27 December 2021: Clinical Research
A Comparative Study of the Clinical Efficacy and Safety of Pneumatic Trabeculoplasty and Selective Laser Trabeculoplasty for Patients with Primary Open-Angle Glaucoma or Ocular Hypertension
Yanling Song1ACE, Qiujie Song1ADG*, Yanhui Qin1BD, Jinfeng Xu1CF, Ping Chen1DF, Hong Li1CD, Wenjie Han1BFDOI: 10.12659/MSM.933454
Med Sci Monit 2021; 27:e933454
Abstract
BACKGROUND: We aimed to evaluate the efficacy and safety of pneumatic trabeculoplasty (PNT) and selective laser trabeculoplasty (SLT) in the treatment of primary open-angle glaucoma (POAG) and ocular hypertension (OHT).
MATERIAL AND METHODS: We randomly divided 120 cases (120 eyes) of POAG or OHT into 2 groups: PNT and SLT. The changes in anterior chamber angle, intraocular pressure (IOP), treatment effect, macular retinal ganglion cell complex (GCC) thickness, visual field, adverse reactions, and complications were observed before and 3 months after treatment.
RESULTS: In the PNT group, the opening range of anterior chamber angle at 1 week, 2 weeks, 1 month, and 3 months after surgery was significantly larger than that before surgery. In the SLT group, the open range of anterior chamber angle was significantly less than that before surgery at 1 week and 2 weeks after surgery. The open range of anterior chamber angle in the PNT group was significantly larger than that in the SLT group at 1 week, 2 weeks, 1 month, and 3 months after surgery. The mean IOP of the 2 groups decreased significantly after surgery. The postoperative mean IOP of the SLT group was significantly higher than that of the PNT group, and the decrease of IOP in the PNT group was significantly greater than that of the SLT group. The effective rate of the PNT group was higher than that of the SLT group.
CONCLUSIONS: Both PNT and SLT can reduce the IOP of patients with POAG and OHT. PNT appears to have better short-term treatment efficiency than SLT.
Keywords: Glaucoma, Open-Angle, Ocular Hypertension, Adult, Female, Humans, Laser Therapy, Male, Trabeculectomy, young adult
Background
Glaucoma is an irreversible blinding eye disease. After cataract, it is the second leading cause of blindness in the world. Glaucoma is characterized by pathological increased intraocular pressure (IOP) and accompanied by irreversible damage of the optic nerve and visual function. Primary open-angle glaucoma (POAG) is an important part of primary glaucoma, and it is a group of diseases in which the IOP exceeds the tolerance of the optic nerve, resulting in optic nerve papilla damage and visual field defect; the angle of the chamber is open and the appearance is normal [1]. At present, there is no effective way to cure glaucoma. Reducing the IOP is the only effective way to prevent progression of glaucoma [2].
Ocular hypertension (OHT) refers to the physiological increase of IOP, excludes ocular or systemic diseases that affect IOP, and has high IOP (>21 mmHg) and open angle without optic disc and visual field changes [3]. OHT cannot be separated from POAG in the short term by current detection methods, which is also called suspected glaucoma or early glaucoma. The prevalence of OHT in people over 40 years old is 4%. About 0.5% to 1% of patients with OHT progress to POAG every year [4].
Pneumatic trabeculoplasty (PNT) is a new non-surgical treatment for glaucoma. The principle of reducing IOP can be explained as follows. The treatment ring is used as the corresponding area on the surface of the eyeball. In the process of vacuum suction, the beam net is pulled, so the resistance of aqueous humor through trabecular meshwork is reduced, and the IOP is reduced. During the process of vacuum suction, the passage between the uvea and sclera is widened and the IOP is decreased [5]. Studies have confirmed that PNT has the advantages of being non-invasive, safe, and convenient, and has a stable effect of reducing IOP in the short term compared to traditional treatment methods [6]. Selective laser trabeculoplasty (SLT) is a repeatable laser therapy for glaucoma and ocular hypertension without coagulative thermal injury. The basis of this method is as follows. A laser with specific wavelength can cause damage to pigment tissue and selectively act on target cells. The functional trabecular meshwork of the human eye is composed of 2 types of cells – the trabecular meshwork cells with pigment and the trabecular meshwork cells without pigment – so selective laser targeting therapy can be applied to the pigmented trabecular meshwork cells without damaging the surrounding tissues, and it can keep the structural integrity of trabecular tissue. After treatment, more cells differentiate in the trabecular meshwork, filtering part of the laser irradiation site. Therefore, the present randomized controlled trial study was performed to evaluate the effectiveness and safety of PNT and SLT by observing changes in anterior chamber angle, 24-h IOP, efficiency, ganglion cell complex (GCC), visual field, adverse reactions, and complications.
Material and Methods
CLINICAL DATA:
Sample size calculation formula:
In the formula, n represents the sample size of each group: α represents inspection level, which is 0.05, so Zα=1.96; β represents inspection efficiency, which is 0.9, so Zβ=1.28; σ represents the estimated value of the standard deviation of the mean intraocular pressure of all patients before treatment, σ=1.98 in this study; and δ represents the estimated value of the D-value between the mean intraocular pressure of PNT group and SLT group after treatment, δ=1.3 in this study.
According to the above formula, 49 subjects are needed in each group. In addition, considering the possible loss to follow-up in the later stage, we estimated the loss to follow-up rate as 20%. Therefore, our study required at least 59 subjects in each group, and at least 118 subjects in 2 groups.
We enrolled 120 patients (120 eyes) affected with POAG or OHT who were treated in the Ophthalmology Department of Dongying People’s Hospital (Shandong, China) from June 2019 to June 2020. Among them, 65 patients (65 eyes) had POAG and 55 patients (55 eyes) had OHT. There were 51 males and 69 females, with an age range of 19–77 years old, with an average age of (39.23±13.07) years old. All eyes were randomly divided into 2 groups, with 60 eyes in each group. The 2 groups were treated with PNT or SLT; according to surgical method, they were named the PNT group and SLT group. There was no significant difference in clinical data between the 2 groups, which was comparable (P>0.05) (Table 1).
Inclusion criteria: (1) over 18 years old; (2) diagnosed as POAG or OHT; (3) IOP less than 30 mmHg (1 mmHg=0.133 kPa); (4) diopter less than – 6 D; (5) no history of intraocular surgery or ocular trauma; (6) could follow up on time.
Exclusion criteria: (1) in the advanced stage of POAG; (2) had vascular and neurological retinopathy that interferes with the results of this study, such as high myopia changes, degeneration, and holes; (3) a history of intraocular surgery, penetrating ocular trauma, or retinal laser treatment; (4) had serious corneal disease, systemic disease, mental disease, or could not complete the follow-up.
The study was approved by the Ethics Committee of Dongying People’s Hospital (approval document No.: DY-IRB-20190021). Patients who participated in the study had complete clinical data. Signed written informed consents were obtained from the patients and/or guardians.
OPTICAL COHERENCE TOMOGRAPHY (OCT): OCT is a non-contact biological tissue imaging technology [7]. The scan mode of GCC (retinal ganglion cell complex in macular region) was selected. The GCC scan consists of 15 vertical scans covering a range of 7 mm2. The scanning center was 1 mm temporal to the macular fovea so as to better cover the temporal area. In addition, the scan also included a horizontal scan at the center to note the depth and perform a fovea search. With the fovea as the center, GCC-a is the average thickness, GCC-s is the upper average thickness, and GCC-i is the lower average thickness.
