29 April 2022: Clinical Research
Evaluation of a Precision Approach to Intraoperative Ropivacaine Nerve Block to Improve Postoperative Analgesia in 120 Patients Undergoing Thyroid Surgery
Yong Wang1B, Jiankang Shen1BCFG, Rongli Xie1AE, Dan Tan1E, Xiaoli Jin1BCD, Liang Shen2BCD*, Jianmin Yuan1ABCDEFDOI: 10.12659/MSM.935563
Med Sci Monit 2022; 28:e935563
Abstract
BACKGROUND: This study aimed to compare a precision approach to intraoperative nerve block with traditional analgesia to reduce postoperative pain in 120 patients during thyroid surgery. The precision intraoperative technique used 0.3% ropivacaine to block the lower branch of the transverse cervical nerve and the inner branches of the supraclavicular nerve.
MATERIAL AND METHODS: A total of 120 patients were prospectively enrolled in this study. All patients were randomly and evenly divided into 3 groups. In the precision group, 0.3% ropivacaine was used through the wound during surgery. In the traditional group, a superficial cervical plexus nerve block was performed before surgery. Saline was injected in the control group. The valuation of postoperative pain was assessed using the visual analogue scale (VAS).
RESULTS: Two hours after surgery, the VAS scores in the precision group, traditional group, and control group were 1.4±0.5, 1.6±0.7, and 2.8±1.0 (P<0.001), respectively. Then, the pain improvement was more significant after 6 h, as the VAS scores in the precision, traditional, and control groups were 1.0±0.5, 1.2±0.6, and 2.6±1.1 (P<0.001), respectively. Twenty-four hours after surgery, the VAS scores in the precision, traditional, and control groups were 0.7±0.3, 0.6±0.4, and 1.9±1.1 (P<0.001), respectively.
CONCLUSIONS: At a single center, the use of a precision intraoperative ropivacaine nerve block significantly reduced postoperative pain when compared with traditional analgesia for patients undergoing thyroid surgery.
Keywords: Analgesia, Nerve Block, Thyroid Cancer, Papillary, Amides, Anesthetics, Local, Humans, Pain, Postoperative, ropivacaine, Thyroid Gland
Background
Thyroid cancer is the most frequently occurring endocrine cancer in China and has the fastest increase in incidence [1,2]. At present, surgery is the essential method of curing thyroid cancer, especially papillary thyroid carcinoma, which is the most common pathological type [3,4]. The pain caused by surgical trauma is one of the main discomforts of patients after thyroid cancer. Since perioperative pain management is one of the core items of the rapid surgical rehabilitation (ERAS) protocol; effective pain management can alleviate the complication and improve the prognosis of patients with thyroid cancer [5]. Therefore, this study aimed to compare a precision approach to intraoperative nerve block with traditional analgesia to reduce postoperative pain in 120 patients during thyroid surgery. The precision intraoperative technique used 0.3% ropivacaine to block the lower branch of the transverse cervical nerve and the inner branches of the supraclavicular nerve.
Material and Methods
ETHICS STATEMENT:
All procedures were implemented based on the principles of the Declaration of Helsinki, and the design of the work was reviewed and approved by the ethics committee of our hospital. All patients agreed to participate in this study and provided their written informed consent.
PATIENTS:
A total of 120 patients were prospectively enrolled in this study. All patients underwent thyroid surgery from January 2020 to March 2021 in Ruijin Hospital Lu Wan Branch, Shanghai Jiaotong University School of Medicine. The sample size was calculated as follows: n=2*[(α+β)σ/δ]2, α=1.645, and β=1.282, with a result of n=38.55. In view of the possibility of a certain loss of samples, we defined the sample size as n=40 per group.
STUDY DESIGN:
The main inclusion criterion for the study was patients who underwent thyroidectomy for benign and malignant thyroid disease. Patients were excluded if any of the following were present: age younger than 18 years or older than 80 years; patient underwent lateral lymph node dissection; patient underwent multiple thyroid surgeries; patient had a history of neck and cervical nerve surgery; patient had a history of mental illness; and patient had visual or hearing impairments and communication difficulties. The collected clinic-pathological characteristics of enrolled patients included age, sex, operation time, pathological diagnosis, scope of operation, and VAS score.
