08 July 2021: Clinical Research
Transurethral Microwave Thermotherapy (TUMT) in the Treatment of Benign Prostatic Hyperplasia: A Preliminary Report
Roger J. Ziętek1BDF, Zbigniew M. ZiętekDOI: 10.12659/MSM.931597
Med Sci Monit 2021; 27:e931597
Abstract
BACKGROUND: One treatment option for benign prostatic hyperplasia (BPH) is transurethral microwave thermotherapy (TUMT). Unfortunately, TUMT has been increasingly marginalized recently. The aim of this study was to evaluate erectile function and urinary symptoms in patients after TUMT for BPH and compare the results with those of patients on pharmacological treatment for BPH.
MATERIAL AND METHODS: The study group consisted of 840 patients with BPH treated with TUMT and a control group consisting of 1040 patients who underwent pharmacotherapy. Erectile dysfunction was evaluated using the International Index of Erectile Function-5 questionnaire and the Individual Postoperative Erectile Assessment (IPEA) questionnaire, which was created by the authors for this study. Urinary symptoms were evaluated using the International Prostate Symptom Score (IPSS) questionnaire.
RESULTS: More than 50% of all patients experienced an improvement in urinary symptoms after TUMT, compared with only approximately 30% in the control group. Differences in each of the IPSS symptom scales between the TUMT and control groups were statistically significant (P<0.031, P<0.041, and P<0.025 for mild, moderate, and severe symptoms, respectively). Improvement in erectile dysfunction after TUMT was also statistically significant (P<0.0001, P<0.0001, P<0.05 for mild, moderate, and severe erectile dysfunction, respectively). Based on the IPEA questionnaire, approximately 24% of the TUMT group reported significant improvement in erectile function, while a decrease in erectile function was reported in the control group.
CONCLUSIONS: TUMT may still be a valuable option in the treatment of BPH. TUMT may be especially suitable for patients who expect to improve urinary symptoms without decreasing erectile function.
Keywords: conservative treatment, Penile Erection, Prostatic Hyperplasia, Transurethral Resection of Prostate, Aged, 80 and over, Hyperthermia, Induced, Microwaves
Background
There are a range of conflicting opinions on transurethral microwave thermotherapy (TUMT) in the literature, from earlier enthusiastic opinions, which even heralded the end of the epoch of transurethral resection of the prostate, to skeptical reports today [1–10]. As a result of recent opinions, the European Association of Urology (EAU) withdrew its recommendations for TUMT as a treatment option for benign prostatic hyperplasia (BPH) [1,11–15]. TUMT is one of the mildest ablative forms of minimally invasive BPH treatment, using a temperature that greatly exceeds the temperature of protein denaturation. This high temperature triggers many useful processes such as coagulation, denervation of α receptors, reduction of smooth muscle tension, and cellular apoptosis. Finally, all these processes lead to the breakdown of the cytoarchitectonics of the prostate adenoma cells and the relief of many symptoms, including lower urinary tract symptoms [3,16,17].
A disadvantage of TUMT is the need for repeating the procedure because of a relatively short period of urinary symptom improvement [3,8,18,19]. However, advantages of TUMT include no mortality, minimal morbidity, appropriateness for patients at high risk, and the ability to be performed as an outpatient procedure [18–22]. Some reports emphasize another benefit – its positive effect on erectile function [11,20].
Most patients undergoing transurethral resection of the prostate or adenomectomy report experiencing problems with erectile function (23–30). Erectile dysfunction seems to be of little importance to urologists when choosing a treatment option for BPH [4,5,15]. However, there are still some patients who expect such methods to be effective without affecting their ability to have an erection [16,31,32]. TUMT could be a suitable method for those patients. Therefore, the qualifications for thermotherapy should be redefined to include factors such as prostate size and the importance of sexual activity [11,16].
The aim of this study was to assess erectile function and urinary symptoms after TUMT for BPH and compare the results with those of patients who underwent pharmacotherapy.
Material and Methods
STATISTICAL METHODS:
All statistical analyses were done using Statistica version 13 (SoftPol, Cracow, Poland). The normality distribution of examined parameters was tested using the Shapiro-Wilk test. The Mann-Whitney test was applied for parameters without a normal distribution. The mean and standard deviation were calculated.
We hypothesized that TUMT would impact erectile function. The hypothesis was tested using the Z test for 2 independent proportions. Additionally, a 2×2 contingency table and Fisher’s exact test were applied to evaluate erectile function after surgery. The confidence interval was determined using the Clopper-Pearson interval. In all tests,
The study was approved by the Institutional Review Board (ethics board) (protocol no. WLS-1/2019).
Results
All results are presented in Tables 1–5. The sociodemographic and clinical data of patients are presented in Table 1. Table 2 shows the analysis of the IPSS results in both groups of patients. The analysis compared the results between the measurements at baseline and at the 6-month follow-up within and between the TUMT and control groups. The distribution of baseline IPSS scores in both groups was similar, indicating that the level of urinary disorders in the groups was similar. The analysis of the IPSS results at the 6-month follow-up in both groups showed a significant improvement in urinary symptoms in the TUMT group (differences in mild, moderate, and severe symptoms were statistically significant between the groups:
Results showed that the general vector of post-TUMT urinary disorders shifted toward the milder forms. Detailed analysis of each voiding disorder scale showed that the number of patients with mild symptoms increased almost 5-fold. Simultaneously, the number of patients with moderate and severe symptoms decreased; all differences were statistically significant. This comparison revealed that more than 50% of patients experienced a significant improvement in urination after TUMT. Similarly, in the control group, the improvement in urinary disorders shifted toward milder forms. However, the improvement in the control group was much smaller than that of the TUMT group and occurred in only about 34% of patients. This analysis showed that the TUMT method was more effective in improving urinary symptoms than was conservative pharmacological treatment.
