17 September 2021: Clinical Research
Factors Associated with Recurrence of Hepatocellular Carcinoma in 197 Patients Following Transarterial Chemoembolization: A Retrospective Study from a Single Center
Hongsheng Zhang1ABCE*, Xiaodong Zhao2AEF, Wenhai Yu1BCDOI: 10.12659/MSM.929879
Med Sci Monit 2021; 27:e929879
Abstract
BACKGROUND: Hepatocellular carcinoma (HCC) is the second leading cause of cancer deaths. Transarterial chemoembolization (TACE) has been widely applied for treating patients with unresectable HCC. This study explored the factors influencing early recurrence (ER) after TACE in HCC patients.
MATERIAL AND METHODS: A total of 197 patients were divided into the ER group and the non-ER group. Univariate and multivariate Cox regression analyses were carried out to explore the influencing factors. Univariate Kaplan-Meier survival curves and restricted cubic splines were plotted for visualizing the relations between the influencing factors and ER.
RESULTS: According to the multivariate analysis, for every 1-cm increase in the maximum tumor diameter, the risk of ER increased by 0.235 times (95% CI: 1.144-1.333, P<0.001). Patients with adjacent lobe invasion had a 1.227-fold higher risk of ER than those without (95% CI: 1.461-3.394, P<0.001). For every unit increase in neutrophil-to-lymphocyte ratio (NLR), the risk increased by 0.107-fold (95% CI: 1.012-1.211, P=0.027). Compared to patients at the very early/early Barcelona clinic liver cancer (BCLC) stage, those at the advanced/end stage had a 2.045-fold increased risk of ER (95% CI: 1.259-7.366, P=0.014).
CONCLUSIONS: The maximum tumor diameter, adjacent lobe invasion, NLR, and advanced/end stage BCLC stage were all risk factors for ER after TACE in HCC patients.
Keywords: Carcinoma, Hepatocellular, Chemoembolization, Therapeutic, Recurrence, Aged, 80 and over, Female, Humans, Liver Neoplasms, Risk Factors
Background
Hepatocellular carcinoma (HCC) is one of the most common cancers globally and accounts for over 90% of cases with primary liver cancer [1,2]. As the second leading cause of cancer deaths, HCC endangers over 780 000 new patients per year [3]. The occurrence and development of HCC are associated with several factors, including hepatitis B virus (HBV), hepatitis C virus (HCV), non-alcoholic fatty liver disease/NASH, and alcohol abuse [4].
HCC treatment can be divided into a radical treatment for tumor cure, and a palliative treatment aimed at controlling tumor growth and prolonging survival [5]. Among them, hepatectomy is regarded as the first option for HCC curative treatment, particularly in early HCC [6]. Although the overall survival rate after hepatectomy has improved, the long-term prognosis remains unsatisfactory due to the high recurrence rate [7,8]. Consequently, transarterial chemoembolization (TACE), as a non-operative option, has been widely applied for treating patients with unresectable HCC [9]. TACE can effectively cut off the blood supply of tumor tissues, block the oxygen and energy supply of tumor cells, and promote tumor cell apoptosis [10]. However, due to the large number of capillary networks distributed in the liver, the residual tumor tissues of patients with HCC after TACE easily form collateral circulation and promote new tumor-related angiogenesis, resulting in recurrence after TACE [11]. Early recurrence (ER), defined as HCC recurring within 2 years after treatment [12], is an important factor leading to poor prognosis of patients. It was reported that patients with HCC treated with TACE showed survival rates of 70.3%, 40.4%, and 32.4% at 1, 2, and 5 years, respectively, which revealed a relatively high ER rate after TACE [13]. It was also shown that low tumor necrosis rate and high recurrence rate may be the key to improve the prognosis of HCC patients [14]. The present study sought to identify influencing factors of ER after TACE in HCC patients.
Material and Methods
STUDY POPULATION:
In this retrospective study, the data of patients who underwent TACE at Weihai Central Hospital between 2016 and 2019 were collected. Inclusion criteria were: 1) patients age ≥18 years old; 2) patients with HCC who were diagnosed by pathology or cytology, or by American Association for the Study of Liver Diseases (AASLD) Practice Guidelines; 3) patients who underwent TACE treatment; 4) patients whose clinical, pathological, and imaging data were completely preserved. Exclusion criteria were: 1) patients with other malignant tumors and autoimmune diseases; 2) patients with severe heart failure, a recent history of cardiovascular and cerebrovascular diseases, or renal insufficiency; 3) patients with poor compliance such as unable or unwilling to contact after discharge; 4) patients who took other experimental drugs within 1 month before inclusion or who were participating in other clinical studies; 5) patients that the physician believes are unsuitable for this study.
This study was approved by the Ethics Committee of Weihai Central Hospital, approval number WHSZXYYKYLL-2020-33. The experiments were carried out following the approved guidelines.
TACE PROCEDURES:
TACE procedures were performed by 2 experienced radiologists. Seldinger technique was used to puncture the right femoral artery. Hepatic angiography was performed using angiographic catheters to observe the presence of portal vein stenosis or obstruction and to determine whether hepatic artery infusion chemotherapy and embolization therapy could be performed. Then, super-selective catheterization was performed to the tumor feeding artery and its branches for angiography to reconfirm the size, location, and number of tumors. Afterward, the feeding artery was selected for slow injection according to the degree of staining, and the tumors in the pigmented area were embolized with iodized oil to observe the degree of deposition. TACE was discontinued if vascular contraindications, poor hepatic function, or other serious adverse effects occurred. Patients were followed up regularly after TACE to monitor the presence of tumor recurrence.
DATA COLLECTION:
According to the electronic medical records system of our hospital, clinicopathological factors, including sex, age, body mass index (BMI), groups, maximum tumor diameter, Child-Pugh score, Barcelona clinic liver cancer (BCLC) staging, and follow-up time, as well as laboratory parameters of the patients, were collected. After TACE, all patients were followed up for a maximum of 2 years, mainly by telephone and laboratory examinations, and we recorded whether having ER during the follow-up time occurred.