PRECISION ANESTHESIA:
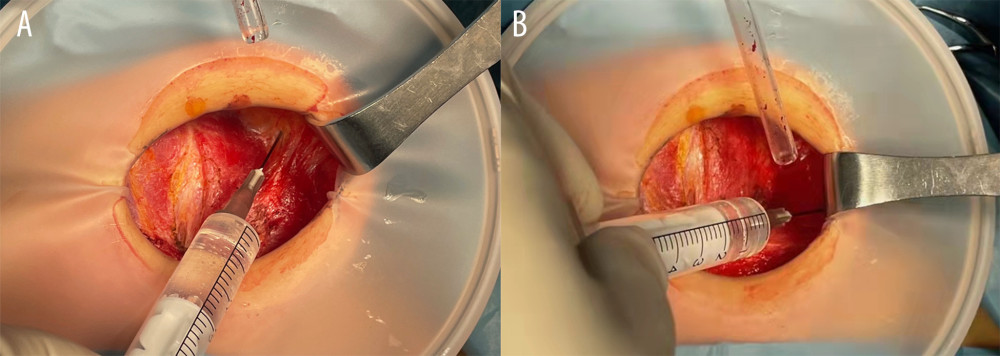
All patients were randomly divided into 3 groups (simple randomization): a precision group (intraoperative precision nerve block through the wound), traditional group (percutaneous superficial cervical plexus block), and control group, with 40 patients per group. This was a double-blind clinical study and was conducted by independent surgical and pain assessment groups. In the precision group, 0.3% ropivacaine (1.5 mL for each nerve) was used through the wound during surgery. At the deep level of the platysma muscle, the ropivacaine firstly was injected upward along the front edge of the sternocleidomastoid muscle to block the lower branch of the transverse cervical nerve, and then was injected along the anterolateral direction of the sternocleidomastoid muscle to block the inner branches of the supraclavicular nerve (Figure 1). In the traditional group, the superficial cervical plexus nerve block (15 mL ropivacaine for each nerve) was performed before surgery. The VAS score was collected at 2, 6, and 24 h after the surgery was completed.
STATISTICAL ANALYSIS:
Normally distributed continuous data are presented as mean±standard deviation. Non-normally distributed data are presented as median (25th percentile to 75th percentile). Categorical data are presented as n (%). Measurement data were compared with
Results
PATIENT CHARACTERISTICS:
We enrolled 120 patients who were pathologically diagnosed with thyroid tumors during the study period. The detailed clinic-pathological characteristics of all patients are listed in Table 1. There were no statistically significant differences in age, sex, operation time, pathological diagnosis, and surgical scope between the 3 groups. The VAS score in all 3 groups was measured at 3 time points. Two hours after surgery, the VAS scores in the precision group, traditional group, and control group were 1.4±0.5, 1.6±0.7, and 2.8±1.0, respectively. The pain improvement was more significant after 6 h, as the VAS scores in the precision group, traditional group, and control group were 1.0±0.5, 1.2±0.6, and 2.6±1.1, respectively. Twenty-four hours after surgery, the VAS scores in the precision group, traditional group, and control group were 0.7±0.3, 0.6±0.4, and 1.9±1.1, respectively. Thus, intraoperative precision nerve block through the wound had the best anesthetic effect for thyroid surgery.
STRATIFIED ANALYSIS OF VAS:
The above results confirmed that this method of intraoperative precision nerve block was effective. Therefore, we conducted further stratified analysis of the VAS scores (Table 2). There were significant differences in VAS scores between men and women in the 3 groups at 2 h after surgery (P=0.001, P<0.001, respectively). However, there was no significant difference in VAS scores between men and women in the precision group (P=0.717). Then, the influence of tumor properties on pain was further analyzed, and we found the VAS scores of the 3 groups of benign and malignant tumors were significantly different at 2 h after surgery (P=0.017, P<0.001, respectively). Similar results were obtained at 6 and 24 h after surgery (P=0.012, P<0.001, P=0.010, P<0.001, respectively). The scope of surgery should have had a significant impact on pain. Hence, we analyzed the data and found that intraoperative precision nerve block through the wound had a significant analgesic effect on unilateral and bilateral thyroidectomy at the 3 experimental time points (P<0.001, P<0.001, P<0.001, P<0.001, P<0.001, P<0.001, respectively).
ASSOCIATED COMPLICATIONS:
There were no unplanned second surgeries or severe surgical complications in all 3 groups, including hoarseness caused by recurrent laryngeal nerve injury, water choking caused by superior laryngeal nerve injury, and hematoma caused by postoperative wound bleeding. There were 3 cases (7.5%), 5 cases (12.5%), and 4 cases (10.0%) of transient hypoparathyroidism (postoperative blood calcium <2.2 mmol/L) in the 3 groups, with no significant difference (
Discussion
In this study, we compared a precision approach to intraoperative nerve block with traditional analgesia to reduce postoperative pain in 120 patients during thyroid surgery. The results demonstrated that, at a single center, the use of a precision intraoperative ropivacaine nerve block significantly reduced postoperative pain when compared with traditional analgesia for patients undergoing thyroid surgery.
