09 November 2020: Clinical Research
Weight Gain Before the Third Trimester and Risk of Hypertensive Disorders of Pregnancy: A Prospective Cohort Study
Xiaoyi Zou12ABCDEF, Ning Yang3ACDG, Wei Cai4B, Xiulong Niu5B, Maoti Wei6CD, Xin Zhang4B, Xuejing Hou7CD, Fang Kang8B, Yuming Li9AG*DOI: 10.12659/MSM.927409
Med Sci Monit 2020; 26:e927409
Abstract
BACKGROUND: The association between excessive gestational weight gain (GWG) and the risk of hypertensive disorders of pregnancy (HDP) remains uncertain in women with increased water retention in late gestation associated with the pathophysiology of HDP. This study aimed to investigate the association between GWG before the third trimester and the risk of HDP.
MATERIAL AND METHODS: This was a prospective cohort study in singleton-pregnant women in Tianjin, China, from 2016. Generalized linear models were used to analyze the relationship between weight gain and the risk of HDP.
RESULTS: A total of 5295 singleton-pregnant women were included. Even after adjusting for relevant confounders, weight gain at approximately 28 weeks remained an independent risk factor for HDP in the normal-weight group. Compared to the reference of low weight gain (<–1 SD), weight gain >+1 SD was associated with an approximately 2.0 times greater likelihood of HDP (RR: 2.08, 95% CI: 1.06–4.08). Moreover, there was a positive relationship between weight gain in the short interval of early pregnancy and risk of HDP in overweight women.
CONCLUSIONS: Excessive weight gain before the third trimester was associated with a greater risk of developing HDP among women with early-pregnancy normal weight, which may provide a chance to identify subsequent hypertensive disorders. Additional research is needed to determine whether early-pregnancy weight gain is associated with HDP risk.
Keywords: Body Mass Index, Hypertension, Pregnancy-Induced, Obesity, Pre-Eclampsia, Weight Gain, Pregnancy, Pregnancy Trimester, Third, Prospective Studies, Risk Factors
Background
Hypertensive disorders of pregnancy (HDP), including gestational hypertension, preeclampsia, and eclampsia, are high-risk factors for future cardiovascular events in women [1,2]. Studies have shown that women with HDP and their offspring have significantly higher risks of cardiovascular events in the future [3–5]; therefore, early diagnosis and prevention of HDP may improve their long-term health. Obesity has been reported to be a modifiable risk factor for HDP in several studies [6–8], but the association between excessive gestational weight gain and the risk of HDP remains uncertain or insufficient [9–11]; greater weight gain is related to a longer pregnancy duration and edema during pregnancy, mainly in the third trimester. Considering HDP as a disorder typically identified by new-onset hypertension in the second half of pregnancy, mainly in the third trimester, the relationship between weight gain before the third trimester and the incidence of HDP are uncertain, and there have been few studies on this topic in the Chinese population.
Conventional measures of gestational weight gain (GWG) can introduce bias into epidemiologic studies of GWG and adverse perinatal outcomes, such as premature birth, neonatal death, stillbirth, and preeclampsia, because both are correlated with gestational duration [10,12,13]. The gestational age-specific z-score of weight gain is a new measure to evaluate weight gain, which is independent of gestational duration. Compared with GWG, it correlates better with preterm birth [12]. Whether the gestational age-specific z-score of weight gain is suitable to assess the risk of HDP remains undetermined.
The main aim of the present study was to assess weight gain in 4 gestational periods 16 weeks (14+0, 17+6), 20 weeks (18+0, 21+6), 24 weeks (22+0, 25+6), and 28 weeks (26+0, 29+6) – and the risk of HDP in 4 early-pregnancy BMI categories – underweight (<18.5 kg/m2), normal-weight (18.5~23.9 kg/m2), overweight (24.0~27.9 kg/m2), and obesity (≥28.0 kg/m2)]. We also aimed to assess these relationships using the gestational age-specific z-score for weight gain.