STATISTICAL ANALYSIS:
According to the outcome, the patients were divided into the ER group and the non-ER group. Univariate Cox regression analysis was carried out, and then significant variables in univariate analysis were included in the multivariate Cox regression analysis to explore the influencing factors of ER after TACE. All data were analyzed using SAS9.4 statistical software (SAS Institute, Inc., Cary, NC, USA), and univariate Kaplan-Meier (K-M) survival curves and restricted cubic splines were plotted for visualizing the relations between the influencing factors and ER.
Results
BASELINE CLINICAL CHARACTERISTICS:
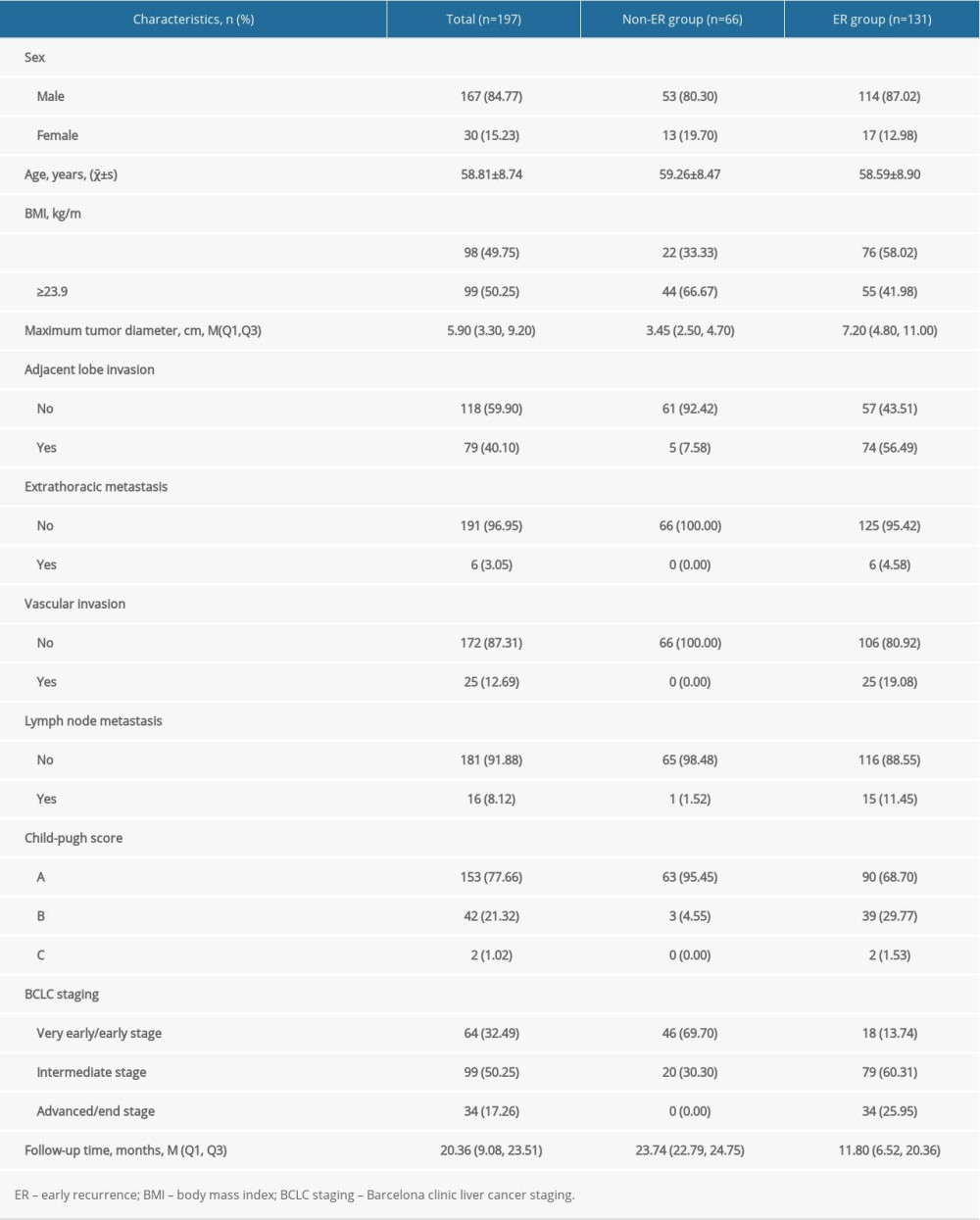
In our study, a total of 197 eligible patients, including 167 (84.77%) males and 30 (15.23%) females, were enrolled (ER group: n=131, non-ER group: n=66). The mean age was (58.81±8.74) years, with the oldest 87 years old and the youngest 37 years old. The average follow-up time was 20.36 (9.08, 23.51) months. By the end of the follow-up, 131 patients (66.50%) had ER and 66 patients (33.50%) had no recurrence. The median maximum tumor diameter was 5.90 (3.30, 9.20) cm. For the BCLC stages, 64 (32.49%) were in the very early/early stage, 99 (50.25%) were in the intermediate stage, and 34 (17.26%) were in the advanced/end stage. All baseline characteristics are shown in Table 1.
