30 March 2021: Clinical Research
Finite Element Analysis of Femoral Neck Fracture Treated with Bidirectional Compression-Limited Sliding Screw
Hai Huang12ABCDEFG, Zhengkuan Feng3CE, Weifei Wang4AD, Cheng Yang2B, Jianwen Liao2F, Jun Ouyang3F*DOI: 10.12659/MSM.929163
Med Sci Monit 2021; 27:e929163
Abstract
BACKGROUND: The rate of femoral neck shortening after internal fixation for femoral neck fracture is high and this complication reduces the function of the affected lower limb. The aim of this study was to design a bidirectional compression-limited sliding screw (BCLSC) that can achieve a full balance between retaining the sliding pressure of the ends of and maintaining the length of the femoral neck.
MATERIAL AND METHODS: We constructed a 3-dimensional model of a Pauwels III femoral neck fracture and models of 3 internal fixation methods (3 cannulated screws [3CS], dynamic hip screw [DHS]+CS, and BCLSC) by finite element analysis (FEA).The finite element model simulated the loading of the human body when standing on 1 leg. Displacement and stress distribution of the models were calculated based on an axial stress of 600 N.
RESULTS: The peak von Mises stress (VMS) values of fracture ends in the 3CS, DHS+CS and BCLSC groups were 94.687 MPa, 26.375 MPa and 45.698 MPa; the peak VMS values of internal fixed stress were 451.53 MPa, 174.45 MPa, and 337.34 MPa; the peak VMS values of the lateral femoral wall were 70.021 MPa, 53.033 MPa, and 20.009 MPa; maximum displacements of the femoral head were 1.4482 mm, 1.3813 mm, and 1.3889 mm; and the internal fixed displacement peaks were 4.1134 mm, 3.91 mm, and 4.1004 mm, respectively.
CONCLUSIONS: The FEA showed that compared with the CS, the new BCLSC showed better performance in resisting shearing force for Pauwels III femoral neck fracture, with better mechanical properties. These data provide a basis for further experiments and clinical application.
Keywords: Bone Screws, Femoral Neck Fractures, Finite Element Analysis, Biomechanical Phenomena, Femur Neck, Fracture Fixation, Internal, healthy volunteers, Models, Anatomic, Pressure
Background
The fracture of the femur is a common type of hip fracture, which can occur at all ages and is a health problem affecting people worldwide. Approximately 1.7 million patients have a femoral neck fracture every year worldwide, and these numbers can increase with a growing aging society. By 2050, the number of patients with femoral neck fracture is estimated to be 6.7 million annually [1]. Due to the characteristics of the proximal femoral anatomical structure and biomechanics and the femoral head blood supply, complications often occur after the internal fixation of femoral neck fracture, such as nonunion and femoral head necrosis. It is very difficult to identify ways to improve the internal fixation success rate in orthopedic trauma treatment [2,3].
Recently, with the improved understanding of the femoral head blood supply, the success rate of the internal fixation of femoral neck fractures has improved. However, with the general improvement in patient quality of life, the problem of postoperative femoral neck shortening has attracted more attention. Owing to the anatomical biomechanics of the femoral neck and the healing characteristics of femoral neck fracture, femoral neck shortening is common after femoral neck fracture surgery, and the incidence of shortening has been reported to occur in 27% to 66% of cases [4–8]. Excessive shortening after femoral neck surgery can reduce lower limb gait function and even cause hip joint dysfunction, especially for patients with osteoporosis, which greatly reduces patient quality of life.
In accordance with the anatomical biomechanics of the femoral neck and the healing characteristics of femoral neck fracture and to promote fracture healing and reduce the incidence of postoperative shortening of the femoral neck, we designed a double-threaded compression-limiting sliding screw. First, the screw has a double-thread compression fixation. The inner core and outer sleeve of the screw have a “hexagonal” chimeric structure, which has the characteristics of coaxial movement. In the process of inserting the inner core, the outer sleeve can be placed at the same time. In the design, the screw head and the screw tail have threads, and the screw pitch at the end of the screw is less than the screw pitch of the screw head. Because the screw head and the end of the screw were limited by the thread, the tail side of the screw could not exit from the lateral bone cortex. Second, the design of the screw imitated the principle of a sliding compression plate. The outer sleeve of the screw tail was fixed into the lateral cortical bone of the femur, so that the inner core of the screw could be limited by sliding in the sleeve. The limited sliding process of the screw promoted fracture healing and helped to avoid excessive shortening of the femoral neck (Figure 1).
To confirm whether the modular structure design of the new bidirectional compression-limited sliding screw (BCLSC) provided adequate stability, we analyzed the von Mises stress (VMS) and displacement of the new screw system and compared it with the 2 traditional methods (3 cannulated screws [3CS] and a dynamic hip screw [DHS]+CS) of repairing Pauwels type III femoral neck fracture by finite element analysis (FEA).We further evaluated the mechanical stability of the new BCLSC, and provided a theoretical basis for its clinical application.
Material and Methods
THE 3-DIMENSIONAL MODEL OF FEMORAL NECK FRACTURE AND INTERNAL FIXATION:
We recruited a healthy 30-year-old man with a body weight of 60 kg as a volunteer participant. The existence of hip injury and disease were excluded by a physician. The left femur was scanned layer by layer using a spiral computed tomography (CT) scanner (Toshiba 64-row 128-slice CT scanner; Toshiba, Tokyo, Japan), and the raw data were collected in DICOM format. After inputting the raw data into Mimics21.0 software (Materialise, Leuven, Belgium), the 3-dimensional (3D) model was preliminarily established by image segmentation, delineation, and edge smoothness, and the model data file was outputted in STL format. The STL format file generated by Mimics was inputted into Geomagic software (3DSystems Inc, Rock Hill, SC, USA) for smoothing, editing contour lines, surface generation, and surface fitting, and then the file was outputted in common STP geometry model format. Finally, we inputted the STP geometric model format file into SolidWorks software (Dassault Systemes, Vélizy-Villacoublay, France) for solid reconstruction, and a Pauwels III fracture was created in the 3D model (Pauwels Angle >70°; Figure 2). The feature/surface module in SolidWorks software was used for modeling various types of internal fixation (CS with thread diameter 7.3 mm, DHS system, BCLSC), and the model was saved in SLDPRT format. Next, the different types of screws were assembled into the bone. Finally, we obtained 3 fracture internal fixation 3D models by using the combination process overlapping part of the intersection (Figure 3).
FINITE ELEMENT MODEL ANALYSIS:
The model generated in SolidWorks was input into Ansys software (Ansys, Canonsburg, PA, USA), and the material property parameters of cortical bone, cancellous bone, and internal fixation were calculated [9, 10]. Different contact surfaces were defined with different contact relations as follows: The fracture surface was set to friction (friction coefficient=0.24). Frictional contact was used between the screw and sleeve (friction coefficient=0.2), The threaded screw area was used for binding to the bone, and the non-threaded area remained frictional contact with the bone (friction coefficient=0.24).
