18 September 2021: Clinical Research
Factors Associated with Outcomes Following Salvage Surgery for Recurrent Laryngeal Cancer: A Retrospective Study of 50 Cases from a Single Center in Poland
Katarzyna Miśkiewicz-Orczyk1ABCDEFG*, Wojciech Ścierski1ABCDEFG, Grażyna Lisowska1ABCDEFG, Natalia Zięba1ABCDE, Maciej Misiołek1ABCDEDOI: 10.12659/MSM.932004
Med Sci Monit 2021; 27:e932004
Abstract
BACKGROUND: This retrospective study from a single center in Poland aimed to identify factors associated with outcomes following salvage surgery in 50 patients with recurrent laryngeal cancer.
MATERIAL AND METHODS: The study group consisted of 50 patients with recurrent laryngeal cancer after primary organ preservation treatment (12 patients after partial surgery, 30 patients after radiation therapy, and 8 patients after prior treatment using both methods). None of the patients received chemotherapy before salvage surgery. All patients with recurrence of laryngeal cancer underwent total laryngectomy with elective bilateral nodal surgery. Local and/or nodal recurrence was considered the failure of primary organ preservation treatment. Efficacy of treatment was assessed in relation to overall survival (OS), disease-free survival (DFS), local control (LC), and locoregional control (LRC).
RESULTS: Treatment results showed a poor prognosis in patients with local and/or nodal recurrence of laryngeal cancer. In the study group, the updated 5-year rates were as follows: OS rate of 26%; DFS rate of 25%; LC rate of 44%; and LRC rate of 39%. Univariate analysis showed that the stage before primary treatment was a predictive factor of OS (P=0.012).
CONCLUSIONS: The findings from this retrospective study of 50 patients with recurrent laryngeal carcinoma showed that salvage surgery following organ preservation treatment resulted in a 5-year OS rate of 26%.
Keywords: Laryngeal Neoplasms, Head and Neck Neoplasms, Laryngectomy, Treatment Refusal, Female, Humans, Larynx, Poland, Salvage Therapy, Survival Rate
Background
Treatment of patients with recurrent laryngeal cancer after the failure of conservative treatment is a serious diagnostic and therapeutic problem [1]. It is possible that a growing number of supporters of conservative treatment contribute to this phenomenon. Conservative treatment helps preserve the function of the larynx [2]; however, the consequences of decisions made at the onset of treatment should be considered since they significantly affect patients’ condition and survival [3]. Even many years of experience in patient enrollment for appropriate therapy of laryngeal cancer does not guarantee success of treatment, and therapeutic decisions are associated with a high risk to the health and survival of patients. Patients with laryngeal cancer constitute a group of patients in whom the prognosis has not improved despite the introduction of many modern treatment methods over the last 30 years [4]. The 5-year survival rate in patients undergoing salvage surgery after failed conservative treatment of laryngeal cancer ranges from 16% to 60% [5–8]. For example, Sullivan et al reported that 5-year overall survival (OS) rates were not significantly different between primary total laryngectomy and salvage total laryngectomy [9]. Other authors indicated worse treatment outcomes in patients with recurrent laryngeal cancer, compared with those primarily treated with organ preservation. Esteller et al reported a 5-year survival rate of 34% in a group of 32 patients [10]. Weiss et al observed a 5-year OS rate of 39.4%, disease-specific survival (DSS) rate of 44.6%, and locoregional control (LRC) rate of 68.8% in a group of 54 patients with advanced tumors treated by salvage total laryngectomy [6]. Similar results were reported by Li et al in a group of 28 patients in the advanced-stage group after salvage surgery: LRC rate of 70% and 5-year DSS rate of 55.2%. They also noticed that total laryngectomy was an effective treatment method of recurrent laryngeal cancer in carefully selected patients [7]. Scharph et al obtained a 2-year OS rate of 65% in patients after salvage laryngectomy and noticed that sarcomatoid pathology, lymphovascular space invasion, and an advanced initial stage before salvage treatment were associated with inferior disease-free survival (DFS) [11].
Several important factors influence such a large discrepancy in results, including that few studies have described the results of treatment failure and single-center analyses are conducted on small groups of patients. Therefore, in this this retrospective study from a single center in Poland, we aimed to identify factors associated with outcomes following salvage surgery in 50 patients with recurrent laryngeal cancer.
Material and Methods
STATISTICAL ANALYSIS:
The Kaplan-Meier method was used to calculate survival curves, taking into account patients lost to follow-up [14]. The analysis allowed for the determination of the percentage of patients in whom a particular event occurred, including patients lost to follow-up and the time to event. The level of statistical significance was P≤0.05. The variables which did not reach statistical significance but revealed some statistical trend were considered in the multivariate analysis, and hence the P value of ≤0.1 was used instead of P≤0.05. To identify patient and tumor factors predictive of survival outcome, the following variables were analyzed in univariate analysis using the Cox proportional hazard test: age, initial T and N stage, grading, and staging. Multivariate analysis was not attempted because of the small number of patients involved.
Results
Men constituted the majority (94%) of 50 patients, and the mean age of the study group was 60 years. In the group of 20 patients after primary partial surgery, all 12 patients with recurrence underwent laser type V cordectomy (Table 1). The other 8 patients underwent partial surgery with subsequent adjuvant radiotherapy (postoperative adjuvant radiotherapy was used in the dose of 45 to 50 Gy, and all patients who qualified for postoperative irradiation had risk factors ≥T3, N+, or R1 resection). In the group of 30 patients who were previously primarily treated with radiotherapy, conformal radical radiation therapy of 66 to 72 Gy was administered. None of the patients underwent chemotherapy before salvage surgery because radiotherapy alone was the standard of treatment that was an alternative to surgery during the years of the study.
In all patients, salvage total laryngectomy with bilateral neck dissection was performed. The procedure was elective in patients without clinical signs of metastases to the neck lymph nodes (74%) and selective in the remaining patients (26%) (Table 2). In all patients, squamous cell carcinoma was detected in postoperative laryngeal specimens. In 7 patients, postoperative surgical margins in the postoperative specimens were positive (14%). Postoperative pharyngocutaneous fistula occurred in 24 patients (48%). All pharyngocutaneous fistulas were treated conservatively.
The characteristics of clinical factors in the study group that were related to the condition before primary oncological treatment showed that the largest group (68%) included patients with locally advanced cancer (cT3) without nodal metastases at the time of cancer diagnosis (cN0: 74% of patients). Cancer was primarily located in the epiglottis in 38% of patients, whereas, in 36% of patients, it was located in the epiglottis and glottis. Patients with clinical stage III cancer comprised more than 50% of the study group before primary treatment (Table 2).
In the study group, the updated 5-year OS rate was 26% (Figure 1), updated 5-year DFS rate was 25% (Figure 2), and updated 5-year LC rate was 44% (Figure 3), whereas the updated 5-year LRC rate was 39% (Figure 4).
Univariate analysis showed that only stage before primary treatment was a predictive factor of OS (
Discussion
The results of our study showed that the prognosis of patients undergoing salvage surgery after failed conservative treatment of laryngeal cancer was highly unsatisfactory. Salvage surgery following conservative treatment resulted in a 5-year OS rate of 26% and a 5-year LRC rate of 39%.