UNIVARIATE ANALYSIS:
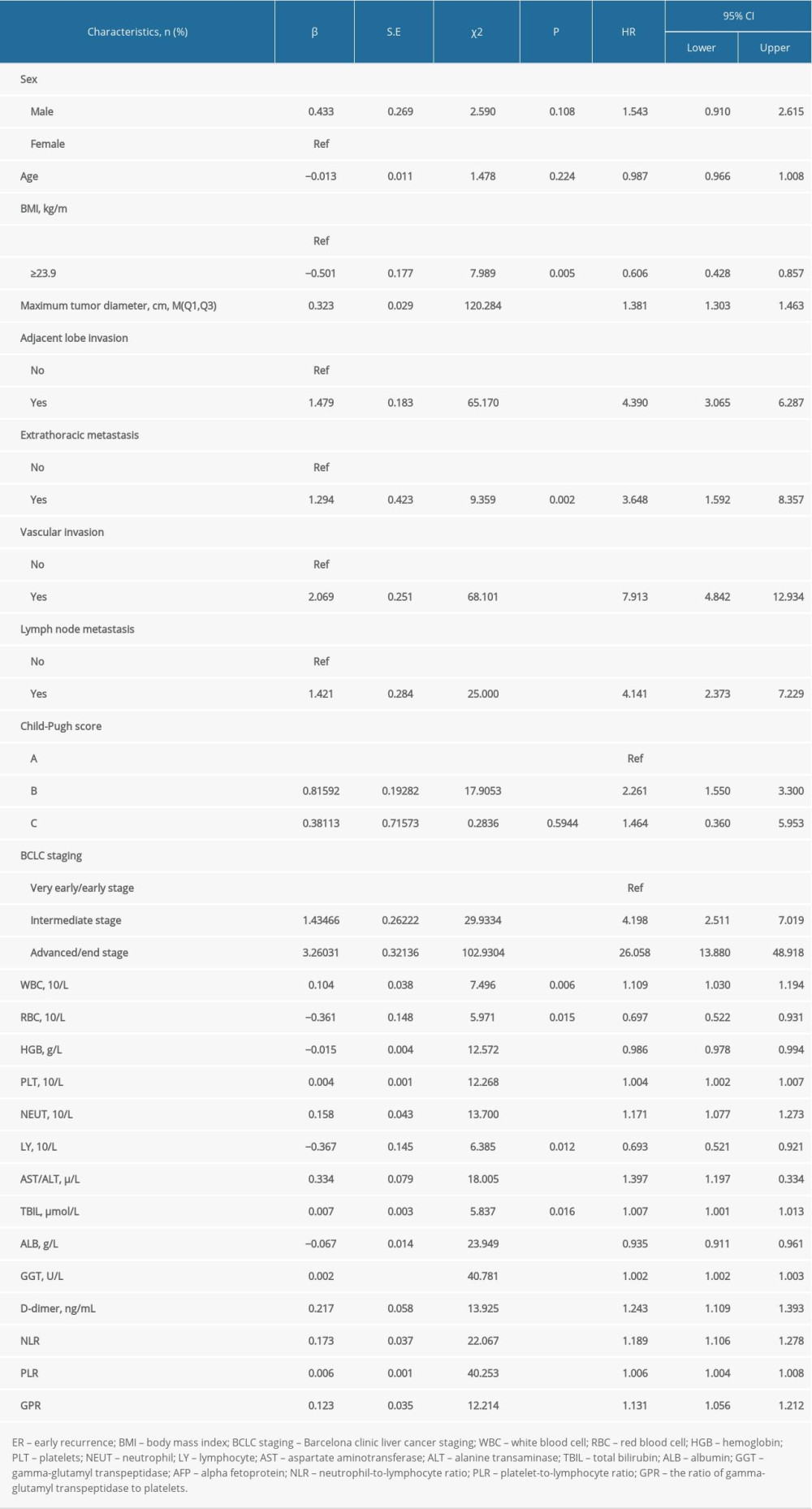
According to univariate Cox regression analysis, several clinicopathologic variables were identified to be potential influencing factors of ER after TACE in HCC patients, including BMI ≥23.9 kg/m2 (P=0.005), maximum tumor diameter (P<0.001), presence of adjacent lobe invasion (P<0.001), presence of extrathoracic metastasis (P=0.002), presence of vascular invasion (P<0.001), presence of lymph node metastasis (P<0.001), Child-Pugh B (P<0.001), and intermediate stage (P<0.001) and advanced/end stage (P<0.001) in BCLC staging. Significant differences were also found in some laboratory variables, including white blood cell (WBC) (P=0.006), red blood cell (RBC) (P=0.015), hemoglobin (HGB) (P<0.001), platelet (PLT) (P<0.001), neutrophil (NEUT) (P<0.001), lymphocyte (LY) (P=0.012), aspartate aminotransferase/alanine transaminase (AST/ALT) (P<0.001), total bilirubin (TBIL) (P=0.016), albumin (ALB) (P<0.001), gamma-glutamyl transpeptidase (GGT) (P<0.001), D-dimer (P <0.001), alpha fetoprotein (AFP) (P<0.001), neutrophil-to-lymphocyte ratio (NLR) (P<0.001), platelet-to-lymphocyte ratio (PLR) (P<0.001), and the ratio of gamma-glutamyl transpeptidase to platelets (GPR) (P<0.001) (Table 2).
MULTIVARIATE ANALYSIS:
After univariate analysis, the significant variables were included in the multivariate Cox regression analysis. The results suggested that the maximum tumor diameter, presence of adjacent lobe invasion, NLR, and advanced/end BCLC stage were all risk factors of ER after TACE in patients with HCC. After age and sex were adjusted, these 4 variables were still found to be risk factors (Figure 1). For every 1-cm increase in the maximum tumor diameter, the risk of ER increased by 0.235 times (95% CI: 1.144–1.333, P<0.001). Patients with adjacent lobe invasion had a 1.227-fold higher risk of ER than those without (95% CI: 1.461–3.394, P<0.001). For every unit increase in NLR, the risk increased 0.107-fold (95% CI: 1.012–1.211, P=0.027). Compared to patients at the very early/early BCLC stage, those at the advanced/end stage had a 2.045-fold increased risk of ER (95% CI: 1.259–7.366, P=0.014).
Based on the results of the multivariate Cox regression model, the C-indexes of the risk factors, including adjacent lobe invasion, maximum tumor diameter, BCLC staging, and NLR, were 0.681 (0.644–0.718), 0.709 (0.674–0.744), 0.743 (0.706–0.780), and 0.670 (0.625–0.715), respectively, suggesting the good predictive ability of these factors. We plotted the K-M survival curves for adjacent lobe invasion (Figure 2) and BCLC staging (Figure 3), and we also used restricted cubic spline to model and visualize the relationship between the maximum tumor diameter and ER after TACE. The results suggested a nonlinear relationship between the maximum diameter and ER after TACE, but with no statistical significance (P=0.135) (Figure 4). Also, the relationship between NLR and ER after TACE was visualized by a restricted cubic spline. The results suggested that there was a nonlinear relationship between NLR and ER (χ2=17.28, P<0.001) (Figure 5).
