VAS results in 716 patients after arthroscopic single-bundle surgical reconstruction of the ACL performed under general anesthesia. Table 3. Comparison of swelling ratings in 716 patients after arthroscopic single-bundle surgical reconstruction of the ACL performed under general anesthesia.
Table 3. Comparison of swelling ratings in 716 patients after arthroscopic single-bundle surgical reconstruction of the ACL performed under general anesthesia.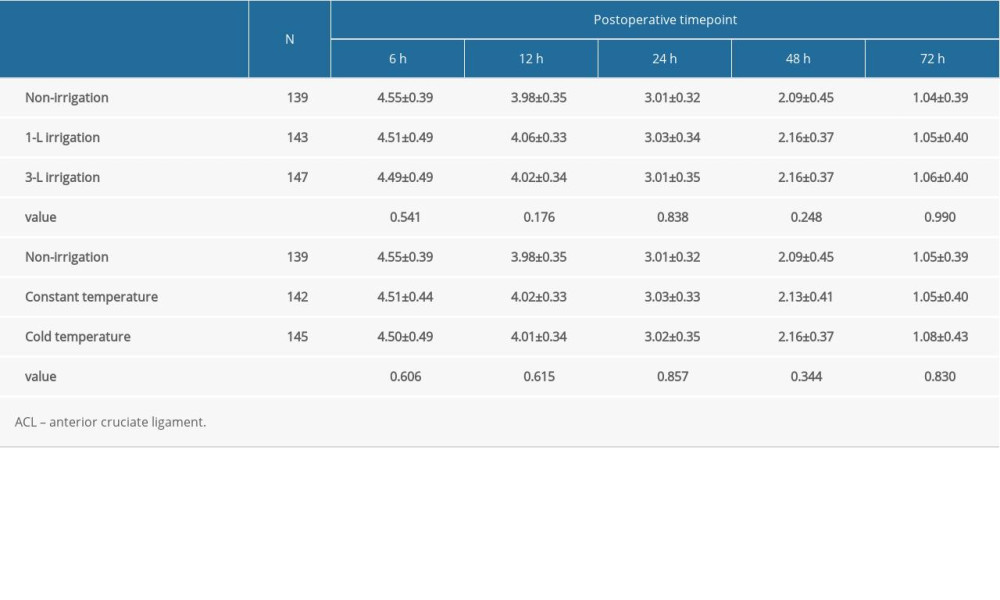 Table 4. Comparison of skin temperature ratings and CRP in 716 patients after arthroscopic single-bundle surgical reconstruction of the ACL performed under general anesthesia.
Table 4. Comparison of skin temperature ratings and CRP in 716 patients after arthroscopic single-bundle surgical reconstruction of the ACL performed under general anesthesia.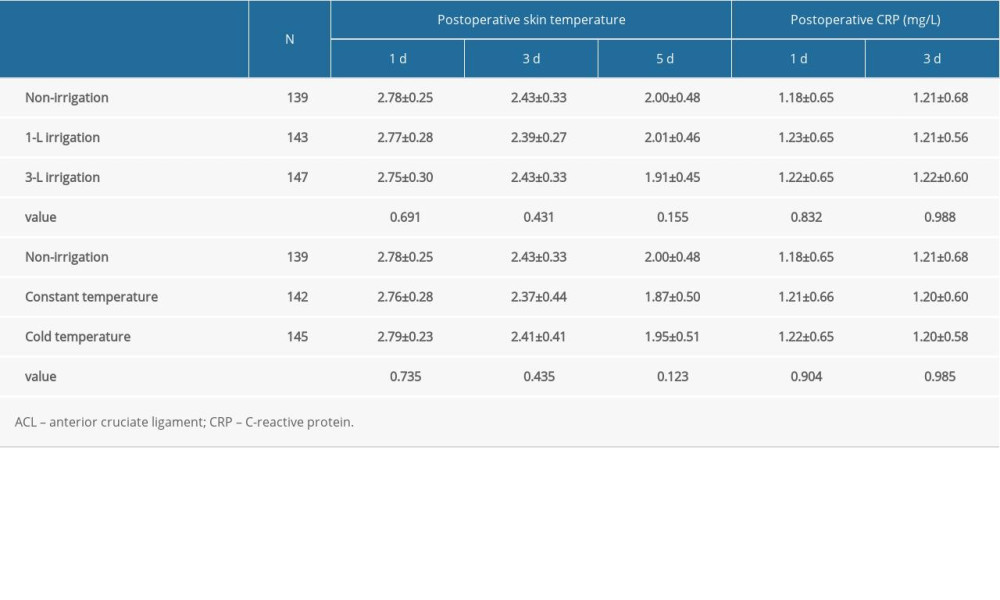 Table 5. Comparison of results with IL-1, IL-6, and IL-10 in 716 patients following arthroscopic single-bundle surgical reconstruction of the ACL performed under general anesthesia.