An important issue that can affect the discrepancy of treatment results is the fact that the study groups are usually heterogeneous and comprise patients after failure of radiation therapy and surgical conservative treatment of laryngeal cancer, and patients having undergone both treatment methods. Our study is no exception in this respect. Similarly, Józefowicz-Korczyńska et al reported a 5-year OS rate of 39% in a group of 58 patients with failed radiation therapy and surgical conservative treatment of laryngeal cancer combined with postoperative radiation therapy [15]. Djordjevic et al divided patients into 2 groups – patients with recurrence after radiotherapy and those with recurrence after previous surgical conservative treatment of laryngeal cancer – and reported 5-year OS rates of 27% and 33%, respectively [16]. Our treatment results of patients who underwent radical radiotherapy as the primary treatment method are in line with some studies in the literature. Holsinger et al reported a total mortality of 73% in a group of 73 patients who underwent total laryngectomy after failed radiation therapy [17]. A similar analysis was conducted by Parsons et al who observed a 5-year OS of 29% following radiation failure in squamous cell carcinoma of the supraglottic larynx [18].
Compared with our study, Maj et al and Żyłka et al reported poorer results. They analyzed a heterogenous groups of patients, including patients undergoing salvage therapy as a result of past failed treatment related to laryngeal cancer, and observed 5-year survival rates of 11% and 13%, respectively [19,20]. Young et al described the results in a group of patients with local recurrence after surgical conservative treatment of laryngeal cancer and reported a mortality rate of 85% [21].
There are several multi-center studies with larger groups of patients with better results than ours. For instance, Francis et al analyzed a large heterogeneous group of 913 patients after failed consecutive treatment of laryngeal cancer. The 5-year post-recurrence survival rate for laryngeal cancer patients was 41%, which is a good result considering such a cohort of patients. They showed that patients with glottic cancer had the best post-recurrence life expectancy. These results were probably influenced by the fact that such patients accounted for nearly 65% of the whole study group [22]. Better results were demonstrated by Dequanter et al who reported a 5-year OS rate of 40% in a group of 75 patients treated after radical radiotherapy [23].
Lyhne et al analyzed a large group comprised of 1511 patients with recurrent laryngeal cancer after radiation therapy in Denmark between 1971 and 2011. The comparison of the study results between the 1970s and the first decade of the 21st century showed a 5-year survival rate of 68% between 2000 and 2011 [24]. Other authors also obtained better results than those of our present study [25–29].
Of note, statistical analyses often include patients with locally advanced cancer (cT1 and cT2) at the time of initial diagnosis. In those patients, the prognosis after salvage surgery is better, which corresponds to a higher 5-year survival rate in the whole study group. For instance, Mimica et al reported a 5-year DSS rate of 57% in the group of patients undergoing salvage surgery for recurrent laryngeal cancer. However, early stage (I/II) disease was identified in 72% of patients at initial diagnosis, which improved the prognosis [27]. Similarly, Ganly et al reported an OS rate of 50% in the group of patients with early-stage squamous cell carcinoma of the glottic larynx who underwent total laryngectomy after radiation therapy [30]. Importantly, Cheraghlou et al showed that clinical outcomes were similar to those of patients undergoing salvage total laryngectomy in patients who experienced recurrence after radiation for T1/T2 laryngeal cancer and underwent conservation salvage laryngeal surgery [31]. In the present study, only 2 patients presented with locally advanced laryngeal cancer (cT2), and the largest group (68%) was comprised of patients staged cT3. In our study, poor survival and cure rates were mainly due to the fact that the study group was comprised mostly of patients staged III/IVa (only 1 patient was stage II at diagnosis). The selection of the study group had a significant impact on the outcomes and prognosis of patients. None of our patients underwent partial salvage surgery, which was due to the stage of the disease at the time of recurrence.
The statistical analyses of studies are frequently based on a short follow-up (2–3 years), which automatically improves treatment outcomes. For example, Scharph et al observed a 2-year OS rate of 65% and LRC rate of 21% in patients after salvage laryngectomy [11]. De Virgilio et al reported a 3-year OS rate of 38% in patients who had undergone supracricoid laryngectomy and of 52% in patients after cordectomy [32]. Moreover, Korolkowa et al observed a 3-year OS rate of 56% in patients after failed treatment of laryngeal cancer [33]. De Ridder et al reported a 2-year OS rate of 31% in patients with recurrent laryngeal cancer after chemoradiotherapy [34]. The results of Aydil et al showed a 3-year OS rate of 19% in patients with recurrent laryngeal cancer after chemoradiotherapy [35]. Of note, in our study, we based our treatment outcomes on 5-year survival and control rates.
It should be added that local and nodal staging at the time of cancer diagnosis is one of the factors affecting the results of salvage surgery in patients with recurrence after oncological treatment [5,8,16,20,25,27,36,37]. For example, Davidson et al reported a 3-year OS rate of only 22% in 108 patients with advanced laryngopharyngeal carcinoma who underwent salvage treatment after failed radiation therapy [36]. Also, Elbers et al observed that salvage total laryngectomy in patients with recurrence following radiotherapy or chemoradiation resulted in a 5-year OS rate of 37% [38]. Putten et al reported a 5-year OS rate of 27% in 60 patients with advanced laryngeal and hypopharyngeal carcinoma [39].
The comparison of the results with those reported in the literature is difficult and does not always allow for drawing reliable conclusions. Also, it is important to note that treatment of local recurrence of laryngeal cancer poses a real challenge to the surgeon. Total laryngectomy is often the only chance for survival for this group of patients. It should be emphasized that a small sample size, use of a single center, and dependence on the information available from medical records were significant limitations of this study that may have affected our results.
Conclusions
The findings from this retrospective study of 50 patients with recurrent laryngeal carcinoma showed that salvage surgery following conservative treatment resulted in a 5-year OS of 26%.
Figures
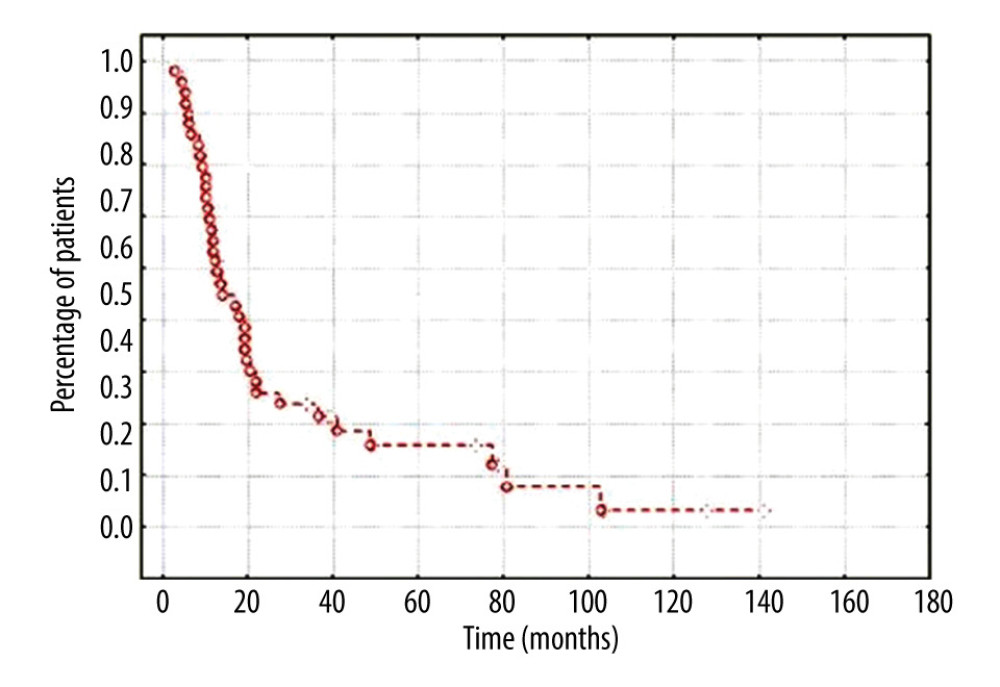 Figure 1. The updated 5-year overall survival rate in the group of 50 patients with recurrent laryngeal cancer.