VISUAL INSPECTION:
A Humphrey – 750 automatic perimeter (Germany Zeiss company) was used for visual field inspection. Program settings were: Center 30-2 inspection procedures, white Stimulus III, 31.5 asb as background brightness, physiological blind spot gaze monitoring. After the whole process of computer processing, the visual field inspection result is given, which mainly includes mean visual field defect (MD) and pattern standard deviation (PSD). The difference from the average threshold of all detection sites and the mean of the same age patients without eye disease was MD, and it reflects the degree of decline in visual average sensitivity due to various reasons. MD may be due to refractive interstitial opacity or optic nerve damage. Detection of MD alone cannot judge specific eye diseases. Therefore, it is necessary to combine another indicator, namely PSD. PSD reflects the visual field irregularity caused by local visual field defect. This PSD result can filter out the decrease of visual sensitivity caused by refractive interstitial opacity. Therefore, this study combined MD and PSD for analysis.
ULTRASOUND BIOMICROSCOPY (UBM) INSPECTION: The patient was placed in supine position, surface anesthesia was performed on the treated eye, we placed a bottomless eye cup in the conjunctival sac and injected sterile water for injection, then a UBM probe scanned vertically near the limbus [8]. Scanning methods: The limbal cornea has 4 quadrants throughout the week, all of which were scanned laterally and radiographically, focused on the observation of the anterior chamber angle and measured the anterior chamber depth. The anterior chamber depth could be measured, analyzed, and stored by the obtained images. The parameters of anterior chamber angle were defined as: taking the scleral process as the center of the circle, made a circle with a radius of 500 μm, then the degree of the angle formed by the intersection of the circle with the corneal endodermis and the iris anterior surface and the line between the scleral process was the degree of the anterior chamber angle.
MEASUREMENT OF 24-H MEAN IOP: We used a non-contact tonometer (Canon) for IOP measurement [9]. The subjects were not allowed to eat food or take medicine that affected IOP 1 week before the measurement, and were told not to drink alcohol. On the day of the measurement, the subject normally ate and drank water. All examinations were done by the same doctor each time the patient’s sitting IOP was measured; it measured 3 times for each eye and we took the average value. We measured IOP at 5: 00, 7: 00, 10: 00, 14: 00, 18: 00, 22: 00, then took the mean value. At 24 h, the mean IOP was measured before surgery and 1 day, 1 week, 2 weeks, 1 month, and 3 months after surgery.
:
The PNT1000 therapeutic instrument produced by Ophthalmic International (USA) was used, and it consists of host, treatment ring, and connecting pipe. The outer diameter of the large ring was 20 mm, the inner diameter was 19 mm, and the diameter of the small ring was 11 mm. The patient was in supine position. The affected eye was topically anesthetized with oxybuprocaine hydrochloride eye drops (Benoxil, Santen Pharmaceutical) for 5 min. The eyelids of the patient were gently opened with fingers. The vacuum suction ring was placed at the limbal of the cornea, and gently pressed down until the suction ring was completely adsorbed on the limbal of the cornea. After starting the machine, we set the maximum negative pressure level of 558.8 mmHg (1 kPa=7.5 mmHg) in advance, raised the IOP to 45–50 mmHg, leaving the vacuum suction ring on the limbus for 60 s, removed the vacuum suction ring, resting for 5 min, and repeat the treatment for 60 s.
:
The patient was in supine position. After topical anesthesia with 0.4% obucaine, the gonioscope was positioned and the treatment was performed with an Australian Ellex LT5106.S Solo laser. The laser wavelength was set at 532 nm, the pulse time was set at 3 ns, the spot diameter was 400 pm, and the pulse energy was 0.8 mJ. The whole trabecular meshwork width was irradiated, and the laser treatment range was 180 functional trabecular meshwork; when the laser irradiated the trabecular meshwork and produced bubbly bubbles, therapeutic energy was reduced to 0.5–1.4 mJ, each quadrant had about 25 points, and the total number of laser points was about 50. The laser beam focused on the area of the pigment trabecular meshwork, and the 400-pm diameter spot covered the pigment trabecular meshwork. Each spot was adjacent but not overlapped, and the final reaction of laser produced decolorized or fine bubbles. The laser energy was adjusted according to the pigment content of the patients. If there was more pigment, the energy was reduced appropriately. The total energy was recorded after surgery.
The patients in both groups were forbidden to use hormonal or hormone containing antibiotic eye drops after surgery. The patients with severe anterior chamber reaction were given nonsteroidal anti-inflammatory drugs (diclofenac sodium or pranoprofen eye drops), 0.02 mL, 4 times a day, until 3 days after surgery.
EFFICACY EVALUATION:
The effective rate evaluation method was as follows, according to the fourth edition of European Glaucoma guidelines (2014). If the initial treatment method reduces the IOP value ≥3 mmHg or the amplitude ≥20%, it is considered that the effect of reducing the IOP is exact. If the initial treatment cannot achieve the target IOP and the second treatment is needed, the effect of the added treatment to reduce the IOP by more than 15% is considered to be exact. The patients included in this study were in the latter situation, so we set the effective standard of treatment for the 2 groups of patients as IOP reduction ≥15%. The effective rate was the number of patients with a definite effect divided by the total number of patients in the group.
POSTOPERATIVE FOLLOW-UP:
We measured and recorded the anterior chamber angle, IOP, macular GCC thickness, and visual field were recorded 2 h before surgery and at 1 week, 2 weeks, 1 month, and 3 months after surgery. We measured and recorded the open range of anterior chamber angle and the IOP of selected patients at 1 h, 1 day, 1 week, 2 weeks, 1 month, and 3 months after the surgery. The IOP values at other timepoints were the mean IOP of 24 h, except for 1 h after surgery. The visual field and visual acuity were recorded 3 months after surgery. We also assessed and recorded the number of adverse reactions to 1 h and 1 day after surgery.
STATISTICAL ANALYSIS:
SPSS 23.0 software (IBM Corp.) was used for the statistical analysis of the data. The visual acuity and intraocular pressure before and after surgery are expressed as χ̄±s. The independent sample
Results
RESULTS OF ANTERIOR CHAMBER ANGLE:
Before surgery, there was no significant difference in the open range of anterior chamber angle between the 2 groups (P>0.05). After surgery, there was no angle adhesion in the 2 groups. In PNT group, the opening range of anterior chamber angle at 1 week, 2 weeks, 1 month, and 3 months after surgery was significantly larger than that before surgery (P<0.05). In the SLT group, the opening range of the anterior chamber angle at 1 week and 2 weeks after surgery was significantly smaller than that before surgery (P<0.05), and there was no significant difference in the opening range of anterior chamber angle between 1 month and 3 months after surgery (P>0.05). The open range of the anterior chamber angle in the PNT group was significantly larger than that in the SLT group at 1 week, 2 weeks, 1 month, and 3 months after surgery (<0.05) (Table 2).
RESULTS OF IOP:
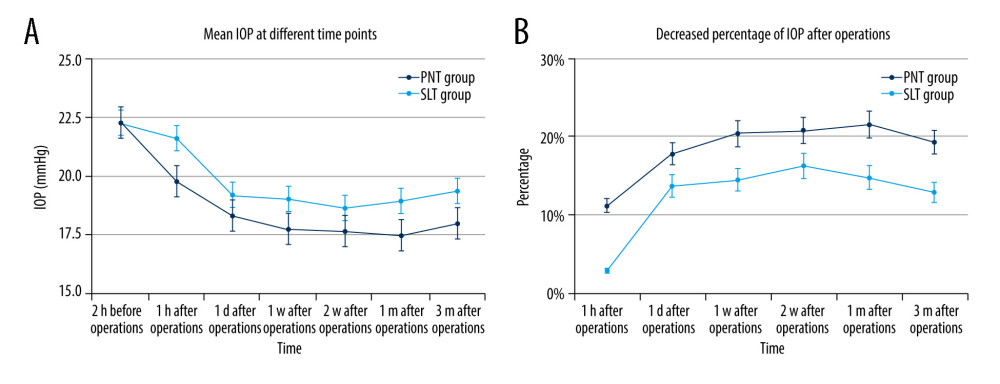
Changes in IOP at each timepoint before and after surgery and the decrease at each timepoint after surgery in the 2 groups (%) are shown in Figure 1. There was no significant difference in IOP between the PNT group and SLT group (P>0.05). At 1 h, 1 day, 1 week, 2 weeks, 1 month, and 3 months after surgery the mean IOP of the 2 groups decreased significantly (P<0.05). There were significant differences in mean IOP between the PNT group and SLT group. IOP in the SLT group was significantly higher than that in the PNT group at 1 h, 1 day, 1 week, 2 weeks, 1 month, and 3 months after surgery (P<0.05). From the decrease of IOP, there were significant differences between the 2 groups at each timepoint after surgery. The decrease in IOP in the PNT group was significantly greater than that in the SLT group (P<0.05).
