22 April 2022: Clinical Research
Closed Reduction Percutaneous Intramedullary Fixation with Kirschner Wires in 4 Children with Displaced Fractures of the Distal Humerus
Rufa Wang1BCDE, Pengfei Zheng1BCDE, Yinming Wang1BCDE, Zhipeng Gao1BD, Mengqiu Xu1BD, Minjie Fan1CD, Yiwei Wang1CD, Khristinn Kellie Leitch2ABCDEF*, Gang Lin3ABCDEFDOI: 10.12659/MSM.935448
Med Sci Monit 2022; 28:e935448
Abstract
BACKGROUND: This study describes the use of closed reduction percutaneous intramedullary fixation with Kirschner wires in 4 children with displaced metaphyseal-diaphyseal junction (MDJ) fractures of the distal humerus.
MATERIAL AND METHODS: Between August 2016 and August 2019, 4 patients (3 boys and 1 girl), whose mean age was 4 years 5 months (range: 3 years 6 months to 5 years 4 months), with displaced MDJ fractures of the distal humerus were treated using closed reduction percutaneous intramedullary fixation with Kirschner wires. Three of the fractures were oblique and 1 was transverse. The operation time and the frequency of intraoperative fluoroscopy were recorded. All children were followed up for greater than 18 months, taking anteroposterior and lateral radiographs of the elbow joint to evaluate the outcomes. At the last follow-up, the Flynn elbow joint function score was used to evaluate clinical outcomes, and complications were recorded.
RESULTS: The mean operation time was 37.5 min (range: 35-40 min) and the frequency of intraoperative fluoroscopy was 11.7 times (range: 8-15 times). All of the fractures were confirmed to be healed based on radiographic results at 4 weeks after surgery. At the last follow-up, 4 children had normal elbow joint motion without elbow deformity. The Flynn score showed their outcomes were excellent.
CONCLUSIONS: Closed reduction percutaneous intramedullary fixation using Kirschner wires was an effective treatment for displaced MDJ fractures of the distal humerus in the 4 children described and was shown to be easy to perform with a short operation time.
Keywords: Bone Wires, Fracture Fixation, Intramedullary, humeral fractures, Humerus, Pediatrics, Child, Diaphyses, Elbow Joint, Female, Fracture Fixation, Internal, Humans, Infant, Male
Background
Supracondylar humerus fractures are the most common elbow fractures in children, but it is important to distinguish them from the rare metaphyseal-diaphyseal junction (MDJ) fracture of the distal humerus [1–3]. As first defined by Fayssoux, MDJ fractures of the distal humerus are located higher than the common supracondylar humerus fracture [1]. On the anteroposterior radiograph of the distal humerus, a horizontal line is drawn at the point where the transverse anteroposterior width of the humerus starts to increase, and the top of olecranon fossa and the fracture between these 2 lines is defined as MDJ fracture of the distal humerus. Fayssoux found that of 422 supracondylar humerus fractures, only 14 (3.3%) were MDJ fractures of the distal humerus [1], and Sen identified only 6 (3.1%) MDJ fractures from 182 supracondylar humerus fractures [3].
The MDJ fractures of the distal humerus were similar to but not exactly the same as the supracondylar fracture of the humerus. It tends to appear completely displaced and unstable on radiographs, making fracture reduction, maintenance of reduction, and fixation difficult [1]. Currently, the most commonly used treatment of supracondylar fracture of the humerus is closed reduction with Kirschner wire fixation. In treating MDJ fractures of the distal humerus, the Kirschner wire needs to pass through the proximal bone cortex of the fracture at an angle close to parallel to the humeral shaft, which was hard to achieve [1–3]. The insertion point of an elastic intramedullary nail should be selected at the metaphysis, while the MDJ fracture was already close to the metaphysis. The distal end of the fracture had very little space to insert the nail. Repeated attempts at inserting will lead to epiphyseal injury, even iatrogenic growth plate injury, and may also affect the stability of fracture fixation [4]. A few scholars suggested using open reduction and fixation with a Kirschner wire combined with a plate [4]. However, these methods are associated with many postoperative complications, making the treatment of these fractures extremely challenging. Therefore, we created a new method named “closed reduction percutaneous intramedullary fixation with Kirschner wires”. We use the Kirschner wires as an elastic intramedullary nail, inserted through the cortex but not the contralateral cortex. This study describes the use of closed reduction percutaneous intramedullary fixation with Kirschner wires in 4 children with displaced MDJ fractures of the distal humerus.
Material and Methods
PATIENTS:
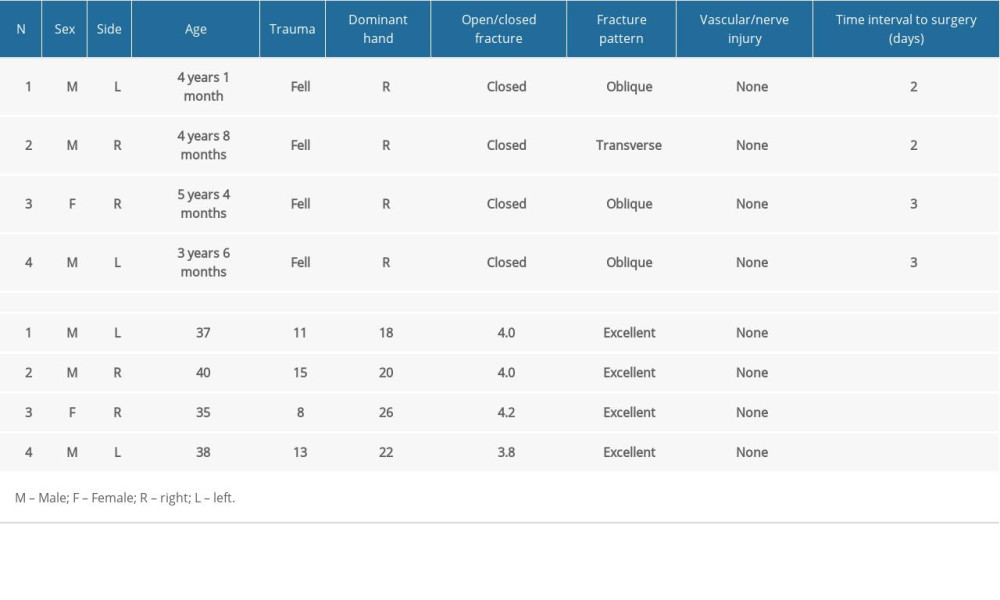
The study was approved by the Ethics Committee of Children’s Hospital of Nanjing Medical University, and informed consent was obtained from the guardians of subjects. Between August 2016 and August 2019, 4 patients (3 boys and 1 girl) with displaced MDJ fractures of the distal humerus were treated with closed reduction and percutaneous intramedullary fixation with Kirschner wire (Table 1). The mean age at injury was 4 years 5 months (range: 3 years 6 months to 5 years 4 months). There were 3 cases of oblique fracture and 1 case of transverse fracture. The operation time and the frequency of intraoperative fluoroscopy were recorded. Anteroposterior and lateral radiographs of the elbow joint were taken for all patients at 1 day, 2 weeks, and 4 weeks after the surgery to observe fracture union. The Kirschner wire and external fixation were removed after fracture union was confirmed by radiography. At the last follow-up, the Flynn elbow joint function score was used to evaluate clinical outcomes [5] (Table 2) and complications were recoded.
