21 March 2021: Clinical Research
Association Between Sigmoid Sinusoidal Tinnitus and Low-Frequency Sensorineural Hearing Loss: A Retrospective Study at a Single Center
Siji Wang1ABCDEF, Jiaqiu Dai1B, Changchao Xiang1C, Ziqi Chen1D, Xi Ouyang1E, Lin Zhu1F, Fenghui Yu1B, Xiaofang Zong1F, Houyong Kang1AG*DOI: 10.12659/MSM.929300
Med Sci Monit 2021; 27:e929300
Abstract
BACKGROUND: We aimed to explore the correlation between patients’ sigmoid sinusoidal tinnitus (SST) and low-frequency sensorineural hearing loss (LFSHL) and illustrate the underlying mechanism.
MATERIAL AND METHODS: Seven healthy volunteers with normal hearing were subjected to 125-, 250-, and 500-Hz pure sound and different white noise-masking intensities. A retrospective analysis was made on the clinical data and postoperative follow-up data of 59 patients with SST in the First Affiliated Hospital of Chongqing Medical University. The patients’ sex, age, chief complaints, affected site, concomitant symptoms, course of disease, pure-tone audiometry (PTA) results, tinnitus discomfort loudness scale results, imaging examination, and complications were collected.
RESULTS: The results of the simulation experiment showed that the threshold of each frequency segment was higher after noise masking than before masking; the intensity of noise masking was positively correlated with hearing loss, and the changes of the hearing threshold of the 3 frequencies before and after masking were statistically significant (P<0.05). Fifty-nine patients with SST were documented between January 2015 and January 2020. After the operation, their low-frequency hearing was recovered to normal; 11 cases had significantly alleviated tinnitus and 9 cases were cured.
CONCLUSIONS: SST often causes corresponding pseudo-low-frequency hearing loss due to the noise-masking effect. The center frequency of tinnitus appears not to be 250-Hz or 500-Hz octave frequency of PTA, barring the detection of the pseudo-hearing loss in the audiometry chart of most patients. Surgery positively affects patients with SST, and the pseudo-LFSHL can be completely recovered after the operation as a result of tinnitus elimination.
Keywords: Correction of Hearing Impairment, Hearing Loss, Sensorineural, Tinnitus, Audiometry, Pure-Tone, Auditory Perception, Auditory Threshold, Hearing, Noise
Background
Tinnitus originates from the Latin word “tinnire,” which means a ringing sound in the ear; it refers to the conscious sense of hearing when there is no corresponding external stimulus and is often accompanied by irritability, anxiety, or depression, affecting patients’ life quality. Severe tinnitus could promote suicidal behavior and other serious consequences [1–3]. Tinnitus is mainly subjective, but some cases are caused by vascular factors, such as pulsating blood flow or rumbling blood turbulence, and in these cases, it is called pulsatile tinnitus (PT) [4,5]. Previous studies have found that surgery could cure the commonly occurring vascular tinnitus caused by structural variation of sigmoid sinus diverticulum (SSD) or sigmoid sinus wall dehiscence (SSWD) [5–7].
Our team has treated many patients with tinnitus caused by structural variation of the sigmoid sinus in recent years. We denominated those patients as having sigmoid sinusoidal tinnitus (SST). The patients with SST were hospitalized after corresponding surgical treatment, and their initial reports of sustained low-frequency buzzing or PT showed significant reduction or elimination. Simultaneously, some patients with ipsilateral low-frequency sensorineural hearing loss (LFSHL) at 250 and 500 Hz recovered entirely after surgery. No chief complaint of hearing loss was found by retrospective analysis or hearing loss frequency associated with preoperative audiograms in patients’ medical history. Several questions arise regarding the underlying mechanism of LFSHL and its categorization as a sensorineural hearing loss rather than conductive or mixed hearing loss. For example, why doesn’t LFSHL affect all patients, and why does tinnitus disappear in some patients after the operation, with hearing restored completely? Our team intends to answer the above questions through simulation experiments and systematic retrospective analysis to explore the mechanism and efficient treatment of SST combined with LFSHL.
Material and Methods
PARTICIPANTS:
Healthy young volunteers with normal hearing were recruited in the present study. The bare-ear thresholds of pure-tone hearing at 125 Hz, 250 Hz, and 500 Hz and the thresholds under white noise masking of different intensities (30, 35, 40 dB) were determined for both ears. Fifty-nine patients with tinnitus (have abnormal sigmoid sinus structure) were enrolled in the present study between January 2015 and January 2020. A detailed physical examination was conducted before admission to determine the participants’ inclusion criteria. The initial diagnosis was SST, and the thin-layer computed tomography (CT) of the temporal bone confirmed that the SSD or the resonance cavity formed by the surrounding mastoid atmosphere chamber was due to the weakness or absence of the sigmoid sinus bone wall. The neck-pressing test was performed; pressing the patients’ neck weakened or stopped tinnitus symptoms. Clinical, audiological, physical, and imaging examinations were performed. Patients with tinnitus caused by nonsigmoid sinus lesions such as temporal bone trauma history, otologic surgery history, Meniere’s disease, chronic otitis media, anxiety disorder, depression, and others were excluded.
DATA COLLECTION:
The patients’ sex, age, chief complaint, affected site, concomitant symptoms, course of disease, pure-tone audiometry (PTA) results, tinnitus discomfort loudness scale results, imaging examination, and complications were collected.
AUDIOLOGICAL ASSESSMENT: All patients underwent PTA at the first visit. Compared with the contralateral asymptomatic side, ipsilateral hearing threshold greater than 10-dB hearing level (HL) at 250 and 500 Hz or 20-dB HL at 250 or 500 Hz was defined as LFSHL [8]. Patients with SST with low-frequency hearing loss underwent PTA assessment after surgical treatment. The changes in low-frequency hearing loss before and after surgery were compared.
TINNITUS RATING SCALE: All patients were classified according to the tinnitus degree before and after the operation [9]. We standardized our classification according to the patients’ tinnitus loudness. The higher the grade, the more serious the tinnitus. Grade 0: no tinnitus; grade 1: extremely low to indistinct tinnitus; grade 2: merely audible tinnitus, only appears in a quiet environment and does not affect everyday routines such as sleep and work; grade 3: relatively loud tinnitus, can be heard in public, but has no apparent intrusion on routine life and work; grade 4: habitually heard tinnitus, affects sleep and distracts attention; grade 5: tumultuous tinnitus, seriously affects sleep and work and results in mild irritability, anxiety, depression, and other mental symptoms; grade 6: raucous tinnitus, entirely affects patients’ sleep and work and associated with obvious mental symptoms such as irritability, anxiety, and depression.
SURGICAL METHODS:
All patients underwent SSD resection (packing) or sigmoid sinus resonance cavity resection combined with autologous bone powder reconstruction of the sigmoid sinus bone wall through the mastoid approach under local anesthesia. The main surgical procedures included: (1) infiltration of 1% lidocaine adrenal fluid around the ear and incision after anesthesia. (2) The cortical area centered on the sinus meningeal angle (the most common site of structural variation and resonance cavity of the sigmoid sinus) was exposed. The cortical bone of the area was excised, and the aseptic bone powder was collected. (3) The surrounding bone of the SSD was gently removed and filled with gelatin sponge combined with bone powder until patients’ tinnitus immediately weakened or disappeared. In the sigmoid sinus resonance cavity, the atmospheric chamber (joint cavity) with the affected area or weak part of the sigmoid sinus bone wall was located. The air chamber was removed; simultaneously, the patients’ tinnitus immediately weakened until it disappeared. (4) The sigmoid sinus’s bone wall was reconstructed with an autologous bone powder layer protected and fixed with a gelatin sponge. (5) After the musculoperiosteal flap, the incision layers were sutured and bandaged.
EVALUATION OF CURATIVE EFFECT: The initial hearing was the low-frequency (250 and 500 Hz) PTA threshold (LF-PTA) examined by our hospital before surgery. The final hearing LF-PTA was re-examined during and after the surgery, and patients’ recovery determined the curative effect [9,10]. (1) Total recovery: hearing frequency threshold was entirely restored to normal. (2) Significantly effective: aberrant hearing frequency threshold ≥30 dB; (3) Effective: aberrant hearing frequency threshold ≥15 dB; (4) ineffective: aberrant hearing frequency threshold <15 dB. Evaluation of tinnitus improvement before and after operation: (1) Total recovery: tinnitus completely disappeared. (2) Significantly effective: compared with preoperation tinnitus degree, decreased by more than or equal to 2 levels. (3) Effective: tinnitus degree decreased by 1 level compared with preoperation tinnitus. (4) Ineffective: tinnitus degree had no change.