Table 5. Comparison of results with IL-1, IL-6, and IL-10 in 716 patients following arthroscopic single-bundle surgical reconstruction of the ACL performed under general anesthesia.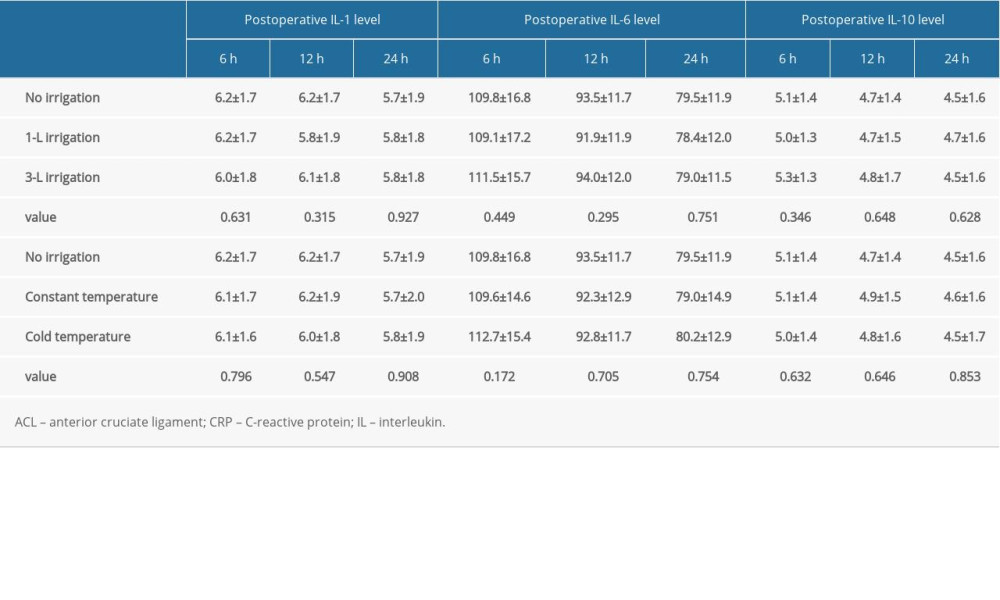
References
1. Wang H, Shen B, Zeng Y, Comparison of topical versus intravenous tranexamic acid in primary total knee arthroplasty: A meta-analysis of randomized controlled and prospective cohort trials: Knee, 2014; 21(6); 987-93
2. Salzler MJ, Lin A, Miller CD, Complications after arthroscopic knee surgery: Am J Sports Med, 2014; 42; 292-96
3. Andrés-Cano P, Godino M, Vides M, Guerado E, Postoperative complications of anterior cruciate ligament reconstruction after ambulatory surgery: Rev Esp Cir Ortop Traumatol, 2015; 59; 157-64
4. Bahl V, Goyal A, Jain V, Joshi D, Chaudhary D, Effect of haemarthrosis on the rehabilitation of anterior cruciate ligament reconstruction: Single bundle versus double bundle: J Orthop Surg Res, 2013; 8; 5
5. King E, Richter C, Jackson M, Factors influencing return to play and second anterior cruciate ligament injury rates in level 1 athletes after primary anterior cruciate ligament reconstruction: 2-year follow-up on 1432 reconstructions at a single center: Am J Sports Med, 2020; 48(4); 812-24
6. Muller B, Yabroudi MA, Lynch A, Defining thresholds for the Patient Acceptable Symptom State for the IKDC subjective knee form and KOOS for patients who underwent ACL reconstruction: Am J Sports Med, 2016; 44(11); 2820-26
7. Spindler KP, Huston LJMOON Knee Group, Ten-year outcomes and risk factors after anterior cruciate ligament reconstruction: A MOON longitudinal prospective cohort study: Am J Sports Med, 2018; 46(4); 815-25
8. Vega JF, Jacobs CA, Strnad GJ, Prospective evaluation of the patient acceptable symptom state to identify clinically successful anterior cruciate ligament reconstruction: Am J Sports Med, 2019; 47(5); 1159-67
9. Hantes ME, Raoulis VA, Doxariotis N, Management of septic arthritis after arthroscopic anterior cruciate ligament reconstruction using a standard surgical protocol: Knee, 2017; 24(3); 588-93
10. Schuster P, Schulz M, Immendoerfer M, Septic arthritis after arthroscopic anterior cruciate ligament reconstruction: Evaluation of an arthroscopic graft-retaining treatment protocol: Am J Sports Med, 2015; 43(12); 3005-12
11. van Montfoort DO, van Kampen PM, Huijsmans PE, Epinephrine diluted saline-irrigation fluid in arthroscopic shoulder surgery: A significant improvement of clarity of visual field and shortening of total operation time. A randomized controlled trial: Arthroscopy, 2016; 32(3); 436-44