Nerve block anesthesia is also called conduction anesthesia, which is a method of injecting anesthetics next to the nerve trunk to temporarily block the nerve conduction function and achieve the effect of local anesthesia [6,7]. Nerve block anesthesia has a great advantage in surgery due to its small dose, slight adverse effects, and long working time; also, the patient is awake and can maintain communication with the surgeon during surgery. Thus, in the early stage of surgical development, cervical plexus anesthesia was widely used in thyroid surgery, because through patient’s communication, recurrent laryngeal nerve injury can be avoided during the surgery. However, it also has many disadvantages, such as an unstable effect, recurrent laryngeal nerve block, and phrenic nerve palsy [8]. Therefore, with the development of anesthesia and surgical techniques, general anesthesia has gradually replaced cervical plexus anesthesia and is widely used in thyroid surgery. However, in recent years, with the widespread application of the ERAS guidelines in surgery, as well as the emphasis on perioperative pain management and the concept of multimodal analgesia, nerve block has once again received the attention of anesthesiologists and surgeons [9].
The cervical plexus is composed of the C1 to C4 spinal nerves, which come out of the intervertebral foramen, pass through the back of vertebral artery to the tip of transverse process, then branch and form a series of rings to construct the cervical nerve plexus [10–12]. In addition, the anatomy of the inferior branch of transverse cervical nerve along with the medial branch of supraclavicular nerve are mainly responsible for skin sensation in the area of thyroid surgeries. It has been reported that the anesthesia effect is satisfied through blocking the supraclavicular nerve in clavicle surgeries while patients are awake [13]. However, due to the specific thin and scattered structure of the inferior branch of the transverse cervical nerve as well as the medial branch of supraclavicular nerve, traditional percutaneous injection in the superficial cervical plexus block is difficult to locate and is mostly dependent on a larger dose of tissue dispersion to achieve an anesthetic effect in practice. However, it has been reported that satisfactory effects can be accomplished when the superficial cervical plexus block is applied in thyroid surgeries for intraoperative and postoperative analgesia [14]. In this study, proper analgesic effects were also achieved in the control group using the superficial cervical plexus block.
Traditional superficial cervical plexus anesthesia generally performs by injecting local anesthetics around sensory branches of C2 to C4, which are marked by either the fourth cervical vertebrae transverse process or the intersection of the external jugular vein and the posterior edge of sternocleidomastoid muscle. Because of the massive number of cervical vessels and nerves, there are possible risks of a series of complications when performing traditional cervical plexus block, such as toxic reactions caused by local anesthetics mistakenly entering vessels, recurrent laryngeal nerve block, phrenic nerve block, vagus nerve block, vertebral artery injuries, and even total spinal anesthesia when local anesthetics are injected into the epidural space or subarachnoid space.
In the control group patients who underwent traditional superficial cervical plexus block, 1 case of vagus nerve block and 1 case of superficial vascular injury occurred. Although it led to no negative clinical consequences, fluctuation ranges of the heart rate and the blood pressure in the patient with vagus nerve block were comparatively wider, which might create a certain risk. Meanwhile, the skin appearance was affected in the patient with superficial vascular damage, resulting in increased nervousness.
With the development of technology, an increasing number of anesthesiologists use visual imaging techniques such as ultrasound to achieve a precise anesthesia effect [15,16]. During thyroid surgery, the separation level of the cervical skin flap is the loose connective tissue of the deep surface of the platysma muscle, which is also the level where the transverse cervical nerve and the supraclavicular nerve are located in. Therefore, that can be operated on directly and have more accurate stereo positioning. Hence, at the deep level of the platysma muscle, we first injected the ropivacaine upward along the front edge of the sternocleidomastoid muscle to block the lower branch of the transverse cervical nerve and then injected it along the anterolateral direction of the sternocleidomastoid muscle to block the inner branches of the supraclavicular nerve.
In the present study, precise nerve block was achieved through the layers opened by the thyroid surgical wound. Its analgesic effect is equivalent to that of traditional superficial cervical plexus anesthesia, with a lower drug dose and few complications, which is in line with the concept of precision treatment. As mentioned above, intraoperative precision nerve block through the wound has a better anesthetic effect for thyroid surgery, and the VAS scores in the precision group were lower than the scores of the other groups in all time points except 24 h, which we assumed was due to its small dose and metabolism that proceeded faster. Clinically, the pain and discomfort after a patient’s surgery is often related to factors such as age, sex, and surgical trauma range. Due to the epidemiology of thyroid tumors and the particularity of the surgery, the age difference between the patients in this study was not large, with only 3 patients over 50 years old. Also, the operation time is greatly affected by the waiting time of freezing pathology during surgery, and the difference in blood loss is very small. Therefore, a stratified analysis was carried out according to sex, pathological type, and scope of surgery. The results of the stratified analysis showed that the precision group and traditional group showed the advantages of preventing postoperative pain. The VAS scores of the men in the control group were higher than the scores of the women at 2 h after surgery, which reflects that different sexes have a different tolerance to pain. The precision group and the traditional group did not show significant differences in the VAS scores at 2 h after surgery by sex or different surgical ranges, which also reflects the good analgesic effect of this method.