Discussion
HCC is one of the most common cancers worldwide, with a high mortality rate, and TACE is the most commonly used treatment modality for patients with unresectable HCC. Recurrence after treatment plays an important role in the long-term prognosis and survival of HCC patients. In the current study, we evaluated the influencing factors for ER in patients treated with TACE. The maximum tumor diameter, adjacent lobe invasion, NLR, and advanced/end BCLC stage were all identified to be risk factors for ER after TACE in HCC patients. Our results may help clinicians to perform early identification and monitoring patients with a higher risk of recurrence after TACE, thereby improving the prognosis and survival of HCC.
In the present study, we found that the maximum diameter and adjacent lobe invasion were independently associated with the increased risk of ER. Similar results were reported in previous studies [15–17]. Cheng et al demonstrated that the tumor diameter >5 cm was a risk factor for ER. Further, Truant et al found that tumor size >8 cm was independently associated with survival in HCC patients. If a tumor with the maximum diameter >5 cm cannot be removed primarily, some tumor tissues may remain after surgery and metastasis may occur in the residual part, which can increase the ER rate of HCC patients. The larger the maximum tumor diameter was, the liver capsule would be easier to be damaged, thereby leading to the increased risks of tumor trans-lobar metastasis, which would eventually cause the ER of HCC after TACE [18]. In our study, the maximum tumor diameter and presence of adjacent lobe invasion were both identified as risk factors that could affect the ER rate after TACE, which may indicate that they are related to each other and reveals the potential mechanism of ER after TACE.
Inflammation has been found to play an important role in the pathogenesis and progression of malignant tumors. As a marker of systemic inflammation, NLR is associated with cancer progression, metastasis, and prognosis in various cancers, including HCC [19]. In our study, the risk of developing postoperative recurrence increased with the rise in NLR. This is consistent with previous findings showing that a high NLR was associated with higher recurrence and poorer survival in HCC patients after TACE [20–25]. TACE can inhibit tumor growth by embolizing the tumor artery to cause tumor ischemia, hypoxia, and necrosis. However, complete embolization cannot be achieved and aseptic and necrotizing inflammation might occur, leading to the proliferation and metastasis of residual tumor cells [22]. Therefore, assessment of NLR before and after TACE is necessary to improve the prognosis of the treatment and reduce the ER rate.
Our study had some limitations. Firstly, some bias was inevitable due to its retrospective nature. Secondly, the sample selected in the study was a Chinese population, which might restrict the general applicability of our results. In the future, prospective studies including more cohorts of patients are needed to confirm our results. Thirdly, the baseline cutoff values of NLR and the maximum tumor diameter varied in different studies, which might be confusing for their clinical use. Further studies are also required for establishing the most appropriate cutoff values for NLR and the maximum tumor diameter.
Conclusions
In our study, the maximum tumor diameter, adjacent lobe invasion, NLR, and advanced/end BCLC stage were all identified to be risk factors for ER after TACE in HCC patients. Our results may help early identification and monitoring of patients with a higher risk of recurrence after TACE, thereby improving the prognosis and survival of HCC.
Figures
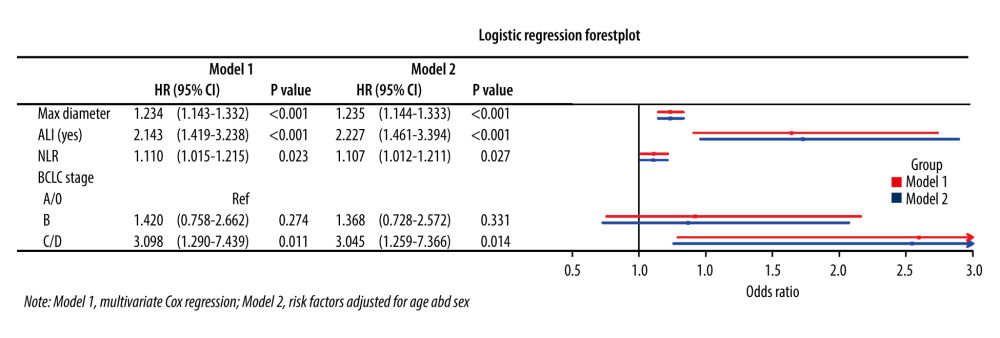 Figure 1. Multivariate Cox regression of ER after TACE in HCC patients.
Figure 1. Multivariate Cox regression of ER after TACE in HCC patients. 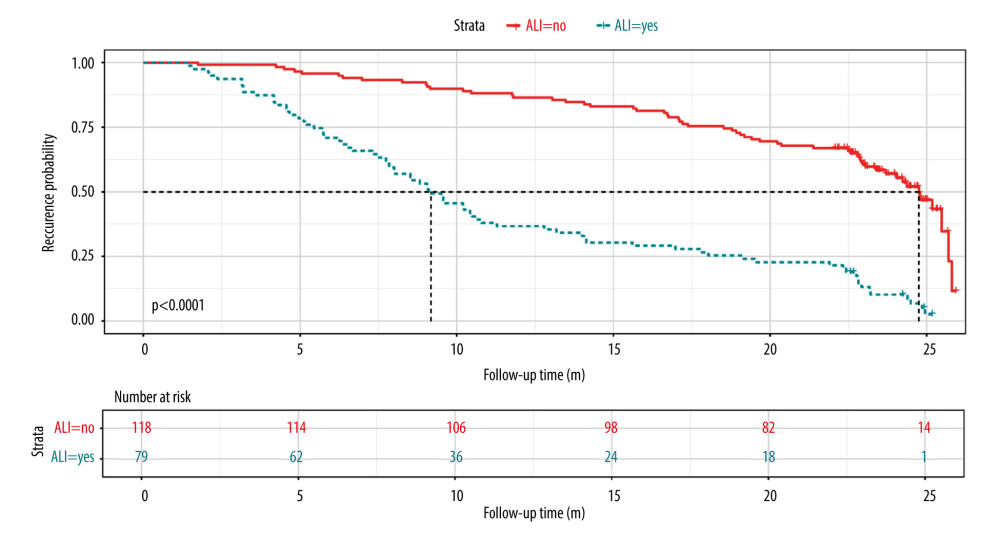 Figure 2. Univariate K-M survival curve for adjacent lobe invasion. ALI – adjacent lobe invasion.
