25 December 2020: Clinical Research
Comparison of the Clinical Efficacy of 3 Surgical Methods for Treating Spinal Tuberculosis in Children
Weidong Liang1ACDEF, Jian Zhang1ACDEF, Zhouliang Ren1BC, Maierdan Maimaiti1B, Fulati Mamati1B, Yakefu Abulizi1B, Tao Xu1C, Rui Cao1C, Jun Sheng1AE*, Weibin Sheng1AEDOI: 10.12659/MSM.926142
Med Sci Monit 2020; 26:e926142
Abstract
BACKGROUND: This study aimed to investigate the safety and clinical efficacy of 3 different surgical methods for treating spinal tuberculosis (ST) in children.
MATERIAL AND METHODS: We reviewed the cases of 62 children with ST who were treated in our hospital from January 2010 to December 2014. In this study, erythrocyte sedimentation rate (ESR), C-reactive protein (CRP) level, Frankel classification of neurological function, pain visual analog scale (VAS) score, and kyphosis Cobb (k-Cobb) angle were dynamically monitored to evaluate the efficacy of different surgical methods. Complications in the patients were evaluated at 3 time points: before surgery (T1), after surgery (T2), and during final follow-up (T3). The average follow-up was 27.4 months. Twenty-two patients underwent simple anterior debridement alone or combined with internal fixation (Method A), 13 patients underwent posterior debridement alone (Method B), and 27 patients received anteroposterior debridement and bone graft fusion together with internal fixation (Method C).
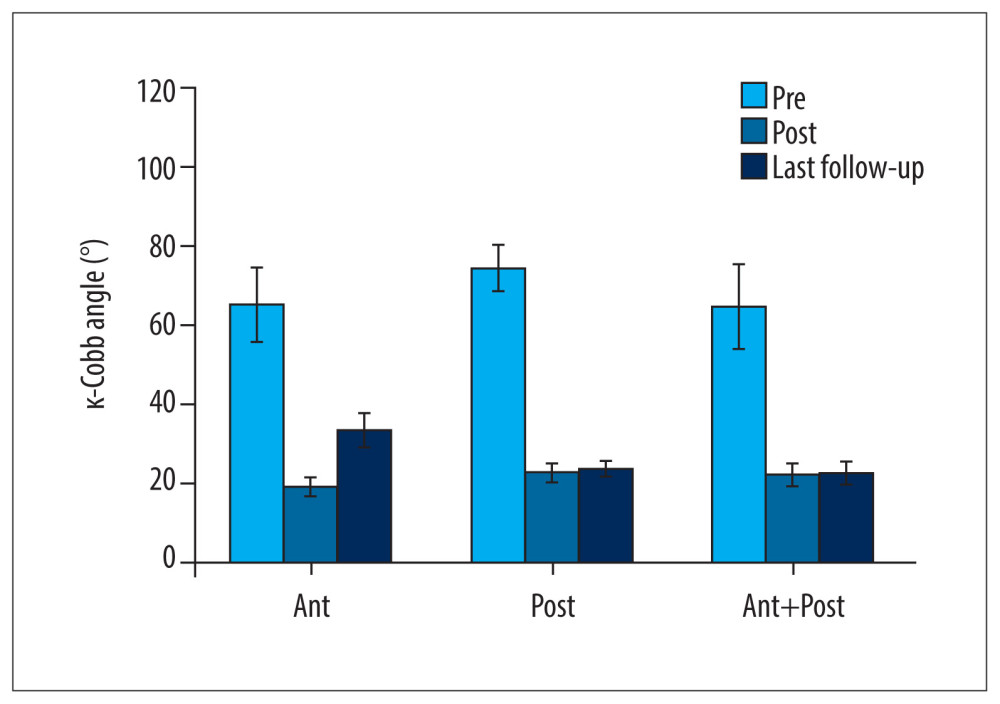
RESULTS: In all 3 groups after surgery, ESR, CRP levels, VAS scores, and k-Cobb angles significantly decreased. However, compared with patients who received Methods B and C, patients who received Method A had a significant rebound in k-Cobb angle and a higher incidence of complications at the T3 time point. The overall reoperation rate during follow-up was 37.10%. Fourteen patients (22.58%) had kyphosis, 2 patients (3.23%) had tuberculosis recurrence combined with kyphosis, and other complications were reported in 5 patients (8.06%).
CONCLUSIONS: Considering the incidence of complications and level of postoperative biochemical indicators, we concluded that caution should be exercised in using an anterior approach to treat pediatric ST.
Keywords: Child, general surgery, Spine, Tuberculosis, Adolescent, Blood Sedimentation, C-Reactive Protein, Child, Preschool, Debridement, Follow-Up Studies, Infant, Postoperative Complications, Tuberculosis, Spinal, visual analog scale
Background
The first documented record of spinal tuberculosis (ST) dates to 3400 BC in Egypt, making it one of the oldest known diseases and a common form of extrapulmonary tuberculosis (TB). ST is characterized by local pain and tenderness, muscle stiffness and cramps, and even apparent degenerative scoliosis [1]. According to previous reports, the majority of cases of ST in infants and young children occur in developing countries, especially in mainland China, where the distribution of medical resources varies greatly among regions [2].
Three types of surgery are widely used to treat ST in adults: simple anterior debridement with bone fusion or plus internal fixation (Method A), simple posterior debridement (Method B), and simple posterior or anteroposterior debridement with bone fusion plus internal fixation (Method C) [3]. Intense debate continues about the selection of a surgical method for infants and children, especially those who are young. Therefore, we compared the advantages and disadvantages of the aforementioned procedures for ST in children, hoping to provide a reliable reference for clinical treatment. In the present study, we collected and retrospectively analyzed clinical data from 62 children with ST who underwent surgery with one of the 3 methods at our hospital from January 2010 to December 2014. Of the children, 29 were male and 33 were female, with an average age of 6.27 years (range, 8 months–14 years).
In adults, diagnosis and treatment of ST are relatively standard [4]. However, in the early stage in children, ST progression is slow, subtle, and even asymptomatic. In young children, symptoms of early TB often are overlooked by parents and doctors because of lack of specificity in growing stages, patient inability to communicate complaints, noncompliance with physical examination, and other factors. Therefore, ST in infants and young children often may only come to medical attention when these patients are in severe pain or have an apparent spinal deformity or neurological abnormalities. Consequently, ST significantly affects spinal development in children, often resulting in spinal deformity, cardiopulmonary dysfunction, and in severe cases, nerve dysfunction or paralysis.
The features of spinal anatomy and physiology in children lead to more ST lesion-involved spinal segments than in adults [5]. Research has shown that the number of lesion-involved spinal segments in children is 1.9 times greater than in adults. The selection of surgical methods for children with ST in different age groups remains the subject of debate. Some clinicians believe that debridement is unsuitable for children younger than age 4 years because it could result in visible spinal deformities in late stages of ST [6]. According to Rajasekaran et al., high-risk factors for postoperative spinal kyphosis deformity include age younger than 10 years, preoperative convex kyphosis Cobb (k-Cobb) angle >30°, and vertebral loss score >1 point [7].
To date, there is no consensus about standard surgical treatment of ST in children [8–11]. Therefore, we compared the advantages and disadvantages of 3 surgeries for ST in children: simple anterior debridement with bone fusion alone or plus internal fixation (Method A); simple posterior debridement (Method B); and simple posterior or anteroposterior debridement with bone fusion plus internal fixation (Method C). We collected and retrospectively analyzed clinical data from 62 children with ST who underwent surgery as described above at our hospital from January 2010 to December 2014, 29 of whom were male and 33 female, with an average age of 6.27 years (range, 8 months-14 years). The surgical methods included simple anterior debridement with bone fusion alone or plus internal fixation, simple posterior debridement, and simple posterior or anteroposterior debridement with bone fusion plus internal fixation. Results with these procedures for treatment of ST in children were retrospectively analyzed and compared to analyze the efficacy and complications of these 3 different approaches and to evaluate the practicality of performing them on children with ST.
