07 November 2020: Clinical Research
Effect of Red Blood Cell Storage Duration on Outcomes of Isolated Traumatic Brain Injury
Kun Xiao1AE, Fei Zhao2AE, Qiang Liu3B, Jinliang Jiang4B, Zhiyong Chen5C, Wei Gong6D, Zengwang Zheng7F, Aiping Le1A*DOI: 10.12659/MSM.923448
Med Sci Monit 2020; 26:e923448
Abstract
BACKGROUND: The aim of this study was to investigate the effects of red blood cell (RBC) storage duration on the outcomes of adult isolated traumatic brain injury (iTBI) patients after transfusion.
MATERIAL AND METHODS: A total of 1252 adult iTBI patients who received the fresh RBCs (stored for £14 days) or old RBCs (stored for >14 days) were finally enrolled in this study. The primary outcome was 90-day mortality. The secondary outcomes were in-hospital mortality, nosocomial infection, and complications.
RESULTS: By 90 days after RBC transfusion, 89 patients (17.0%) had died in the fresh RBC group, and 107 had died (14.7%) in the old RBC group, with no significant difference in 90-day mortality between the 2 groups (OR=1.192, 95% CI: 0.877–1.620, P=0.261). According to ISS score, no differences were discovered in mild injury (OR=1.079, 95% CI: 0.682–1.707, P=0.746), severe injury (OR=1.055, 95% CI: 0.634–1.755, P=0.838), and more severe injury (OR=1.940, 95% CI: 0.955–3.943, P=0.064). For GCS score, there were no differences in mild injury (OR=1.546, 95% CI: 0.893–2.676, P=0.118), moderate injury (OR=0.965, 95% CI: 0.616–1.513, P=0.877), and severe injury (OR=1.332, 95% CI: 0.677–2.620, P=0.406). We also observed no significant differences in secondary outcomes.
CONCLUSIONS: Use of old RBCs did not increase the 90-day mortality in adult iTBI patients.
Keywords: Brain Injuries, Erythrocytes, Mortality, Brain Injuries, Traumatic, Erythrocyte Transfusion, Multivariate Analysis, Preservation, Biological, Regression Analysis, Risk Factors, Time Factors
Background
Traumatic brain injury (TBI), a leading cause of long-term disability and death [1], is characterized by traumatic structural damage and/or cerebral dysfunction caused by external forces [2]. More than 10.0 million humans experience TBI annually worldwide [3], and over 2.5 million present to the emergency department each year [4]. Early observational research reported that the mortality rate of TBI was approximately 40% [5]. Previous studies reported the effects of red blood cells (RBCs) storage duration on outcomes in critical patients [6,7]. Due to the large oxygen consumption of the human brain, anemia can easily lead to brain damage that requires blood transfusion [8]. To the best of our knowledge, however, there have been few large-sample clinical studies of the effect of RBC storage duration on TBI outcomes. Therefore, it is important for clinicians to focus on the effects of RBCs storage duration in patients with TBI.
Anemia is associated with poor outcomes in brain injury patients [9–12], such as TBI and ischemic stroke, which is a common symptom of TBI, with 30–40% incidence [13]. In the early development of anemia, vasodilation in a healthy brain can maintain the cerebral oxygen delivery [14]. When brain injury occurs, the compensatory mechanisms are blocked and cellular hypoxia exacerbates due to the decreased concentrations of hemoglobin (Hb) [15]. Evidence indicates that RBCs transfusion can improve brain metabolism and oxygenation [8,16]. Early studies found that nearly 50% of patients needed to receive a blood transfusion [17], and approximately 50% of anemic patients with TBI were transfused with RBCs at least once in the neurological intensive care unit (NICU) during hospitalization [13,18,19].
The blood storage medium can lead to significant alterations in the biochemical and metabolic processes of RBCs. These changes, called “storage lesions”, worse with longer duration of storage, and can affect the function, viability, and quality of RBCs [20–23]. Trauma studies discovered that use of old RBCs was associated with increasing risk of mortality, infections, and deep-vein thrombosis (DVT) [24], while several studies failed to find any adverse effects of transfusion with old RBCs [25,26], indicating that the effect of RBCs storage duration in TBI patients is unclear. However, there is no consensus on the definition of fresh or old RBCs. A study in the New England Journal of Medicine demonstrated that transfusion with RBCs stored for more than 2 weeks was associated with a significantly increased risk of postoperative complications, as well as reduced short-term and long-term survival, in patients undergoing cardiac surgery [27]. In the present study, we formed 2 groups according to the storage duration of RBCs to investigate the differences in adult isolated TBI (iTBI) patients who received the RBCs transfusion with different storage durations.
Material and Methods
PATIENTS:
This study retrospectively screened 3468 consecutive patients with TBI admitted to the Department of Neurosurgery at the First Affiliated Hospital of Nanchang University from Jan 2013 to Jan 2018. After screening, 1252 patients with iTBI were finally enrolled and divide into 2 groups in this study. The fresh RBC group was defined as the RBCs transfusion with a storage period ≤14 days, and the old RBC group was referred to the RBCs transfusion with a storage duration >14 days. iTBI was defined as the presence of intracranial hemorrhage, brain contusion, diffuse axonal injury, or cerebral edema with an abbreviated injury scale (AIS) score ≤1 for all other body regions. This research was approved by the Institutional Review Board (IRB) of the First Affiliated Hospital of Nanchang University, and the approval number was 2019 (052).
Patients who met the following criteria were included: (1) age ≥16 years old; (2) admission to hospital within 12 h after injuring; (3) the RBCs transfusion at least once during hospitalization; (4) AIS score ≥3 for head and AIS ≤1 for all other body regions in iTBI patients [28]. Exclusion criteria were: (1) the length of hospital stay (LOS) <72 h; (2) patients who received both fresh and old RBCs transfusion in the hospital; (3) pregnancy; (4) lost to follow-up.
DATA COLLECTION:
All RBCs were leuko-reduced without irradiation or washing, and citrate phosphate dextrose adenine (CPDA) was used as the anticoagulant. After pretreatment, the RBCs were stored in the blood storage refrigerator at 2°C to 6°C. All RBCs had been transfused within 35 days after collection.
The demographic and injury information was recorded, including Glasgow coma scale (GCS) score, injury severity score (ISS), head and neck AIS, and Hb and RBCs transfusion history. The ISS score is the quadratic sum of the highest AIS values for the 3 most severely damaged areas of the body. The definitions for the severity of injury were: (1) mild injury: ISS score ≤16; (2) severe injury: 16< ISS score ≤25; (3) more severe injury: ISS score >25. The classification for injury based on GCS score were: (1) mild injury: score at 3–8; (2) moderate injury: score at 9–12; (3) severe injury: score at 13–14.
ITBI MANAGEMENT:
All patients were strictly managed in accordance with iTBI hospital guidelines, which were proposed based on the Brain Trauma Foundation information [29]. In general, patients underwent the RBCs test with 8 g/dL of Hb transfusion trigger to maintain the target concentration of Hb close to 10 g/dL. However, the transfusion indications and Hb target concentrations for each particular patient were decided by the attending physician, which were independent of the research purposes. The Department of Blood Transfusion randomly provided patients with fresh or old RBCs transfusion.
OUTCOMES:
The 90-day mortality rate served as the primary outcome. secondary outcomes were in-hospital mortality, nosocomial infection (pulmonary, wound, and urinary tract infections), and complications (myocardial infarction, acute kidney injury (AKI) and DVT).
STATISTICAL ANALYSIS:
The statistical analysis was performed using SPSS version 22.0 (IBM Corp., Armonk, NY, USA) and GraphPad Prism 6 (GraphPad Software, Inc., San Diego, CA, USA). Numerical variables are presented as the mean±standard deviation (SD) by
Results
PATIENT CHARACTERISTICS:
A total of 3468 patients were screened with an electronic medical record system. Of these, 2162 cases (62.34%) met 1 of exclusion criterion, and 1306 cases (554 in the fresh RBCs group and 752 in the old RBCs group) were finally enrolled to conduct the 90-day mortality analysis. The overall rate of loss to follow-up in patients with iTBI was 4.13% at 90 days (Figure 1).