RESULTS OF EFFECTIVE RATE:
After PNT or SLT surgery, the number of effectively treated patients and the effective rate of the 2 groups first increased and then decreased. At 1 h after surgery, the effective rate of the 2 groups was the lowest, at 28.3% in the PNT group and 3.3% in the SLT group. The maximum effective rate was 98.3% in the PNT group 1 m after surgery, and 78.3% in the SLT group 2 weeks after surgery; 3 months after surgery, the effective rates of the PNT group and SLT group were lower than before, at 88.3% and 61.7%, respectively. The effective rate of the PNT group was higher than that of the SLT group at each timepoint after surgery. The chi-square test showed that the difference between the 2 groups at each timepoint was statistically significant (P<0.05) (Table 3).
RESULTS OF GCC:
Before surgery, there was no significant difference in the preoperative GCC-a, GCC-s, and GCC-i between the 2 groups. There was no statistically significant difference in GCC thickness before and 3 months after surgery. At 3 months after surgery, there was no significant difference in GCC-a, GCC-s, and GCC-i between the PNT group and SLT group (P>0.05) (Table 4).
RESULTS OF VISUAL FIELD:
There was no significant difference in MD and PSD between the PNT group and SLT group before surgery; 3 months after surgery, the MD and PSD of the 2 groups had some changes, but there was no significant difference before and after surgery. There was no significant difference in the MD and PSD between the 2 groups 3 months after surgery (P>0.05) (Table 5).
RESULTS OF ADVERSE REACTIONS AND COMPLICATIONS:
After PNT and SLT treatment, no serious complications occurred in the 2 groups. The adverse reactions 1 h and 1 day after surgery are shown in Table 6. At 1 h after surgery, conjunctival congestion occurred in all patients, and most of them subsided 1 day after surgery. Eleven 11 eyes (18.3%) in the PNT group and 29 eyes (48.3%) in the SLT group had postoperative IOP rebound, with the highest rebound IOP of 6 mmHg (33%). Some patients in the 2 groups recovered to below the preoperative IOP level at 1 day after surgery without increasing medication. Twenty-one eyes (35.0%) in the PNT group and 11 eyes (18.3%) in the SLT group had subconjunctival punctate and patchy hemorrhage, which disappeared 1 day to 1 week after surgery. Intraoperative and postoperative ocular distension occurred in 7 eyes (11.7%) in the PNT group and 15 eyes (25.0%) in the SLT group. Most of the patients’ symptoms disappeared from 1 day to 1 week after surgery.
Discussion
The main manifestations of POAG are optic atrophy and visual field defect. The pathological mechanism of glaucoma is that resistance of the trabecular meshwork to aqueous humor is increased, which leads to increased IOP, then the retinal ganglion cells are progressively lost and the optic nerve fibers are damaged irreversibly [12]. There are 2 proposed mechanisms of trabecular meshwork lesions: one is the change of the composition and content of the matrix outside the trabecular meshwork, which makes the trabecular meshwork narrow and collapse; the other is the abnormal cytoskeleton of trabecular meshwork cells, which leads to the decrease of their contractility [2]. OHT is a special phenomenon in the diagnosis and treatment of POAG after decades of clinical experience, which is different from open angle glaucoma [4]. Epidemiological data show that OHT is more common than POAG, and some patients with OHT develop into POAG [4]. OHT develops slowly; it rarely causes damage to the optic nerve and visual field, but it has the same important pathological factor as open-angle glaucoma, that is, high IOP [3]. IOP is the only risk factor that can be controlled in the treatment of glaucoma.
The aim of glaucoma treatment is to preserve existing visual function, stabilize the optic nerve and retinal nerve fiber layer, and prevent further visual field damage [2]. Reducing IOP is an effective way to preserve visual function. At present, the main means of IOP control are drug therapy and surgical treatment, which have shortcomings in reducing IOP, including adverse effects of drugs, decreased tolerance caused by ocular surface damage, fluctuation of IOP caused by poor compliance, and the complications of surgery and risk of resurgery [13].
It is worth noting that both eyes of POAG and OHT patients are affected. In order not to affect the treatment effect, in this study, the same treatment mode and surgery method were used for both eyes of the same patient. The data obtained from 2 eyes of the same patient often have a strong positive correlation, which means that the amount of information provided by 2 eyes of 1 person is less than that provided by the single eyes of 2 person. In an extreme case, 2 eyes of the same patient may provide exactly the same information, and the other eye of that person may not provide additional information. Therefore, the data provided by 1 person’s 2 eyes cannot be regarded as being the same as the monocular data of 2 persons [14]. In this study, even if both eyes of the patients met the inclusion criteria, only 1 eye of each patient was included as the research subject, and the selection method was random selection.
The exact mechanism of PNT in the treatment of glaucoma is still unclear. It may be that the trabecular meshwork is extended and expanded under the action of the treatment ring and continuous negative pressure mechanical traction, thus improving the outflow of aqueous humor [6]. PNT mainly acts on the trabecular meshwork, and can also affect the uveoscleral channel. The mechanism of SLT in lowering IOP has not been fully elucidated. In vitro culture experiments have shown that a short-pulse low-energy 532 nm frequency doubled laser can selectively act on cultured trabecular meshwork pigment cells without causing thermal damage to surrounding non-pigment tissues [15]. This study showed that the anterior chamber angle was significantly widened after PNT at 1 week, 2 weeks, 1 month, and 3 months after surgery. The opening range of anterior chamber angle was significantly larger than that before surgery (
PNT is a non-invasive treatment. It has been reported that PNT can reduce the IOP in patients with POAG and OHT [16]. SLT is also an effective method to reduce the IOP in patients with POAG and OHT. Through 5 years of follow-up observation, Juzych et al [17] found that SLT can reduce the IOP of patients, and the reduction is from 18.1% in the first year to 27.1% in the fifth year, which fully proves the effect of this method in reducing IOP. These results are consistent with the results of the present study. We studied the changes of mean IOP before and after PNT and SLT, and we found that both methods can significantly reduce the IOP of patients, and the decrease amplitude of the PNT group is higher than that of the SLT group, indicating that the effect of PNT is better than that of SLT in reducing IOP. The reason for this result may be that PNT is a physical treatment based on the effect of reducing intraocular pressure by negative pressure suction during excimer laser in situ keratomileusis. The onset time of PNT is short, but the long-term effect needs to be further studied. SLT improves the porosity of the trabecular meshwork by upregulating the expression of matrix metalloproteinases, cytokines, and macrophages, which is not a purely physical method. SLT needs internal regulation to take effect, so the onset time is longer than with PNT, but the control of intraocular pressure may have a more lasting long-term effect, which needs further research. The observation time of this study mainly includes the period from before treatment to 3 months after treatment. This period can only show that the short-term effect of PNT is better than that of SLT, and the long-term effect needs to be further studied.