Figure 1. The updated 5-year overall survival rate in the group of 50 patients with recurrent laryngeal cancer. 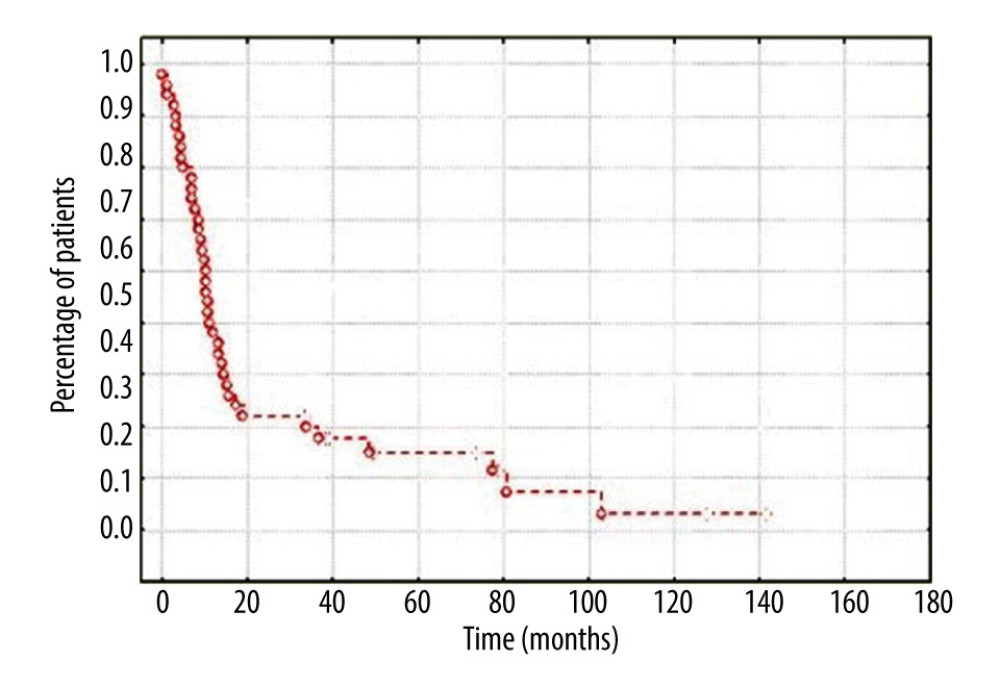 Figure 2. The updated 5-year disease-free survival rate in the group of 50 patients with recurrent laryngeal cancer.
Figure 2. The updated 5-year disease-free survival rate in the group of 50 patients with recurrent laryngeal cancer. 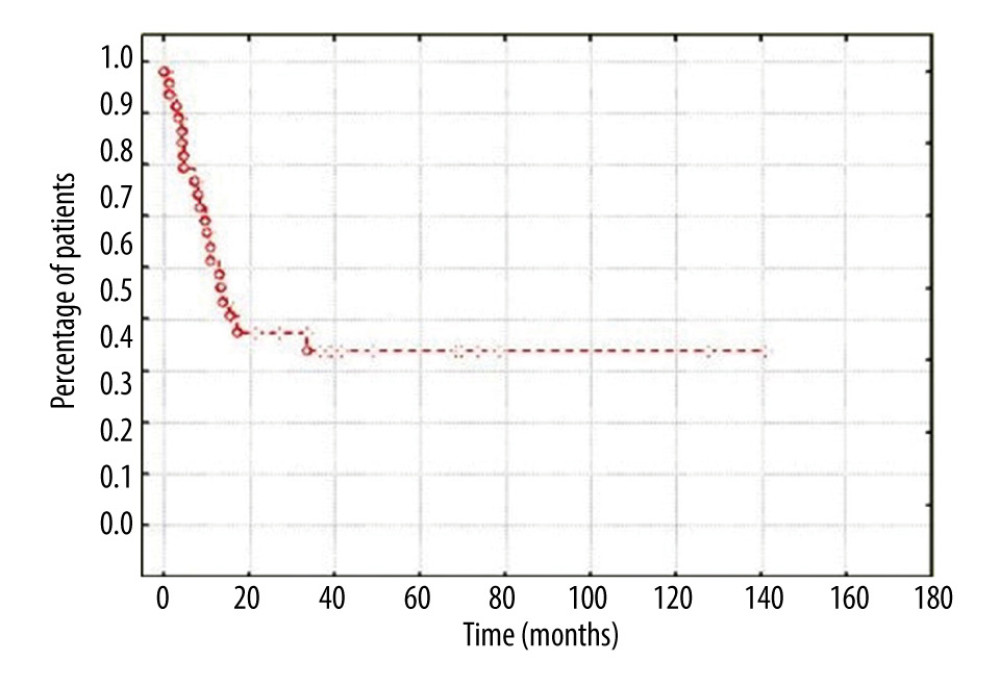 Figure 3. The updated 5-year local control rate in the group of 50 patients with recurrent laryngeal cancer.
Figure 3. The updated 5-year local control rate in the group of 50 patients with recurrent laryngeal cancer. 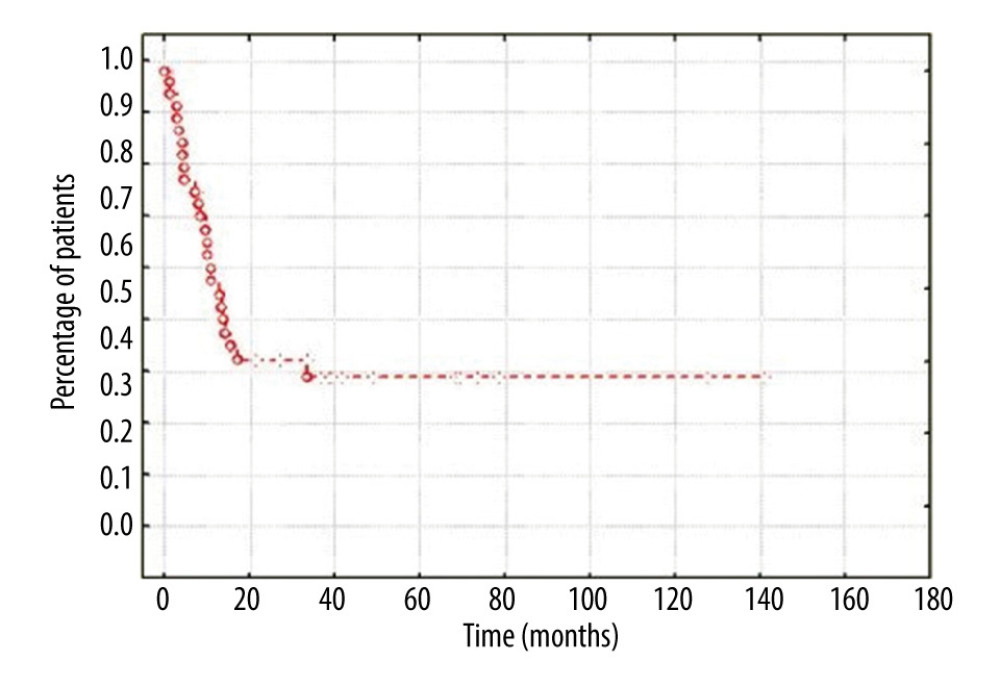 Figure 4. The updated 5-year locoregional control rate in the group of 50 patients with recurrent laryngeal cancer.