As shown in Table 1, the parameters age (t=1.730, P=0.084), sex (χ2=3.044, P=0.081), weight (t=−1.647, P=0.100), diabetes history (χ2<0.001, P=0.992), hypertension history (χ2=0.002, P=0.968), GCS score on admission (t=0.916, P=0.360), head and neck AIS (t=0.009, P=0.993), ISS score (t=−0.810, P=0.405), LOS in hospital (t=−1.183, P=0.237), LOS in ICU (t=0.904, P=0.336), duration of mechanical ventilation (t=−1.37, P=0.172), brain injury (subdural hematoma, epidural hematoma, subarachnoid hemorrhage, intracerebral hemorrhage, intraventricular hemorrhage, brain contusion and diffuse axonal injury) (χ2=10.662, P=0.099), and causes of injury (non-accidental injury, fall over injury, traffic injury, and falling from a height injury) (χ2=6.353, P=0.096) were no significantly different between the 2 groups.
TRANSFUSION OF RBCS IN PATIENTS WITH ITBI:
In Table 2, there were no statistically significant differences in patients who received ≥4 u RBCs (χ2=0.492, P=0.483), RBC transfusion volumes of per patient (t=−1.180, P=0.238), or pre-transfusion Hb (t=−1.579, P=0.115) between the 2 groups. The dose-response relationship curve of blood transfusion volumes of iTBI patients is presented in Figure 2. The results revealed no dose-response relationship between blood transfusion volumes and 90-day mortality. In addition, no obvious differences were founded in patients who were transfused other blood components, including platelets (Z<0.001, P=1.000), FFP (Z=0.997, P=0.319) and cryoprecipitate (Z<0.001, P=1.000), between the 2 groups.
OUTCOMES RELATED TO DEATH AND MAJOR ILLNESSES:
The results of single-factor logistic regression are shown in Figures 3 and 4. At 90 days after RBC transfusion, 89 patients (17.0%) died in the fresh RBC group, and 107 died (14.7%) in the old RBC group, with no significant difference in 90-day mortality between the 2 groups (OR=1.192, 95% CI: 0.877–1.620, P=0.261). According to ISS score, no differences were discovered among mild injury (OR=1.079, 95% CI: 0.682–1.707, P=0.746), severe injury (OR=1.055, 95% CI: 0.634–1.755, P=0.838), and more severe injury (OR=1.940, 95% CI: 0.955–3.943, P=0.064). For GCS score, there were no significant differences in mild injury (OR=1.546, 95% CI: 0.893–2.676, P=0.118), moderate injury (OR=0.965, 95% CI: 0.616–1.513, P=0.877), and severe injury (OR=1.332, 95% CI: 0.677–2.620, P=0.406) (Figure 3).
We also observed no significant differences in secondary outcomes (Figure 4), including in-hospital mortality (OR=0.985, 95% CI: 0.727–1.334, P=0.922), pulmonary infection (OR=0.481, 95% CI: 0.202–1.146, P=0.091), wound infection (OR=0.752, 95% CI: 0.447–1.267, P=0.283), urinary tract infection (OR=1.243, 95% CI: 0.968–1.597, P=0.088), myocardial infarction (OR=0.987, 95% CI: 0.525–1.856, P=0.967), AKI (OR=0.902, 95% CI: 0.629–1.294, P=0.576), and DVT (OR=1.062, 95% CI: 0.779–1.447, P=0.706). The survival time on the basis of RBC storage duration is presented in Figure 5.
UNIVARIATE AND MULTIVARIATE REGRESSION ANALYSES OF 90-DAY MORTALITY IN ITBI PATIENTS:
We investigated the death-related factors of iTBI patients utilizing univariate and multivariate regression analyses, as shown in Table 3. There were significant statistical differences regarding age (OR=1.020, 95% CI: 1.008–1.033, P=0.001), weight (OR=0.983, 95% CI: 0.969–0.997, P=0.020), hypertension history (OR=2.031, 95% CI: 1.377–2.997, P<0.001), LOS in hospital (OR=1.197, 95% CI: 1.163–1.233, P<0.001), subarachnoid hemorrhage (OR=0.286, 95% CI: 0.156–0.524, P<0.001), intraventricular hemorrhage (OR=2.053, 95% CI: 1.037–4.063, P=0.039), and traffic injury (OR=0.563, 95% CI: 0.330–0.959, P=0.035). No differences were discovered in sex, fresh RBCs transfusion, diabetes history, GCS score on admission, head and neck AIS, ISS score, LOS in ICU, duration of mechanical ventilation, epidural hematoma, intracerebral hemorrhage, brain contusion, diffuse axonal injury, falling over injury, and falling from a height injury between the 2 groups (all P>0.05).
The findings of the multivariate analysis showed obvious differences in age (OR=1.026, 95% CI: 1.006–1.045,
Discussion
TBI is a critical public health problem worldwide, with profound and persistent impacts on the individual, society, and economy globally. In clinical treatment, blood transfusion is often used for anemic patients with TBI [30]. However, the effects of RBCs storage duration in TBI patients have been unclear. In the present study, we assessed differences in outcomes in adult iTBI patients who received RBC transfusion with different storage durations. Our results showed that there were no significant differences in 90-day mortality among patients who received fresh or old RBCs transfusion. We also found that the secondary outcomes, including in-hospital mortality, nosocomial infection, and complications, were similar in the 2 groups, which has important implications for intensive care and transfusion therapies.
Multiple studies have produced conflicting results on the effects of RBC storage duration in trauma patients. A previous study reported that the transfusion of RBCs stored for more than 2 weeks can increase the mortality of trauma patients, and that RBCs storage duration for transfusion may be an independent predictor of mortality, despite universal leukoreduction [31]. Weinberg et al. retrospectively assessed trauma patients who received ≥1 unit of exclusively old (≥14 days)
At present, it is not possible to infer that the alterations of biochemistry, physiology, and structure in RBCs stored for approximately more than 14 days do not harm patients with iTBI. In our study, compared with old RBCs, transfusing fresh RBCs did not improve the primary or secondary outcomes in iTBI patients. However, our results differ from previous observational studies that suggested transfusion with fresh RBC produces better clinical outcomes for patients [24,34]. Interpretation of these findings may be complicated by the potential confounders, such as differently defined storage durations, inclusion or exclusion criteria, research designs, and subjects.
The revised RBC transfusion guidelines proposed by the American Association of Blood Banks (AABB) recommend that patients should receive RBCs selected at any point within the licensed dating period (standard issue) rather than limiting transfusion to fresh RBCs [35]. This is consistent with our study results, and we do not support the selective use of fresh RBCs. Our research provides strong evidence that fresh RBC transfusion has no clinical benefits in comparison with old RBC transfusion among adult iTBI patients, which supports the current international practice of transfusion using older RBCs.
Conclusions
In this study, we assessed differences in outcomes in adult iTBI patients who received RBCs transfusions with different storage durations. The results revealed no differences in the primary and secondary outcomes among iTBI patients transfused the fresh or old RBCs, which indicates the use of old RBCs did not increase the 90-day mortality rate in adult iTBI patients.
Figures
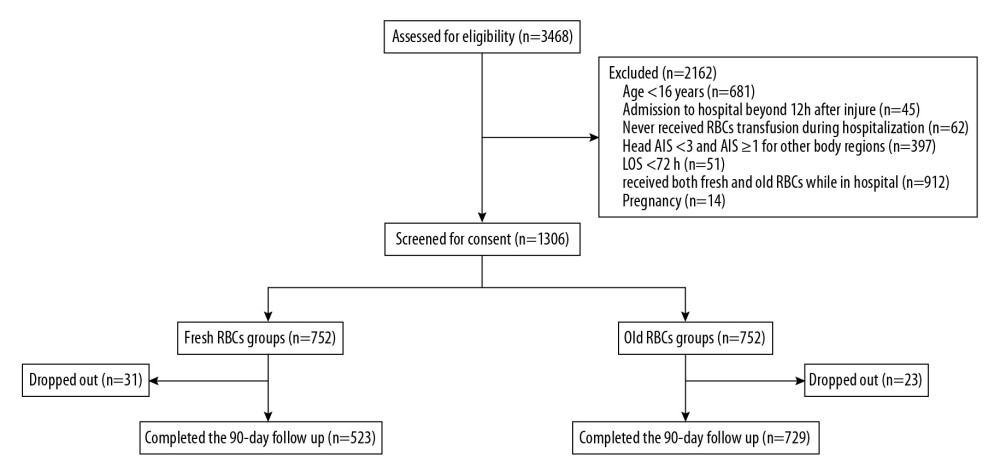 Figure 1. Flow chart of the study.
