15 October 2021: Clinical Research
The Serum Metabolomics Study of Liver Failure and Artificial Liver Therapy Intervention
Shipeng Huang1ABC, Dali Hu2BCD, Songsong Yuan3BCD, Ying He3BCD, Chengmu Li3BCD, Ying Zhu3BCD, Xiaoping Wu3AEF*DOI: 10.12659/MSM.930638
Med Sci Monit 2021; 27:e930638
Abstract
BACKGROUND: This study was designed to study the serum metabolites of patients with liver failure.
MATERIAL AND METHODS: The study included 50 patients with liver failure, 30 patients with chronic hepatitis B treated with an artificial liver, 11 patients with an artificial liver, and 32 healthy controls. Clinical data were recorded, and blood samples were analyzed by gas chromatography–mass spectrometry (GC-MS). The random forest algorithm was used to construct a multidimensional scale map to preliminarily reflect the differences between samples. The data were then analyzed to obtain the correlation of different variables among samples, from which the differential metabolites were screened.
RESULTS: Thirty-five metabolites were identified by GC-MS. There were significant differences in serum metabolites levels before and after treatment in the liver failure group and in the chronic hepatitis group, healthy control group, and artificial liver group. Different metabolites were screened according to the importance of different variables among samples. Significant differences were found between the liver failure group, the chronic hepatitis group, and the healthy control group. In addition, there were significant differences in the liver group before and after treatment with an artificial liver, including differences in boric acid, 2-(methoxyamino)-propionic acid, glycine, l-methionine, aminopropionic acid, glyceryl monostearate, cholesterol, and other substances.
CONCLUSIONS: A variety of differences in metabolites were found in each group, some of which revealed possible metabolic pathways leading to differences between groups. Blood metabolomics analysis has great potential in real-time dynamic monitoring of liver failure and evaluation of artificial liver therapy.
Keywords: Liver failure, Liver, Artificial, Metabolomics, Case-Control Studies, Female, Gas Chromatography-Mass Spectrometry, healthy volunteers, Hepatitis B, Chronic, Humans
Background
Liver failure is the main pathological feature of hepatocyte necrosis, which leads to disruption of the various functions of liver, including synthesis, detoxification, secretion, and biogenesis. It may also cause metabolic disorders, which mainly manifest as jaundice, coagulation dysfunction, hepatic encephalopathy, and ascites, among others. Liver failure has many causes, including viral attack, drug toxicity or hepatotoxicity, and genetic and metabolic diseases, among which hepatitis virus infection is prominent [1]. According to the World Health Organization, there are 257 million people infected with chronic hepatitis B virus worldwide, and the incidence of liver failure is increasing annually. Liver failure is a serious public health problem endangering human health [2]. The development of liver failure is a dynamic process, and real-time monitoring of the patient’s condition is very important [3]. An artificial liver system is one of the most important methods for the treatment of patients with liver failure [4]. It removes toxic metabolites from the patients’ blood and partially replaces the metabolic and synthetic functions of the liver, allowing time for liver regeneration and saving the life of patients with liver failure [5].
At present, the diagnosis of liver diseases is mainly based on histological or clinical and imaging results, but these methods are often invasive and lack specificity and sensitivity. The use of new technologies and noninvasive diagnostic methods can overcome these limitations and contribute to the early diagnosis of liver diseases. Metabolomics has great potential in identifying biomarkers for the evaluation of metabolites in biological systems, and as the field develops, its advantages are becoming increasingly prominent in medical research. Ikeda et al [6] detected 60 classes of metabolites in the serum based on gas chromatography-mass spectrometry (GC-MS) techniques. They found that the abundance of 18 classes of metabolites was significantly altered in patients with pancreatic cancer compared with healthy controls. These metabolites served as markers for the early detection of pancreatic cancer with high sensitivity and specificity [6]. Therefore, the detection of serum metabolic markers can assess human health status and provide early real-time monitoring of the occurrence and development of disease. Metabolomics research has also had some achievements in the field of liver disease. When liver failure occurs, a large number of hepatocytes undergo necrosis. In this situation, protein, sugar, fat, and other components cannot be broken down or utilized normally, which produces a large number of endogenous metabolic abnormalities. In theory, if highly sensitive detection equipment is used for real-time monitoring of the levels of serum metabolites in patients with liver failure, it can provide an effective method for determining accurate treatment opportunities in patients with early liver failure. Nuclear magnetic resonance (NMR) and mass spectrometry (MS) are 2 of the most widely used methods [7,8]. The resonance frequencies emitted by different nuclei absorbing radiation vary, and NMR technology can use this characteristic to obtain molecular, chemical, and structural information on substances for analysis and accurate identification [9]. Mass spectrometry analysis gathers information on the charge mass ratio of ions in electric and magnetic fields, and then separates and detects the charge mass ratio. Compared with NMR methods, accelerator MS has the advantages of high sensitivity, high resolution, and a wider detection range. This detection function can simultaneously detect thousands of metabolites in a large dynamic range. Therefore, MS is the first choice to obtain data on metabolites or to separately identify thousands of metabolites at the same time. MS can be divided into GC-MS, liquid chromatography MS, and capillary electrophoresis MS. Among these 3 methods, GC-MS has the advantages of higher separation efficiency and higher sensitivity. Therefore, the serum metabolites of patients with liver failure were studied by GC-MS. The results were then used to further analyze and verify the serum differential metabolites related to liver failure.
Material and Methods
SAMPLES AND GROUPS:
All patients with liver failure met the diagnostic criteria used at our institution for the diagnosis and treatment of liver failure [1]. Our study included 50 patients with liver failure (liver failure group) and 30 patients with chronic hepatitis B (chronic hepatitis group). Eleven patients with liver failure were first treated with artificial liver and were divided into a separate artificial liver group in our analysis. Artificial liver therapy purifies the blood of patients through extracorporeal circulation to achieve detoxification (elimination of various toxins that accumulate in liver failure), transformation metabolism, and synthesis (eg, supplementation of protein, coagulation factors and other substances, anti-inflammatory substances). The artificial liver treatment mainly includes plasma exchange, selective plasma exchange, bilirubin adsorption, continuous hemodiafiltration, plasma diafiltration, and plasma adsorption dialysis, among other functions. Exclusion criteria for this study were (1) combined A, C, D, and E viral hepatitis; (2) presence of drug-induced, alcoholic, or autoimmune hepatitis; (3) presence of malignancies such as liver cancer; (4) presence of other metabolic diseases such as diabetes mellitus and hyperthyroidism; and (5) pregnancy or lactation. The healthy control group was composed of 32 health examination personnel without a previous medical history. All participants provided informed consent before enrollment.
METHODS OF STUDY:
Venous blood samples were collected from all participants in the morning and centrifuged at 3500 rpm for 5 min. The upper serum was quickly collected and stored at −80°C. The samples were later thawed and detected by GC-MS to determine metabolite profiles for the liver failure, chronic hepatitis, artificial liver, and healthy control groups. Experimental data were collected alongside an internal standard and with the use of quality control. Random forest algorithm (RF) was used to construct a multidimensional scale map to preliminarily show the differences between samples, and then RF was used to analyze the data to determine the importance of different variables among the samples and to screen out different metabolites.
STATISTICAL ANALYSIS:
Data processing and analysis in this study used SPSS 20.0 statistical software. The data of the same group before and after treatment were compared by paired
Results
ANALYSIS OF CLINICAL DATA:
A total of 123 individuals were included in this study: 50 in the liver failure group, 30 in the chronic hepatitis group, 32 in the healthy control group, and 11 in the liver failure artificial liver therapy group. The general and clinical data are shown in Tables 1 and 2. There were no significant differences in age, sex, and other general data across all groups. Laboratory examination: alanine aminotransferase, aspartate aminotransferase, total bilirubin, albumin, and other data and specific differences between groups are as follows.