SURGICAL PROCEDURES:
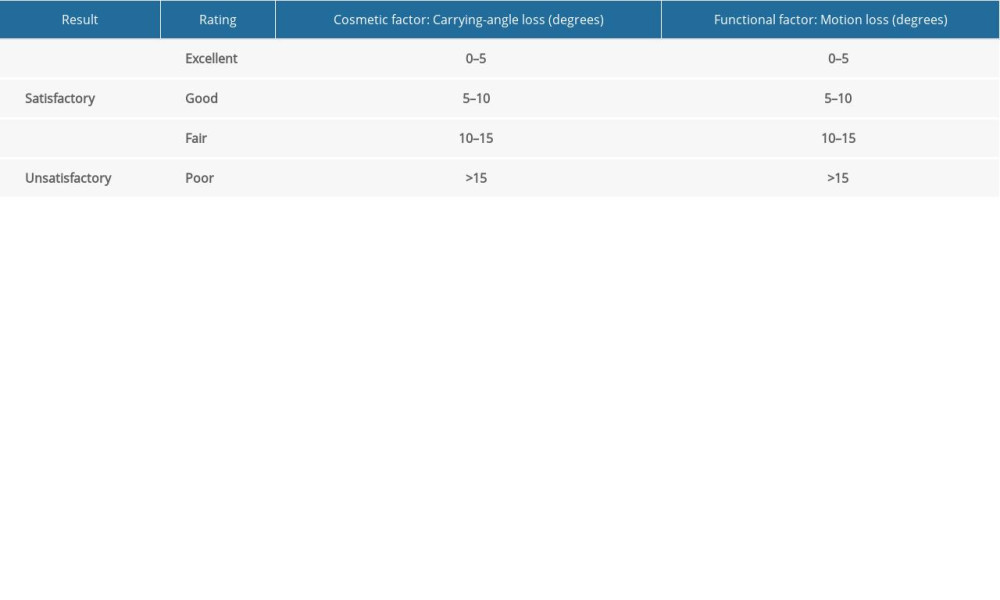
The patient with displaced MDJ fracture (Figure 1) was placed in the supine position, and the affected limb was abducted on the fluoroscopic table (Philips, Amsterdam, Netherlands). The first attempt at closed reduction was made with the same technique as closed reduction used to treat supracondylar fractures of the humerus in children [6]. The C-arm machine (Philips, Amsterdam, Netherlands) was used to obtain an anteroposterior and lateral radiograph of the elbow joint to confirm satisfactory reduction, and the following procedures were performed.
Two pre-bent Kirschner wires (1.5 mm and 2.0 mm in diameter), whose radii were 3 times the diameter of humeral shaft, were inserted into the medial and lateral epicondyle of humerus, respectively, at the angle of approximately 45° to the longitudinal axis of the humerus. C-arm fluoroscopy was used to confirm the position of the top of the Kirschner wire and the reduction status. After 2 Kirschner wires were inserted intramedullary (Figure 2A, 2B), the third Kirschner wire was placed in a retrograde direction into the lateral side of the distal humerus and passed through the contralateral bone cortex to achieve anti-flexion/extension and rotation fixation (Figure 2C, 2D). After the position of Kirschner wires and satisfactory fracture reduction were confirmed by C-arm fluoroscopy, the end of the Kirschner wire outside the skin was cut and covered with sterile gauze. Finally, the elbow was fixed at a 90° flexion position with plaster (Figure 3).
Results
SURGICAL DATA AND FOLLOW-UP DATA:
The 4 patients in this study were followed up for more than 18 months. The mean operation time was 37.5 min (range: 35–40 min), and the frequency of intraoperative radiation exposure was 11.7 times (range: 8–15 times). The fractures in all 4 patients were confirmed to be healed based on radiographic images taken at postoperative 4 weeks, and no early complications, including osteofascial compartment syndrome, neurovascular injury, pin tract infection, and pin site irritation, were observed. At the last follow-up, the outcomes of Flynn evaluation were excellent. Further, all 4 children had normal elbow joint motion and none of them had any long-term complications, including clinical or radiographic elbow deformity (Figure 4). The features of each case are described in detail below.
CASE 1:
A boy aged 4 years 1 month with a dominant right hand fell down the stairs and landed on his left hand, and this resulted in a left oblique displaced MDJ fracture of the distal humerus. The injury was treated after 2 days using the technique described above. At 18 months of follow-up, elbow motion was normal with no clinical or radiographic elbow deformity. X-ray findings indicated satisfactory fracture healing.
CASE 2:
A boy aged 4 years 8 months with a dominant right hand fell off a bicycle and landed on his right hand, and this resulted in a right transverse displaced MDJ fracture of the distal humerus. The injury was treated after 2 days using the technique described above. At 20 months of follow-up, elbow motion was normal with no clinical or radiographic elbow deformity, and X-ray results indicated satisfactory fracture healing.
CASE 3:
A girl aged 5 years 4 months with a dominant right hand fell off a balance bike and landed on her right hand, and this resulted in a right oblique displaced MDJ fracture of the distal humerus. The injury was treated after 3 days using the technique described above. At 26 months of follow-up, elbow motion was normal with no clinical or radiographic elbow deformity, and radiography indicated satisfactory fracture healing.
CASE 4:
A boy aged 3 years 6 months with a dominant right hand fell while walking and landed on his left hand. He was diagnosed with a left oblique displaced MDJ fracture of the distal humerus. The injury was treated after 3 days using the technique described above. At 22 months of follow-up, elbow motion was normal with no clinical or radiographic elbow deformity, and radiographs indicated satisfactory fracture healing.