12. Tuijthof GJ, de Vaal MM, Sierevelt IN, Performance of arthroscopic irrigation systems assessed with automatic blood detection: Knee Surg Sports Traumatol Arthrosc, 2011; 19; 1948-54
13. Wright R, Spindler K, Huston L, Revision ACL reconstruction outcomes: MOON cohort: J Knee Surg, 2011; 24(4); 289-94
14. Samuelsson K, Magnussen RA, Alentorn-Geli E, Equivalent knee injury and osteoarthritis outcome scores 12 and 24 months after anterior cruciate ligament reconstruction: Results from the Swedish national knee ligament register: Am J Sports Med, 2017; 45(9); 2085-91
15. Fincher LA, Woods WG, O’Connor DP, Intraoperative arthroscopic cold irrigation solution does not affect postoperative pain and swelling: J Athl Train, 2004; 39(1); 12-16
16. Wang C, Yang P, Zhang DThe effect of different continuous saline irrigation volume under arthroscopy on early postoperative pain and swelling of the knee: Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi, 2021; 35(2); 178-82 [in Chinese]
17. Lattermann C, Jacobs CA, Bunnell MP, Logistical challenges and design considerations for studies using acute anterior cruciate ligament injury as a potential model for early posttraumatic osteoarthritis: J Orthop Res, 2017; 35(3); 641-50
18. Hamrin Senorski E, Svantesson E, Beischer S, Factors affecting the achievement of a patient-acceptable symptom state 1 year after anterior cruciate ligament reconstruction: A cohort study of 343 patients from 2 registries: Orthop J Sports Med, 2018; 6(4) 2325967118764317
19. Deabate L, Previtali D, Grassi A, Anterior cruciate ligament reconstruction within 3 weeks does not increase stiffness and complications compared with delayed reconstruction: A meta-analysis of randomized controlled trials: Am J Sports Med, 2020; 48; 1263-72
20. Rashkovska A, Trobec R, Avbelj V, Veselko M, Knee temperatures measured in vivo after arthroscopic ACL reconstruction followed by cryotherapy with gel-packs or computer controlled heat extraction: Knee Surg Sports Traumatol Arthrosc, 2014; 22(9); 2048-56
21. van der List JP, Jonkergouw A, van Noort A, Identifying candidates for arthroscopic primary repair of the anterior cruciate ligament: A case-control study: Knee, 2019; 26(3); 619-27
22. Wilson WK, Morris R, Coskey A, Quadriceps augmentation of undersized hamstrings during ACL reconstruction: Knee, 2019; 26(1); 73-78
23. Kroker A, Manske SL, Mohtadi N, Boyd SK, A study of the relationship between meniscal injury and bone microarchitecture in ACL reconstructed knees: Knee, 2018; 25(5); 746-56