Figure 4. The updated 5-year locoregional control rate in the group of 50 patients with recurrent laryngeal cancer. References
1. Silverman DA, Puram SV, Rocco JW, Salvage laryngectomy following organ-preservation therapy – an evidence-based review: Oral Oncol, 2019; 88; 137-44
2. Forastiere AA, Weber RS, Trotti A, Organ preservation for advanced larynx cancer: Issues and outcomes: J Clin Oncol, 2015; 33(29); 3262-68
3. Chawla S, Carney AS, Organ preservation surgery for laryngeal cancer: Head Neck Oncol, 2009; 1; 12
4. Bozec A, Culié D, Poissonnet G, current role of total laryngectomy in the era of organ preservation: Cancers (Basel), 2020; 12(3); 584
5. Sessions DG, Lenox J, Spector GJ, Supraglottic laryngeal cancer: Analysis of treatment results: Laryngoscope, 2005; 115(8); 1402-10
6. Weiss BG, Bertlich M, Canis M, Ihler F, Transoral laser microsurgery or total laryngectomy for recurrent squamous cell carcinoma of the larynx: Retrospective analysis of 199 cases: Head Neck, 2017; 39(6); 1166-76
7. Li M, Lorenz RR, Khan MJ, Salvage laryngectomy in patients with recurrent laryngeal cancer in the setting of nonoperative treatment failure: Otolaryngol Head Neck Surg, 2013; 149(2); 245-51
8. Piazza C, Peretti G, Cattaneo A, Salvage surgery after radiotherapy for laryngeal cancer: From endoscopic resection to open-neck partial and total laryngectomies: Arch Otolaryngol Head Neck Surg, 2007; 133(10); 1037-43
9. Sullivan CB, Ostedgaard KL, Al-Qurayshi Z, Primary laryngectomy versus salvage laryngectomy: A comparison of outcomes in the chemoradiation era: Laryngoscope, 2020; 130(9); 2179-85
10. Esteller E, Vega MC, López M, Salvage surgery after locoregional failure in head and neck carcinoma patients treated with chemoradiotherapy: Eur Arch Otorhinolaryngol, 2011; 268(2); 295-301
11. Scharpf J, Ward M, Adelstein D, Elucidation of salvage laryngectomy pathologic and clinical variables to guide further treatment intensification investigation: Laryngoscope, 2018; 128(4); 823-30
12. Edge SB, Compton CC: Ann Surg Oncol, 2010; 17(6); 1471-74
13. Remacle M, Haverbeke Ch, Eckel H, Proposal for revision of the European Laryngological Society classification of endoscopic cordectomies: Eur Arch Otorhinolaryngol, 2007; 264(5); 499-504
14. Kaplan El, Meier P, Nonparametric estimation from incomplete observations: J Am Stat Assoc, 1958; 53; 457-81
15. Józefowicz-Korczyńska M, Pietruszewska W, Łukomski M, Wyniki chirurgicznego leczenia chorych z rakiem krtani po radioterapii: Otolaryngol Pol, 2000; 32; 248-51 [in Polish]
16. Djordjević V, Milovanović J, Petrović ZRadical surgery of the malignant laryngeal tumors: Acta Chir Iugosl, 2004; 51(1); 31-35 [in Serbian]
17. Holsinger FC, Funk E, Roberts DB, Conservation laryngeal surgery versus total laryngectomy for radiation failure in laryngeal cancer: Head Neck, 2006; 28(9); 779-84
18. Parsons JT, Mendenhall WM, Stringer SP, Salvage surgery following radiation failure in squamous cell carcinoma of the supraglottic larynx: Int J Radiat Oncol Biol Phys, 1995; 32(3); 605-9
19. Maj P, Jaworowska E, Ziętek E, Wyniki leczenia chirurgicznego zaawansowanych przypadków (T3, T4) raka krtani: Otolaryngol Pol, 2000; 31; 228-31 [in Polish]
20. Żyłka S, Bień S, Niepowodzenia leczenia chirurgicznego i skojarzonego (chirurgia i telegammaterapia) u chorych na raka krtani i krtaniowej części gardła leczonych na Oddziale Otolaryngologii Wojewódzkiego Szpitala Zespolonego w Kielcach w latach 1987–1997: Otolaryngol Pol, 2004; 58(2); 311-19 [in Polish]
21. Young VN, Mangus BD, Bumpous JM, Salvage laryngectomy for failed conservative treatment of laryngeal cancer: Laryngoscope, 2008; 118(9); 1561-68
22. Francis DO, Yueh B, Weymuller EA, Merati AL, Impact of surveillance on survival after laryngeal cancer in the medicare population: Laryngoscope, 2009; 119(12); 2337-44
