25 October 2020: Clinical Research
Model to Predict Need for Subtrochanteric Shortening Osteotomy During Total Hip Arthroplasty for Crowe Type IV Developmental Dysplasia
Hai-yang Ma1CDE, Jing-yang Sun1BE, Yin-qiao Du1F, Zhi-sen Gao1BF, Jun-min Shen1EF, Tie-jian Li1F, Yong-gang Zhou1AA*DOI: 10.12659/MSM.926239
Med Sci Monit 2020; 26:e926239
Abstract
BACKGROUND: Indications for subtrochanteric shortening osteotomy (SSOT) during Crowe type IV developmental dysplasia of the hip (DDH) are unclear. The aim of this retrospective study was to create a model to predict the need for performing SSOT.
MATERIAL AND METHODS: One hundred forty-nine patients (186 hips) with Crowe Type IV DDH who underwent total hip arthroplasty (THA) with S-ROM implants from January 2010 to November 2018 were included in the study. The acetabular components were placed at the true acetabulum and the trial femoral component was inserted. Reduction then was attempted and if it could not be achieved, SSOT was performed. Using multivariable Cox regression analysis, a model was constructed that included age, sex, surgical history, use of a cone- or triangle-shaped sleeve, secondary acetabulum formation, and percentage of dislocation as predictive factors for SSOT.
RESULTS: SSOTs were performed on 140 of 186 hips. Secondary acetabulum formation was present in 27 hips (58.70%) in which SSOT was not performed 7 (5.00%) in which it was performed. Cone-shaped sleeves were used in 17 hips (36.96%) in which SSOT was not performed versus 15 (10.71%) hips in which it was performed. Dislocation occurred in 31.30±5.80% hips in which SSOT was performed versus 24.05±4.39% of those in which it was not performed. Percentage of dislocation was associated with an increased likelihood of SSOT (odds ratio [OR] 1.24, 95% confidence interval 1.11–1.38), whereas secondary acetabulum formation (OR 0.10, 0.03–0.33) and use of a cone-shaped sleeve (0.18, 0.06–0.53) were associated with decreased likelihood of SSOT. We established a model for prediction of SSOT with a nanogram and the discriminative ability (C statistic) of it was 0.918 (0.79–0.92).
CONCLUSIONS: Factors that significantly affect likelihood of performing an SSOT were identified and a model with significant ability to predict the need for SSOT in patients with Crowe Type IV DDH was created.
Keywords: Arthroplasty, Decision Support Techniques, Hip Dislocation, Congenital, Osteotomy, Arthroplasty, Replacement, Hip, developmental dysplasia of the hip, Postoperative Complications, Risk Factors
Background
Developmental dysplasia of the hip (DDH) is a common cause of secondary osteoarthritis in young adults for which total hip arthroplasty (THA) eventually is required [1–4]. Crowe Type IV DDH, which generally is recognized as the most complicated form, is characterized by lateral and anterior acetabular deficiency and abnormality in anteversion, significant dislocation of the proximal femur, narrowing of the femoral canal, and contraction of soft tissue [5,6]. Therefore, in patients with Crowe Type IV DDH, THA is technically demanding and poses challenges to the surgeon on both the acetabular and femoral sides of the hip [7,8].
It is widely accepted by surgeons that placing the cup at the anatomical hip center is biomechanically optimal because it decreases the joint reaction force, increases the lever arm of the abductor musculature, and improves the longevity of the implant [9–11].
However, restoration of the anatomical hip center in patients may lead to unacceptable lengthening of the limb, which can result in complications such as sciatic nerve palsy and injury to arteries [12]. Thus, a femoral shortening osteotomy may be required [13]. To date, proximal, subtrochanteric, and distal osteotomies have been described. Of those techniques, subtrochanteric shortening osteotomy (SSOT) is preferred in our hospital. Although performing an easy and safe reduction is advantageous, it is also technically demanding and can increase blood loss and prolong procedure time, especially in the hands of inexperienced surgeons. Thus, an unnecessary SSOT should be avoided. It is crucial to identify factors that could predispose patients to need for SSOT, but to the best of our knowledge, no study has focused on those issues.
The aims of the present study were to identify factors that affect SSOT and establish a clinical predictive model that can be used to help inexperienced surgeons with preoperative planning.
Material and Methods
PATIENTS:
Our database included 156 patients (193 hips) with Crowe Type IV DDH who were managed with THA in our department from January 2010 to November 2018. Seven patients with THA for Crowe Type IV DDH were excluded: 2 had no preoperative X-rays, 3 were lost to follow-up, and 2 patients had septic hip sequelae. Therefore, 149 consecutive patients with Crowe Type IV DDH and 186 hips were included in our study.
The prostheses used in the patients were modular S-ROM stems (Depuy, Warsaw, Indiana, U.S.A.) and cementless acetabular cups. Duraloc Option cups (Depuy, Warsaw, Indiana, U.S.A.) were used in 33 hips, while Pinnacle cups (Depuy) were used in 153 hips. A 28-mm ceramic head was used in all procedures (Forte ceramic head, N=33; Delta ceramic head, N=53).
Leg length discrepancy (LLD) was measured during clinical examination. Leg length was defined as the distance between the anterior superior iliac spine and the medial malleolus of the leg and the differences in leg lengths calculated were the LLD. We measured and analyzed LLD in patients with unilateral and bilateral Crowe Type IV DDH. The average preoperative LLD in the 119 patients who were diagnosed with unilateral Crowe Type IV DDH was 4.96±1.24 cm (range 3.0–9.0), whereas there was no LLD before THA in the 37 patients who had bilateral Crowe Type IV DDH. At final follow-up, the average LLD in all patients was 0.94±0.45 cm (range 0.3–2.5).
The study participants were divided into SSOT (140 hips; 16 men, 124 women) and non-SSOT groups (46 hips; 1 man, 45 women). No differences were detected between the 2 groups in distribution of age or sex.
Each patient’s medical records were checked and radiographs reviewed to determine the extent of proximal displacement of the femur, the presence of secondary acetabulum, and the type of proximal sleeve of the femoral component: cone or triangle. We defined H1 as dislocation height and H0 as pelvic width. The ratio of H1 to H0 represented the severity of dislocation (Figure 1). If the femoral head was free-floating within the gluteal musculature, we defined it as “without secondary acetabulum” (Figure 1). If the femoral head articulated with the ilium, we defined it as “with secondary acetabulum” (Figure 2). The distance between the inter-teardrop line (A line) and the center of the 28-mm ceramic femoral head was measured, using calibration.
SURGICAL TECHNIQUE:
All procedures were performed by the same senior surgeon, using a posterolateral approach, as described in our previous studies [14,15]. All the acetabular components were placed in their anatomical positions. Adipose tissue and transverse ligaments were used as markers to locate the true acetabulum. The acetabular components were introduced as close as possible to the true acetabulum level. The abnormal anteversion and straight narrow femoral canal seen in Crowe IV DDH were the main reasons for the choice of S-ROM. The modularity of the S-ROM stem facilitated correction of excess anteversion and abnormal offset and restoration of leg length. The shape of the proximal femur dictated the choice of a cone- or triangle-shaped sleeve (Figure 2) [14,16]. In almost all patients, it was possible to use a triangle-shaped sleeve, which is highly desirable because it allows for more rotational control of the proximal fragment. However, with a triangle-shaped sleeve, the prosthesis cannot be implanted deeply, which increases the height of the hip rotation center and inevitably increases the difficulty of performing a safe reduction. With a cone-shaped sleeve, the prosthesis can be implanted deeper and osteotomy avoided when dislocation is not significant. Thus, a cone-shaped sleeve was chosen to reduce unnecessary osteotomy.