There are still some limitations in our study. First, the number of enrolled patients was not large enough at only 120. Second, this was a single-center analysis, and there might have been some selection bias. Third, many factors can also affect a patient’s pain perception, and patient educational level and family status were not analyzed in this study.
Conclusions
In this study, intraoperative injection of ropivacaine through the wound accurately blocked the “target nerve” and effectively reduced postoperative pain. This was shown to be an effective clinical method and provides new ideas for multi-modal analgesia for thyroid surgery.
Tables
Table 1. The effect of precision intraoperative ropivacaine nerve block on postoperative pain. The collected clinic-pathological characteristics of enrolled patients were as follows: age, sex, operation time, pathological diagnosis, and scope of operation, and visual analogue scale (VAS) score.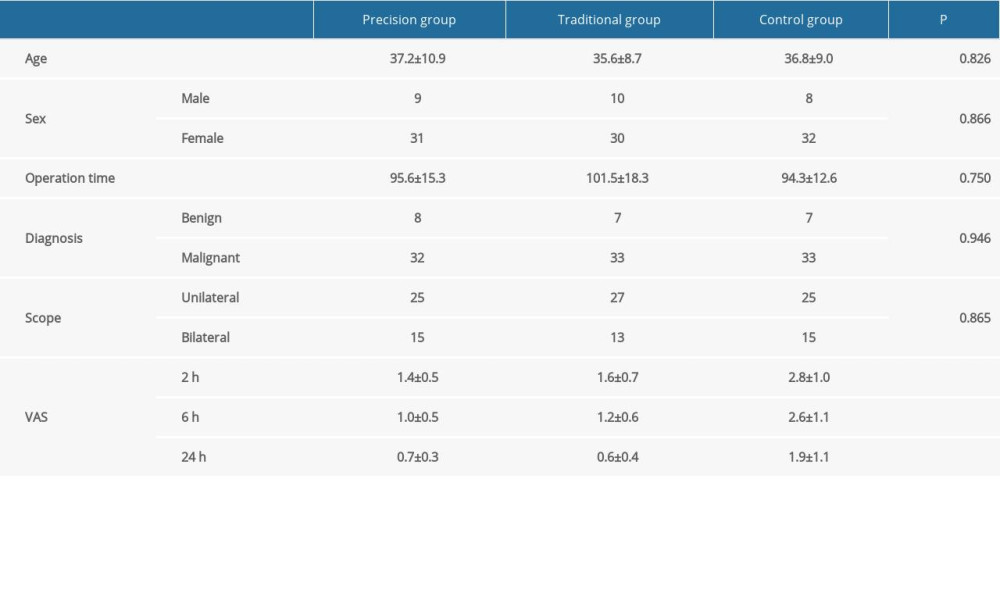 Table 2. The effect of precision intraoperative ropivacaine nerve block on visual analogue scale (VAS) scores. The VAS was performed at 2 h, 6 h, and 24 h after surgery was completed. Visual Analogue Score (VAS).
Table 2. The effect of precision intraoperative ropivacaine nerve block on visual analogue scale (VAS) scores. The VAS was performed at 2 h, 6 h, and 24 h after surgery was completed. Visual Analogue Score (VAS).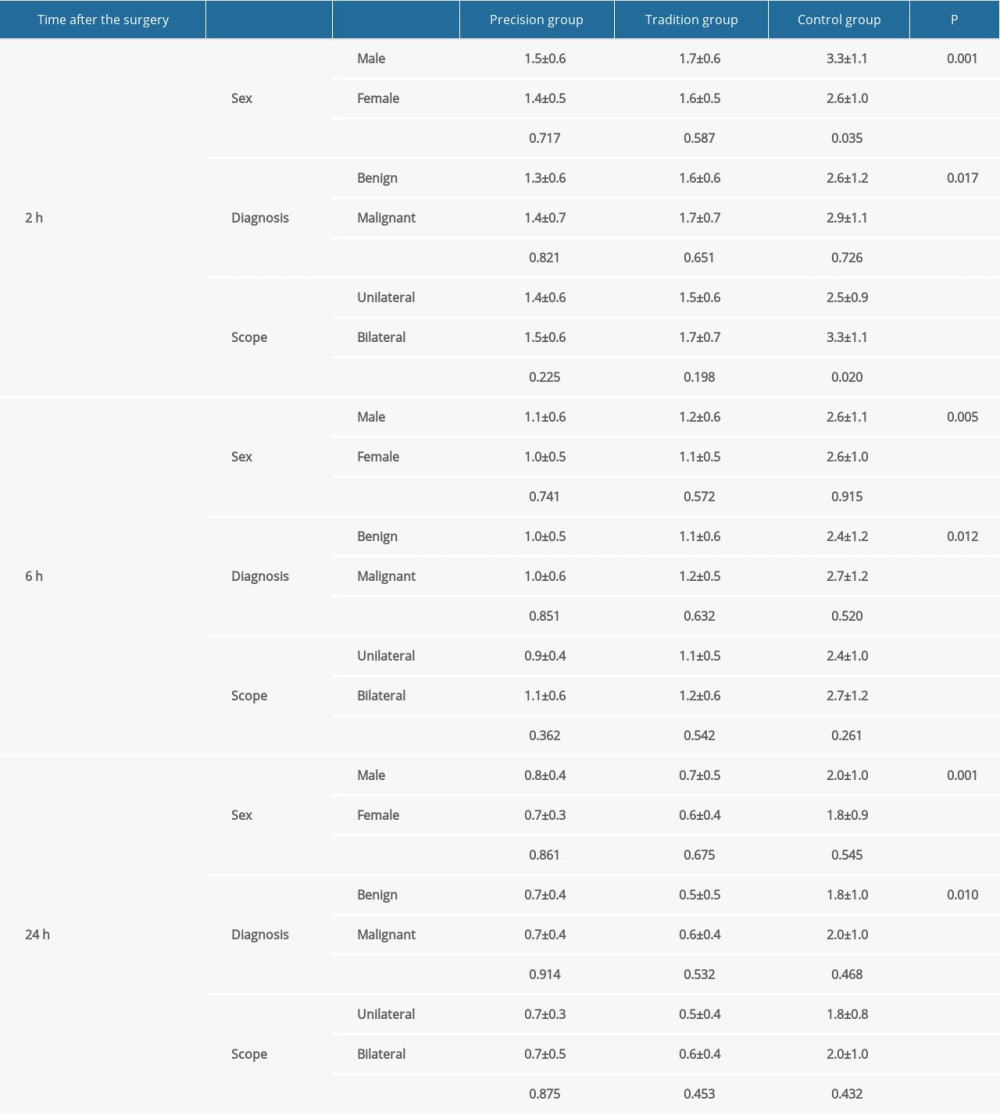