Finally, the model was meshed. To ensure that the calculation accuracy met the requirements of analysis, the mesh type and mesh size were controlled, with the mesh type set as a hexahedral mesh, and the mesh size set as 1.5 mm (Table 1).
BOUNDARY CONDITIONS AND LOADS:
A simplified bone model was created, and the force of the acetabular fossae on the femoral head was mainly used to simulate the force of the unilateral femur during walking (close to the midpoint data of the normal human walking cycle). Six degrees of freedom were fixed on the bone surface of the distal femur, and a 600 N load was applied vertically down from the femoral head [11,12] (Figure 4).
EVALUATION INDEX:
To evaluate the different internal fixation methods for femoral neck fractures under mechanical loading conditions, we needed to focus on the following variables: (1) VMS peak and distribution of fracture broken ends; (2) VMS peak and distribution of internal fixation; (3) VMS peak and distribution on the lateral wall of the femur; (4) displacement distribution and peak value of the femoral head and internal fixation; and (5) displacement distribution and peak value, and VMS distribution and peak value of the inside of the new screw type.
Results
VMS DISTRIBUTION AT FRACTURE ENDS:
The stress distribution at the femoral neck section showed that the stress peaks of all models were concentrated in the contact region of the medial femur with the internal fixation and the proximal medial femur near the lesser trochanter. The peak stress of fracture end of the 3CS group was 94.687 MPa, and that of the DHS+CS group was 26.375 MPa. Compared with the stress peak of the 3CS group, that of the BCLSC group was significantly lower at 45.698 MPa (Figure 5, Table 2).
VMS DISTRIBUTION AND PEAK VALUES OF INTERNAL FIXATION:
Stress distribution maps of the internal fixation methods showed that the stress of internal fixation was concentrated in 3 areas: where the head and tail of the screw contacted the bone, in the screw itself, and at the broken end of the bone. The peak stress was 451.53 MPa in the 3CS group, 174.45 MPa in the DHS+CS group, and 337.34 MPa in the BCLSC group. In the 3CS and BCLSC groups, the stress peak of the posterior upper distributed screw was the highest.
STRESS DISTRIBUTION AND PEAK VALUES AT THE LATERAL FEMORAL WALL:
According to the map of stress distribution at the femoral lateral wall, the stress peak value in the 3CS group was 70.021 MPa and was concentrated in the area where the distal screw was in contact with bone. In the DHS+CS group, the stress peak was 53.033 MPa, concentrated in the area where the proximal screw contacted the bone. The BCLSC group had no obvious stress concentration, and its stress peak value was only 20.009 MPa.
FEMORAL HEAD AND INTERNAL FIXATION DISPLACEMENT PEAK AND DISTRIBUTION:
Due to axial force on the neck of the femur, the femoral head sunk and shifted downward. Displacement maps of the femoral head and internal fixation showed that the displacement of the femoral head in the 3 groups was as follows: the maximum displacements of the femoral head were 1.4482 mm, 1.3813 mm, and 1.3889 mm in the 3CS, DHS+CS, and BCLSC groups, respectively. The displacement direction was the same on the internal fixator and the femur. The internal fixator displacement of the 3 groups was concentrated on the screw head under the femoral head and was decreased from the head to the tail of the screw. The maximum internal fixation displacement values of different groups were 4.1134 mm, 3.91 mm, and 4.1004 mm in the 3CS, DHS+CS, and BCLSC groups, respectively. In the 3CS and BCLSC groups, the displacement peak values were largest at the head of the screw on the upper screws.
DISPLACEMENT AND STRESS DISTRIBUTION OF THE BCLSC:
The stress distribution of the BCLSC showed that the stress of the inner core was concentrated at the junction of the tail end and the outercoat and was distributed evenly and gradually toward the proximal screw end. However, the stress peak of the outercoat was concentrated at the junction of the outercoat head and the inner core. The displacement peaks of the inner core and the outercoat were located at the proximal screw end.
Discussion
LIMITATIONS:
This study has some limitations. First, data analyses of the joint capsule, ligament, and periosteum were not included. Second, only a single perpendicular stress to the femoral head was applied, which did not replicate the complex stress under the normal physiological conditions; therefore, the experimental results will be somewhat different from actual clinical conditions. Further biomechanical experiments are needed to verify the results. Third, in this study, only the inverted triangle fixation was compared, and the different combination of screws was ignored. Finally, this study was limited to the observation of immediate stability after fracture fixation, and could not completely simulate the biomechanical process of fracture healing. Thus, further clinical trials and observations need to be performed.
Conclusions
In this study, the FEA results showed that compared with the CS, the new BCLSC showed a better performance in resisting shearing force for Pauwels type III femoral neck fracture, with better mechanical properties. These data provide a basis for further experiments and clinical application.
Figures
 Figure 1. (A, B) Design of a new type of sliding screw with bidirectional compression limits for the femoral neck.
Figure 1. (A, B) Design of a new type of sliding screw with bidirectional compression limits for the femoral neck. 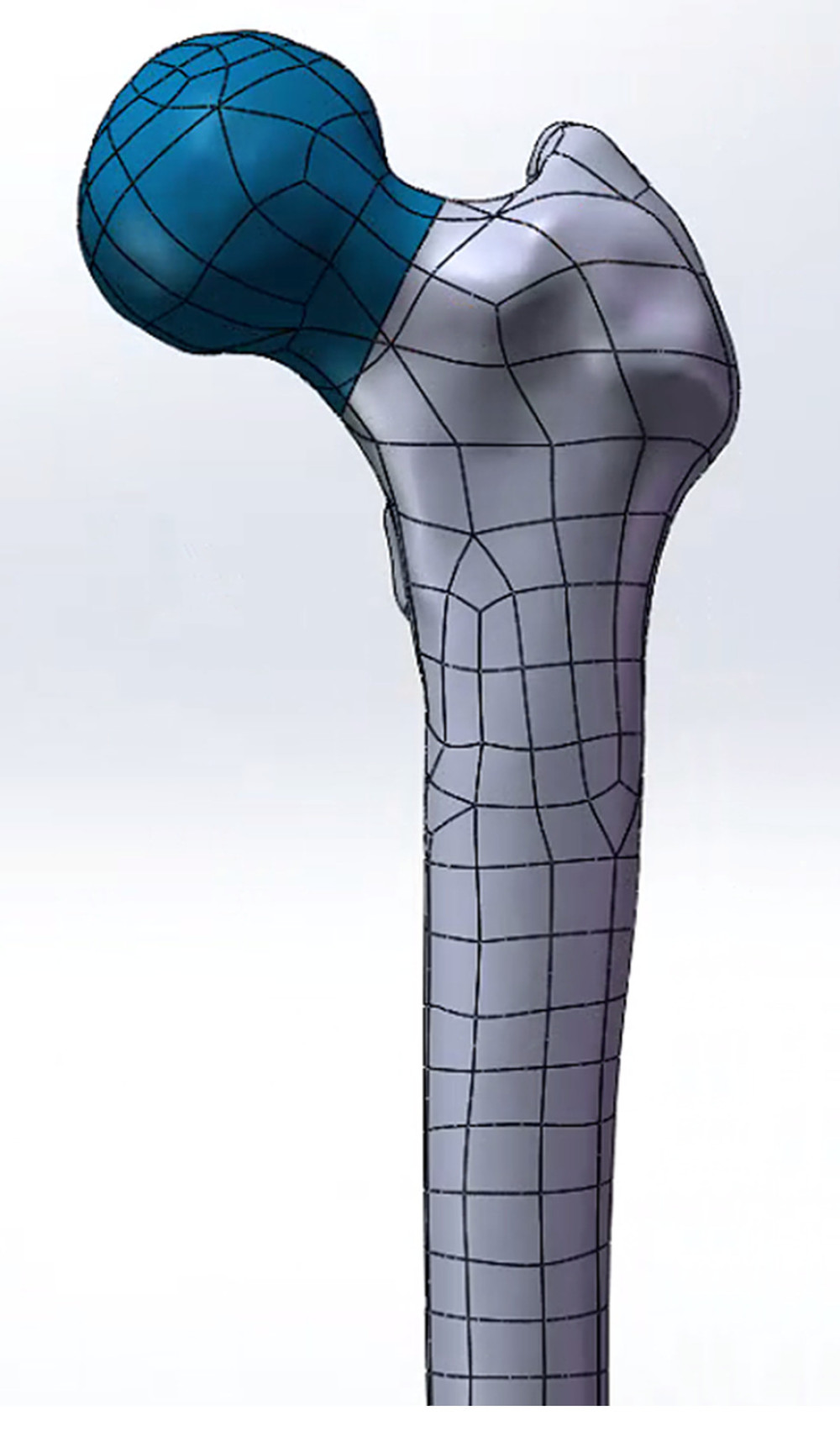 Figure 2. Femoral neck fracture; Pauwels type III fracture.