Material and Methods
SUBJECTS:
Sixty-two children with ST who underwent 3 surgical procedures in the Department of Spine Surgery from January 2010 to December 2014 were included in this study. The patients ranged in age from 8 months to 14 years (average 6.27±3.98 years); 29 were male and 33 female. Among these patients, 5 had lesions in the cervical spine, 5 had lesions in the chest and thoracic segment, 28 had lesions in the thoracic segment, 7 had lesions in the thoracolumbar segment, and 17 had lesions in the lower lumbar and sacral vertebrae. According to the Frankel grading of neurological function, 8 of 62 cases of ST were Grade B, 13 were Grade C, 16 Grade D, and 25 cases were Grade E. Thirty-two of 62 cases were complicated by kyphosis (average preoperative k-Cobb angle, 77.75±26.02), with a mean erythrocyte sedimentation rate of 35.7 mm/h on admission, together with a C-reactive protein level of 19.9 μg/L and a visual analog scale (VAS) score of 8.1 points. All patients were followed up for an average of 27.4 months (range, 12–60 months). This study was conducted in accordance with the Declaration of Helsinki with approval from the Ethics Committee of Xinjiang Medical University. Written informed consent was obtained from the legal guardians of all participants.
DIAGNOSTIC CRITERIA:
ST typically is diagnosed based on a combination of clinical manifestations and findings on X-rays, computed tomography (CT) scans, and magnetic resonance imaging (MRI). Results of laboratory testing also can be used. Clinical manifestations suspicious for ST included in diagnostic criteria are symptoms of systemic tuberculosis poisoning, such as night sweats, low-grade fever, lack of appetite, and fatigue. The most common chief complaints in children with early-stage ST are stiffness and pain in the neck, back, and waist or restricted movement of the spine and limbs. As the disease progresses, some children with ST have obvious kyphosis, which causes compression of the spinal cord, resulting in abnormal posture and even varying degrees of limb paralysis. CT scans and X-rays of patients with ST show obvious spinal bone destruction, including dead bone formation, spinal structure damage, and kyphosis; MRI shows typical vertebral body and intervertebral disc destruction, abscess formation. and spinal nerve compression. Indicators of ST on laboratory testing include increased ESR, CRP levels, and
SURGICAL METHODS AND INDICATIONS:
The indications for surgery in children with ST are as follows: (1) massive abscess formation; (2) large areas of dead spinal bones or small dead bones found in the spinal canal; (3) spinal instability caused by damage to the vertebral body or intervertebral disc; (4) varying degrees of neurological dysfunction caused by compression of the spinal cord; and (5) severe spine deformity or destruction of more than 1 vertebral body growth plate.
Of the 9 children with cervical TB in this study, 4 children were treated with right lateral oblique incision through the sternocleidomastoid muscle, 3 with posterior cervical incision, and 2 with anterior and posterior approaches combined. Of the 38 patients with thoracic vertebra or thoracolumbar TB, 7 were treated with a paraspinous process approach or a combined thoracoabdominal approach, 8 with a posterior median thoracic approach, and 23 with a single-stage anterior and posterior approach. Of the 15 patients with lumbar TB, 11 were treated with anterior inverted incision, 2 with a posterior median incision, and 2 with anterior and posterior approaches combined. In the operations, pus and necrotic tissue were removed as much as possible. If the spinal cord was compressed, anterior or lateral anterior decompression of the spinal canal was performed at the same time. The kyphosis deformity was corrected intraoperatively. If 2 or more growth plates were lost in front of the vertebral body, a posterior lamina fusion was performed concurrently. Children older than age 8 years underwent posterior laminectomy and facet osteotomy, and were treated with pedicle screw plate fixation and bone graft fusion. In all cases, 1.0 g streptomycin powder was applied to the lesion before wound closure. A closed thoracic drain was placed in patients with pleural rupture.
PREOPERATIVE PREPARATION:
The diagnosis of ST was confirmed in all patients with plain X-ray film, CT, and MRI. In patients who had kyphosis, routine and lateral X-rays were performed, together with whole-spine CT and MRI. Routine laboratory testing for ESR and CRP levels, and cardiopulmonary function examination also were performed to exclude active and miliary TB.
All of the patients were treated with quadruple anti-TB drugs for 2 to 5 weeks before surgery. First-line anti-TB drugs include isoniazid, rifampin, pyrazinamide, ethambutol, and streptomycin. Recommended drug dosages in children with ST are as follows: isoniazid, 5 to 15 mg/kg/day; rifampin, 10 to 20 mg/kg/day; pyrazinamide, 30 to 40 mg/kg/day; ethambutol, 15 to 25 mg/kg/day; and streptomycin, 12 to 18 mg/kg/day. These dosages were adjusted based on patient age and weight. For younger and lighter patients, the dosage was decreased. ESR, CRP levels, and liver and kidney function were monitored every 1 to 2 weeks because side effects such as auditory nerve damage and nephrotoxicity are commonly associated with anti-TB drugs.
SURGICAL PROCEDURES:
Appropriate surgical methods were carefully selected according to the extent of TB lesions, degree of bone destruction, angle of kyphosis, extent of spinal cord compression, combination of abscesses, and the general conditions of the patients. In this study, patients were divided into 3 groups: Group A (22 patients) underwent simple anterior debridement alone or plus with internal fixation [9]; Group B (13 patients) had posterior debridement alone [10]; and Group C (27 patients) underwent single-stage anteroposterior debridement, bone graft fusion, and internal fixation (11 patients) or multi-stage anterior debridement, bone graft fusion, and internal fixation (16 patients) [11]. In all surgeries, the goal was to remove as many lesions and as much necrotic tissue as possible. Decompression was performed for any cases of nerve compression. In patients with kyphosis, a correction was made to bring the spine back to normal physiological curvature. For bone grafting, allogeneic ilium (Bone Bank of Shanxi Province) or autologous ilium or rib was used. Importantly, before surgery, 1.0 g of streptomycin was injected into each lesion as a skin test. In addition, patients with pleural rupture underwent conventional pleural drainage using a closed thoracic drainage tube.
POSTOPERATIVE TREATMENT:
After surgery, patient vital signs, including blood pressure, breathing, and pulse, were monitored. Drainage tubes were removed when the amount of postoperative fluid decreased to <50 mL in 24 h. Patient postoperative recovery and internal fixation were evaluated every 1 to 2 weeks. Following surgery, patients who did not have severe neurological dysfunction were advised to wear a brace during early ambulation. For those with severe neurological dysfunction or paraplegia, improvements in neurological function dictated the pace of return to physical activity. A full range of anti-TB treatments were regularly administered, together with regular testing of ESR, CRP levels, liver and kidney function, and imaging studies.
CLINICAL ASSESSMENT:
To compare and evaluate the outcomes of the 3 different surgical outcomes, we collected information about procedure duration, blood loss, ESR, CRP levels, neurological function, VAS scores, k-Cobb angle at different time points, and complications.
STATISTICAL ANALYSIS:
SPSS26.0 was used to analyze the differences between the Frankel grades, ESR, CRP levels, VAS scores, and k-Cobbs angles preoperatively and postoperatively using a paired
Results
DEMOGRAPHICS:
All patients were followed up for 12 to 60 months (average 27.4 months). The average blood loss was 215 mL (range, 90–520 mL) and the average operative time was 160 min (range, 110–340 min). The results of the paired t test showed that ESR, CRP levels, and VAS scores at the T3 time point were significantly lower than those at T1 in patients with ST who underwent surgery. After surgery, ESR and VAS scores in the 3 groups of patients with ST decreased into the normal range (ESR, 0–10 mm/h; VAS, 0–10 points). The greatest reduction in ESR, which was statistically significant, was seen in Group A, (T1 40.31 mm/h–T3 3.68 mm/h), whereas the smallest change was seen in Group C (T1 18.14 mm/h–T3 1.02 mm/h). Reductions in VAS scores were similar in all 3 groups. Moreover, although CRP levels decreased significantly in all 3 groups following surgery, only in Group C (T1 22.30 mg/L–T3 3.02 mg/L) were the reductions into the normal range (0–5 mg/L) (Table 1).
IMPROVEMENTS IN NEUROLOGICAL FUNCTION:
According to Frankel’s classification, 21 of 62 patients with ST were diagnosed with neurological dysfunction (Grades A to C) before surgery, with 12 cases in Group A (6 Grade B, 6 Grade C), 5 cases in Group B (2 Grade B, 3 Grade C3), and 4 cases in Group C (all Grade C). All patients basically had a return to normal neurological function (Grades D and E) except for 1 who did not recover (Grade B) and 3 patents in Group A who improved from Grade B to C (Table 2).