24. Choi S, Kim MK, Kwon YS, Kang H, Clinical and arthroscopic outcome of single bundle anterior cruciate ligament reconstruction: Comparison of remnant preservation versus conventional technique: Knee, 2017; 24(5); 1025-32
25. Gulihar A, Bryson DJ, Taylor GJ, Effect of different irrigation fluids on human articular cartilage: An in vitro study: Arthroscopy, 2013; 29(2); 251-56
26. Teeple E, Karamchedu NP, Larson KM, Arthroscopic irrigation of the bovine stifle joint increases cartilage surface friction and decreases superficial zone lubricin: J Biomech, 2016; 49(13); 3106-10
27. Avery DM, Gibson BW, Carolan GF, Surgeon-rated visualization in shoulder arthroscopy: A randomized blinded controlled trial comparing irrigation fluid with and without epinephrine: Arthroscopy, 2015; 31(1); 12-18
28. Hsiao MS, Kusnezov N, Sieg RN, Use of an irrigation pump system in arthroscopic procedures: Orthopedics, 2016; 39(3); e474-78
29. Mayo M, Wolsky R, Baldini T, Gravity fluid flow more accurately reflects joint fluid pressure compared with commercial peristaltic pump systems in a cadaveric model: Arthroscopy, 2018; 34(12); 3132-38
30. Stärke F, Awiszus F, Lohmann CH, Stärke C, The effect of irrigation time and type of irrigation fluid on cartilage surface friction: J Mech Behav Biomed Mater, 2018; 77; 187-91
31. Yazdi H, Moradi A, Herbort M, The effect of gentamicin in irrigating solutions on articular infection prophylaxis during arthroscopic ACL reconstruction: Arch Orthop Trauma Surg, 2014; 134(2); 257-61
32. Tanavalee A, Honsawek S, Rojpornpradit T, Inflammation related to synovectomy during total knee replacement in patients with primary osteoarthritis: A prospective, randomised study: J Bone Joint Surg Br, 2011; 93(8); 1065-70
33. Alonso B, Bravo B, Mediavilla L, Osteoarthritis-related biomarkers profile in chronic anterior cruciate ligament injured knee: Knee, 2020; 27(1); 51-60
34. Brenner SS, Klotz U, Alscher DM, Osteoarthritis of the knee – clinical assessments and inflammatory markers: Osteoarthritis Cartilage, 2004; 12(6); 469-75
Tables
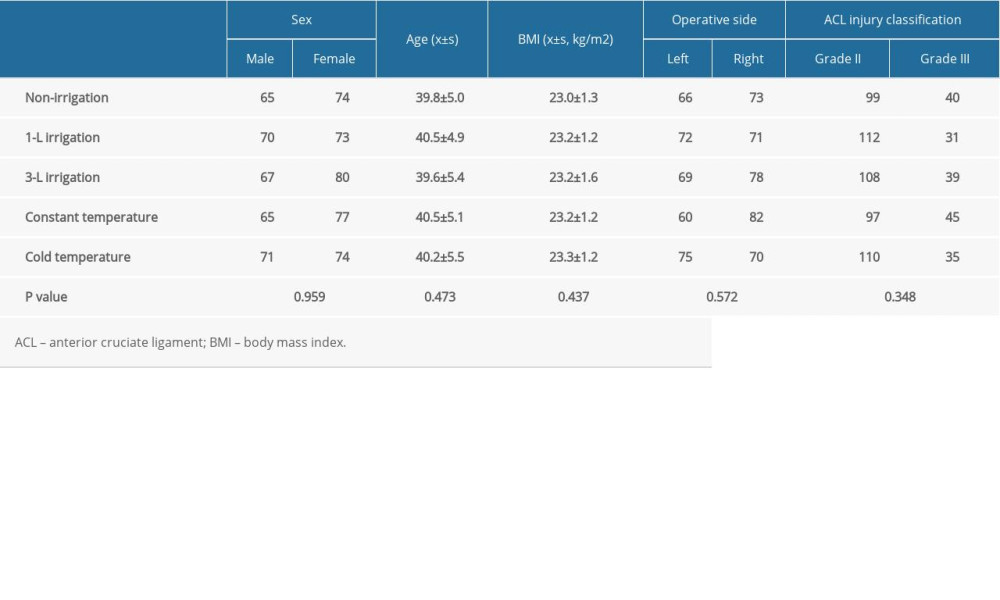 Table 1. Clinical and demographic characteristics of 716 patients after arthroscopic single-bundle surgical reconstruction of the ACL performed under general anesthesia.
Table 1. Clinical and demographic characteristics of 716 patients after arthroscopic single-bundle surgical reconstruction of the ACL performed under general anesthesia. Table 2. Comparison of VAS results in 716 patients after arthroscopic single-bundle surgical reconstruction of the ACL performed under general anesthesia.