Figure 2. Femoral neck fracture; Pauwels type III fracture. 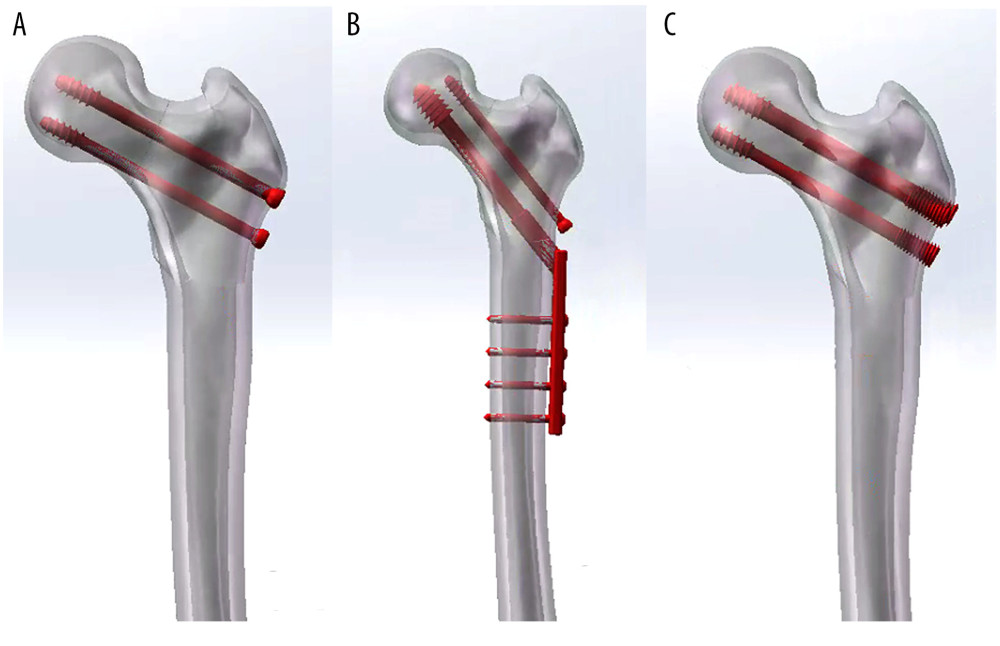 Figure 3. Model of a femoral neck fracture treated with internal fixation in the 3 groups: (A) 3 cannulated screws (3CS); (B) dynamic hip screw and cannulated screw (DHS+CS); (C) bidirectional compression-limited sliding screw (BCLSC).
Figure 3. Model of a femoral neck fracture treated with internal fixation in the 3 groups: (A) 3 cannulated screws (3CS); (B) dynamic hip screw and cannulated screw (DHS+CS); (C) bidirectional compression-limited sliding screw (BCLSC). 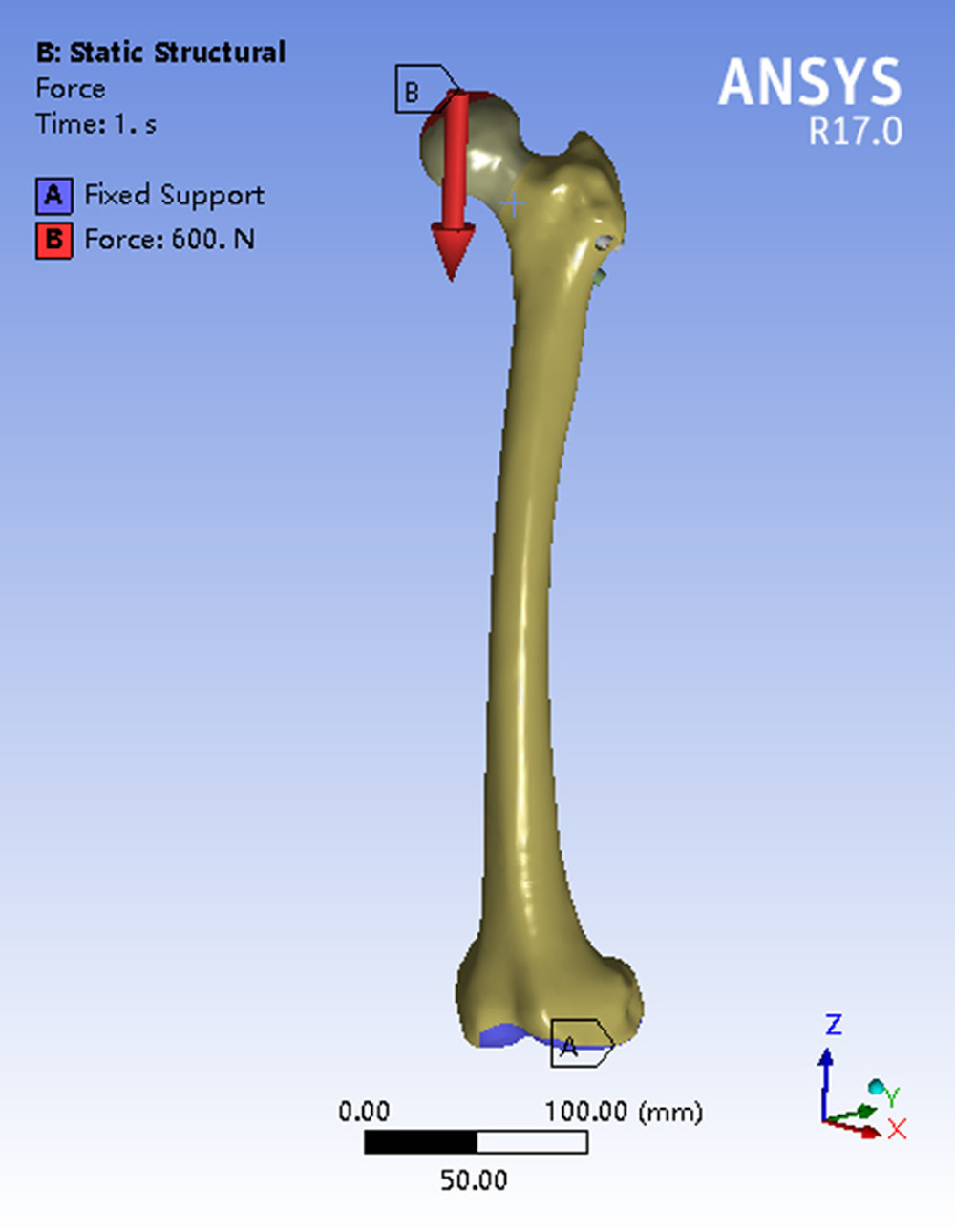 Figure 4. Schematic diagram of mechanical loading.