LOW-FREQUENCY MASKING HEARING CHANGES IN SIMULATED SST:
Seven healthy young volunteers without tinnitus and vertigo were recruited to simulate the effect of tinnitus with different loudness on low-frequency hearing. The pure-tone hearing thresholds at 125, 250, and 500 Hz and the white noise-masking threshold under different intensities (30, 35, 40 dB) were conducted. Four pure-tone tests were performed in the low-frequency band, including 1 pure-tone detection without masking and 3 pure-tone detections with different white noise-masking intensity. The average value after 3 maskings was taken as the postmasking threshold of the frequency band.
STATISTICAL METHODS:
All data analyses were done using SPSS22.0 software. The values were presented as mean±standard deviation. The
Results
LOW-FREQUENCY HEARING CHANGES IN NORMAL SUBJECTS WITH SIMULATED SST:
Different stimulations of healthy patients’ ears showed that at 125 Hz, the bare-ear threshold of 7 participants (14 ears) was 11±3.63 dB HL; the average threshold was 38±3.25, 43±3.23, and 47±4.21 dB HL under 3 kinds of noise-masking intensities. At 250 Hz, the bare-ear threshold was 6±3.63 dB HL, and the average threshold was 35±3.40, 42±2.49, and 45±2.77 dB HL under 3 kinds of noise-masking intensities. At 500 Hz, the bare-ear threshold was 9±3.63 dB HL, and the average threshold was 34±4.01, 40±4.99, and 45±3.08 dB HL under 3 kinds of noise-masking intensities (Table 1). The average thresholds of each frequency band after noise masking were significantly higher than those before masking (Table 2).
OVERALL DATA OF PATIENTS WITH SST:
Among the 59 patients, 57 were women and 2 were men – 39 having SST in the right ear and 20 in the left ear. The patients’ average age was 39±11.59 years, and the disease course ranged from 0.08 to 20 years. There were 20 patients with low-frequency hearing loss (19 women, 1 man), and their ages ranged between 22 and 54 years, with an average age of 34±9.67 years. Thirty-nine patients without low-frequency hearing loss (38 women, 1 man) ranged in age from 20 to 69 years, with an average age of 42±11.60 years. The onset age of different SST types was statistically low, and there was no significant difference in sex and affected ear site (Table 3).
TINNITUS AND HEARING EVALUATION IN PATIENTS WITH LFSHL SST:
Table 4 summarizes the patients’ demographic characteristics, symptom duration, preoperative and postoperative audiological changes, and tinnitus degree. In 20 cases of SST with low-frequency hearing loss, 19 patients (95%) were women and 1 patient (5%) was a man; 15 patients (75%) showed SST in the right ear and 5 patients (25%) in the left ear; 6 patients (30%) presented with SSD, 10 (50%) showed SSWD, and 4 (20%) had both SSD and SSWD. All patients’ low-frequency hearing was recovered after the operation; 11 patients had significantly alleviated tinnitus and 9 patients were cured. The typical cases are shown in Figures 1 and 2. It has been shown that after the resection of the SSD or resonance cavity combined with bone wall reconstruction, tinnitus was prevented and low-frequency hearing was normal.
Discussion
SST is the most common type of vascular tinnitus. It is characterized by persistent low-tone tinnitus and partially PT. Our team retrospectively analyzed 59 participants; all of them met the above characteristics of tinnitus. Simultaneously, thin-layer CT examination of the temporal bone showed a formation of SSD or sigmoid sinus-derived resonant cavity. The tinnitus weakened or disappeared after the neck-pressing test; this observation was consistent with most previous studies [11–14]. We found that about one-third of the patients with SST (20/59) showed sensorineural hearing loss at frequencies of 250 and 500 Hz on the audiogram without hearing loss complaints. Previous studies have paid little attention to this phenomenon. In 2016, a study proposed that patients with SST and LFSHL are more likely to have vascular structural abnormalities near the cochlea and speculated that the masking effect of PT might lead to the change of hearing threshold in the low-frequency region, which may also be used for objective diagnosis and evaluation of therapeutic efficiency [8]. However, only 11 of 22 patients with tinnitus and LFHL were treated with surgery or interventional therapy. Among the treated patients, 8 had PTA outcomes before and after treatment. Therefore, a larger experimental population is required to confirm the validity of the low-frequency threshold change in diagnosing and evaluating therapeutic efficiency.
In the present study, a simulation experiment was designed to simulate the tinnitus effect with different loudness on low-frequency hearing by masking different white noise intensities. The results indicated that all healthy subjects showed significant hearing loss at corresponding frequencies under the masking effect, and the threshold increased gradually with the increase of masking sound intensity. In the simulation experiment, we introduced a 125-Hz low-frequency hearing test consistent with the masking effect of 250 Hz and 500 Hz. In clinical practice, a 125-Hz hearing test is not typical. In this study, only a few of 59 SST cases were tested at 125 Hz, and the hearing loss of 20 cases with LFSHL at 250-Hz frequency was significantly higher than that at 500 Hz. The sigmoid sinus stimulates sound and might have a higher central frequency of amplified tinnitus by turbulence or air chamber resonance cavity at 125 Hz or even lower. Therefore, on the basis of the above analysis, we believe that all SST patients will have LFSHL consistent with its central frequency distribution lower than 125 Hz. Because the loudness perception of human ears is weak in the low-frequency region, and the central frequency band involved in human communication is 500–4000 Hz, few patients feel the hearing loss. This is consistent with our study participants’ hearing loss complaints.
Taken together, we can conclude that LFSHL is caused by tinnitus masking, which can be regarded as pseudo-hearing loss. After resection of diverticulum or resonance cavity under local anesthesia, patients can immediately perceive that tinnitus is significantly reduced or even eliminated. Three months after surgery, the wound and incision in the operation area were entirely healed, and the inflammatory effusion produced by the mastoid air chamber and middle ear cavity had been completely absorbed because the tinnitus was weakened or eliminated. The cochlea has no masking effect of tinnitus, and its pseudo-sensorineural hearing loss can be fully recovered. Therefore, surgery is the best method for patients with SST. Surgery can not only effectively eliminate tinnitus, but also recover the concomitant LFSHL. The key point of surgical treatment of SST is to locate the diverticulum and resonance cavity. Local anesthesia can promote direct interaction with patients and help the operator judge the localization accuracy by whether the tinnitus sound is weakened or eliminated; it is more likely recommended for young surgeons, especially in SST with more difficult localization or multiple resonators.
Numerous clinical studies have shown that surgical intervention can achieve good therapeutic outcomes [7,15–18]. The surgical plan focuses on the elimination of the sigmoid diverticulum or resection of the resonance cavity.
This study retrospectively analyzed the clinical data of 59 patients who underwent surgery, including postoperative hearing and imaging follow-up. Our results summed up the common ground of this kind of tinnitus, related to the sigmoid sinus. The causes of tinnitus are either the turbulence sound of the diverticulum or the blood-flow sound of the sigmoid sinus directly into the cochlea through the resonance cavity formed by its mastoid air chamber and passing through the anterior part of the cochlea. The simulation results showed that the masking effect promoted LFSHL.
Therefore, we propose that the present type of tinnitus can be called SST; this reflects the essential characteristics of this type of tinnitus. The presented simplified name is also convenient for standardizing the academic exchanges and substituting the obsolete names of SSD, sigmoid sinus wall dehiscence, vascular tinnitus, PT, and other diseases. We suggest that SSD resection or sigmoid sinus resonance cavity resection plus sigmoid sinus bone wall reconstruction as a unified operation name be recommended for both diverticulum and resonance cavity repair.
Sigmoid sinus resection operation primarily exposes the diverticulum’s sigmoid sinus tissue, alleviating the tinnitus by the filling, pressing, and returning autologous materials like bone powder, fascia, or paraffin wax. The sigmoid sinus resonant cavity resection mainly depends on removing the mastoid air chamber, which produces resonance to eliminate tinnitus.
The purpose of combined sigmoid sinus bone wall reconstruction is to thicken the defective or weak bone wall tissue area with autogenous bone powder or bone wax. The reconstructed bone wall can protect this critical vascular structure and prevent tinnitus without diverticulum or resonance cavity formation.