Material and Methods
STUDY DESIGN:
This was a prospective cohort study of singleton-pregnant women in Tianjin, China, from 2016. This study was approved by the Medical Ethics and Human Clinical Trial Committee of the local hospital, and all participants agreed to participate in the study and signed a written informed consent form. Participants were recruited from 19 community hospitals if they met the following criteria:
Inclusion criteria: (I) Singleton pregnancy; (II) Gestational age at enrolment <13 completed weeks; and (III) No presence of chronic hypertension. Exclusion criteria: (I) Incomplete or abnormal enrolment information or follow-up information; (II) Pregnancy termination for various reasons before 24 weeks of pregnancy; and (III) Systolic blood pressure ≥140 mmHg (1 mmHg=0.133 kPa) and/or diastolic blood pressure ≥90 mmHg before 20 weeks of pregnancy.
The participants completed a pre-designed questionnaire to collect baseline characteristics, including age, ethnicity, education level, family history, pregnancy, and delivery times. Height and weight at enrolment were simultaneously recorded. Gestational age was calculated according to the last menstrual period and checked by B-ultrasonic examination in early pregnancy. Pregnant women were followed up once every 4 weeks up to 28~30 weeks of gestation, and the diagnoses were recorded by the medical record system of the hospitals for delivery.
OBSERVATION OUTCOMES:
The early pregnancy BMI was calculated based on maternal height and weight recorded at the first prenatal visit. Gestational weight gain was defined as the difference between the weight at the corresponding gestational age and the weight at the first prenatal visit. Patients with weight gain above or below 4 SD of each group at each gestational age were flagged and excluded according to their weight trajectory and clinical plausibility. If there were multiple weight measurements during some periods, the last one was analysed. The weight gain z-score was calculated using BMI-specific z-score charts for Chinese women [14]. The z-scores were analysed as continuous variables and categorical variables, referring to the method used by Bodnar et al. [11]; the weight gain z-score was modelled as a 3-level categorical variable (<−1 SD, −1 to +1 SD, >+1 SD), where <−1 SD was the reference category, which was assumed to indicate low HDP risk.
The diagnostic criteria for HDP were based on the Guidelines for the Diagnosis and Treatment of Hypertensive Disorders in Pregnancy (2015) [15]. Gestational hypertension was defined as a systolic blood pressure ≥140 mmHg and/or diastolic blood pressure ≥90 mmHg after 20 weeks of pregnancy, which returned to normal within 12 weeks after delivery, and a negative urine protein test. Preeclampsia was defined as a systolic blood pressure ≥140 mmHg and/or diastolic blood pressure ≥90 mmHg after 20 weeks of pregnancy accompanied by any of the following: urine protein ≥0.3 g/24 h, urine protein/creatinine ratio ≥0.3, random urine protein ≥(+) (examination method when urinary protein quantification could not be performed), or no proteinuria but heart, lung, liver, kidney or other important organ involvement or abnormal changes in the blood system, digestive system, nervous system, or the fetus. Eclampsia was defined as seizures that occurred during preeclampsia that could not be explained by other causes.
STATISTICAL ANALYSES:
Quartiles and percentage counts were used to describe the baseline characteristics of pregnant women. Non-parametric tests and chi-square tests were used to analyze the differences between groups. Relative risks (RRs) with 95% confidence intervals (CIs) were obtained using general linear models to analyse the relationship between weight gain or weight gain z-scores at the corresponding gestational week and the risk of HDP. Moreover, analyses were adjusted for the age at enrolment, early-pregnancy BMI, primipara, and family history of hypertension. Statistical analyses were performed using SPSS version 23.0 (IBM Corp, Armonk, NY, USA) and STATA version 14.0 (Stata Corp, College Station, TX, USA).