Figure 4. Schematic diagram of mechanical loading. 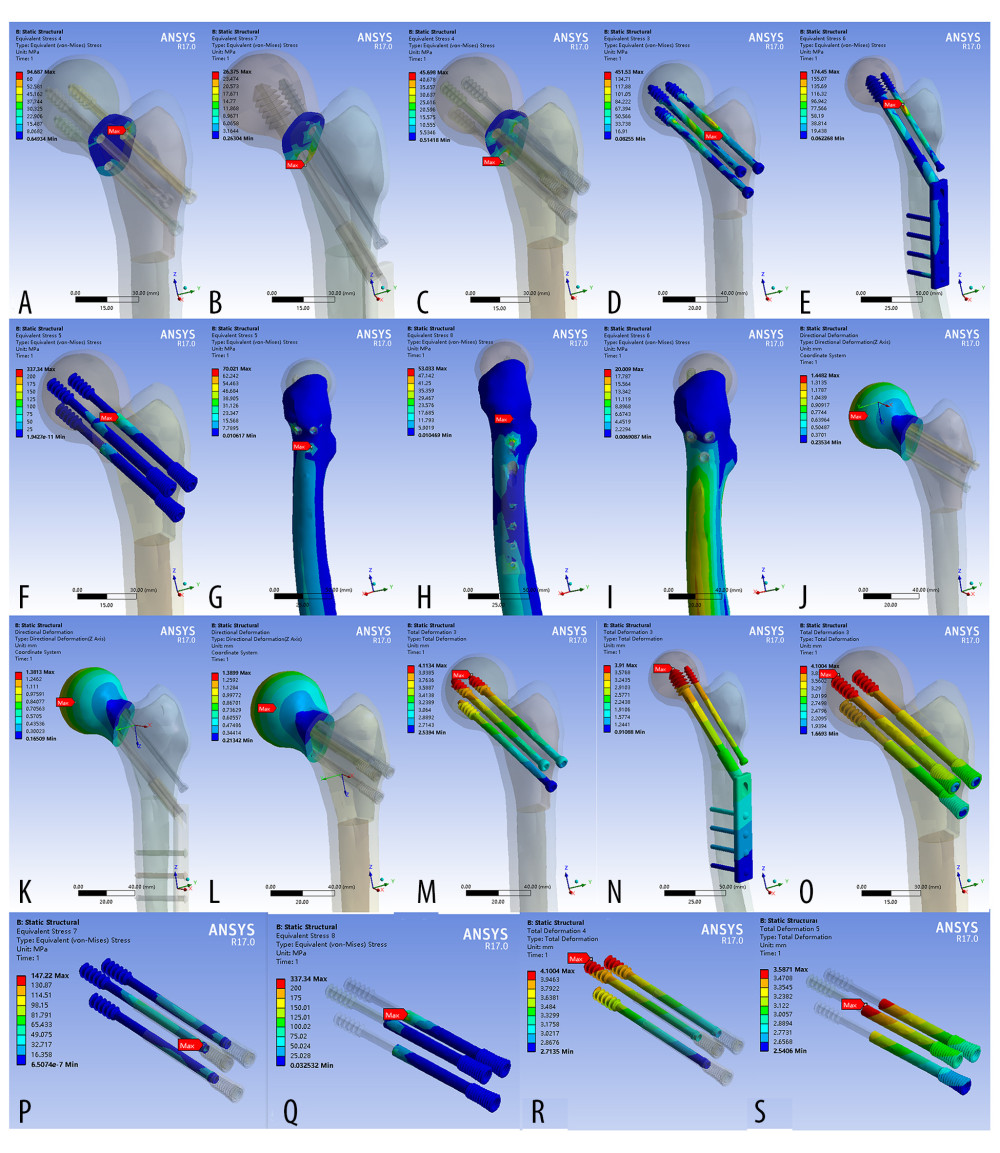 Figure 5. Finite element stress and displacement map of the model. (A–C) Stress distribution map of the fractured bone ends of the finite element model; (D–F) Map of internal fixed stress distribution in the finite element model; (G–I) Map of stress distribution on the lateral femoral wall of the finite element model; (J–L) Distribution map of femoral head displacement in the finite element model; (M–O) Map of internal fixed displacement distribution in the finite element model; (P–Q) Map of stress distribution in the internal structure of the bidirectional compression-limited sliding screw (BCLSC); (R–S) Map of displacement distribution of internal structure of the BCLSC.