QUALITATIVE AND QUANTITATIVE ANALYSIS OF METABOLITES IN SERUM SAMPLES:
Serum samples from all participants were underwent an optimized pretreatment method and chromatographic MS. As shown in Figure 1, 35 common peaks were obtained for a more accurate characterization of complex metabolites in serum. We classified these peaks into 3 categories: amino acids, sugars, and fatty acid metabolites. Due to a large number of previous fatty acid studies, the NIST database contains abundant information on the derivatives of fatty acid substances. After derivatization in the mass spectrum database, amino acids and carbohydrates had low matching rates; therefore, assessment was qualitative using 22 alkanes as internal standards and the quantitative results are expressed as the ratio of the metabolite peak area to the internal standard peak area. Table 3 lists the qualitative and quantitative analysis of 35 common chromatographic peaks in the serum of participants in the liver failure, chronic hepatitis, and healthy control groups. Table 4 lists the qualitative and quantitative analysis of 35 chromatographic common peaks in the serum before and after treatment in the artificial liver group versus the liver failure group before treatment.
DIFFERENTIAL METABOLITE ANALYSIS:
RF classification of the 3 groups of serum metabolites and serum metabolites before and after treatment in the artificial liver group, along with the resulting multidimensional scale, is shown in Figure 2. The samples from the liver failure, chronic hepatitis, and healthy groups were clearly distinguished, and the group before and after artificial liver treatment was far away in the 3-dimensional map, indicating that the grouping effect was good. The results showed that the metabolic spectrum of patients with liver failure was significantly different from that of patients with chronic hepatitis and the healthy control group. There were also significant differences in serum metabolites before and after artificial liver therapy in patients with liver failure. The distribution and classification of amino acid, carbohydrate, and fatty acid metabolites in 3 groups of samples and artificial liver samples were systematically analyzed by RF to determine the variable importance of metabolites in each group. As shown in Figure 3A, the main differences in substances in the liver failure group and the healthy group included differences in boric acid, 2-(methoxyamino)-propionic acid, l-threonine, l-methionine, dl-phenylalanine, d-mannose, 1-palmitate monoglyceride, and cholesterol. As shown in Figure 3B, the main differences in substances between the chronic hepatitis group and the healthy group included 2-(methoxyamino)-propionic acid, glycine, aminopropionic acid, and glycerol monostearate. Before and after artificial liver treatment, there were significant differences in the group as shown in Figure 3C, including boric acid, 2-(methoxyamino)-propionic acid, glycine, l-methionine, aminomalonic acid, glycerol monostearate, and cholesterol.
Discussion
Based on the GC-MS technique, the metabolic profiles of patients with liver failure and chronic hepatitis group and individuals in a healthy control group were analyzed. The trend of sample grouping in the RF map was good and could effectively distinguish the samples between groups. Further RF multivariate analysis of metabolomics data suggested that there were many different metabolites in the liver failure group, the chronic hepatitis group, and the healthy control group. We also analyzed the changes in spectrum before and after artificial liver treatment in patients with liver failure and identified differential metabolites. These substances have different biological functions due to their different metabolic pathways, but they may be biomarkers related to the degree of liver injury. In comparison with reference materials, fatty acids and their derivatives can be identified by comparison with mass spectrometry.
The abundance of glycine was significantly different between the liver failure group, the chronic hepatitis group, and the healthy group, with the liver failure group having the lowest amounts. Glycine is widely present in the body, and its biological effects are mainly broad-spectrum anti-inflammatory, liver protection, cell protection, improving blood perfusion, and immune regulation. Glycine is also involved in the metabolism of proteins, nucleotides, porphyrins, and bile acids. Animal experiments have shown that glycine biometabolism is complex and diverse and plays an important therapeutic role in many diseases [10]. It may act on glycine-gated Cl− channels on inflammatory cells such as (leukocytes and macrophages); regulate the production of Ca2+, peroxides, and oxygen free radicals in inflammatory cells; correct immune dysfunction; and play a protective role in the liver. Glycine can also play a protective role in ischemia and reperfusion injury [11]. Glycine content in patients with liver failure was significantly decreased, which may be related to protective consumption and synthesis disorders. In vivo glycine synthesis requires serine hydroxyltransferase catalysis, which is mainly found in liver and kidney cells. Therefore, it is speculated that due to the large area of hepatocyte necrosis, the decrease of transferase and the weakening of catalytic effect, the synthesis of glycine in hepatocytes is reduced. In addition, the body’s own protective consumption may have caused the serum glycine content in patients with liver failure to be much lower than that in the chronic hepatitis group and the healthy group. Compared with the healthy control group, the liver cells of the chronic hepatitis group were slightly damaged and the normal liver cells compensated with increased synthesis of glycine, resulting in a higher glycine content. Therefore, a change in the glycine level in patients with liver disease could predict the evolution of the disease.
Another characteristic protein found in this study was l-methionine, which is the only sulfur-containing amino acid among the essential amino acids. It plays a decisive role in the process of metabolism and maintains the nitrogen balance in the body. Methionine also promotes intrahepatic fat metabolism, and it is used clinically for the prevention and treatment of fatty liver and chronic hepatitis [12]. Methionine and its derivatives can effectively protect the liver from damage through an antioxidant effect and have a therapeutic and protective effect on the liver. There was no significant difference between methionine levels in the chronic hepatitis group and the healthy group. The content of methionine in serum metabolites of the liver failure group was higher than that of the chronic hepatitis group and the healthy group. The possible reason is that S-adenosylmethionine, as a substrate, regenerates methionine in patients with liver failure through the methionine rescue pathway, resulting in an increase of methionine content in patients with liver failure.
This study showed that the abundance of phenylalanine in serum metabolites was significantly higher in patients with liver failure than in healthy people, which may be related to an imbalance of intestinal flora, a decrease in phenylalanine conversion ability, or an accumulation of phenylalanine in serum. In a comparison of the hepatitis group and the control group, there was no difference in the classification of phenylalanine owing to mild liver injury and normal intestinal flora. Increased concentrations of phenylalanine are commonly found in liver diseases, such as hepatic cirrhosis [13]. In patients with hepatic encephalopathy, an inverse correlation between arterial phenylalanine levels and the residual liver volume was observed following hepatectomy, suggesting that phenylalanine may play a causal role in the pathogenesis of this disease [14]. It has also been found that when phenylalanine reaches a certain concentration, it will seriously affect the blood-brain barrier transport of neutral amino acids and restrict the entry of other large neutral amino acids into the brain [15], thus inducing hepatic encephalopathy. Therefore, the abnormal increase of phenylalanine in patients with liver failure indicates an increased risk of hepatic encephalopathy.
Conclusions
Early diagnosis, accurate assessment, and timely treatment are very important for patients with liver failure. In clinical practice, the diagnosis of liver failure is based on hyperbilirubinemia and prolonged coagulation time, but these 2 indicators cannot fully reflect liver function, which is of great significance for the early diagnosis of liver failure. Through the study of blood metabolomics in a liver failure group, a chronic hepatitis group, a healthy control group, and an artificial liver group, we found that there were many differences in metabolites such as glycine, l-methionine, and phenylalanine, and the possible metabolic pathways leading to these differences were revealed. At the same time, the changes of metabolomics were used to dynamically monitor liver failure and evaluate the therapeutic effect of artificial liver. However, many problems in this study need to be addressed, including the small sample size of the artificial liver group, the lack of specificity of most substances detected, and the lack of metabolic pathways of many substances. Therefore, it is necessary to expand the sample for further research. In addition, blood metabolomics analysis for the diagnosis and treatment of liver failure also needs more theoretical basis and clinical research to support the implementation.
