13 October 2020: Clinical Research
Three-Dimensional Ultrasonography in Preoperative and Postoperative Volume Assessment of the Undescended Testicle
Jian-Hong You1DEF, Yi-Fan Zhuang2C, Ming-Zhu Lu3B, Ling Chen4B, Ze-Kun Chen5F, Xiao-Kang Chen5AG*DOI: 10.12659/MSM.924325
Med Sci Monit 2020; 26:e924325
Abstract
BACKGROUND: Ultrasound (US) is the preferred imaging method for cryptorchidism, but most guidelines indicate that its value is questionable. The aim of this study was to evaluate the clinical value of ultrasonic mobility and testicular atrophy index (TAI) based on three‑dimensional US (3DUS) in preoperative and postoperative assessment of the undescended testis.
MATERIAL AND METHODS: Data from 158 children with unilateral extraperitoneal cryptorchidism were collected and their diagnoses were surgically confirmed. They were divided into different age groups and into 2 ultrasonic mobility groups: the mobile group (MG) and the restricted group (RG). Differences in sonographic characteristics between different groups were compared. Three-dimensional ultrasound performed with virtual organ computer-aided analysis (VOCAL) was used to determined preoperative and postoperative TAI and the reliability of TAI was analyzed.
RESULTS: Measurement of testicular volume with the VOCAL method was significantly more reliable than that done with the two-dimensional Lambert method. In all age groups, preoperative testicular volumes were smaller than that in the contralateral scrotal testis and postoperatively, they increased steadily. Both preoperative and postoperative TAI were higher in the RG than in the MG. In the MG, postoperative TAI decreased significantly in all age groups. In the RG, in contrast, effective volume growth was only achieved in patients who had undergone surgery before they reached age 1 year.
CONCLUSIONS: TAI values determined with 3DUS using the VOCAL technique objectively reflect recovery of testicular volume following surgery for undescended testicle. Ultrasonic mobility evaluation is beneficial for clinical management of the condition.
Keywords: Cryptorchidism, orchiopexy, Ultrasonography, Child, Echocardiography, Three-Dimensional, Organ Size, Postoperative Care, Preoperative Care, Testis
Background
Undescended testis or cryptorchidism, in which one or both testes fail to descend from the retroperitoneum to the scrotum, is one of the most common genitourinary malformations in children. Approximately 80% of undescended testes are located at the neck of the scrotum or in the inguinal canal [1–3]. Spontaneous descent of a testis is uncommon after age 6 months. Persistent cryptorchidism may cause a series of physiological and pathological changes in the testicles, leading to impairment in fertility and increased incidence of testicular malignancy [3]. Therefore, both the American Urological Association (AUA) and the European Association of Urology (EAU) recommend that surgical intervention be completed within the first 18 months of life (corrected for gestational age) [2,3]. For visible cryptorchidism, the classic clinical operation is scrotal or inguinal orchiopexy [2].
Clinical decision-making and postoperative management of cryptorchidism is determined by its presence and location [4]. As the criterion standard for functional evaluation, histological biopsy is rarely acceptable because of ethical issues [5]. Detection of levels in the serum of hormones such as follicle-stimulating hormone and testosterone is of limited clinical value due to the compensation of the contralateral testis. The preferred imaging method is ultrasound (US), which can be used to directly observe the structure and location of cryptorchidism, detect mobility in real time, and also visualize surrounding tissues such as the processus vaginalis, spermatic cord, and inferior epigastric artery [6].
On US, 97% of visible extraperitoneal undescended testes can be detected [1]. The spermatogenic activity of the testis reportedly has a good correlation with testis volume [7]. Ultrasonic volume measurement is one of the most important indexes used to evaluate testicular development and function. In the past, the most widely used formula for volume estimation was volume=0.71×length×width×height [8]. However, a recent study on intergroup and intragroup consistency of the testes measured with this method showed that even if the same testes were measured, the difference could reach 20% [9].The advent of three-dimensional US (3DUS) allows for more precise and reliable assessment of a developing organ [10].The virtual organ computer-aided analysis (VOCAL) technique for 3DUS has been widely applied in recent years for assessment of fetal growth, monitoring of benign and malignant tumors, and applications in reproductive medicine [11–13]. However, there are no reports in the literature about use of the VOCAL technique for measurement of testicular volume in postoperative follow-up of cryptorchidism.
For intraperitoneal cryptorchidism, mobility assessment is particularly important, as it can reflect spermatic cord length, guide selection of surgical methods, and predict prognosis [14], but mobility of extraperitoneal cryptorchidism has rarely been reported. There is a strong correlation between the position of an undescended testis and persistence of the processus vaginalis [15]. US has significant value for evaluating the inguinal canal and cryptorchidism [16,17], as well as motion in the spermatic cord [18]. Nevertheless, the relationship between sonographic mobility in cryptorchidism and persistence of the processus vaginalis and their associations with prognosis after orchiopexy remain unclear.
Therefore, the primary aim of this study was to determine the intraobserver and interobserver agreement of testicular volume measurements done using the 3DUS VOCAL technique. The secondary aim was to evaluate the clinical value of ultrasonic mobility and TAI value in management and postoperative follow-up of the undescended testicle.
Material and Methods
STUDY SITE AND DEVICE:
This study was performed in Zhongshan Hospital of Xiamen University and Children’s Hospital of Fudan University Xiamen Branch (Xiamen Children’s Hospital) between September 2015 and December 2019. The study protocol was approved by our institution’s Ethics Committee. Written informed consent was obtained from all the participants prior to the study.
Examinations were performed with a GE Voluson E8 Expert 3DUS instrument equipped with an internal 3DUS VOCAL program and a SP4-6-D high-frequency 3D probe (General Electric Healthcare, Milwaukee, Wisconsin, United States). To ensure safe use of US for medical diagnosis [19], the mechanical index and the heat index was controlled below 0.2 and the color scale was set to 9 with a minimal detectable flow rate of 0.2 cm/s with the lowest filter adopted.
STUDY POPULATION AND DESIGN:
This retrospective study included, 158 children (right, 86 cases; left, 72 cases) with surgery-confirmed unilateral extraperitoneal cryptorchidism (in the inguinal canal or the roots of the scrotum) for whom complete preoperative and postoperative clinical and ultrasound information was available.
All the children underwent scrotal or inguinal orchiopexy at ages ranging from 6 mo to 9 years (corrected for gestational age). Exclusion criteria included sliding testes, retractable testes, intraperitoneal cryptorchidism, testicular atrophy (intraoperatively, cystic dermoid tissue was found at the end of the spermatic cord vessels but no testicular parenchyma), testicular ectopia, recurrent cryptorchidism (patients who had undergone cryptorchidopexy before this study, but were admitted to the hospital with postoperative recurrent cryptorchidism within the time limit of this study), bilateral cryptorchidism, and other systemic or severe systemic diseases. Earlier than normal sexual maturation has been reported in some patients with cryptorchidism [20]. Therefore, we reviewed patients’ drug history, detailed physical examination records, imaging results, and serum levels of thyroid and sex hormones (if available) to ensure that increased testicular volume due to drugs or precocious puberty was excluded. Participants were divided into 3 groups according to age at surgery: Group I (0 to 1 year, n=45), Group II (>1 to <6 years, n=81), and Group III (6 to 9 years, n=32). For cryptorchidism, sonographic mobility examination is often performed with the patient in the supine and frog-legged position, assisted by Valsalva maneuver or cough to increase intraperitoneal pressure. The clinician then can ask the patient to stand up and repeat the manipulation under ultrasound guidance. In addition, the clinician can flatten and fix the skin in the groin area with the right hand, palpate and locate the cryptorchidism with the left hand assisted by US, and gently move it up and down to observe testicular mobility. For the cut-off values, based on experience, we used a 2-finger distance (increasing abdominal pressure [cough or Valsalva maneuver]) or postural change (from supine to standing position or manipulative push) and divided the participants into 2 groups: a mobile group (MG) and a restricted group (RG).