COMPARISON OF K-COBB ANGLE:
Our results have demonstrated that with any of the 3 surgical treatments, the k-Cobb angle in children with cervical TB, thoracic tuberculosis (TT) and lumbar tuberculosis (LT) can be restored to the normal angle range (<25°) in the short term (T2). However, long-term follow-up showed that the recurrence rate for TT and LT treated with Method A was higher than that for Methods B and C. After the patients with TT and LT underwent surgery with Method A, their average k-Cobb angle increased from 21.36° at T2 to 37.45° at T3, and 19.71° at T2 to 35.00° at T3, respectively. The k-Cobb angle of patients with ST treated with Method A at time T3 reached an average of 24° and approached the threshold. Compared with Method A, Methods B and C methods showed similar and excellent stability in maintaining a normal k-Cobb angle postoperatively in patients with ST (Figure 1, Table 3A–3C).
COMPLICATIONS AND TREATMENT DURING FOLLOW-UP:
During postoperative follow-up, 20 patients in Group A underwent a second surgery. Six of the procedures were attributed to bone graft absorption/collapse, internal fixation looseness, or fracture. The other 14 patients underwent repeat surgery because of a kyphotic deformity, which increased, on average, by 14.68° at T3 compared with T2 (Figure 1). Two patients in Group A exhibited single-stage healing and had no significant postoperative aggravation of their kyphosis (Table 4). One patient in Group B had an incision sinus after surgery, which was treated successfully with debridement, catheterization, and therapy for symptoms. Two patients in Group C underwent another surgery because of bone graft absorption/collapse or internal fixation loosening/fracture. No complications were reported in the remaining patients.
Discussion
ANTEROPOSTERIOR DEBRIDEMENT, BONE GRAFT FUSION, AND INTERNAL FIXATION:
Based on their general condition, patients with larger lesions, in whom selection of anterior fixation material is difficult, and who require correction of combined kyphosis should be assessed for single-stage anteroposterior debridement plus bone graft fusion and orthopedic internal fixation, or multi-stage anterior debridement plus bone graft fusion and posterior orthopedic internal fixation [28,29].
In addition to the advantages of simple anterior or posterior surgery, some researchers believe that in PST, kyphosis is caused not only by loss of height in the anterior vertebral column but also because of an imbalance in growth between the anterior and posterior vertebral bodies. Growth ratio indicators for the anterior and posterior vertebral bodies show that anterior debridement with bone graft fusion plus posterior debridement with bone graft fusion can reduce the incidence of growth imbalance between the anterior and posterior vertebral bodies, thus avoiding the aggravation of kyphosis in late-stage ST [29]. Of the 27 patients in Group C, 1 had postoperative hemopneumothorax and was cured following closed thoracic drainage; 1 patient had formation of an anterior incision sinus, which was treated successfully with re-debridement; and 1 patient had a fracture of internal fixation, which was repaired with surgery. None of the 27 patients had signs of aggravation of kyphosis.
Based on the results of the present study, we concluded that each surgical method was effective in clearing TB lesions and satisfactory for decompressing the spinal cord, improving neurological function, and correcting preoperative kyphosis. Follow-up of the patients revealed that 63.64% of patients (14/22) in Group A required repeat surgery for kyphosis, which was a much higher rate than in younger patients, but such a phenomenon was not observed in Groups B or C.
It is necessary to note that our research had several limitations. First, follow-up in our series is indicative of short-term but not long-term results and revealed a high rate of revision in the anterior group. In addition, the small sample sizes in each group limited the power of our conclusions. Therefore, a randomized controlled trial is required to compare different treatments for TB in children. However, the preliminary results from our study can serve as an aid to surgeons in decision-making and help direct future studies.
Conclusions
In summary, we concluded that the 3 surgical methods can be used in the treatment of PST. However, considering the higher complication rate associated with it, caution should be exercised in using an anterior approach to treat PST and research is still needed to track the long-term adverse effects of that method.
Tables
Table 1. Comparison of erythrocyte sedimentation rates, C-reactive protein levels, and visual analog scale scores among the 3 groups at different time points.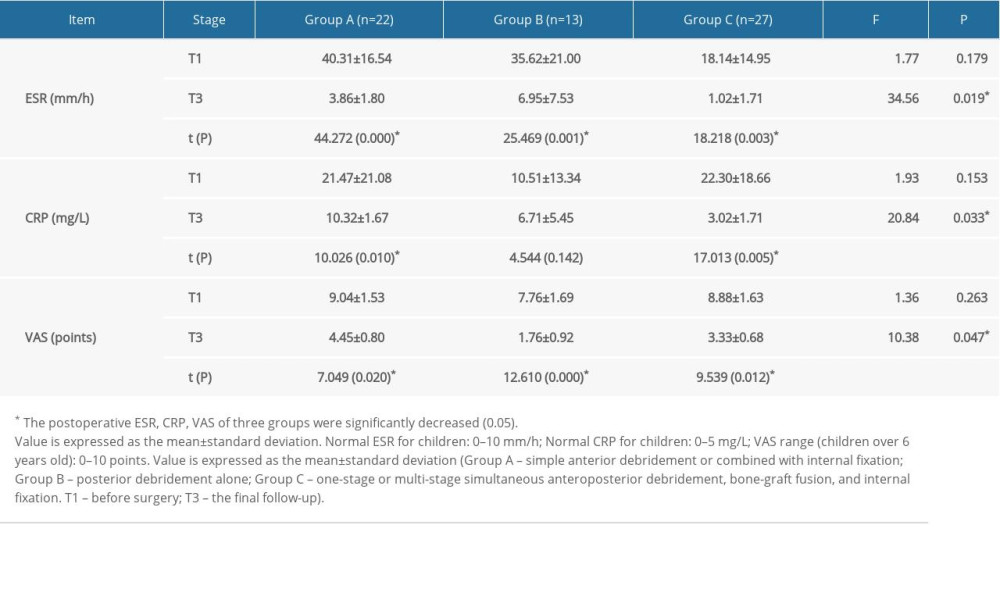 Table 2. Frankel grades for all patients at T3.
Table 2. Frankel grades for all patients at T3.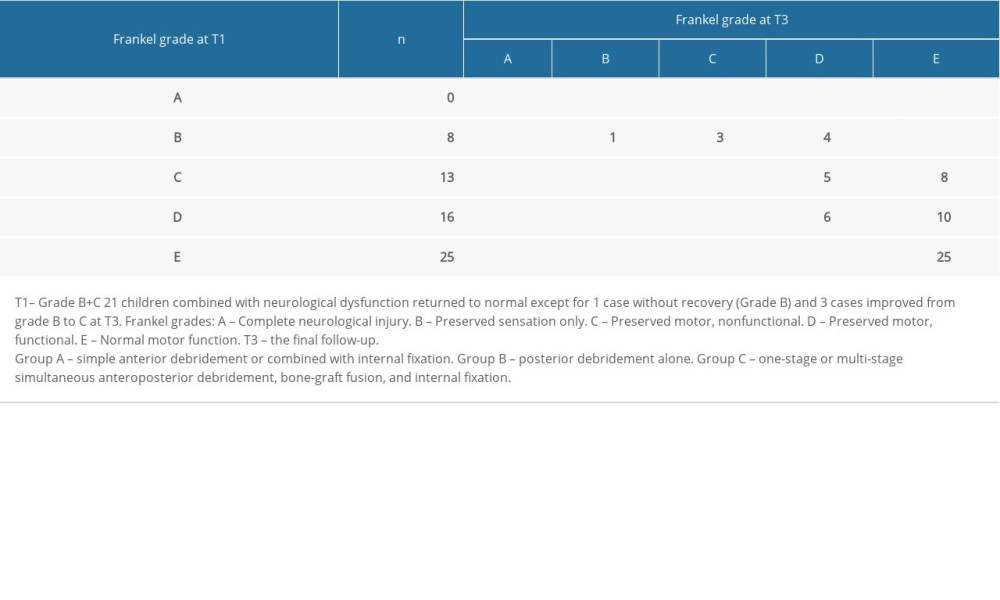 Table 3A. Changes of k-Cobb angle of different segmental spinal tuberculosis in Group A.