Figures
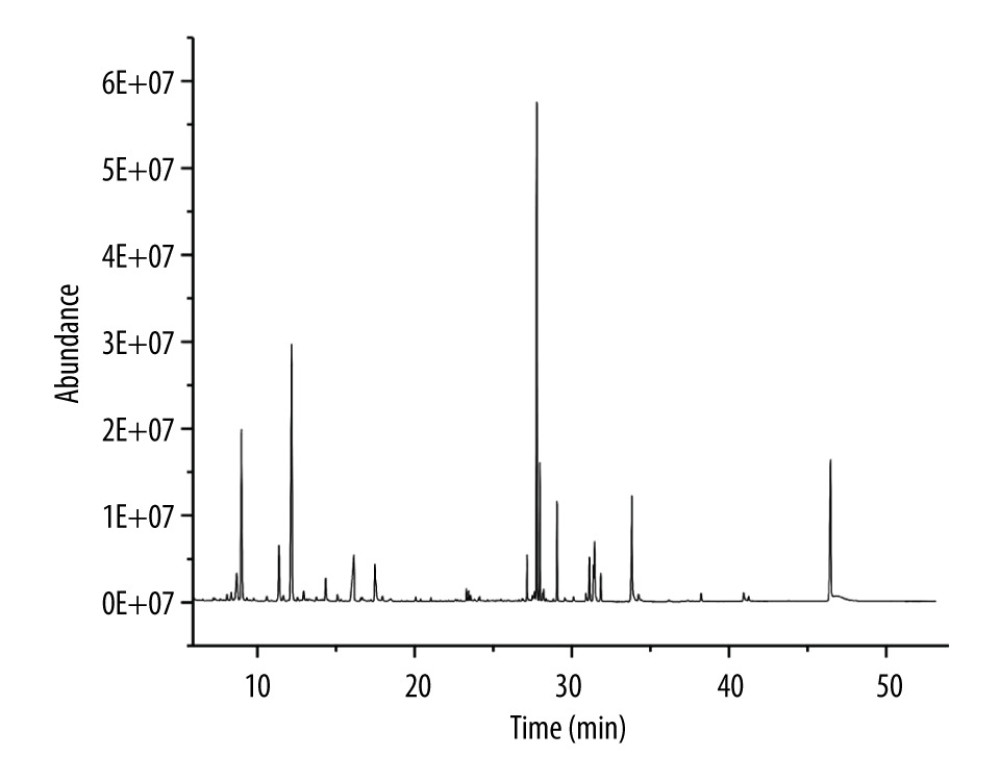 Figure 1. Chromatographic analysis of serum gas chromatography-mass spectrometry in liver failure.
Figure 1. Chromatographic analysis of serum gas chromatography-mass spectrometry in liver failure. 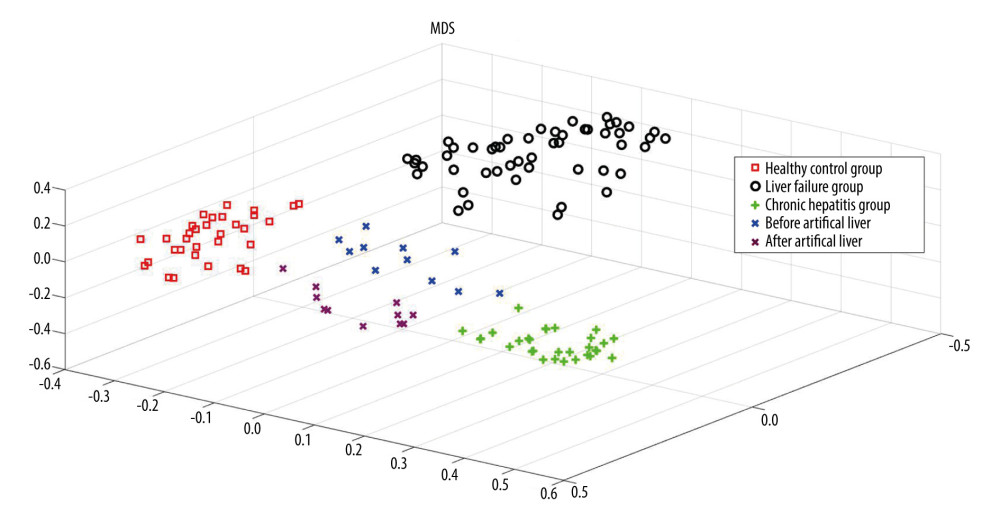 Figure 2. Multidimensional scaling of each control group.
Figure 2. Multidimensional scaling of each control group. 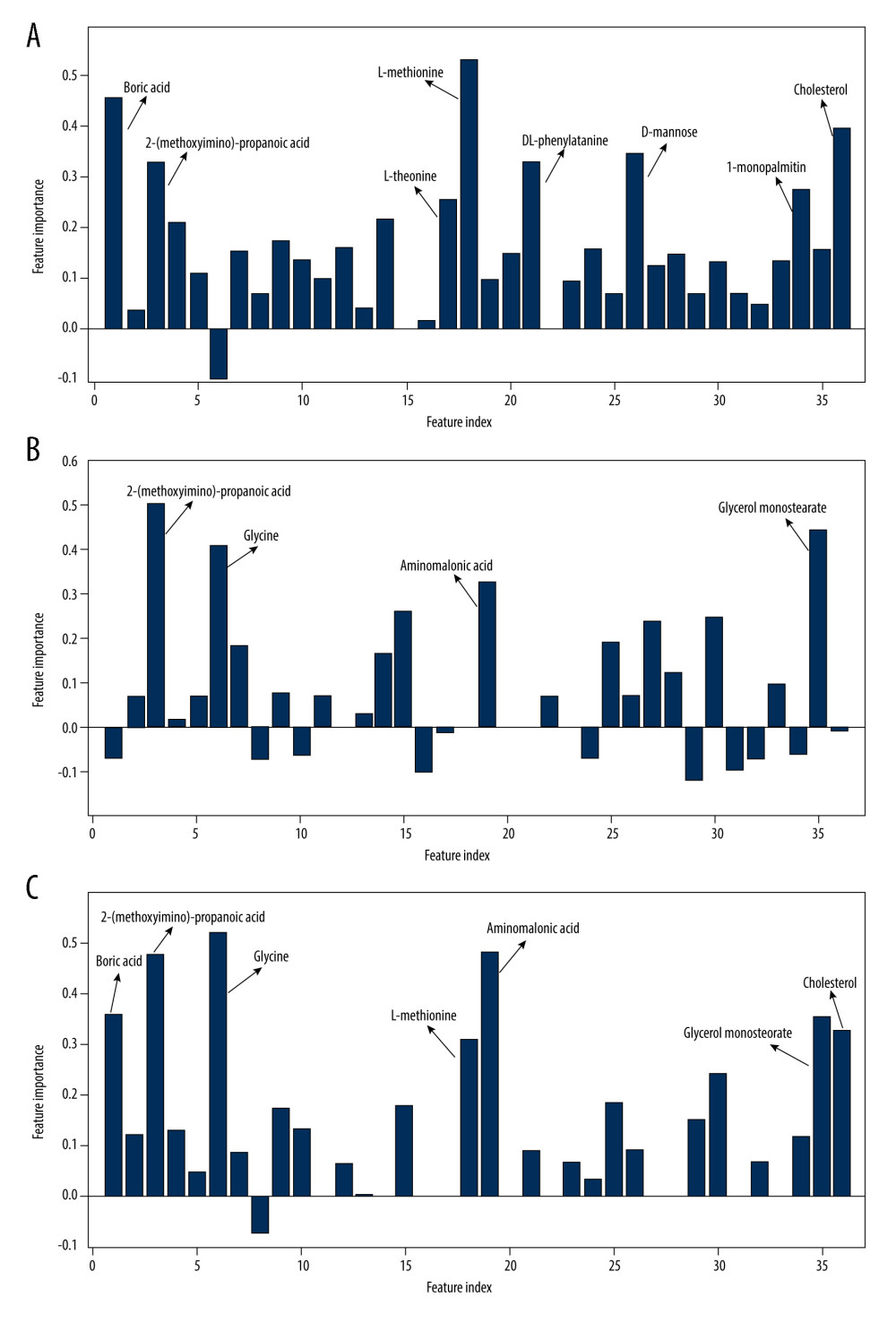 Figure 3. Importance of variables in each group. (A) The main different substances in the liver failure group and the healthy group; (B) the main different substances between the chronic hepatitis group and the healthy group; (C) the main different substances before and after artificial liver treatment.