ULTRASONIC DATA ACQUISITION AND MEASUREMENT:
The morphology and structure of the testes were observed and measured using US while the children were anesthetized prior to surgery. A child was placed in the supine position with the probe on the scrotal skin to determine the condition of the testicle inside the scrotum. If no testicles were found, scanning was done with the probe placed in the inguinal area, the root of the scrotum, the inner ring, and other areas. After undescended testicles were found, their morphology, size, boundary, internal echo, and mobility were observed with conventional 2-dimensional US (2DUS). Testicular volume was calculated according to the formula of Lambert [21]: testicular volume (TV)=L (length)×W (width)×D (depth)×0.71. Then, distribution of testicular blood flow was detected with Doppler US. Finally, 3DUS was activated to view the maximum longitudinal section of testis. After sampling, 3D images were reconstructed and postprocessed using the VOCAL method. With 3 orthogonal slices simultaneously displayed, the maximum diameter plane was selected as A plane. While rotating at a 30° angle around plane A, 6 slices were obtained to manually trace the contours of the testicle. Information on testicular volume and a 3D rendering were generated automatically (Figure 1D). An average value was obtained based on 3 measurements.
The testicular atrophy index (TAI) [22] was defined as the ratio of the volume difference (contralateral scrotal testis–undescended testis) to contralateral scrotal testis volume in the same child. As suggested, a TAI in excess of 20% to 25% is clinically significant.
CHARACTERISTICS OF DIFFERENT GROUPS OBSERVED BY ULTRASOUND:
Testicular location, morphology, volume, boundary, internal echo, blood distribution, and processus vaginalis in the MG and RG groups as detected with 2DUS and 3DUS were observed and compared. Classification of gray-scale US characteristics was based on previous studies [17]. Doppler US assessment of superficial tissue perfusion with a semi-quantitative method has been proven feasible by Adler et al. [23]. They suggested dividing vascularity into 4 grades: absent, minimal, moderate, and marked. With the semi-quantitative method, we divided blood distribution in cryptorchidism into well-filled and sparse. Well-filled blood flow corresponded to Adler classification of moderate and marked vascularity. Sparse blood flow corresponded to Adler classification of absent and minimal vascularity.
RELIABILITY ANALYSIS OF VOLUME MEASUREMENT:
For reliability analysis using the Lambert formula and the VOCAL method, 50 cases were collected by systematic sampling. Each of the observers collected 2 sets of consecutive images per subject within a 10-min interval. The images were saved for blind analysis offline. The method of measurement was as previously described.
TESTICULAR VOLUME FOLLOW-UP AFTER ORCHIOPEXY:
Testicular volume and TAI of different age groups were recorded preoperatively and postoperatively at 3, 6, and 12 months. Clinical follow-up included a 2DUS/3DUS scan and a thorough physical examination. Recovery of testicular volume in different age groups and different ultrasonic mobility groups was compared and analyzed.
STATISTICAL ANALYSIS:
Statistical analysis was performed using the SPSS 21.0 software package (SPSS, Chicago, Illinois, United States). Measurement data were expressed as the mean±standard deviations and compared by single-factor analysis of variance. Contingency tables were constructed for comparison of categorical data using Fisher’s exact test. The repeatability and consistency within and between observers were evaluated with intraclass correlation coefficient (ICC) and Bland-Altman plots. P<0.05 was set as the threshold for statistical significance.
Results
GENERAL CONDITION:
This retrospective study included 158 patients with unilateral cryptorchidism (inguinal, 128 cases; scrotal root,25 cases). In all the children, cryptorchidism was successfully resolved after scrotal or inguinal orchiopexy. No obvious testicular or epididymal damage was observed intraoperatively and no testicular atrophy or re-ascended testes were observed postoperatively.
On the basis of the mobility of cryptorchidism monitored by real-time US, there were 113 cases in the MG and 45 cases in the RG.
CHARACTERISTICS OF DIFFERENT GROUPS OBSERVED BY US:
As shown in Figure 1, the morphology, volume, boundary, internal echo, blood distribution, and processus vaginalis of cryptorchidism was effectively observed by US. Testes in the RG tended to have blurrier borders, smaller volumes, sparser perfusion, and more uneven echoes than that in the MG (all P<0.05). There was no difference in the morphology between the MG and RG. Details of ultrasonic characteristics in the MG and RG are listed in Table 1.
Moreover, testicle location differed according to mobility. Cryptorchidism in the RG was always in a higher position, which was closer to the inner inguinal ring. Persistent processus vaginalis was more common in cryptorchidism in the MG (P=0.00) compared with that in the RG.
RELIABILITY OF VOLUME MEASUREMENT:
Bland-Altman plots demonstrated that the difference between 2 measurements taken using the VOCAL method was very close to 0, and most of the points fell within the consistent range in analysis of both intraobserver and interobserver consistency and repeatability. As shown in Figure 2, the mean differences and limits of agreement were 2.31×10−3 mL and – 31.25×10−3 to 35.86×10−3 mL for intraobserver reliability and 2.88×10−3 mL and – 83.11×10−3 to 88.87×10−3 mL for interobserver reliability, respectively.
Intraobserver and interobserver measurements of volume made using the VOCAL method were found to be strongly reliable. The intraobserver ICC was0.996 and the interobserver ICC was 0.993, with 95%confidence intervals (CIs) from 0.994 to 0.998 and 0.988 to 0.996, respectively. With the 2DUS Lambert method, the intraobserver ICC was 0.981 and the interobserver ICC was 0.962, with 95% CIs from 0.943 to 0.995 and 0.917 to 0.984, respectively. The results showed that the VOCAL method had good consistency and repeatability in volume measurement of an undescended testis, both of which were superior to the 2DUS Lambert method.
TESTICULAR VOLUME CHANGES AFTER ORCHIOPEXY IN DIFFERENT AGE GROUPS:
Testicular volume increased steadily with time after operation in all age groups (Figure 3A). Testicular volumes in Groups I and II increased significantly at 6 and 12 months after surgery compared with preoperatively (all P<0.05). In Group III, a significant increase in testicular volume was found at 12 months after surgery (P=0.049).
Preoperatively, volumes in the affected testes were smaller than that in the contralateral scrotal testes, with TAI ranging from 32.77±6.54% in Group I to 46.56±6.27% in Group III (Figure 3B). Degree of postoperative TAI decline varied with age at time of surgery. Among all age groups, TAI decreased more significantly in the 12 months postoperatively in Group I than it did preoperatively (20.35±5.65% vs. 32.77±6.54%, P=0.01). In Group II, postoperative (12-min) TAI was 39.41±5.99%, showing a tendency for decline compared to the preoperative measurement (P=0.08). No difference between preoperative and postoperative TAI measurements was observed in Group III (P>0.05).
