31 January 2021: Clinical Research
Using a Combined Classification of Increased Signal Intensity on Magnetic Resonance Imaging (MRI) to Predict Surgical Outcome in Cervical Spondylotic Myelopathy
Hu Ren1ADEF, Tao Feng1AEF, Linfeng Wang1ADF, Junchuan Liu1BCD, Peng Zhang1BC, Guangqing Yao1BCD, Yong Shen1ADF*DOI: 10.12659/MSM.929417
Med Sci Monit 2021; 27:e929417
Abstract
BACKGROUND: The aim of this study was to verify whether the combined classification of increased signal intensity (ISI) on magnetic resonance imaging is more closely related to surgical outcomes than signal quality changes or signal longitudinal extent changes alone and to evaluate whether the combined classification ISI method could be used to predict surgical outcomes in cervical spondylotic myelopathy.
MATERIAL AND METHODS: Eighty-four patients (61 men and 23 women) who underwent surgery for cervical spondylotic myelopathy were included in this retrospective study. The patterns of ISI were classified into 3 categories based on (1) the quality of ISI into Grade 0: none, Grade 1: faint (fuzzy), and Grade 2: intense (sharp); (2) the longitudinal extent of ISI into none, focal, and multisegmental; and (3) the combined classification of the quality and longitudinal extent into Type 1 (none/none), Type 2 (focal/faint), Type 3 (focal/intense), Type 4 (multisegmental/faint), and Type 5 (multisegmental/intense). The multifactorial effects of variables were studied. A stepwise regression analysis was performed to verify whether this combined classification could predict outcome.
RESULTS: Of the 3 categories, the combined classification type of ISI was most closely related to recovery rate. Stepwise regression analysis confirmed the significance of combined classification of ISI as a predictor for surgical outcome.
CONCLUSIONS: A combined classification of ISI is more closely related to surgical outcomes than either signal quality changes or signal longitudinal extent changes alone and it could be used as a meaningful indicator for predicting surgical outcomes. We recommend further studies to confirm this finding.
Keywords: Magnetic Resonance Imaging, spondylosis, Cervical Vertebrae, Decompression, Surgical, Spinal Cord Diseases
Background
Cervical spondylotic myelopathy (CSM) is a progressive degenerative disease, and surgical intervention has been shown to be superior to conservative options for the treatment of moderate to severe CSM [1]. Increased signal intensity (ISI) of the spinal cord on T2-weighted magnetic resonance imaging (MRI) can reflect pathological change within the spinal cord [2–4], which has been reported in many studies to be a poor prognostic indicator for neurological and functional outcome after surgical decompression in patients with CSM [5,6]. However, this conclusion is controversial since other studies have had conflicting results [7,8]. One reason for this inconsistency may be that most studies did not categorize the signal intensity changes on the MRI [9]. More recently, some researchers have used different methods to classify intramedullary signal changes, since the type of signal intensity changes appears to be important in predicting clinical outcome. The 2 classifications used most frequently are based on the quality (none, faint or fuzzy, intense or sharp) or longitudinal extent (focal and multisegmental) of the MR image [7,10,11]. Unfortunately, to our knowledge, there is still no consensus on the most important type of signal intensity changes for prognostication. We think one of the important reasons for this deviation may be that each classification focuses on only a single aspect of quality or longitudinal extent. Conceivably, the signal changes can be divided into 5 different types if the 2 classifications are applied together. It remains unclear whether cross combinations of different qualities and longitudinal extent have different roles in predicting clinical outcome. The purpose of this study was to verify whether the combined classification of ISI relates more closely to surgical outcomes than either signal quality changes or signal longitudinal extent changes alone and to evaluate whether this method could be used as an indicator for predicting surgical outcomes.
Material and Methods
RADIOLOGICAL ASSESSMENT:
MRI scanning was performed with a 1.5T system (Siemens Magnetom Symphony) before surgery. ISI was defined as a high-intensity area in contrast to the adjacent iso-intensity portion of the spinal cord in the sagittal and axial plane on T2-weighted images [12]. The patterns of ISI were classified in 3 ways: (1) based on the quality of ISI into Grade 0: none, Grade 1: faint (fuzzy), and Grade 2: intense (sharp) [10]; (2) based on the longitudinal extent of ISI into none, focal (when ISI was confined to 1 disc level with spinal cord compression), and multisegmental (more than 1 disc level) [11]; and (3) based on the combined classification of both the quality and longitudinal extent in which Type 1 (none/none) displayed normal intensity, Type 2 (focal/faint) displayed focal and faint ISI, Type 3 (focal/intense) displayed focal and intense ISI, Type 4 (multisegmental/faint) displayed multisegmental and faint ISI, and Type 5 (multisegmental/intense) displayed multisegmental and intense ISI (Figure 1). Intramedullary ISI changes on the T2-weighted images were evaluated by 2 independent observers who were blinded to the patients’ clinical data. They independently interpreted the T2-weighted images to determine the type of signal intensity changes.
The compression ratio was measured by dividing the smallest anteroposterior dimension of the spinal cord by the broadest transverse diameter at the same level on axial MRI scans [13].
FUNCTIONAL OUTCOME MEASURES:
Neurologic status was assessed with the modified Japanese Orthopedic Association (JOA) scoring system for CSM before and after surgery [6]. The JOA score has a total of 17 points which quantifies neurological impairment by evaluating upper extremity function, lower extremity function, sensory function, and bladder function. The improvement of symptoms after surgery was evaluated as recovery rate of the JOA score, which was calculated as follows: recovery rate=(postoperative JOA score-preoperative JOA score)/(17−preoperative JOA score)×100% [14].