Table 3 presents the analysis of the IIEF-5 results in both groups of patients, showing baseline and 6-month follow-up scores. The analysis compared the results at baseline and the 6-month follow-up between the TUMT and control group. In addition, a separate analysis compared baseline and 6-month follow-up scores within each group. As with the IPSS, the distribution of IIEF-5 scores showed no significant differences at baseline, indicating the groups were similar at baseline.
The analysis showed that TUMT significantly improved erectile function (
Table 4 presents the IPEA questionnaire results. Approximately 25% of all patients treated with TUMT (202 patients) reported an improvement in their erectile function, while in the control group there was no similar effect (
The PSA levels in the 2 groups are shown in Table 5. After 3 months, a statistically significant increase in PSA levels was observed in patients who underwent TUMT (
Discussion
Erectile dysfunction is strongly correlated with age [31–35]. The condition is correlated not only with the physiology of aging, but also with comorbidities and their treatment [31–33]. More than 70% of men over the age of 50 years have various diseases of the prostate, including BPH [6,12,43]. In the present study, erectile dysfunction occurred in over 75% of our patients. It is understood that erectile dysfunction worsens with the duration of diseases of the prostate and especially with their treatment [20,24–26]. TUMT is a non-ablative minimally invasive treatment method that can be performed in an outpatient clinic without anesthesia or other inconveniences associated with conventional surgical procedures, such as transurethral electroresection of the prostate. Our results demonstrated the beneficial effect of TUMT on urinary symptoms and erectile function. Approximately 24% of patients positively rated the effect of TUMT on erectile function and over 50% positively rated its effect on urinary symptoms. Based on epidemiological data and the data in the literature, only 20% of patients with BPH require invasive surgery, and the remainder are likely to be treated conservatively. Both the surgical procedure and drug therapy can worsen erectile function, which is difficult for some patients to accept. Therefore, an alternative treatment option for these patients should be considered. There are few studies in the literature that focused on the sexual activity of patients after TUMT. Most studies focused mainly on the aspects of urinary disorders [2,11–16,36,37], which made it difficult for us to comprehensively compare our results with those of other studies. Many studies mainly focused on the problem of urination, showing a significant advantage for transurethral electroresection over other therapies, with a therapeutic effectiveness rate on urination disorders of over 80% [9,27], while in our research the positive effects of TUMT on urinary problems was only around 50%. However, there are more optimistic reports on TUMT in the literature, in which improvement in urination was achieved in about 70% of patients [7,11,12,15,38]. Despite TUMT having some limitations, its lack of mortality and low morbidity make it an almost optimal strategy for patients with high expectations of sexual activity after the procedure [7,39,40]. Consistent with the present study, Hoffman et al did not report any serious erectile dysfunction in patients after TUMT [11,12]. Also, several authors, such as Skolarus et al and Kocznur et al, estimated a low risk ratio of 0.39 for erectile dysfunction and retrograde ejaculation after TUMT [11,36,37].
Many skeptical researchers have stopped using the TUMT method because it does not alleviate lower urinary tract symptoms as effectively as other minimally invasive methods. However, research by Maderbascher et al showed that there was an improvement in IPSS scores and no observed urethral stenosis after TUMT [41].
Even more promising reports for the TUMT method were provided by Ahmed et al, who observed improvement in the American Urological Association symptom score and in some parameters such as peak flow rate in the urodynamic study, although the level of improvement was not as high as that of electroresection of the prostate [42]. Very interesting conclusions on the use of TUMT were presented by Aagaard et al, who, based on over 12 years of observation, concluded the TUMT procedure is a strong alternative to electroresection of the prostate [43].
Arai et al showed a lower percentage of problems with maintaining an erection or retrograde ejaculation in patients after TUMT compared with those who underwent electroresection of the prostate [44]. Regarding BPH treatment, apart from the usual indications, other aspects should be taken into account, including the patient’s preferences regarding the effect of treatment on sexual functioning [42,45,46].
Conclusions
The positive effect of TUMT on urinary symptoms and erectile dysfunction may prompt some urologists and patients to choose this option. It should also be emphasized that the etiopathogenesis of erectile dysfunction improvement is not fully understood. One of many explanations that seems most reasonable is the discontinuation of pharmacotherapy, but other possibilities require further research.
Overall, TUMT appears to be an effective treatment for BPH and, based on the results of our study, does not deserve withdrawal or marginalization. The involvement of more research centers may give new impetus to the further technical development of thermotherapy and new scientific reports. All of the above may contribute to popularizing this method once again. Therefore, further studies on TUMT are needed to redefine the criteria and find its suitable place among BPH treatment options.