The results showed that when cryptorchidism was extraperitoneal, as long as surgical indications were followed, orchidopexy at any age was conducive to recovery of testicular volume. However, testicular growth was more vigorous when orchiopexy was done before a child reached age 1 year.
PREOPERATIVE AND POSTOPERATIVE TAI IN DIFFERENT MOBILITY CLASSIFICATIONS:
In all age groups, the preoperative TAI in the RG was always significantly higher than in the MG (all P<0.05, Figure 4). Clinical outcomes after orchiopexy of undescended testicles differed between the 2 groups. Compared to preoperative values, postoperative TAI significantly declined in the MG in all age groups. The youngest patients with postoperative TAI of 11.76±3.65% recovered the most volume. In the RG, the difference between postoperative and preoperative TAI in Group I (age <1 year) was statistically significant (61.22± 4.40% vs. 50.42±5.15%; P<0.05).
The results showed that for the MG, performing surgery at any age is beneficial, whereas for the RG, surgery can improve testicular development only if it is performed before a patient reaches age 1 year.
Discussion
In this study, 158 patients with unilateral cryptorchidism were evaluated preoperatively and postoperatively using 3DUS with the VOCAL technique. Reliability was excellent with narrow limits of agreement for intraobserver and interobserver volume measurements, and superior to using the 2D Lambert method. TAI values can objectively reflect the degree of testicular volume damage and postoperative volume recovery. Ultrasonic mobility evaluation is beneficial for preoperative and postoperative management of cryptorchidism.
Our results showed that the VOCAL method had good consistency and repeatability in volume measurement of undescended testes. Compared to the reliability rating list raised by Martins and Nastri [24], our intraobserver and interobserver ICCs were 0.996 and 0.993, respectively, which both rank as good. As shown in Table 2, the VOCAL method was superior to the 2DUS Lambert method (intraobserver ICC ranked as moderate; interobserver ICC ranked as poor). In a recent study of pediatric testicular volume measurement [9], the authors found that even if the same testes were measured, a 20% difference in ultrasonic volumes was seen in 25% of intraobserver measurements and in 35% of interobserver measurements. In that study, testicular volume was calculated by the ellipsoid formula: volume=0.71×length×width×height. Usually, 2 aspects of volume measurements can be captured in one image: length and height. However, the probe must then be rotated to obtain the width. Because the testis is mobile in the scrotum, finding the appropriate location to make the third measurement is prone to error caused by failure to line up along one of the previously measured axes. The compressibility of the testis can also lead to variation in measurements. Thus, small differences may be magnified when multiplied in 3 dimensions [9]. Given the mobility and compressibility of testicles, and the presence of irregularities in cryptorchidism, it may be impossible to accurately obtain 2 maximum vertical planes. However, these deficiencies can be avoided when volume is measured using the VOCAL technique. VOCAL is well recognized and widely used in many fields, especially for evaluation of irregularly shaped objects [10]. We believe that 3DUS with the VOCAL technique is clinically useful and very suitable for preoperative and postoperative evaluation of cryptorchidism, given its reliability and the testicular volume measurements and TAI values demonstrated in this study.
TAI was first proposed for use in patients with varicocele. In that application, studies suggest that a 20% volume differential is physiologically significant and it serves as an indication for surgical correction [25]. In this study, we found that in patients of any age, the preoperative volume of an undescended testis was always less than that of the contralateral scrotal testis, with TAI values ranging from 32.77% in the youngest (0 to 1 year) to 46.56% in the oldest (6 to 9 years). The findings are consistent with those from a study reported by Niedzielski et al. [26]. They found that the volume differential at initial diagnosis ranged from 27.1% to 52.8%. The biggest loss in volume was in boys aged 4 to 10 years (35.4% to 52.8%). In similar follow-up studies of cryptorchidism, a preoperative reduction >50% of testicular volume or a postoperative testicular volume <25% of volume of the contralateral testis was defined as testicular atrophy [27]. From this perspective, does traditional orchidopexy still make sense for patients who have a loss of volume >50% at their initial diagnosis? We found that after surgery, testicular volume increased to varying degrees in patients of all ages, regardless of their preoperative index TAI value and even if their preoperative volume lost was approximately 50%. Testicular growth was more vigorous when orchiopexy was done before age 1 year. This result is consistent with previous studies [26]. In short, our recommendation is that, once cryptorchidism is diagnosed, orchiopexy should be performed as soon as possible, and preferably before the patient reaches age 1 year, as long as indications for surgery are satisfied. In children aged >1 year, more or less volume recovery can be achieved with aggressive surgery.
In our study, mobility induced by position changes, Valsalva movements, and manipulation of extraperitoneal cryptorchidism was detected with US. We found that cryptorchidism in the RG was located closer to the inner inguinal ring and tended to have blurrier borders, smaller volumes, sparser perfusion, and more uneven echo. Cryptorchidism in the MG was better developed than that in the RG at initial diagnosis, and, most importantly, the prognosis for undescended testicles differed between the 2 groups. In MG, the postoperative TAI fell significantly in each age group, indicating that even if the prime time for orchiopexy (within 18 months suggested by AUA [3]) has passed, aggressive surgery can still lead to volume recovery. In the RG, in contrast, only surgery before age 1 year results in a significant improvement in testicular volume. For boys older than age 1 year with a restricted undescended testis, no significant volume catch-up growth was observed during our 12-month postoperative follow-up. We continue to recommend that these children undergo early orchiopexy to prevent testicular pathology. In this group, additional data and longer follow-up may be needed to evaluate postoperative increases in testicular volume. In particular, it should be noted that in addition to performing conventional US imaging in initial diagnosis of cryptorchidism, information on testis mobility also should be obtained. Once restricted cryptorchidism is found, orchidopexy should be performed before a child reaches age 1 year to ensure a better postoperative outcome, which is important in these individuals. In general, US evaluation of extraperitoneal cryptorchidism mobility is of great significance in determining timing of surgery.
Factors important to determining mobility in cases of cryptorchidism include testis location, spermatic cord development, and condition of the processus vaginalis (persistence or occlusion) [14,27]. The processus vaginalis is usually occluded during the first year of life [28]. When it is partially degenerated, it leaves behind fibrous and inelastic tissue. This residual structure blocks the spermatic cord’s response to somatic cell growth, anchoring the testicles at a higher position [29]. In this study, we found that incidence of widely patent processus vaginalis was lower in the RG. Meanwhile, testes in the RG were located higher in the retroperitoneum and the TAI value was increased. The strong correlation between TAI in cryptorchid testes and their location in various age groups was noted by Zvizdic et al. [22]. In addition, there was no significant decrease in TAI after orchiopexy in the older patients in the RG, despite the success of surgery. The key factor for testis survival after orchidopexy is to retain as much blood supply to them as possible. The testicular artery and vas deferens artery running through the spermatic cord are the primary source of blood supply to the testes. The postoperative blood supply may be reduced if the spermatic cord is twisted and pulled too tightly, it is injured when being dissociated or fixed, or fibrous scars are compressed or adhesions develop [18,27,29]. We suspect that these scenarios may be related to the poor postoperative volume recovery in the RG. In a paper discussing possible causes of chronic pain after inguinal herniorrhaphy, scholars explained how US can be used to identify the angle at which the spermatic cord is bent and to assess adherence of the spermatic cord to the deep inguinal ring [18]. Therefore, we believe that assessment of cryptorchidism mobility may be helpful for clinical management. Unfortunately, we did not assess postoperative testicular mobility and spermatic cord bending angle in the follow-up of this study. The focus of our next work will be to reveal the underlying reasons for poor postoperative recovery from cryptorchidism, especially in the group with limited activity.