Table 2. Comparison of VAS results in 716 patients after arthroscopic single-bundle surgical reconstruction of the ACL performed under general anesthesia.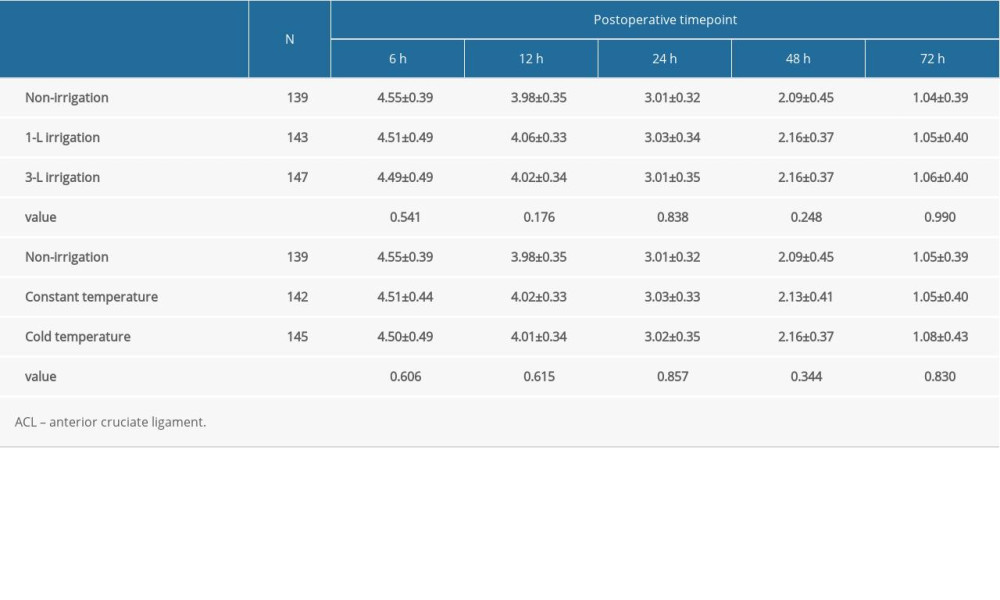 Table 3. Comparison of swelling ratings in 716 patients after arthroscopic single-bundle surgical reconstruction of the ACL performed under general anesthesia.
Table 3. Comparison of swelling ratings in 716 patients after arthroscopic single-bundle surgical reconstruction of the ACL performed under general anesthesia.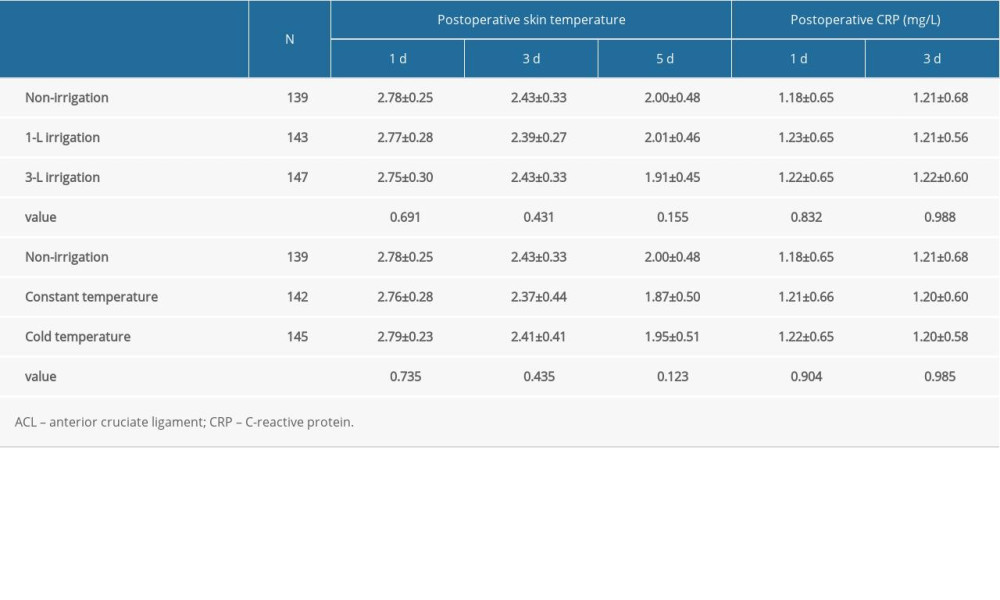 Table 4. Comparison of skin temperature ratings and CRP in 716 patients after arthroscopic single-bundle surgical reconstruction of the ACL performed under general anesthesia.