References
1. Dong Y, Wang D, Luo Y, Comprehensive evaluation of risk factors for lymph node metastasis in patients with papillary thyroid carcinoma: Oncol Lett, 2021; 21(3); 188
2. Zhao Y, Wang Y, Zhang X, Papillary thyroid carcinoma in patients with acromegaly from a single center in China: World Neurosurg, 2021; 149; e22-e28
3. Bible KC, Kebebew E, Brierley J, 2021 American Thyroid Association guidelines for management of patients with anaplastic thyroid cancer: Thyroid, 2021; 31(3); 337-86
4. Deng Y, Li H, Wang M, Global burden of thyroid cancer from 1990 to 2017: JAMA Netw Open, 2020; 3(6); e208759
5. Brindle M, Nelson G, Lobo DN: Bjs Open, 2019; 4(1); 157-63
6. Re M, Blanco J, deSegura IAG, Ultrasound-guided nerve block anesthesia: Vet Clin North Am Food Animal Pract, 2016; 32(1); 133-47
7. Liao YC, Wu WC, Hsieh MH, Ultrasound-guided superior laryngeal nerve block assists in anesthesia for bronchoscopic surgical procedure: Medicine, 2020; 99(27); e20916
8. Okmen K, Efficacy of different doses of superficial cervical plexus block on pain after thyroid surgery: J Clin Anal Medicine, 2017; 8(6); JCAM.5241
9. Chen Q, Jiang JH, Yang B, Modified thoracoabdominal sensory nerves block through subcostal exterior semilunaris approach (SE-TAP) provide broader analgesia for abdominal surgery: J Clin Anesth, 2021; 68; 110077