STATISTICAL ANALYSIS:
The following patient parameters were obtained and studied: age, duration of symptoms, compression ratio, surgical approach, preoperative JOA score, preoperative types of ISI on T2-weighted images, postoperative JOA score, and recovery rate of the JOA score. Statistical analysis was performed using SPSS for Windows, version 17.0 (SPSS Inc, Chicago, IL). The analysis of variance (ANOVA) and the Student-Newman-Keuls (SNK) test were used for differences among more than 2 groups. Univariate analysis was performed using Spearman’s rank correlation test to measure the relationship between neural recovery rate and each independent variable. A stepwise regression analysis was performed to verify whether this combined classification could be used to predict outcome. A
Results
Neurological outcomes for patients with CSM were improved in the mean follow-up period. Overall, the mean preoperative and postoperative JOA scores at the final follow-up were 10.1±2.3 and 13.2±2.4, respectively (
According to the quality of ISI, the preoperative MRI showed 30 patients with Grade 0, 32 patients with Grade 1, and 22 patients with Grade 2. The ANOVA results showed significant differences in the recovery rate among the 3 groups (Grade 0, 67.9±18.8%; Grade 1, 43.2±26.0%; Grade 2, 28.4±13.7%). The SNK test showed significant differences between Grades 0 and 1 (
According to the longitudinal extent of ISI, there was no ISI in 30 patients, focal ISI in 30 patients, and multisegmental ISI in 24 patients. ANOVA results showed significant differences in the recovery rate among the 3 groups (none, 67.9±18.8%; focal, 47.1±22.6%; and multisegmental, 24.7±16.4%). The SNK test showed significant differences between the none and focal groups (
According to the combined classification of ISI, there were 30 patients in Type 1, 19 patients in Type 2, 11 patients in Type 3, 13 patients in Type 4, and 11 patients in Type 5. The ANOVA results for age, duration of symptoms, preoperative JOA score, postoperative JOA score, and recovery rate showed significant differences among the 5 types (Table 1). The age and duration of symptoms gradually increased with increasing ISI type. The preoperative JOA score, postoperative JOA score, and recovery rate of the JOA score gradually decreased with increasing ISI type. There were no significant differences in compression ratio among the 5 ISI types. The SNK test on recovery rate showed significant differences between Type 1 and Type 2 and between Type 3, Type 4, and Type 5 (
The Spearman’s rank correlation test showed that the factors closely related to the recovery rate included the combined classification type of ISI (
Discussion
Various factors that may influence the neurological outcome after decompression surgery for CSM have been discussed by many authors [15,16]. Among these factors, the value of ISI on T2-weighted MRI remains controversial [17]. Some authors have proposed that ISI on T2-weighted images coincided with pathological changes of the spinal cord [6,18,19]. Takahashi et al. speculated that signal intensity changes reflect myelomalacia or cord gliosis secondary to sustained compression of the spinal cord and can be used to predict neurological recovery after surgical decompression [2]. However, from a clinical perspective, the earlier studies that focused only on whether or not the signal intensity changed had conflicting results. Some scholars speculated that ISI on T2-weighted images includes a broad spectrum of compressive myelomalacic pathology, from edema to syrinx formation, and reflects a broad spectrum of spinal cord recuperative potentials, which are nonspecific [20]. The pathological changes in the spinal cord cannot be accurately reflected according to this simple classification method.
To improve this situation, there has been more emphasis placed on classifying these signal intensity changes, since the type of ISI appears to be more important in determining patient outcome than merely its presence or absence. Two of these classification methods are most widely used. The first method is based on a qualitative description of ISI, which was provided by Chen et al. in 2001 to grade the signal intensity change patterns on T2-weighted MR images as follows: Grade 0: no signal change, Grade 1: faint or fuzzy signal, and Grade 2: intense or sharp signal [10]. Their study demonstrated that a predominantly intense and sharp bordered ISI on T2-weighted MR images was associated with a poorer prognosis than those with faint and fuzzy or no change in signal intensity. It is assumed that the faint or fuzzy signal intensity on T2-weighted MR images may be associated with potentially reversible changes such as edema, Wallerian degeneration, demyelination, and ischemia. T2 imaging showing intense or sharp signal changes considered to be irreversible include cavitation, neural tissue loss, myelomalacia, necrosis, and spongiform changes in gray matter [21]. Although some subsequent studies, including the present one, confirmed the above conclusions, there are still differing views. Avadhani et al. found that there was no significant difference in the recovery rates of patients with different signal intensity changes on the T2-weighted MR images [9]. Machino et al. also found there was no significant relationship between ISI grades and surgical outcomes after they prospectively studied 505 consecutive patients with CSM [22]. The second main classification method assesses the longitudinal extent of ISI, which classifies ISI changes as absent, focal, and multisegmental [7]. Some studies reported that patients with multisegmental ISI showed a poorer prognosis after surgical decompression than patients with local ISI [7,23,24]. However, there are authors who have refuted the above finding, stating that the longitudinal extent of the ISI on T2-weighted images has no predictive value [25,26].