Figure 5. Finite element stress and displacement map of the model. (A–C) Stress distribution map of the fractured bone ends of the finite element model; (D–F) Map of internal fixed stress distribution in the finite element model; (G–I) Map of stress distribution on the lateral femoral wall of the finite element model; (J–L) Distribution map of femoral head displacement in the finite element model; (M–O) Map of internal fixed displacement distribution in the finite element model; (P–Q) Map of stress distribution in the internal structure of the bidirectional compression-limited sliding screw (BCLSC); (R–S) Map of displacement distribution of internal structure of the BCLSC. References
1. Miyamoto RG, Kaplan KM, Levine BR, Surgical management of hip fractures: An evidence-based review of the literature. I: Femoral neck fractures: J Am Acad Orthop Surg, 2008; 16; 596-607
2. Estrada LS, Volgas DA, Stannard JP, Alonso JE, Fixation failure in femoral neck fractures: Clin Orthop Relat Res, 2002(399); 110-18
3. Davidovitch RI, Jordan CJ, Egol KA, Vrahas MS, Challenges in the treatment of femoral neck fractures in the nonelderly adult: J Trauma, 2010; 68; 236-42
4. Zlowodzki M, Ayeni O, Petrisor BA, Bhandari M, Femoral neck shortening after fracture fixation with multiple cancellous screws: incidence and effect on function: J Trauma, 2008; 64; 163-69
5. Zlowodzki M, Brink O, Switzer J, The effect of shortening and varus collapse of the femoral neck on function after fixation of intracapsular fracture of the hip: A multi-centre cohort study: J Bone Joint Surg Br, 2008; 90; 1487-94
6. Stockton DJ, Lefaivre KA, Deakin DE, Incidence, magnitude, and predictors of shortening in young femoral neck fractures: J Orthop Trauma, 2015; 29; e293-98
7. Slobogean GP, Stockton DJ, Zeng BF, Femoral neck shortening in adult patients under the age of 55 years is associated with worse functional outcomes: Analysis of the prospective multi-center study of hip fracture outcomes in China (SHOC): Injury, 2017; 48; 1837-42
8. Felton J, Slobogean GP, Jackson SS, Femoral neck shortening after hip fracture fixation is associated with inferior hip function: Results from the FAITH trial: J Orthop Trauma, 2019; 33; 487-96
9. Heiner AD, Structural properties of fourth-generation composite femurs and tibias: J Biomech, 2008; 41; 3282-84
10. Grassi L, Vaananen SP, Amin YS, Experimental validation of finite element model for proximal composite femur using optical measurements: J Mech Behav Biomed Mater, 2013; 21; 86-94
11. Kuan F, Hsu K, Lin C, Biomechanical properties of off-axis screw in Pauwels III femoral neck fracture fixation: Bicortical screw construct is superior to unicortical screw construct: Injury, 2019; 50; 1889-94
12. Samsami S, Saberi S, Sadighi S, Rouhi G, Comparison of three fixation methods for femoral neck fracture in young adults: Experimental and numerical investigations: J Med Biol Eng, 2015; 35; 566-79
13. Abdel Rahman AF, Gouda A, Ibrahim R, Methods of fixation used in management of femoral neck fractures in adults: A systematic review: Curr Orthop Pract, 2018; 29; 378-83
14. Ye Y, Hao J, Mauffrey C, Optimizing stability in femoral neck fracture fixation: Orthopedics, 2015; 38; 625-30
15. Stoffel K, Zderic I, Gras F, Biomechanical evaluation of the femoral neck system in unstable Pauwels III femoral neck fractures: A comparison with the dynamic hip screw and cannulated screws: J Orthop Trauma, 2017; 31; 131-37
16. Li J, Zhao Z, Yin P, Zhang L, Tang P, Comparison of three different internal fixation implants in treatment of femoral neck fracture - a finite element analysis: J Orthop Surg Res, 2019; 14; 76
17. Zlowodzki M, Nsson JA, Paulke R, Shortening after femoral neck fracture fixation: Clin Orthop Relat Res, 2007; 461; 213-18
18. Fixation using Alternative Implants for the Treatment of Hip fractures (FAITH) Investigators, Fracture fixation in the operative management of hip fractures (FAITH): An international, multicentre, randomised controlled trial: Lancet, 2017; 389; 1519-27
Figures
 Figure 1. (A, B) Design of a new type of sliding screw with bidirectional compression limits for the femoral neck.
Figure 1. (A, B) Design of a new type of sliding screw with bidirectional compression limits for the femoral neck.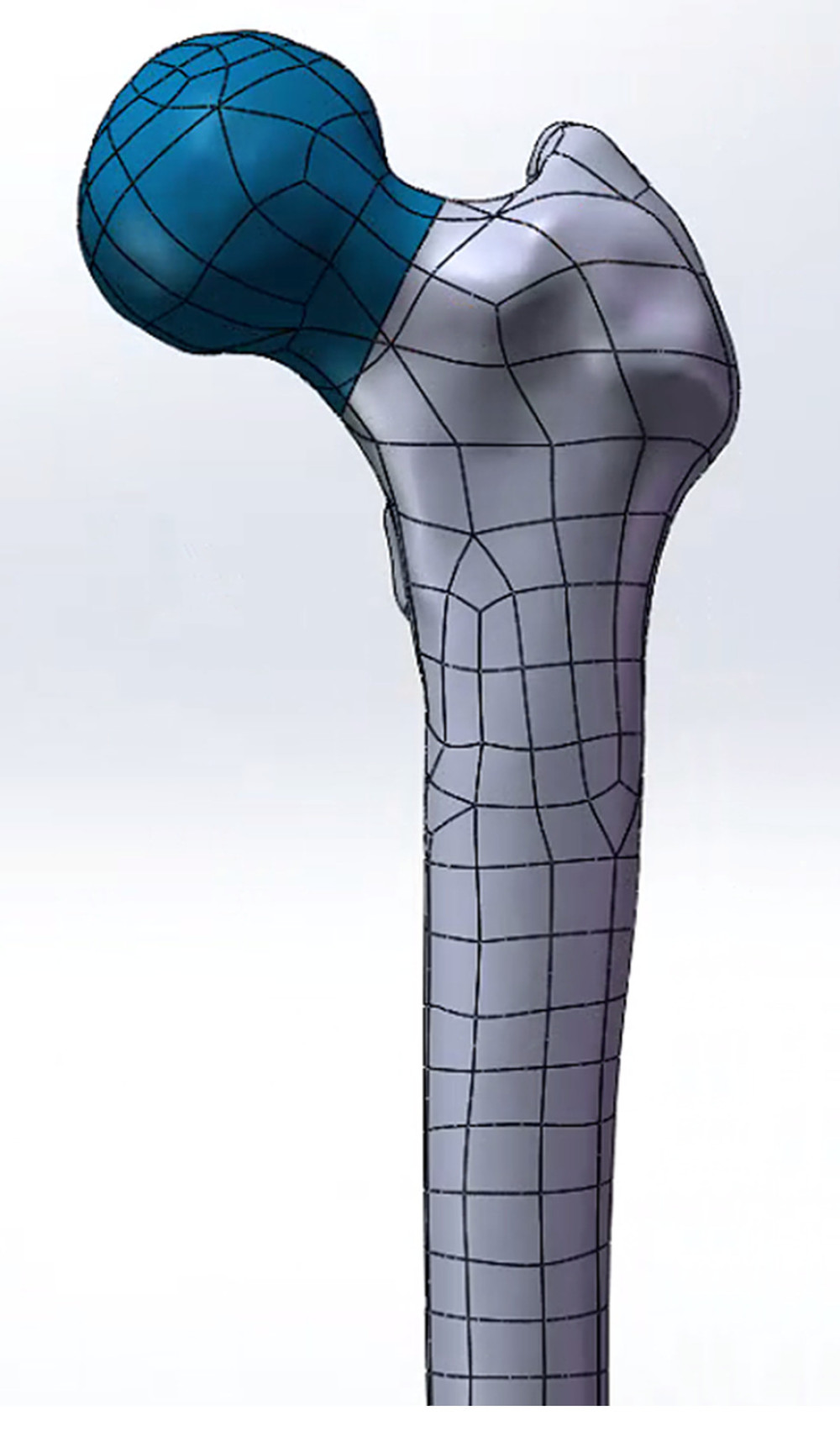 Figure 2. Femoral neck fracture; Pauwels type III fracture.