Results
A total of 6081 non-hypertensive singleton-pregnant women with a gestational age at enrolment of <13 completed weeks were enrolled. Among these women, 28 were eventually diagnosed with chronic hypertension or chronic hypertension complicated with preeclampsia; 166 women had terminated pregnancies for various reasons before 24 weeks; 355 women withdrew from follow-up or were lost to follow-up; 109 participants had incomplete enrolment or delivery information or illogical weight records; and 128 participants had ≤2 weight measurements in the 4 periods. Finally, 5295 pregnant women were included. The study flowchart is outlined in Figure 1.
The characteristics of the 5295 women who participated in the study are presented in Table 1. Among them, 512 (9.7%), 3231 (61.0%), 1156 (21.8%), and 396 (7.5%) women were underweight, normal-weight, overweight, and obese, respectively. There were 177 cases of preeclampsia, 3 cases of eclampsia, and 105 cases of gestational hypertension. The total incidence of HDP was 5.4%. The corresponding incidence rates of HDP in the underweight, normal-weight, overweight, and obese groups were 2.3%, 3.5%, 9.3%, and 13.1%, respectively. In this Chinese cohort, 96% were of Han ethnicity, which is the ethnic majority in China, and 69% were nulliparous. The mean maternal age at enrolment was 30 years. With the increase in early-pregnancy BMI, the chance of developing HDP gradually increased, and the mean weight gain during each gestational period gradually decreased. However, there was no significant difference in weight gain z-scores between the 4 BMI groups.
Tables 2 and 3 compare the characteristics of women with or without HDP overall and in each BMI group. Overall, compared to women who did not progress to HDP, women who eventually progressed to HDP had higher early-pregnancy BMIs, were more likely to be primipara, and had family histories of hypertension and caesarean section, but they had a lower gestational age at delivery and lower neonatal weight. There were no statistically significant differences in education level, gestational age at enrolment, or neonatal sex. In the underweight group, only weight gain and weight gain z-scores of women with HDP at approximately 28 weeks were higher than those of the control group, and there were no significant differences in the other parameters. In the normal-weight group, which accounted for 61% of the entire cohort, weight gain in women with HDP at approximately 24–28 weeks and weight gain z-scores at approximately 28 weeks were higher than those of the control group. In the overweight and obese groups, weight gain and weight gain z-scores of women with HDP at approximately 16 weeks were higher than those of normotensive women in the overweight group, while the opposite result was obtained in the obese group. There were no significant differences in weight gain and the weight gain z-scores in the other periods.
Crude and adjusted RRs for weight gain or weight gain z-scores before the third trimester and the risk of HDP according to early-pregnancy BMI category are shown in Table 4. In underweight women, weight gain at approximately 28 weeks was positively correlated with the risk of HDP (crude RR: 1.23, 95% CI: 1.02–1.47). After adjusting for confounding factors, such as age, early pregnancy BMI, primipara, and family history of hypertension, the adjusted RR was 1.21 (95% CI: 1.01–1.45). The association of the weight gain z-score at approximately 28 weeks with the risk of HDP was null. Considering the small sample and the low incidence of HDP in the underweight group, the test efficiency may have been insufficient. Weight gain and weight gain z-scores at approximately 28 weeks in the normal-weight group were associated with the risk of HDP (weight gain RR: 1.08, 95% CI: 1.02–1.15; weight gain z-score RR: 1.29, 95% CI: 1.05–1.58). Compared to the reference of low weight gain (<−1 SD), weight gain >+1 SD was associated with an approximately 2.0 times greater likelihood of HDP (RR: 2.08, 95% CI: 1.06–4.08). Weight gain and weight gain z-scores at the remaining time points were not related to the risk of HDP, and the relationships among the other periods were not significant. Among the overweight women, weight gain and weight gain z-scores at approximately 16 weeks were associated with an increased risk of HDP (weight gain RR: 1.12, 95% CI: 1.01–1.25; weight gain z-score RR: 1.32, 95% CI: 1.09–1.57). Compared to the reference of low weight gain (<−1 SD), weight gain >+1 SD at approximately 16 weeks significantly increased the risk of developing HDP (RR: 4.21, 95% CI: 1.36–13.01), while in obese women, there was a negative relationship between weight gain at approximately 16 weeks and the risk of HDP. Associations were null for the other periods.