In the non-SSOT group, the trial component was implanted and reduction attempted after the femur had been prepared. During a trial of reduction, it was necessary to control rotation of the proximal fragment with the S-ROM sleeve
In the SSOT group, during reduction, we used a caliper to measure the distance between the centers of the acetabular cup and the femoral head prosthesis. The osteotomy site was approximately 2 cm below the trochanter and as close to the sleeve as possible. Osteotomy length was determined with reference to the distance previously measured.
In both groups, reduction was performed as follows. The hip was flexed and internally rotated with persistent distal traction. During reduction, the surgeon applied pressure on the trial femoral head and an assistant firmly fixed the pelvis on the operating table. When the femoral head reached the acetabular rim, a second assistant deflexed and externally rotated the limb to reduce the hip. During the procedure, the level at which the patellar tendon was inserted was used as a marker to evaluate LLD.
When the trial reduction was complete and the patient’s hip was stable and the limb length was acceptable, the prosthesis was implanted. During the procedure, the proximal sleeve was implanted and the femoral stem inserted with appropriate anteversion. Before osteotomy, the femur was marked with an electric knife. During stem implantation, the distal end of the femoral osteotomy was clamped with pliers to ensure good rotation alignment.
POSTOPERATIVE REHABILITATION:
During the first 2 weeks after surgery, patients were asked to flex their hip and knee no more than 30 degrees when in bed so as to protect the neurovascular tissue and avoid excessive stretching. They were encouraged to ambulate as soon as possible and carry out partial weight bearing with the aid of crutches, which were discarded at 6 to 7 weeks postoperatively.
FOLLOW-UP:
Detailed physical examinations were carried out and standard X-rays taken of each patient during follow-up, which lasted at least 3 months. The Harris Hip (HH) score, which rates pain, function, and mobility, was used to assess patient outcome. At each follow-up visit, detailed information was recorded on clinical outcomes and complications in patients.
STATISTICAL ANALYSIS:
Statistics are presented as means±SD for continuous variables and percentages for categorical variables. A two-sided, paired
Results
During the follow-up period, mean HHS scores increased from 52.9±12.1 to 93.2±3.0 (P<0.001). All patients (184 THAs) had good or excellent results, with the exception of 1 patient who underwent 2 THAs and had a fair result. In all cases the acetabular components were introduced into the true acetabulum to restore the anatomical hip center. In all but 1 patient, who had bone nonunion at the osteotomy site, no radiolucent lines were seen. In 140 osteotomies, all but 1 hip were united without complications. The mean healing time was 5.2 months (range 3–9).
Nerve palsy occurred in 2 hips (1.1%) and the symptom disappeared within 1 year. Nonunion at the osteotomy site occurred in 1 hip (0.5%). Femur fracture occurred in 5 hips (2.7%). Deep venous thrombosis occurred in 1 hip (0.5%). Postoperative hip dislocation occurred in 9 hips (4.8%). An obvious LLD of 2.5 cm occurred in 1 patient and a revision was performed.
SSOT was performed on 140 of 186 hips. The mean length of the resected part of the proximal femur in patients who underwent SSOT was 3.6±0.9 cm (2.0–6.0).
The demographic and clinical characteristics of the 2 groups are shown in Table 1.
Surgery had previously been performed on 7 hips (15.22%) in patients in the non-SSOT group versus 8 hips (5.71%) in the SSOT group. Secondary acetabulum formation was present in 27 hips (58.70%) in the non-SSOT group versus 7 (5.00%) in the SSOT group. A cone-shaped sleeve was used in 17 hips (36.96%) in the SSOT group versus 15 hips (10.71%) in the non-SSOT group. The average dislocation height was 5.56±1.16 cm in the SSOT group versus 4.15±0.97 cm in the non-SST group. The mean H1/H0 ratio was 31.30±5.80% in the SSOT group versus 24.05±4.39% in the non-SSOT group.
After multivariate regression analysis, presence of a secondary acetabulum, use of a cone-shaped sleeve, dislocation height, and H1/H0 ratio were significantly different between the 2 groups. A secondary acetabulum and use of a cone-shaped sleeve decreased the likelihood of SSOT whereas a higher H1/H0 ratio increased the likelihood of its performance (Table 2).
Using the previously described variables, a clinical predictive model for SSOT was created. The corresponding nomogram is shown in Figure 3. To establish the clinical prediction model, the H1/H10 ratio, which reflects location severity, was used as an indicator rather than the specific dislocation height. For example, in patients with 30% dislocation (score 35 points; black arrow), no secondary acetabulum (score 45 points; green arrow), and use of a triangle-shaped sleeve (35 points; blue arrow), the total score was 110 (red arrow) and the corresponding probability of osteotomy was greater than 90% (Figure 3). The C-index of the clinical prediction model was 0.918, which implies a high predictive value (Figure 4).
Discussion
The present study is the first to investigate risk factors for performance of SSOT in high-riding DDH by analyzing a large-sample cohort with S-ROM prostheses. Clinical results after SSOT are promising, but it is not a complication-free method [17]. In our clinical practice, we have found that in some patients with Crowe Type IV DDH, it is possible to perform THA without SSOT, but in others it is necessary to perform femoral shortening.
Based on our data, the H1/H0 ratio increases the likelihood of using SSOT, while a secondary acetabulum and use of an intraoperative cone-shaped sleeve decrease the likelihood. In addition, we created a predictive model to help inexperienced surgeons develop preoperative plans that will support excellent clinical outcomes.
In the present study, patients had significant improvement in hip function. Rates of intraoperative fracture, postoperative dislocation, and nerve injury were 2.7%, 4.8%, and 1.1%, respectively. Previous studies [18–22] have reported intraoperative fracture rates as high as 28%, postoperative dislocation rates ranging from 1% to 17%, and nerve injury rates of approximately 10%. These comparisons indicate that the decision-making in the present study was appropriate and can be used as the basis for establishing a predictive model.
Higuchi et al. reported that leg lengthening by >5 cm should be avoided to prevent sciatic nerve injury [23]. Kabata et al. found that lengthening the femoral shaft by more than 8.7% results in a high risk of neurologic or soft tissue complications following primary THA [24]. Placing the acetabular prosthesis at the anatomic level would inevitably lengthen the limb and increase the risk of neurovascular injury when THA is performed in patients with Crowe Type IV DDH. When the degree of dislocation is increased, subtrochanteric osteotomy is optimal for avoiding neurovascular injury caused by violent reduction. In the present study, we used the H1/H0 ratio rather than the height of dislocation as a factor in evaluating the likelihood of need for SSOT. The true degree of dislocation is influenced not only by the height of dislocation but also by the height of the pelvis. Therefore, a patient with a small pelvis may have a more severe condition even if the 2 heights are the same. The higher the dislocation, the more severe the soft tissue contracture and the more difficult the reduction. Sankar et al. suggested that previous superior displacement of the proximal femur >30% of pelvic width could be an indicator for SSOT [25]. In the present study, SSOT was required when the dislocation was greater than 30%, there was no secondary acetabular formation, and a triangle-shaped sleeve was used.