We think one of the important reasons for the above disagreement may be that each classification focuses only on a single aspect of quality or longitudinal extent, and the superposition of these 2 factors has not been considered together. According to the above independent classification method, our study also reached the same conclusion that the quality or longitudinal extent of the ISI could reflect surgical outcomes. Our findings demonstrated significant differences in the recovery rate among the 3 groups. Postoperative recovery rate declined as the ISI quality and longitudinal extent increased. However, if the 2 classifications are applied together, the signal changes can be divided into 5 different types, which is normal in clinical work.
Although this classification method may sound subjective, whether it is more closely related to surgical outcomes than signal quality changes or signal longitudinal extent changes alone and whether it could be used as an indicator for predicting surgical outcomes remain unclear. These questions constitute the main purpose of this study.
In the present study, univariate analysis showed that the most closely related factor among the 3 categories to the recovery rate was the combined classification type of ISI (
In addition, according to further analysis, our data showed that multisegmental ISI in patients was correlated with a poorer prognosis after surgical decompression than focal and faint ISI, which supports the view that the longitudinal extent of the ISI could reflect surgical outcomes. More importantly, we identified 2 major differences from previous studies. First, the patients with multisegmental ISI had no significant differences in recovery rate when compared with the patients with focal and intense ISI, although they appear to have had different longitudinal extent. Second, the patients with focal or multisegmental and intense ISI experienced significantly less improvement through surgery than patients with focal and faint ISI or no change in signal intensity; however, there was no significant difference in surgical outcome between patients with focal or multisegmental and intense ISI compared with the patients with multisegmental and faint ISI. At the same time, our data showed that the age, duration of symptoms, and preoperative JOA score varied across different groups, as previous studies have confirmed that MRI signal changes tended to be associated with clinical characteristics [11,12,27]. But also because of this reason, it may be difficult to separate out the isolated effect of MRI signal changes since the other confounding variables were not clearly addressed. We recommend further research be conducted to control for other clinical variables to investigate the difference of recovery rate between the 5 groups.
There are some limitations to our study. First, it was a retrospective study and the number of patients included in the study was small, which may have caused data bias in the statistical analysis. Nevertheless, we believe that this study provides some meaningful information for practical work and future research directions. Further high-quality clinical studies with large samples are needed to explore this combined classification of the longitudinal extent and quality for CSM. Second, this study did not conduct further analyses on other predictors of surgical outcome, such as age, duration of symptoms, compression ratio, and preoperative JOA score, because these were not the main purpose of this study. But what we need to emphasize is that the neurological outcome of cervical decompressive surgery is influenced by multiple factors and the basic radiographic features alone cannot predict surgical outcome in individual patients. Only in combination with clinical features can it play a better role.
Conclusions
In summary, we categorized signal changes on T2-weighted MR images into 5 types: Type 1 displayed normal intensity, Type 2 displayed focal and faint ISI, Type 3 displayed focal and intense ISI, Type 4 displayed multisegmental and faint ISI, and Type 5 displayed multisegmental and intense ISI. Our study showed that this combined classification of ISI was more closely related to surgical outcomes than either signal quality changes or signal longitudinal extent changes alone and it could be used as a meaningful indicator for predicting surgical outcomes. We recommend further studies to confirm this finding.
Figures
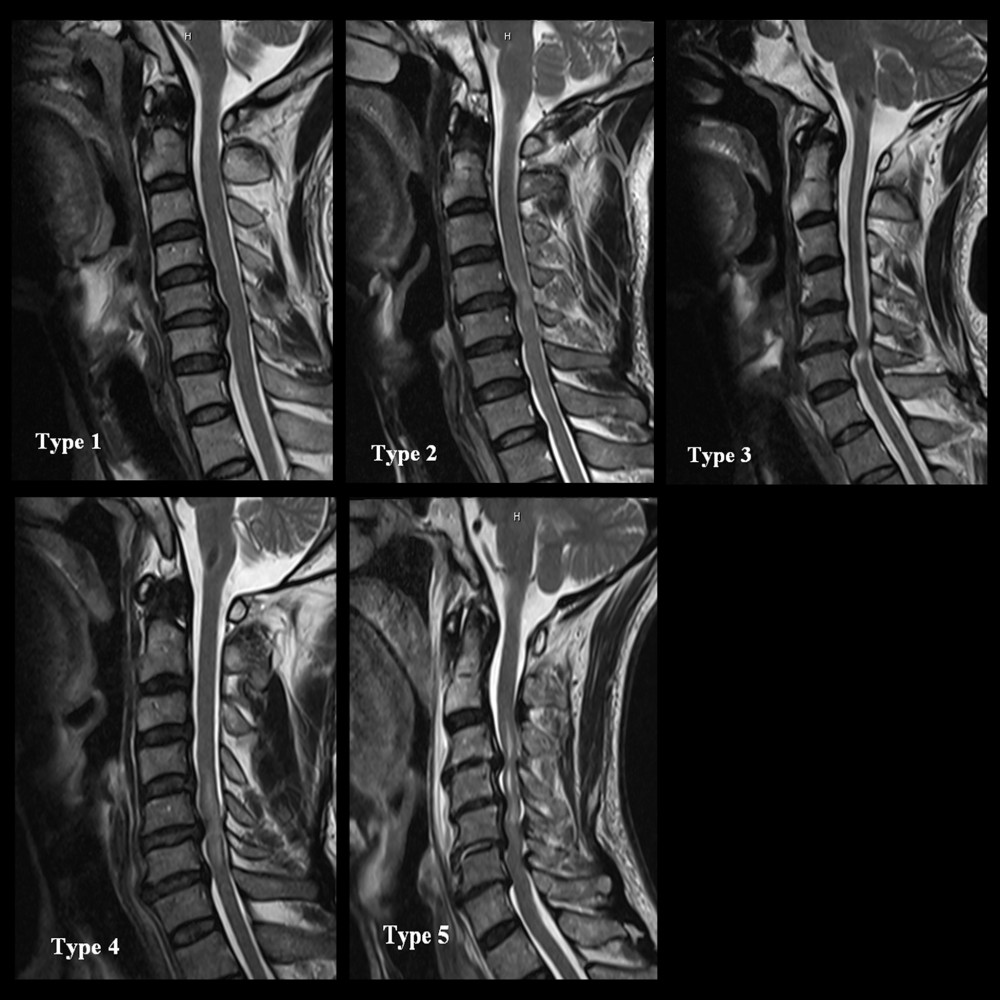 Figure 1. The combined classification of both the quality and longitudinal extent of increased signal intensity (ISI) on T2-weighted images: Type 1 (none/none) displayed normal intensity; Type 2 (focal/faint) displayed focal and faint ISI; Type 3 (focal/intense) displayed focal and intense ISI; Type 4 (multisegmental/faint) displayed multisegmental and faint ISI; and Type 5 (multisegmental/intense) displayed multisegmental and intense ISI.