Tables
Table 1. Sociodemographic and clinical data of patients with benign prostatic hyperplasia in the transurethral microwave thermotherapy (TUMT) and pharmacotherapy (control) groups.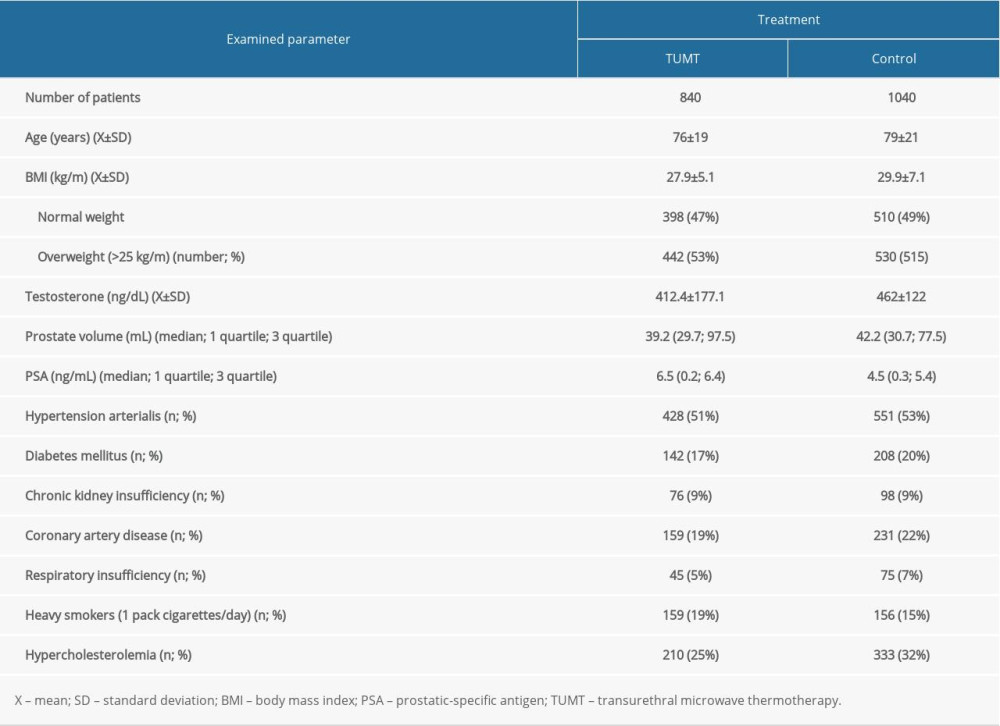 Table 2. Baseline and 6-month follow-up International Prostate Symptom Score of patients in the transurethral microwave thermotherapy (TUMT) and pharmacologic (control) groups. P, P1, P2, and P3 indicate statistical significance according to the Z test: P, baseline comparison between TUMT and control group; P1, 6-month follow-up comparison between the TUMT and control groups; P2, only within the TUMT group, baseline vs 6-month follow-up; P3, only within the control group, baseline vs 6-month follow-up.
Table 2. Baseline and 6-month follow-up International Prostate Symptom Score of patients in the transurethral microwave thermotherapy (TUMT) and pharmacologic (control) groups. P, P1, P2, and P3 indicate statistical significance according to the Z test: P, baseline comparison between TUMT and control group; P1, 6-month follow-up comparison between the TUMT and control groups; P2, only within the TUMT group, baseline vs 6-month follow-up; P3, only within the control group, baseline vs 6-month follow-up.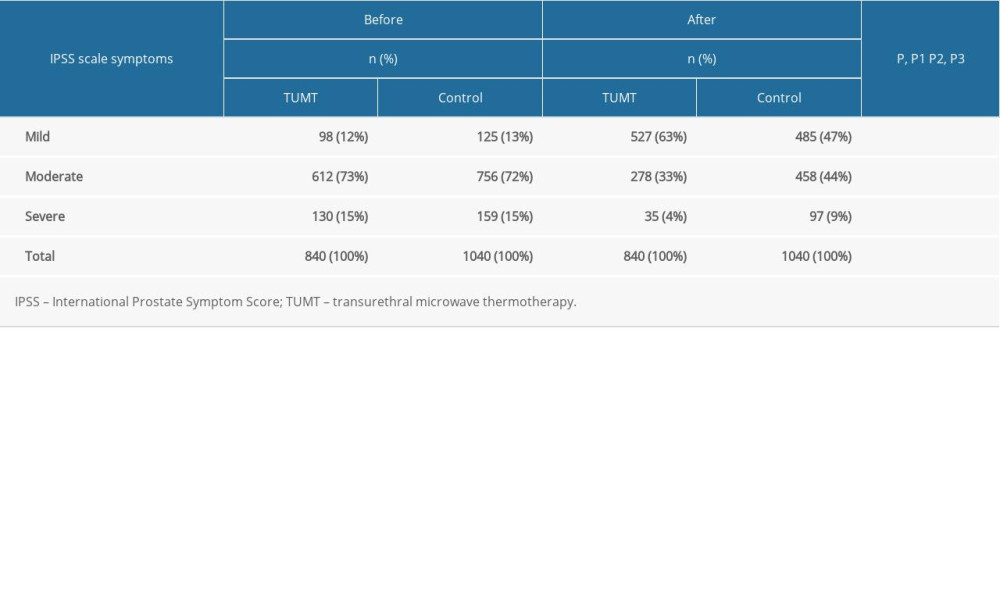 Table 3. Baseline International Index of Erectile Function-5 IIEF-5 scores and after 6 months of observations in the patients allocated in the transurethral microwave thermotherapy (TUMT) and pharmacologic (control) group. P, P1, P2, and P3 indicate statistical significance according to the Z test: P, baseline comparison between TUMT and control group; P1, 6-month follow-up comparison between the TUMT and control groups; P2, only within the TUMT group, baseline vs 6-month follow-up; P3, only within the control group, baseline vs 6-month follow-up.
Table 3. Baseline International Index of Erectile Function-5 IIEF-5 scores and after 6 months of observations in the patients allocated in the transurethral microwave thermotherapy (TUMT) and pharmacologic (control) group. P, P1, P2, and P3 indicate statistical significance according to the Z test: P, baseline comparison between TUMT and control group; P1, 6-month follow-up comparison between the TUMT and control groups; P2, only within the TUMT group, baseline vs 6-month follow-up; P3, only within the control group, baseline vs 6-month follow-up.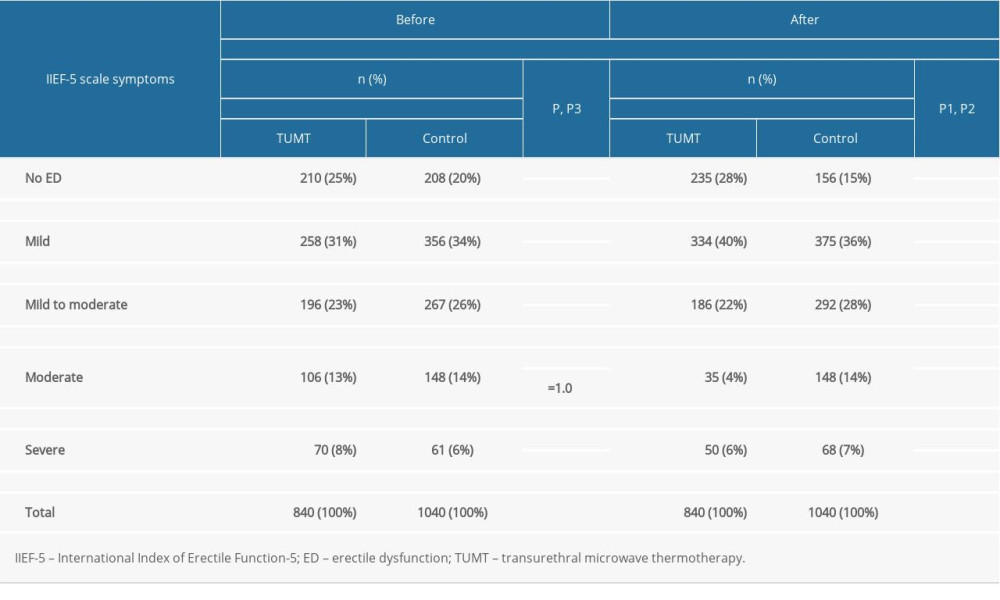 Table 4. Evaluation of erectile function using the Individual Postoperative Erectile Assessment (IPEA) questionnaire at the 6-month follow-up in the transurethral microwave thermotherapy (TUMT) and pharmacologic (control) groups. P, statistical significance according to Fisher’s exact test.