Figure 1. Flow chart of the study. 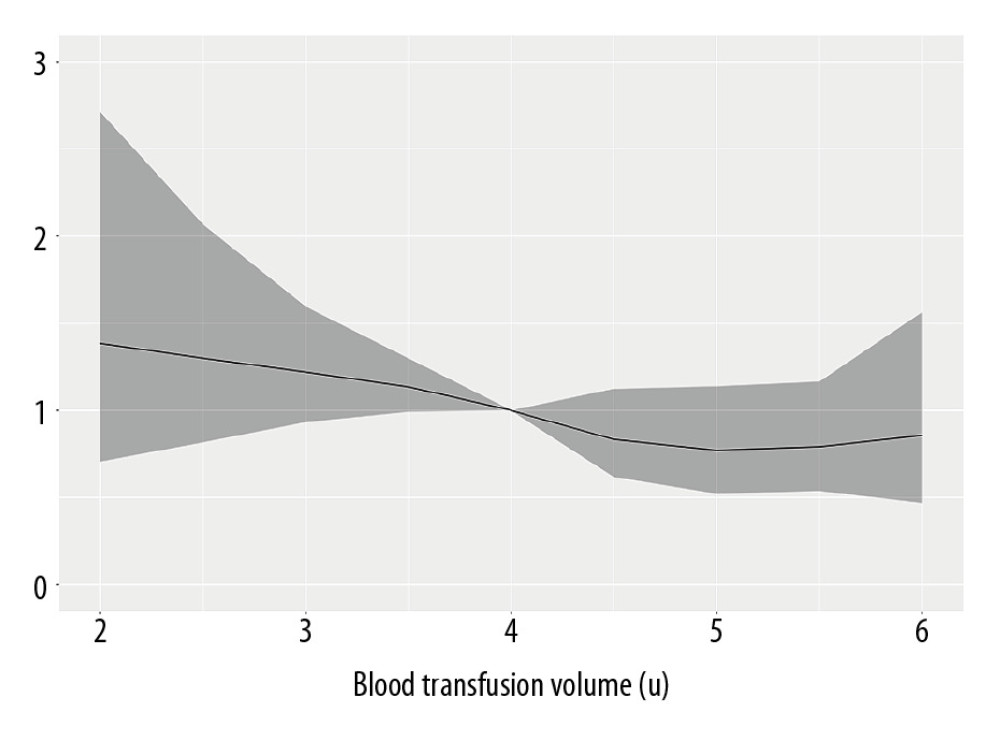 Figure 2. The dose-response relationship curve of blood transfusion volumes of iTBI patients.
Figure 2. The dose-response relationship curve of blood transfusion volumes of iTBI patients. 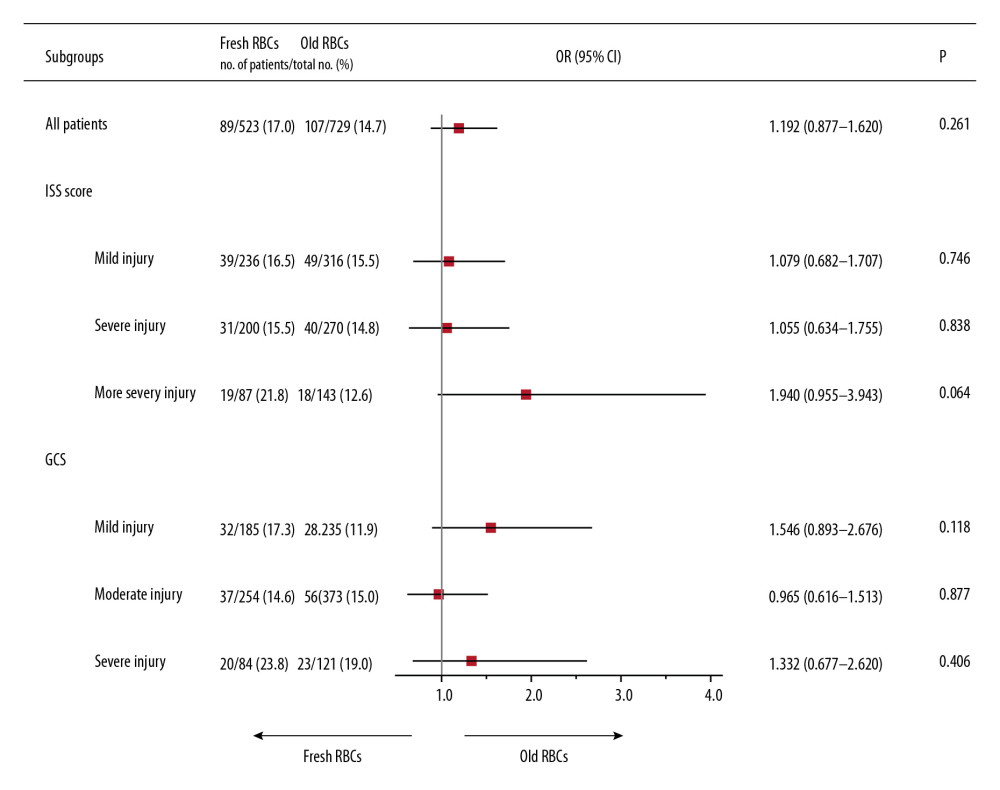 Figure 3. Forest plot of absolute risk differences in primary outcomes.
Figure 3. Forest plot of absolute risk differences in primary outcomes. 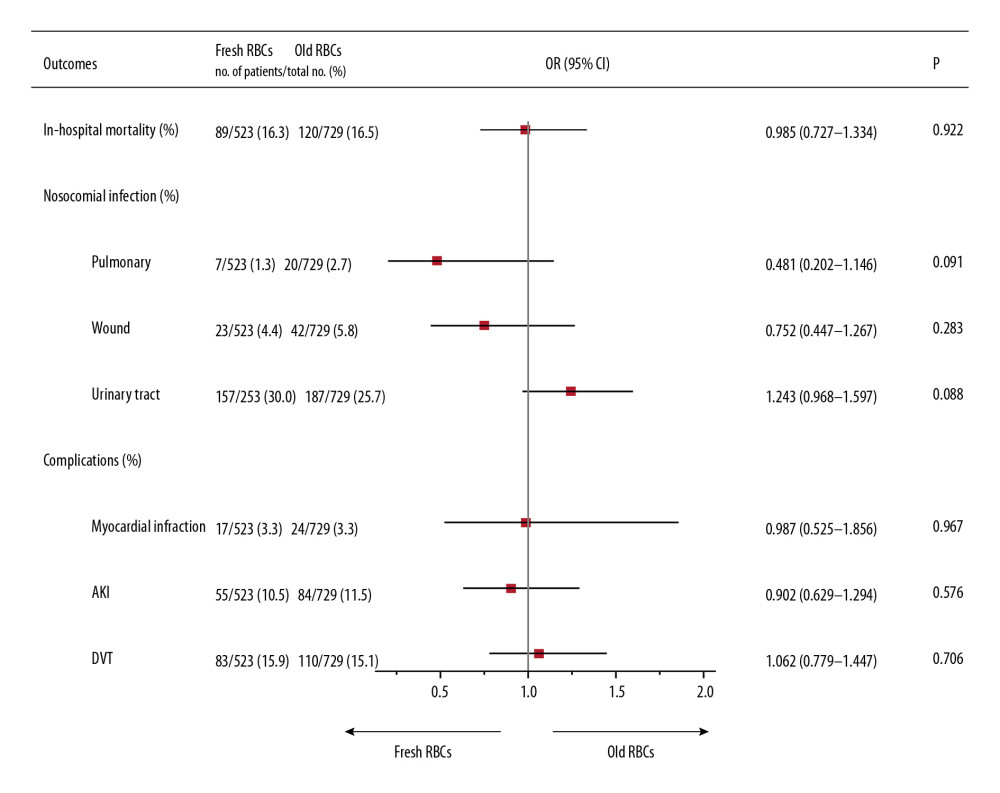 Figure 4. Forest plot of absolute risk differences in secondary outcomes.