Figure 2. Femoral neck fracture; Pauwels type III fracture.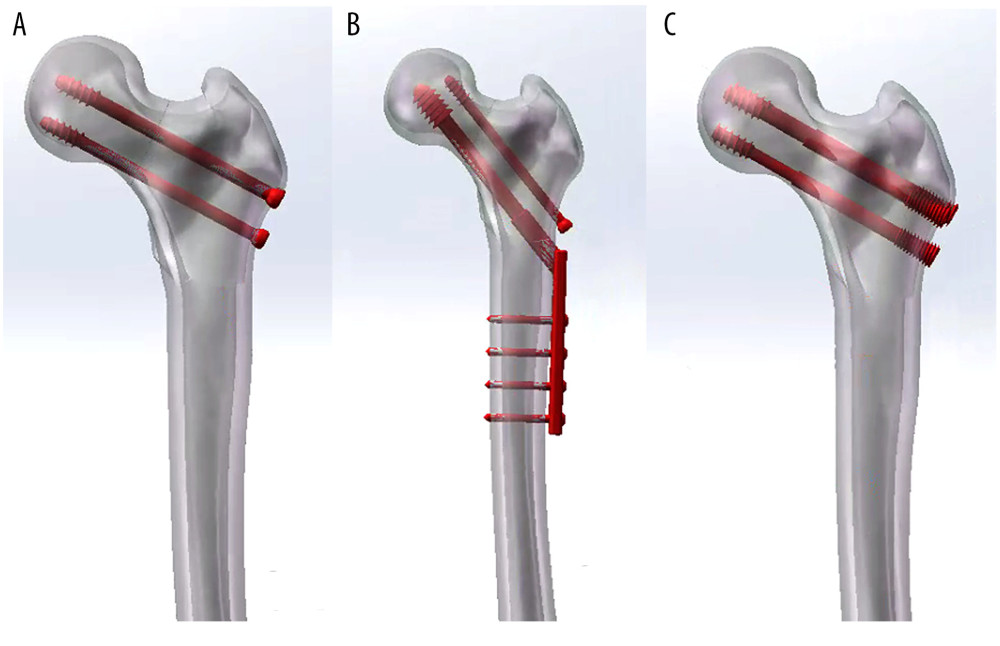 Figure 3. Model of a femoral neck fracture treated with internal fixation in the 3 groups: (A) 3 cannulated screws (3CS); (B) dynamic hip screw and cannulated screw (DHS+CS); (C) bidirectional compression-limited sliding screw (BCLSC).
Figure 3. Model of a femoral neck fracture treated with internal fixation in the 3 groups: (A) 3 cannulated screws (3CS); (B) dynamic hip screw and cannulated screw (DHS+CS); (C) bidirectional compression-limited sliding screw (BCLSC).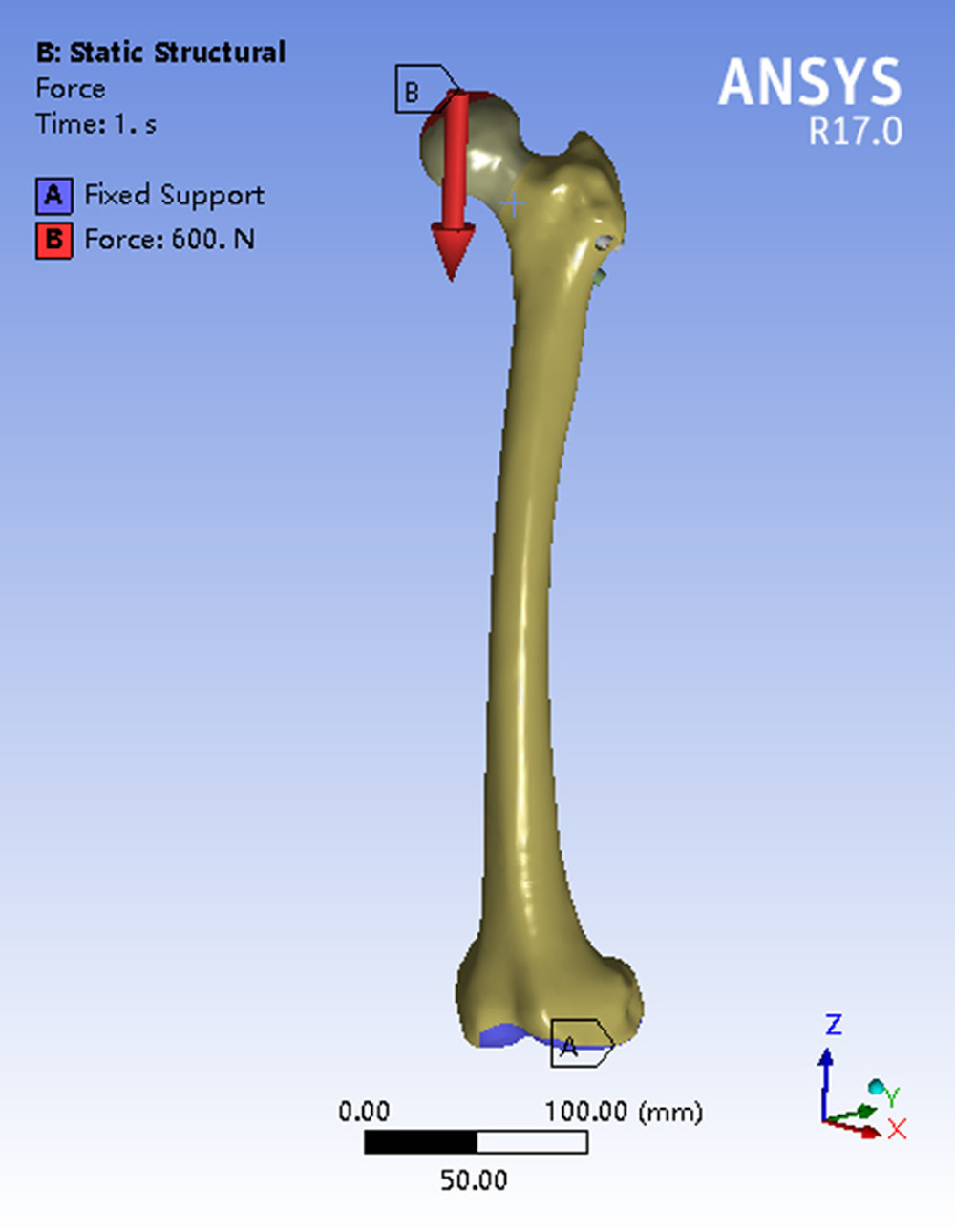 Figure 4. Schematic diagram of mechanical loading.