Figure 2. Univariate K-M survival curve for adjacent lobe invasion. ALI – adjacent lobe invasion. 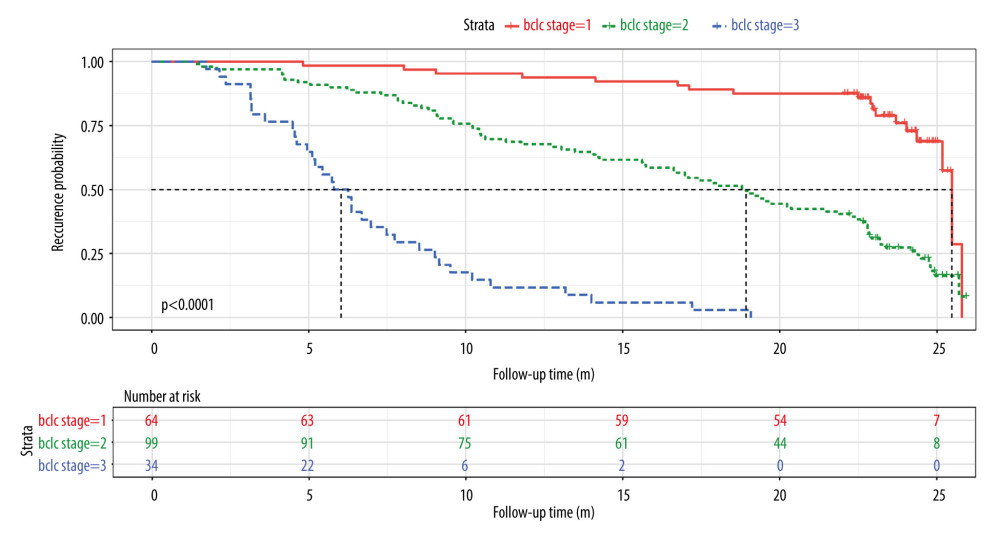 Figure 3. Univariate K-M survival curve for BCLC staging.
Figure 3. Univariate K-M survival curve for BCLC staging. 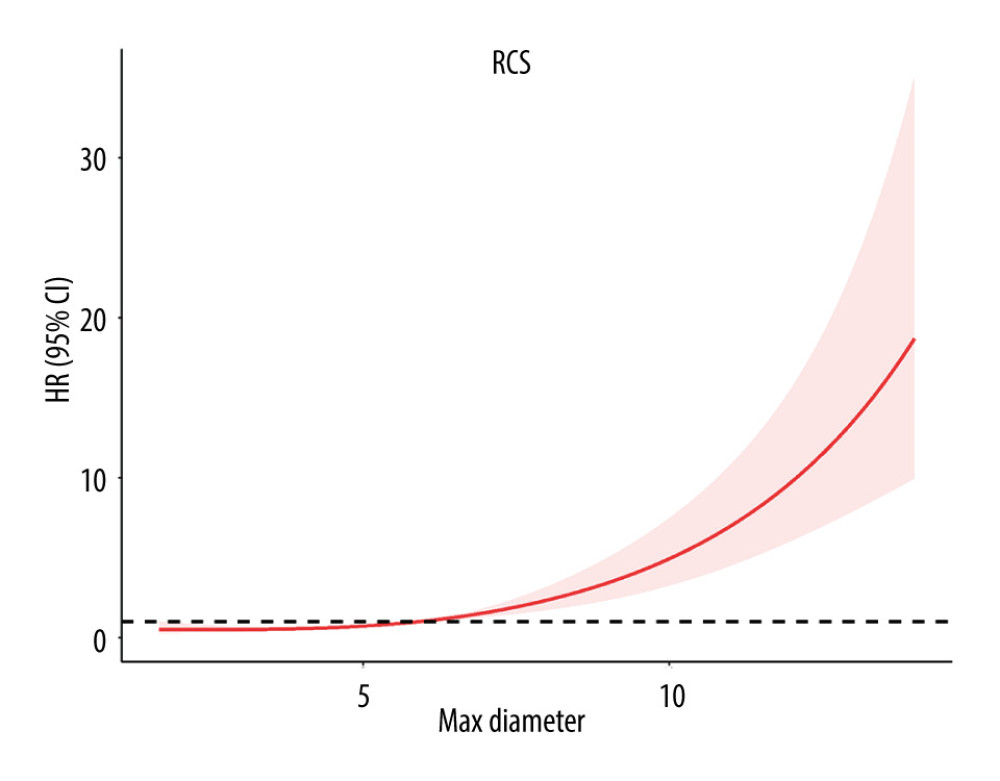 Figure 4. Restricted cubic spline for the maximum tumor diameter.