Figure 4. Forest plot of absolute risk differences in secondary outcomes. 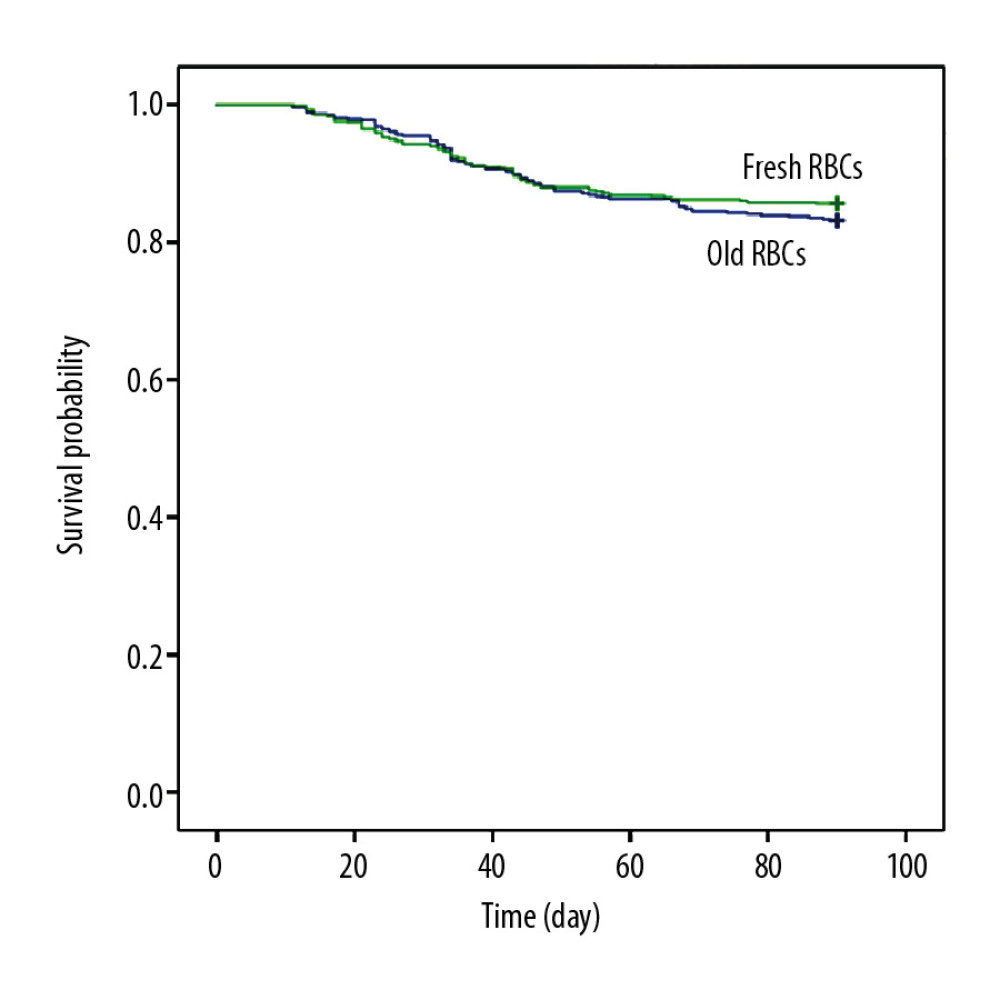 Figure 5. Kaplan-Meier survival analysis of time to death in iTBI patients.
Figure 5. Kaplan-Meier survival analysis of time to death in iTBI patients. References
1. Rincon F, Hunter K, Schorr C, The epidemiology of spontaneous fever and hypothermia on admission of brain injury patients to Intensive Care Units: A multicenter cohort study: J Neurosurg, 2014; 121(4); 950-60
2. Kay T, Harrington DE, Adams R, Definition of mild traumatic brain injury: J Head Trauma Rehab, 1993; 8; 86-87
3. Hyder AA, Wunderlich CA, Puvanachandra P, The impact of traumatic brain injuries: A global perspective: Neurorehabilitation, 2007; 22(5); 341-53
4. Taylor CA, Bell JM, Breiding MJ, Xu L, Traumatic brain injury-related emergency department visits, hospitalizations, and deaths-United States, 2007 and 2013: MMWR Surveillance Summaries, 2017; 66(9); 1-18
5. Roozenbeek B, Maas AI, Menon DK, Changing patterns in the epidemiology of traumatic brain injury: Nat Rev Neurol, 2013; 9(4); 231-36
6. Cooper DJ, McQuilten ZK, Nichol A, Age of red cells for transfusion and outcomes in critically Ill adults: N Engl J Med, 2017; 377(19); 1858-67
7. Heddle NM, Cook RJ, Arnold DM: N Engl J Med, 2016; 375(20); 1937-45
8. Dhar R, Scalfani MT, Zazulia AR, Comparison of induced hypertension, fluid bolus, and blood transfusion to augment cerebral oxygen delivery after subarachnoid hemorrhage clinical article: J Neurosurg, 2012; 116(3); 648-56
9. Salim A, Hadjizacharia P, DuBose J, Role of anemia in traumatic brain injury: J Am Coll Surgeons, 2008; 207(3); 398-406
10. Kellert L, Schrader F, Ringleb P, The impact of low hemoglobin levels and transfusion on critical care patients with severe ischemic stroke: STroke: RelevAnt Impact of HemoGlobin, Hematocrit and Transfusion (STRAIGHT) – an observational study: J Crit Care, 2014; 29(2); 236-40
11. Kuramatsu JB, Gerner ST, Lücking H, Anemia is an independent prognostic factor in intracerebral hemorrhage: An observational cohort study: Crit Care, 2013; 17(4); R148
12. Kramer AH, Zygun DA, Anemia and red blood cell transfusion in neurocritical care: Crit Care, 2009; 13(3); R89
13. Desjardins P, Turgeon AF, Tremblay MH, Hemoglobin levels and transfusions in neurocritically ill patients: A systematic review of comparative studies: Crit Care, 2012; 16(2); R54
14. Borgström L, Jóhannsson H, Siesjö BK, The influence of acute normovolemic anemia on cerebral blood flow and oxygen consumption of anesthetized rats: Acta Physiol, 2010; 93(4); 505-14
15. LeRoux P, Haemoglobin management in acute brain injury: Curr Opin Crit Care, 2013; 19(2); 83-91
16. Oddo M, Milby A, Chen I, Hemoglobin concentration and cerebral metabolism in patients with aneurysmal subarachnoid hemorrhage: Stroke, 2009; 40(4); 1275-81
17. Utter GH, Shahlaie K, Zwienenberg-Lee M, Muizelaar JP, Anemia in the setting of traumatic brain injury: The arguments for and against liberal transfusion: J Neurotraum, 2011; 28; 155-65
18. Elterman J, Brasel K, Brown S, Transfusion of red blood cells in patients with a prehospital Glasgow Coma Scale score of 8 or less and no evidence of shock is associated with worse outcomes: J Trauma Acute Care, 2013; 75(1); 8-14
19. Menon DK, Zahed C, Prediction of outcome in severe traumatic brain injury: Curr Opin Crit Care, 2009; 15(5); 437-41
20. Murphy GJ, Pike K, Rogers CA, Liberal or restrictive transfusion after cardiac surgery: N Engl J Med, 2015; 372(11); 997-1008
21. Carson JL, Terrin ML, Noveck H, Liberal or restrictive transfusion in high-risk patients after hip surgery: N Engl J Med, 2011; 365(26); 2453-62
22. Hajjar LA, Vincent JL, Galas F, Transfusion requirements after cardiac surgery the TRACS randomized controlled trial: JAMA, 2010; 304(14); 1559-67
23. van de Watering L, Red cell storage and prognosis: Vox Sang, 2011; 100(1); 36-45
24. Weinberg JA, McGwin G, Marques MB, Transfusions in the less severely injured: Does age of transfused blood affect outcomes?: J Trauma Acute Care, 2008; 65(4); 794-98
25. Yamal JM, Benoit JS, Doshi P, Association of transfusion red blood cell storage age and blood oxygenation, long-term neurologic outcome, and mortality in traumatic brain injury: J Trauma Acute Care, 2015; 79(5); 843-49
26. George ME, Skarda DE, Watts CR, Aggressive red blood cell transfusion: No association with improved outcomes for victims of isolated traumatic brain injury: Neurocrit Care, 2008; 8(3); 337-43
27. Koch CG, Li L, Sessler DI, Duration of red-cell storage and complications after cardiac surgery: N Engl J Med, 2008; 358(12); 1229-39
28. Weinberg JA, McGwin G, Vandromme MJ, Duration of red cell storage influences mortality after trauma: J Trauma, 2010; 69(6); 1427-30
29. Bishnoi AK, Garg P, Patel K, Effect of red blood cell storage duration on outcome after paediatric cardiac surgery: A prospective observational study: Heart Lung Circ, 2019; 28(5); 784-91
30. Kramer AH, Le Roux P, Red blood cell transfusion and transfusion alternatives in traumatic brain injury: Curr Treat Option, 2012; 14(2); 150-63
31. Weinberg JA, McGwin G, Griffin RL, Age of transfused blood: An independent predictor of mortality despite universal leukoreduction: J Trauma, 2008; 65(2); 279-82 discussion 282–84
32. Epstein DS, Mitra B, Cameron PA, Acute traumatic coagulopathy in the setting of isolated traumatic brain injury: Definition, incidence and outcomes: Brit J Neurosurg, 2015; 29(1); 118-22
33. Ruel-Laliberte J, Bonaventure PL, Fergusson D, Effect of age of transfused red blood cells on neurologic outcome following traumatic brain injury (ABLE-tbi Study): A nested study of the Age of Blood Evaluation (ABLE) trial: Can J Anesth, 2019; 66(6); 696-705
34. Spinella PC, Carroll CL, Staff I, Duration of red blood cell storage is associated with increased incidence of deep vein thrombosis and in hospital mortality in patients with traumatic injuries: Crit Care, 2009; 13(5); R151
35. Carson JL, Guyatt G, Heddle NM, Clinical practice guidelines from the AABB: Red blood cell transfusion thresholds and storage: JAMA, 2016; 316(19); 2025
Figures
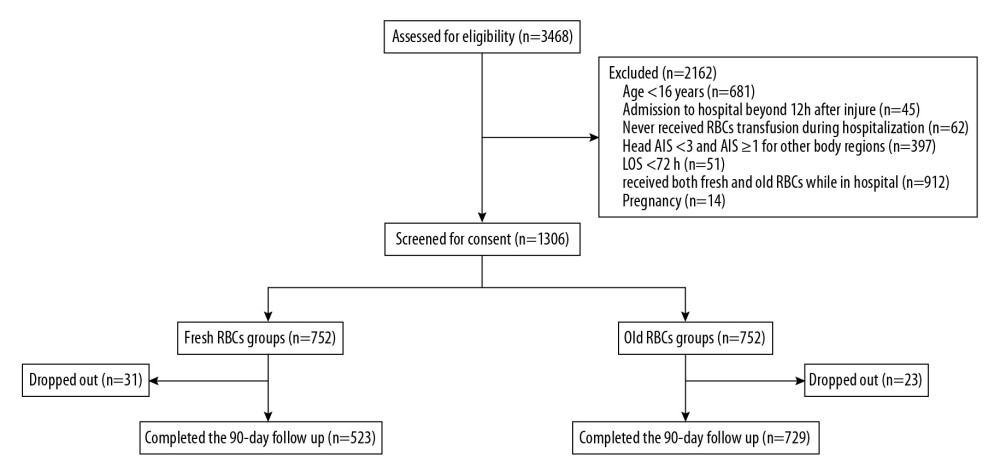 Figure 1. Flow chart of the study.