The main pathological changes of POAG and OHT are retinal ganglion cell apoptosis, resulting in optic nerve damage and visual field defect [18]. At present, most studies have focused on the defect of the optic nerve fiber layer, but the thickness of macular area, as the concentration of retinal ganglion cells, can reflect the pathological changes of glaucoma [19]. Some studies have found that the macular structure consists of only a nerve fiber layer, ganglion cell layer, and inner plexiform layer. These 3 layers are significantly damaged in glaucoma. These 3 layers are called GCC [20]. Therefore, observing the changes of GCC can further diagnose and follow up the progression of disease [21]. OCT can be used to check the GCC examination, with high accuracy and repeatability, and the process of checking the thickness of GCC in the macular area is simpler than in the optic nerve fiber layer [22]. Therefore, in the present study, OCT was used to compare GCC-a, GCC-s, and GCC-i before and 3 months after PNT or SLT, and we found that the differences were not statistically significant (
The adverse reactions of PNT and SLT are less, and they need no treatment and can disappear within a few days. No serious complications occurred during and after PNT treatment in this study. According to the statistics of adverse reactions 1 h after surgery and 1 days after surgery, we found that the adverse reactions mainly included mild conjunctival edema and congestion, conjunctival bleeding, and some mild discomfort. These symptoms usually disappeared 1–3 days after surgery, and 1 week at the most. In this study, no serious adverse reactions or complications were found, and no visual field defect or retinal ganglion cell damage were found. There were fewer adverse reactions with PNT than with SLT, and there were relatively few adverse reactions with PNT.
Limitations of this study include the small sample size and short observation period. The stability, long-term complications, repeatability, cross-reactions of drugs, and whether it is suitable for other types of glaucoma need further study and discussion.
Conclusions
PNT and SLT can reduce the IOP of patients with POAG and OHT. The postoperative adverse reactions are mild, safety is high, and they can be used as an alternative treatment for such diseases. The short-term effect of PNT is better than that of SLT in increasing the opening range of anterior chamber angle and reducing IOP, and there were fewer adverse reactions in the PNT group. In addition, PNT is simple and non-invasive and patient compliance is high, which helps improve patients’ cooperation with treatment and ensures smooth surgery. Therefore, it PNT is conducive to patients’ postoperative rehabilitation, so that patients can recover their vision as soon as possible, and it warrants consideration for use in clinical practice.
Tables
Table 1. Characteristics of the studied population in the 2 groups.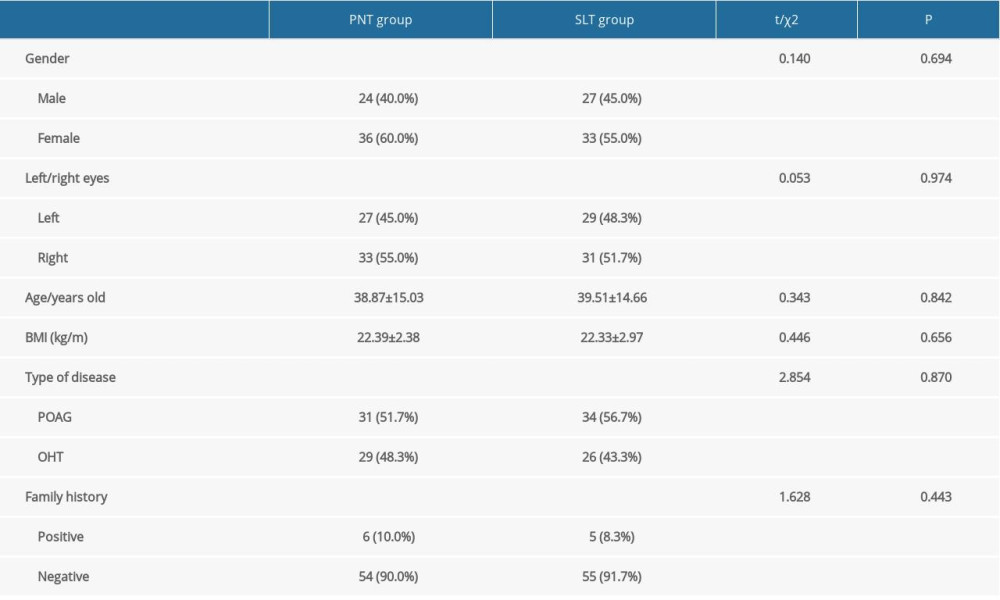 Table 2. Changes of anterior chamber angle opening range before and after surgery (χ̄±s, degree).
Table 2. Changes of anterior chamber angle opening range before and after surgery (χ̄±s, degree).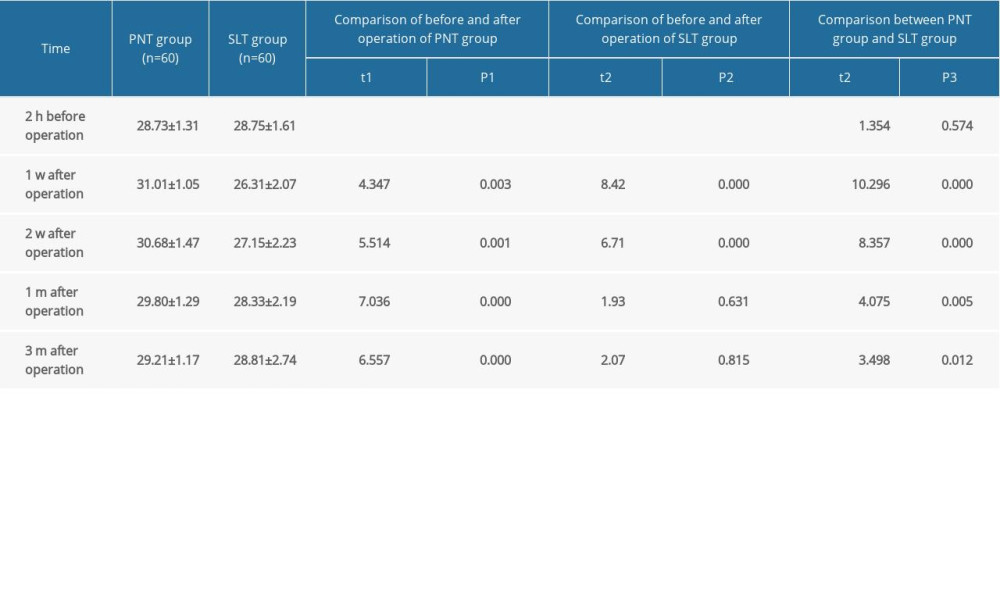 Table 3. Effective rate at different timepoints after surgery [eye (%)].
Table 3. Effective rate at different timepoints after surgery [eye (%)].![Effective rate at different timepoints after surgery [eye (%)].](https://jours.isi-science.com/imageXml.php?i=t3-medscimonit-27-e933454.jpg&idArt=933454&w=1000) Table 4. GCC thickness in different areas of macular area before and after surgery (χ̄±s, μm).