10. Martinez-Pereira MA: Surgical anatomy of the cervical plexus and its branches; 71-79 Published online 2022
11. Ciftci B, Develi T, Münevveroglu S, Ekinci M, Superficial cervical plexus block for orthognathic surgery: Rev Esp Anestesiol Reanim (Engl Ed), 2021; 68(7); 428-29
12. Marcuzzo AV, Šuran-Brunelli AN, Cin ED, Surgical anatomy of the marginal mandibular nerve: A systematic review and meta-analysis: Clin Anat, 2020; 33(5); 739-50
13. Sanllorente-Sebastián R, Wilk P, Garcés-Pérez GM, Awake clavicle surgery with PECS1 and ultrasound selective supraclavicular nerve block combination: J Clin Anesth, 2020; 66; 109937
14. Woldegerima YB, Hailekiros AG, Fitiwi GL, The analgesic efficacy of bilateral superficial cervical plexus block for thyroid surgery under general anesthesia: A prospective cohort study: BMC Res Notes, 2020; 13(1); 42
15. Adler AC, Siddiqui A, Chandrakantan A, Matava CT, Lung and airway ultrasound in pediatric anesthesia: Pediatr Anesth, 2022; 32(2); 202-8
16. Tucker RV, Peterson WJ, Mink JT, Defining an ultrasound-guided regional anesthesia curriculum for emergency medicine: AEM Educ Train, 2021; 5(3); e10557
Tables