Figure 4. Restricted cubic spline for the maximum tumor diameter. 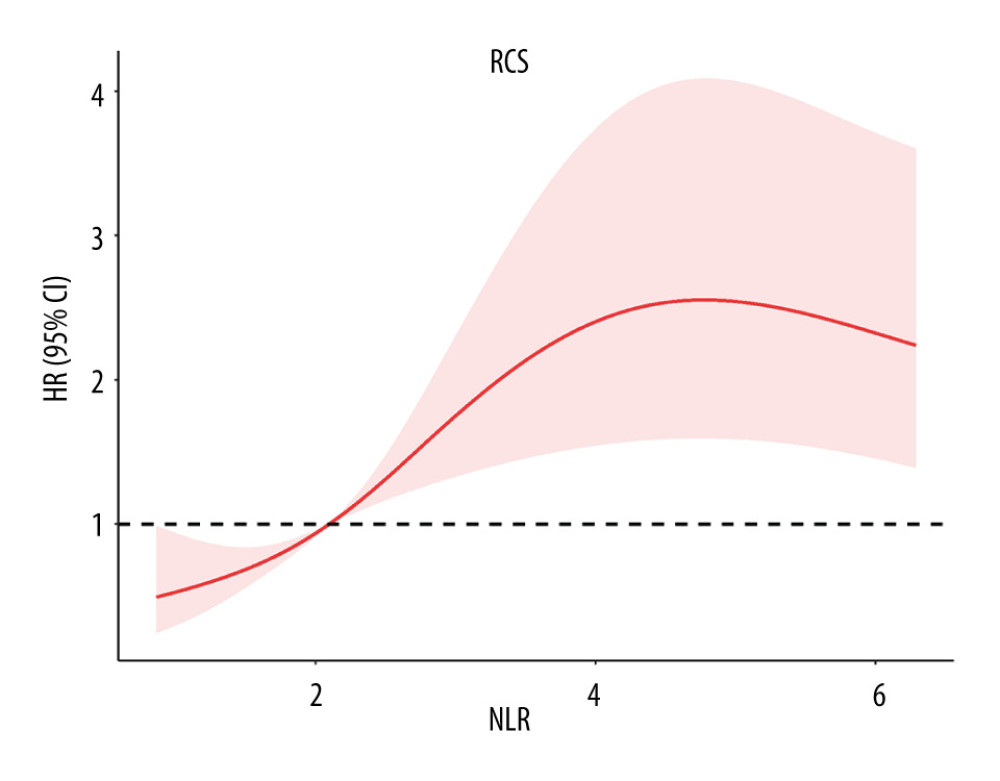 Figure 5. Restricted cubic spline for NLR.
Figure 5. Restricted cubic spline for NLR. References
1. Salem R, Lewandowski RJ, Chemoembolization and radioembolization for hepatocellular carcinoma: Clin Gastroenterol Hepatol, 2013; 11(6); 604-11
2. Kumar VAKA, Aster JC: The breast in Robbins and Cotran pathologic basis of diseases, 2015, Elseview Saunder
3. Fattovich G, Stroffolini T, Zagni I, Hepatocellular carcinoma in cirrhosis: incidence and risk factors: Gastroenterology, 2004; 127(5 Suppl 1); S35-50
4. Dongiovanni P, Romeo S, Valenti L, Hepatocellular carcinoma in nonalcoholic fatty liver: Role of environmental and genetic factors: World J Gastroenterol, 2014; 20(36); 12945-55
5. Hartke J, Johnson M, Ghabril M, The diagnosis and treatment of hepatocellular carcinoma: Semin Diagn Pathol, 2017; 34(2); 153-59
6. Llovet JM, Burroughs A, Bruix J, Hepatocellular carcinoma: Lancet, 2003; 362(9399); 1907-17
7. Hong YM, Cho M, Yoon KT, Risk factors of early recurrence after curative hepatectomy in hepatocellular carcinoma: Tumour Biol, 2017; 39(10); 1010428317720863
8. Lim KC, Chow PK, Allen JC, Systematic review of outcomes of liver resection for early hepatocellular carcinoma within the Milan criteria: Br J Surg, 2012; 99(12); 1622-29
9. Tsurusaki M, Murakami T, Surgical and Locoregional Therapy of HCC: TACE: Liver Cancer, 2015; 4(3); 165-75
10. Cerban R, Ester C, Iacob S, Predictive factors of tumor recurrence and survival in patients with hepatocellular carcinoma treated with transarterial chemoembolization: J Gastrointestin Liver Dis, 2018; 27(4); 409-17
11. Zhang XT, Chen XJStudy on the progression of recurrence of primary liver cancer after TACE: Medical Innovation of China, 2019; 16(31); 159-64 [in Chinese]
12. Benson AB, D’Angelica MI, Abbott DE, NCCN Guidelines insights: Hepatobiliary cancers, version 1. 2017: J Natl Compr Canc Netw, 2017; 15(5); 563-73
13. Lencioni R, de Baere T, Soulen MC, Lipiodol transarterial chemoembolization for hepatocellular carcinoma: A systematic review of efficacy and safety data: Hepatology, 2016; 64(1); 106-16
14. Kim BK, Kim SU, Kim KA, Complete response at first chemoembolization is still the most robust predictor for favorable outcome in hepatocellular carcinoma: J Hepatol, 2015; 62(6); 1304-10
15. Cheng Z, Yang P, Qu S, Zhou J, Risk factors and management for early and late intrahepatic recurrence of solitary hepatocellular carcinoma after curative resection: HPB (Oxford), 2015; 17(5); 422-27