Figure 1. The combined classification of both the quality and longitudinal extent of increased signal intensity (ISI) on T2-weighted images: Type 1 (none/none) displayed normal intensity; Type 2 (focal/faint) displayed focal and faint ISI; Type 3 (focal/intense) displayed focal and intense ISI; Type 4 (multisegmental/faint) displayed multisegmental and faint ISI; and Type 5 (multisegmental/intense) displayed multisegmental and intense ISI. 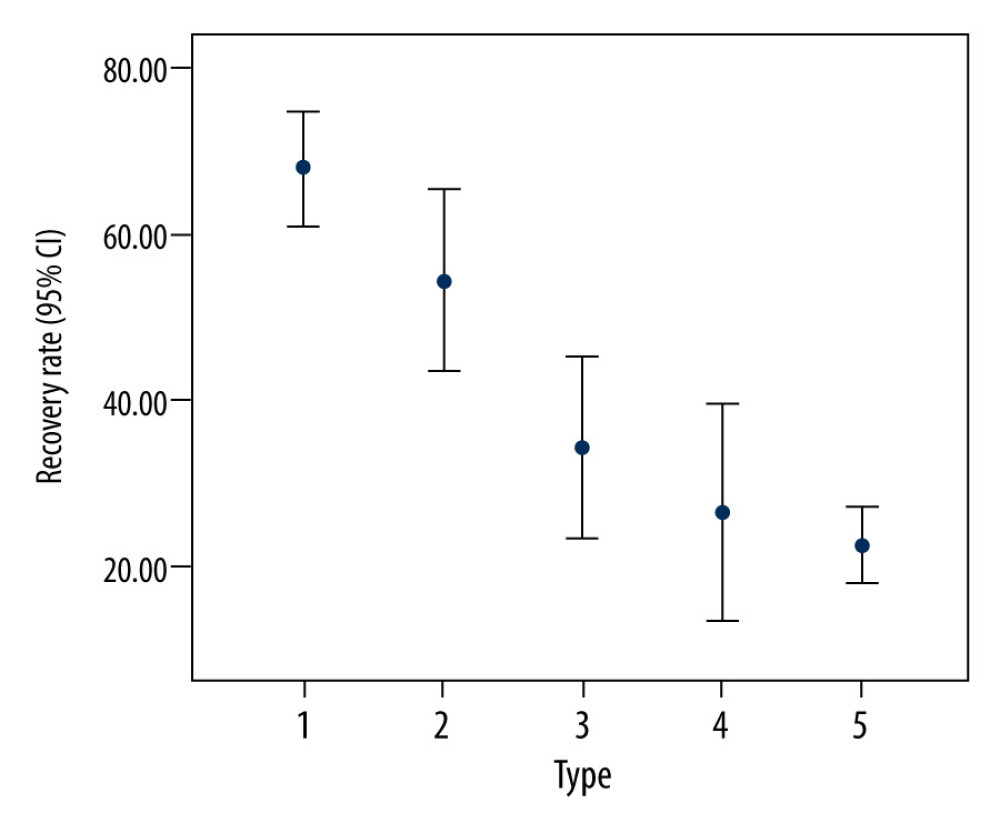 Figure 2. Relationship between recovery rate after surgery for cervical spondylotic myelopathy and preoperative combined classification of increased signal intensity on T2-weighted images.