Our study has some limitations. First, it was a retrospective analysis and only subjects who had undergone successful orchiopexy and for whom complete clinical and ultrasonic data were available were included. That may have caused bias in the research. Second, no age-specific nomogram for contralateral scrotal testis and undescended testis has been published. Whether the TAI value is exaggerated to some extent because of asymmetric growth (contralateral scrotal testis/undescended testis) in patients close to puberty remains to be determined. Follow-up in our study ended at 12 months after surgery. A survey of cryptorchidism with average follow-up of 34 months showed that most testicular atrophy occurred within the first 2 years after orchiopexy, with a median time of 13 months [27]. Therefore, studies with longer follow-up may be confirm our results. Last but not least, although testicle volume may reflect development of convoluted fine tubules in the testes and spermatogenic function, it cannot replace a histopathological examination. Fortunately, in recent years, scholars have devoted time to studying the role of new ultrasonic techniques such as shear wave elastography, 3D energy Doppler, and application of artificial intelligence in follow-up of surgery for cryptorchidism.
Conclusions
Undescended testis is one of the most common genitourinary malformations in children. Clinical decision-making about treatment of the condition depends on accurate preoperative assessment. With preoperative and postoperative evaluation using the VOCAL technique for 3DUS, we found that characteristics of an undescended testis can be observed effectively. The VOCAL technique for 3DUS is superior to the 2DUS Lambert method and produces measurements of volume of an undescended testis that are highly reliable. Measurement of TAI value and evaluation of ultrasonic mobility are beneficial for management of an undescended testis.
Figures
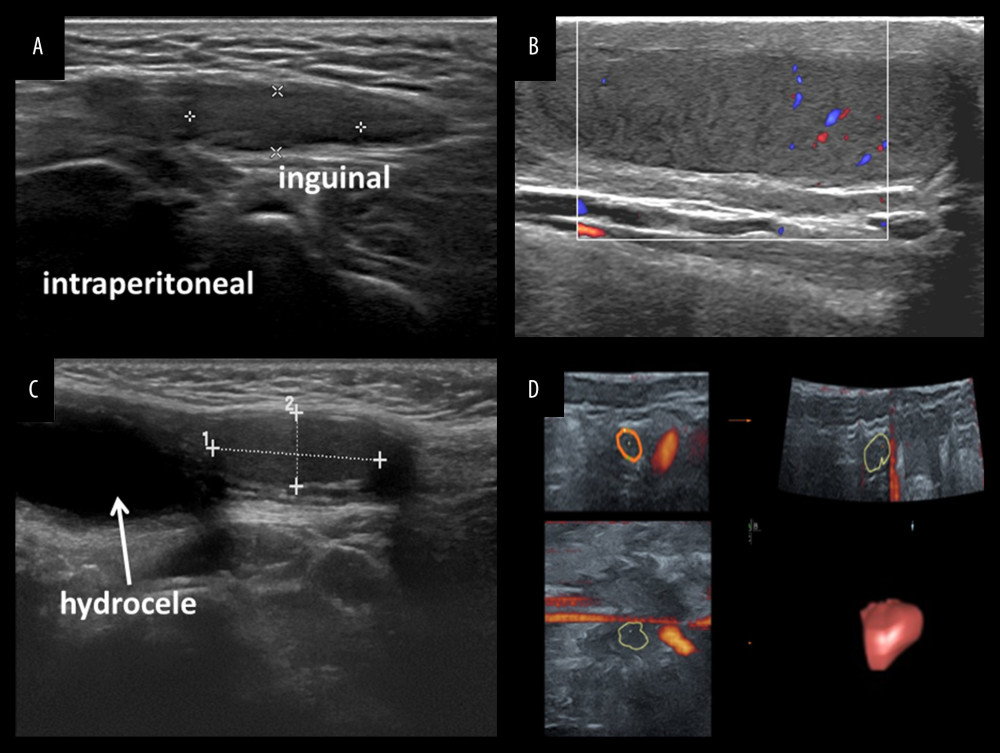 Figure 1. Ultrasonography of undescended testicle and volume measurement by VOCAL technique. (A) Inguinal clear boundary and reduced volume; (B) Prescrotal cryptorchidism with uneven echo and sparse perfusion; (C) Cryptorchidism with patent processus vaginalis (D) Testicular volume measured by 3-dimensional ultrasound VOCAL technique.
Figure 1. Ultrasonography of undescended testicle and volume measurement by VOCAL technique. (A) Inguinal clear boundary and reduced volume; (B) Prescrotal cryptorchidism with uneven echo and sparse perfusion; (C) Cryptorchidism with patent processus vaginalis (D) Testicular volume measured by 3-dimensional ultrasound VOCAL technique. 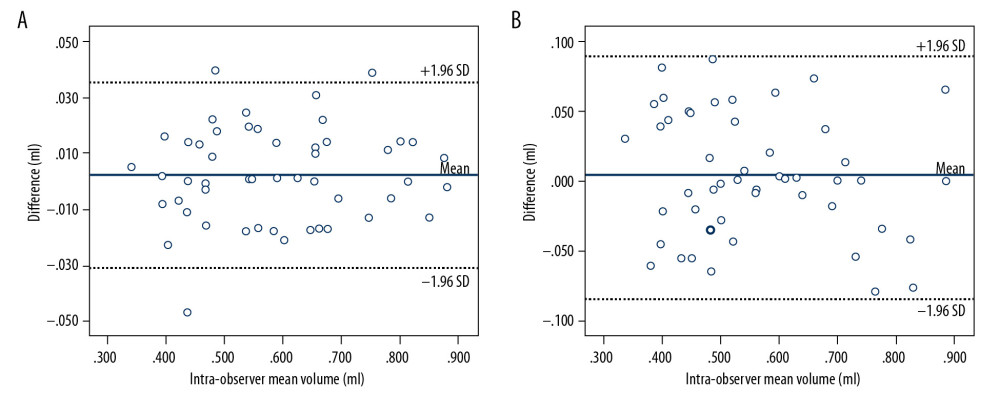 Figure 2. Difference in intraobserver and interobserver volume measurements plotted against their means. (A) Intraobserver volume measurements; (B) Interobserver volume measurements.