Conclusions
To sum up, the cause of tinnitus in patients with SST is formation of the SSD or sigmoid sinus resonance cavity by the sigmoid sinus’s abnormal structure in the mastoid part of the temporal bone. Because of the masking effect of tinnitus on the cochlea, patients with SST can exhibit the corresponding band of pseudo-sensorineural hearing loss in the PTA. However, because patients with SST are not sensitive to the loudness of the frequency band, they have no complaints of LFSHL. Following the patients’ medical history and different examinations, an accurate diagnosis can be made. We can conclude that SSD resection or sigmoid sinus resonance cavity resection plus sigmoid sinus bone wall reconstruction under local anesthesia is an effective way to treat patients with SST.
Figures
![A typical case of sigmoid sinusoidal tinnitus and low-frequency sensorineural hearing loss (right sigmoid sinus diverticulum [SSD]). (A) Preoperative temporal bone computed tomography (CT). (B) Postoperative temporal bone CT. (C) Preoperative pure-tone audiometry (PTA). (D) Postoperative PTA. (E) Intraoperative SSD. (F) After excision of the sigmoid diverticulum during the operation, the autologous bone powder was covered. In PTA, the dotted red line represents the right side; the star blue line represents the variation of the left.](https://jours.isi-science.com/imageXml.php?i=medscimonit-27-e929300-g001.jpg&idArt=929300&w=1000) Figure 1. A typical case of sigmoid sinusoidal tinnitus and low-frequency sensorineural hearing loss (right sigmoid sinus diverticulum [SSD]). (A) Preoperative temporal bone computed tomography (CT). (B) Postoperative temporal bone CT. (C) Preoperative pure-tone audiometry (PTA). (D) Postoperative PTA. (E) Intraoperative SSD. (F) After excision of the sigmoid diverticulum during the operation, the autologous bone powder was covered. In PTA, the dotted red line represents the right side; the star blue line represents the variation of the left.
Figure 1. A typical case of sigmoid sinusoidal tinnitus and low-frequency sensorineural hearing loss (right sigmoid sinus diverticulum [SSD]). (A) Preoperative temporal bone computed tomography (CT). (B) Postoperative temporal bone CT. (C) Preoperative pure-tone audiometry (PTA). (D) Postoperative PTA. (E) Intraoperative SSD. (F) After excision of the sigmoid diverticulum during the operation, the autologous bone powder was covered. In PTA, the dotted red line represents the right side; the star blue line represents the variation of the left. 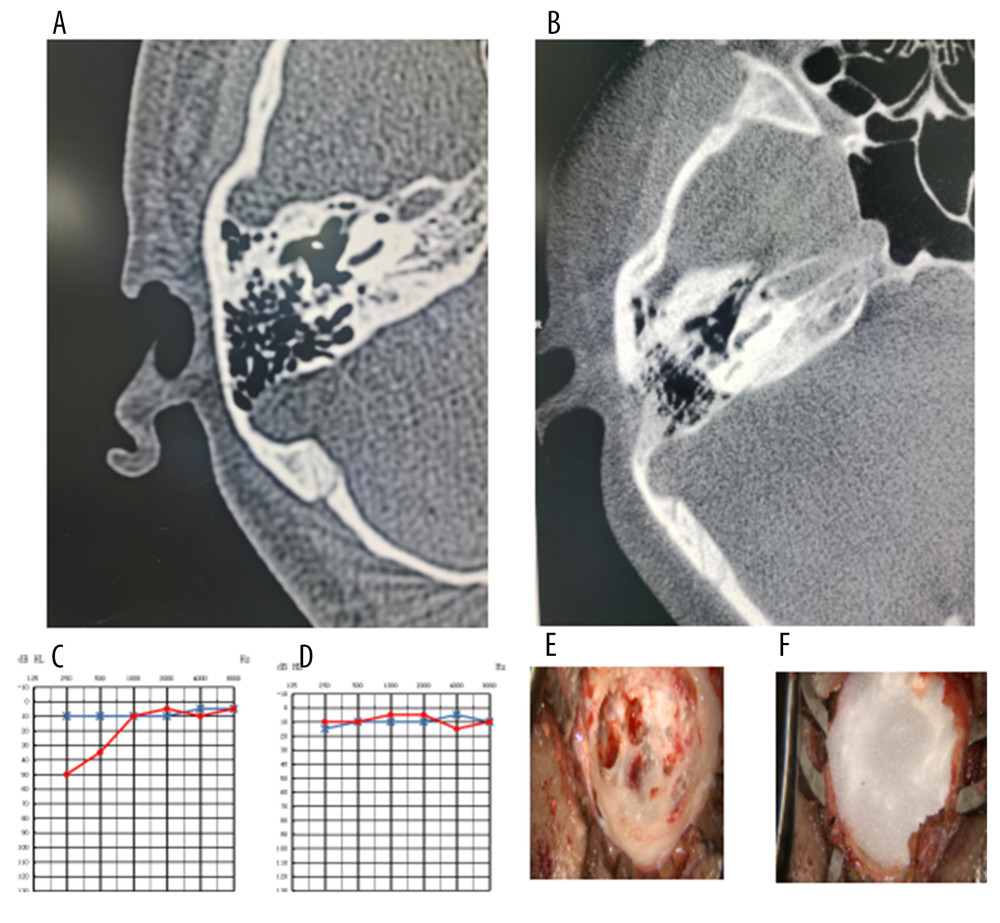 Figure 2. A typical case of sigmoid sinusoidal tinnitus and low-frequency sensorineural hearing loss (the defect in the bone wall of the right sigmoid sinus forms a resonating cavity). (A) Preoperative temporal bone computed tomography (CT). (B) Postoperative temporal bone CT. (C) Preoperative pure-tone audiometry (PTA). (D) Postoperative PTA. (E) Resonance cavity formation was observed intraoperatively. (F) After excision of the resonance cavity during the operation, the autologous bone powder was covered. In PTA, the dotted red line represents the right side; the star blue line represents the variation of the left.
Figure 2. A typical case of sigmoid sinusoidal tinnitus and low-frequency sensorineural hearing loss (the defect in the bone wall of the right sigmoid sinus forms a resonating cavity). (A) Preoperative temporal bone computed tomography (CT). (B) Postoperative temporal bone CT. (C) Preoperative pure-tone audiometry (PTA). (D) Postoperative PTA. (E) Resonance cavity formation was observed intraoperatively. (F) After excision of the resonance cavity during the operation, the autologous bone powder was covered. In PTA, the dotted red line represents the right side; the star blue line represents the variation of the left. Tables
Table 1. Masking thresholds of healthy subjects with different masking intensity.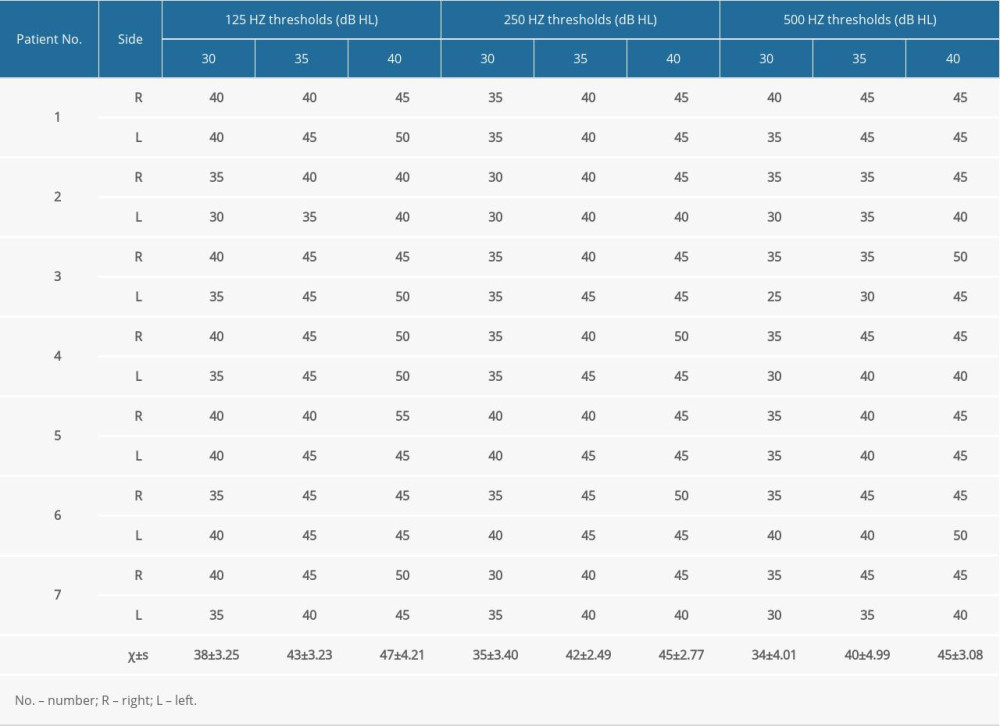 Table 2. Different frequency thresholds of healthy participants with or without masking.