Secondary acetabulum formation is a predictive factor that can decrease the likelihood of SSOT. Hartofilakidis [26] suggested that high hip dislocation could be divided into 2 subtypes according to the presence or absence of a secondary acetabulum. Zhou et al. [27] found that the 2 subtypes differed in morphology, and the proximal femur with a secondary acetabulum developed better. Xu et al. [28] demonstrated that the presence or absence of a secondary acetabulum in high hip dislocations is associated with different loading patterns, which can affect the development and shape of the proximal femur [26,28,29]. A secondary acetabulum can stimulate femur development, thus resulting in deep seating of the femoral prosthesis and restoration of the normal rotation center of the head.
Based on our data, cone use also was a predictive factor. That may be because it can encourage deep seating of the sleeve and a lower center of rotation, decreasing the probability of needing to perform SSOT. The indication for use of a cone sleeve is narrowing at the distal end of the proximal femoral medullary cavity, which reduces the available space such that a triangle sleeve cannot be implanted. In addition, for some patients with Crowe Type IV DDH, use of a cone to achieve prosthetic sinking can avert the need for SSOT, even if the proximal femur is relatively well developed.
We have provided a clear protocol for when an SSOT can be performed during a THA, especially by inexperience surgeons, and we also developed a nomogram that can predict the need for SSOT. With these tools, unnecessary repeated attempts at reduction or forced reduction can be avoided, reducing neurovascular damage. The preoperative planning process also can be improved, resulting in shorter operations and less blood loss.
For the nanogram, the C-index value of our predictive model was as high as 0.918 (95% confidence interval, 0.79 to 0.92), which means it was highly accurate for predicting the need for SSOT. In addition, the curve fit was good, indicating that the model is valid.
The present study has several limitations. First, it was single-center and retrospective. Second, only one type of S-ROM femoral component was used in all the SSOT procedures. Finally, the model we created does not take into account the effect of the contralateral side on the clinical decision to perform SSTO in patients with bilateral Crowe Type IV DDH. A future study with a large number of patients is required to validate the model.
Conclusions
Clinical results with SSOT are promising, but the technique is not complication-free. In the present study, we demonstrated that 3 key factors can predict the likelihood of performing SSOT in patients undergoing THA for Crowe Type IV DDH. We created a protocol and developed a nomogram that can help inexperienced surgeons predict whether SSOT will be necessary. By using the nomogram, it may be possible to avoid unnecessary repeated attempts at reduction or forced reduction.
Figures
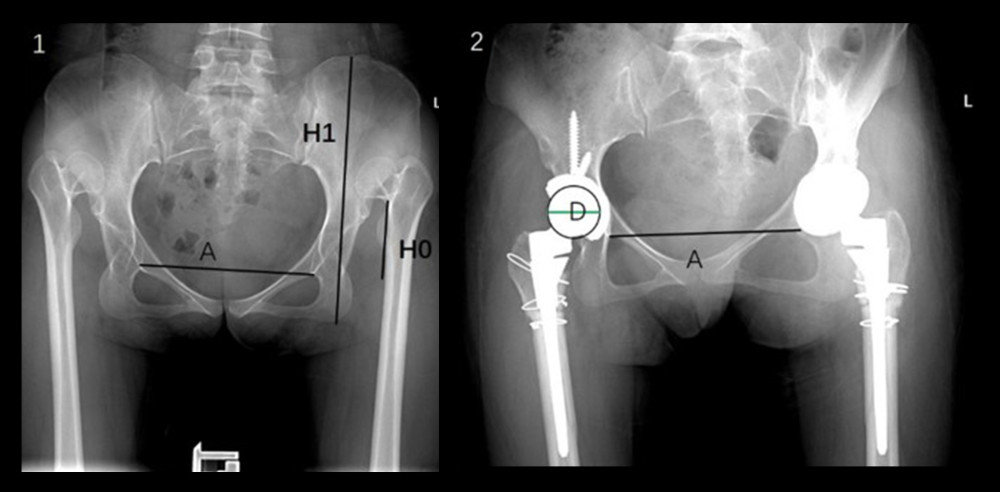 Figure 1. Measurement of dislocation height on anteroposterior radiographs. A: Inter-teardrop line. H0: Dislocation height, defined as the vertical distance from the junction of the femoral head and neck to the inter-teardrop line. H1: Pelvic width, defined as the vertical distance between the horizontal line of the highest point of the pelvis and the horizontal line of the lowest point of the pelvis. D: Femoral head diameter (28 mm), as a calibration standard.
Figure 1. Measurement of dislocation height on anteroposterior radiographs. A: Inter-teardrop line. H0: Dislocation height, defined as the vertical distance from the junction of the femoral head and neck to the inter-teardrop line. H1: Pelvic width, defined as the vertical distance between the horizontal line of the highest point of the pelvis and the horizontal line of the lowest point of the pelvis. D: Femoral head diameter (28 mm), as a calibration standard. 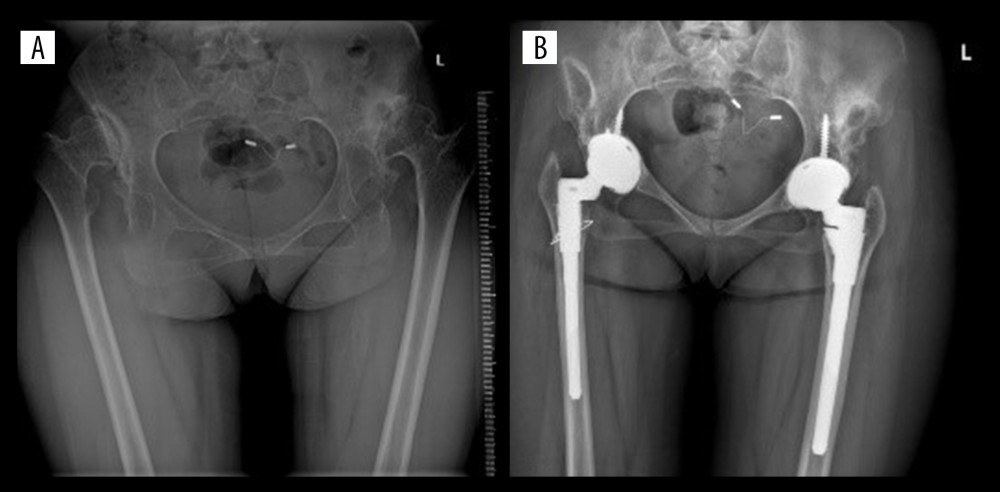 Figure 2. Total hip arthroplasty with S-ROM prosthesis in patients with bilateral Crowe Type IV DDH. (A) Preoperative radiograph: secondary acetabulum formation in bilateral hips; (B) Postoperative radiograph: S-ROM prosthesis with cone-shaped sleeve (right) and S-ROM prosthesis with triangle-shaped sleeve (left).