Figure 2. Difference in intraobserver and interobserver volume measurements plotted against their means. (A) Intraobserver volume measurements; (B) Interobserver volume measurements. 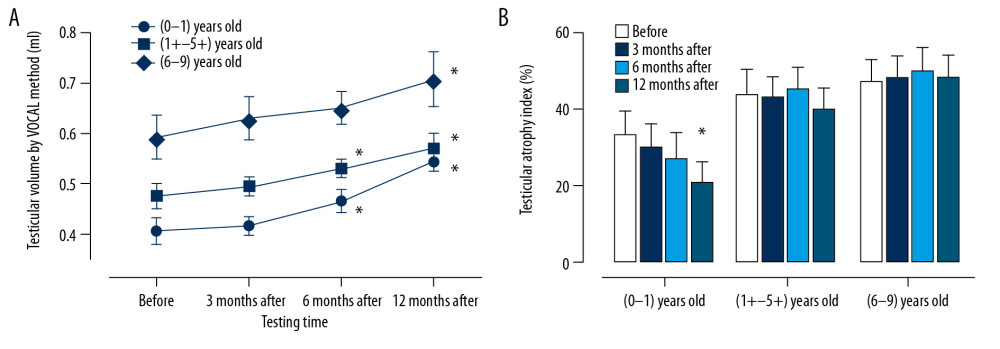 Figure 3. Testicular volume changes after orchiopexy in different age groups. (A) Line chart of testicular volume plotted against testing time; (B) Histogram of testicular atrophy index at different periods. * Compared with before operation, P<0.05.
Figure 3. Testicular volume changes after orchiopexy in different age groups. (A) Line chart of testicular volume plotted against testing time; (B) Histogram of testicular atrophy index at different periods. * Compared with before operation, P<0.05. 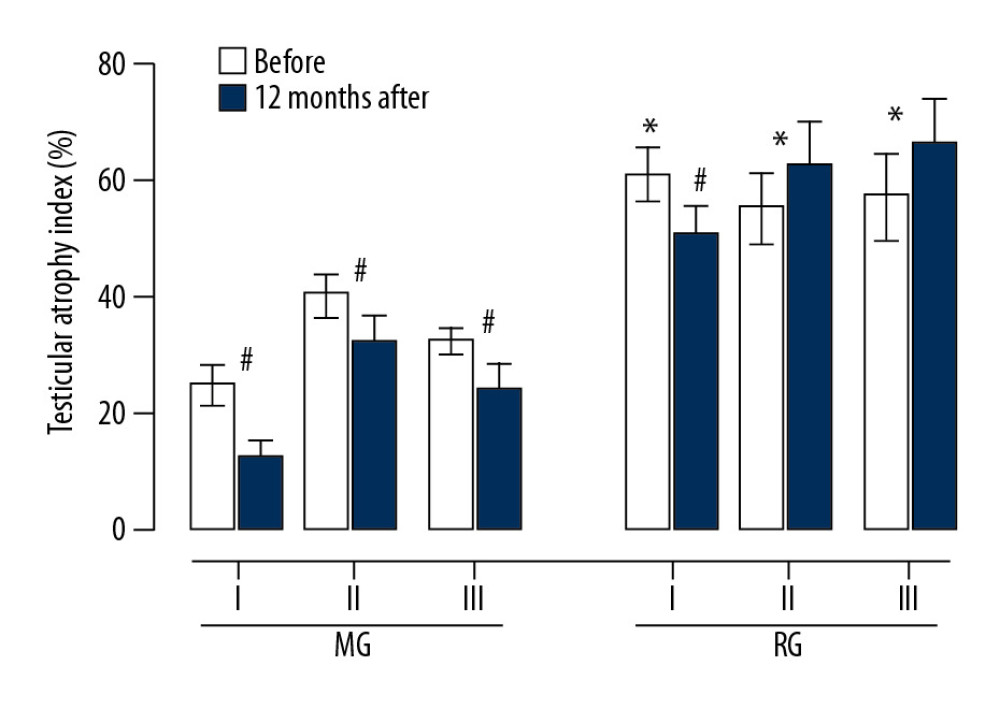 Figure 4. Preoperative and postoperative TAI in different ultrasonic classifications. MG – mobile group; RG – restricted group; I – Group I (age 0 to 1 year); II – Group II (age >1 to <6 years); III – Group III (age 6 to 9 years). * Compared with MG, P<0.05; # Compared with before, P<0.05.
Figure 4. Preoperative and postoperative TAI in different ultrasonic classifications. MG – mobile group; RG – restricted group; I – Group I (age 0 to 1 year); II – Group II (age >1 to <6 years); III – Group III (age 6 to 9 years). * Compared with MG, P<0.05; # Compared with before, P<0.05. References
1. Shepard CL, Kraft KH, The nonpalpable testis: A narrative review: J Urol, 2017; 198(6); 1410-17
2. Kim JK, Chua ME, Ming JM, A critical review of recent clinical practice guidelines on management of cryptorchidism: J Pediatr Surg, 2018; 53(10); 2041-47
3. Kolon TF, Herndon CD, Baker LAAmerican Urological Association, Evaluation and treatment of cryptorchidism: AUA guideline: J Urol, 2014; 192(2); 337-45
4. Fratrić I, Šarac D, Antić J, Impalpable testis: Evaluation of diagnostic and treatment procedures and our treatment protocol: Biomed Res Int, 2018; 2018 3143412
5. Shin HJ, Lee YS, Yoon H, Testicular volume and elasticity changes in young children with undescended testes: Med Ultrason, 2017; 19(4); 380-85
6. Moriya K, Nakamura M, Nishimura Y, Impact of preoperative ultrasonographic evaluation for detection of a viable testis in patients with a unilateral nonpalpable testis: J Ultrasound Med, 2018; 37(7); 1665-70
7. Kim SO, Hwang EC, Hwang IS, Testicular catch up growth: The impact of orchiopexy age: Urology, 2011; 78(4); 886-89
8. Oehme NHB, Roelants M, Bruserud IS, Ultrasound-based measurements of testicular volume in 6- to16-year-old boys – intra- and interobserver agreement and comparison with Prader orchidometry: Pediatr Radiol, 2018; 48(12); 1771-78
9. Welliver C, Cardona-Grau D, Elebyjian L, Surprising interobserver and intra-observer variability in pediatric testicular ultrasound volumes: J Pediatr Urol, 2019; 15(4); 386.e1-6
10. You JH, Lv GR, Liu XL, He SZ, Reference ranges of fetal spleen biometric parameters and volume assessed by three-dimensional ultrasound and their applicability in spleen malformations: Prenat Diagn, 2014; 34(12); 1189-97
11. Bravo-Valenzuela NJ, Peixoto AB, Carrilho MC, Fetal cardiac function by three-dimensional ultrasound using 4D-STIC and VOCAL – an update: J Ultrason, 2019; 19(79); 287-94
12. Wang H, Yan B, Yue L, The diagnostic value of 3d power doppler ultrasound combined with vocal in the vascular distribution of breast masses: Acad Radiol, 2020; 27(2); 198-203
13. Czuczwar P, Wozniak S, Szkodziak P, Influence of ulipristal acetate therapy compared with uterine artery embolization on fibroid volume and vascularity indices assessed by three-dimensional ultrasound: Prospective observational study: Ultrasound Obstet Gynecol, 2015; 45(6); 744-50