Table 4. Evaluation of erectile function using the Individual Postoperative Erectile Assessment (IPEA) questionnaire at the 6-month follow-up in the transurethral microwave thermotherapy (TUMT) and pharmacologic (control) groups. P, statistical significance according to Fisher’s exact test.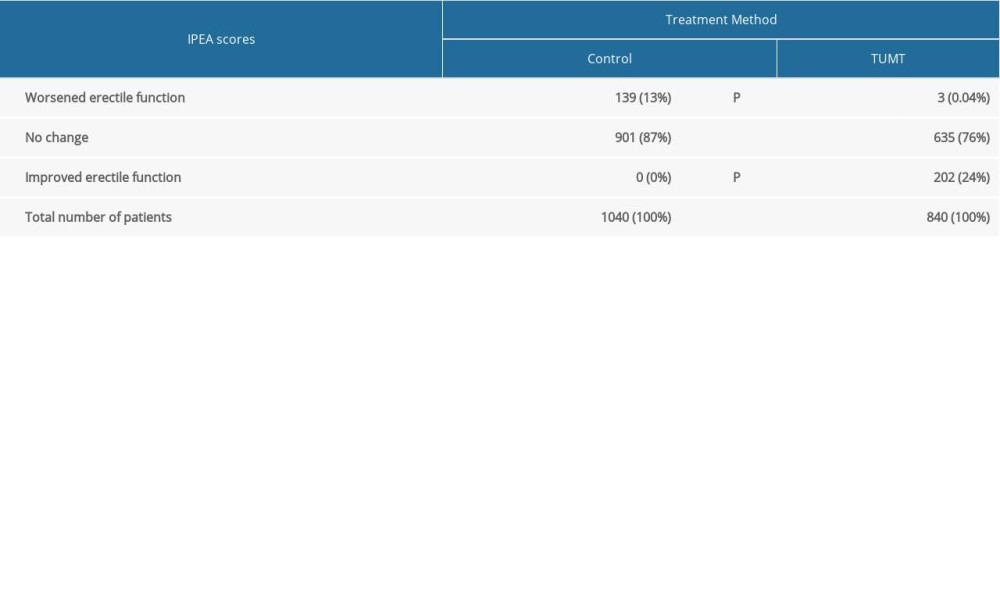 Table 5. Prostate-specific antigen concentration at the 3-month follow-up in the transurethral microwave thermotherapy (TUMT) and pharmacologic (control) groups.
Table 5. Prostate-specific antigen concentration at the 3-month follow-up in the transurethral microwave thermotherapy (TUMT) and pharmacologic (control) groups.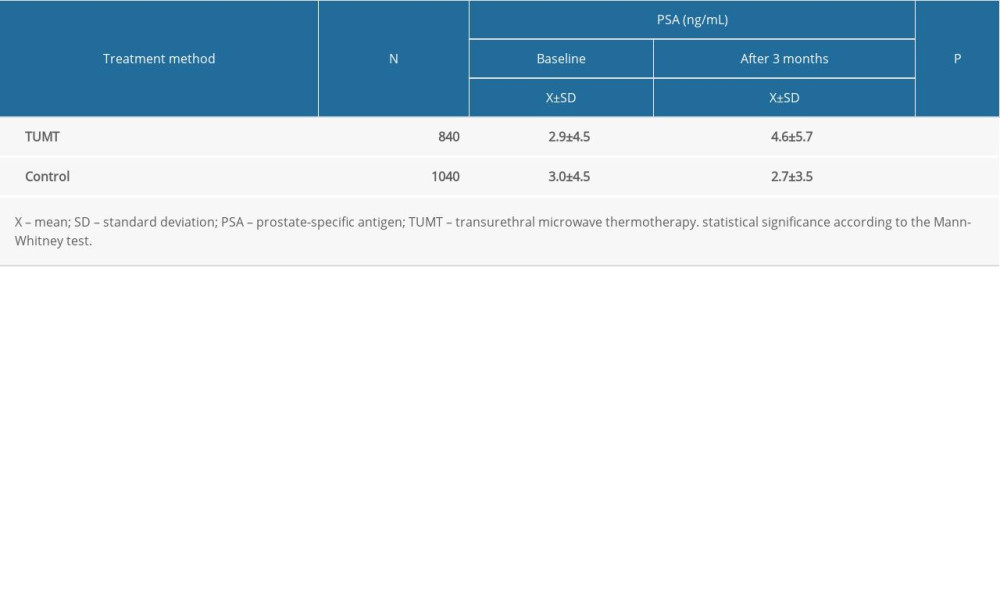
References
1. Gravas S, Melekos MD, Transurethral microwave thermotherapy: From evidence-based medicine to clinical practice: Curr Opin Urol, 2007; 17; 12-16
2. Aagaard MF, Niebuhr MH, Jacobsen JD, Transurethral microwave thermotherapy treatment of chronic urinary retention in patients unsuitable for surgery: Scand J Urol, 2014; 48; 290-94
3. Shinohara K, Thermal ablation of prostate diseases: Advantages and limitations: Int J Hyperthermia, 2004; 20; 679-97
4. Larson BT, Mynderse L, Ulchaker J, Transurethral microwave thermotherapy effectiveness in small prostates: Urology, 2006; 68; 790-94
5. de la Rosette JJ, Laguna MP, Gravas S, de Wildt MJAM, TUMT: The gold standard for minimally invasive therapies for patients with benign prostatic hyperplasia?: J Endourol, 2004; 17; 4
6. Madersbacher S, Marberger M, Is transurethral resection of the prostate still justified?: BJU Int, 1999; 83; 227-37
7. Ekstrand V, Westermark S, Wiksel H, Long-term clinical outcome of transurethral microwave thermotherapy (TUMT) 1991–1999 at Karolinska Hospital, Sweden: Scand J Urol Nephrol, 2002; 36; 113-18
8. Djavan B, Kazzazi A, Bostanci Y, Revival of thermotherapy for benign prostatic hyperplasia: Review Curr Opin Urol, 2012; 22; 16-21
9. Vesely S, Knutson K, Damber JE, TURP and low-energy TUMT treatment in men with LUTS suggestive of bladder outlet obstruction selected by means of pressure-flow studies: 8-year follow-up: Neurourol Urodyn, 2006; 25; 770-75
10. Herrmann TR, Gross AJ, Schultheiss D, Transurethral microwave thermotherapy for the treatment of BPH: Still a challenger?: World J Urol, 2006; 24; 389-96
11. Hoffman RM, Monga M, Elliott SP, Microwave thermotherapy for benign prostatic hyperplasia: Cochrane Database Syst Rev, 2012(9); CD004135
12. Hoffman RM, MacDonald R, Monga M, Wilt TJ, Transurethral microwave thermotherapy vs transurethral resection for treating benign prostatic hyperplasia: A systematic review: BJU Int, 2004; 94; 1031-36
13. Dahlstrand C, Geirsson G, Fall M, Pettersson S, Transurethral microwave thermotherapy versus transurethral resection for benign prostatic hyperplasia: Preliminary results of a randomized study: Eur Urol, 1993; 23; 292-98
14. Gravas S, Cornu JN, Gacci M, Management of non-neurogenic male lower urinary tract symptoms (LUTS): European Association of Urology Guidelines, 2019 https://uroweb.org/guideline/treatment-of-non-neurogenic-male-luts/