Discussion
RESEARCH LIMITATIONS:
First, our study population was located in 19 communities in Tianjin, and the resident population is mostly of Han ethnicity. Therefore, this study can only represent the characteristics of the Han population in northern China. Second, considering the low incidence of HDP, the overall population of the study was not large, especially for the underweight and obese women, so the research data in these 2 groups were not sufficiently accurate. Third, some studies have shown that the relationship between weight gain and the risk of HDP subtypes was not the same. The present study did not analyze this relationship because of the number of people enrolled. Results are still being collated, and future large-sample cohort studies may provide a sufficient number of cases for analysis. Finally, using early-pregnancy BMI as the basis for grouping may have caused bias in enrolment. However, the pre-pregnancy weight mainly depended on the memory of the pregnant woman, and there may be recall errors. The grouping basis of the z-score chart in the Chinese population that our study represented is the early-pregnancy BMI, and the sensitivity analyses in the study indicated that the possibility of misclassification was small and acceptable [14].
Conclusions
Excessive weight gain before the third trimester, independent of age, early pregnancy BMI, primipara, and family history of hypertension, was associated with a greater risk of developing HDP among women with early-pregnancy normal weight, which may provide a chance to identify subsequent hypertensive disorders. The relationship between weight gain in early pregnancy and the risk of HDP remains unclear. Additional large-sample research with serial antenatal weight measure (including pre-pregnancy weight) are need to determine whether early-pregnancy weight gain is associated with HDP risk.
Figures
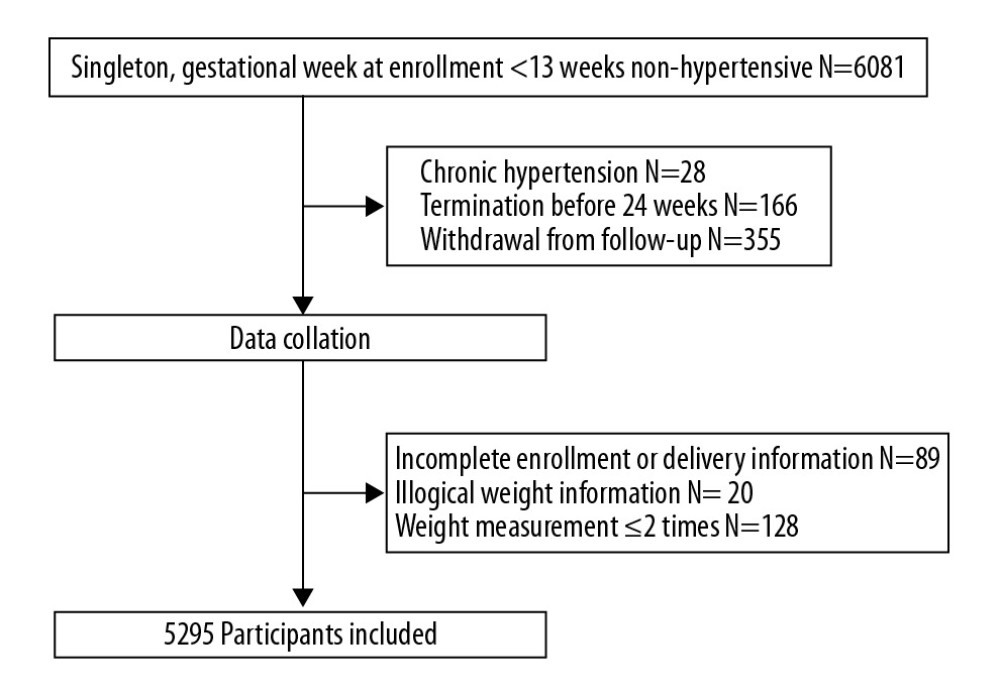 Figure 1. Study flowchart.