23. Dequanter D, Lothaire P, Comblain M, Pharyngolaryngectomy for advanced and recurrent cancer: Prognostic factors and complications: Rev Laryngol Otol Rhinol, 2004; 125(2); 93-101
24. Lyhne NM, Johansen J, Kristensen CA, Pattern of failure in 5001 patients treated for glottic squamous cell carcinoma with curative intent – a population based study from the DAHANCA group: Radiother Oncol, 2016; 118(2); 257-66
25. Stoeckli SJ, Pawlik AB, Lipp M, Salvage surgery after failure on nonsurgical therapy for carcinoma of the larynx and hypopharynx: Arch Otorynolaryngol Head Neck Surg, 2000; 126; 1473-77
26. León X, Quer M, Orus C, Results of salvage surgery for local or regional recurrence after larynx preservation with induction and chemotherapy and radiotherapy: Head Neck, 2001; 23(9); 733-38
27. Mimica X, Hanson M, Patel SG, Salvage surgery for recurrent larynx cancer: Head Neck, 2019; 41(11); 3906-15
28. Fowler BZ, Muller S, Chen AY, Johnstone PAS, Factors influencing long-term survival following salvage total laryngectomy after initial radiotherapy or conservative surgery: Head Neck, 2006; 28(2); 99-106
29. Janczewski G, Osuch J, Bień S, Jegliński T, Wyniki chirurgicznego leczenia raka krtani po napromienianiu zakończonym niepowodzeniem: Otolaryngol Pol, 1986; 153-57 [in Polish]
30. Ganly I, Patel SG, Matsuo J, Results of surgical salvage after failure of definitive radiation therapy for early-stage squamous cell carcinoma of the glottic larynx: Arch Otolaryngol Head Neck Surg, 2006; 132(1); 59-66
31. Cheraghlou S, Kuo P, Mehra S, salvage surgery after radiation failure in T1/T2 larynx cancer: Outcomes following total versus conservation surgery: Otolaryngol Head Neck Surg, 2018; 158(3); 497-504
32. De Virgilio A, Greco A, Bussu F, Salvage total laryngectomy after conservation laryngeal surgery for recurrent laryngeal squamous cell carcinoma: Acta Otorhinolaryngol Ital, 2016; 36(5); 373-80
33. Korolkowa O, Osuch-Wójcikiewicz E, Operacje ratujące w zaawansowanych rakach krtani i gardła dolnego: Pol MerkLek, 2005; 19; 365-67 [in Polish]
34. de Ridder M, de Veij Mestdagh PD, Elbers JBW, Disease course after the first recurrence of head and neck squamous cell carcinoma following (chemo)radiation: Eur Arch Otorhinolaryngol, 2020; 277(1); 261-68
35. Aydil U, Akmansu M, Gümüşay Ö, Failure of concurrent chemoradiotherapy for organ preservation in laryngeal cancer: Survival outcomes and recurrence patterns: Ear Nose Throat J, 2019; 98(7); 92-96
36. Davidson J, Keane T, Brown D, Surgical salvage after radiotherapy for advanced laryngopharyngeal carcinoma: Arch Otolaryngol Head Neck Surg, 1997; 123(4); 420-24
37. Taguchi T, Nishimura G, Takahashi M, Treatment results and prognostic factors for advanced squamous cell carcinoma of the head and neck treated with salvage surgery after concurrent chemoradiotherapy: Int J Clin Oncol, 2016; 21(5); 869-74
38. Elbers JBW, Veldhuis LI, Bhairosing PA, Salvage surgery for advanced stage head and neck squamous cell carcinoma following radiotherapy or chemoradiation: Eur Arch Otorhinolaryngol, 2019; 276(3); 647-55
39. Putten L, Bree R, Doornaert PA, Salvage surgery in post-chemoradiation laryngeal and hypopharyngeal carcinoma: Outcome and review: Acta Otorhinolaryngol Ital, 2015; 35(3); 162-72
Figures
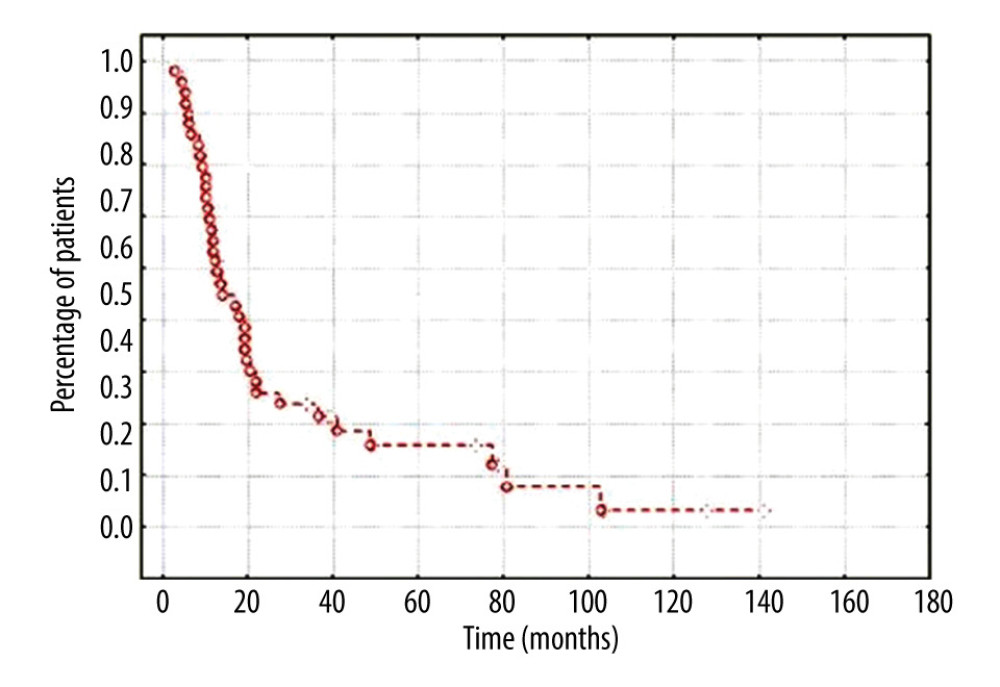 Figure 1. The updated 5-year overall survival rate in the group of 50 patients with recurrent laryngeal cancer.
Figure 1. The updated 5-year overall survival rate in the group of 50 patients with recurrent laryngeal cancer.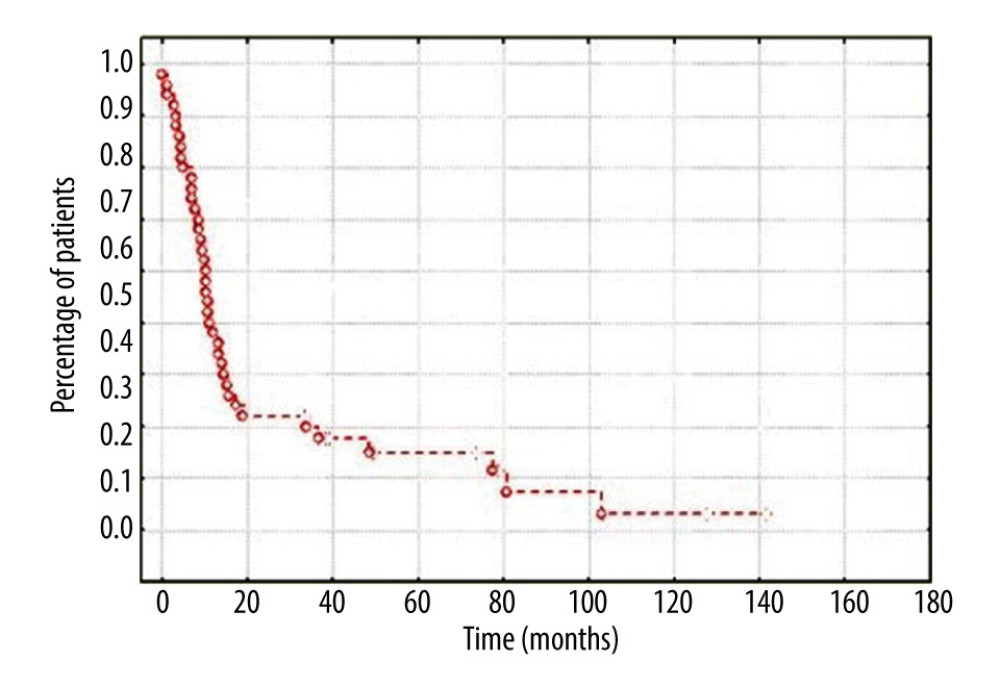 Figure 2. The updated 5-year disease-free survival rate in the group of 50 patients with recurrent laryngeal cancer.