Table 3A. Changes of k-Cobb angle of different segmental spinal tuberculosis in Group A.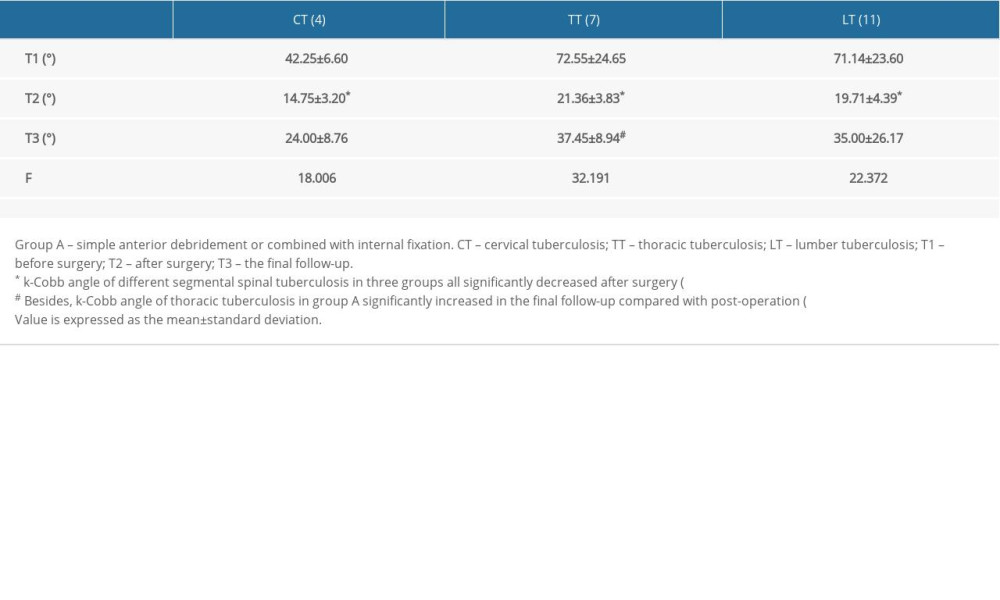 Table 3B. Changes of k-Cobb angle of different segmental spinal tuberculosis in Group B.
Table 3B. Changes of k-Cobb angle of different segmental spinal tuberculosis in Group B.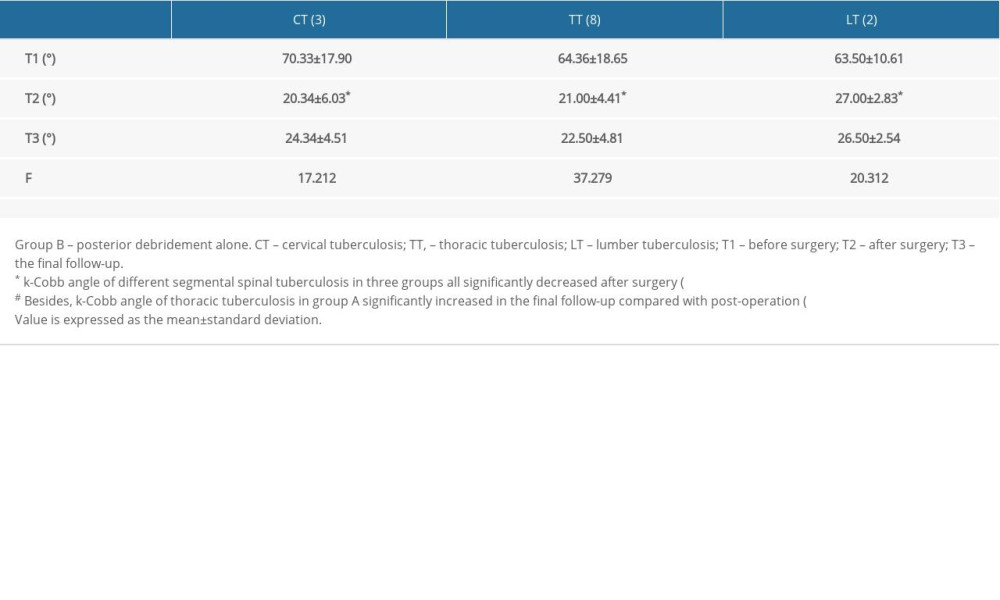 Table 3C. Changes of k-Cobb angle of different segmental spinal tuberculosis in Group C.
Table 3C. Changes of k-Cobb angle of different segmental spinal tuberculosis in Group C.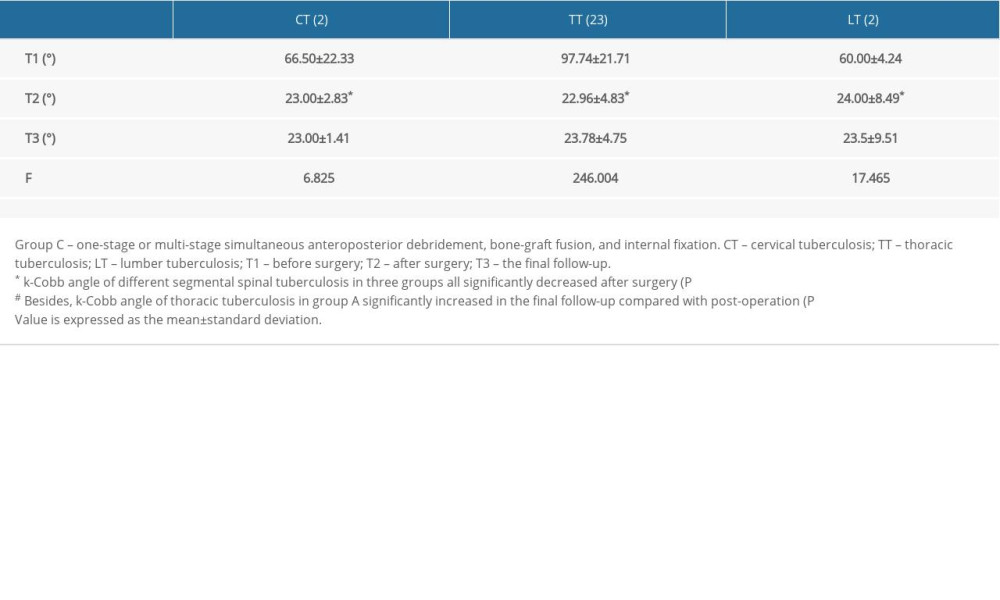 Table 4. Distribution of complications among the 3 groups.