Table 2. Different frequency thresholds of healthy participants with or without masking.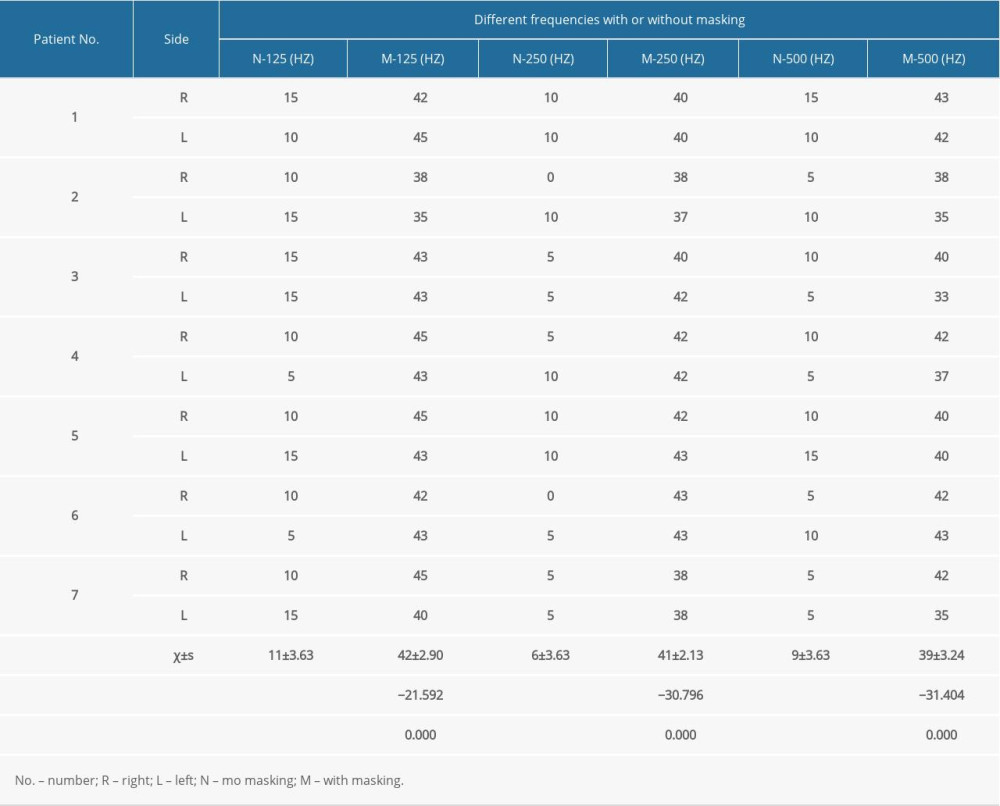 Table 3. Clinical summary of patients with sigmoid sinusoidal tinnitus.
Table 3. Clinical summary of patients with sigmoid sinusoidal tinnitus.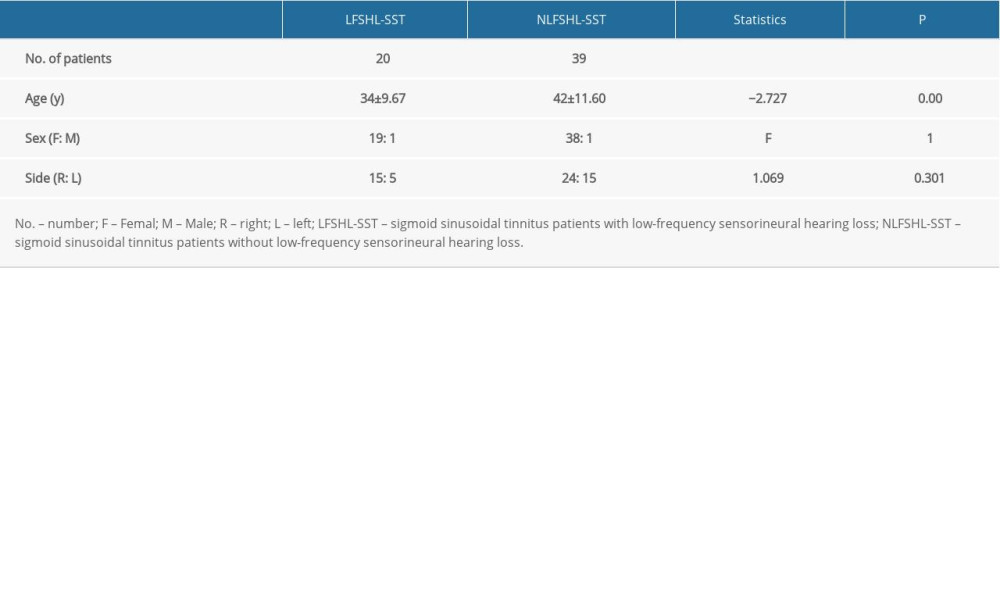 Table 4. Efficacy evaluation of tinnitus and hearing loss in 20 patients with sigmoid sinusoidal tinnitus and low-frequency sensorineural hearing loss.
Table 4. Efficacy evaluation of tinnitus and hearing loss in 20 patients with sigmoid sinusoidal tinnitus and low-frequency sensorineural hearing loss.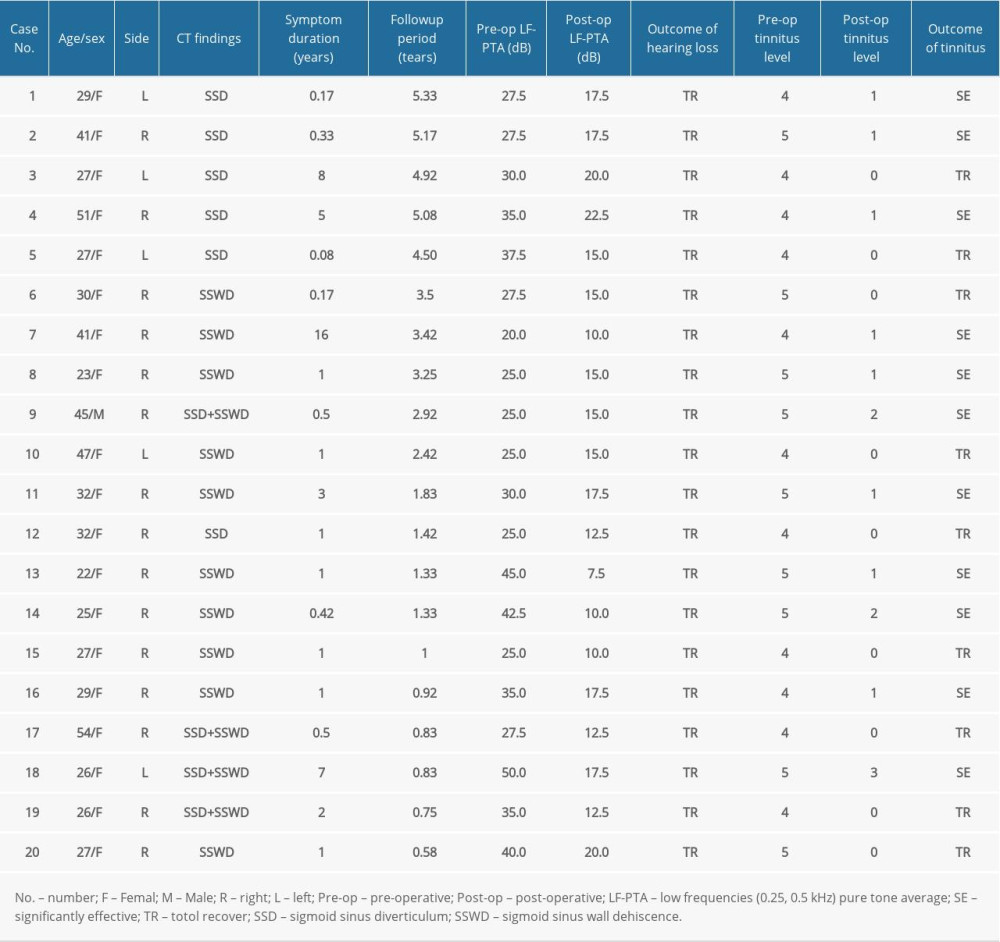
References
1. Baguley D, McFerran D, Hall D, Tinnitus: Lancet, 2013; 382(9904); 1600-7
2. Pattyn T, Van Den Eede F, Vanneste S, Tinnitus and anxiety disorders: A review: Hear Res, 2016; 333; 255-65
3. Bhatt JM, Bhattacharyya N, Lin HW, Relationships between tinnitus and the prevalence of anxiety and depression: Laryngoscope, 2017; 127(2); 466-69
4. Chari DA, Limb CJ, Tinnitus: Med Clin North Am, 2018; 102(6); 1081-93
5. Liu XD, Fan ZM, Research progress of vascular pulsatile tinnitus: J Clin Otolaryngol Head Neck Surg, 2017; 31(18); 1450-54
6. Wang D, Zhao Y, Tong B, Treatment of pulsatile tinnitus caused by anomalies of the sigmoid sinus wall via combined internal and external sigmoid sinus wall reconstruction with 3D temporal bone CT guidance: Eur Arch Otorhinolaryngol, 2020; 277(9); 2439-45
7. Eisenman DJ, Raghavan P, Hertzano R, Evaluation and treatment of pulsatile tinnitus associated with sigmoid sinus wall anomalies: Laryngoscope, 2018; 128(Suppl 2); S1-13
8. Jeon HW, Kim SY, Choi BS, Pseudo-low frequency hearing loss and its improvement after treatment may be objective signs of significant vascular pathology in patients with pulsatile tinnitus: Otol Neurotol, 2016; 37(9); 1344-49
9. Liu BDiscussion on the grade of tinnitus and the standard of efficacy evaluation: Chin J Integr Chin West Med Otolaryngol, 2004; 4; 181-83 [in Chinese]
10. Guidelines for the diagnosis and treatment of sudden deafness (2015): Chin J Otolaryngol Head Neck Surg, 2015; 50(6); 443-46 [in Chinese]