15. Hoffman RM, Monga M, Elliott SP, Microwave thermotherapy for benign prostatic hyperplasia: Cochrane Database Syst Rev, 2007(4); CD004135
16. Tabatabaei S, Zangi M, Outpatient surgery for lower urinary tract symptoms/benign prostatic hyperplasia: Truth or myth?: Curr Opin Urol, 2015; 25; 27-31
17. Terai A, Arai Y, Yamamoto I, Newly developed transurethral radiofrequency thermotherapy device for benign prostatic hyperplasia: A pilot study in canine prostate: Int J Hyperthermia, 1995; 11; 627-35
18. Kontis V, Bennett JE, Mathers CD, Future life expectancy in 35 industrialised countries: Projections with a Bayesian model ensemble: Lancet, 2017; 389; 1323-35
19. Pająk A, Borówka AThe incidence of lower urinary tract ailments in men aged 50–79 years. Results of the first epidemiological studies carried out in Poland: Urologia Polska, 1998; 51(Suppl 1a); 10-11 [in Polish]
20. Kaplan SA, Gonzalez RR, Te AE, Combination of alfuzosin and sildenafil is superior to monotherapy in treating lower urinary tract symptoms and erectile dysfunction: Eur Urol, 2007; 51; 1717-23
21. Sciarra A, Lower urinary tract symptoms (LUTS) and sexual dysfunction (SD): New targets for new combination therapies?: Eur Urol, 2007; 51; 1485-87
22. Saitz TR, Conlin MJ, Tessier CD, Safety and efficacy of transurethral microwave therapy in high-risk catheter-dependent men: Turk J Urol, 2019; 45; 27-30
23. Rosen R, Altwein J, Boyle P, Lower urinary tract symptoms and male sexual dysfunction: The multinational survey of the aging male (MSAM-7): Eur Urol, 2003; 44; 637-49
24. Kaminetsky J, Comorbid LUTS and erectile dysfunction: Optimizing their management: Curr Med Res Opin, 2006; 22; 2497-506
25. Pawlicki B, Gałka M, Mrozicki S, Erectile dysfunction following transurethral resection of the prostate following bladder outlet obstruction: Sex Pol, 2003; 1; 47-50
26. Kunelius P, Hakkienen J, Lukkarinen O, Sexual functions in patients with benign prostatic hyperplasia before and after transurethral resection of the prostate: Urol Res, 1998; 26; 7-9
27. Soderdahl DW, Knight RW, Hansberry KL, Erectile dysfunction following transurethral resection of the prostate: J Urol, 1996; 156; 1354-56
28. Liu CK, Liao CH, Wan KS, Change in intraoperative rectal temperature influencing erectile dysfunction following transurethral resection of the prostate: J Formos Med Assoc, 2012; 111; 320-24
29. Zhao QQ, Meng XH, Xue JImpact of transurethral resection of the prostate on erectile function: A report of 64 cases: Zhongua Nan Ke Xue, 2013; 19; 710-13 [in Chinese]
30. Becher EF, McVary KT, Surgical procedures for BPH/LUTS: Impact on male sexual health: Sex Med Rev, 2014; 2; 47-55
31. Oka AAG, Duarsa GKD, Novianti PA, The impact of prostate-transurethral resection on erectile dysfunction in benign prostatic hyperplasia: Res Rep Urol, 2019; 11; 91-96