Figure 2. Total hip arthroplasty with S-ROM prosthesis in patients with bilateral Crowe Type IV DDH. (A) Preoperative radiograph: secondary acetabulum formation in bilateral hips; (B) Postoperative radiograph: S-ROM prosthesis with cone-shaped sleeve (right) and S-ROM prosthesis with triangle-shaped sleeve (left). 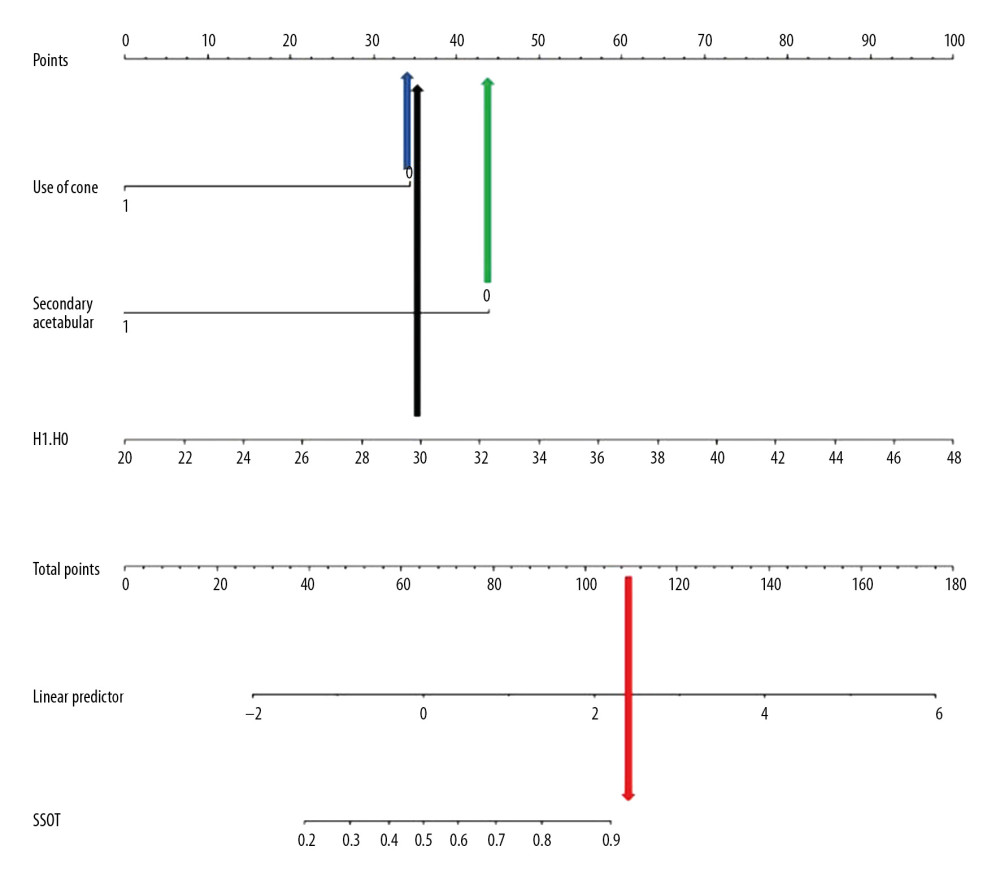 Figure 3. A clinical model with nomogram for predicting the likelihood of performing SSOT on patients with Crowe Type IV developmental dysplasia of the hip. Each factor corresponds to a specific point in a line on the axis. The likelihood of SSOT corresponds to the total of the points.
Figure 3. A clinical model with nomogram for predicting the likelihood of performing SSOT on patients with Crowe Type IV developmental dysplasia of the hip. Each factor corresponds to a specific point in a line on the axis. The likelihood of SSOT corresponds to the total of the points. 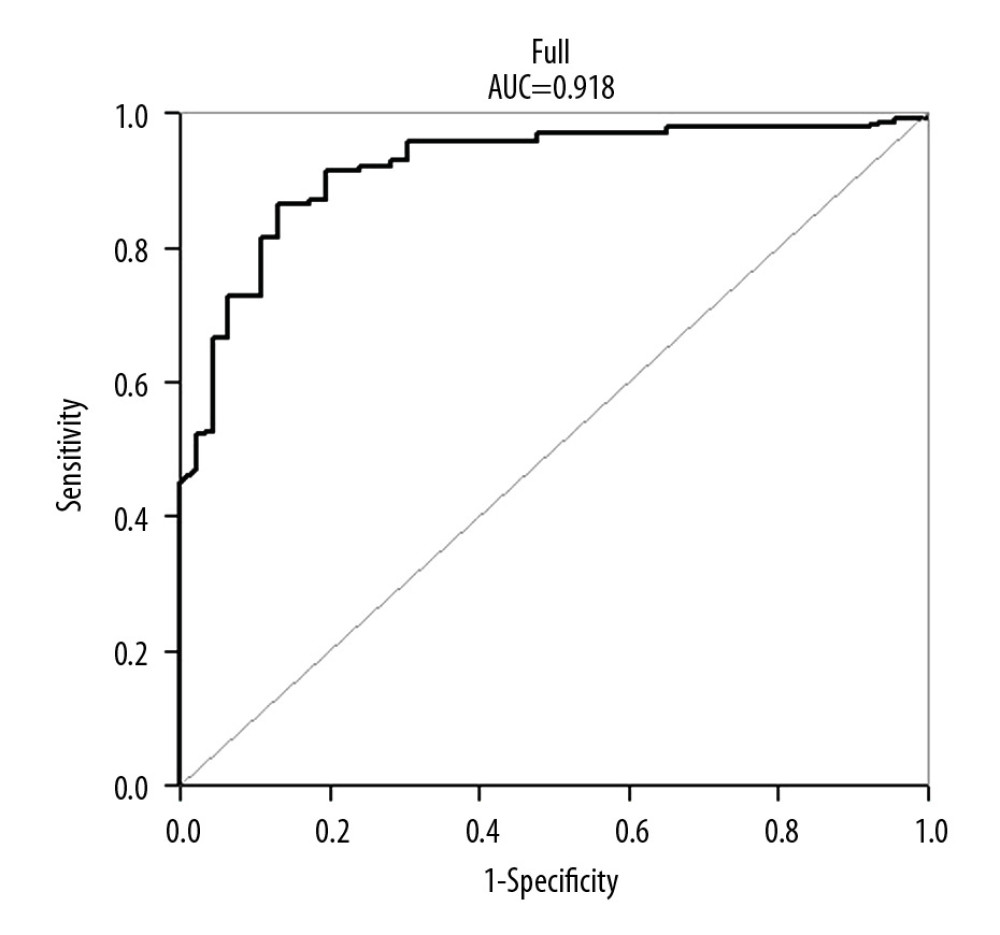 Figure 4. Receiver operating characteristic curve of the discriminatory ability of the model, as measured by the C-index, which was 0.831 (95% confidence interval, 0.784–0.878).