Table 4. Distribution of complications among the 3 groups.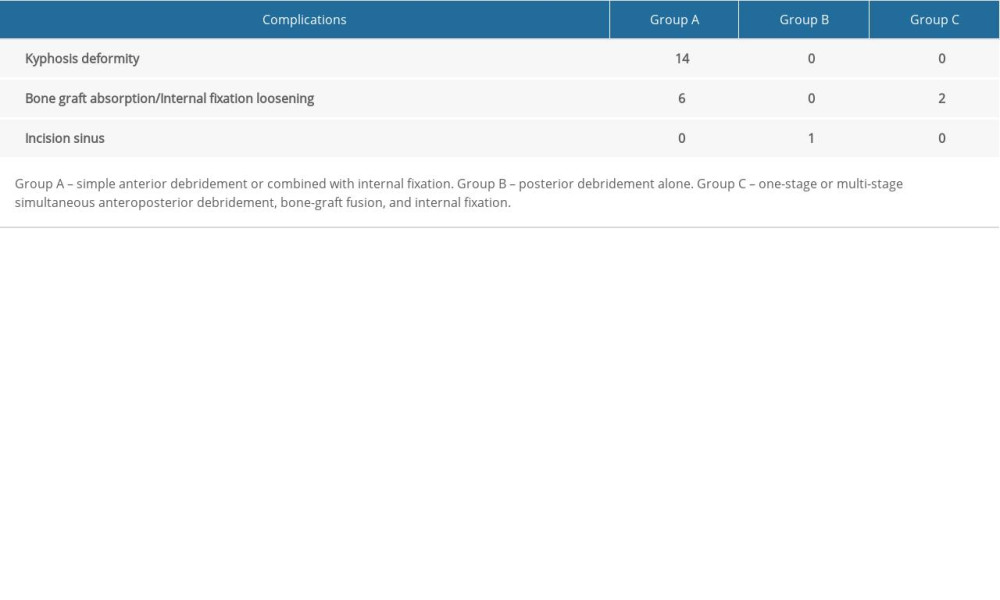
References
1. Garg RK, Somvanshi DS, Spinal tuberculosis: A review: J Spinal Cord Med, 2011; 34(5); 440-54
2. World Health Organization: Global tuberculosis report 2018, 2018, Geneva, World Health Organization
3. Yang P, Zang Q, Kang J, Comparison of clinical efficacy and safety among three surgical approaches for the treatment of spinal tuberculosis: A meta-analysis: Eur Spine J, 2016; 25(12); 3862-74
4. Yang P, He X, Li H, Clinical efficacy of posterior versus anterior instrumentation for the treatment of spinal tuberculosis in adults: A meta-analysis: J Orthop Surg Res, 2014; 9(1); 10
5. Rajasekaran S, Shanmugasundaram TK, Prabhakar R, Tuberculous lesions of the lumbosacral region. A 15-year follow-up of patients treated by ambulant chemotherapy: Spine (Phila Pa 1976), 1998; 23(10); 1163-67
6. Wiley AM, Trueta J, The vascular anatomy of the spine and its relationship to pyogenic vertebral osteomyelitis: J Bone Joint Surg Br, 1959; 41-B; 796-809
7. Rajasekaran S, Vijay K, Shetty AP, Single-stage closing-opening wedge osteotomy of spine to correct severe post-tubercular kyphotic deformities of the spine: A 3-year follow-up of 17 patients: Eur Spine J, 2010; 19(4); 583-92
8. Rajasekaran S, Khandelwal G, Drug therapy in spinal tuberculosis: Eur Spine J, 2013; 22(Suppl 4); 587-93
9. Jin D, Qu D, Chen J, Zhang H, One-stage anterior interbody autografting and instrumentation in primary surgical management of thoracolumbar spinal tuberculosis: Eur Spine J, 2004; 13(2); 114-21
10. Sahoo MM, Mahapatra SK, Sethi GC, Dash SK, Posterior-only approach surgery for fixation and decompression of thoracolumbar spinal tuberculosis: A retrospective study: J Spinal Disord Tech, 2012; 25(7); E217-23
11. Hu J, Li D, Kang Y, Active thoracic and lumbar spinal tuberculosis in children with kyphotic deformity treated by one-stage posterior instrumentation combined anterior debridement: Preliminary study: Eur J Orthop Surg Traumatol, 2014; 24(Suppl 1); S221-29
12. Rangel-Castilla L, Hwang SW, Whitehead WE, Surgical treatment of thoracic Pott disease in a 3-year-old child, with vertebral column resection and posterior-only circumferential reconstruction of the spinal column: Case report: J Neurosurg Pediatr, 2012; 9(4); 447-51
13. Wang YX, Zhang HQ, Tang MX, One-stage posterior focus debridement, interbody grafts, and posterior instrumentation and fusion in the surgical treatment of thoracolumbar spinal tuberculosis with kyphosis in children: A preliminary report: Childs Nerv Syst, 2016; 32(8); 1495-502
14. Zhang HQ, Li JS, Guo CF, Two-stage surgical management using posterior instrumentation, anterior debridement and allografting for tuberculosis of the lower lumbar spine in children of elementary school age: Minimum 3-year follow-up of 14 patients: Arch Orthop Trauma Surg, 2012; 132(9); 1273-79
15. Zhang HQ, Lin MZ, Guo HB, One-stage surgical management for tuberculosis of the upper cervical spine by posterior debridement, short-segment fusion, and posterior instrumentation in children: Eur Spine J, 2013; 22(1); 72-78
16. Shi T, Zhang Z, Dai F, Retrospective study of 967 patients with spinal tuberculosis: Orthopedics, 2016; 39(5); e838-43
17. Jain AK, Sreenivasan R, Mukunth R, Dhammi IK, Tubercular spondylitis in children: Indian J Orthop, 2014; 48(2); 136-44
18. Rauf F, Chaudhry UR, Atif M, ur Rahaman M, Spinal tuberculosis: Our experience and a review of imaging methods: Neuroradiol J, 2015; 28(5); 498-503
19. Rajasekaran S, Kanna RM, Shetty AP, Pathophysiology and treatment of spinal tuberculosis: JBJS Rev, 2014; 2(9); M.00130
20. Lu G, Wang B, Li J, Anterior debridement and reconstruction via thoracoscopy-assisted mini-open approach for the treatment of thoracic spinal tuberculosis: Minimum 5-year follow-up: Eur Spine J, 2012; 21(3); 463-69
21. Garg B, Kandwal P, Nagaraja UB, Anterior versus posterior procedure for surgical treatment of thoracolumbar tuberculosis: A retrospective analysis: Indian J Orthop, 2012; 46(2); 165-70
22. Cui X, Li LT, Ma YZ, Anterior and posterior instrumentation with different debridement and grafting procedures for multi-level contiguous thoracic spinal tuberculosis: Orthop Surg, 2016; 8(4); 454-61
23. Liu C, Lin L, Wang W, Long-term outcomes of vertebral column resection for kyphosis in patients with cured spinal tuberculosis: Average 8-year follow-up: J Neurosurg Spine, 2016; 24(5); 777-85
24. Jain AK, Dhammi IK, Jain S, Mishra P, Kyphosis in spinal tuberculosis – Prevention and correction: Indian J Orthop, 2010; 44(2); 127-36
25. Pang X, Li D, Wang X, Thoracolumbar spinal tuberculosis in children with severe post-tubercular kyphotic deformities treated by single-stage closing-opening wedge osteotomy: Preliminary report a 4-year follow-up of 12 patients: Childs Nerv Syst, 2014; 30(5); 903-9
26. Hu X, Zhang H, Yin X, One-stage posterior focus debridement, fusion, and instrumentation in the surgical treatment of lumbar spinal tuberculosis with kyphosis in children: Childs Nerv Syst, 2016; 32(3); 535-39
27. Tang MX, Zhang HQ, Wang YX, Treatment of spinal tuberculosis by debridement, interbody fusion and internal fixation via posterior approach only: Orthop Surg, 2016; 8(1); 89-93
28. Liu J, Wan L, Long X, Efficacy and Safety of posterior versus combined posterior and anterior approach for the treatment of spinal tuberculosis: A meta-analysis: World Neurosurg, 2015; 83(6); 1157-65
29. Yin XH, Zhou ZH, Yu HG, Comparison between the antero-posterior and posterior only approaches for treating thoracolumbar tuberculosis (T10–L2) with kyphosis in children: A minimum 3-year follow-up: Childs Nerv Syst, 2016; 32(1); 127-33
Tables
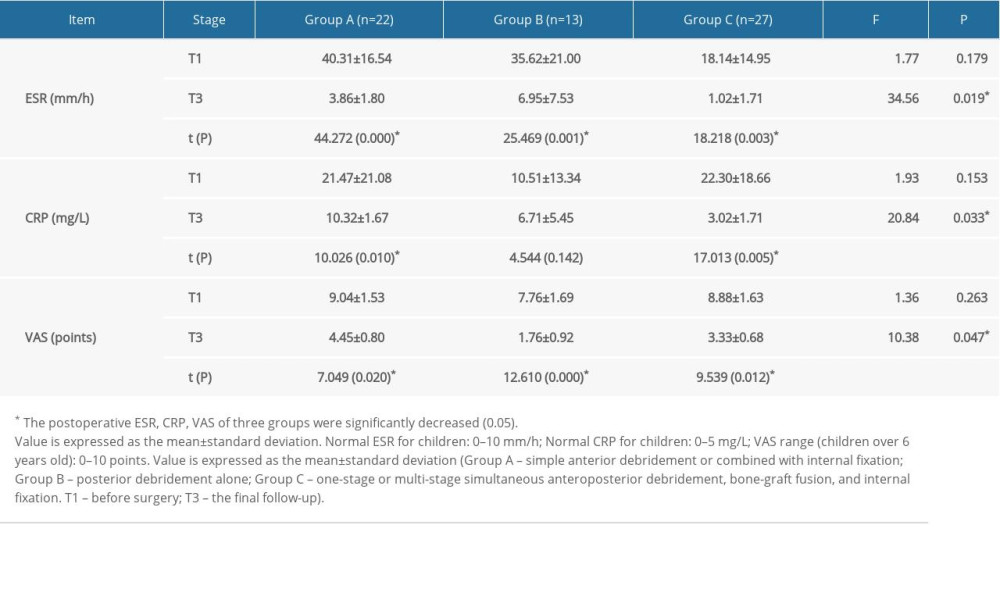 Table 1. Comparison of erythrocyte sedimentation rates, C-reactive protein levels, and visual analog scale scores among the 3 groups at different time points.