Table 4. Comparison of skin temperature ratings and CRP in 716 patients after arthroscopic single-bundle surgical reconstruction of the ACL performed under general anesthesia.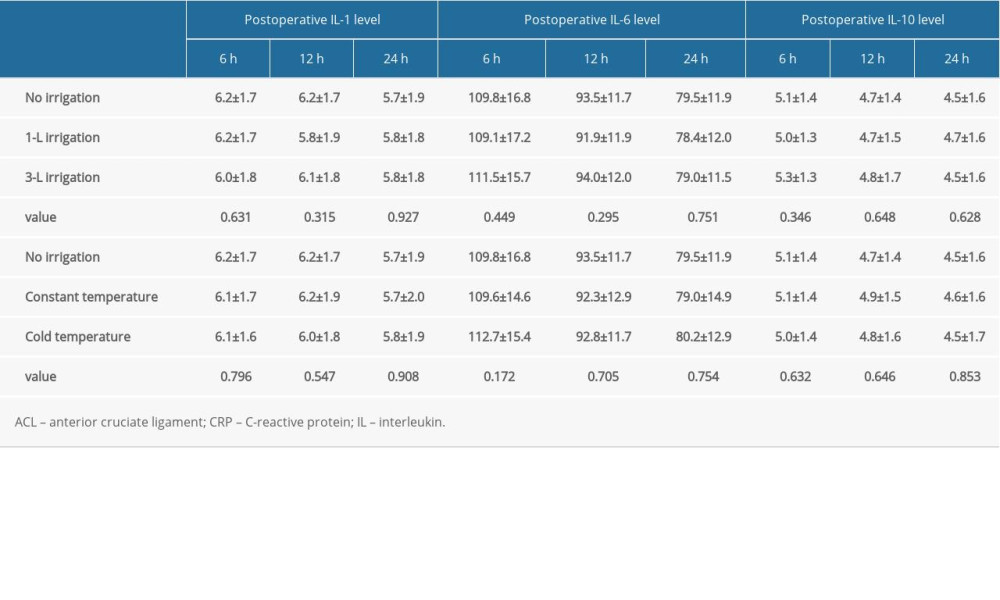 Table 5. Comparison of results with IL-1, IL-6, and IL-10 in 716 patients following arthroscopic single-bundle surgical reconstruction of the ACL performed under general anesthesia.
Table 5. Comparison of results with IL-1, IL-6, and IL-10 in 716 patients following arthroscopic single-bundle surgical reconstruction of the ACL performed under general anesthesia.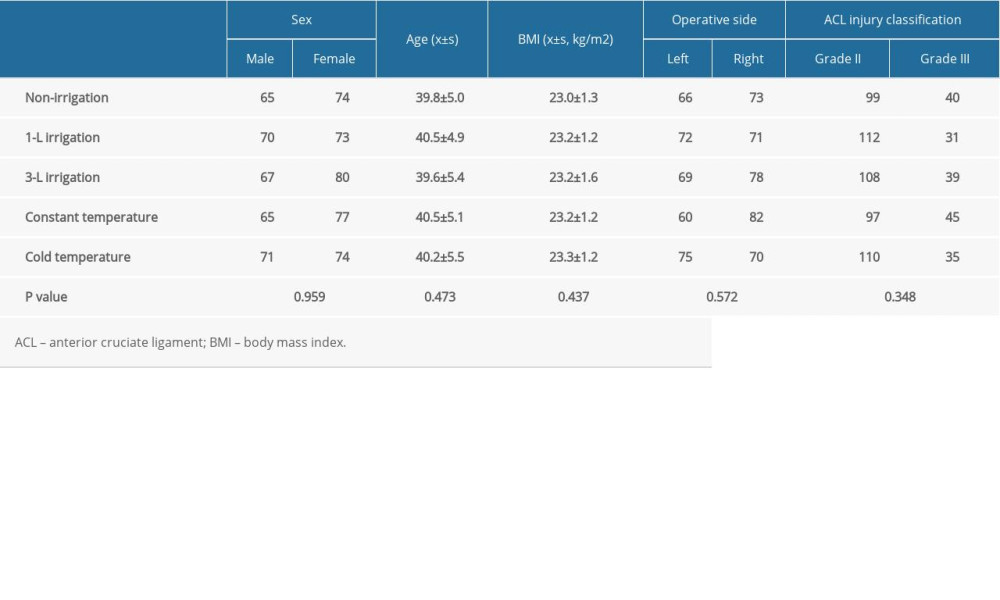 Table 1. Clinical and demographic characteristics of 716 patients after arthroscopic single-bundle surgical reconstruction of the ACL performed under general anesthesia.