14. Banieghbal B, Davies M, Laparoscopic evaluation of testicular mobility as a guide to management of intra-abdominal testes: World J Urol, 2003; 20(6); 343-45
15. Caterino S, Lorenzon L, Cavallini M, Epididymal-testicular fusion anomalies in cryptorchidism are associated with proximal location of the undescended testis and with a widely patent processus vaginalis: J Anat, 2014; 225(4); 473-78
16. Sameshima YT, Yamanari MG, Silva MA, The challenging sonographic inguinal canal evaluation in neonates and children: An update of differential diagnoses: Pediatr Radiol, 2017; 47(4); 461-72
17. Jedrzejewski G, Wieczorek AP, Osemlak P, Nachulewicz P, The role of ultrasound in the management of undescended testes before and after orchidopexy – an update: Medicine (Baltimore), 2016; 95(51); e5731
18. Qiu ZY, Chen Y, Tang JX, Chen L, Ultrasonography in diagnosis and analysis of chronic pain following anterior open inguinal herniorrhaphy: BMC Surg, 2018; 18(1); 28
19. Moran CM, The safe use of ultrasound in medical diagnosis: Ultrasound, 2013; 21(2); 107
20. Kim YJ, Kwon A, Jung MK, Incidence and prevalence of central precocious puberty in Korea: An epidemiologic study based on a national database: J Pediatr, 2019; 208; 221-28
21. Lambert B, The frequency of mumps and mumps orchitis, and the consequences for sexuality and fertility: Acta Genet, 1951; 2; 1
22. Zvizdic Z, Milisic E, Halimic A, Testicular volume and testicular atrophy index as predictors of functionality of unilaterally cryptorchid testis: Med Arch, 2014; 68(2); 79-82
23. Adler DD, Carson PL, Rubin JM, Doppler ultrasound color flow imaging in the study of breast cancer: Preliminary findings: Ultrasound Med Biol, 1990; 16(6); 553-59
24. Martins WP, Nastri CO, Interpreting reproducibility results for ultrasound measurements: Ultrasound Obstet Gynecol, 2014; 43(4); 479-80
25. Diamond DA, Gargollo PC, Caldamone AA, Current management principles for adolescent varicocele: Fertil Steril, 2011; 96(6); 1294-98
26. Niedzielski J, Pisarska K, Przewratil P, The usefulness of testicular atrophy index in the assessment of undescended testicle – preliminary report: Rocz Akad Med Bialymst, 2003; 48; 112-14
27. Tseng CS, Huang KH, Kuo MC, The impact of primary location and age at orchiopexy on testicular atrophy for congenital undescended testis: Sci Rep, 2019; 9(1); 9489
28. Rafailidis V, Varelas S, Apostolopoulou F, Rafailidis D, Non-obliteration of the processus vaginalis: Sonography of related abnormalities in children: J Ultrasound Med, 2016; 35(4); 805-18
29. Favorito LA, Costa WS, Sampaio FJ, Relationship between the persistence of the processus vaginalis and age in patients with cryptorchidism: Int Braz J Urol, 2005; 31(1); 57-61
Figures
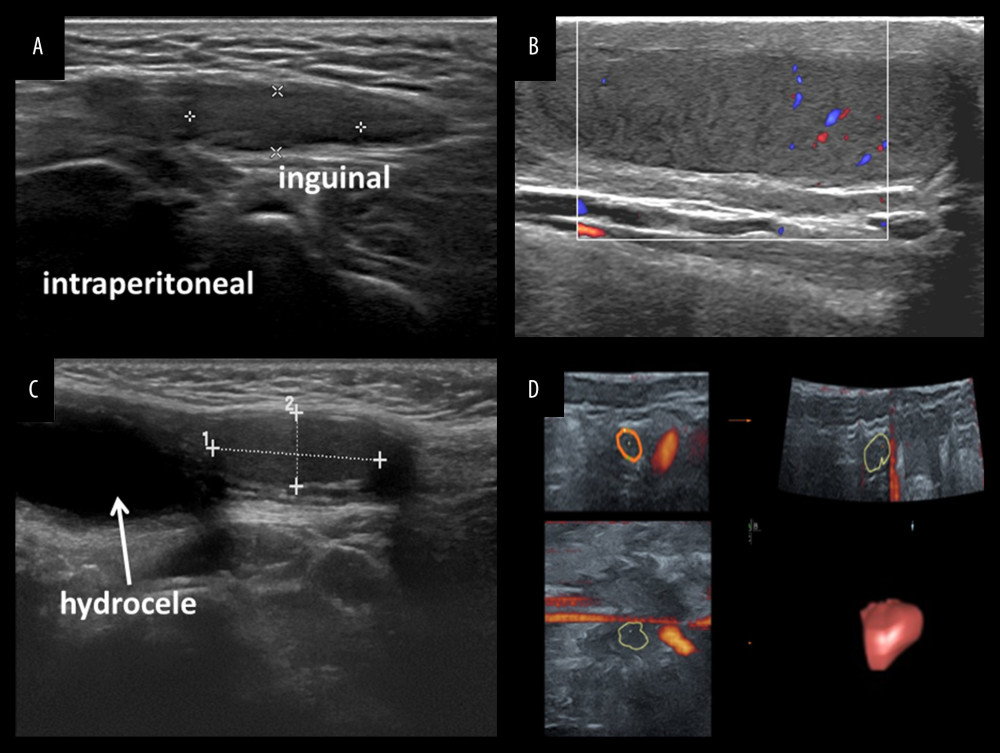 Figure 1. Ultrasonography of undescended testicle and volume measurement by VOCAL technique. (A) Inguinal clear boundary and reduced volume; (B) Prescrotal cryptorchidism with uneven echo and sparse perfusion; (C) Cryptorchidism with patent processus vaginalis (D) Testicular volume measured by 3-dimensional ultrasound VOCAL technique.
Figure 1. Ultrasonography of undescended testicle and volume measurement by VOCAL technique. (A) Inguinal clear boundary and reduced volume; (B) Prescrotal cryptorchidism with uneven echo and sparse perfusion; (C) Cryptorchidism with patent processus vaginalis (D) Testicular volume measured by 3-dimensional ultrasound VOCAL technique.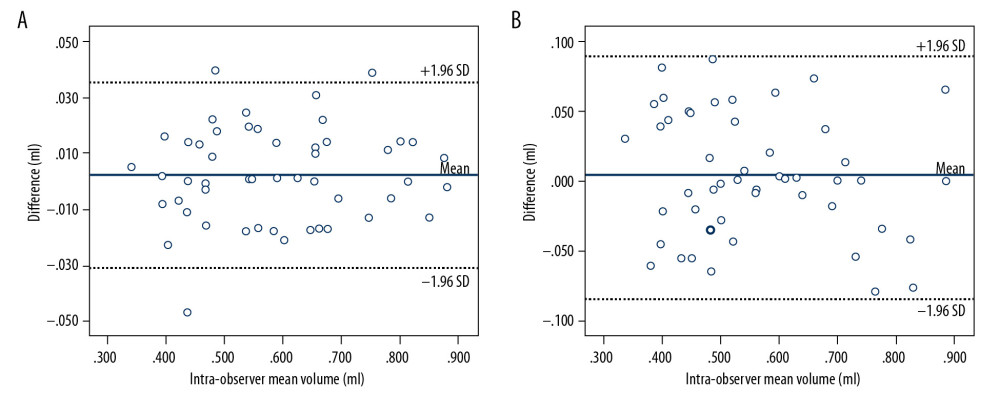 Figure 2. Difference in intraobserver and interobserver volume measurements plotted against their means. (A) Intraobserver volume measurements; (B) Interobserver volume measurements.