Table 4. GCC thickness in different areas of macular area before and after surgery (χ̄±s, μm).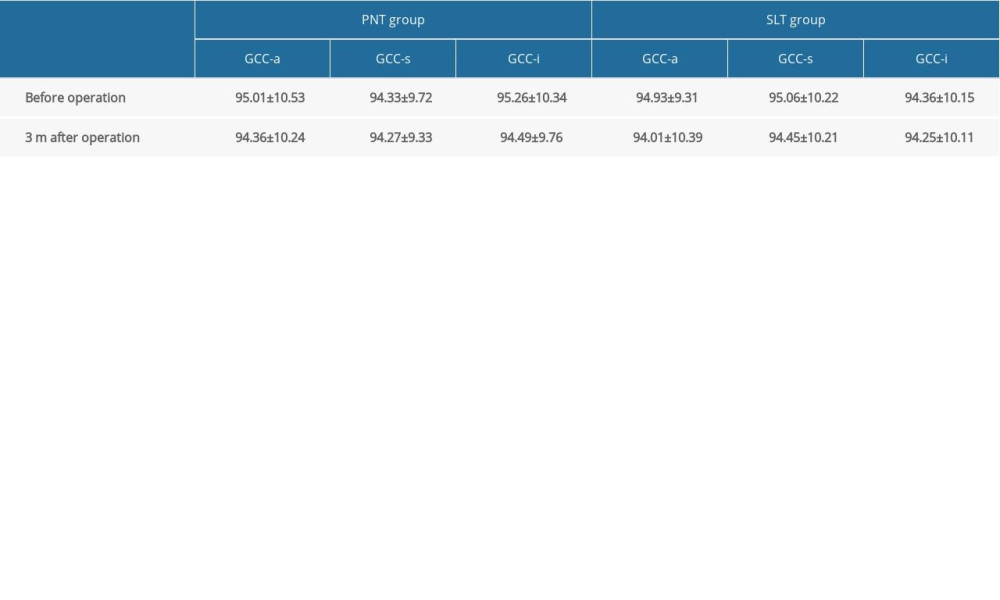 Table 5. Comparison of visual field before and after surgery (χ̄±s, dB).
Table 5. Comparison of visual field before and after surgery (χ̄±s, dB).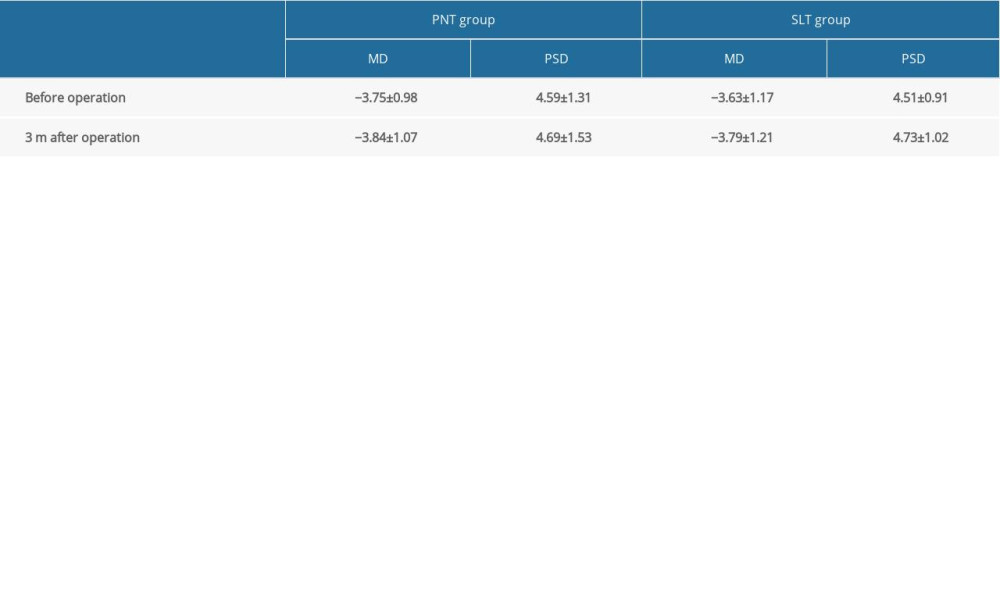 Table 6. Incidence of adverse reactions and complications (eye).
Table 6. Incidence of adverse reactions and complications (eye).
References
1. Evangelho K, Mogilevskaya M, Losada-Barragan M, Vargas-Sanchez JK, Pathophysiology of primary open-angle glaucoma from a neuroinflammatory and neurotoxicity perspective: A review of the literature: Int Ophthalmol, 2019; 39; 259-71
2. Bertaud S, Aragno V, Baudouin C, Labbe APrimary open-angle glaucoma: Rev Med Interne, 2019; 40; 445-52 [in French]
3. Sun YY, Chen WW, Wang NLDiagnosis and treatment of ocular hypertension: Zhonghua Yan Ke Za Zhi, 2016; 52; 542-46 [in Chinese]
4. Hoffmann EM, Lamparter JDifferentiation of ocular hypertension: Ophthalmologe, 2016; 113; 715-28 [in German]
5. Fogagnolo P, Rossetti L, Marchini G, The effect of pneumatic trabeculoplasty on intraocular pressure: The results of a 6-month, open-label, multicenter study: Eur J Ophthalmol, 2008; 18; 922-28
6. Kocabora MS, Ozsutcu M, Kandemir N, Efficacy and safety of pneumatic trabeculoplasty versus timolol added to latanoprost in primary open angle glaucoma: Clin Ter, 2013; 164; e259-62
7. Tan O, Chopra V, Lu AT, Detection of macular ganglion cell loss in glaucoma by Fourier-domain optical coherence tomography: Ophthalmology, 2009; 116; 2305-14
8. Hershberger VS, Augsburger JJ, Hutchins RK, Fibrovascular ingrowth at sclerotomy sites in vitrectomized diabetic eyes with recurrent vitreous hemorrhage: Ultrasound biomicroscopy findings: Ophthalmology, 2004; 111; 1215-21
9. Carlos GR, Hugo PV, Mercedes M, Reliability of the non-contact tono-pachymeter Tonopachy NT-530P in healthy eyes: Clin Exp Optom, 2013; 96; 286-94
10. Uva MG, Longo A, Reibaldi M, Pneumatic trabeculoplasty vs latanoprost as adjunctive therapy to timolol in primary open-angle glaucoma or ocular hypertension: Graefes Arch Clin Exp Ophthalmol, 2009; 247; 1103-9
11. Konstantakopoulou E, Gazzard G, Vickerstaff VThe Laser in Glaucoma and Ocular Hypertension (LiGHT) trial, A multicentre randomised controlled trial: Baseline patient characteristics: Br J Ophthalmol, 2018; 102; 599-603