Figure 1. Flow chart of the study.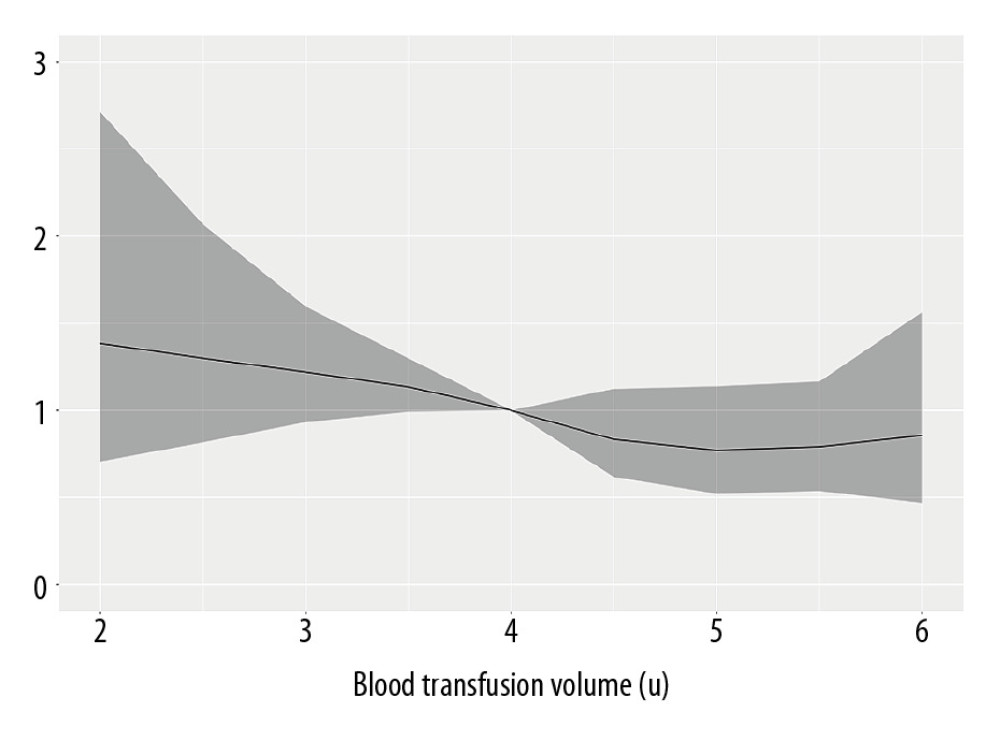 Figure 2. The dose-response relationship curve of blood transfusion volumes of iTBI patients.
Figure 2. The dose-response relationship curve of blood transfusion volumes of iTBI patients.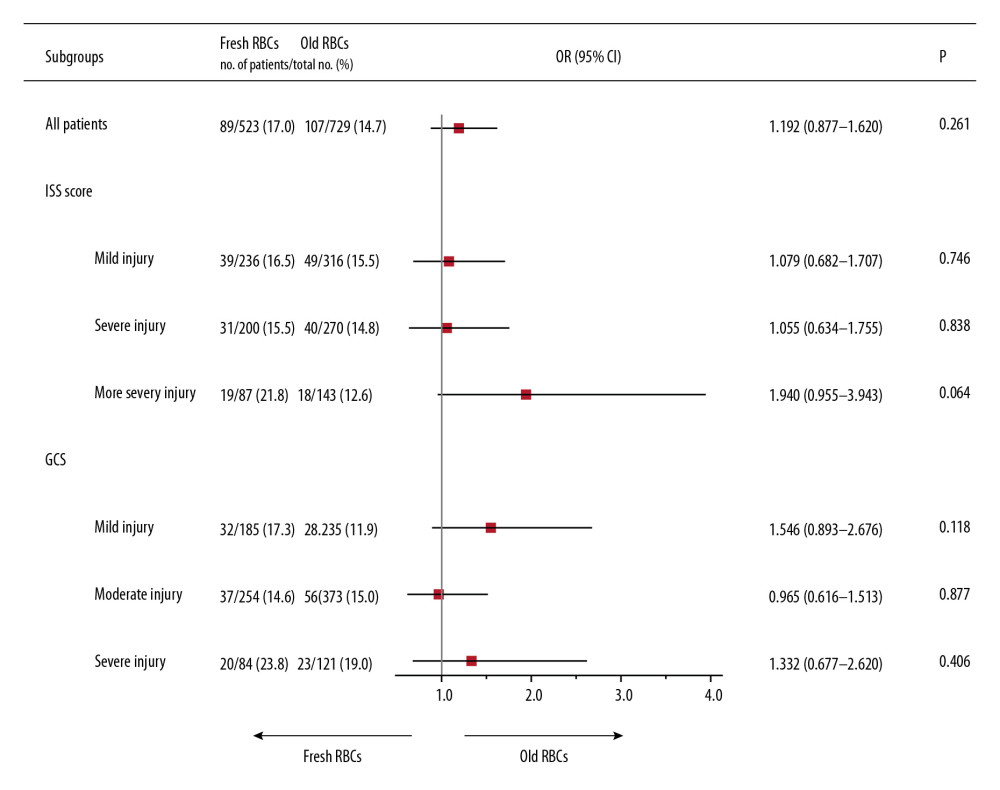 Figure 3. Forest plot of absolute risk differences in primary outcomes.