Figure 2. Relationship between recovery rate after surgery for cervical spondylotic myelopathy and preoperative combined classification of increased signal intensity on T2-weighted images. References
1. Bakhsheshian J, Mehta VA, Liu JC, Current diagnosis and management of cervical spondylotic myelopathy: Global Spine J, 2017; 7(6); 572-86
2. Takahashi M, Yamashita Y, Sakamoto Y, Kojima R, Chronic cervical cord compression: Clinical significance of increased signal intensity on MR images: Radiology, 1989; 173(1); 219-24
3. Batzdorf U, Flannigan BD, Surgical decompressive procedures for cervical spondylotic myelopathy: A study using magnetic resonance imaging: Spine (Phila PA 1976), 1991; 16(2); 123-27
4. Takahashi M, Sakamoto Y, Miyawaki M, Bussaka H, Increased MR signal intensity secondary to chronic cervical cord compression: Neuroradiology, 1987; 29(6); 550-56
5. Miyazaki M, Notani N, Ishihara T, Surgical outcomes after laminoplasty for cervical spondylotic myelopathy: A focus on the dynamic factors and signal intensity changes in the intramedullary spinal cord on MRI: Clin Neurol Neurosurg, 2017; 162; 108-14
6. Mehalic TF, Pezzuti RT, Applebaum BI, Magnetic resonance imaging and cervical spondylotic myelopathy: Neurosurgery, 1990; 26(2); 217-26
7. Wada E, Yonenobu K, Suzuki S, Can intramedullary signal change on magnetic resonance imaging predict surgical outcome in cervical spondylotic myelopathy?: Spine (Phila PA 1976), 1999; 24(5); 455-61
8. Chung SS, Lee CS, Chung KH, Factors affecting the surgical results of expansive laminoplasty for cervical spondylotic myelopathy: Int Orthop, 2002; 26(6); 334-38
9. Avadhani A, Rajasekaran S, Shetty AP, Comparison of prognostic value of different MRI classifications of signal intensity change in cervical spondylotic myelopathy: Spine J, 2010; 10(6); 475-85
10. Chen CJ, Lyu RK, Lee ST, Intramedullary high signal intensity on T2-weighted MR images in cervical spondylotic myelopathy: Prediction of prognosis with type of intensity: Radiology, 2001; 221(3); 789-94
11. Vedantam A, Rajshekhar V, Does the type of T2-weighted hyperintensity influence surgical outcome in patients with cervical spondylotic myelopathy? A review: Eur Spine J, 2013; 22(1); 96-106
12. Yukawa Y, Kato F, Yoshihara H, MR T2 image classification in cervical compression myelopathy: Predictor of surgical outcomes: Spine (Phila PA 1976), 2007; 32(15); 1675-78
13. Fujiwara K, Yonenobu K, Ebara S, The prognosis of surgery for cervical compression myelopathy. An analysis of the factors involved: J Bone Joint Surg Br, 1989; 71(3); 393-98
14. Hirabayashi K, Miyakawa J, Satomi K, Operative results and postoperative progression of ossification among patients with ossification of cervical posterior longitudinal ligament: Spine (Phila PA 1976), 1981; 6(4); 354-64
15. Wei L, Cao P, Xu C, Clinical and radiologic results of anterior cervical discectomy and fusion for cervical spondylotic myelopathy in elderly patients with T2-weighted increased signal intensity: World Neurosurg, 2018; 112; e520-26
16. Sun LQ, Li M, Li YM, Predictors for surgical outcome of laminoplasty for cervical spondylotic myelopathy: World Neurosurg, 2016; 94; 89-96