Figure 4. Receiver operating characteristic curve of the discriminatory ability of the model, as measured by the C-index, which was 0.831 (95% confidence interval, 0.784–0.878). References
1. Jacobsen S, Sonne-Holm S, Soballe K, Hip dysplasia and osteoarthrosis: A survey of 4151 subjects from the Osteoarthrosis Substudy of the Copenhagen City Heart Study: Acta Orthop, 2005; 76; 149-58
2. Sanchez-Sotelo J, Berry DJ, Trousdale RT, Cabanela ME, Surgical treatment of developmental dysplasia of the hip in adults: II. Arthroplasty options: J Am Acad Orthop Surg, 2002; 10; 334-44
3. Hartofilakidis G, Karachalios T, Georgiades G, Kourlaba G, Total hip arthroplasty in patients with high dislocation: A concise follow-up, at a minimum of fifteen years, of previous reports: J Bone Joint Surg Am, 2011; 93; 1614-18
4. Tian FD, Zhao DW, Wang W, Prevalence of developmental dysplasia of the hip in chinese adults: A cross-sectional survey: Chin Med J (Engl), 2017; 130; 1261-68
5. Engesaeter LB, Engesaeter IO, Fenstad AM, Low revision rate after total hip arthroplasty in patients with pediatric hip diseases: Acta Orthop, 2012; 83; 436-41
6. Sochart DH, Porter ML, The long-term results of Charnley low-friction arthroplasty in young patients who have congenital dislocation, degenerative osteoarthrosis, or rheumatoid arthritis: J Bone Joint Surg Am, 1997; 79; 1599-617
7. Bao N, Meng J, Zhou L, Lesser trochanteric osteotomy in total hip arthroplasty for treating CROWE type IV developmental dysplasia of hip: Int Orthop, 2013; 37; 385-90
8. Rosenfeld SB, Weinstein SL, Schoenecker JG, Matheney T, Developmental dysplasia of the hip from birth to arthroplasty: Clear indications and new controversies: Instr Course Lect, 2019; 68; 319-36
9. Pagnano W, Hanssen AD, Lewallen DG, Shaughnessy WJ, The effect of superior placement of the acetabular component on the rate of loosening after total hip arthroplasty: J Bone Joint Surg Am, 1996; 78; 1004-14
10. Yoder SA, Brand RA, Pedersen DR, O’Gorman TW, Total hip acetabular component position affects component loosening rates: Clin Orthop Relat Res, 1988(228); 79-87
11. Crowe JF, Mani VJ, Ranawat CS, Total hip replacement in congenital dislocation and dysplasia of the hip: J Bone Joint Surg Am, 1979; 61; 15-23
12. Eggli S, Hankemayer S, Muller ME, Nerve palsy after leg lengthening in total replacement arthroplasty for developmental dysplasia of the hip: J Bone Joint Surg Br, 1999; 81; 843-45
13. Krych AJ, Howard JL, Trousdale RT, Total hip arthroplasty with shortening subtrochanteric osteotomy in Crowe type-IV developmental dysplasia: Surgical technique: J Bone Joint Surg Am, 2010; 92(Suppl 1 Pt 2); 176-87
14. Wang S, Zhou Y, Ma H, Mid-term results of total hip replacement with subtrochanteric osteotomy, modular stem, and ceramic surface in Crowe IV hip dysplasia: Arthroplast Today, 2018; 4(3); 363-69
15. Du Y, Sun J, Ma H, Leg length balance in total hip arthroplasty for patients with unilateral Crowe Type IV developmental dysplasia of the hip: Orthop Surg, 2020; 12(3); 749-55
16. Zhou YG, Zhang Q, Wang YA comparative study of the role of two femoral shortening techniques in total hip arthroplasty on patients with Crowe’s IV congenital dislocated hips: Zhonghua Wai Ke Za Zhi, 2008; 46(17); 1288-92 [in Chinese]
17. Necas L, Hrubina M, Melisik M, Cementless hip arthroplasty and transverse shortening femoral osteotomy with the S-ROM stem for Crowe type IV developmental dysplasia: Eur J Orthop Surg Traumatol, 2019; 29(5); 1025-33
18. Mu W, Yang D, Xu B, Midterm outcome of cementless total hip arthroplasty in Crowe IV-Hartofilakidis Type III developmental dysplasia of the hip: J Arthroplast, 2016; 31; 668-75
19. Sofu H, Kockara N, Gursu S, Transverse subtrochanteric shortening osteotomy during cementless total hip arthroplasty in Crowe Type-III or IV developmental dysplasia: J Arthroplast, 2015; 30; 1019-23
20. Bernasek TL, Haidukewych GJ, Gustke KA, Total hip arthroplasty requiring subtrochanteric osteotomy for developmental hip dysplasia: 5- to 14-year results: J Arthroplast, 2007; 22(6 Suppl 2); 145-50
21. Kong X, Chai W, Chen J, Intraoperative monitoring of the femoral and sciatic nerves in total hip arthroplasty with high-riding developmental dysplasia: Bone Joint J; 2019; 1438-46
22. Ding ZC, Zeng WN, Mou P, Risk of dislocation after total hip arthroplasty in patients with Crowe Type IV developmental dysplasia of the hip: Orthop Surg, 2020; 12; 589-600
23. Higuchi Y, Hasegawa Y, Ishiguro N, Leg lengthening of more than 5 cm is a risk factor for sciatic nerve injury after total hip arthroplasty for adult hip dislocation: Nagoya Med Sci, 2015; 77; 455-63
24. Kabata T, Kajino Y, Inoue D, Safety range for acute limb lengthening in primary total hip arthroplasty: Int Orthop, 2019; 43(9); 2047-56
25. Sankar WN, Tang EY, Moseley CF, Predictors of the need for femoral shortening osteotomy during open treatment of developmental dislocation of the hip: J Pediatr Orthop, 2009; 29; 868-71
26. Hartofilakidis G, Yiannakopoulos CK, Babis GC, The morphologic variations of low and high hip dislocation: Clin Orthop Relat Res, 2008; 466(4); 820-24
27. Ma HY, Zhou YG, Zheng CNew classification of Crowe type IV developmental dysplasia of the hip: Zhongguo Gu Shang, 2016; 29(5); 119-24 [in Chinese]
28. Xu H, Zhou Y, Liu Q, Femoral morphologic differences in subtypes of high developmental dislocation of the hip: Clin Orthop Relat Res, 2010; 468(12); 3371-76
29. Sugano N, Noble PC, Kamaric E, The morphology of the femur in developmental dysplasia of the hip: J Bone Joint Surg Br, 1998; 80; 711-19
Figures
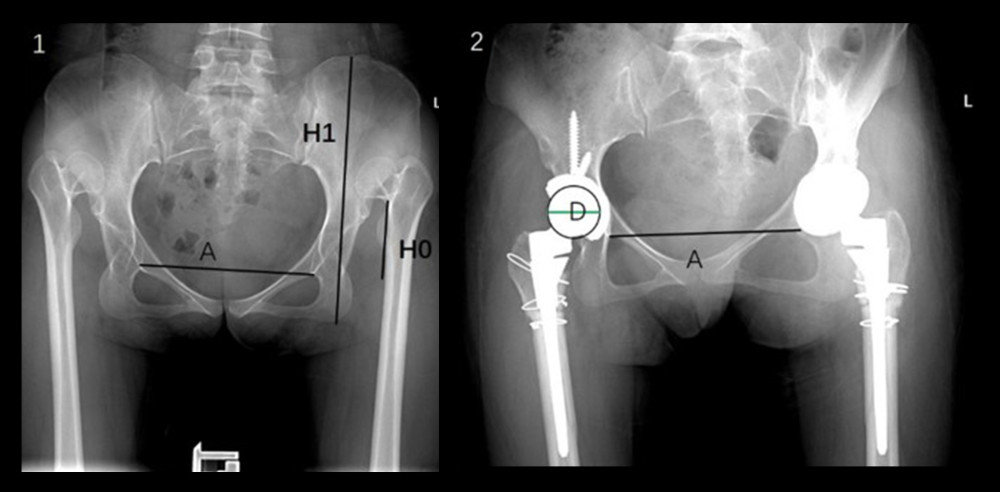 Figure 1. Measurement of dislocation height on anteroposterior radiographs. A: Inter-teardrop line. H0: Dislocation height, defined as the vertical distance from the junction of the femoral head and neck to the inter-teardrop line. H1: Pelvic width, defined as the vertical distance between the horizontal line of the highest point of the pelvis and the horizontal line of the lowest point of the pelvis. D: Femoral head diameter (28 mm), as a calibration standard.