16. Truant S, Boleslawski E, Duhamel A, Tumor size of hepatocellular carcinoma in noncirrhotic liver: A controversial predictive factor for outcome after resection: Eur J Surg Oncol, 2012; 38(12); 1189-96
17. Liu YJ, Jiang P, Li WCurative effect of TACE in patients with recurrence after operation and influence factors analysis: Chinese Journal of Gastroenterology and Hepatology, 2020; 29(1); 18-21 [in Chinese]
18. Choi JY, Lee JM, Sirlin CB, CT and MR imaging diagnosis and staging of hepatocellular carcinoma: Part I. Development, growth, and spread: Key pathologic and imaging aspects: Radiology, 2014; 272(3); 635-54
19. Chang Y, Jeong SW, Young Jang J, Jae Kim Y, Recent updates of transarterial chemoembolilzation in hepatocellular carcinoma: Int J Mol Sci, 2020; 21(21); 8165
20. Yue L, Zhong-Xia W, Yin C, Preoperative inflammation-based markers predict early and late recurrence of hepatocellular carcinoma after curative hepatectomy: Hepatobiliary Pancreat Dis Int, 2016; 15(3); 266-74
21. Zheng J, Cai J, Li H, Neutrophil to lymphocyte ratio and platelet to lymphocyte ratio as prognostic predictors for hepatocellular carcinoma patients with various treatments: A meta-analysis and systematic review: Cell Physiol Biochem, 2017; 44(3); 967-981
22. Fan W, Zhang Y, Wang Y, Neutrophil-to-lymphocyte and platelet-to-lymphocyte ratios as predictors of survival and metastasis for recurrent hepatocellular carcinoma after transarterial chemoembolization: PLoS One, 2015; 10(3); e0119312
23. Zhou D, Liang J, Xu LI, Derived neutrophil to lymphocyte ratio predicts prognosis for patients with HBV-associated hepatocellular carcinoma following transarterial chemoembolization: Oncol Lett, 2016; 11(5); 2987-94
24. He C, Zhang Y, Cai Z, Lin X, The prognostic and predictive value of the combination of the neutrophil-to-lymphocyte ratio and the platelet-to-lymphocyte ratio in patients with hepatocellular carcinoma who receive transarterial chemoembolization therapy: Cancer Manag Res, 2019; 11; 1391-400
25. Chon YE, Park H, Hyun HK, Development of a new nomogram including neutrophil-to-lymphocyte ratio to predict survival in patients with hepatocellular carcinoma undergoing transarterial chemoembolization: Cancers (Basel), 2019; 11(4); 509
Figures
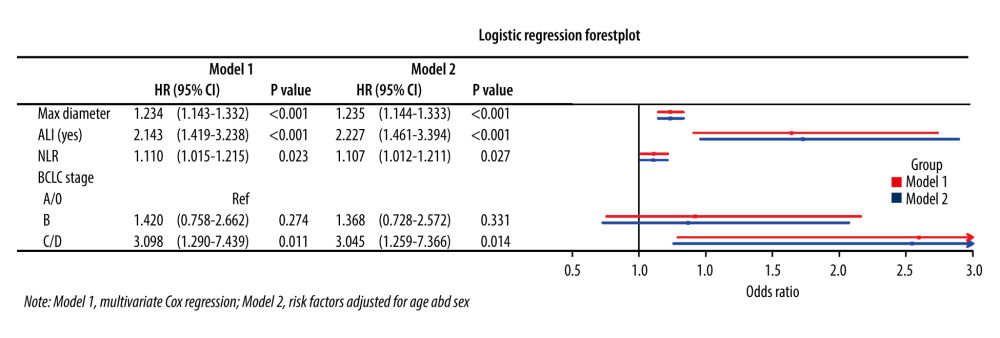 Figure 1. Multivariate Cox regression of ER after TACE in HCC patients.
Figure 1. Multivariate Cox regression of ER after TACE in HCC patients.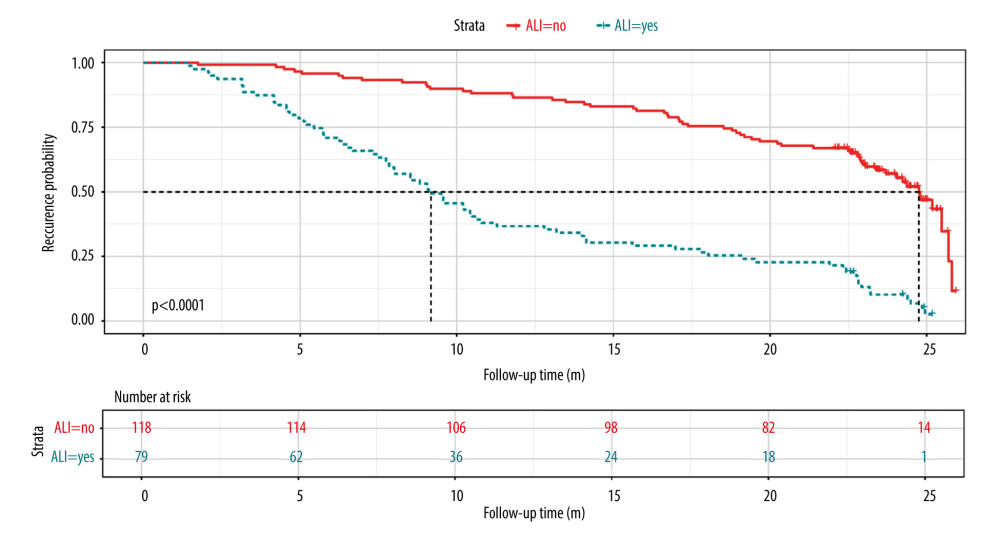 Figure 2. Univariate K-M survival curve for adjacent lobe invasion. ALI – adjacent lobe invasion.
Figure 2. Univariate K-M survival curve for adjacent lobe invasion. ALI – adjacent lobe invasion.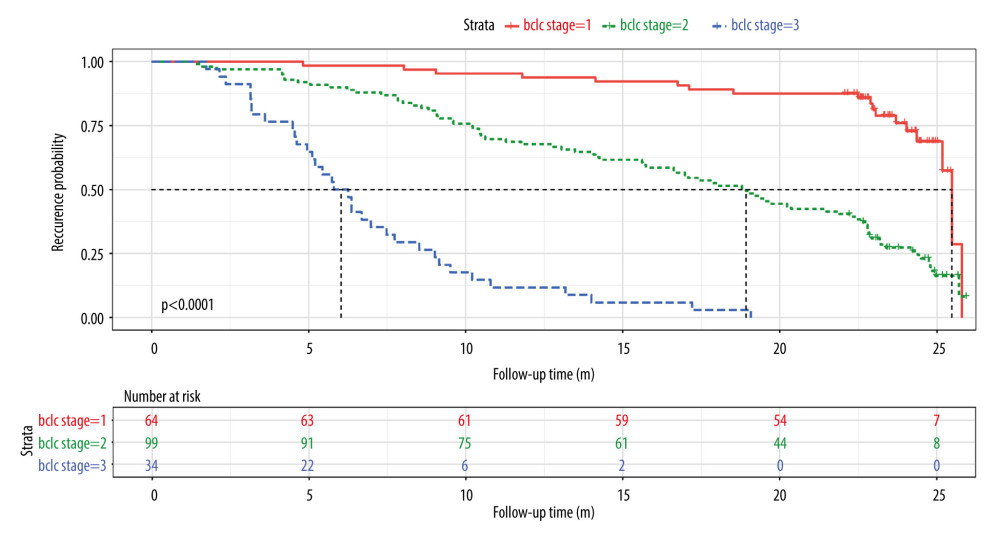 Figure 3. Univariate K-M survival curve for BCLC staging.