12. Sihota R, Angmo D, Ramaswamy D, Dada T, Simplifying “target” intraocular pressure for different stages of primary open-angle glaucoma and primary angle-closure glaucoma: Indian J Ophthalmol, 2018; 66; 495-505
13. Li F, Huang W, Zhang X, Efficacy and safety of different regimens for primary open-angle glaucoma or ocular hypertension: A systematic review and network meta-analysis: Acta Ophthalmol, 2018; 96; e277-84
14. Armstrong RA, Statistical guidelines for the analysis of data obtained from one or both eyes: Ophthalmic Physiol Opt, 2013; 33; 7-14
15. Stunf PS, Drnovsek-Olup B, Impact of laser pulse duration on the reduction of intraocular pressure during selective laser trabeculoplasty: Int Ophthalmol, 2018; 38; 83-91
16. Liu JH, Zhang X, Kripke DF, Weinreb RN, Twenty-four-hour intraocular pressure pattern associated with early glaucomatous changes: Invest Ophthalmol Vis Sci, 2003; 44; 1586-90
17. Juzych MS, Chopra V, Banitt MR, Comparison of long-term outcomes of selective laser trabeculoplasty versus argon laser trabeculoplasty in open-angle glaucoma: Ophthalmology, 2004; 111; 1853-59
18. Medeiros FA, Zangwill LM, Bowd C, Evaluation of retinal nerve fiber layer, optic nerve head, and macular thickness measurements for glaucoma detection using optical coherence tomography: Am J Ophthalmol, 2005; 139; 44-55
19. Liang YB, Friedman DS, Zhou Q, Prevalence of primary open angle glaucoma in a rural adult Chinese population: The Handan eye study: Invest Ophthalmol Vis Sci, 2011; 52; 8250-57
20. Tan O, Li G, Lu AT, Mapping of macular substructures with optical coherence tomography for glaucoma diagnosis: Ophthalmology, 2008; 115; 949-56
21. Chen J, Huang H, Wang M, Fourier domain OCT measurement of macular, macular ganglion cell complex, and peripapillary RNFL thickness in glaucomatous Chinese eyes: Eur J Ophthalmol, 2012; 22; 972-79
22. Seong M, Sung KR, Choi EH, Macular and peripapillary retinal nerve fiber layer measurements by spectral domain optical coherence tomography in normal-tension glaucoma: Invest Ophthalmol Vis Sci, 2010; 51; 1446-52
Tables
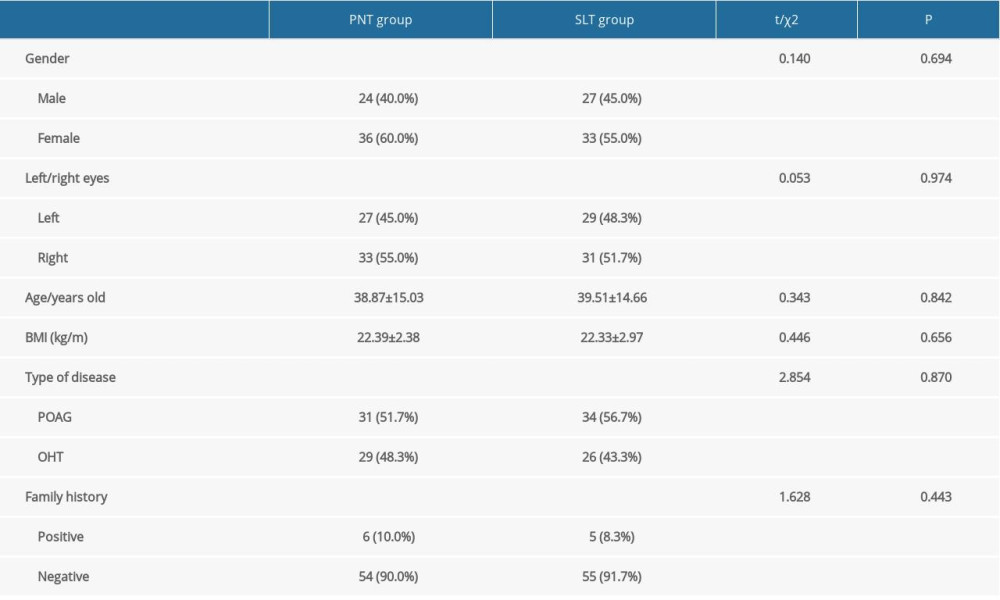 Table 1. Characteristics of the studied population in the 2 groups.
Table 1. Characteristics of the studied population in the 2 groups.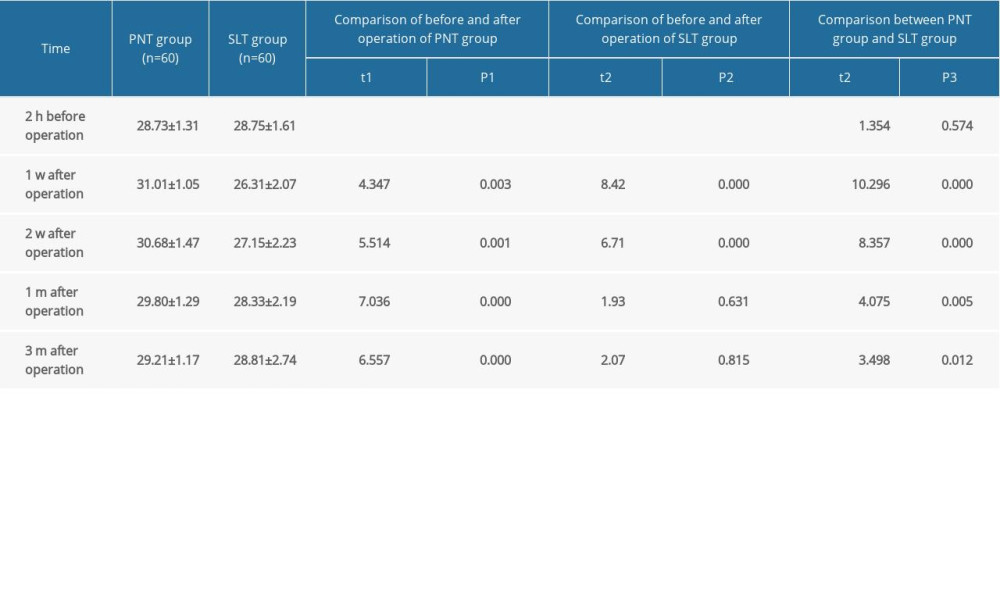 Table 2. Changes of anterior chamber angle opening range before and after surgery (χ̄±s, degree).
Table 2. Changes of anterior chamber angle opening range before and after surgery (χ̄±s, degree).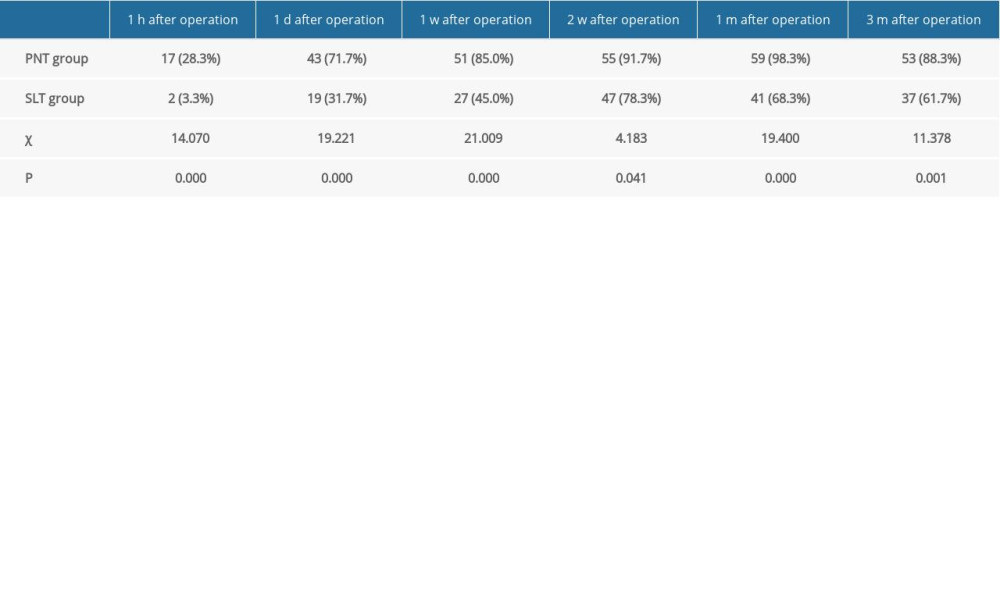 Table 3. Effective rate at different timepoints after surgery [eye (%)].