Figure 2. The updated 5-year disease-free survival rate in the group of 50 patients with recurrent laryngeal cancer.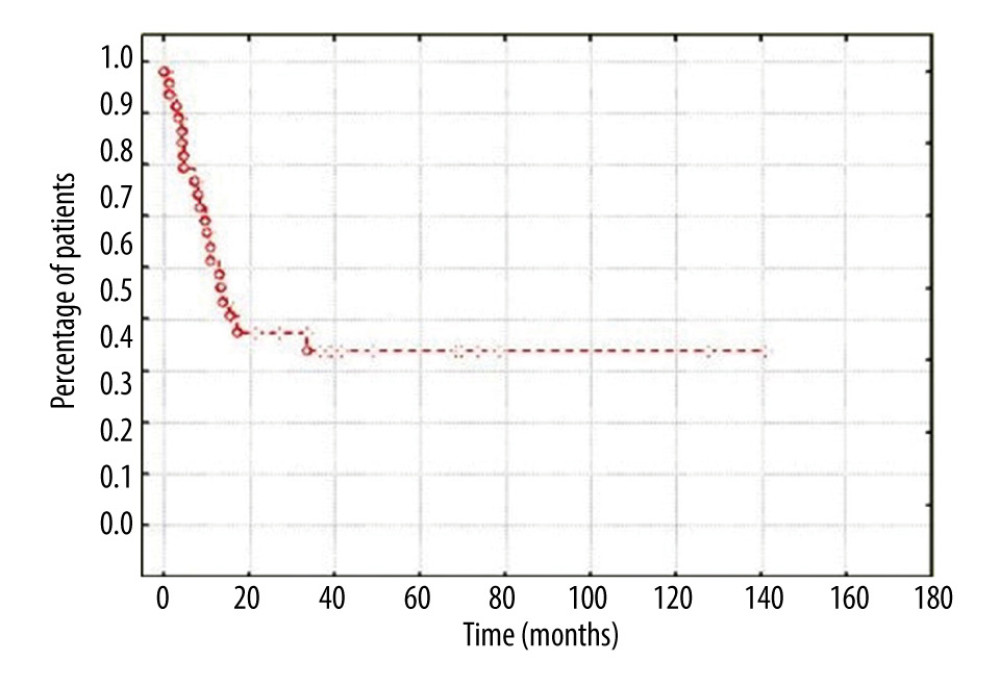 Figure 3. The updated 5-year local control rate in the group of 50 patients with recurrent laryngeal cancer.
Figure 3. The updated 5-year local control rate in the group of 50 patients with recurrent laryngeal cancer.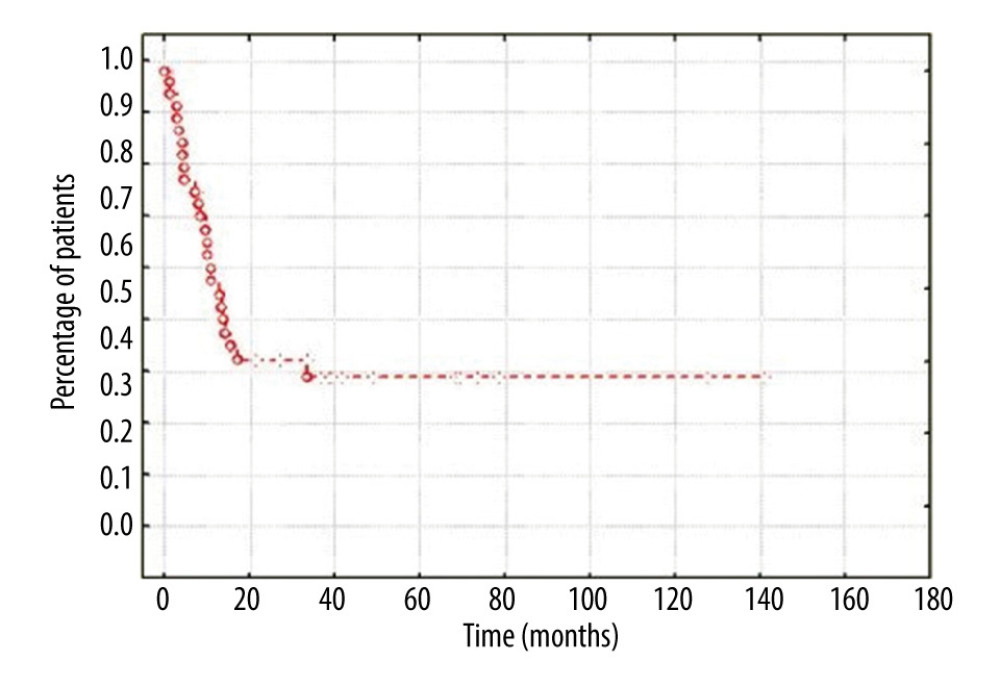 Figure 4. The updated 5-year locoregional control rate in the group of 50 patients with recurrent laryngeal cancer.
Figure 4. The updated 5-year locoregional control rate in the group of 50 patients with recurrent laryngeal cancer. Tables
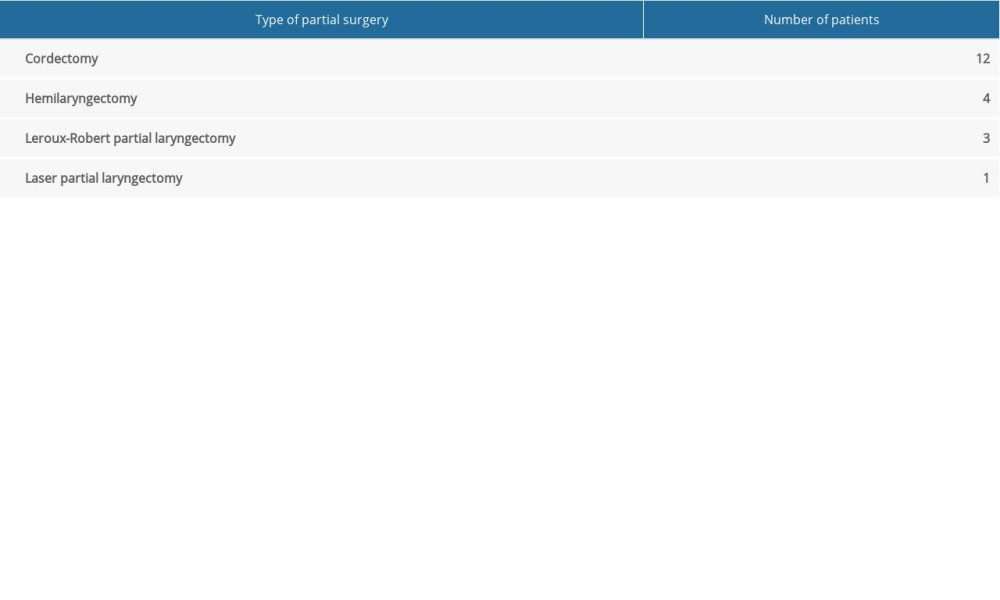 Table 1. Type of partial surgery in the group of 50 patients with primary laryngeal cancer (n=20).