Figure 3. Univariate K-M survival curve for BCLC staging.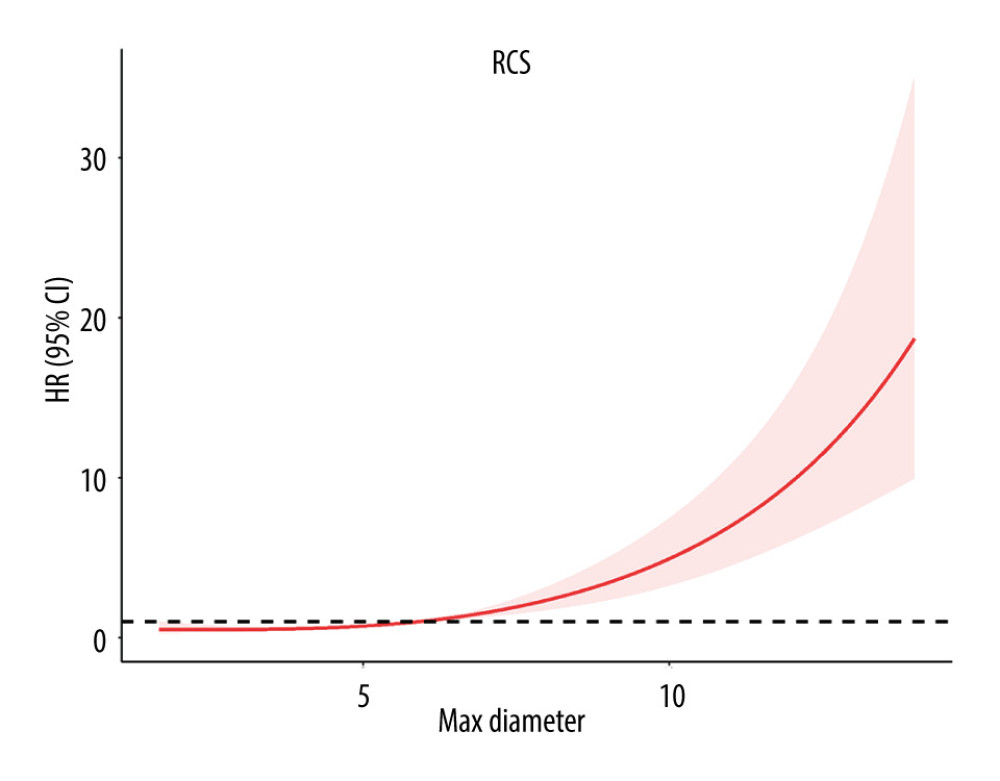 Figure 4. Restricted cubic spline for the maximum tumor diameter.
Figure 4. Restricted cubic spline for the maximum tumor diameter.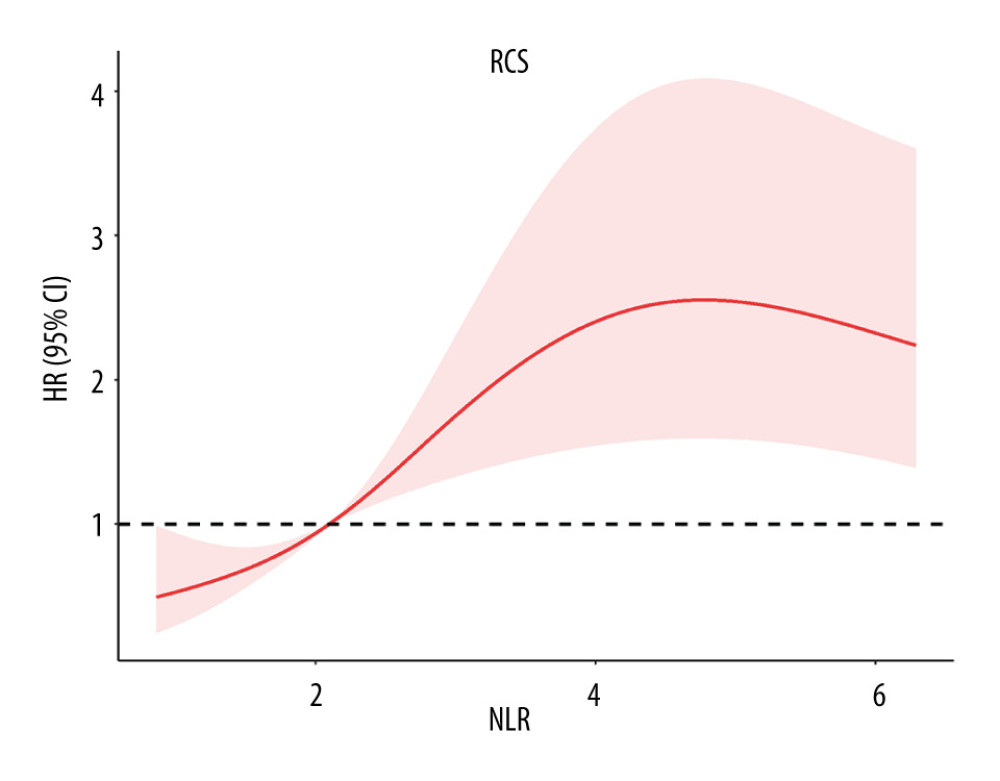 Figure 5. Restricted cubic spline for NLR.
Figure 5. Restricted cubic spline for NLR. In Press
05 Mar 2024 : Clinical Research
Effects of Thermal Insulation on Recovery and Comfort of Patients Undergoing Holmium Laser LithotripsyMed Sci Monit In Press; DOI: 10.12659/MSM.942836
05 Mar 2024 : Clinical Research
Role of Critical Shoulder Angle in Degenerative Type Rotator Cuff Tears: A Turkish Cohort StudyMed Sci Monit In Press; DOI: 10.12659/MSM.943703
06 Mar 2024 : Clinical Research
Comparison of Outcomes between Single-Level and Double-Level Corpectomy in Thoracolumbar Reconstruction: A ...Med Sci Monit In Press; DOI: 10.12659/MSM.943797
21 Mar 2024 : Meta-Analysis
Economic Evaluation of COVID-19 Screening Tests and Surveillance Strategies in Low-Income, Middle-Income, a...Med Sci Monit In Press; DOI: 10.12659/MSM.943863
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952