Figure 3. Importance of variables in each group. (A) The main different substances in the liver failure group and the healthy group; (B) the main different substances between the chronic hepatitis group and the healthy group; (C) the main different substances before and after artificial liver treatment. Tables
Table 1. General data and clinical characteristics of the patients.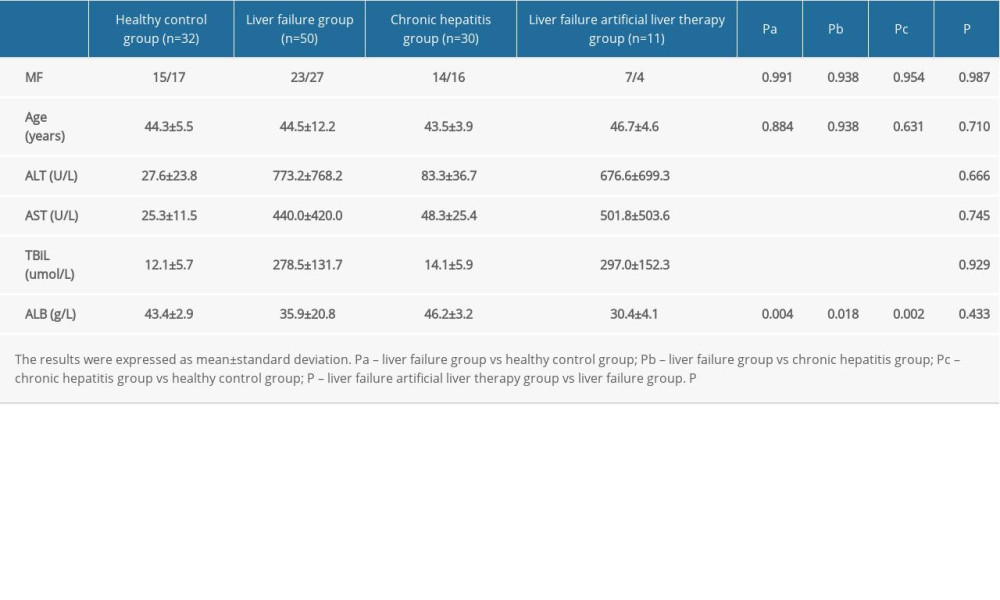 Table 2. Comparison of laboratory data of patients with liver failure before and after artificial liver treatment.
Table 2. Comparison of laboratory data of patients with liver failure before and after artificial liver treatment.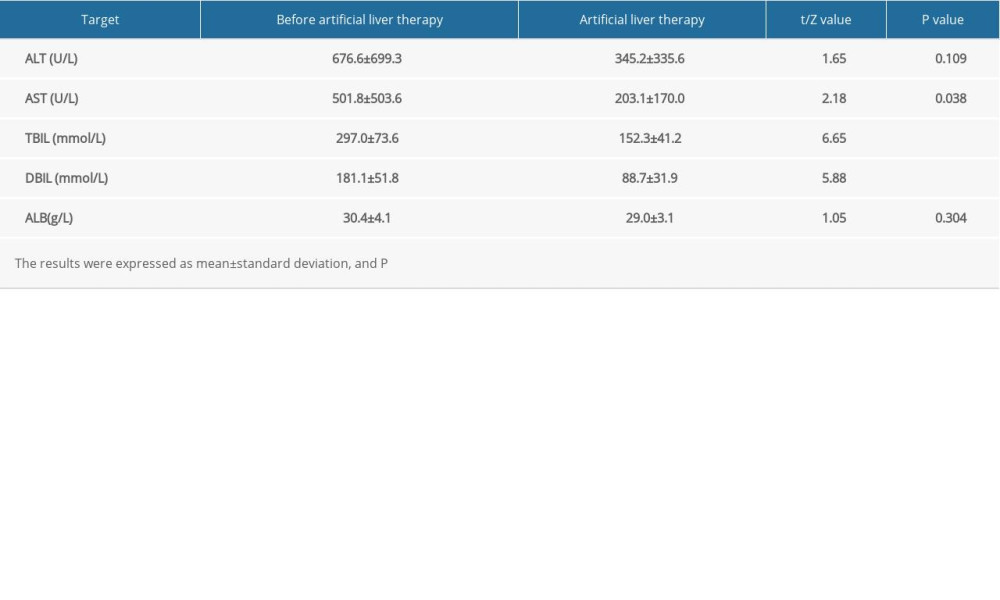 Table 3. Qualitative and quantitative analysis of 35 chromatographic peaks in serum from the liver failure group and chronic hepatitis groups and from the healthy control group.
Table 3. Qualitative and quantitative analysis of 35 chromatographic peaks in serum from the liver failure group and chronic hepatitis groups and from the healthy control group.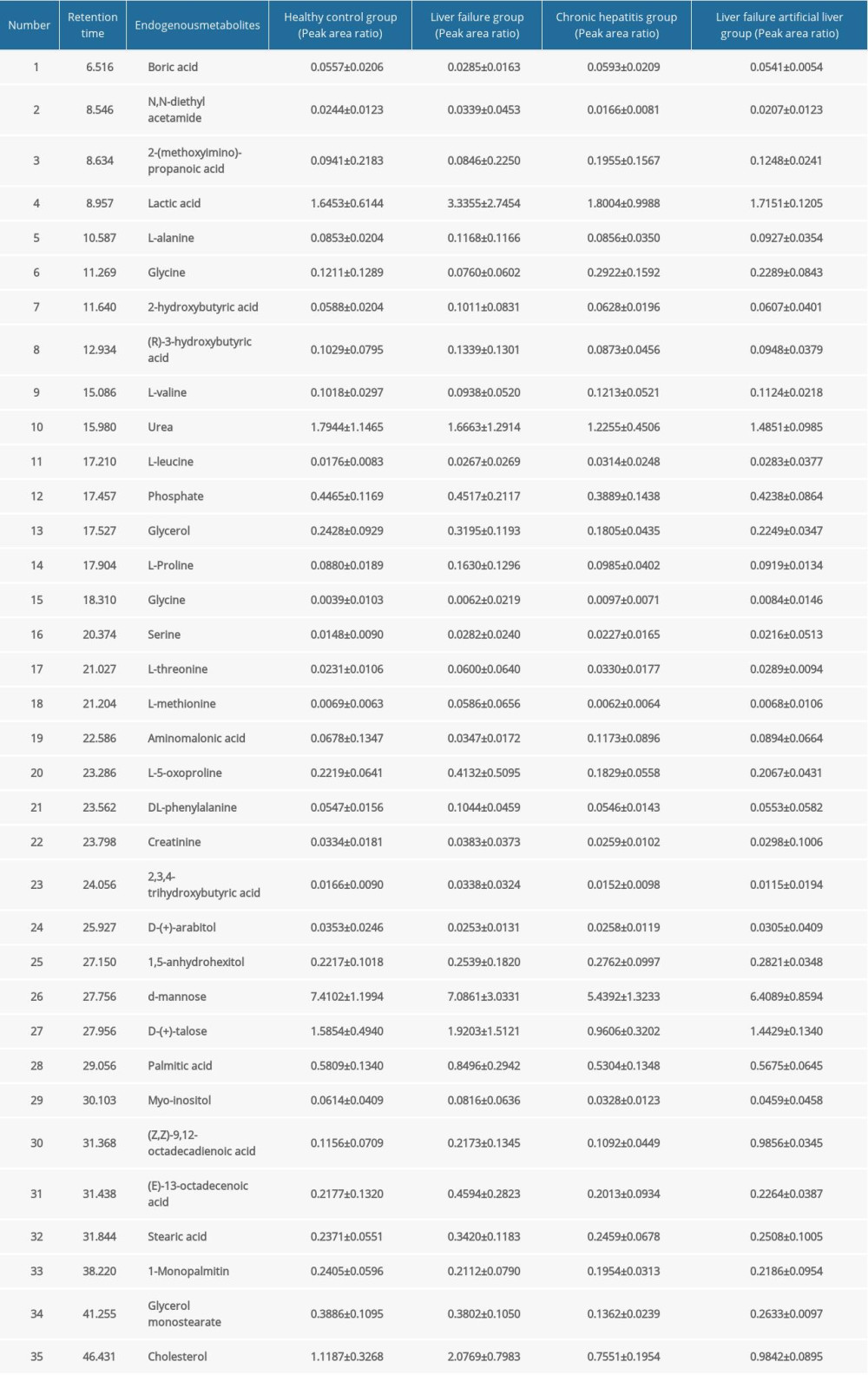 Table 4. Qualitative and quantitative analysis of 35 common chromatographic peaks in serum before and after treatment in the artificial liver group.