17. Karpova A, Arun R, Cadotte DW, Assessment of spinal cord compression by magnetic resonance imaging – Can it predict surgical outcomes in degenerative compressive myelopathy?: Spine (Phila PA 1976), 2013; 38(16); 1409-21
18. Uchida K, Nakajima H, Sato R, Multivariate analysis of the neurological outcome of surgery for cervical compressive myelopathy: J Orthop Sci, 2005; 10(6); 564-73
19. Al-Mefty O, Harkey LH, Middleton TH, Myelopathic cervical spondylotic lesions demonstrated by MRI: J Neurosurg, 1988; 68(2); 217-22
20. Morio Y, Teshima R, Nagashima H, Correlation between operative outcomes of cervical compression myelopathy and MRI of the spinal cord: Spine (Phila PA 1976), 2001; 26(11); 1238-45
21. Gibson J, Nouri A, Krueger B, Degenerative cervical myelopathy: A clinical review: Yale J Biol Med, 2018; 91(1); 43-48
22. Machino M, Imagama S, Ando K, Image diagnostic classification of magnetic resonance T2 increased signal intensity in cervicalspondylotic myelopathy: Clinical evaluation using quantitative and objective assessment: Spine (Phila PA 1976), 2018; 43(6); 420-26
23. Wei L, Cao P, Xu C, Comparison of the prognostic value of different quantitative measurements of increased signal intensity on T2-weighted MRI in cervical spondylotic myelopathy: World Neurosurg, 2018; 118; e505-12
24. Li XY, Lu SB, Sun XY, Clinical and magnetic resonance imaging predictors of the surgical outcomes of patients with cervical spondylotic myelopathy: Clin Neurol Neurosurg, 2018; 174; 137-43
25. Yagi M, Ninomiya K, Kihara M, Horiuchi Y, Long-term surgical outcome and risk factors in patients with cervical myelopathy and a change in signal intensity of intramedullary spinal cord on magnetic resonance imaging: J Neurosurg Spine, 2010; 12(1); 59-65
26. Ahn JS, Lee JK, Kim BK, Prognostic factors that affect the surgical outcome of the laminoplasty in cervical spondylotic myelopathy: Clin Orthop Surg, 2010; 2(2); 98-104
27. Ito K, Imagama S, Ito K, MRI signal intensity classification in cervical ossification of the posterior longitudinal ligament: Predictor of surgical outcomes: Spine (Phila PA 1976), 2017; 42(2); E98-103
Figures
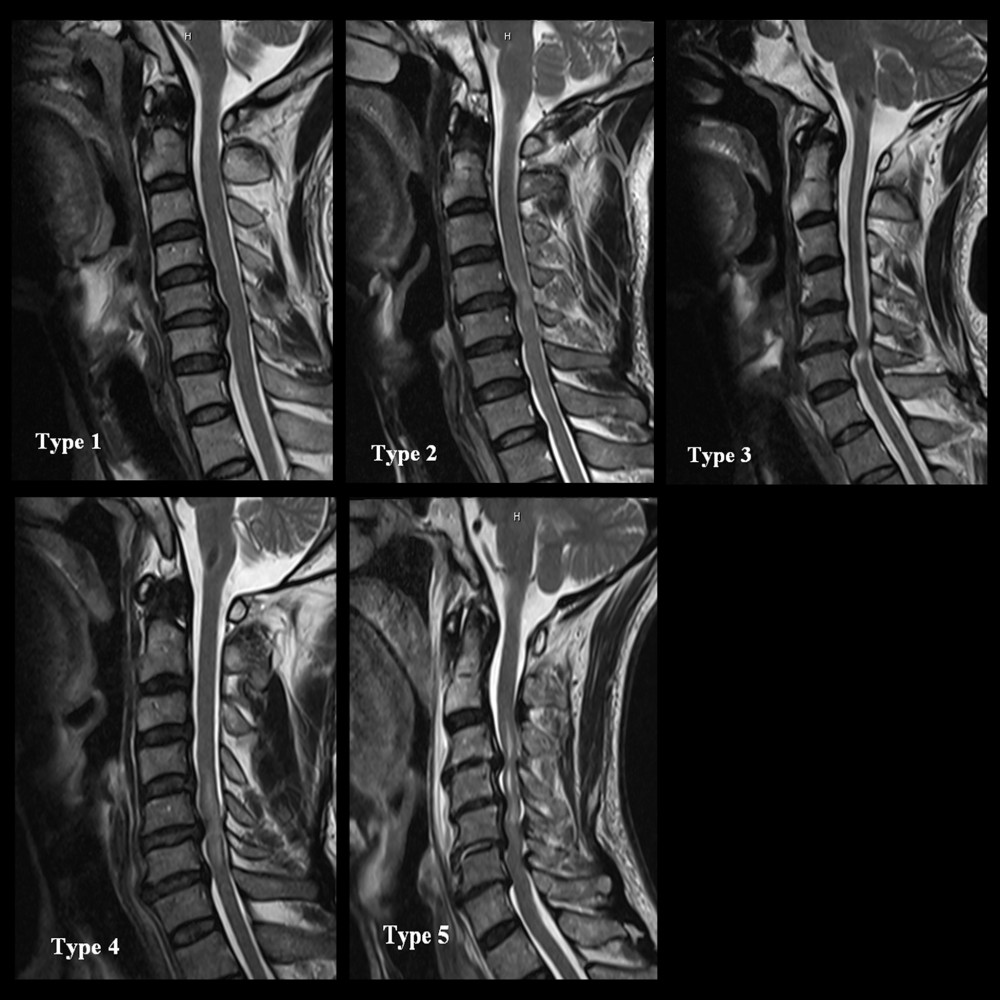 Figure 1. The combined classification of both the quality and longitudinal extent of increased signal intensity (ISI) on T2-weighted images: Type 1 (none/none) displayed normal intensity; Type 2 (focal/faint) displayed focal and faint ISI; Type 3 (focal/intense) displayed focal and intense ISI; Type 4 (multisegmental/faint) displayed multisegmental and faint ISI; and Type 5 (multisegmental/intense) displayed multisegmental and intense ISI.
Figure 1. The combined classification of both the quality and longitudinal extent of increased signal intensity (ISI) on T2-weighted images: Type 1 (none/none) displayed normal intensity; Type 2 (focal/faint) displayed focal and faint ISI; Type 3 (focal/intense) displayed focal and intense ISI; Type 4 (multisegmental/faint) displayed multisegmental and faint ISI; and Type 5 (multisegmental/intense) displayed multisegmental and intense ISI.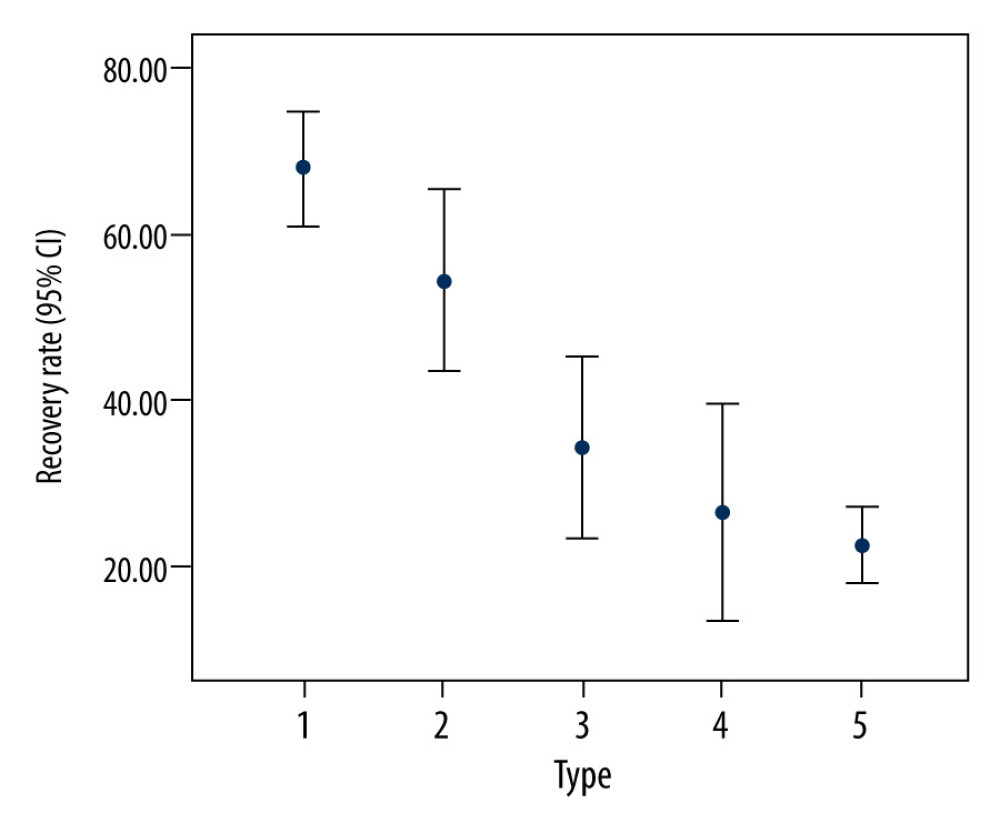 Figure 2. Relationship between recovery rate after surgery for cervical spondylotic myelopathy and preoperative combined classification of increased signal intensity on T2-weighted images.