11. Schoeff S, Nicholas B, Mukherjee S, Imaging prevalence of sigmoid sinus dehiscence among patients with and without pulsatile tinnitus: Otolaryngol Head Neck Surg, 2014; 150(5); 841-46
12. Xu S, Ruan S, Liu S, CTA/V detection of bilateral sigmoid sinus dehiscence and suspected idiopathic intracranial hypertension in unilateral pulsatile tinnitus: Neuroradiology, 2018; 60(4); 365-72
13. Liu Z, Dong C, Wang X, Association between idiopathic intracranial hypertension and sigmoid sinus dehiscence/diverticulum with pulsatile tinnitus: A retrospective imaging study: Neuroradiology, 2015; 57(7); 747-53
14. Dong C, Zhao PF, Yang JG, Incidence of vascular anomalies and variants associated with unilateral venous pulsatile tinnitus in 242 patients based on dual-phase contrast-enhanced computed tomography: Chin Med J (Engl), 2015; 128(5); 581-85
15. Cuellar H, Maiti T, Patra DP, Endovascular treatment of pulsatile tinnitus by sigmoid sinus aneurysm: Technical note and review of the literature: World Neurosurg, 2018; 113; 238-43
16. Wang GP, Zeng R, Ma XB, Surgical treatment of pulsatile tinnitus caused by the sigmoid sinus diverticulum: A preliminary study: Medicine (Baltimore), 2015; 94(21); e882
17. Wang AC, Nelson AN, Pino C, Management of sigmoid sinus associated pulsatile tinnitus: A systematic review of the literature: Otol Neurotol, 2017; 38(10); 1390-96
18. Yeo WX, Xu SH, Tan TY, Surgical management of pulsatile tinnitus secondary to jugular bulb or sigmoid sinus diverticulum with review of literature: Am J Otolaryngol, 2018; 39(2); 247-52
Figures
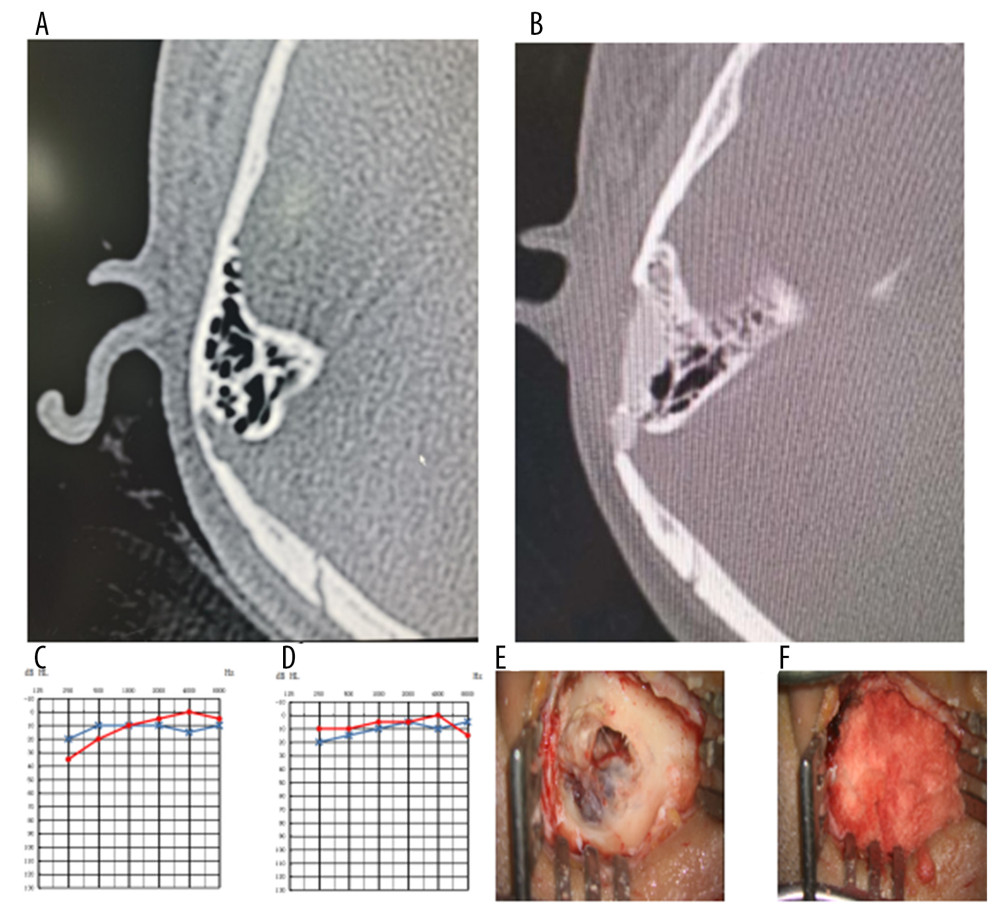 Figure 1. A typical case of sigmoid sinusoidal tinnitus and low-frequency sensorineural hearing loss (right sigmoid sinus diverticulum [SSD]). (A) Preoperative temporal bone computed tomography (CT). (B) Postoperative temporal bone CT. (C) Preoperative pure-tone audiometry (PTA). (D) Postoperative PTA. (E) Intraoperative SSD. (F) After excision of the sigmoid diverticulum during the operation, the autologous bone powder was covered. In PTA, the dotted red line represents the right side; the star blue line represents the variation of the left.