Figure 1. Measurement of dislocation height on anteroposterior radiographs. A: Inter-teardrop line. H0: Dislocation height, defined as the vertical distance from the junction of the femoral head and neck to the inter-teardrop line. H1: Pelvic width, defined as the vertical distance between the horizontal line of the highest point of the pelvis and the horizontal line of the lowest point of the pelvis. D: Femoral head diameter (28 mm), as a calibration standard.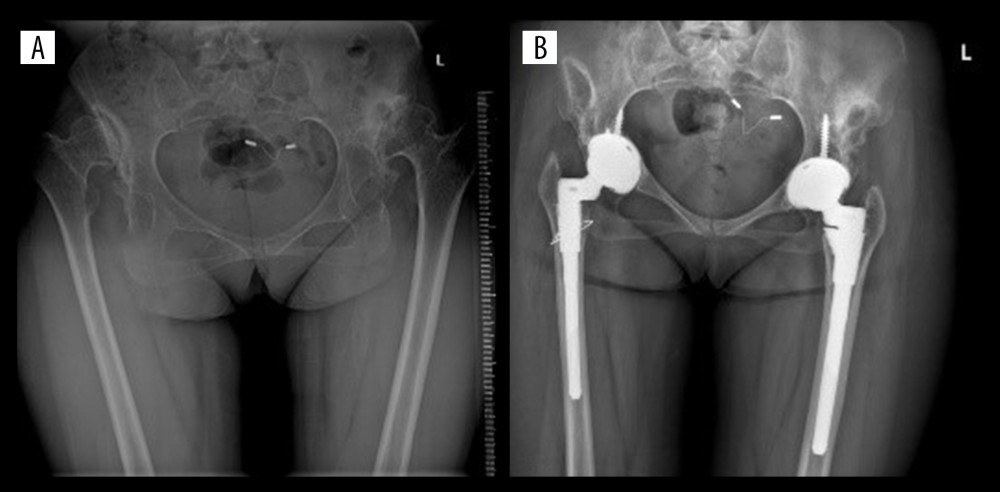 Figure 2. Total hip arthroplasty with S-ROM prosthesis in patients with bilateral Crowe Type IV DDH. (A) Preoperative radiograph: secondary acetabulum formation in bilateral hips; (B) Postoperative radiograph: S-ROM prosthesis with cone-shaped sleeve (right) and S-ROM prosthesis with triangle-shaped sleeve (left).
Figure 2. Total hip arthroplasty with S-ROM prosthesis in patients with bilateral Crowe Type IV DDH. (A) Preoperative radiograph: secondary acetabulum formation in bilateral hips; (B) Postoperative radiograph: S-ROM prosthesis with cone-shaped sleeve (right) and S-ROM prosthesis with triangle-shaped sleeve (left).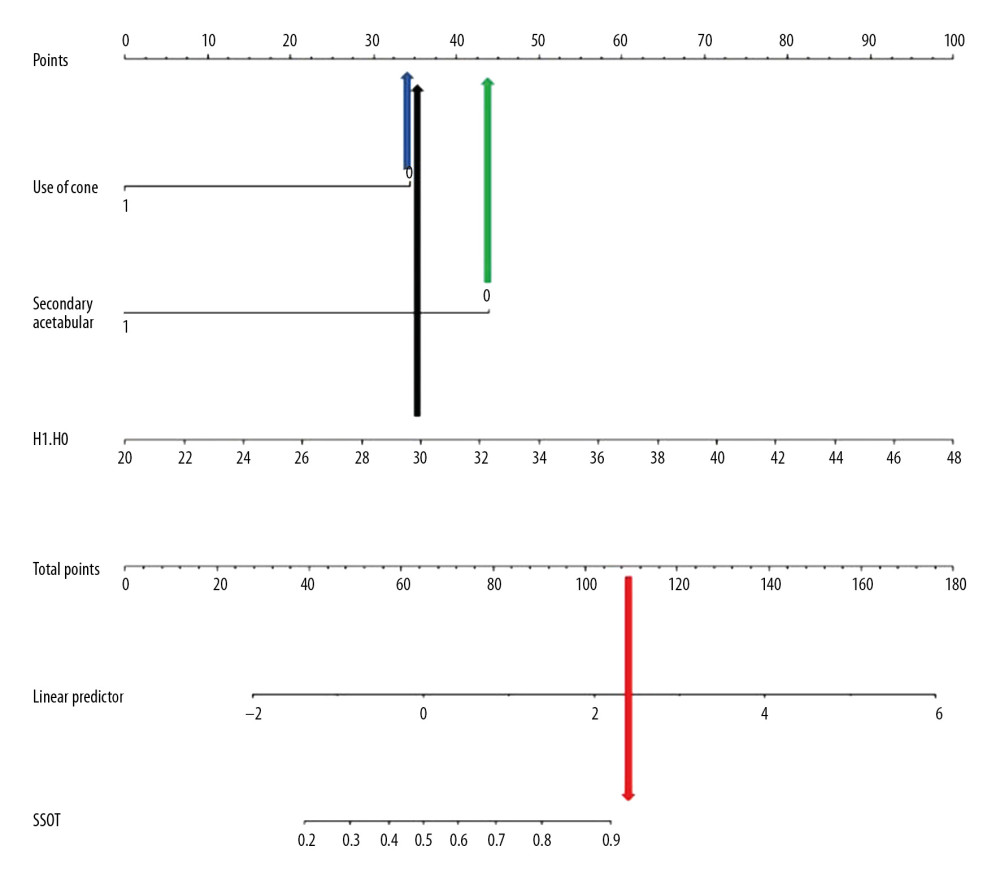 Figure 3. A clinical model with nomogram for predicting the likelihood of performing SSOT on patients with Crowe Type IV developmental dysplasia of the hip. Each factor corresponds to a specific point in a line on the axis. The likelihood of SSOT corresponds to the total of the points.