Table 1. Comparison of erythrocyte sedimentation rates, C-reactive protein levels, and visual analog scale scores among the 3 groups at different time points.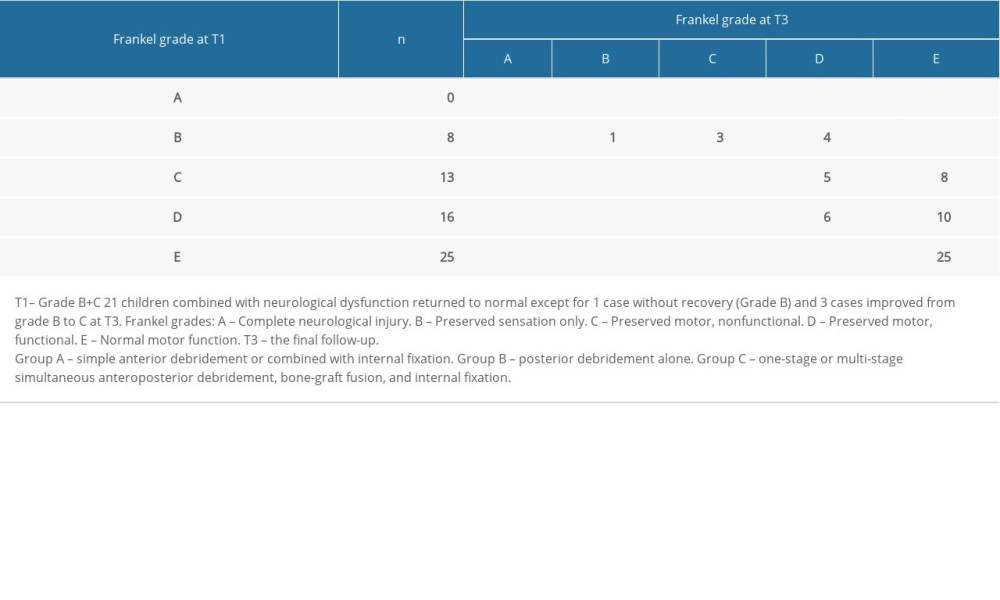 Table 2. Frankel grades for all patients at T3.
Table 2. Frankel grades for all patients at T3.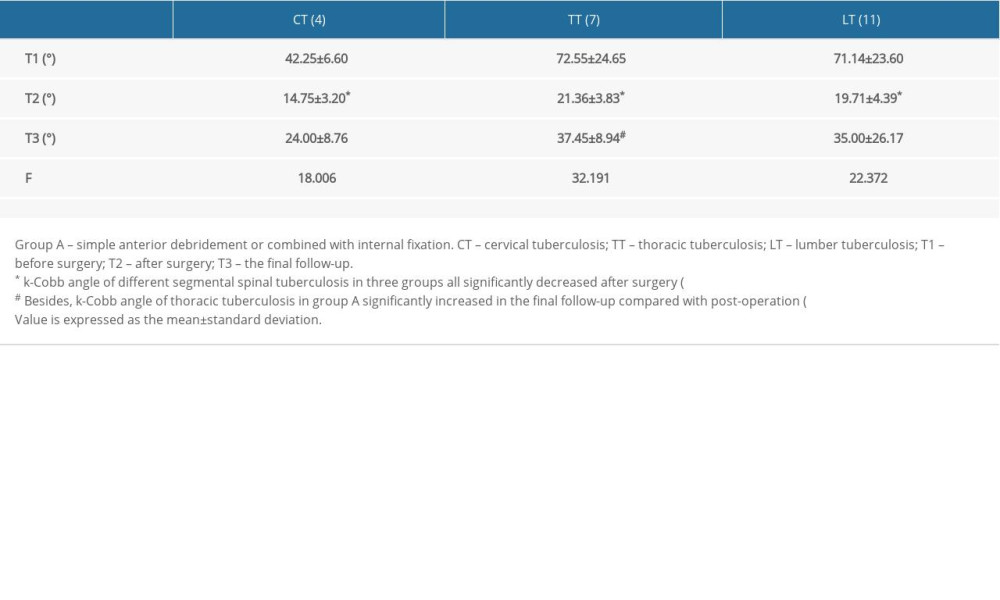 Table 3A. Changes of k-Cobb angle of different segmental spinal tuberculosis in Group A.
Table 3A. Changes of k-Cobb angle of different segmental spinal tuberculosis in Group A.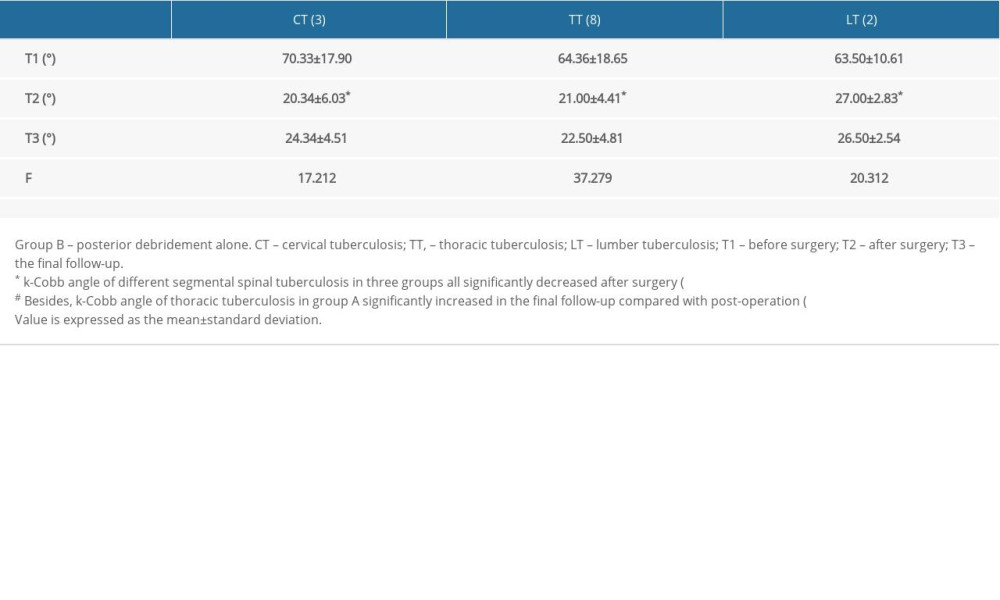 Table 3B. Changes of k-Cobb angle of different segmental spinal tuberculosis in Group B.
Table 3B. Changes of k-Cobb angle of different segmental spinal tuberculosis in Group B.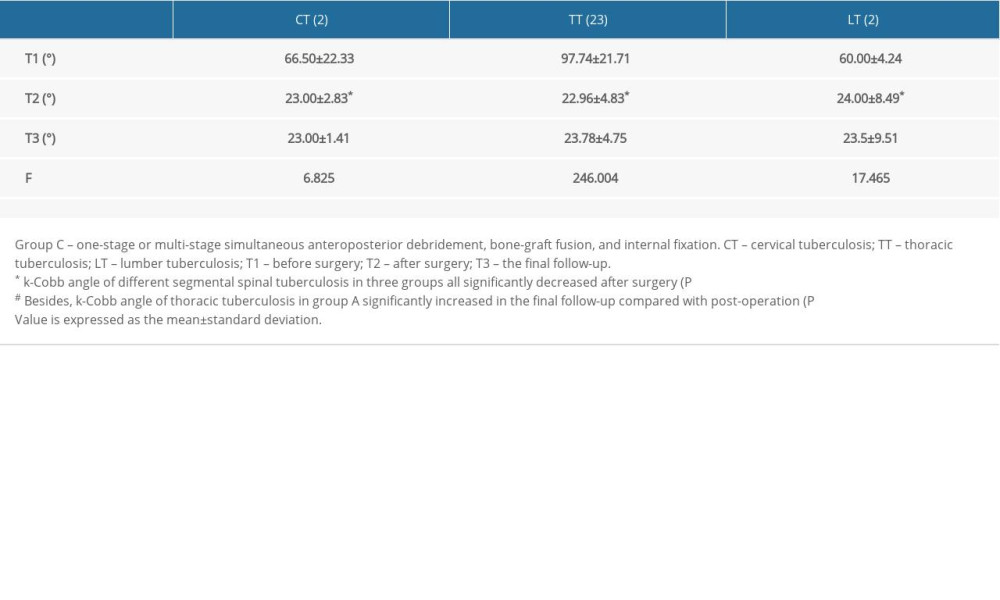 Table 3C. Changes of k-Cobb angle of different segmental spinal tuberculosis in Group C.