Table 4. Qualitative and quantitative analysis of 35 common chromatographic peaks in serum before and after treatment in the artificial liver group.
References
1. Guidelines for diagnosis and treatment of liver failure (2018 edition): Chin J Infect Dis, 2019; 37(1); 1-9 [in Chinese]
2. Wang G, Wang F, Zhuang HGuidelines for the prevention and treatment of chronic hepatitis B (2019 edition): Chin J Viral Dis, 2020; 10(1); 5-29 [in Chinese]
3. Han T, Zhang Y, Predictive and prognostic evaluation of hepatitis B virus-induced liver failure: J Clin Hepatol, 2015; 31(4); 505-9
4. Wang X, Wang H, Zuo D, Huang GProgress in the application of metabolomics and its analytical techniques in medical research: Chinese Modern Doctor, 2019; 57(1); 171-75 [in Chinese]
5. Tandon R, Froghi S, Artificial liver support systems: J Gastroenterol Hepatol, 2021; 36(5); 1164-79
6. Ikeda A, Nishiumi S, Shinohara M, Serum metabolomics as a novel diagnostic approach for gastrointestinal cancer: Biomed Chromatogr, 2012; 26(5); 548-58
7. Au A, Cheng KK, Wei LK, Metabolomics, lipidomics and pharmacometabolomics of human hypertension: Adv Exp Med Biol, 2017; 956; 599-613
8. Emwas AH, The strengths and weaknesses of NMR spectroscopy and mass spectrometry with particular focus on metabolomics research: Methods Mol Biol, 2015; 1277; 161-93
9. Bothwell JH, Griffin JL, An introduction to biological nuclear magnetic resonance spectroscopy: Biol Rev Camb Philos Soc, 2011; 86(2); 493-510
10. Wu G, Functional amino acids in growth, reproduction, and health: Adv Nutr, 2010; 1(1); 31-37
11. Petrat F, Boengler K, Schulz R, de Groot H, Glycine, a simple physiological compound protecting by yet puzzling mechanism(s) against ischaemia-reperfusion injury: Current knowledge: Br J Pharmacol, 2012; 165(7); 2059-72
12. Zhang C, Comparative study on the efficacy of different doses of adenosylmethionine in the treatment of viral hepatitis: China Modern Medicine Application, 2015; 9(24); 134-35
13. Tessari P, Kiwanuka E, Vettore M, Phenylalanine and tyrosine kinetics in compensated liver cirrhosis: Effects of meal ingestion: Am J Physiol Gastrointest Liver Physiol, 2008; 295(3); G598-604
14. Dejong CH, van de Poll MC, Soeters PB, Aromatic amino acid metabolism during liver failure: J Nutr, 2007; 137(6 Suppl 1); 1579S-85S discussion 1597S–98S
15. van Spronsen FJ, Hoeksma M, Reijngoud DJ, Brain dysfunction in phenylketonuria: Is phenylalanine toxicity the only possible cause?: J Inherit Metab Dis, 2009; 32(1); 46-51
Figures
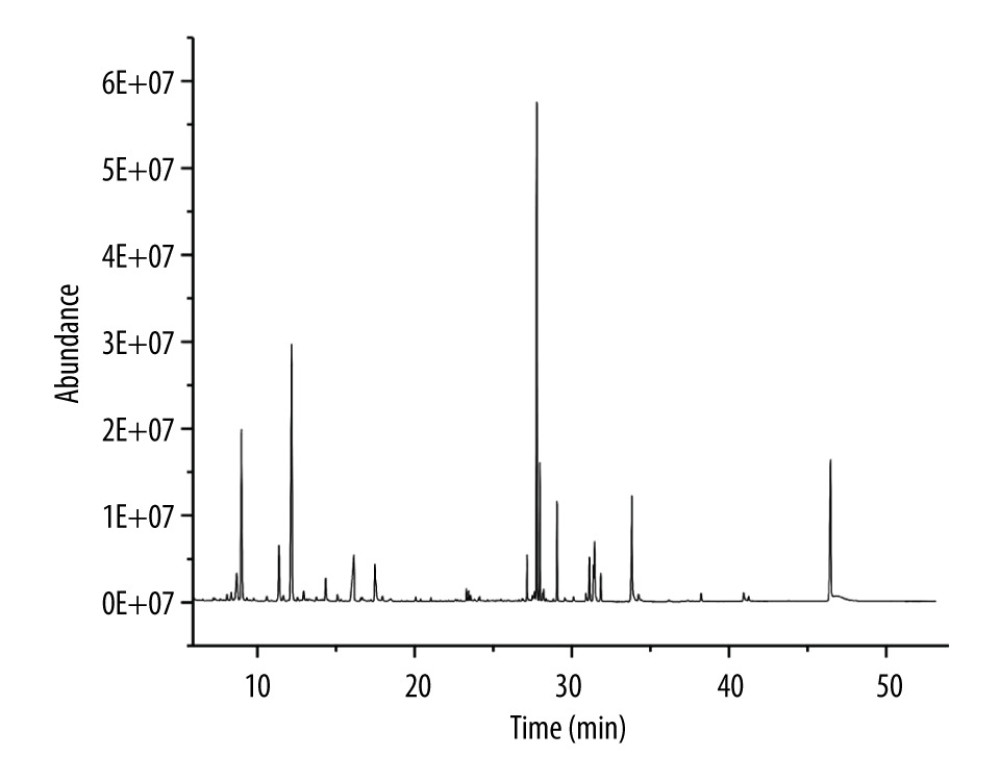 Figure 1. Chromatographic analysis of serum gas chromatography-mass spectrometry in liver failure.