Figure 3. Forest plot of absolute risk differences in primary outcomes.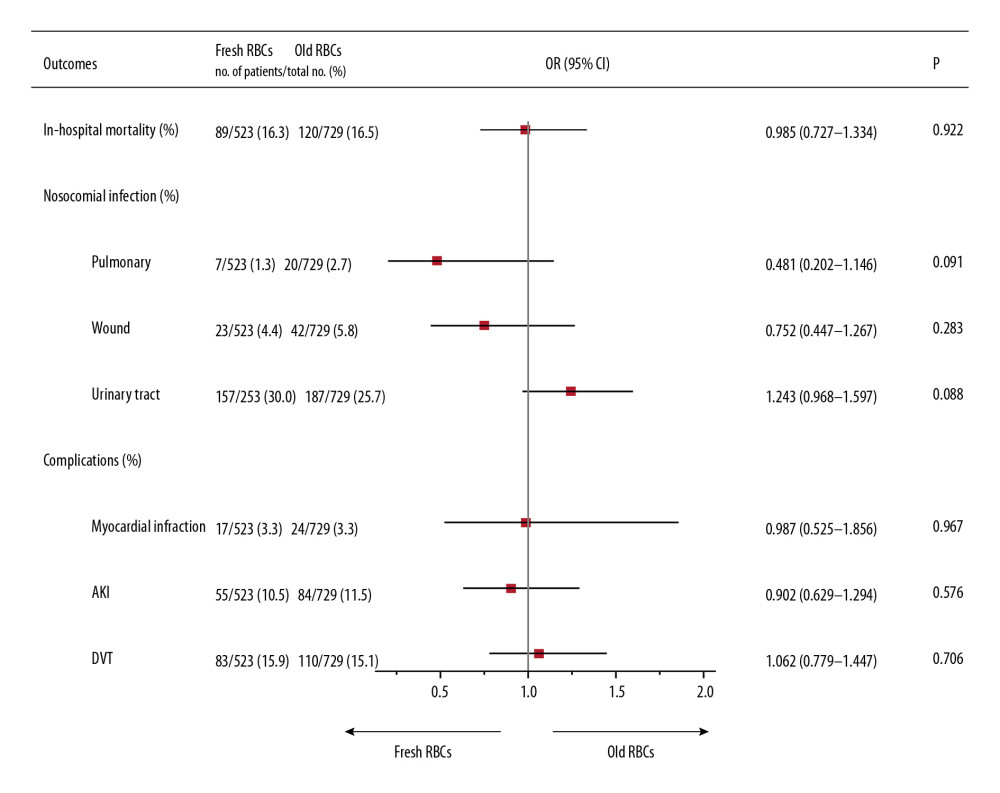 Figure 4. Forest plot of absolute risk differences in secondary outcomes.
Figure 4. Forest plot of absolute risk differences in secondary outcomes.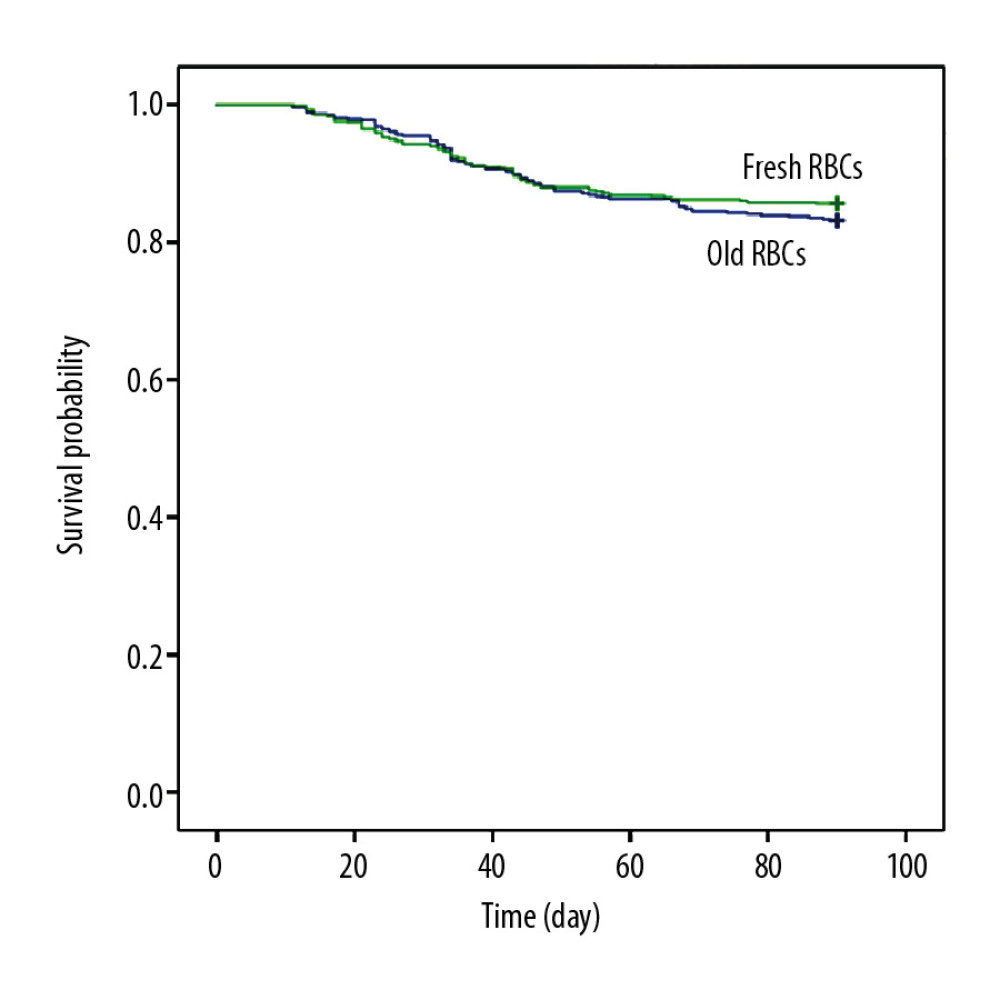 Figure 5. Kaplan-Meier survival analysis of time to death in iTBI patients.
Figure 5. Kaplan-Meier survival analysis of time to death in iTBI patients. Tables
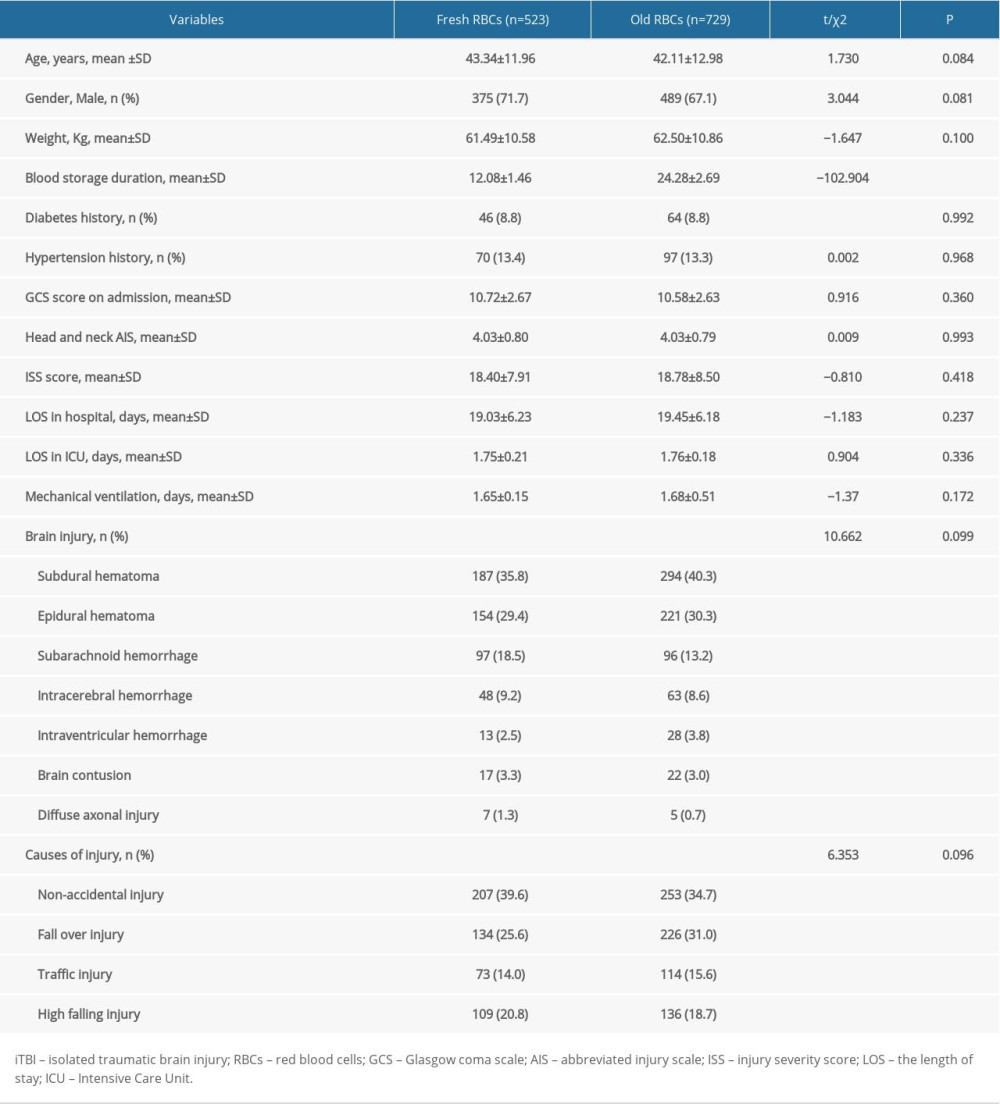 Table 1. Characteristics of the iTBI patients.