Figure 2. Difference in intraobserver and interobserver volume measurements plotted against their means. (A) Intraobserver volume measurements; (B) Interobserver volume measurements.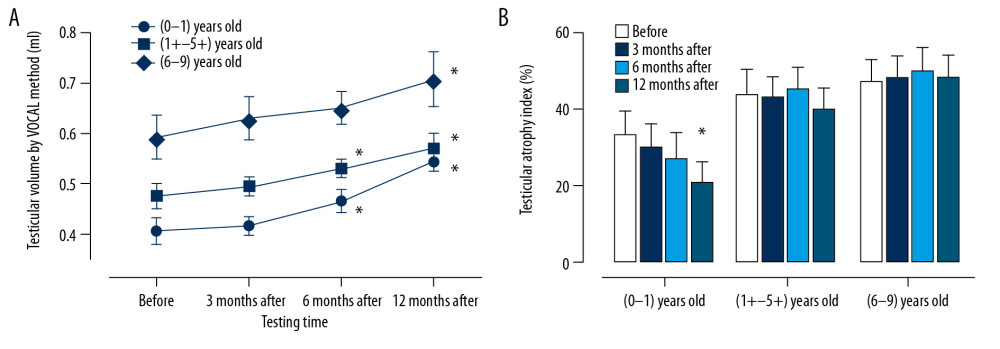 Figure 3. Testicular volume changes after orchiopexy in different age groups. (A) Line chart of testicular volume plotted against testing time; (B) Histogram of testicular atrophy index at different periods. * Compared with before operation, P<0.05.
Figure 3. Testicular volume changes after orchiopexy in different age groups. (A) Line chart of testicular volume plotted against testing time; (B) Histogram of testicular atrophy index at different periods. * Compared with before operation, P<0.05.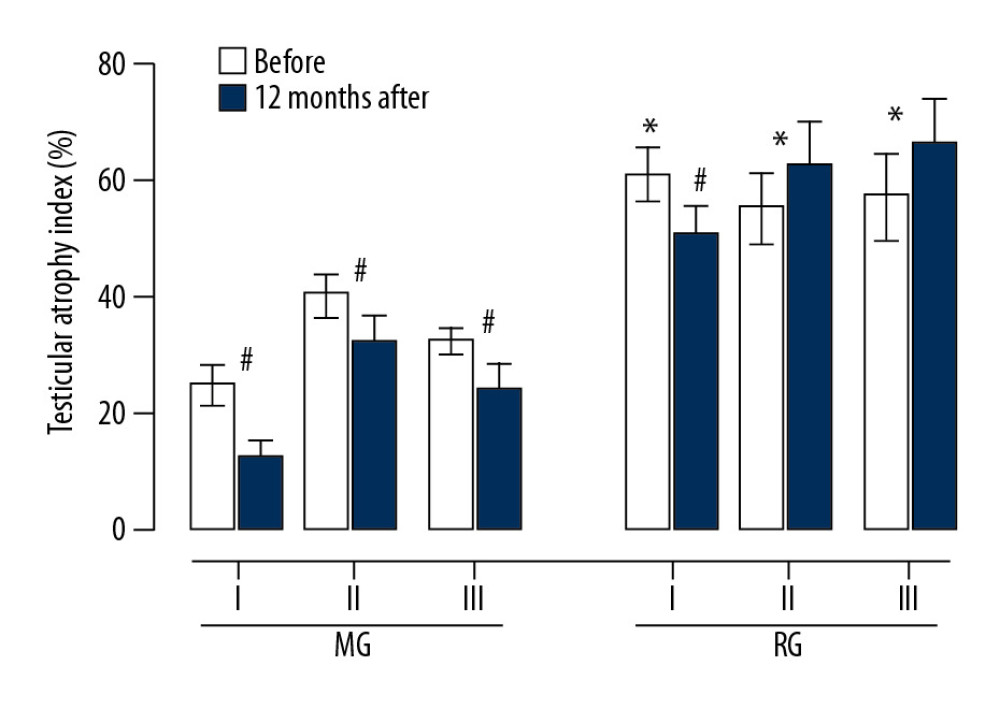 Figure 4. Preoperative and postoperative TAI in different ultrasonic classifications. MG – mobile group; RG – restricted group; I – Group I (age 0 to 1 year); II – Group II (age >1 to <6 years); III – Group III (age 6 to 9 years). * Compared with MG, P<0.05; # Compared with before, P<0.05.
Figure 4. Preoperative and postoperative TAI in different ultrasonic classifications. MG – mobile group; RG – restricted group; I – Group I (age 0 to 1 year); II – Group II (age >1 to <6 years); III – Group III (age 6 to 9 years). * Compared with MG, P<0.05; # Compared with before, P<0.05. Tables
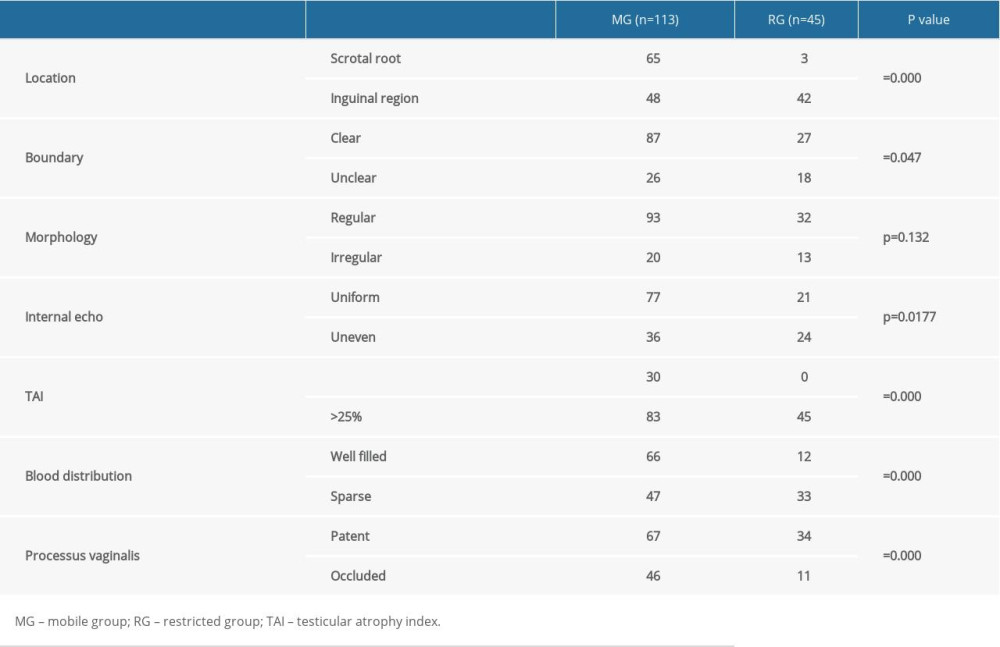 Table 1. Characteristics of different groups observed by ultrasound.