Figure 1. Chromatographic analysis of serum gas chromatography-mass spectrometry in liver failure.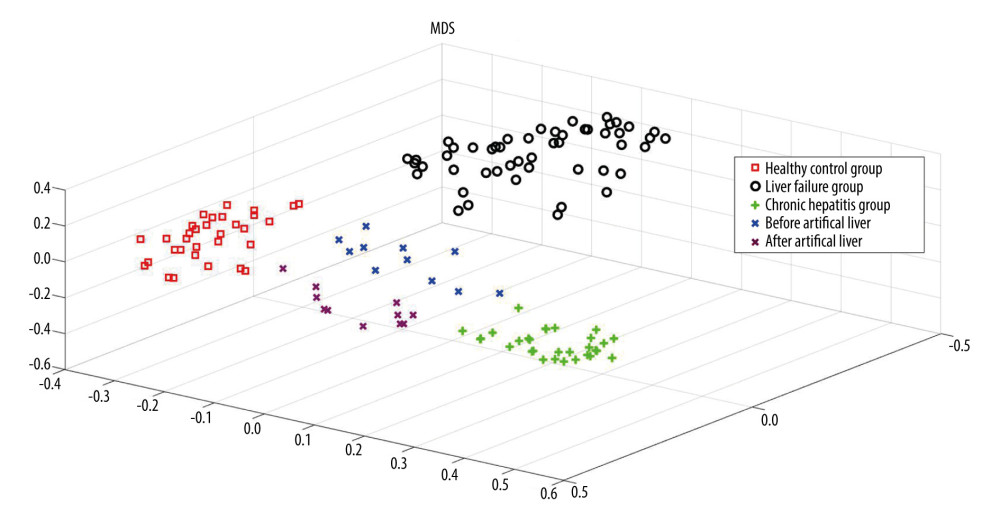 Figure 2. Multidimensional scaling of each control group.
Figure 2. Multidimensional scaling of each control group.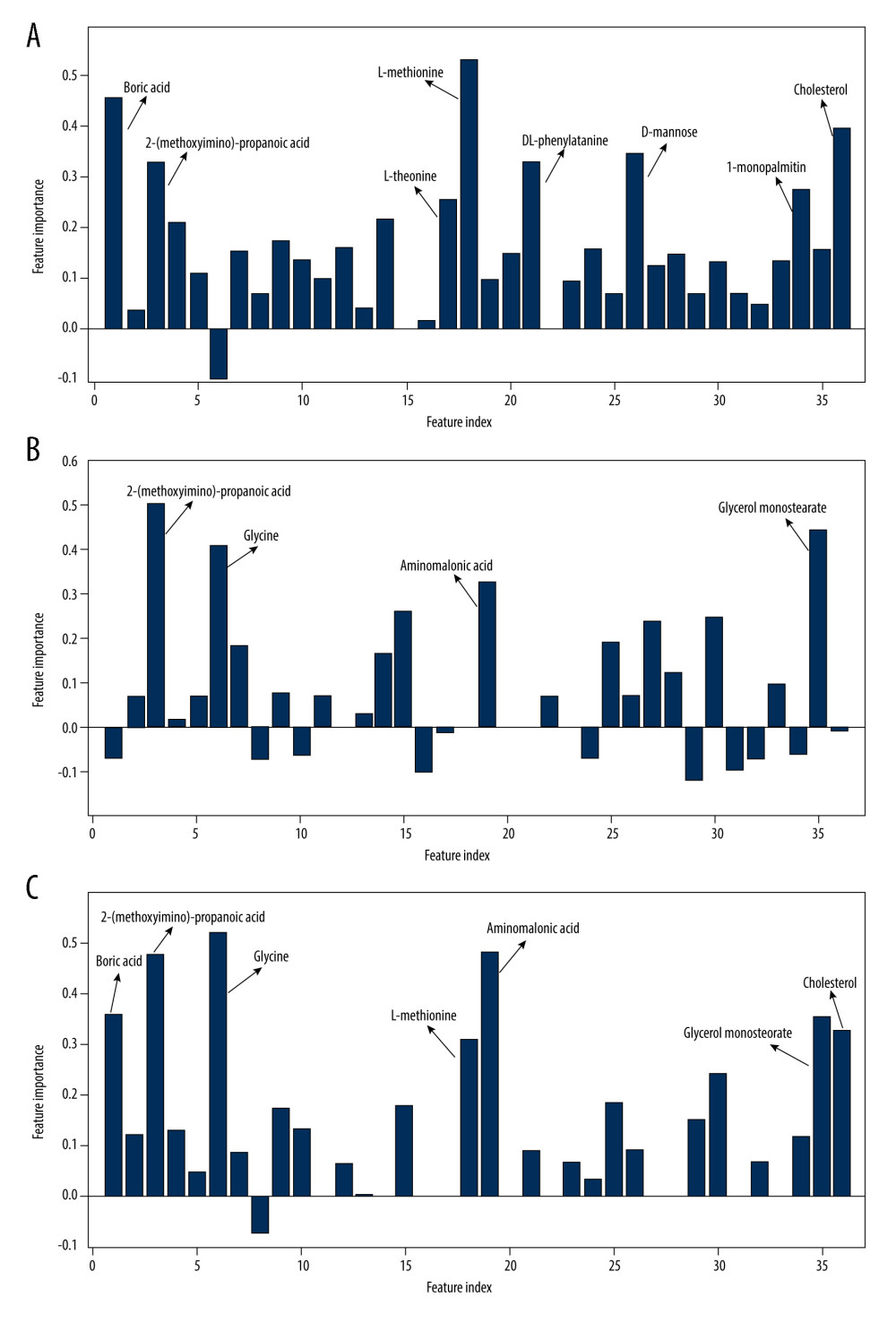 Figure 3. Importance of variables in each group. (A) The main different substances in the liver failure group and the healthy group; (B) the main different substances between the chronic hepatitis group and the healthy group; (C) the main different substances before and after artificial liver treatment.
Figure 3. Importance of variables in each group. (A) The main different substances in the liver failure group and the healthy group; (B) the main different substances between the chronic hepatitis group and the healthy group; (C) the main different substances before and after artificial liver treatment. Tables
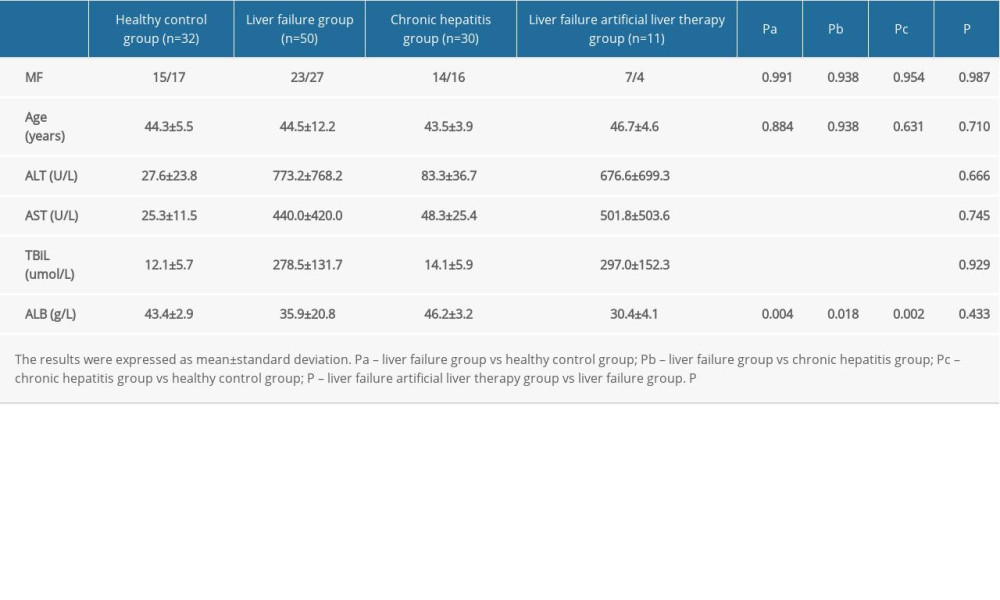 Table 1. General data and clinical characteristics of the patients.