Discussion
This study describes a new method for treating the MDJ fractures of distal humerus in children, which we call “closed reduction and percutaneous intramedullary fixation with Kirschner wires”. MDJ fractures of the distal humerus tend to appear completely displaced and unstable on radiographs. The fractures are oblique or transverse, but they are occasionally comminuted. Oblique fractures have a larger contact surface area and is more stable than transverse fracture, but its longitudinal shear force is greater. Transverse fracture has a smaller contact surface area and a longer distal end, which increases the lever arm length. Additionally, the traction of surrounding soft tissues is likely to result in displacement of the fracture end [1]. Overall, regardless of fracture type, it is difficult to access a stable reduction. The previously preferred treatment for displaced MDJ fracture of distal humerus in children was closed reduction and internal fixation. The reduction procedure is the same as that for supracondylar humeral fractures, while the methods of internal fixation used are various. Below, we describe the advantages and limitations of known fixation methods for these fractures, and compare them with this new method.
Fayssoux et al [1] treated 14 cases of MDJ fractures of the distal humerus (8 oblique fractures and 6 transverse fractures) by closed reduction with Kirschner wire fixation, using different Kirschner wire configurations, including cross-pinning, lateral approach, and a medial approach. Wire fixation and maintenance of reduction were difficult and were associated with a longer operation time (an average increase of 53 min) and more severe trauma. Additionally, it was more difficult to achieve a stable reduction with transverse fractures than with oblique fractures, and failure of internal fixation and loss of reduction occurred in 5 cases (83%) with transverse fractures. In this technique, the angle of the Kirschner wire must be acute for it to pass through the contralateral cortex. However, as the Kirschner wire is almost parallel to the contralateral cortex, repeated attempts are often required. This increases the risk of radiation exposure and decreases fracture stability. Based on these findings, Fayssoux suggested that this fracture be differentiated from conventional supracondylar fractures and be managed differently.
Ge et al [7] treated 39 cases of MDJ fractures of the distal humerus with closed reduction flexible intramedullary nailing or Kirschner wire fixation (elastic nail, 20 patients; Kirschner wire, 19 patients). Postoperative cubitus varus occurred in 6 cases in the Kirschner wire group, and was associated with the internal fixation technique. They concluded that flexible intramedullary nailing fixation is superior to Kirschner wire fixation because it is associated with a lower incidence of postoperative cubitus varus, shorter operation time, less bleeding, and faster fracture healing. Therefore, even though use of the Kirschner wire is less invasive and less expensive and is associated with a lower incidence of trauma than flexible intramedullary nailing, it is difficult to pass the Kirschner wire through the contralateral cortex and this results in poor fixation stability. Additionally, use of the Kirschner wire is more likely to result in displacement and long-term residual deformity. Finally, repeated attempts at passing the Kirschner wire cause damage to the epiphysis as well as increased risk of radiation exposure. In our study, there was no need to pass the Kirschner wire through the contralateral cortex. The insertion point of the elastic intramedullary nail should be selected at the metaphysis, while the MDJ fracture was already close to the metaphysis. The distal end of the fracture had very little space to insert the nail, repeated attempts at inserting will lead to epiphyseal injury, even iatrogenic growth plate injury, and may also affect the stability of fracture fixation [4]. Our new method combines the advantages of elastic intramedullary nail fixation and Kirschner wire fixation; more importantly, the Kirschner wire can cross the growth plate from the distal end of the humerus into the proximal medullary cavity of the fracture, which makes the operation easier.
De Gheldere et al [2] proposed a retrograde intramedullary fixation technique for the treatment of MDJ fractures of the distal humerus that involves internal fixation via the insertion of 2 Kirschner wires, 1 each into the medial and lateral columns of the distal humerus. However, the use of crossed Kirschner wires for transverse fractures such that the 2 wires intersect at an angle close to parallel to the humeral shaft lead to the exit points of the 2 wires being situated too close to the fracture line, making the fracture reduction unstable. So, we inserted a third Kirschner wire to achieve anti-flexion/extension and rotation fixation. Ge et al [7] found that retrograde insertion of flexible intramedullary nails could provide better control of the distal end of the fracture and better stability of the medial and lateral columns of the distal humerus than did anterograde insertion. Marengo et al [8] treated 14 cases of MDJ fractures of the distal humerus with closed reduction and anterograde flexible intramedullary nailing, which showed good coronal and rotation stability. However, subsequent follow-up found that flexible intramedullary nailing could not completely prevent the flexion or extension displacement of the distal end of the fracture. Since flexible intramedullary nails are parallel to each other in planar fixation and cannot provide multi-directional three-dimensional fixation, control of rotational and sagittal deformity was difficult. In addition, in the process of antegrade flexible intramedullary nail fixation, the S-shaped pre-contoured flexible intramedullary nail often loses its curvature after it enters the medullary cavity. Therefore, precise placement of the distal medial side of the fracture is difficult without repeated attempts. Compared with the Kirschner wire fixation method we have proposed, intramedullary nail fixation is more expensive and requires a surgical incision and administration of a second general anesthetic for removal. The tail of the Kirschner wires in our study was left outside the skin, so it can be removed much more economical and easily. Ge et al [7] found that the flexible intramedullary nailing technique allowed for simple reduction and fixation of the fracture with axial and lateral stability against rotation. In this procedure, the distal end of the wire is firmly placed against the humeral lateral condyle and medial epicondyle and the proximal end is curved against the medullary wall of the humerus. In agreement with their findings, Kamara et al [9] explored the best method of fixation for MDJ fractures of the distal humerus in children from the point of view of biomechanics, and they found that flexible intramedullary nailing provided the best overall stability for fractures in the upper half of the junction zone, while Kirschner wire fixation was the most effective in stabilizing fractures in the lower half.
Xue et al [4] treated 21 cases of MDJ fractures of the distal humerus with open reduction plate and Kirschner wire fixation and obtained good stability. However, plate fixation is traumatic and associated with postoperative incision scar and poor skin conditions. Moreover, the cost is higher and removal of the internal fixation requires administration of a second general anesthetic. More importantly, during the operation, the distal periosteum of the fracture needs to be extensively stripped for fixation of at least 2 screws at the distal end of the plate. This can increase the risk of delayed union and nonunion of the fracture, as well as a risk to the distal epiphysis as a result of iatrogenic injury. Given all these limitations and potential complications of open reduction when compared with our new method, plate fixation was too traumatic, uneconomic, and requires secondary general anesthesia to remove internal fixation, which was not the best choice for pediatric MDJ fractures of the distal humerus.