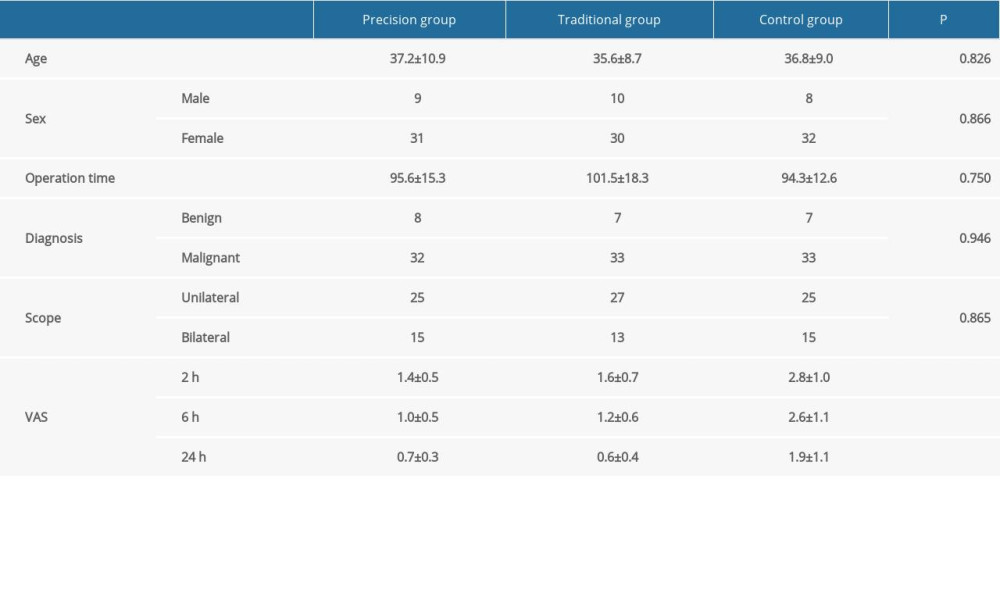 Table 1. The effect of precision intraoperative ropivacaine nerve block on postoperative pain. The collected clinic-pathological characteristics of enrolled patients were as follows: age, sex, operation time, pathological diagnosis, and scope of operation, and visual analogue scale (VAS) score.
Table 1. The effect of precision intraoperative ropivacaine nerve block on postoperative pain. The collected clinic-pathological characteristics of enrolled patients were as follows: age, sex, operation time, pathological diagnosis, and scope of operation, and visual analogue scale (VAS) score.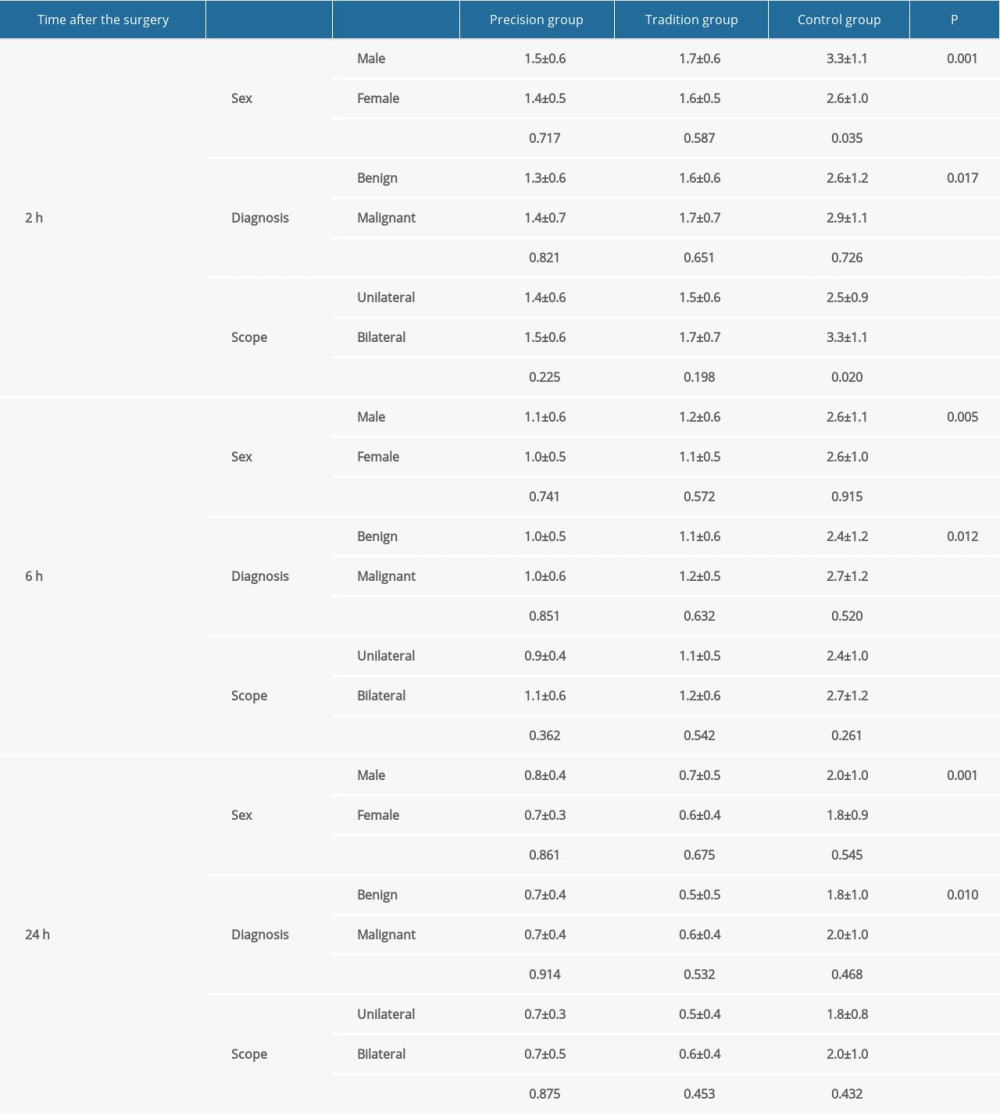 Table 2. The effect of precision intraoperative ropivacaine nerve block on visual analogue scale (VAS) scores. The VAS was performed at 2 h, 6 h, and 24 h after surgery was completed. Visual Analogue Score (VAS).
Table 2. The effect of precision intraoperative ropivacaine nerve block on visual analogue scale (VAS) scores. The VAS was performed at 2 h, 6 h, and 24 h after surgery was completed. Visual Analogue Score (VAS).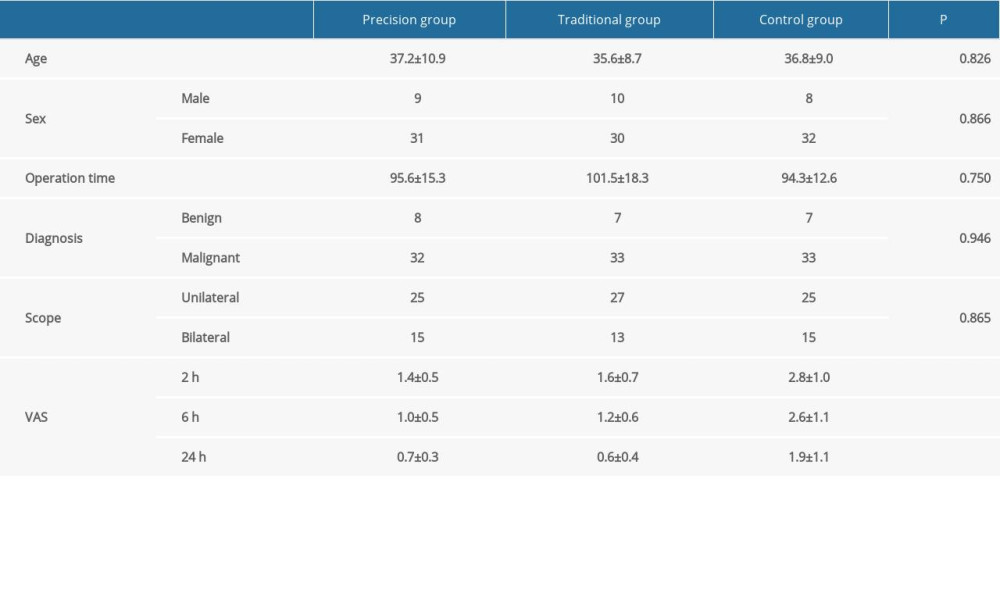 Table 1. The effect of precision intraoperative ropivacaine nerve block on postoperative pain. The collected clinic-pathological characteristics of enrolled patients were as follows: age, sex, operation time, pathological diagnosis, and scope of operation, and visual analogue scale (VAS) score.