Figure 3. A clinical model with nomogram for predicting the likelihood of performing SSOT on patients with Crowe Type IV developmental dysplasia of the hip. Each factor corresponds to a specific point in a line on the axis. The likelihood of SSOT corresponds to the total of the points.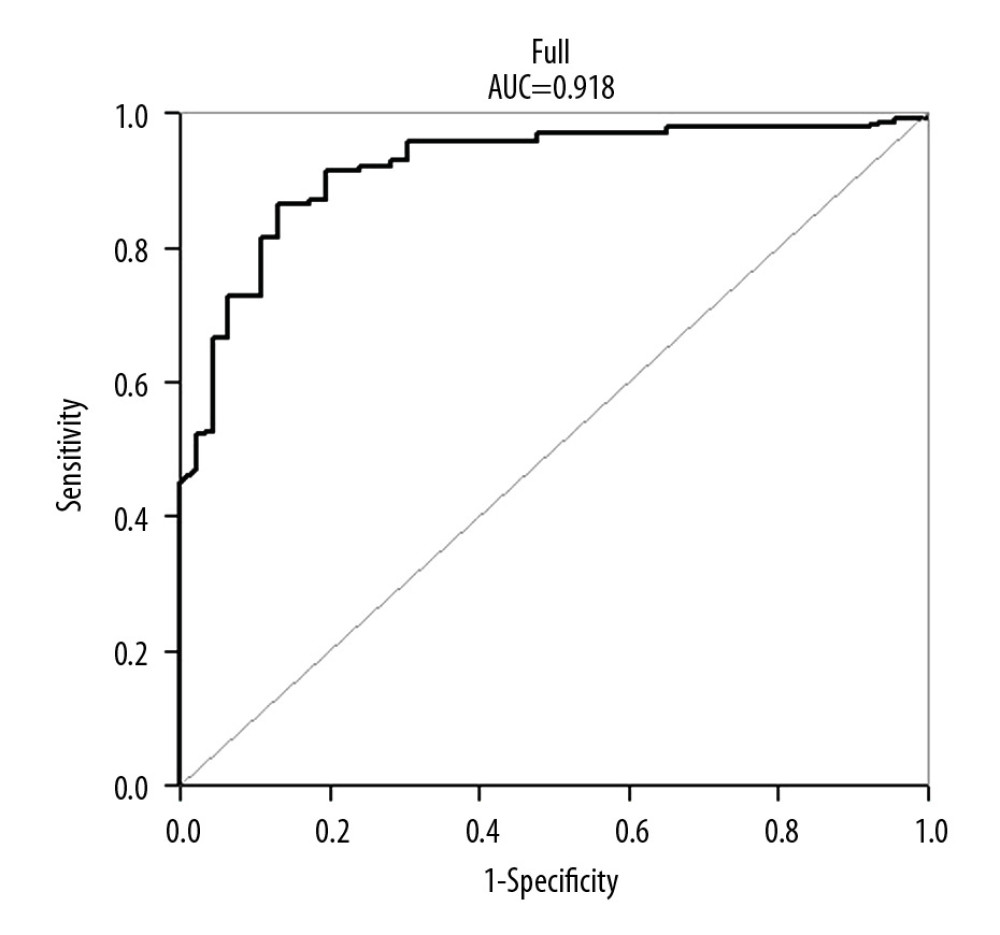 Figure 4. Receiver operating characteristic curve of the discriminatory ability of the model, as measured by the C-index, which was 0.831 (95% confidence interval, 0.784–0.878).
Figure 4. Receiver operating characteristic curve of the discriminatory ability of the model, as measured by the C-index, which was 0.831 (95% confidence interval, 0.784–0.878). Tables
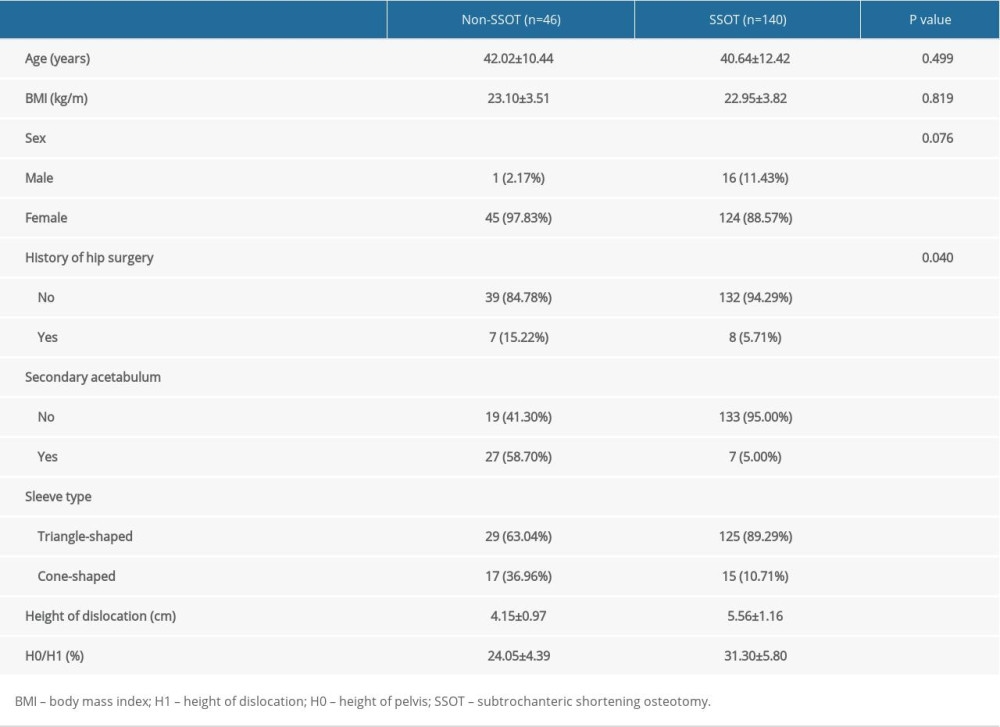 Table 1. Demographic and clinical characteristics of patients with Crowe Type IV DDH in the non-SSOT and SSOT groups.
Table 1. Demographic and clinical characteristics of patients with Crowe Type IV DDH in the non-SSOT and SSOT groups.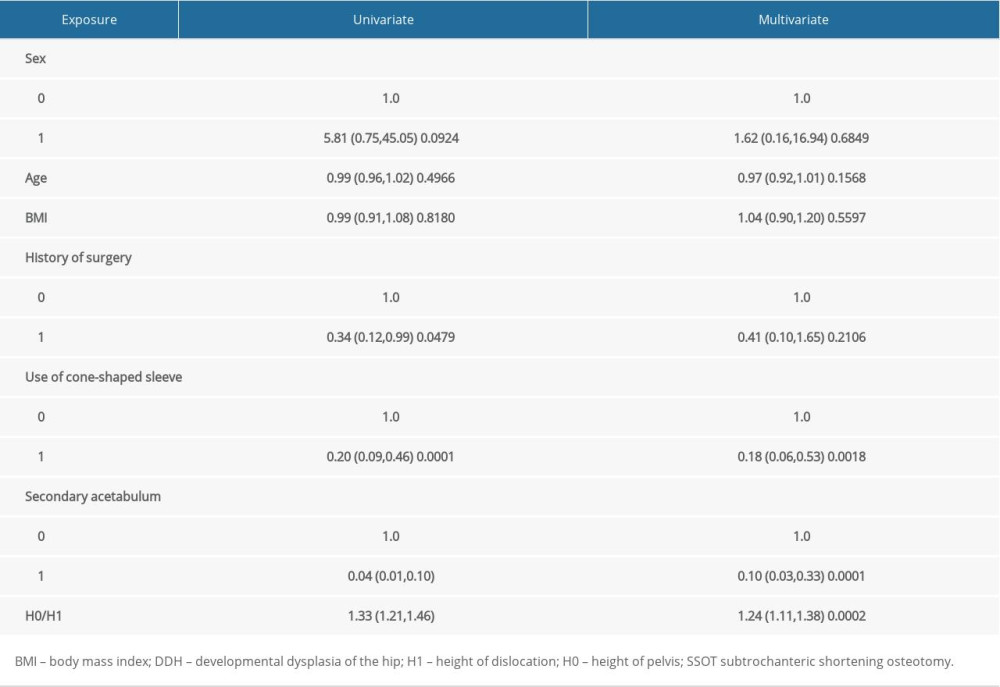 Table 2. Predictive factors for SSOT use in patients with Crowe Type IV DDH according to Cox proportional hazards regression models.