Table 3. Effective rate at different timepoints after surgery [eye (%)].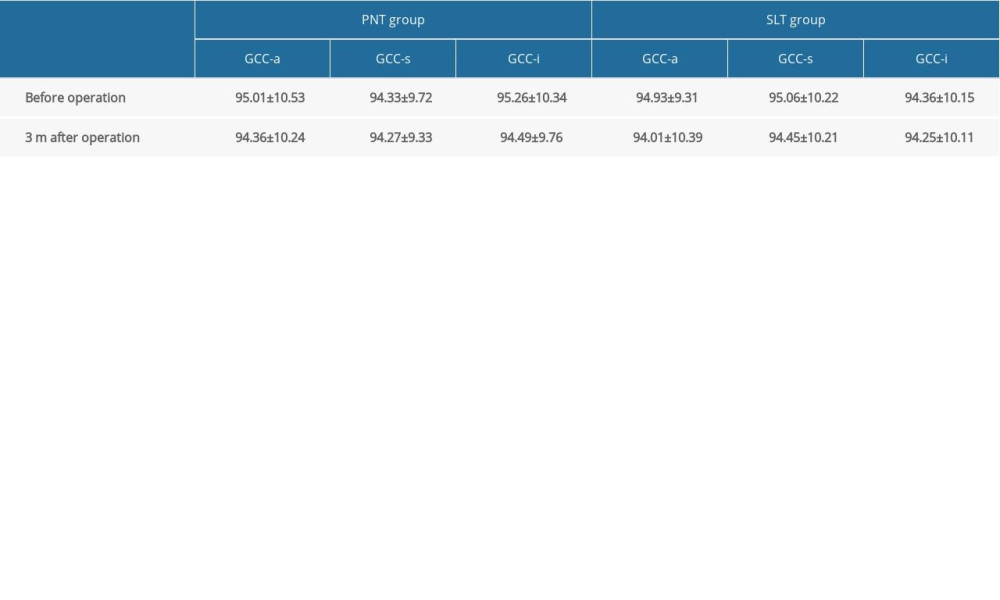 Table 4. GCC thickness in different areas of macular area before and after surgery (χ̄±s, μm).
Table 4. GCC thickness in different areas of macular area before and after surgery (χ̄±s, μm).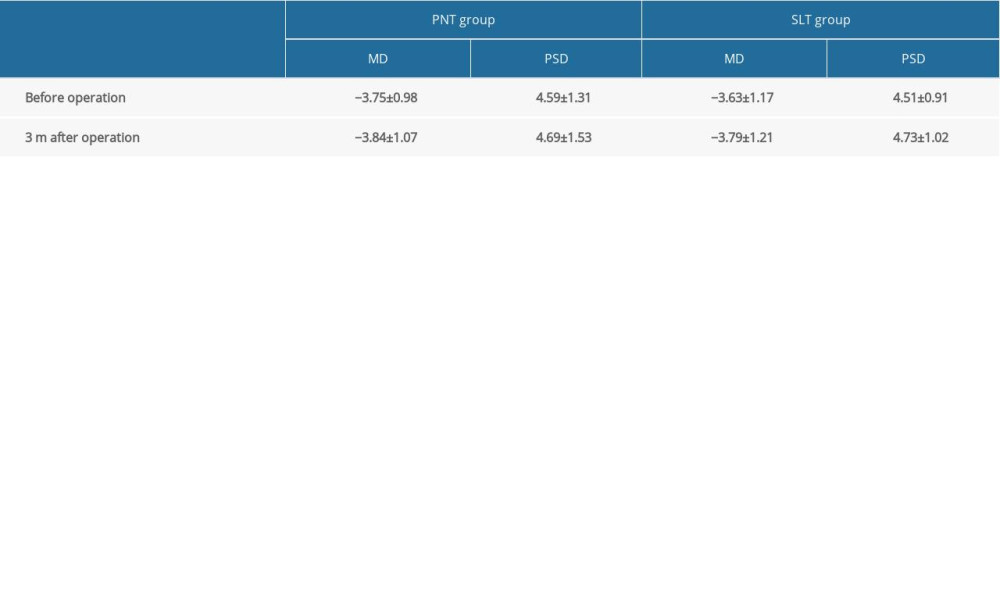 Table 5. Comparison of visual field before and after surgery (χ̄±s, dB).
Table 5. Comparison of visual field before and after surgery (χ̄±s, dB). Table 6. Incidence of adverse reactions and complications (eye).
Table 6. Incidence of adverse reactions and complications (eye).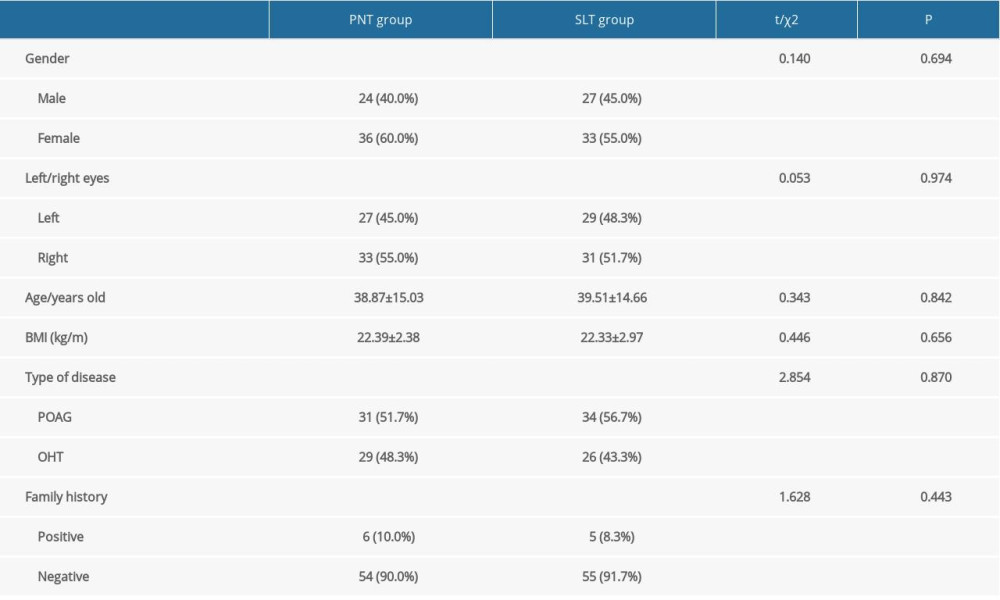 Table 1. Characteristics of the studied population in the 2 groups.
Table 1. Characteristics of the studied population in the 2 groups.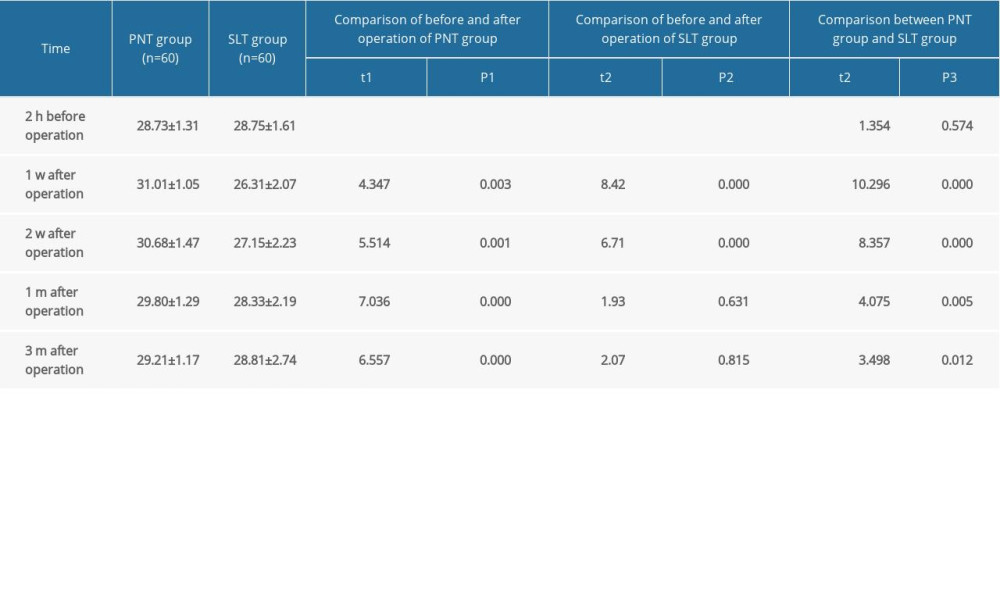 Table 2. Changes of anterior chamber angle opening range before and after surgery (χ̄±s, degree).