32. Arai Y, Aoki Y, Okubo K, Impact of interventional therapy for benign prostatic hyperplasia on quality of life and sexual function: A prospective study: J Urol, 2000; 164; 1206-11
33. Oelke M, Bachmann A, Descazeaud AEuropean Association of Urology, EAU guidelines on the treatment and follow-up of non-neurogenic male lower urinary tract symptoms including benign prostatic obstruction: Eur Urol, 2013; 64; 118-40
34. Dutkiewicz S, Duda W, Duda MAssessment of sexual function and erectile dysfunction in patients with benign prostatic hyperplasia: Seksuologia Polska, 2010; 8(2); 55-59 [in Polish]
35. Shamloul R, Ghanem H, Erectile dysfunction: Lancet, 2013; 381; 153-65
36. Skolarus TA, Wei JT, Measurement of benign prostatic hyperplasia treatment effects on male sexual function: Int J Impot Res, 2009; 21; 267-74
37. Kocznur K, Minimally invasive methods of treating benign prostatic hyperplasia: Rev Urol, 2010; 3; 61-65
38. Tzortzis V, Gravas S, de la Rosette JMCH, Minimally invasive surgical treatments for benign prostatic hyperplasia: Eur Urol Suppl, 2009; 8; 513-22
39. Mattiasson A, Wagrell L, Schelin S, Five-year follow-up of feedback microwave thermotherapy versus TRUP for clinical BPH: A prospective randomized multicenter study: Urology, 2007; 69; 91-96
40. Osterberg EC, No D, Otto BJ, A retrospective review of office-based 532-nm Greenlight laser prostatectomy in men with symptomatic benign prostatic hyperplasia: Urology, 2013; 82; 680-85
41. Madersbacher S, Alivizatos G, Nordling J, EAU 2004 guidelines on assessment, therapy and follow-up of men with lower urinary tract symptoms suggestive of benign prostatic obstruction (BPH guidelines): Eur Urol, 2004; 46; 547-54
42. Ahmed M, Bell T, Lawrence WT, Transurethral microwave thermotherapy (Prostatron version 2.5) compared with transurethral resection of the prostate for the treatment of benign prostatic hyperplasia: A randomized, controlled, parallel study: Br J Urol, 1997; 79; 181-85
43. Aagaard MF, Niebuhr MH, Jacobsen JD, Transurethral microwave thermotherapy treatment of chronic urinary retention in patients unsuitable for surgery: Scand J Urol, 2014; 48; 290-94
44. Reich O, Gratzke C, Bachmann A, Morbidity, mortality and early outcome of transurethral resection of the prostate: A prospective multicenter evaluation of 10,654 patients: J Urol, 2008; 180; 246-49
45. McNicholas T, Kirby R, Benign prostatic hyperplasia and male lower urinary tract symptoms (LUTS): BMJ Clin Evid, 2011; 1801-41
46. Norby B, Nielsen HV, Frimodt-Moller PC, Transurethral interstitial laser coagulation of the prostate and transurethral microwave thermotherapy vs. transurethral resection or incision of the prostate: Results of a randomized, controlled study in patients with symptomatic benign prostatic hyperplasia: BJU Int, 2002; 90; 853-62
Tables
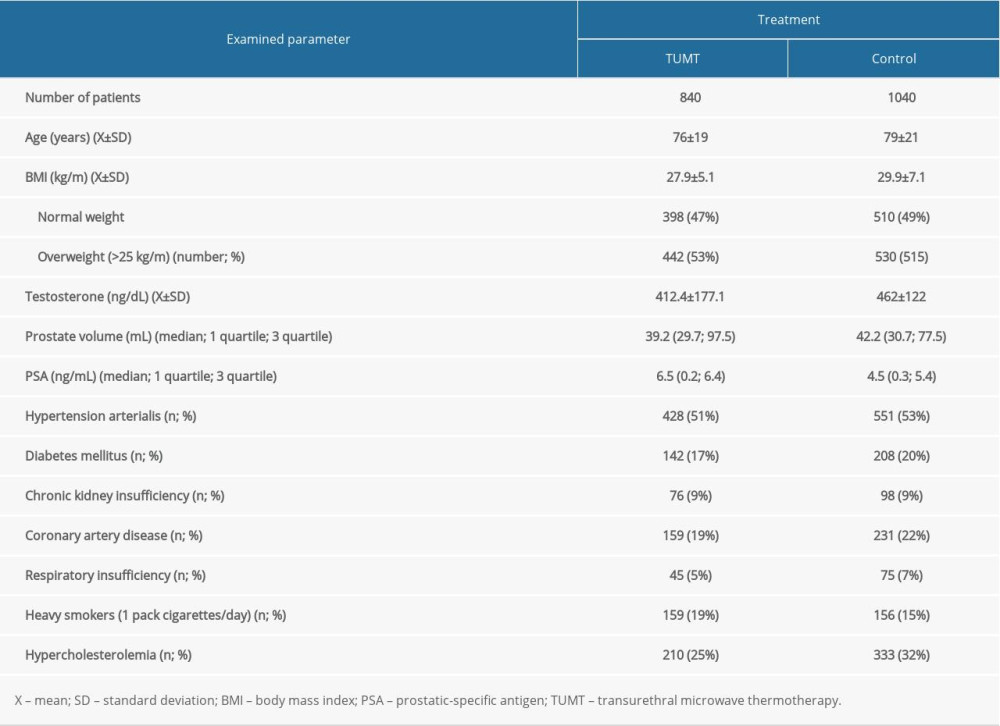 Table 1. Sociodemographic and clinical data of patients with benign prostatic hyperplasia in the transurethral microwave thermotherapy (TUMT) and pharmacotherapy (control) groups.