Table 1. General data and clinical characteristics of the patients.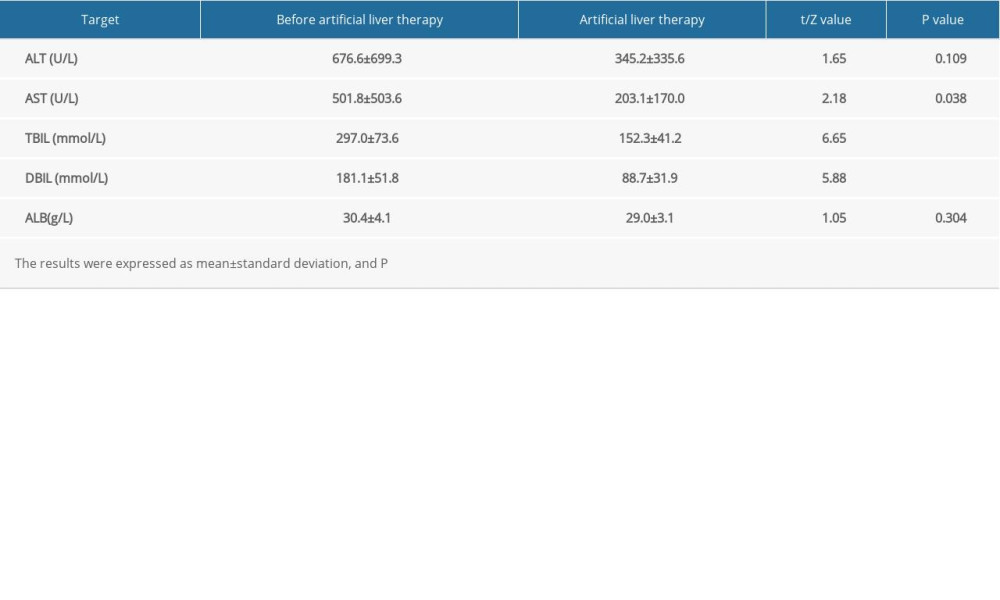 Table 2. Comparison of laboratory data of patients with liver failure before and after artificial liver treatment.
Table 2. Comparison of laboratory data of patients with liver failure before and after artificial liver treatment.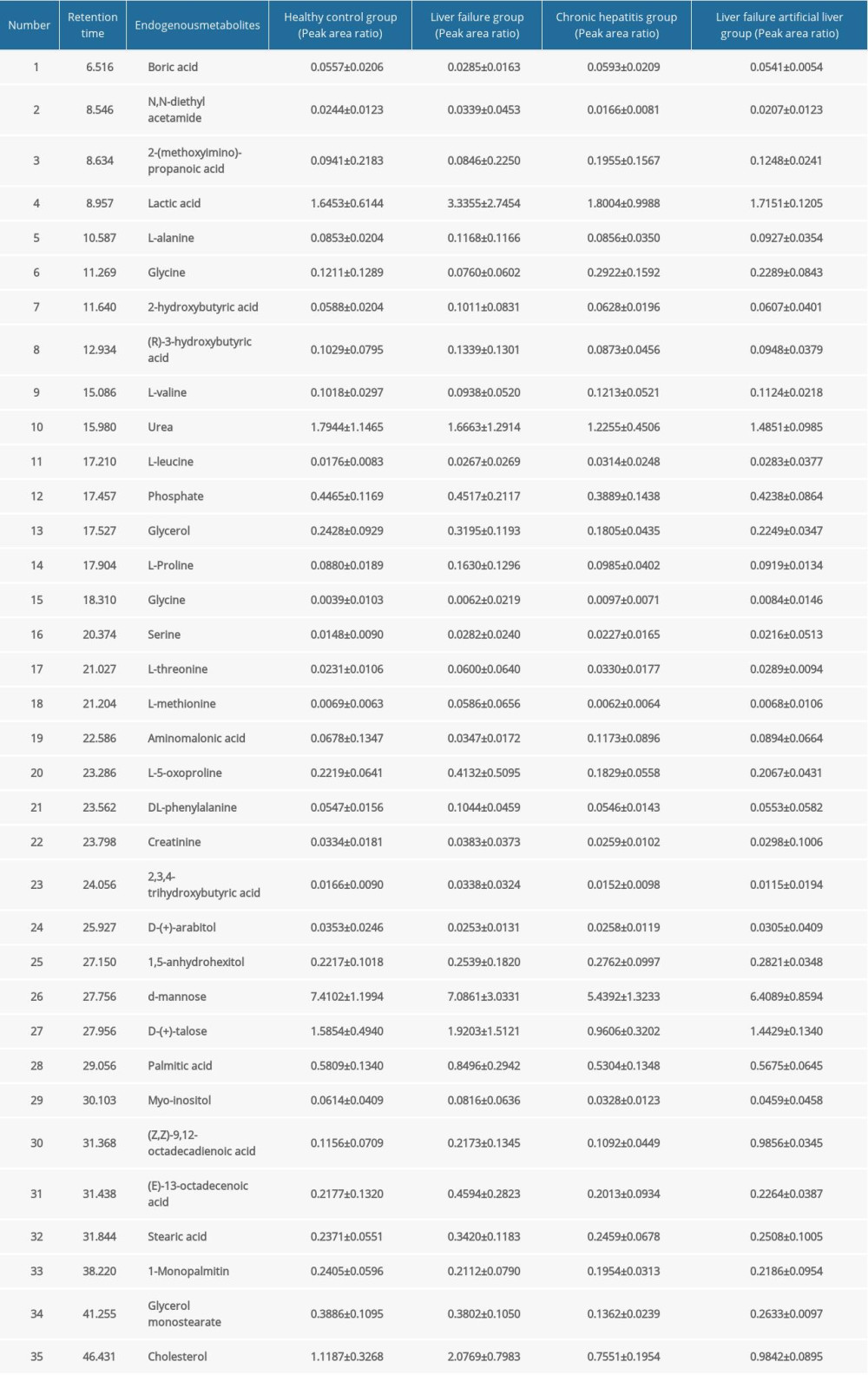 Table 3. Qualitative and quantitative analysis of 35 chromatographic peaks in serum from the liver failure group and chronic hepatitis groups and from the healthy control group.
Table 3. Qualitative and quantitative analysis of 35 chromatographic peaks in serum from the liver failure group and chronic hepatitis groups and from the healthy control group. Table 4. Qualitative and quantitative analysis of 35 common chromatographic peaks in serum before and after treatment in the artificial liver group.
Table 4. Qualitative and quantitative analysis of 35 common chromatographic peaks in serum before and after treatment in the artificial liver group.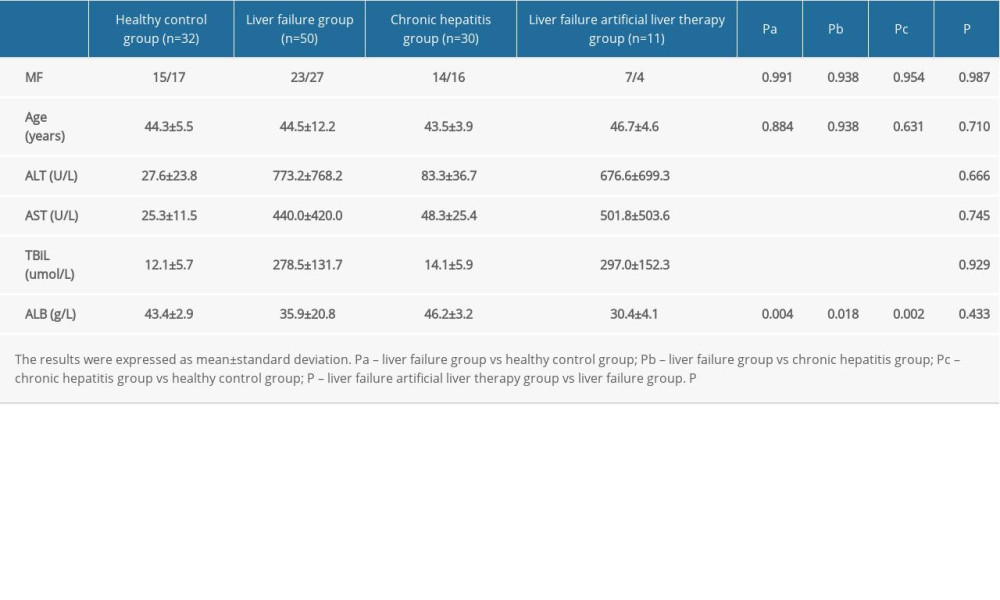 Table 1. General data and clinical characteristics of the patients.