Figure 2. Relationship between recovery rate after surgery for cervical spondylotic myelopathy and preoperative combined classification of increased signal intensity on T2-weighted images. Tables
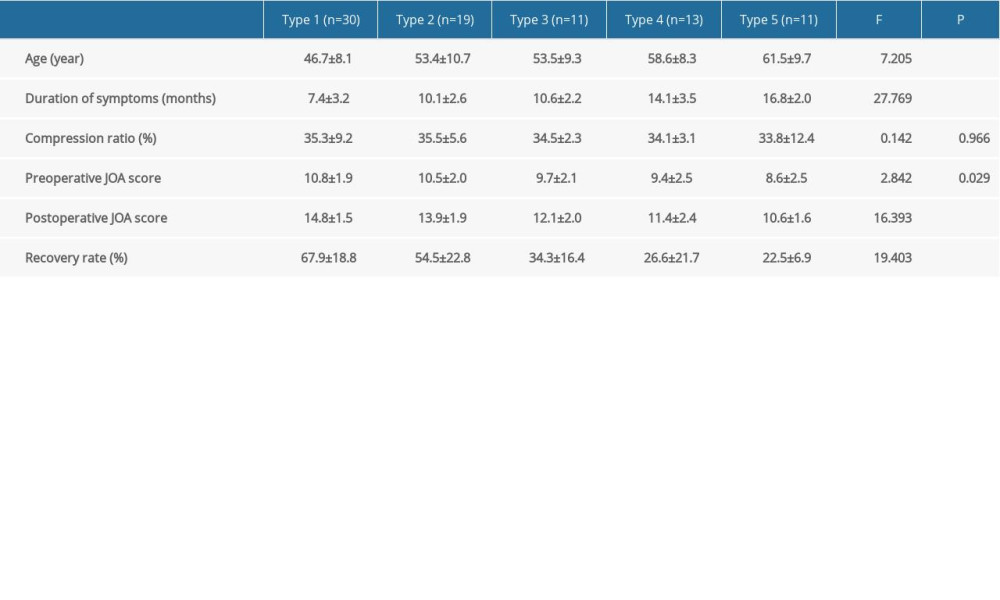 Table 1. Clinical feature and surgical outcome in each of the 5 types.
Table 1. Clinical feature and surgical outcome in each of the 5 types.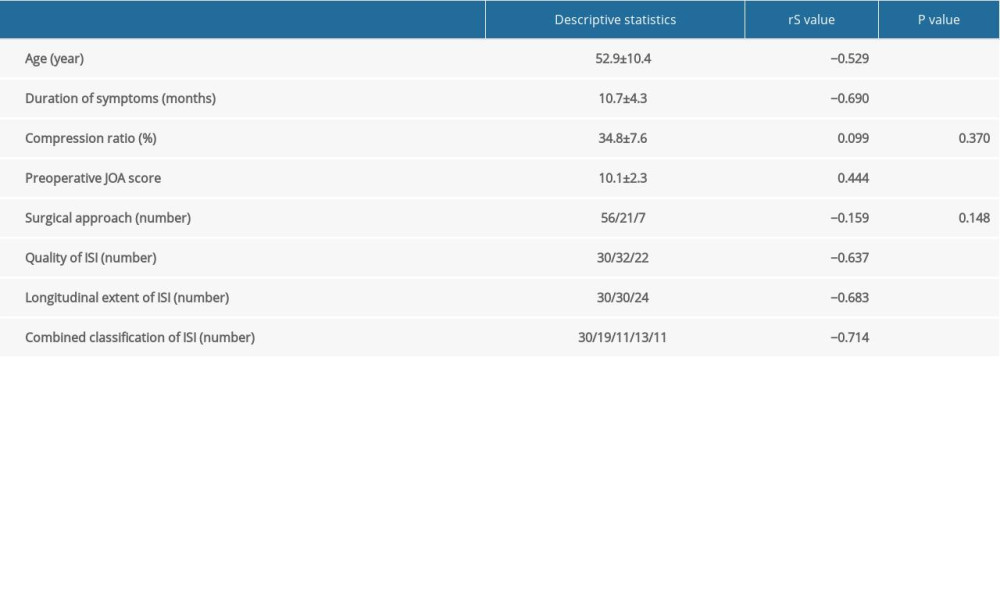 Table 2. Univariate analysis between the recovery rate and clinical features using Spearman’s rank correlation test.