Based on the above reported findings of our literature review and our clinical experience, our closed reduction percutaneous intramedullary fixation technique with Kirschner wires for displaced MDJ fractures of the distal humerus has the following advantages: (1) No surgical incision is needed and the sharp Kirschner wire can be driven directly into the humerus, which is more acceptable to parents. (2) The retrograde placement approach is simple and safe and has less intraoperative radiation exposure based on the above findings and our clinical experience. (3) The Kirschner wire entry point is more distal than that of the flexible intramedullary nail; moreover, a smooth Kirschner wire with a diameter of less than 2 mm is less likely to cause damage even if it goes through the epiphysis. (4) The use of 2 Kirschner wires for intramedullary fixation is easier and provides more stability than the insertion of a single Kirschner wire across the distal and proximal cortices, and if necessary, a third Kirschner wire could be passed through the contralateral cortex to prevent rotation and sagittal displacement. (5) Compared with flexible intramedullary nail and plate fixation, the cost is lower and the removal of internal fixation does not need a second general anesthetic.
There are several limitations in this study. First, our sample size was small and the follow-up time was short, so a large multi-center study with long-term follow-up is needed to confirm the efficacy of this new method in the future. Second, prospective studies are required for comparing this new method with other traditional methods to demonstrate its benefits.
Conclusions
To conclude, closed reduction percutaneous intramedullary fixation using Kirschner wires was an effective treatment for displaced MDJ fractures of the distal humerus in the 4 children described and was shown to be easy to perform with a short operation time.
Figures
 Figure 1. Pre-operative fluoroscopy of a 4-year-old boy with left distal humerus metaphyseal-diaphyseal junction (DMJ) fracture (Case 1). (A) Pre-operative anteroposterior fluoroscopy of left distal humerus. (B) Pre-operative lateral fluoroscopy of left distal humerus.
Figure 1. Pre-operative fluoroscopy of a 4-year-old boy with left distal humerus metaphyseal-diaphyseal junction (DMJ) fracture (Case 1). (A) Pre-operative anteroposterior fluoroscopy of left distal humerus. (B) Pre-operative lateral fluoroscopy of left distal humerus. 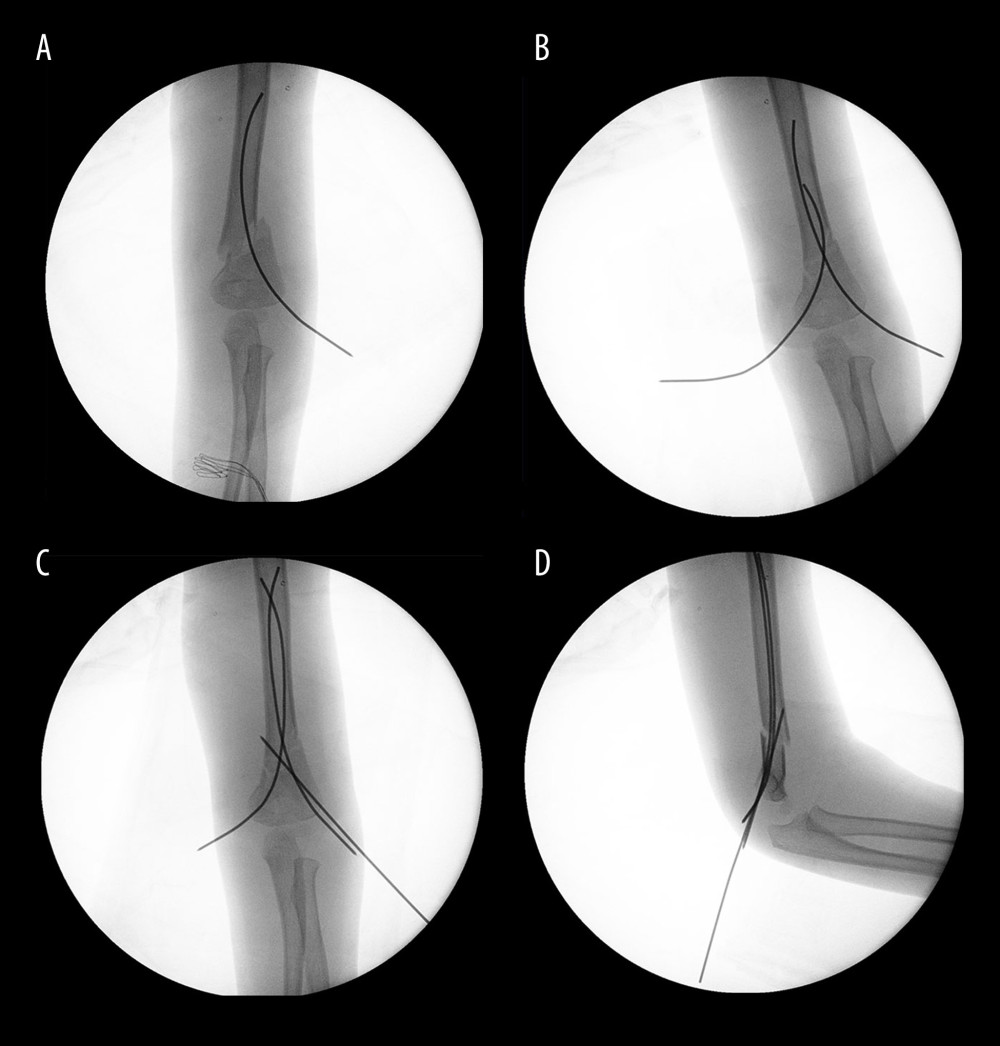 Figure 2. Surgical procedures of closed reduction percutaneous intramedullary fixation with Kirschner wire for Case 1. (A) The first pre-bent Kirschner wires was inserted into the lateral epicondyle of the humerus. (B) Another pre-bent Kirschner wires was inserted into the medial epicondyle of the humerus. (C, D) The third Kirschner wire was placed in a retrograde direction into the lateral side of distal humerus and passed through the contralateral bone cortex to achieve anti-flexion/extension and rotation-stable fixation. Intra-operative fluoroscopy showed satisfactory fracture reduction.