Table 2. Predictive factors for SSOT use in patients with Crowe Type IV DDH according to Cox proportional hazards regression models.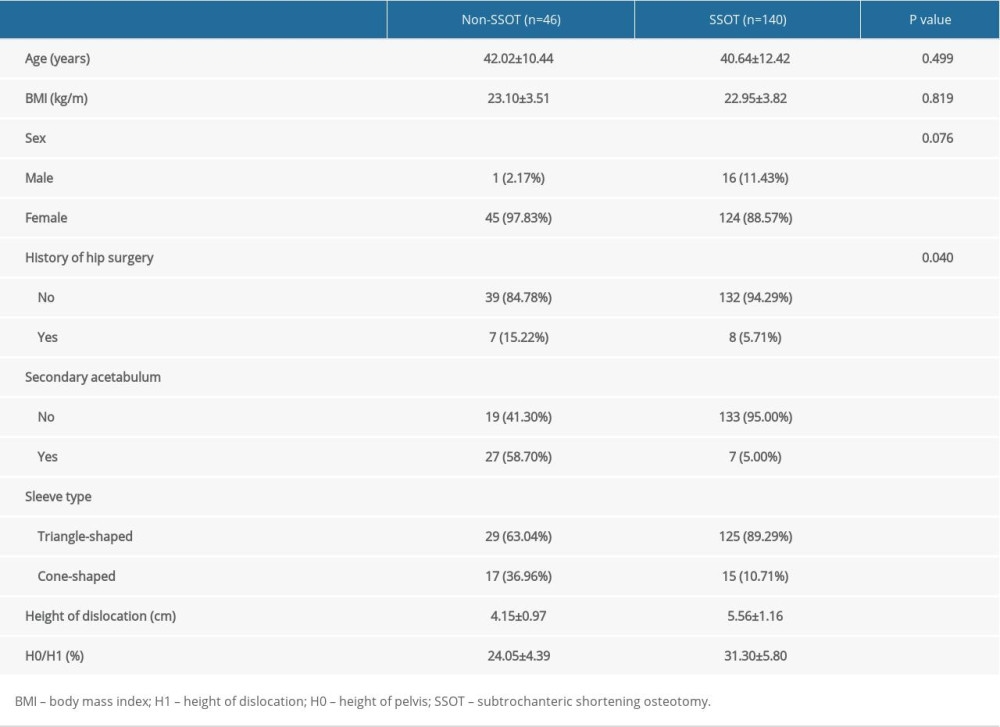 Table 1. Demographic and clinical characteristics of patients with Crowe Type IV DDH in the non-SSOT and SSOT groups.
Table 1. Demographic and clinical characteristics of patients with Crowe Type IV DDH in the non-SSOT and SSOT groups.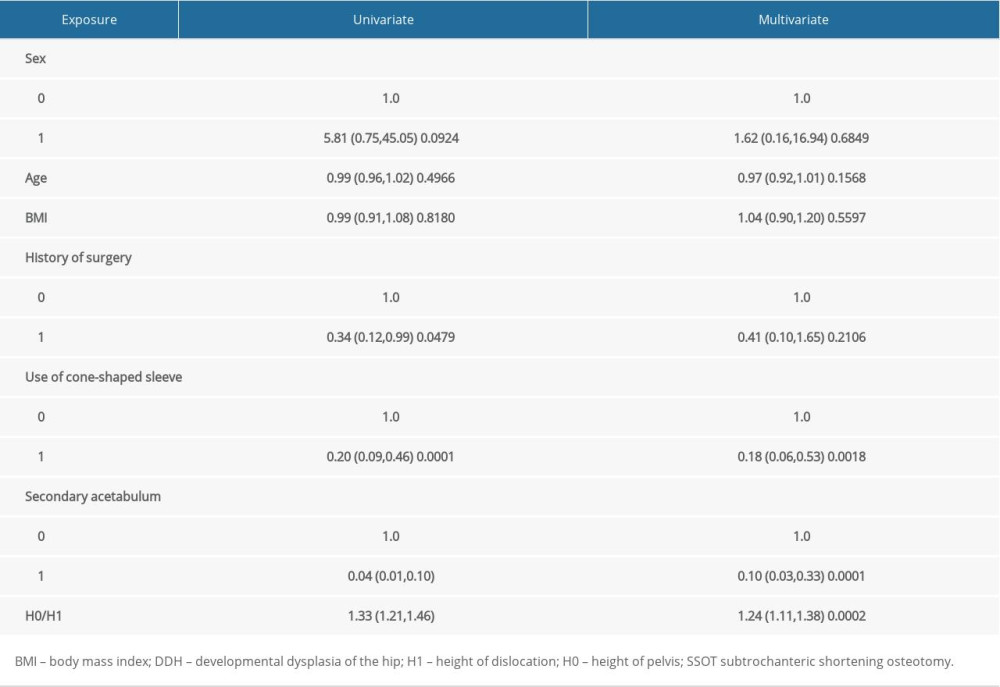 Table 2. Predictive factors for SSOT use in patients with Crowe Type IV DDH according to Cox proportional hazards regression models.
Table 2. Predictive factors for SSOT use in patients with Crowe Type IV DDH according to Cox proportional hazards regression models. In Press
06 Mar 2024 : Clinical Research
Comparison of Outcomes between Single-Level and Double-Level Corpectomy in Thoracolumbar Reconstruction: A ...Med Sci Monit In Press; DOI: 10.12659/MSM.943797
21 Mar 2024 : Meta-Analysis
Economic Evaluation of COVID-19 Screening Tests and Surveillance Strategies in Low-Income, Middle-Income, a...Med Sci Monit In Press; DOI: 10.12659/MSM.943863
10 Apr 2024 : Clinical Research
Predicting Acute Cardiovascular Complications in COVID-19: Insights from a Specialized Cardiac Referral Dep...Med Sci Monit In Press; DOI: 10.12659/MSM.942612
06 Mar 2024 : Clinical Research
Enhanced Surgical Outcomes of Popliteal Cyst Excision: A Retrospective Study Comparing Arthroscopic Debride...Med Sci Monit In Press; DOI: 10.12659/MSM.941102
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