Table 1. Clinical and demographic characteristics of 716 patients after arthroscopic single-bundle surgical reconstruction of the ACL performed under general anesthesia. Table 2. Comparison of VAS results in 716 patients after arthroscopic single-bundle surgical reconstruction of the ACL performed under general anesthesia.
Table 2. Comparison of VAS results in 716 patients after arthroscopic single-bundle surgical reconstruction of the ACL performed under general anesthesia.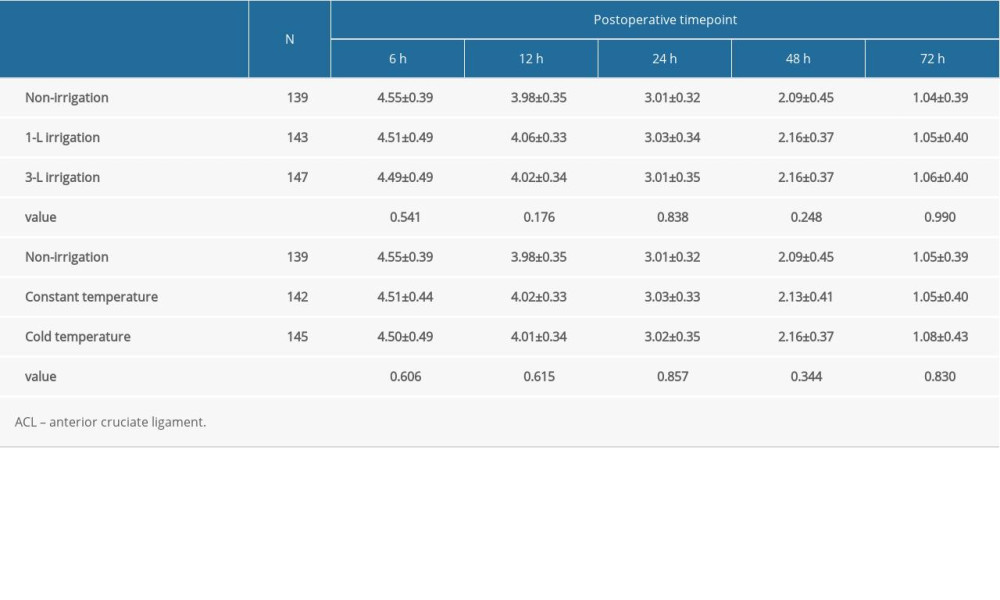 Table 3. Comparison of swelling ratings in 716 patients after arthroscopic single-bundle surgical reconstruction of the ACL performed under general anesthesia.
Table 3. Comparison of swelling ratings in 716 patients after arthroscopic single-bundle surgical reconstruction of the ACL performed under general anesthesia.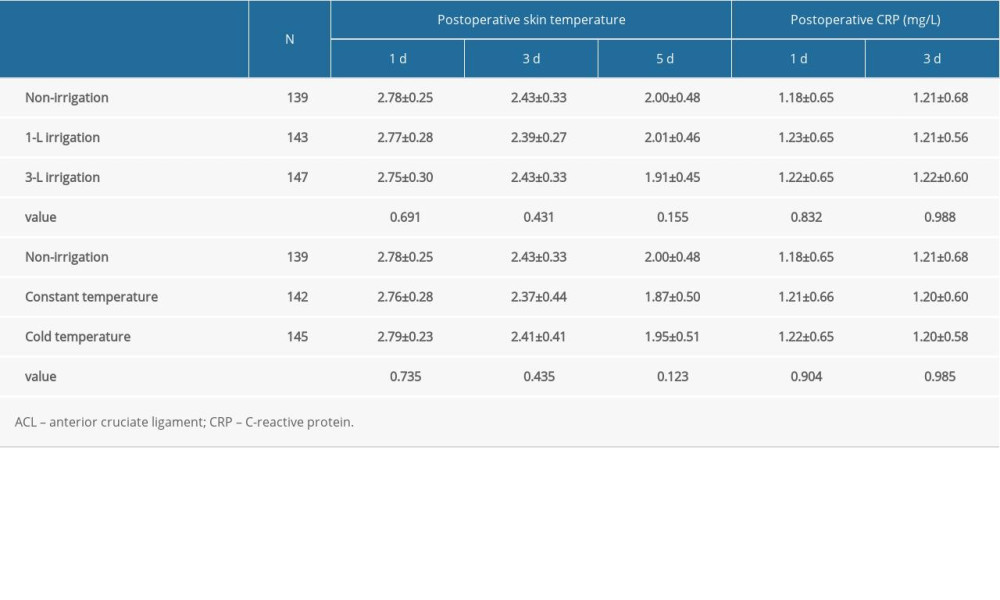 Table 4. Comparison of skin temperature ratings and CRP in 716 patients after arthroscopic single-bundle surgical reconstruction of the ACL performed under general anesthesia.