Figure 2. Surgical procedures of closed reduction percutaneous intramedullary fixation with Kirschner wire for Case 1. (A) The first pre-bent Kirschner wires was inserted into the lateral epicondyle of the humerus. (B) Another pre-bent Kirschner wires was inserted into the medial epicondyle of the humerus. (C, D) The third Kirschner wire was placed in a retrograde direction into the lateral side of distal humerus and passed through the contralateral bone cortex to achieve anti-flexion/extension and rotation-stable fixation. Intra-operative fluoroscopy showed satisfactory fracture reduction. 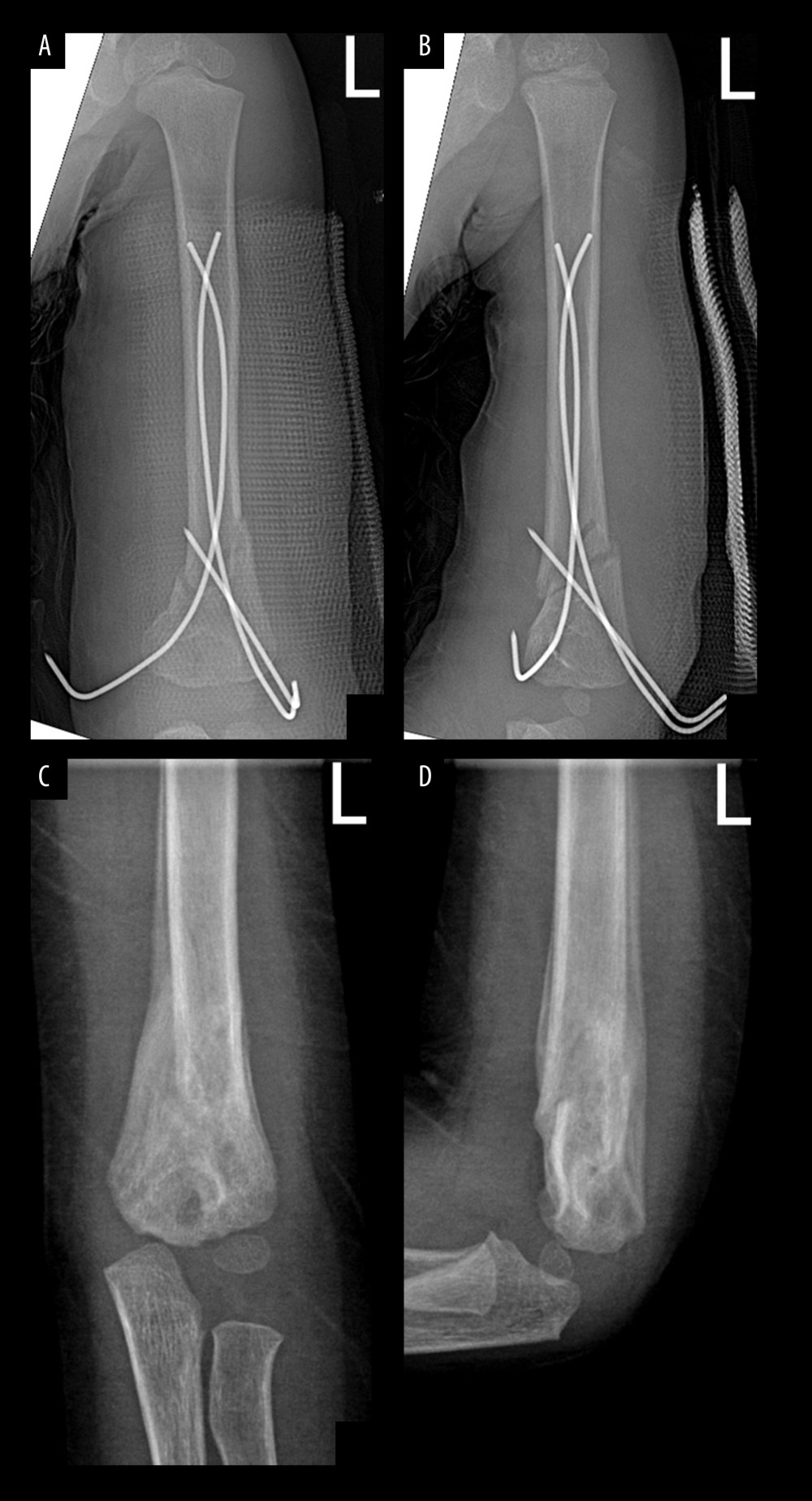 Figure 3. Postoperative fluoroscopy showed excellent results. (A) Seven days postoperative anteroposterior fluoroscopy of left distal humerus. (B) Seven days postoperative lateral fluoroscopy of left distal humerus. (C) Six weeks postoperative anteroposterior fluoroscopy of left distal humerus after Kirschner wires removed. (D) Six weeks postoperative lateral fluoroscopy of left distal humerus after Kirschner wires removed.
Figure 3. Postoperative fluoroscopy showed excellent results. (A) Seven days postoperative anteroposterior fluoroscopy of left distal humerus. (B) Seven days postoperative lateral fluoroscopy of left distal humerus. (C) Six weeks postoperative anteroposterior fluoroscopy of left distal humerus after Kirschner wires removed. (D) Six weeks postoperative lateral fluoroscopy of left distal humerus after Kirschner wires removed. 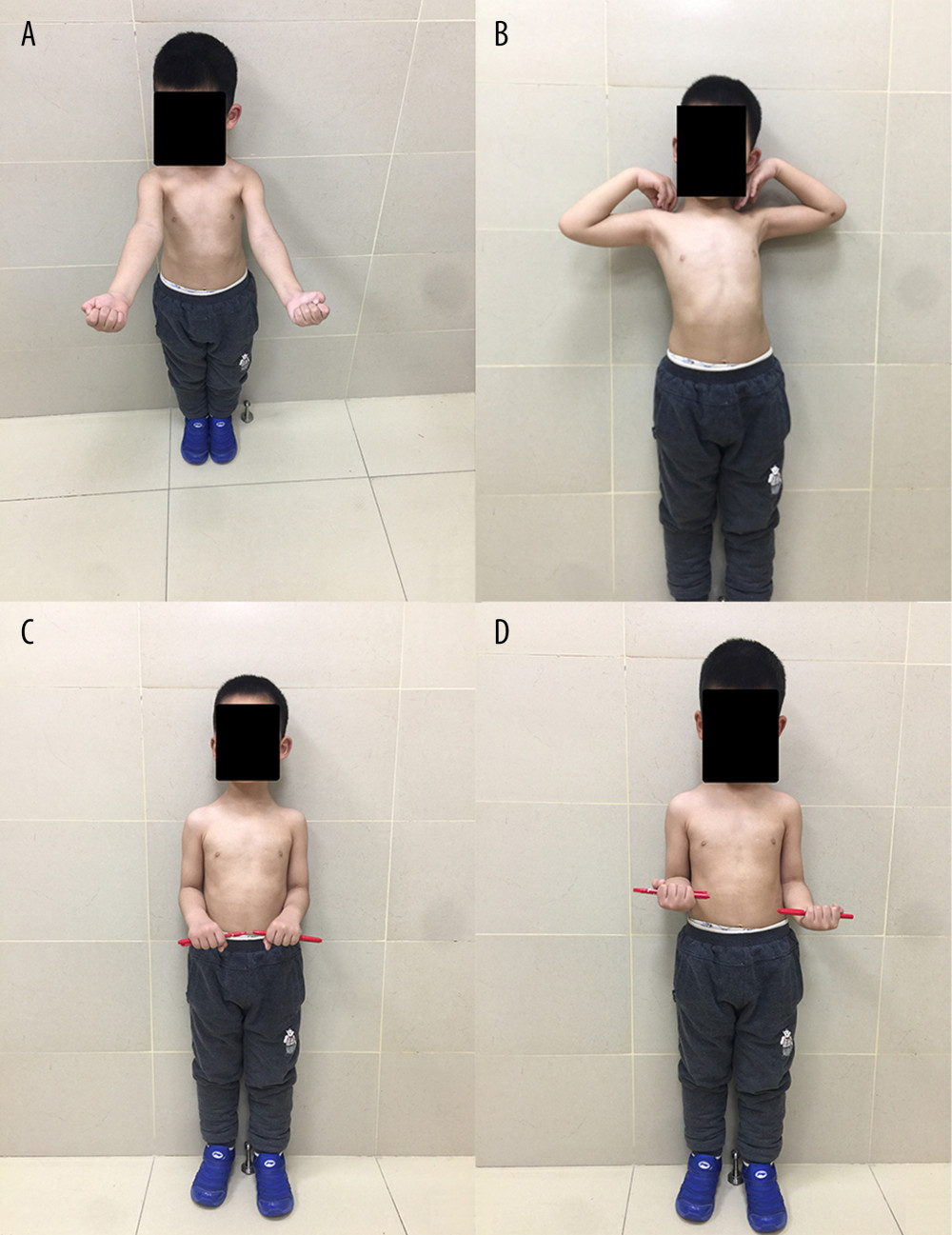 Figure 4. Clinical outcome at the last follow-up showed excellent function. (A, B) Elbow joint has normal flexion and extension function. (C, D) Elbow joint has normal pronation and supination function.
Figure 4. Clinical outcome at the last follow-up showed excellent function. (A, B) Elbow joint has normal flexion and extension function. (C, D) Elbow joint has normal pronation and supination function. References