Table 2. Univariate analysis between the recovery rate and clinical features using Spearman’s rank correlation test.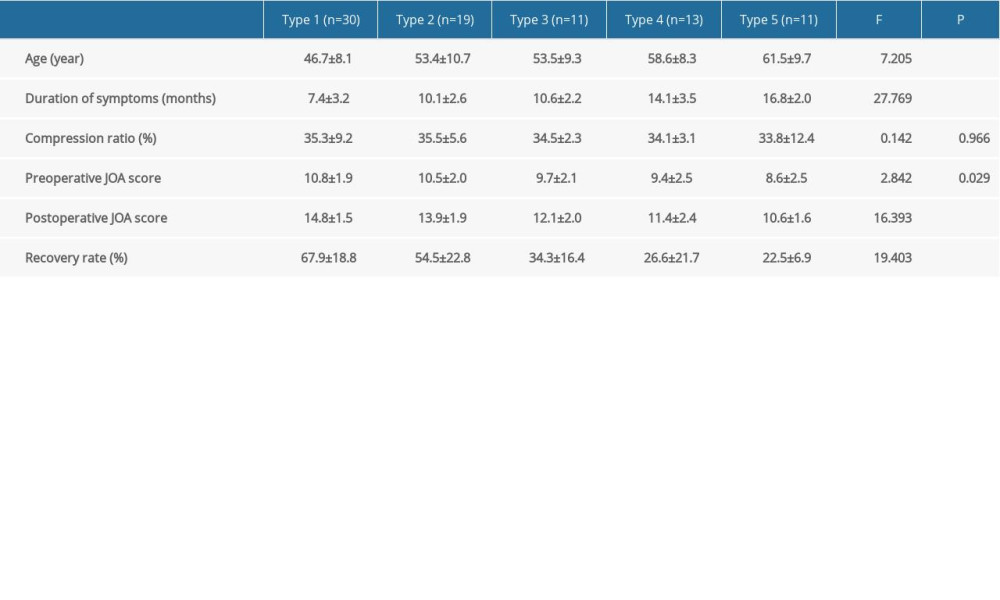 Table 1. Clinical feature and surgical outcome in each of the 5 types.
Table 1. Clinical feature and surgical outcome in each of the 5 types.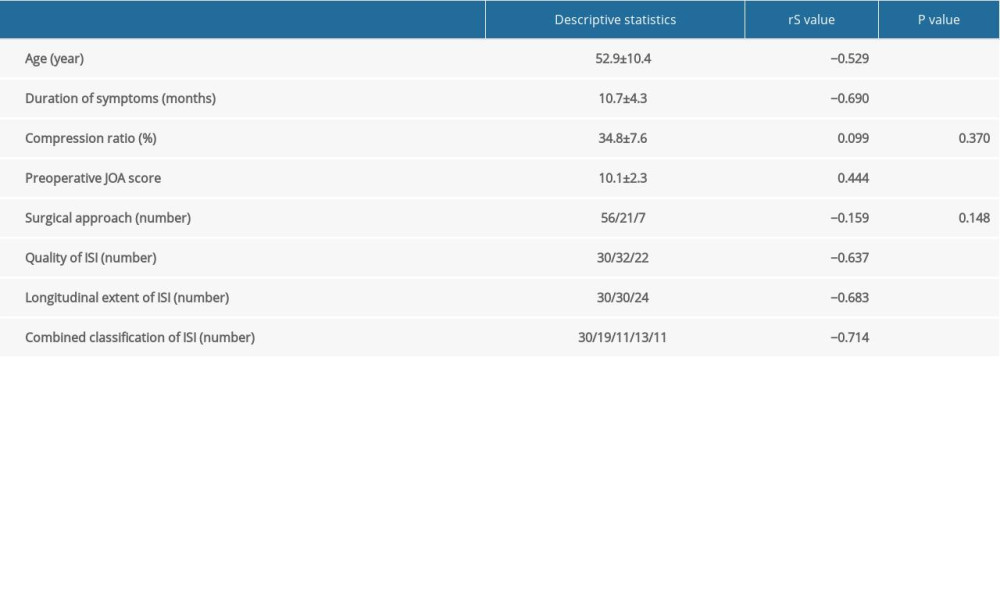 Table 2. Univariate analysis between the recovery rate and clinical features using Spearman’s rank correlation test.
Table 2. Univariate analysis between the recovery rate and clinical features using Spearman’s rank correlation test. In Press
05 Mar 2024 : Clinical Research
Muscular Function Recovery from General Anesthesia in 132 Patients Undergoing Surgery with Acceleromyograph...Med Sci Monit In Press; DOI: 10.12659/MSM.942780
05 Mar 2024 : Clinical Research
Effects of Thermal Insulation on Recovery and Comfort of Patients Undergoing Holmium Laser LithotripsyMed Sci Monit In Press; DOI: 10.12659/MSM.942836
05 Mar 2024 : Clinical Research
Role of Critical Shoulder Angle in Degenerative Type Rotator Cuff Tears: A Turkish Cohort StudyMed Sci Monit In Press; DOI: 10.12659/MSM.943703
06 Mar 2024 : Clinical Research
Comparison of Outcomes between Single-Level and Double-Level Corpectomy in Thoracolumbar Reconstruction: A ...Med Sci Monit In Press; DOI: 10.12659/MSM.943797
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