Table 1. Characteristics of the iTBI patients.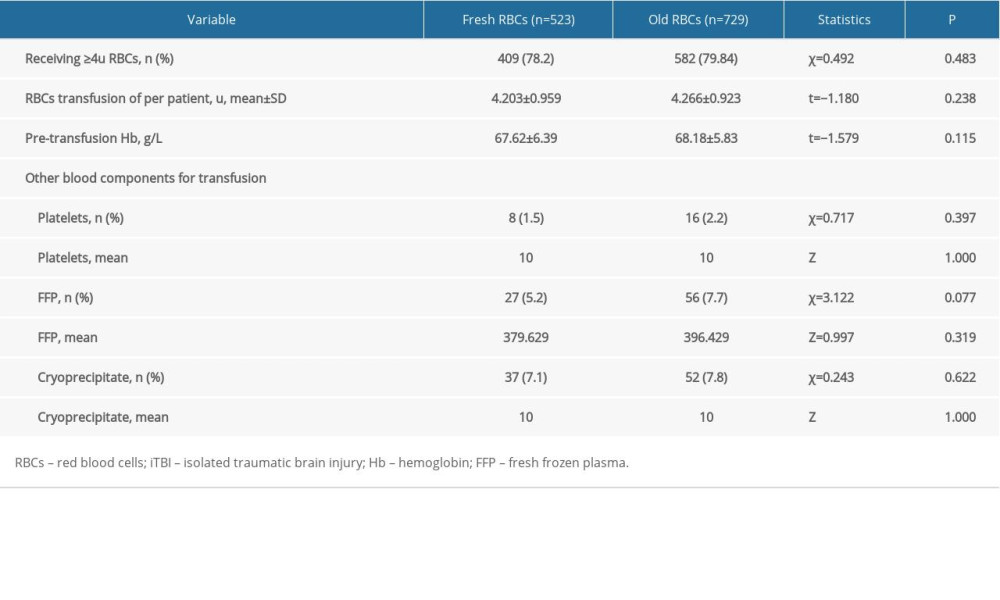 Table 2. RBCs transfusion for iTBI patients.
Table 2. RBCs transfusion for iTBI patients.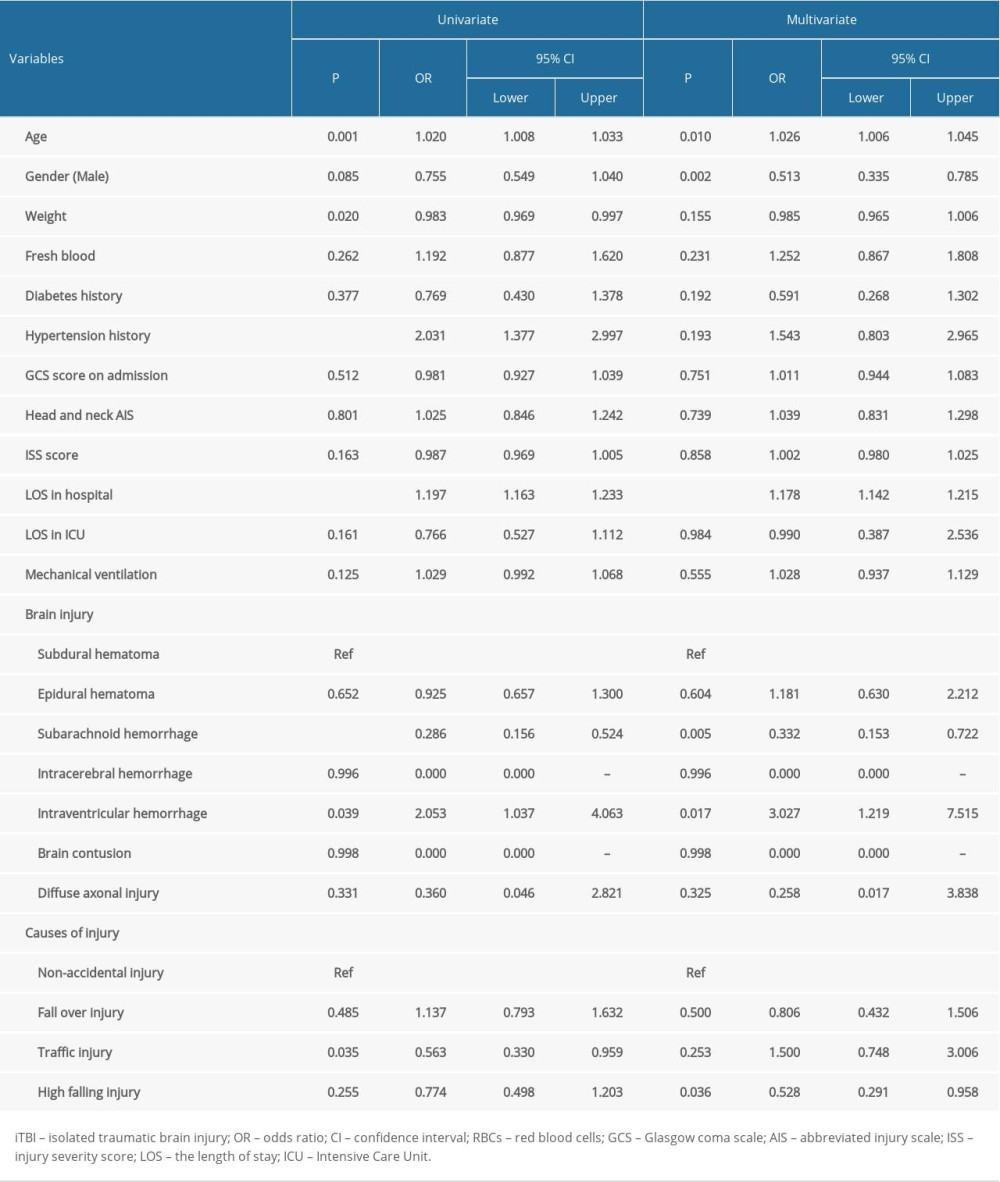 Table 3. Univariate regression analysis of 90-day mortality in patients with iTBI.
Table 3. Univariate regression analysis of 90-day mortality in patients with iTBI.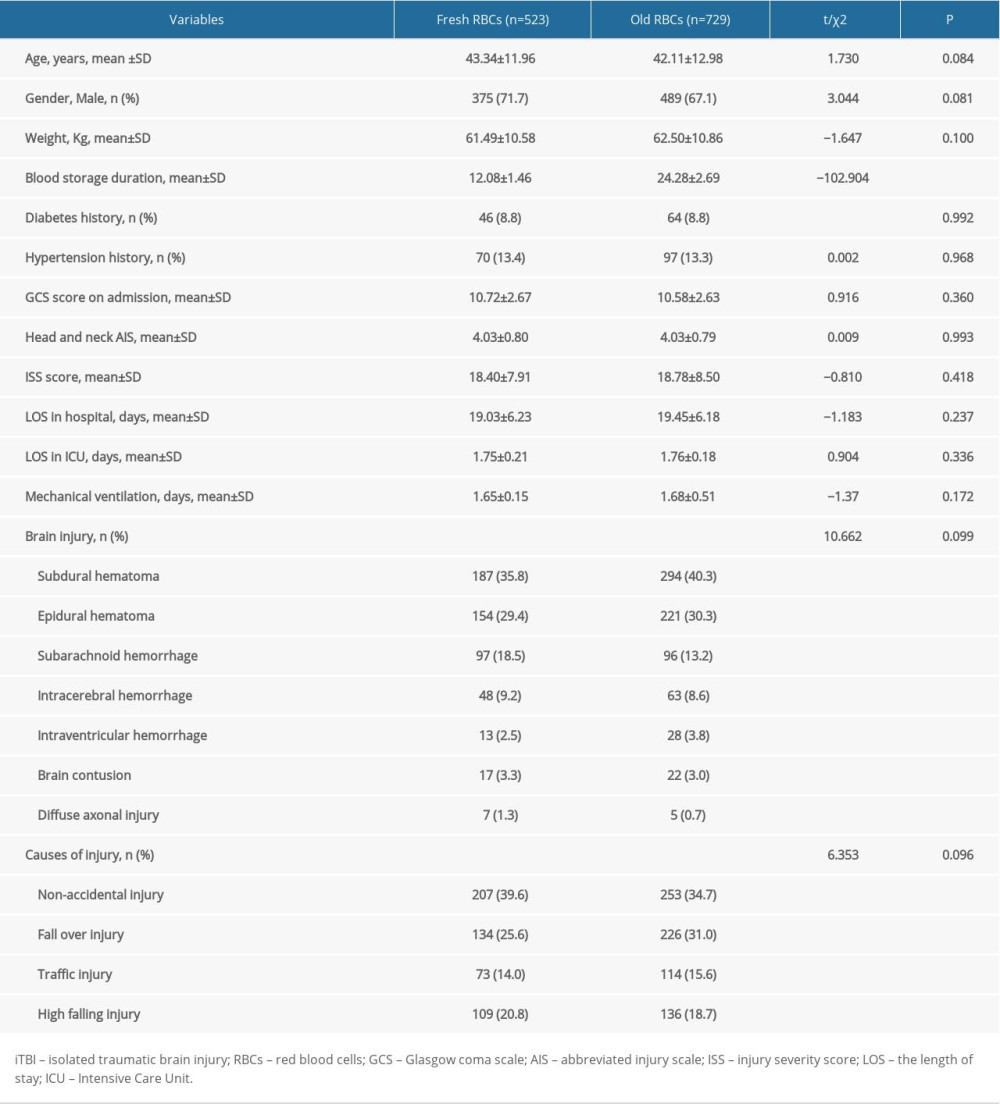 Table 1. Characteristics of the iTBI patients.