Figure 1. A typical case of sigmoid sinusoidal tinnitus and low-frequency sensorineural hearing loss (right sigmoid sinus diverticulum [SSD]). (A) Preoperative temporal bone computed tomography (CT). (B) Postoperative temporal bone CT. (C) Preoperative pure-tone audiometry (PTA). (D) Postoperative PTA. (E) Intraoperative SSD. (F) After excision of the sigmoid diverticulum during the operation, the autologous bone powder was covered. In PTA, the dotted red line represents the right side; the star blue line represents the variation of the left.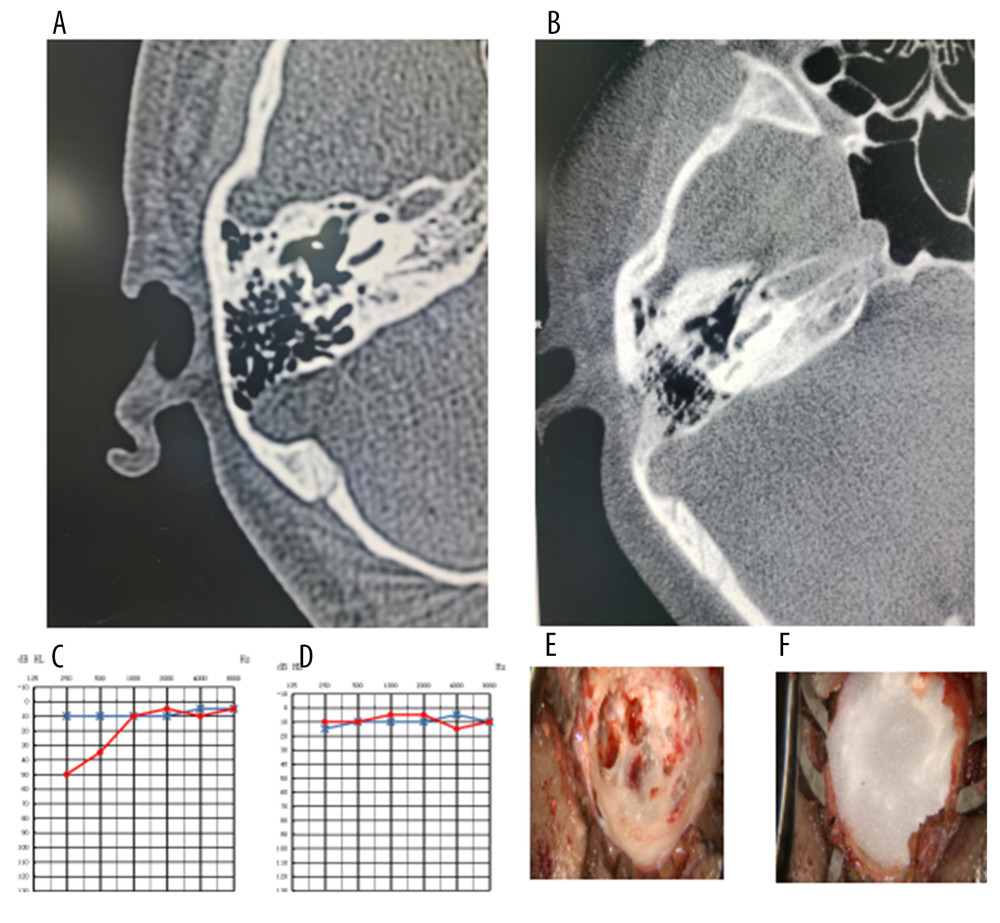 Figure 2. A typical case of sigmoid sinusoidal tinnitus and low-frequency sensorineural hearing loss (the defect in the bone wall of the right sigmoid sinus forms a resonating cavity). (A) Preoperative temporal bone computed tomography (CT). (B) Postoperative temporal bone CT. (C) Preoperative pure-tone audiometry (PTA). (D) Postoperative PTA. (E) Resonance cavity formation was observed intraoperatively. (F) After excision of the resonance cavity during the operation, the autologous bone powder was covered. In PTA, the dotted red line represents the right side; the star blue line represents the variation of the left.
Figure 2. A typical case of sigmoid sinusoidal tinnitus and low-frequency sensorineural hearing loss (the defect in the bone wall of the right sigmoid sinus forms a resonating cavity). (A) Preoperative temporal bone computed tomography (CT). (B) Postoperative temporal bone CT. (C) Preoperative pure-tone audiometry (PTA). (D) Postoperative PTA. (E) Resonance cavity formation was observed intraoperatively. (F) After excision of the resonance cavity during the operation, the autologous bone powder was covered. In PTA, the dotted red line represents the right side; the star blue line represents the variation of the left. Tables
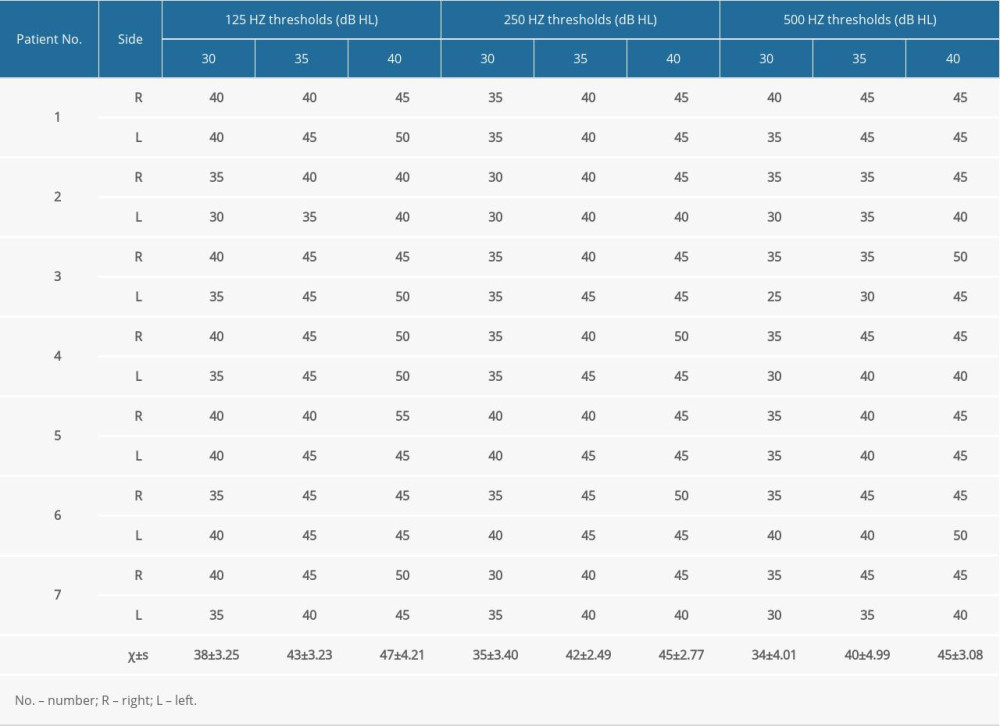 Table 1. Masking thresholds of healthy subjects with different masking intensity.
Table 1. Masking thresholds of healthy subjects with different masking intensity.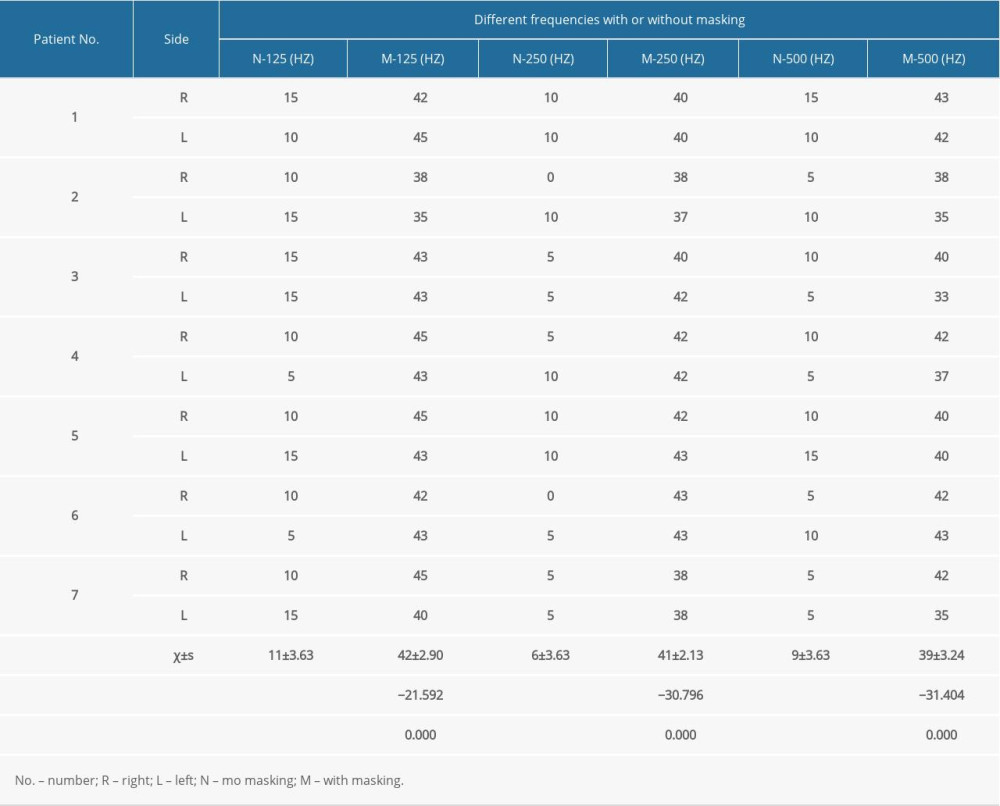 Table 2. Different frequency thresholds of healthy participants with or without masking.