Table 2. Changes of anterior chamber angle opening range before and after surgery (χ̄±s, degree).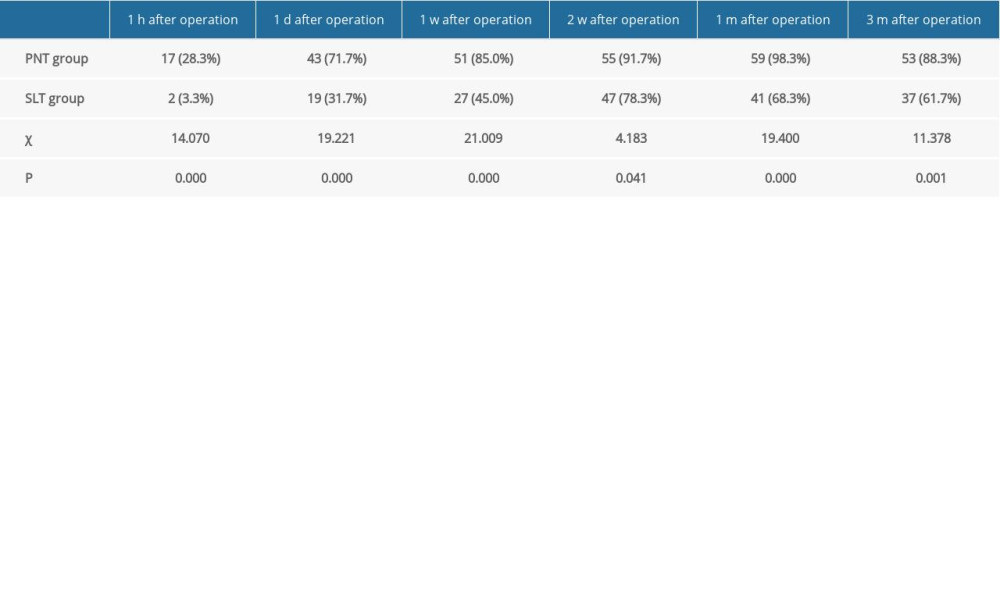 Table 3. Effective rate at different timepoints after surgery [eye (%)].
Table 3. Effective rate at different timepoints after surgery [eye (%)].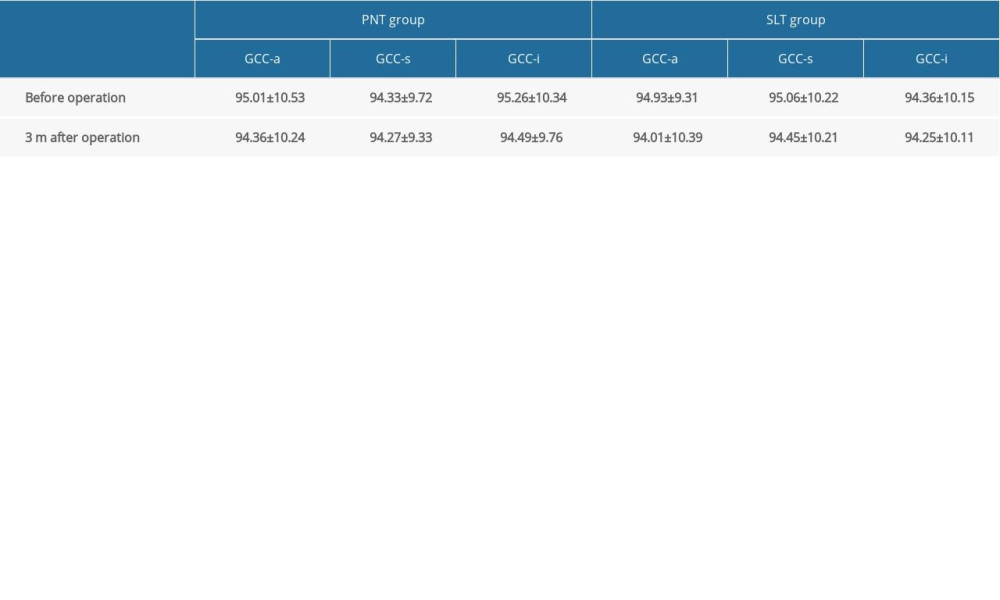 Table 4. GCC thickness in different areas of macular area before and after surgery (χ̄±s, μm).
Table 4. GCC thickness in different areas of macular area before and after surgery (χ̄±s, μm).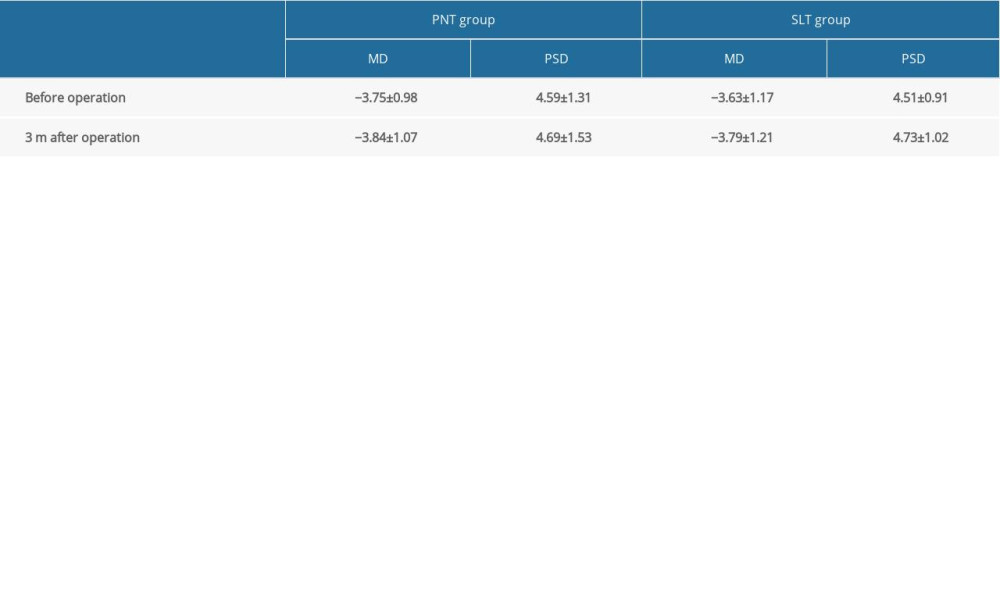 Table 5. Comparison of visual field before and after surgery (χ̄±s, dB).
Table 5. Comparison of visual field before and after surgery (χ̄±s, dB). Table 6. Incidence of adverse reactions and complications (eye).
Table 6. Incidence of adverse reactions and complications (eye). In Press
21 Mar 2024 : Meta-Analysis
Economic Evaluation of COVID-19 Screening Tests and Surveillance Strategies in Low-Income, Middle-Income, a...Med Sci Monit In Press; DOI: 10.12659/MSM.943863
10 Apr 2024 : Clinical Research
Predicting Acute Cardiovascular Complications in COVID-19: Insights from a Specialized Cardiac Referral Dep...Med Sci Monit In Press; DOI: 10.12659/MSM.942612
06 Mar 2024 : Clinical Research
Enhanced Surgical Outcomes of Popliteal Cyst Excision: A Retrospective Study Comparing Arthroscopic Debride...Med Sci Monit In Press; DOI: 10.12659/MSM.941102
06 Mar 2024 : Clinical Research
Prevalence and Variation of Medical Comorbidities in Oral Surgery Patients: A Retrospective Study at Jazan ...Med Sci Monit In Press; DOI: 10.12659/MSM.943884
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952