Table 1. Type of partial surgery in the group of 50 patients with primary laryngeal cancer (n=20).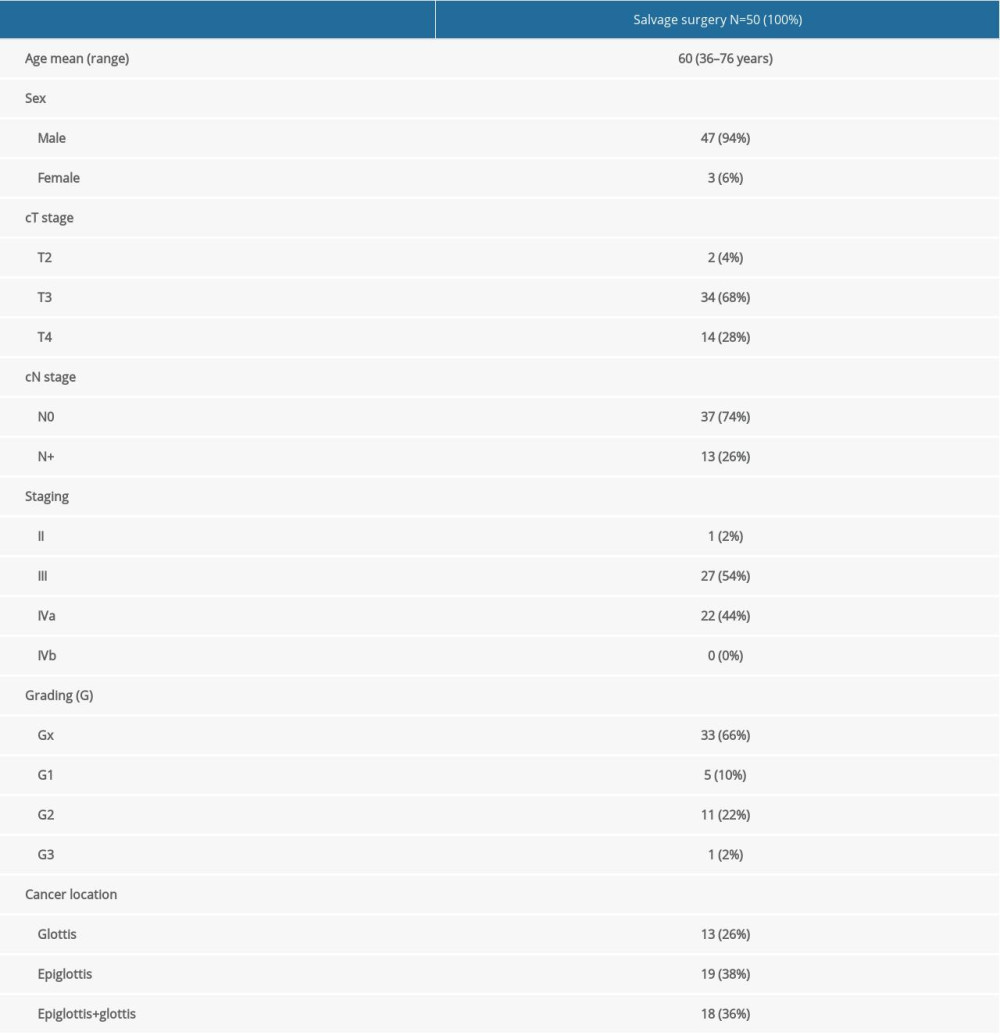 Table 2. Clinical factors in the group of 50 patients with recurrence of laryngeal cancer before conservative treatment (n=50).
Table 2. Clinical factors in the group of 50 patients with recurrence of laryngeal cancer before conservative treatment (n=50).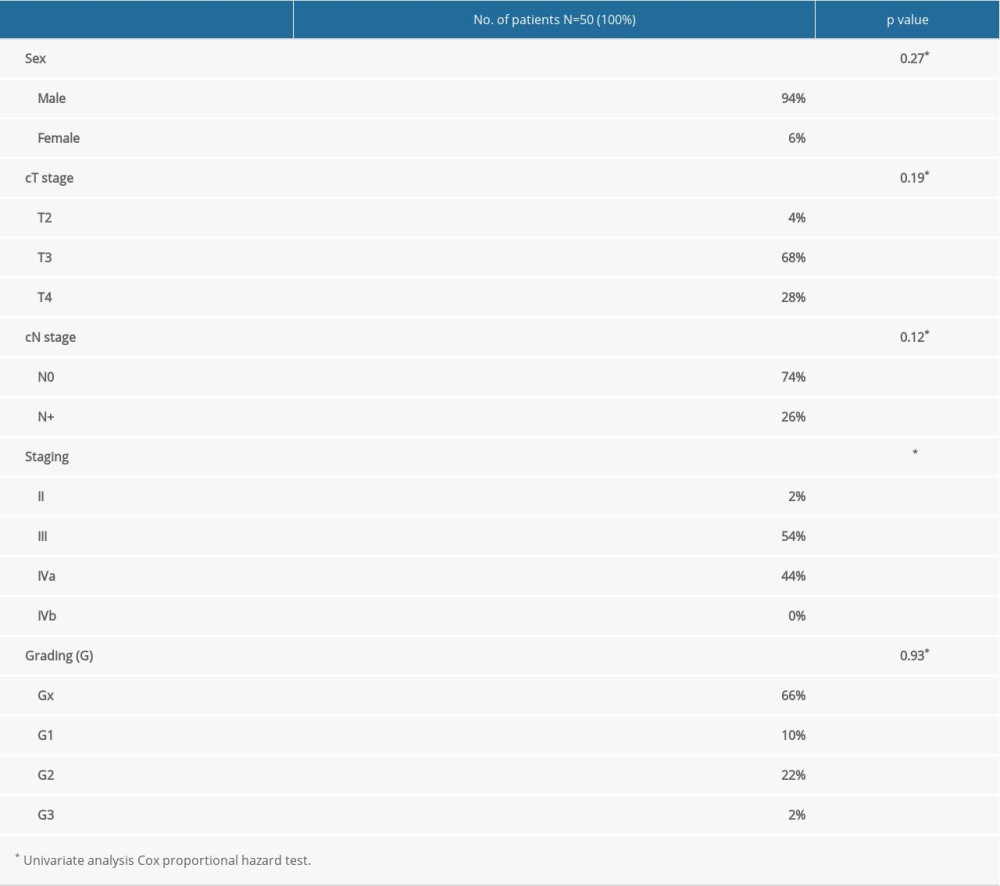 Table 3. Predictive factors of overall survival.
Table 3. Predictive factors of overall survival.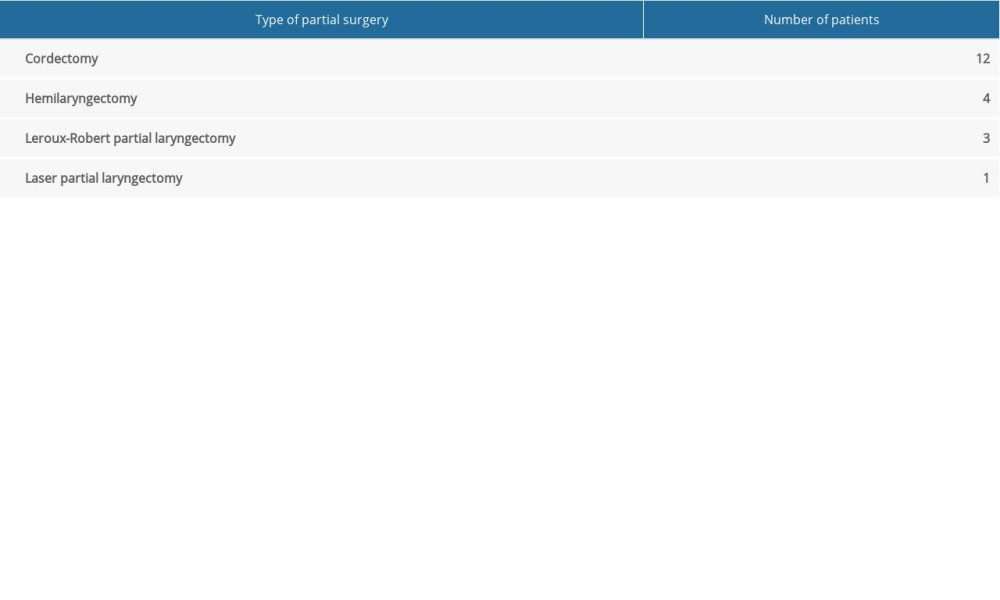 Table 1. Type of partial surgery in the group of 50 patients with primary laryngeal cancer (n=20).