Table 3C. Changes of k-Cobb angle of different segmental spinal tuberculosis in Group C.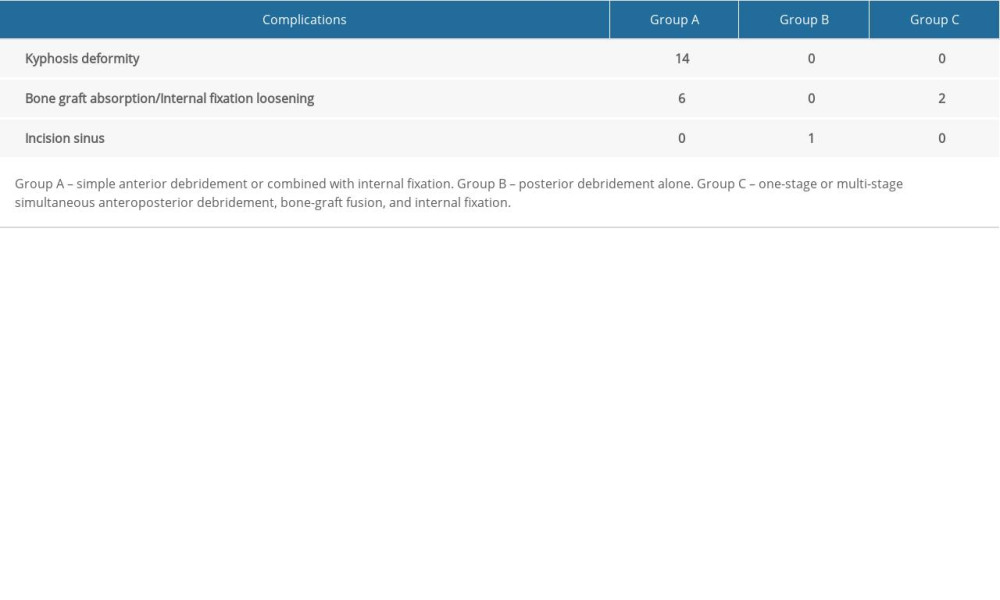 Table 4. Distribution of complications among the 3 groups.
Table 4. Distribution of complications among the 3 groups.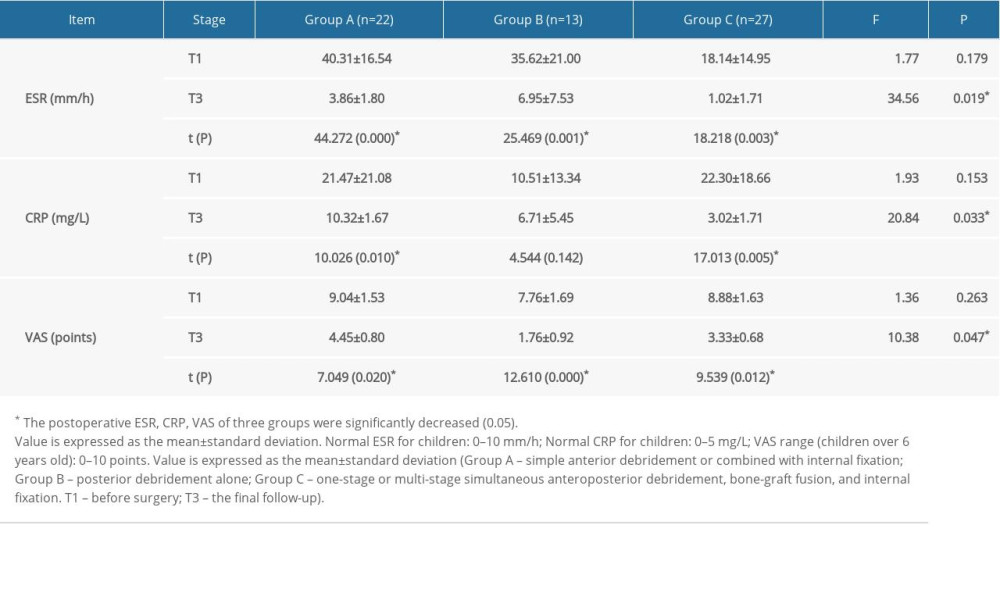 Table 1. Comparison of erythrocyte sedimentation rates, C-reactive protein levels, and visual analog scale scores among the 3 groups at different time points.
Table 1. Comparison of erythrocyte sedimentation rates, C-reactive protein levels, and visual analog scale scores among the 3 groups at different time points.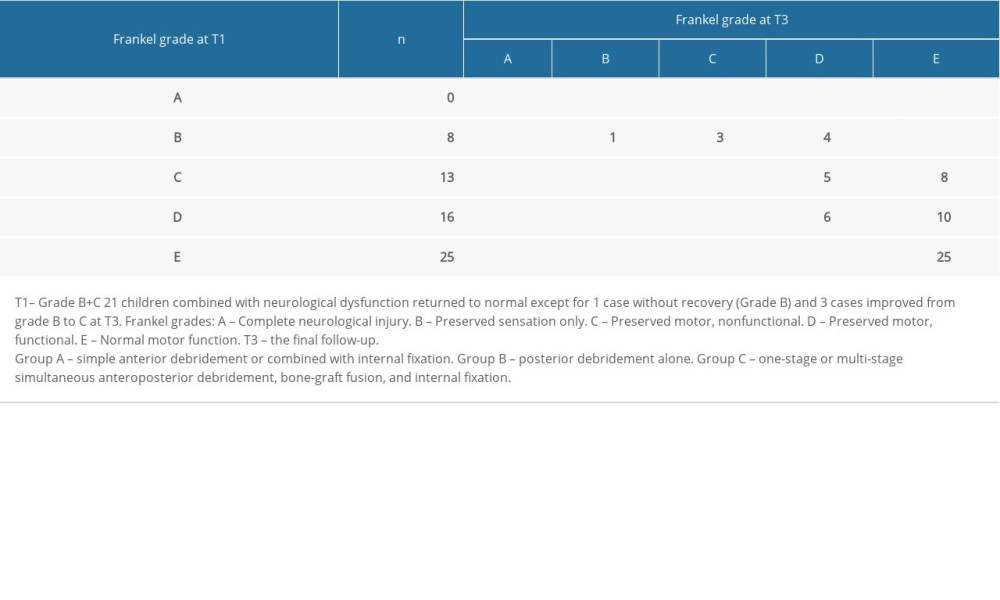 Table 2. Frankel grades for all patients at T3.
Table 2. Frankel grades for all patients at T3.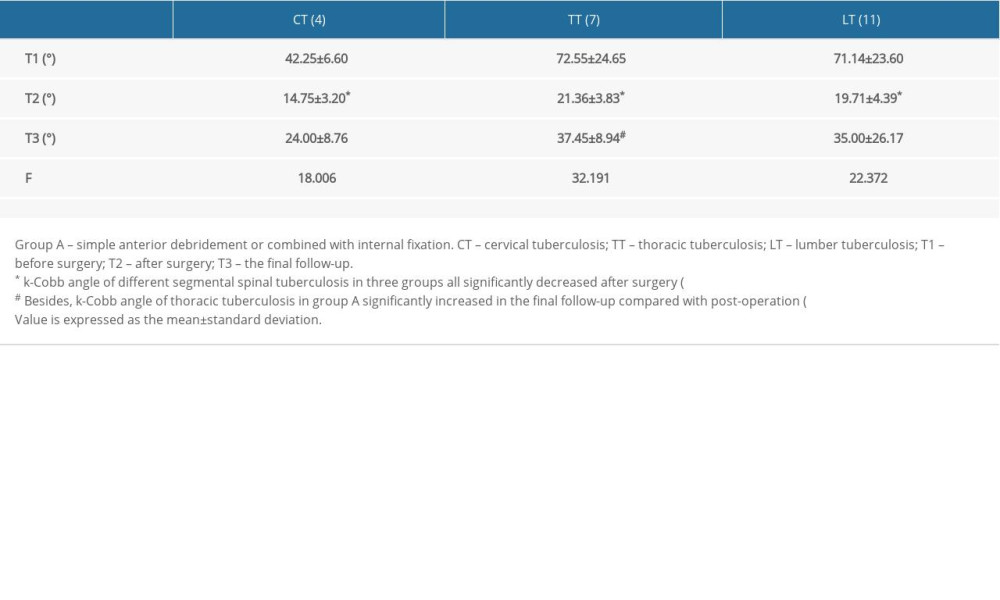 Table 3A. Changes of k-Cobb angle of different segmental spinal tuberculosis in Group A.