Figure 4. Schematic diagram of mechanical loading.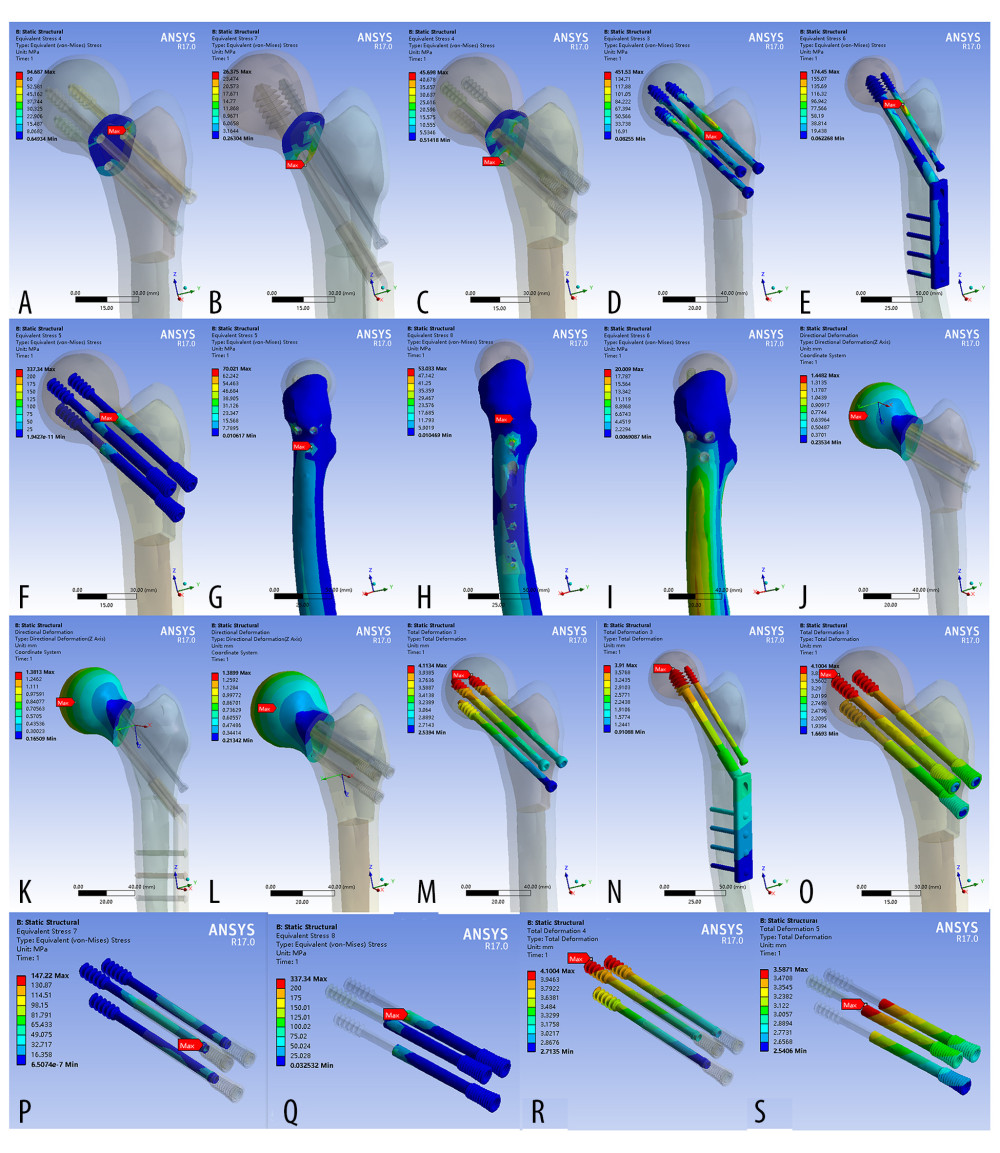 Figure 5. Finite element stress and displacement map of the model. (A–C) Stress distribution map of the fractured bone ends of the finite element model; (D–F) Map of internal fixed stress distribution in the finite element model; (G–I) Map of stress distribution on the lateral femoral wall of the finite element model; (J–L) Distribution map of femoral head displacement in the finite element model; (M–O) Map of internal fixed displacement distribution in the finite element model; (P–Q) Map of stress distribution in the internal structure of the bidirectional compression-limited sliding screw (BCLSC); (R–S) Map of displacement distribution of internal structure of the BCLSC.
Figure 5. Finite element stress and displacement map of the model. (A–C) Stress distribution map of the fractured bone ends of the finite element model; (D–F) Map of internal fixed stress distribution in the finite element model; (G–I) Map of stress distribution on the lateral femoral wall of the finite element model; (J–L) Distribution map of femoral head displacement in the finite element model; (M–O) Map of internal fixed displacement distribution in the finite element model; (P–Q) Map of stress distribution in the internal structure of the bidirectional compression-limited sliding screw (BCLSC); (R–S) Map of displacement distribution of internal structure of the BCLSC. Tables
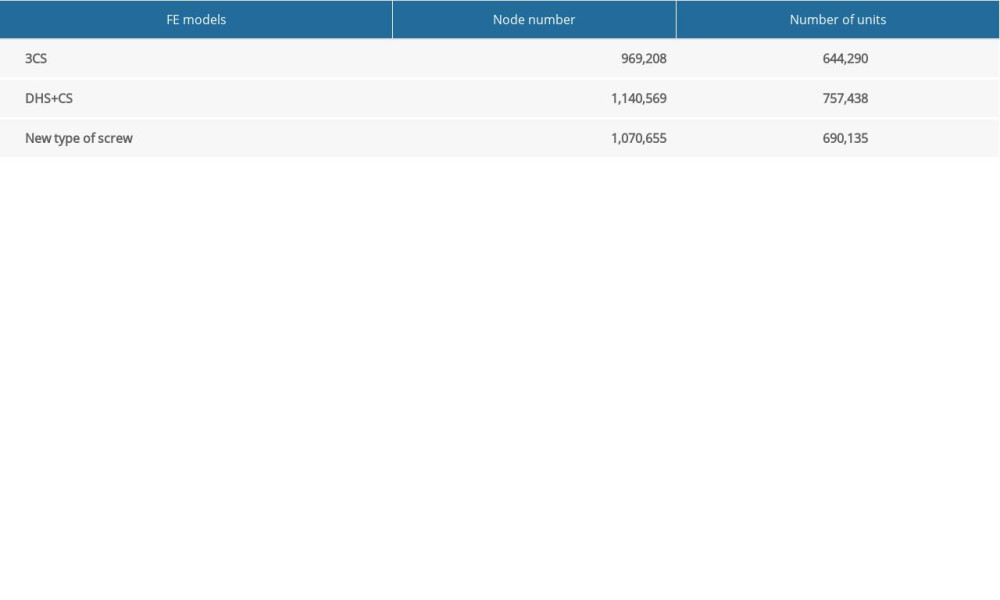 Table 1. Number of nodes and elements of the finite element model.