Table 1. The effect of precision intraoperative ropivacaine nerve block on postoperative pain. The collected clinic-pathological characteristics of enrolled patients were as follows: age, sex, operation time, pathological diagnosis, and scope of operation, and visual analogue scale (VAS) score.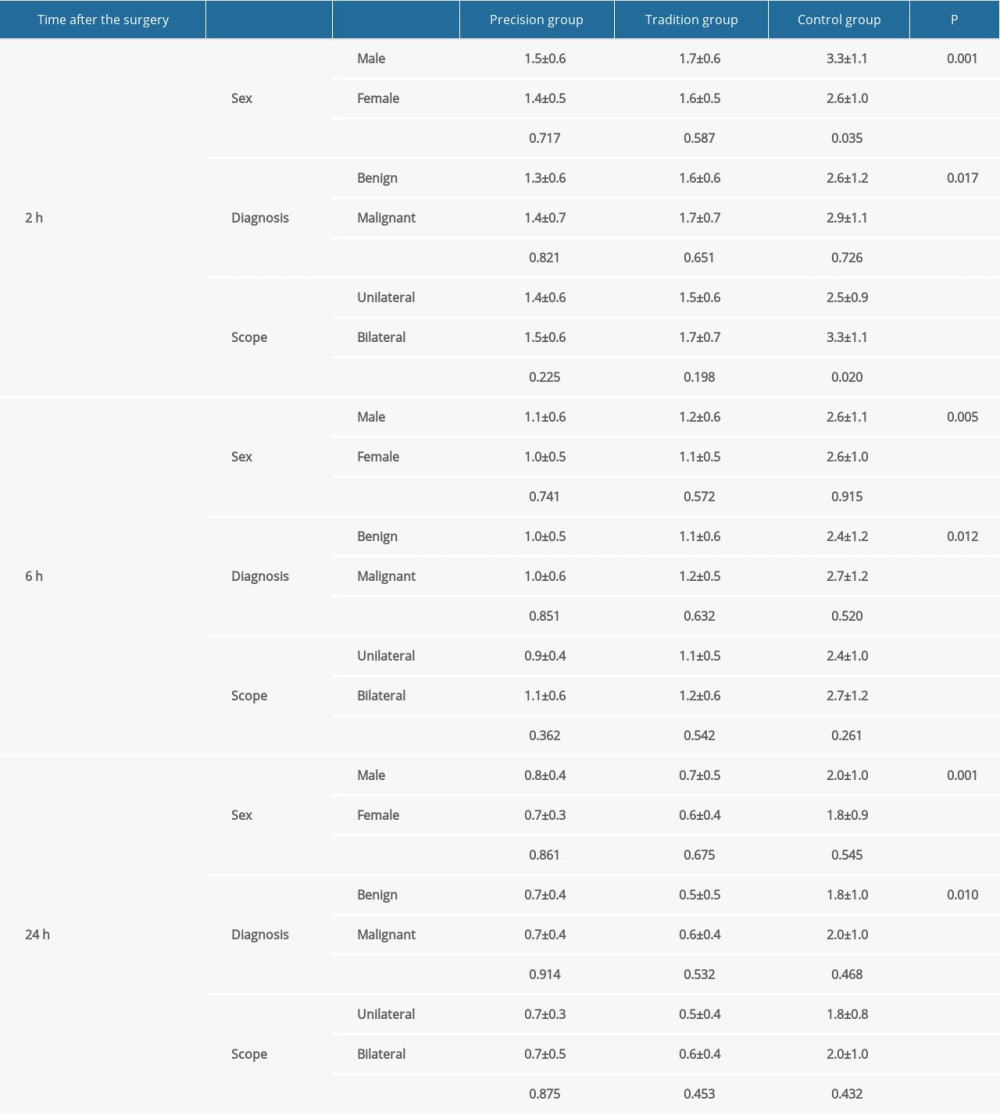 Table 2. The effect of precision intraoperative ropivacaine nerve block on visual analogue scale (VAS) scores. The VAS was performed at 2 h, 6 h, and 24 h after surgery was completed. Visual Analogue Score (VAS).
Table 2. The effect of precision intraoperative ropivacaine nerve block on visual analogue scale (VAS) scores. The VAS was performed at 2 h, 6 h, and 24 h after surgery was completed. Visual Analogue Score (VAS). In Press
06 Mar 2024 : Clinical Research
Comparison of Outcomes between Single-Level and Double-Level Corpectomy in Thoracolumbar Reconstruction: A ...Med Sci Monit In Press; DOI: 10.12659/MSM.943797
21 Mar 2024 : Meta-Analysis
Economic Evaluation of COVID-19 Screening Tests and Surveillance Strategies in Low-Income, Middle-Income, a...Med Sci Monit In Press; DOI: 10.12659/MSM.943863
10 Apr 2024 : Clinical Research
Predicting Acute Cardiovascular Complications in COVID-19: Insights from a Specialized Cardiac Referral Dep...Med Sci Monit In Press; DOI: 10.12659/MSM.942612
06 Mar 2024 : Clinical Research
Enhanced Surgical Outcomes of Popliteal Cyst Excision: A Retrospective Study Comparing Arthroscopic Debride...Med Sci Monit In Press; DOI: 10.12659/MSM.941102
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952