Table 1. Type of partial surgery in the group of 50 patients with primary laryngeal cancer (n=20).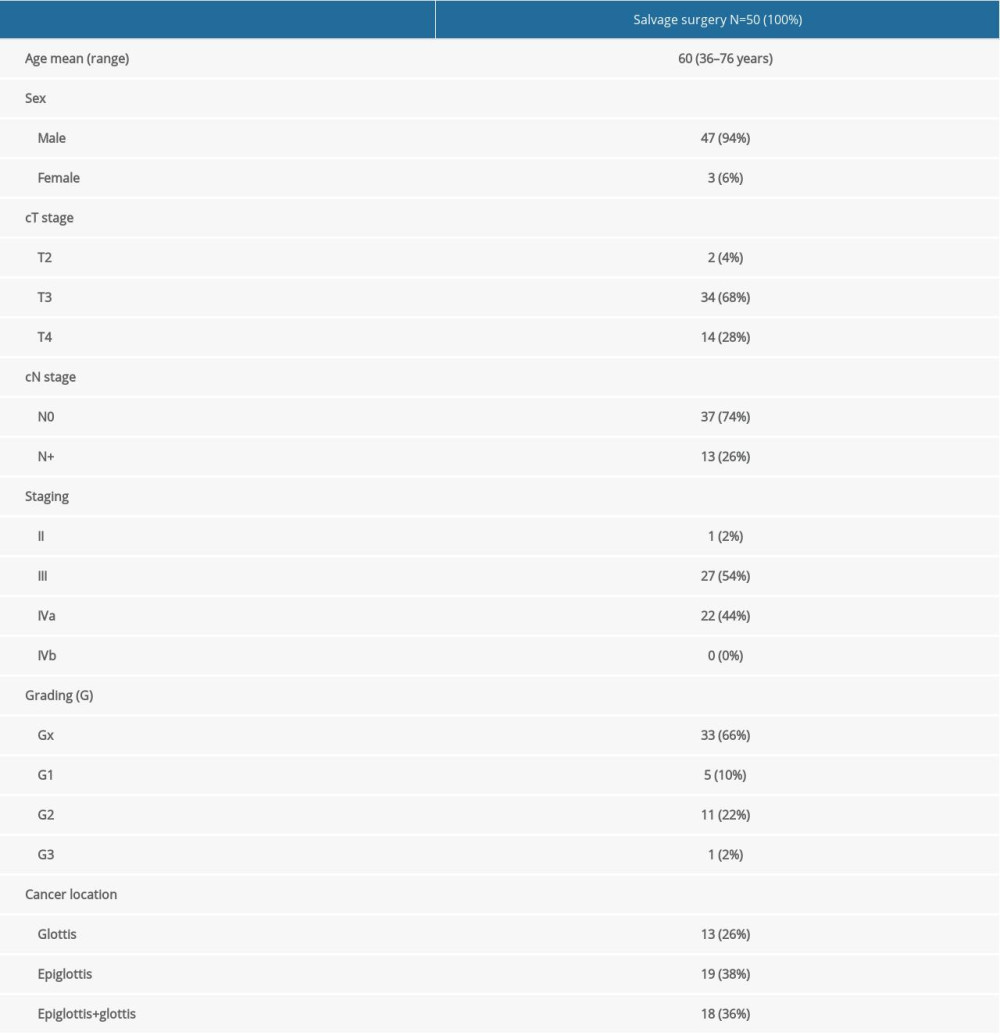 Table 2. Clinical factors in the group of 50 patients with recurrence of laryngeal cancer before conservative treatment (n=50).
Table 2. Clinical factors in the group of 50 patients with recurrence of laryngeal cancer before conservative treatment (n=50).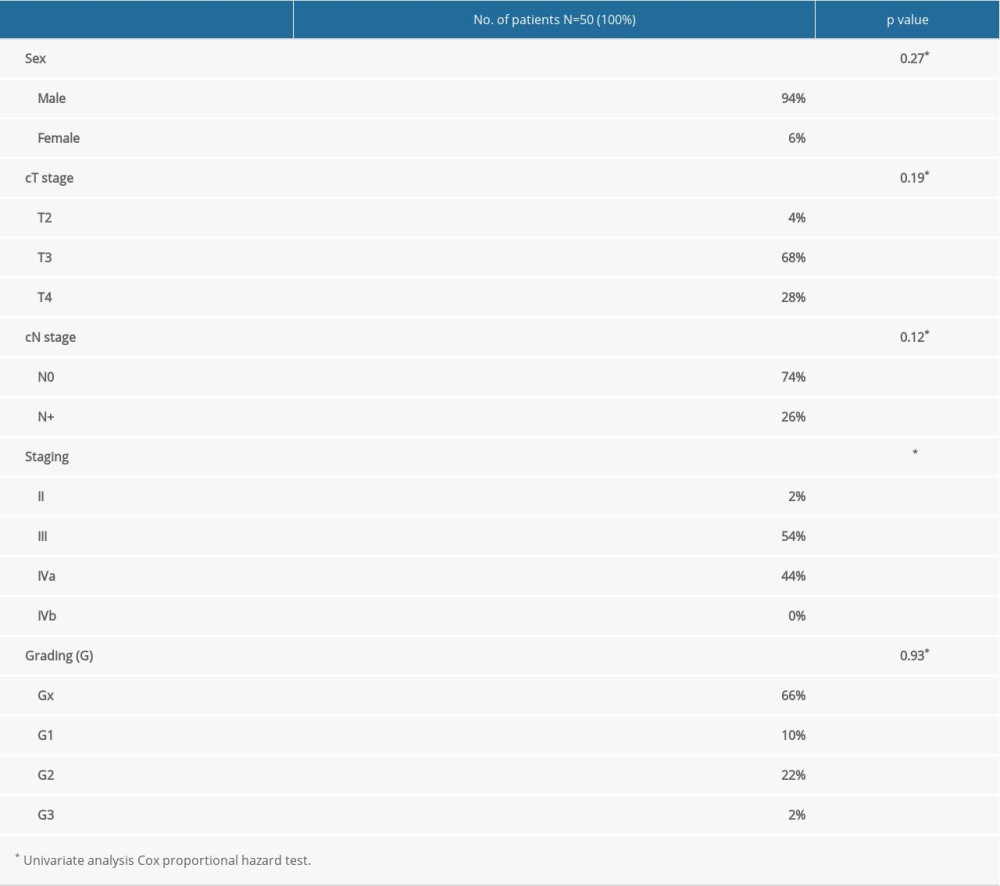 Table 3. Predictive factors of overall survival.
Table 3. Predictive factors of overall survival. In Press
06 Mar 2024 : Clinical Research
Comparison of Outcomes between Single-Level and Double-Level Corpectomy in Thoracolumbar Reconstruction: A ...Med Sci Monit In Press; DOI: 10.12659/MSM.943797
21 Mar 2024 : Meta-Analysis
Economic Evaluation of COVID-19 Screening Tests and Surveillance Strategies in Low-Income, Middle-Income, a...Med Sci Monit In Press; DOI: 10.12659/MSM.943863
10 Apr 2024 : Clinical Research
Predicting Acute Cardiovascular Complications in COVID-19: Insights from a Specialized Cardiac Referral Dep...Med Sci Monit In Press; DOI: 10.12659/MSM.942612
06 Mar 2024 : Clinical Research
Enhanced Surgical Outcomes of Popliteal Cyst Excision: A Retrospective Study Comparing Arthroscopic Debride...Med Sci Monit In Press; DOI: 10.12659/MSM.941102
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