Table 2. Different frequency thresholds of healthy participants with or without masking.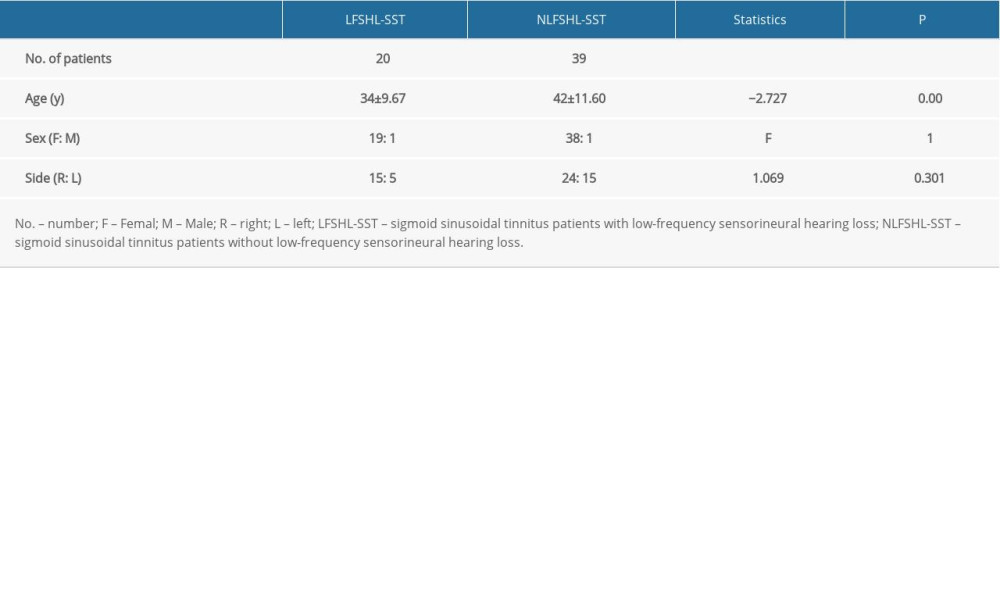 Table 3. Clinical summary of patients with sigmoid sinusoidal tinnitus.
Table 3. Clinical summary of patients with sigmoid sinusoidal tinnitus.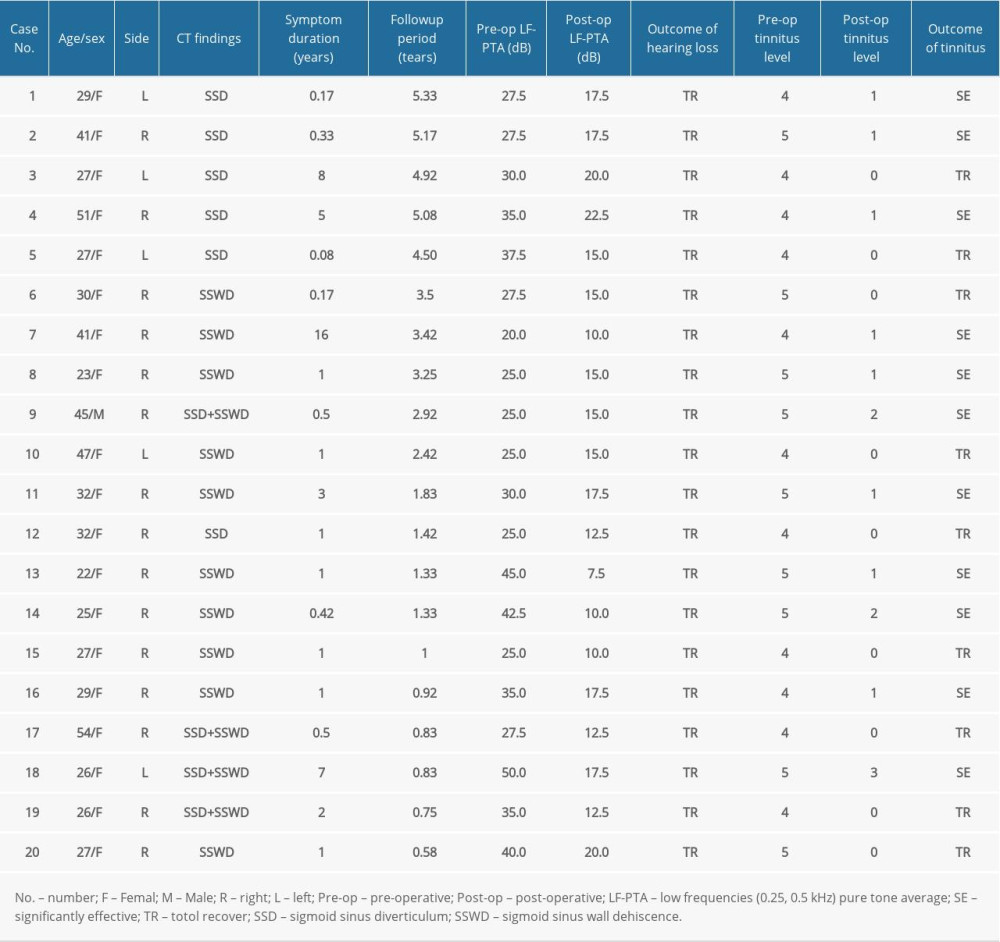 Table 4. Efficacy evaluation of tinnitus and hearing loss in 20 patients with sigmoid sinusoidal tinnitus and low-frequency sensorineural hearing loss.
Table 4. Efficacy evaluation of tinnitus and hearing loss in 20 patients with sigmoid sinusoidal tinnitus and low-frequency sensorineural hearing loss.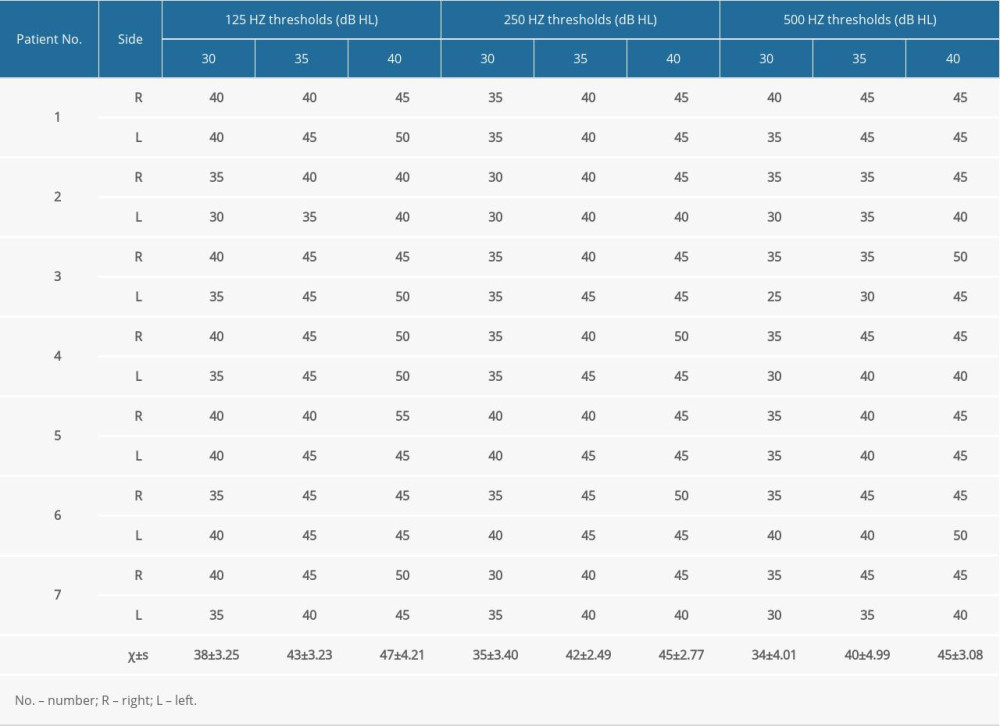 Table 1. Masking thresholds of healthy subjects with different masking intensity.