Table 1. General data and clinical characteristics of the patients.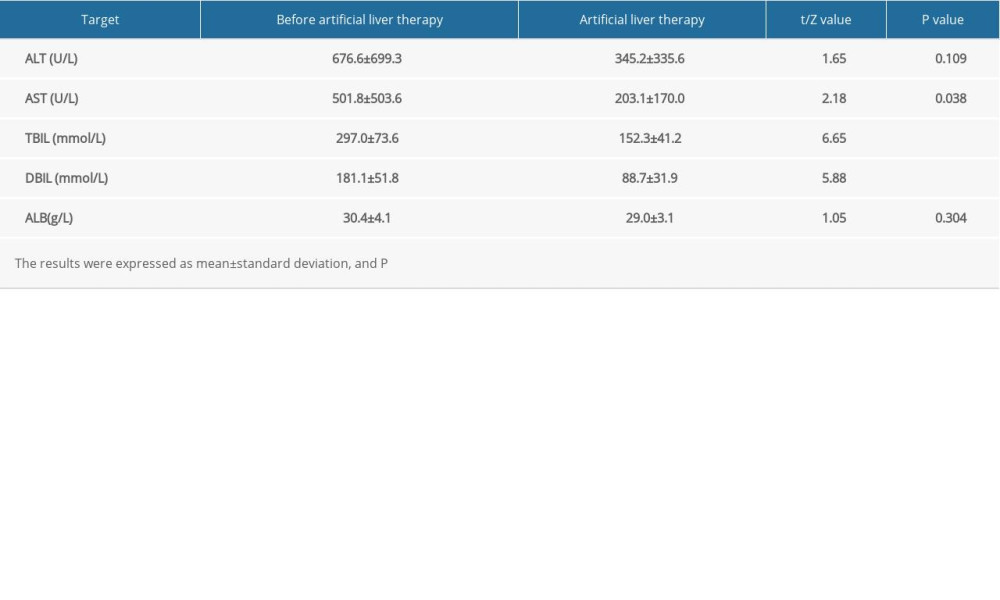 Table 2. Comparison of laboratory data of patients with liver failure before and after artificial liver treatment.
Table 2. Comparison of laboratory data of patients with liver failure before and after artificial liver treatment.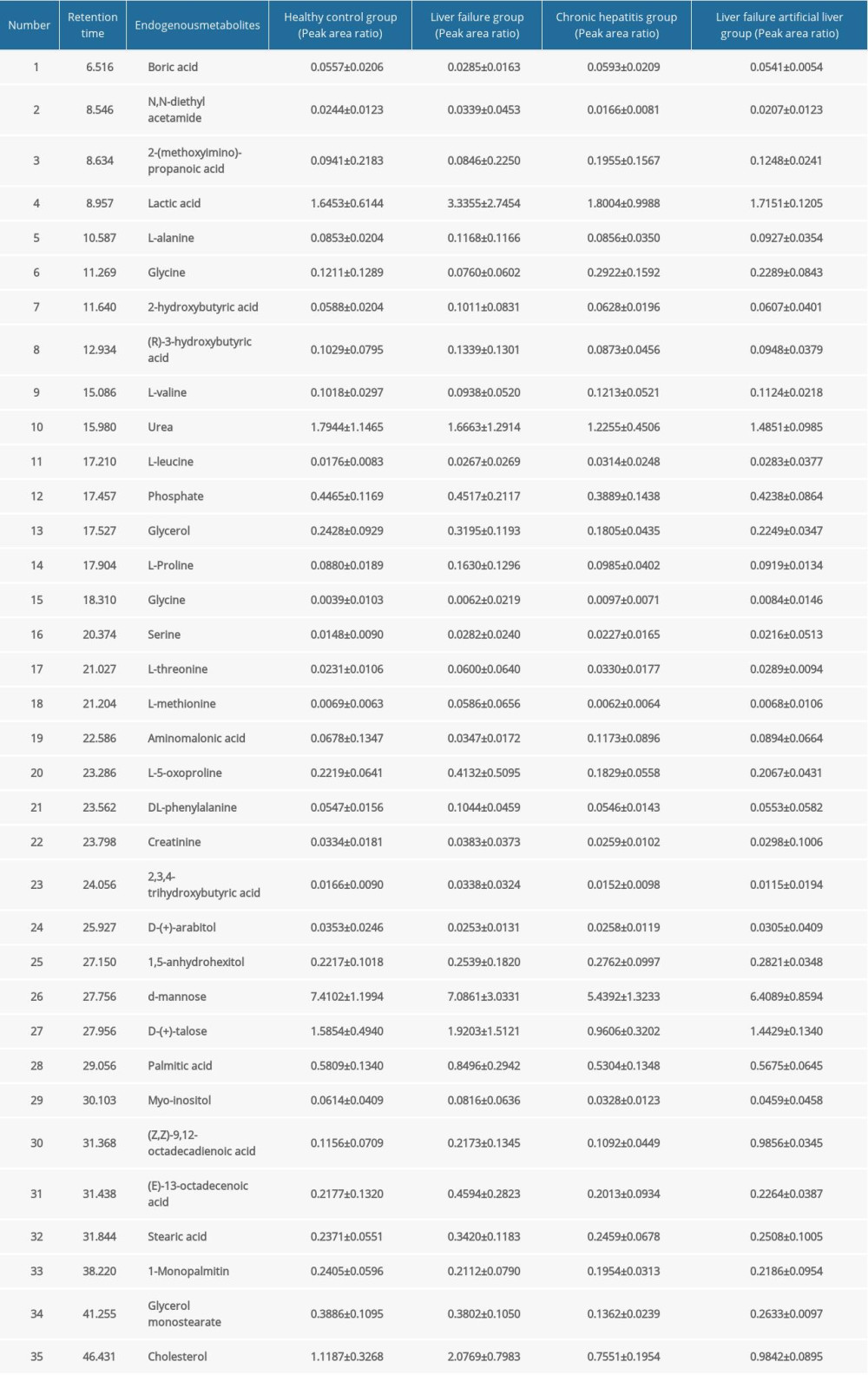 Table 3. Qualitative and quantitative analysis of 35 chromatographic peaks in serum from the liver failure group and chronic hepatitis groups and from the healthy control group.
Table 3. Qualitative and quantitative analysis of 35 chromatographic peaks in serum from the liver failure group and chronic hepatitis groups and from the healthy control group. Table 4. Qualitative and quantitative analysis of 35 common chromatographic peaks in serum before and after treatment in the artificial liver group.
Table 4. Qualitative and quantitative analysis of 35 common chromatographic peaks in serum before and after treatment in the artificial liver group. In Press
06 Mar 2024 : Clinical Research
Comparison of Outcomes between Single-Level and Double-Level Corpectomy in Thoracolumbar Reconstruction: A ...Med Sci Monit In Press; DOI: 10.12659/MSM.943797
21 Mar 2024 : Meta-Analysis
Economic Evaluation of COVID-19 Screening Tests and Surveillance Strategies in Low-Income, Middle-Income, a...Med Sci Monit In Press; DOI: 10.12659/MSM.943863
10 Apr 2024 : Clinical Research
Predicting Acute Cardiovascular Complications in COVID-19: Insights from a Specialized Cardiac Referral Dep...Med Sci Monit In Press; DOI: 10.12659/MSM.942612
06 Mar 2024 : Clinical Research
Enhanced Surgical Outcomes of Popliteal Cyst Excision: A Retrospective Study Comparing Arthroscopic Debride...Med Sci Monit In Press; DOI: 10.12659/MSM.941102
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