Table 1. Characteristics of different groups observed by ultrasound.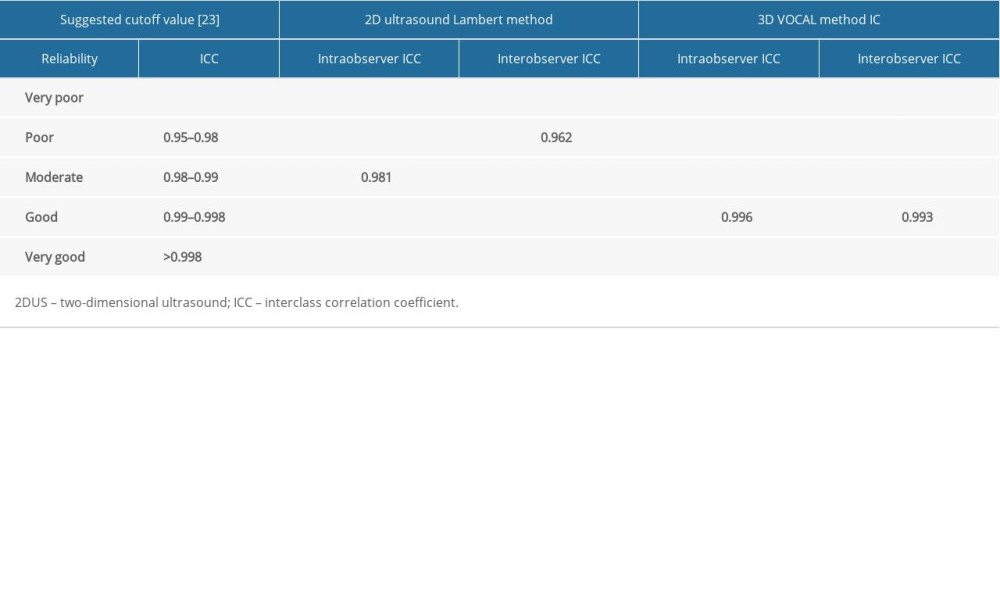 Table 2. Comparison of reliability of volume measurement by 2DUS Lambert method and 3D VOCAL method.
Table 2. Comparison of reliability of volume measurement by 2DUS Lambert method and 3D VOCAL method.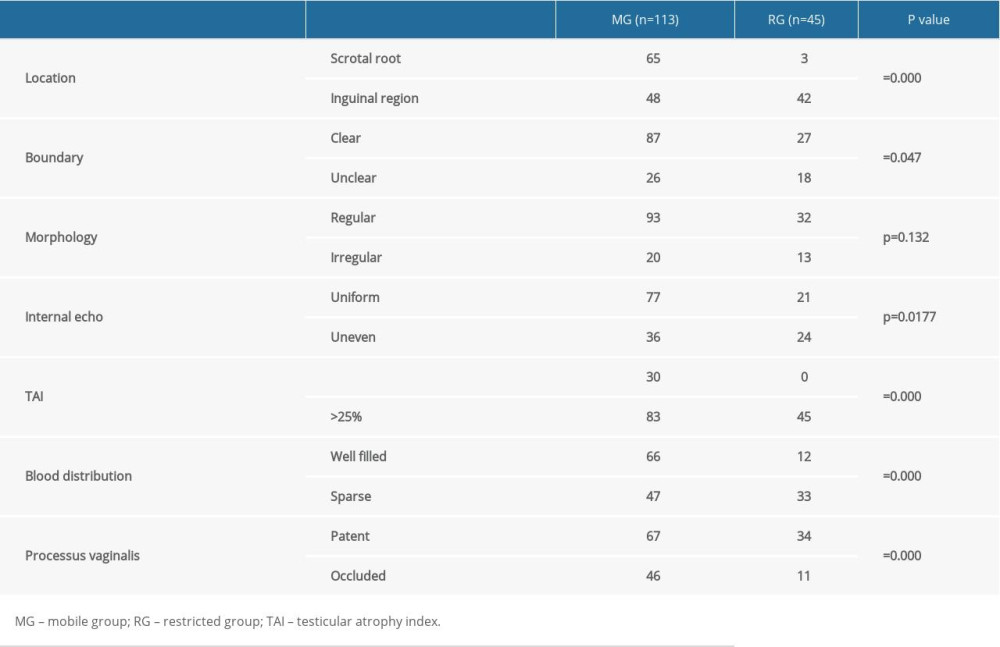 Table 1. Characteristics of different groups observed by ultrasound.
Table 1. Characteristics of different groups observed by ultrasound.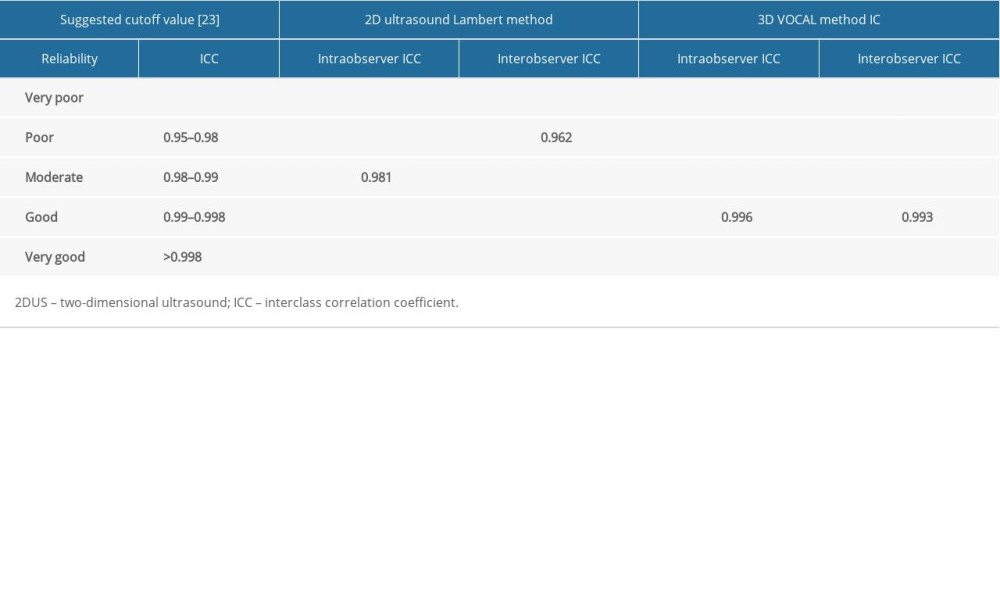 Table 2. Comparison of reliability of volume measurement by 2DUS Lambert method and 3D VOCAL method.
Table 2. Comparison of reliability of volume measurement by 2DUS Lambert method and 3D VOCAL method. In Press
06 Mar 2024 : Clinical Research
Comparison of Outcomes between Single-Level and Double-Level Corpectomy in Thoracolumbar Reconstruction: A ...Med Sci Monit In Press; DOI: 10.12659/MSM.943797
21 Mar 2024 : Meta-Analysis
Economic Evaluation of COVID-19 Screening Tests and Surveillance Strategies in Low-Income, Middle-Income, a...Med Sci Monit In Press; DOI: 10.12659/MSM.943863
10 Apr 2024 : Clinical Research
Predicting Acute Cardiovascular Complications in COVID-19: Insights from a Specialized Cardiac Referral Dep...Med Sci Monit In Press; DOI: 10.12659/MSM.942612
06 Mar 2024 : Clinical Research
Enhanced Surgical Outcomes of Popliteal Cyst Excision: A Retrospective Study Comparing Arthroscopic Debride...Med Sci Monit In Press; DOI: 10.12659/MSM.941102
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