1. Fayssoux RS, Stankovits L, Domzalski ME, Fractures of the distal humeral metaphyseal-diaphyseal junction in children: J Pediatr Orthop, 2008; 28(2); 142-46
2. de Gheldere A, Re: Article by Fayssoux et al entitled “Fractures of the distal humeral metaphyseal-diaphyseal junction in children” (J Pediatr Orthop 2008;28:142–146): J Pediatr Orthop, 2010; 30(7); 746-47
3. Sen RK, Tripathy SK, Kumar A, Metaphyseo-diaphyseal junction fracture of distal humerus in children: J Pediatr Orthop B, 2012; 21(2); 109-14
4. Xue YL, Chen YG, Bian XJLateral mini plate and Kirschner wire assisted fixation for the treatment of distal humeral metaphyseal junction fracture in children: Zhongguo Gu Shang, 2020; 33(4); 379-82 [in Chinese]
5. Flynn JC, Matthews JG, Benoit RL, Blind pinning of displaced supracondylar fractures of the humerus in children. Sixteen years’ experience with long-term follow-up: J Bone Joint Surg Am, 1974; 56(2); 263-72
6. Vuillermin C, May C, Kasser J, Closed reduction and percutaneous pinning of pediatric supracondylar humeral fractures: JBJS Essent Surg Tech, 2018; 8(2); e10
7. Ge YH, Wang ZG, Cai HQ, Flexible intramedullary nailing had better outcomes than kirschner wire fixation in children with distal humeral metaphyseal-diaphyseal junction fracture: A retrospective observational analysis: Int J Clin Exp Med, 2014; 7(10); 3568-72
8. Marengo L, Canavese F, Cravino M, Outcome of displaced fractures of the distal metaphyseal-diaphyseal junction of the humerus in children treated with elastic stable intramedullary nails: J Pediatr Orthop, 2015; 35(6); 611-16
9. Kamara A, Ji X, Liu T, A comparative biomechanical study on different fixation techniques in the management of transverse metaphyseal-diaphyseal junction fractures of the distal humerus in children: Int Orthop, 2019; 43(2); 411-16
Figures
 Figure 1. Pre-operative fluoroscopy of a 4-year-old boy with left distal humerus metaphyseal-diaphyseal junction (DMJ) fracture (Case 1). (A) Pre-operative anteroposterior fluoroscopy of left distal humerus. (B) Pre-operative lateral fluoroscopy of left distal humerus.