Table 1. Characteristics of the iTBI patients.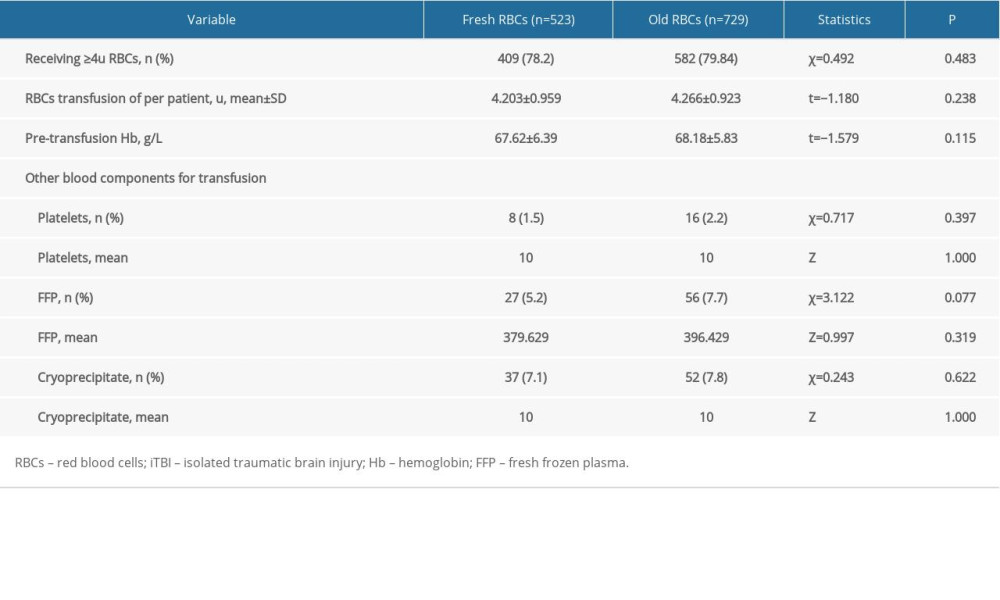 Table 2. RBCs transfusion for iTBI patients.
Table 2. RBCs transfusion for iTBI patients.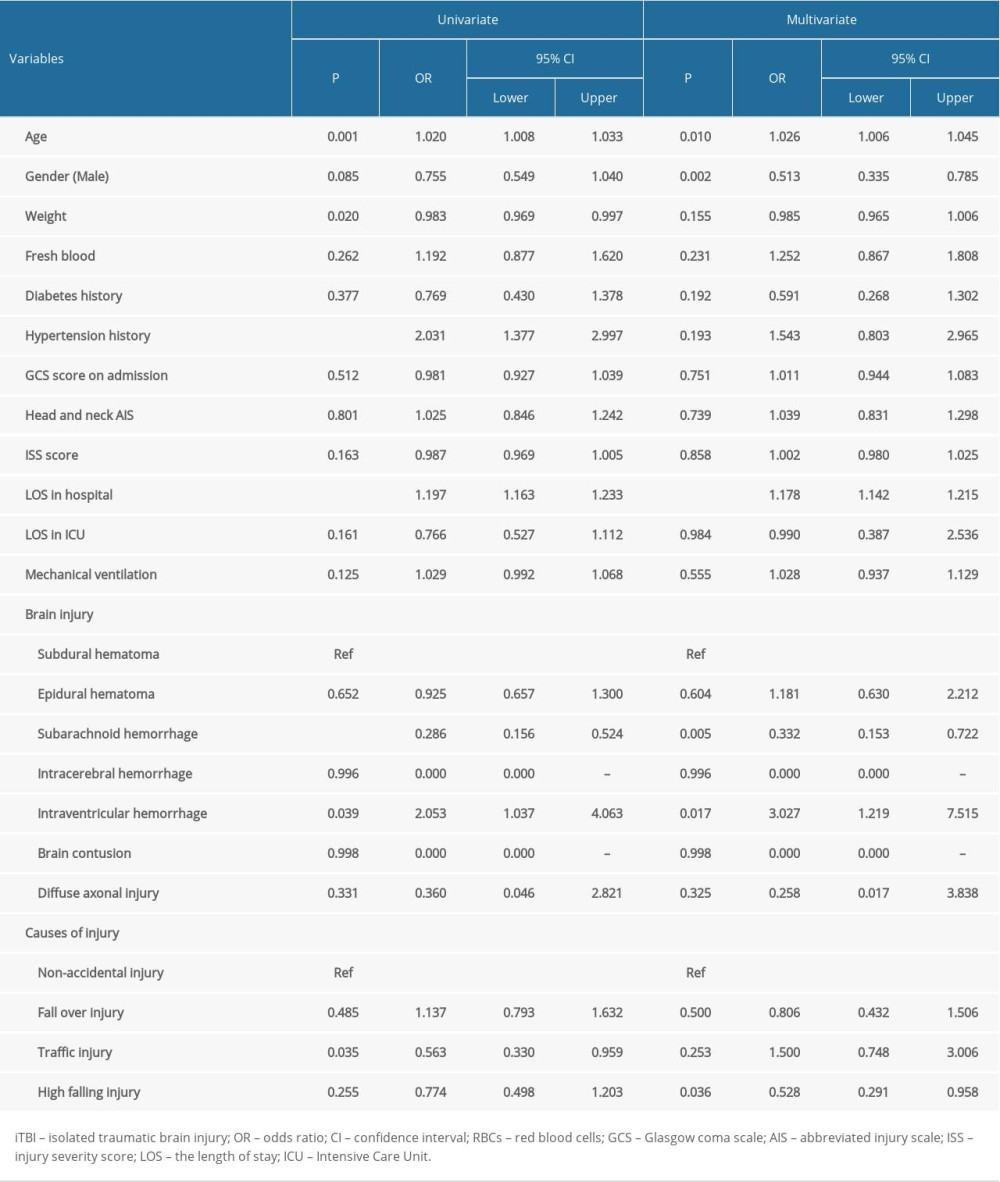 Table 3. Univariate regression analysis of 90-day mortality in patients with iTBI.
Table 3. Univariate regression analysis of 90-day mortality in patients with iTBI. In Press
05 Mar 2024 : Clinical Research
Role of Critical Shoulder Angle in Degenerative Type Rotator Cuff Tears: A Turkish Cohort StudyMed Sci Monit In Press; DOI: 10.12659/MSM.943703
06 Mar 2024 : Clinical Research
Comparison of Outcomes between Single-Level and Double-Level Corpectomy in Thoracolumbar Reconstruction: A ...Med Sci Monit In Press; DOI: 10.12659/MSM.943797
21 Mar 2024 : Meta-Analysis
Economic Evaluation of COVID-19 Screening Tests and Surveillance Strategies in Low-Income, Middle-Income, a...Med Sci Monit In Press; DOI: 10.12659/MSM.943863
10 Apr 2024 : Clinical Research
Predicting Acute Cardiovascular Complications in COVID-19: Insights from a Specialized Cardiac Referral Dep...Med Sci Monit In Press; DOI: 10.12659/MSM.942612
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