Table 3A. Changes of k-Cobb angle of different segmental spinal tuberculosis in Group A.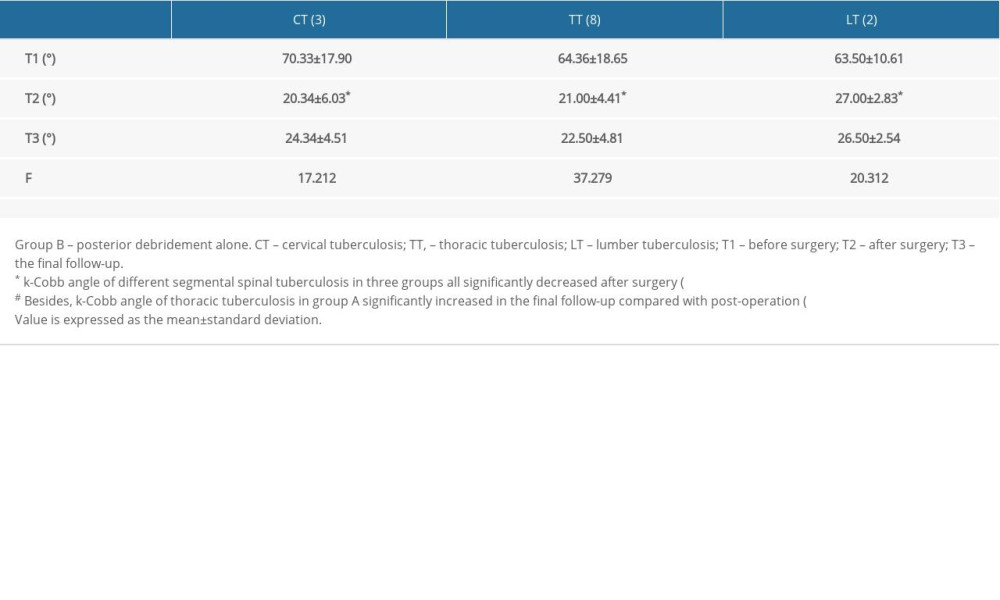 Table 3B. Changes of k-Cobb angle of different segmental spinal tuberculosis in Group B.
Table 3B. Changes of k-Cobb angle of different segmental spinal tuberculosis in Group B.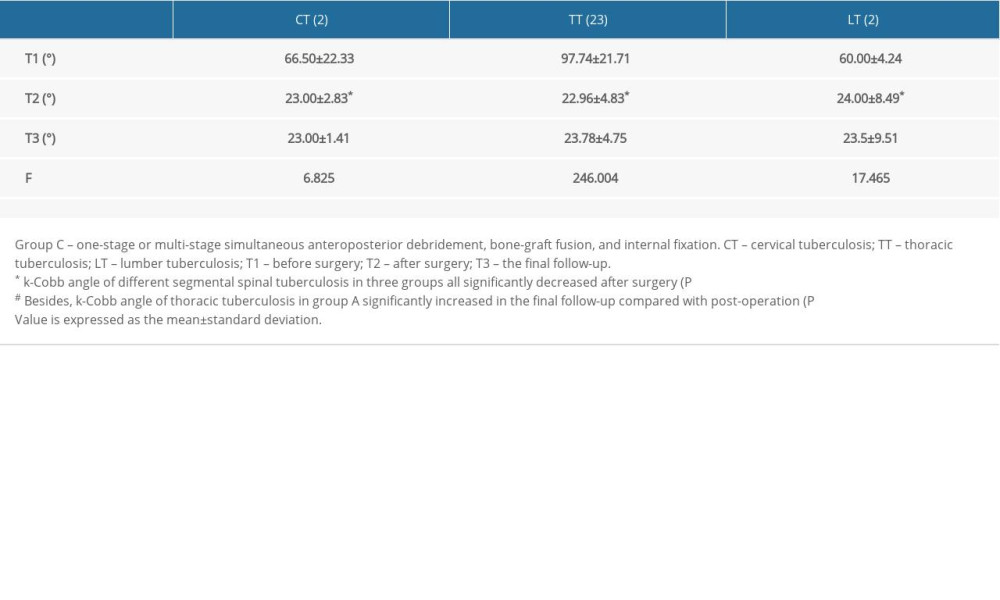 Table 3C. Changes of k-Cobb angle of different segmental spinal tuberculosis in Group C.
Table 3C. Changes of k-Cobb angle of different segmental spinal tuberculosis in Group C.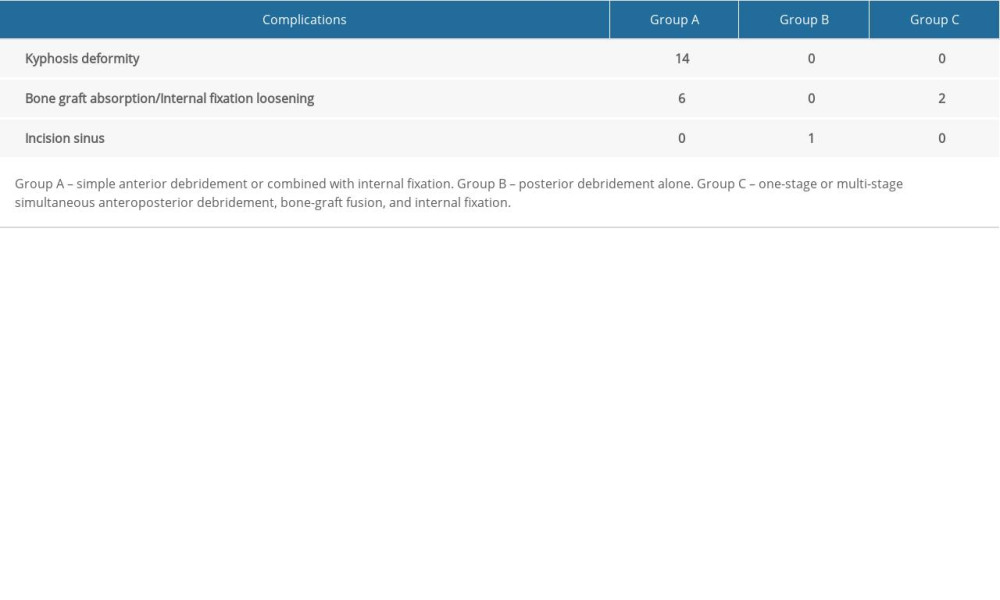 Table 4. Distribution of complications among the 3 groups.
Table 4. Distribution of complications among the 3 groups. In Press
21 Mar 2024 : Meta-Analysis
Economic Evaluation of COVID-19 Screening Tests and Surveillance Strategies in Low-Income, Middle-Income, a...Med Sci Monit In Press; DOI: 10.12659/MSM.943863
10 Apr 2024 : Clinical Research
Predicting Acute Cardiovascular Complications in COVID-19: Insights from a Specialized Cardiac Referral Dep...Med Sci Monit In Press; DOI: 10.12659/MSM.942612
06 Mar 2024 : Clinical Research
Enhanced Surgical Outcomes of Popliteal Cyst Excision: A Retrospective Study Comparing Arthroscopic Debride...Med Sci Monit In Press; DOI: 10.12659/MSM.941102
06 Mar 2024 : Clinical Research
Prevalence and Variation of Medical Comorbidities in Oral Surgery Patients: A Retrospective Study at Jazan ...Med Sci Monit In Press; DOI: 10.12659/MSM.943884
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952