Table 1. Number of nodes and elements of the finite element model.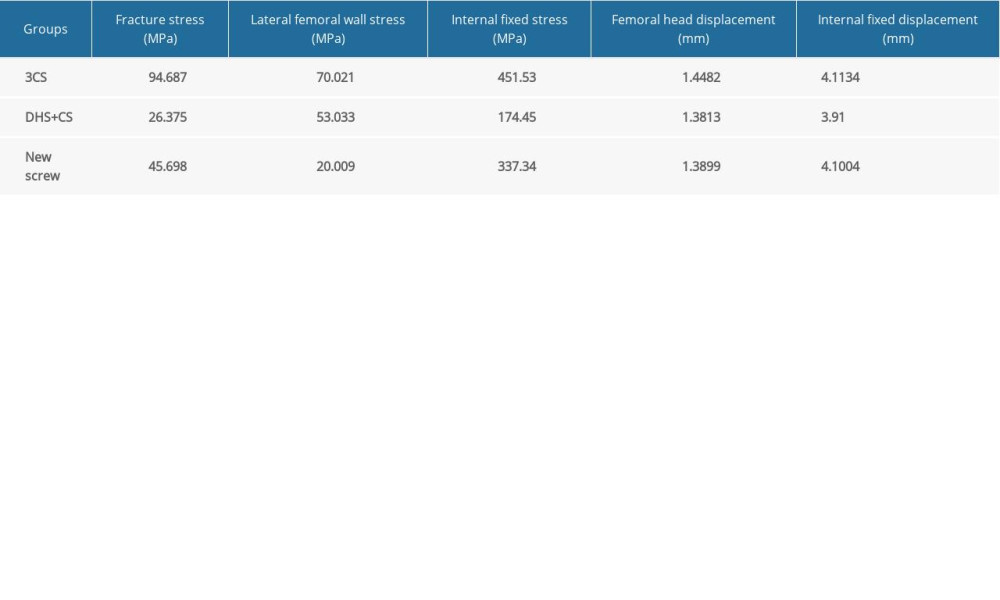 Table 2. Results of maximum stress and displacement of the finite element model of the different groups.
Table 2. Results of maximum stress and displacement of the finite element model of the different groups.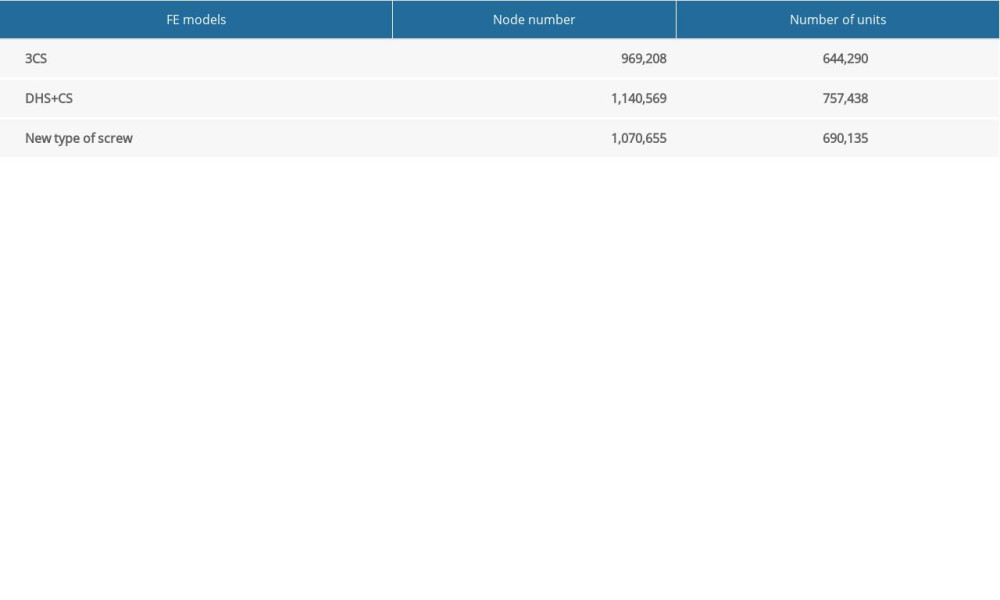 Table 1. Number of nodes and elements of the finite element model.
Table 1. Number of nodes and elements of the finite element model.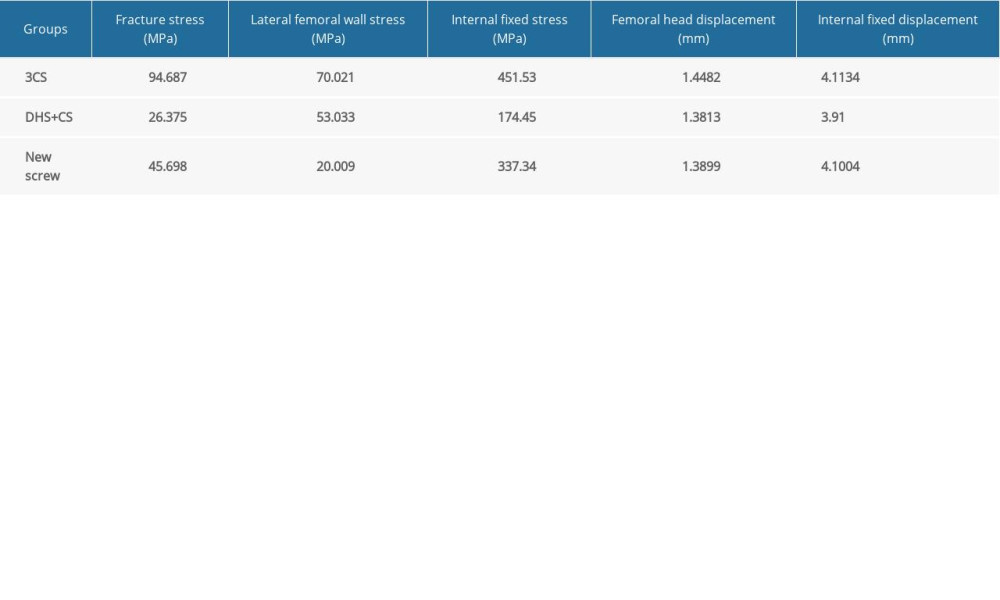 Table 2. Results of maximum stress and displacement of the finite element model of the different groups.
Table 2. Results of maximum stress and displacement of the finite element model of the different groups. In Press
21 Mar 2024 : Meta-Analysis
Economic Evaluation of COVID-19 Screening Tests and Surveillance Strategies in Low-Income, Middle-Income, a...Med Sci Monit In Press; DOI: 10.12659/MSM.943863
10 Apr 2024 : Clinical Research
Predicting Acute Cardiovascular Complications in COVID-19: Insights from a Specialized Cardiac Referral Dep...Med Sci Monit In Press; DOI: 10.12659/MSM.942612
06 Mar 2024 : Clinical Research
Enhanced Surgical Outcomes of Popliteal Cyst Excision: A Retrospective Study Comparing Arthroscopic Debride...Med Sci Monit In Press; DOI: 10.12659/MSM.941102
06 Mar 2024 : Clinical Research
Prevalence and Variation of Medical Comorbidities in Oral Surgery Patients: A Retrospective Study at Jazan ...Med Sci Monit In Press; DOI: 10.12659/MSM.943884
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