Figure 1. Pre-operative fluoroscopy of a 4-year-old boy with left distal humerus metaphyseal-diaphyseal junction (DMJ) fracture (Case 1). (A) Pre-operative anteroposterior fluoroscopy of left distal humerus. (B) Pre-operative lateral fluoroscopy of left distal humerus.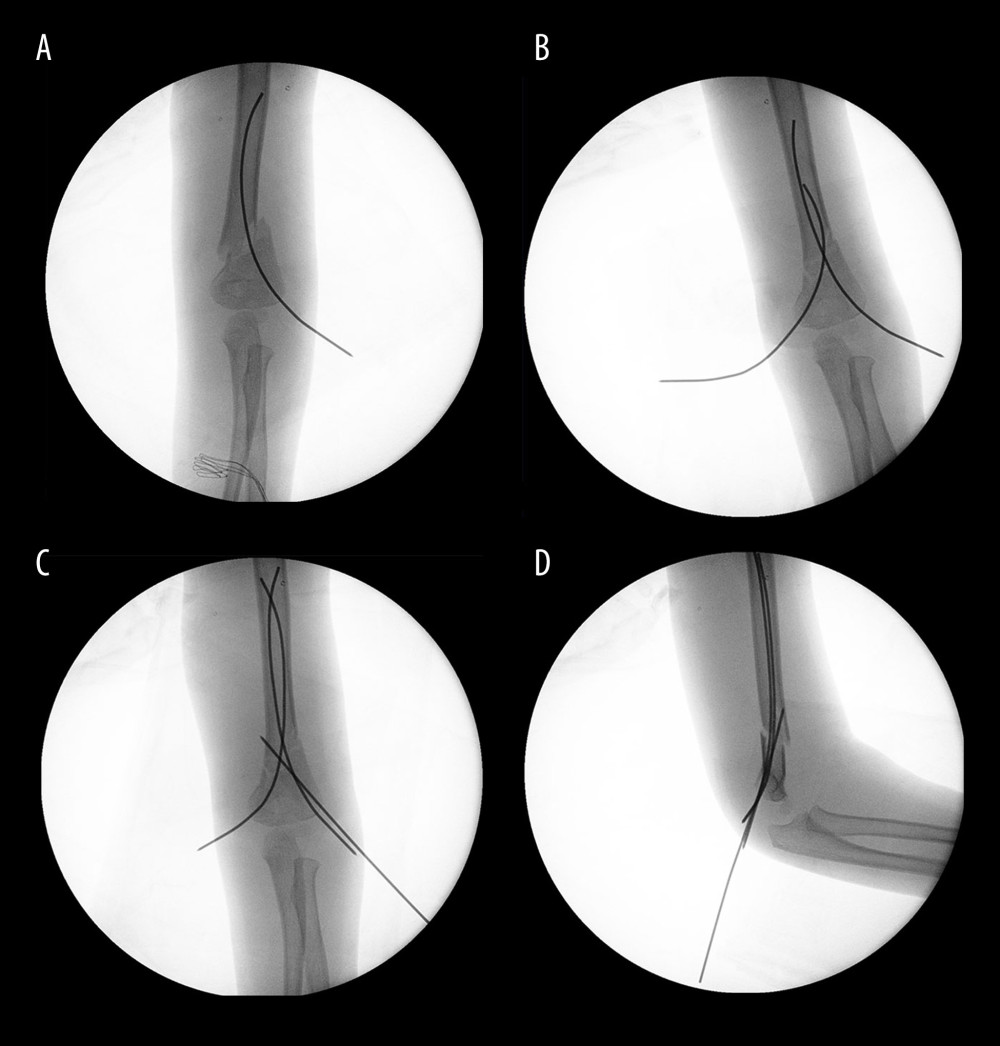 Figure 2. Surgical procedures of closed reduction percutaneous intramedullary fixation with Kirschner wire for Case 1. (A) The first pre-bent Kirschner wires was inserted into the lateral epicondyle of the humerus. (B) Another pre-bent Kirschner wires was inserted into the medial epicondyle of the humerus. (C, D) The third Kirschner wire was placed in a retrograde direction into the lateral side of distal humerus and passed through the contralateral bone cortex to achieve anti-flexion/extension and rotation-stable fixation. Intra-operative fluoroscopy showed satisfactory fracture reduction.
Figure 2. Surgical procedures of closed reduction percutaneous intramedullary fixation with Kirschner wire for Case 1. (A) The first pre-bent Kirschner wires was inserted into the lateral epicondyle of the humerus. (B) Another pre-bent Kirschner wires was inserted into the medial epicondyle of the humerus. (C, D) The third Kirschner wire was placed in a retrograde direction into the lateral side of distal humerus and passed through the contralateral bone cortex to achieve anti-flexion/extension and rotation-stable fixation. Intra-operative fluoroscopy showed satisfactory fracture reduction.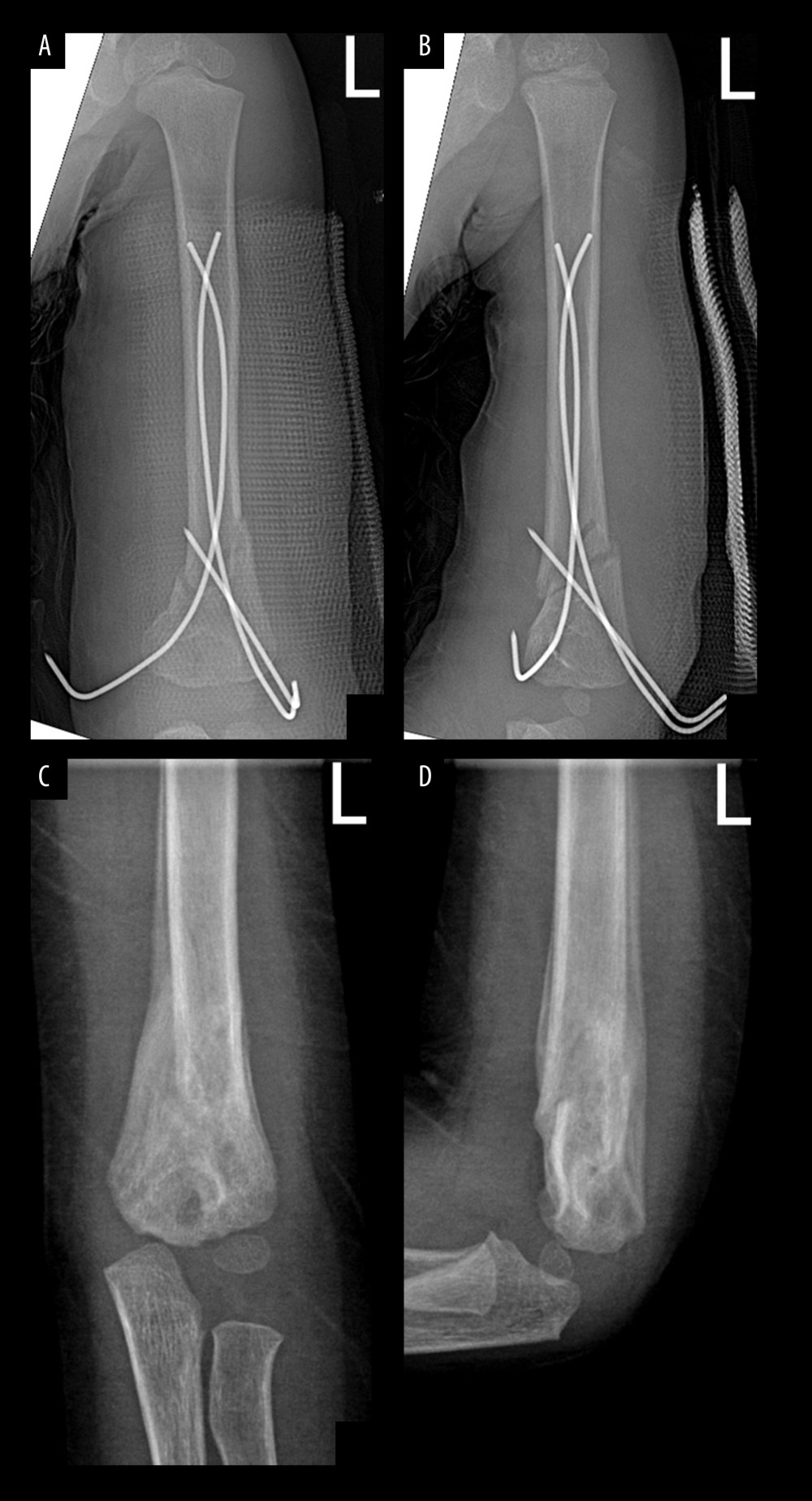 Figure 3. Postoperative fluoroscopy showed excellent results. (A) Seven days postoperative anteroposterior fluoroscopy of left distal humerus. (B) Seven days postoperative lateral fluoroscopy of left distal humerus. (C) Six weeks postoperative anteroposterior fluoroscopy of left distal humerus after Kirschner wires removed. (D) Six weeks postoperative lateral fluoroscopy of left distal humerus after Kirschner wires removed.