Table 4. Comparison of skin temperature ratings and CRP in 716 patients after arthroscopic single-bundle surgical reconstruction of the ACL performed under general anesthesia.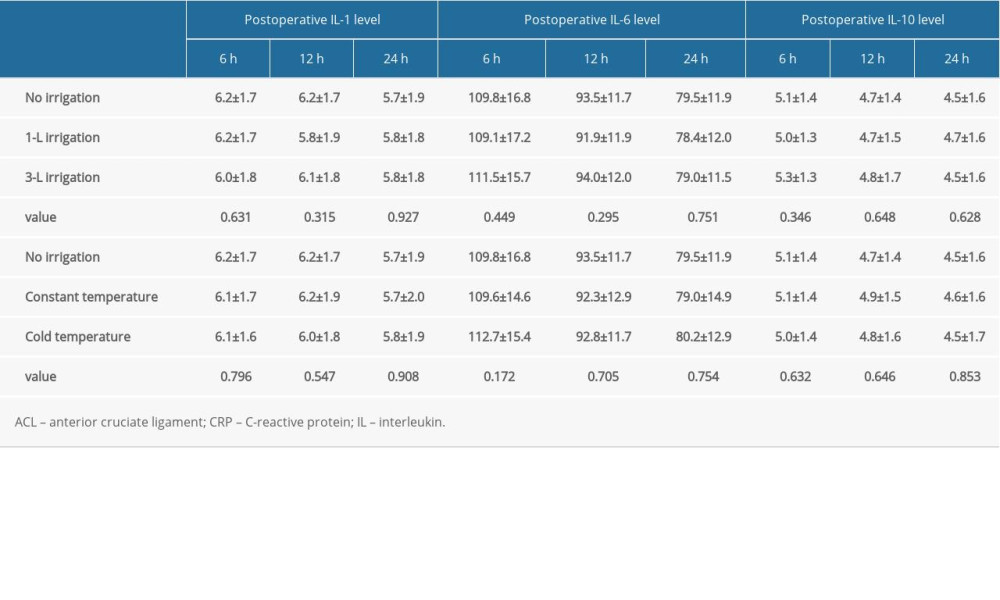 Table 5. Comparison of results with IL-1, IL-6, and IL-10 in 716 patients following arthroscopic single-bundle surgical reconstruction of the ACL performed under general anesthesia.
Table 5. Comparison of results with IL-1, IL-6, and IL-10 in 716 patients following arthroscopic single-bundle surgical reconstruction of the ACL performed under general anesthesia. In Press
05 Mar 2024 : Clinical Research
Role of Critical Shoulder Angle in Degenerative Type Rotator Cuff Tears: A Turkish Cohort StudyMed Sci Monit In Press; DOI: 10.12659/MSM.943703
06 Mar 2024 : Clinical Research
Comparison of Outcomes between Single-Level and Double-Level Corpectomy in Thoracolumbar Reconstruction: A ...Med Sci Monit In Press; DOI: 10.12659/MSM.943797
21 Mar 2024 : Meta-Analysis
Economic Evaluation of COVID-19 Screening Tests and Surveillance Strategies in Low-Income, Middle-Income, a...Med Sci Monit In Press; DOI: 10.12659/MSM.943863
10 Apr 2024 : Clinical Research
Predicting Acute Cardiovascular Complications in COVID-19: Insights from a Specialized Cardiac Referral Dep...Med Sci Monit In Press; DOI: 10.12659/MSM.942612
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952