Table 1. Masking thresholds of healthy subjects with different masking intensity.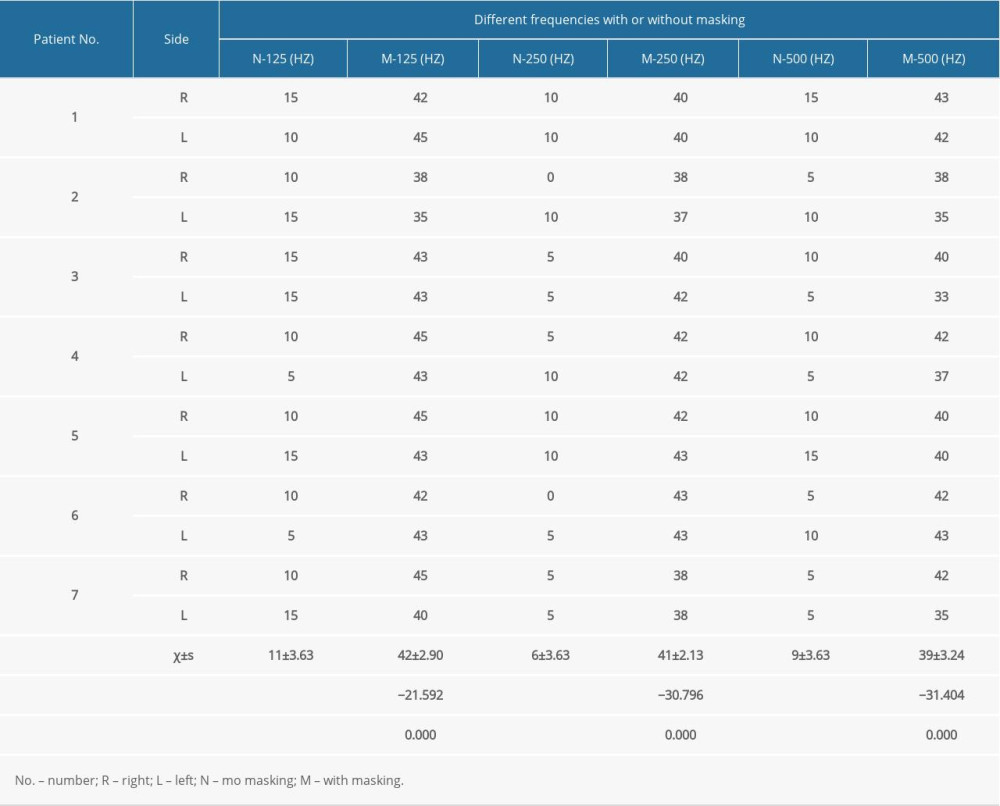 Table 2. Different frequency thresholds of healthy participants with or without masking.
Table 2. Different frequency thresholds of healthy participants with or without masking.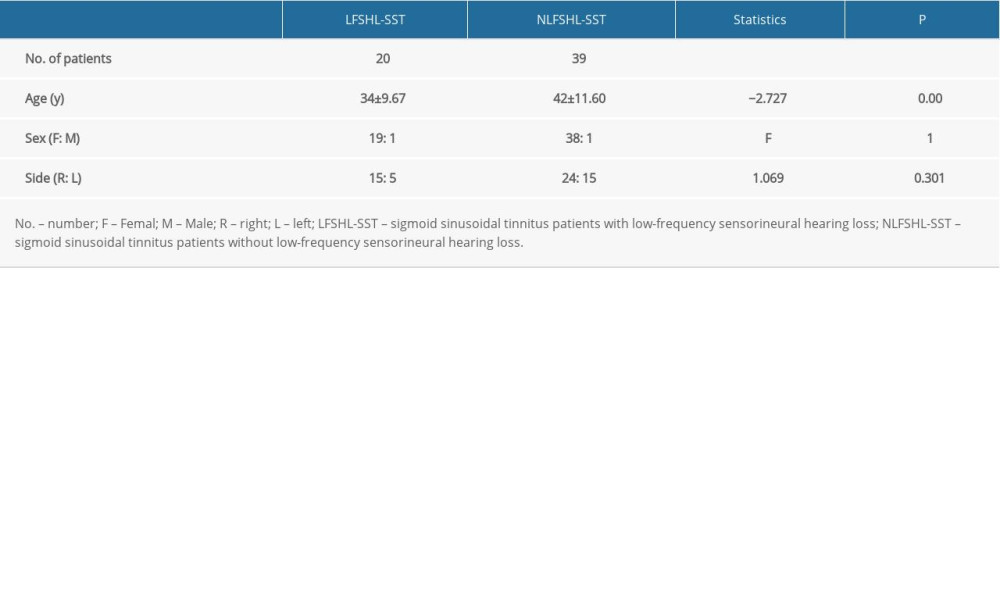 Table 3. Clinical summary of patients with sigmoid sinusoidal tinnitus.
Table 3. Clinical summary of patients with sigmoid sinusoidal tinnitus.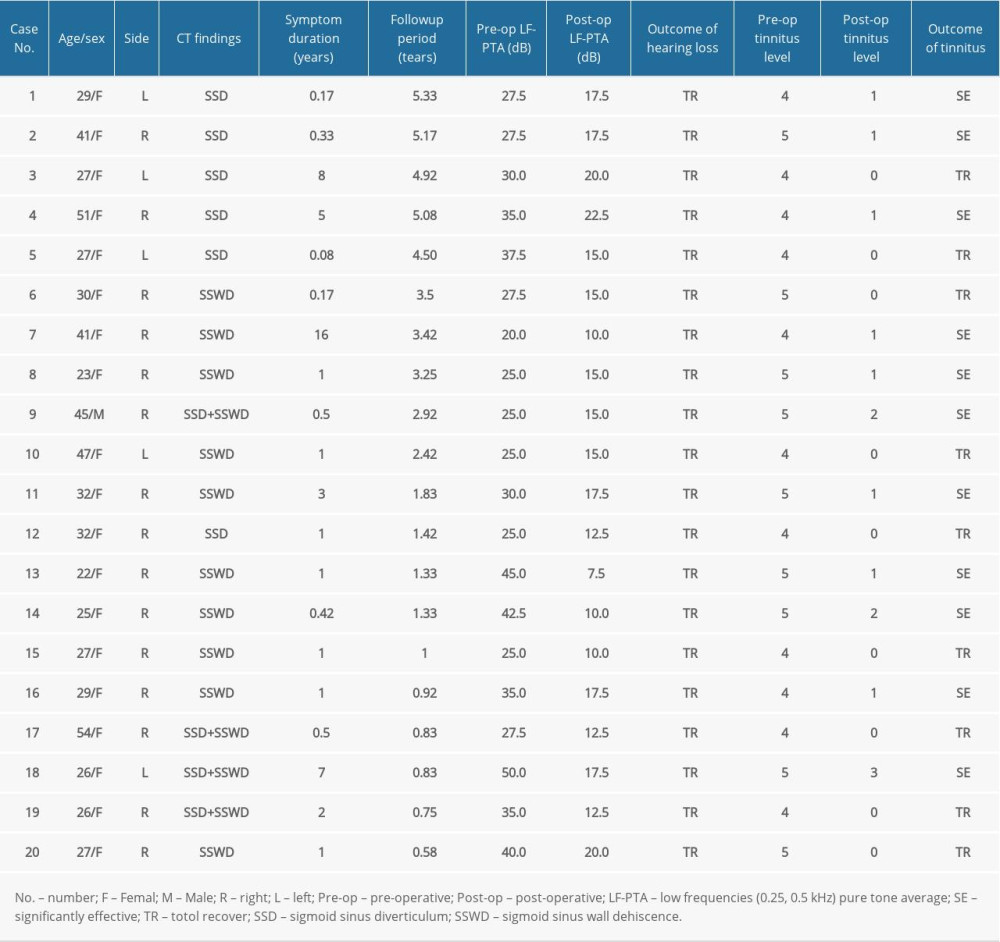 Table 4. Efficacy evaluation of tinnitus and hearing loss in 20 patients with sigmoid sinusoidal tinnitus and low-frequency sensorineural hearing loss.
Table 4. Efficacy evaluation of tinnitus and hearing loss in 20 patients with sigmoid sinusoidal tinnitus and low-frequency sensorineural hearing loss. In Press
06 Mar 2024 : Clinical Research
Comparison of Outcomes between Single-Level and Double-Level Corpectomy in Thoracolumbar Reconstruction: A ...Med Sci Monit In Press; DOI: 10.12659/MSM.943797
21 Mar 2024 : Meta-Analysis
Economic Evaluation of COVID-19 Screening Tests and Surveillance Strategies in Low-Income, Middle-Income, a...Med Sci Monit In Press; DOI: 10.12659/MSM.943863
10 Apr 2024 : Clinical Research
Predicting Acute Cardiovascular Complications in COVID-19: Insights from a Specialized Cardiac Referral Dep...Med Sci Monit In Press; DOI: 10.12659/MSM.942612
06 Mar 2024 : Clinical Research
Enhanced Surgical Outcomes of Popliteal Cyst Excision: A Retrospective Study Comparing Arthroscopic Debride...Med Sci Monit In Press; DOI: 10.12659/MSM.941102
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