Table 1. Sociodemographic and clinical data of patients with benign prostatic hyperplasia in the transurethral microwave thermotherapy (TUMT) and pharmacotherapy (control) groups.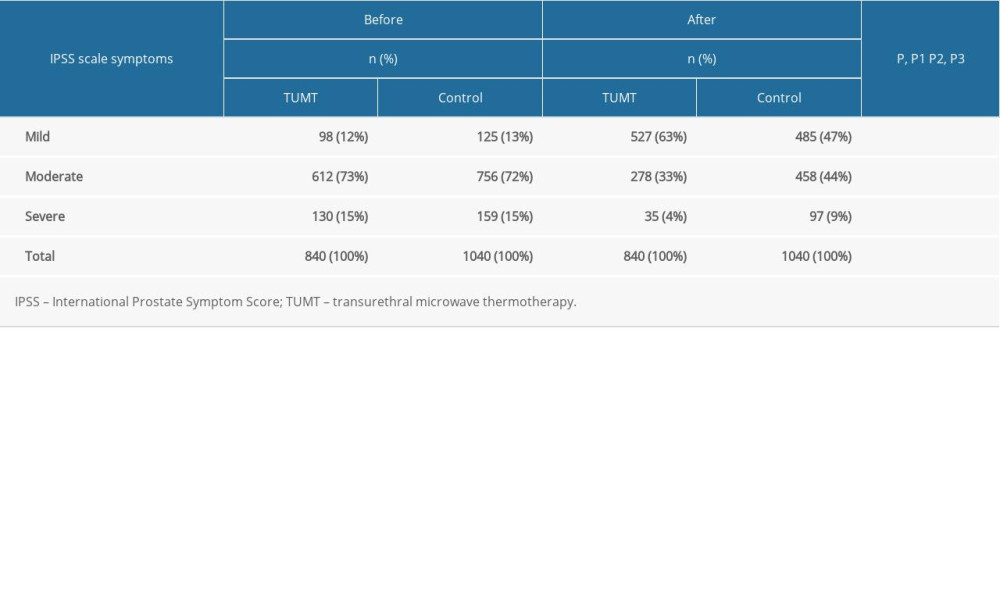 Table 2. Baseline and 6-month follow-up International Prostate Symptom Score of patients in the transurethral microwave thermotherapy (TUMT) and pharmacologic (control) groups. P, P1, P2, and P3 indicate statistical significance according to the Z test: P, baseline comparison between TUMT and control group; P1, 6-month follow-up comparison between the TUMT and control groups; P2, only within the TUMT group, baseline vs 6-month follow-up; P3, only within the control group, baseline vs 6-month follow-up.
Table 2. Baseline and 6-month follow-up International Prostate Symptom Score of patients in the transurethral microwave thermotherapy (TUMT) and pharmacologic (control) groups. P, P1, P2, and P3 indicate statistical significance according to the Z test: P, baseline comparison between TUMT and control group; P1, 6-month follow-up comparison between the TUMT and control groups; P2, only within the TUMT group, baseline vs 6-month follow-up; P3, only within the control group, baseline vs 6-month follow-up.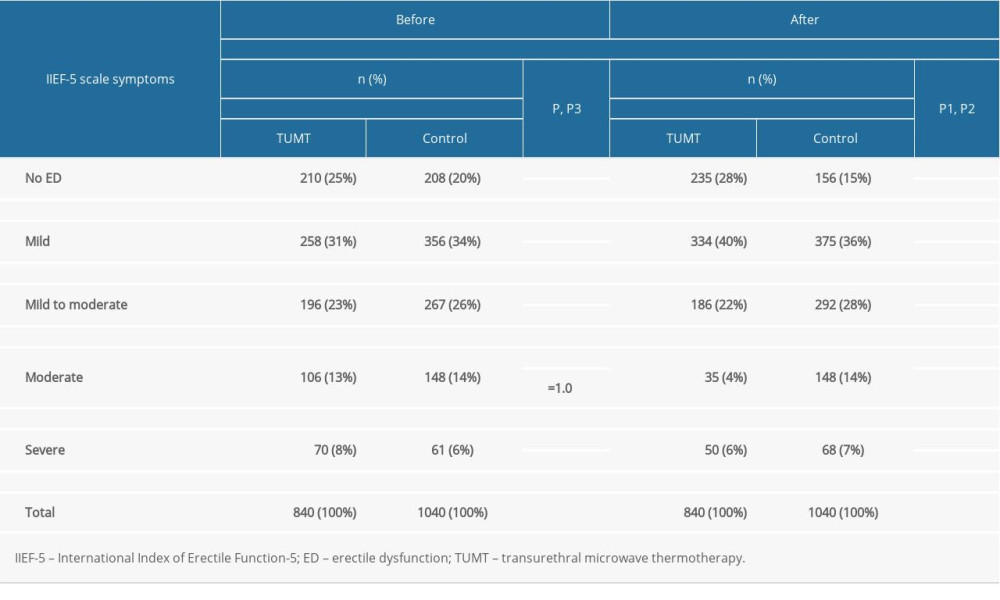 Table 3. Baseline International Index of Erectile Function-5 IIEF-5 scores and after 6 months of observations in the patients allocated in the transurethral microwave thermotherapy (TUMT) and pharmacologic (control) group. P, P1, P2, and P3 indicate statistical significance according to the Z test: P, baseline comparison between TUMT and control group; P1, 6-month follow-up comparison between the TUMT and control groups; P2, only within the TUMT group, baseline vs 6-month follow-up; P3, only within the control group, baseline vs 6-month follow-up.