Figure 3. Postoperative fluoroscopy showed excellent results. (A) Seven days postoperative anteroposterior fluoroscopy of left distal humerus. (B) Seven days postoperative lateral fluoroscopy of left distal humerus. (C) Six weeks postoperative anteroposterior fluoroscopy of left distal humerus after Kirschner wires removed. (D) Six weeks postoperative lateral fluoroscopy of left distal humerus after Kirschner wires removed.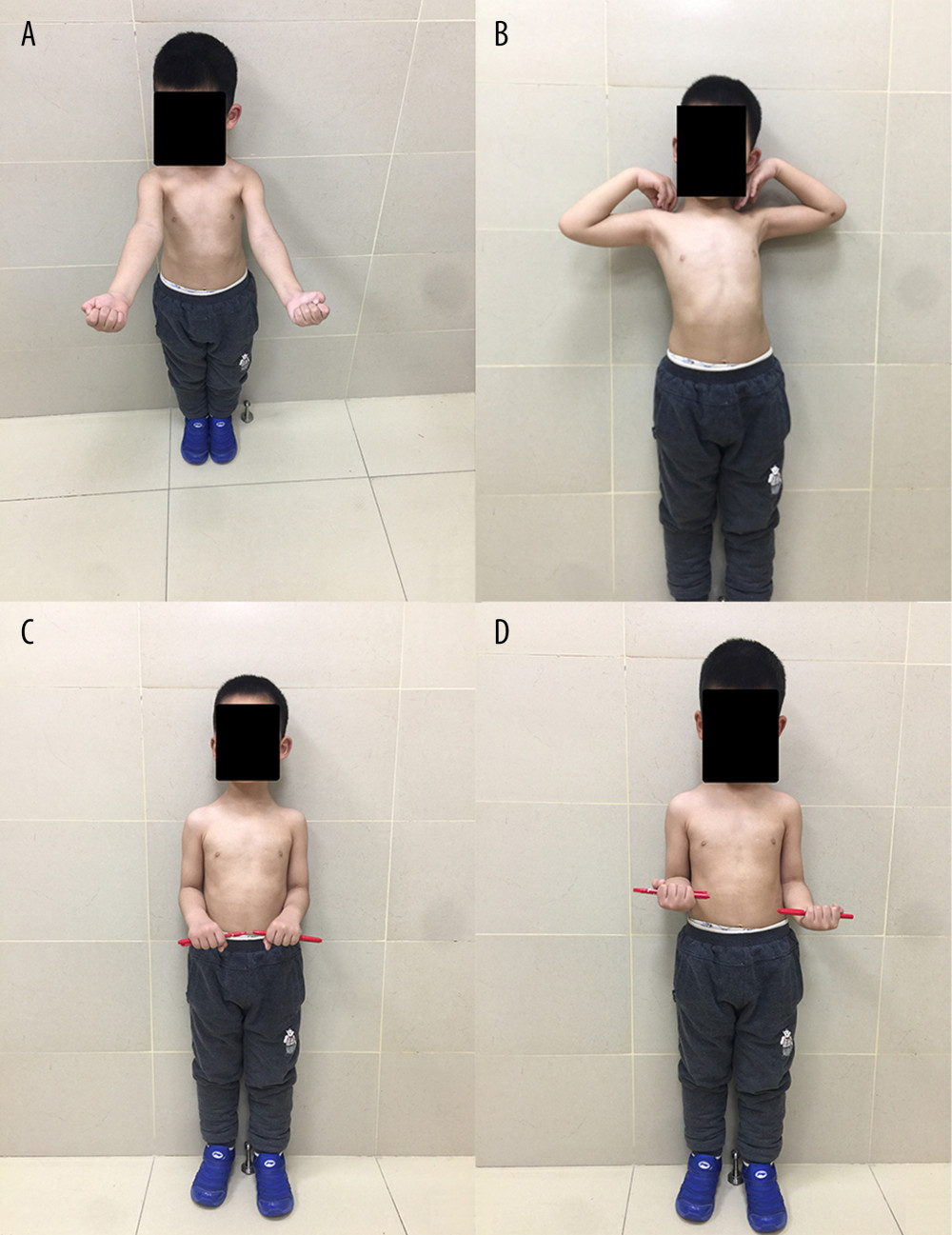 Figure 4. Clinical outcome at the last follow-up showed excellent function. (A, B) Elbow joint has normal flexion and extension function. (C, D) Elbow joint has normal pronation and supination function.
Figure 4. Clinical outcome at the last follow-up showed excellent function. (A, B) Elbow joint has normal flexion and extension function. (C, D) Elbow joint has normal pronation and supination function. In Press
05 Mar 2024 : Clinical Research
Role of Critical Shoulder Angle in Degenerative Type Rotator Cuff Tears: A Turkish Cohort StudyMed Sci Monit In Press; DOI: 10.12659/MSM.943703
06 Mar 2024 : Clinical Research
Comparison of Outcomes between Single-Level and Double-Level Corpectomy in Thoracolumbar Reconstruction: A ...Med Sci Monit In Press; DOI: 10.12659/MSM.943797
21 Mar 2024 : Meta-Analysis
Economic Evaluation of COVID-19 Screening Tests and Surveillance Strategies in Low-Income, Middle-Income, a...Med Sci Monit In Press; DOI: 10.12659/MSM.943863
10 Apr 2024 : Clinical Research
Predicting Acute Cardiovascular Complications in COVID-19: Insights from a Specialized Cardiac Referral Dep...Med Sci Monit In Press; DOI: 10.12659/MSM.942612
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952