Table 3. Baseline International Index of Erectile Function-5 IIEF-5 scores and after 6 months of observations in the patients allocated in the transurethral microwave thermotherapy (TUMT) and pharmacologic (control) group. P, P1, P2, and P3 indicate statistical significance according to the Z test: P, baseline comparison between TUMT and control group; P1, 6-month follow-up comparison between the TUMT and control groups; P2, only within the TUMT group, baseline vs 6-month follow-up; P3, only within the control group, baseline vs 6-month follow-up.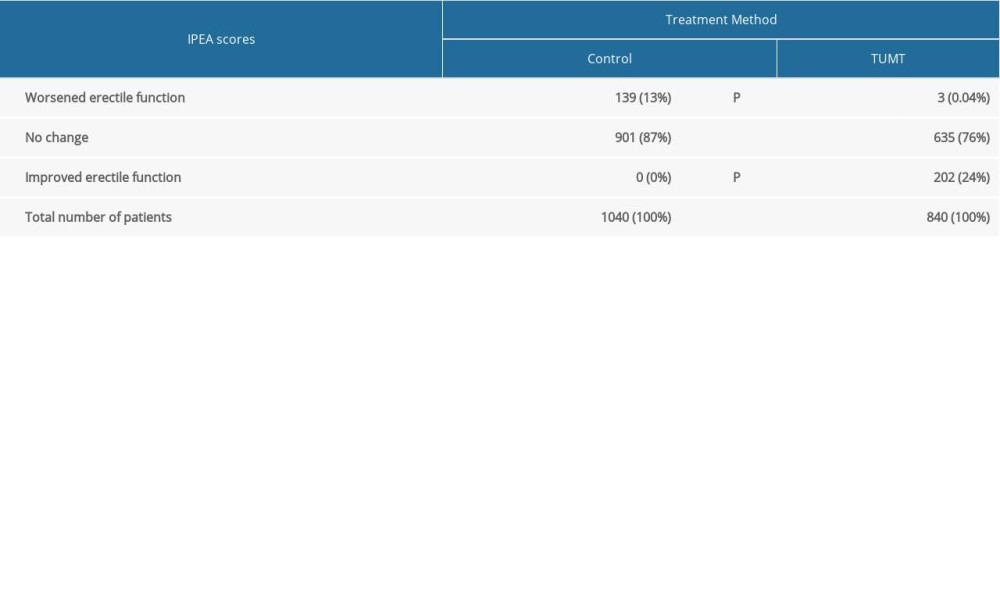 Table 4. Evaluation of erectile function using the Individual Postoperative Erectile Assessment (IPEA) questionnaire at the 6-month follow-up in the transurethral microwave thermotherapy (TUMT) and pharmacologic (control) groups. P, statistical significance according to Fisher’s exact test.
Table 4. Evaluation of erectile function using the Individual Postoperative Erectile Assessment (IPEA) questionnaire at the 6-month follow-up in the transurethral microwave thermotherapy (TUMT) and pharmacologic (control) groups. P, statistical significance according to Fisher’s exact test.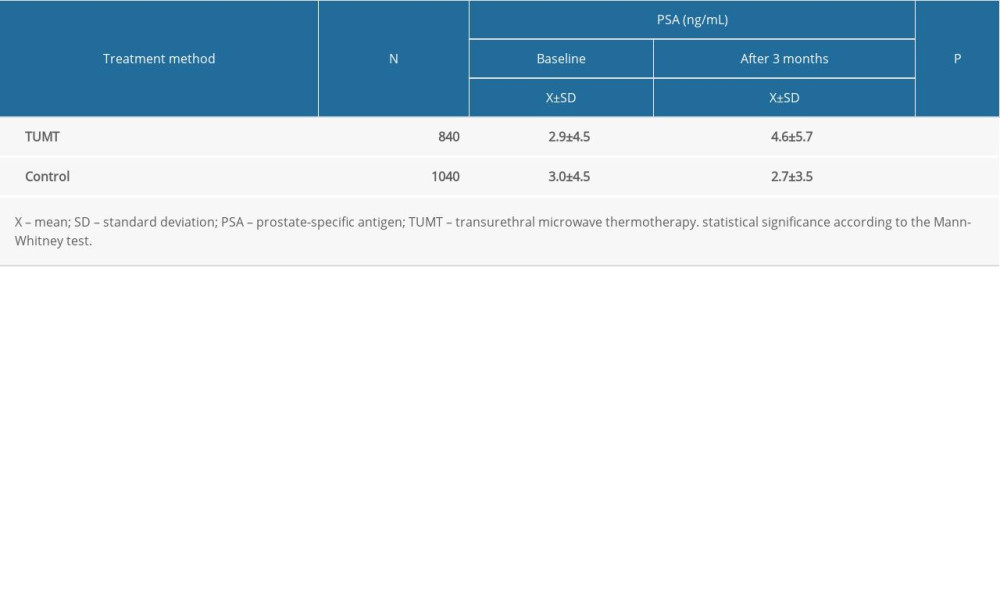 Table 5. Prostate-specific antigen concentration at the 3-month follow-up in the transurethral microwave thermotherapy (TUMT) and pharmacologic (control) groups.
Table 5. Prostate-specific antigen concentration at the 3-month follow-up in the transurethral microwave thermotherapy (TUMT) and pharmacologic (control) groups. In Press
05 Mar 2024 : Clinical Research
Muscular Function Recovery from General Anesthesia in 132 Patients Undergoing Surgery with Acceleromyograph...Med Sci Monit In Press; DOI: 10.12659/MSM.942780
05 Mar 2024 : Clinical Research
Effects of Thermal Insulation on Recovery and Comfort of Patients Undergoing Holmium Laser LithotripsyMed Sci Monit In Press; DOI: 10.12659/MSM.942836
05 Mar 2024 : Clinical Research
Role of Critical Shoulder Angle in Degenerative Type Rotator Cuff Tears: A Turkish Cohort StudyMed Sci Monit In Press; DOI: 10.12659/MSM.943703
06 Mar 2024 : Clinical Research
Comparison of Outcomes between Single-Level and Double-Level Corpectomy in Thoracolumbar Reconstruction: A ...Med Sci Monit In Press; DOI: 10.12659/MSM.943797
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