Figure 1. Study flowchart. Tables
Table 1. Baseline characteristics of pregnancies according to early-pregnancy BMI category.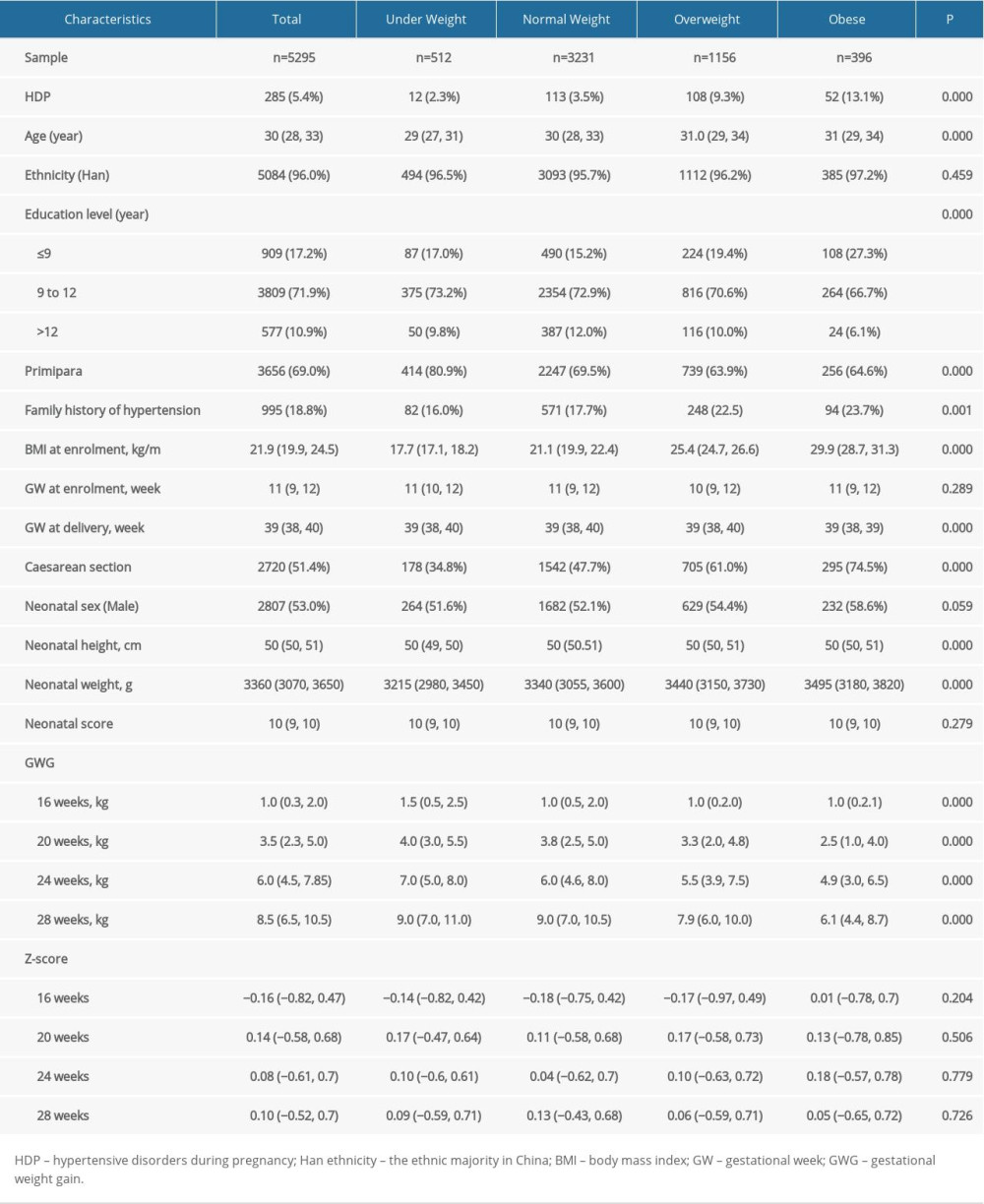 Table 2. Descriptive characteristics of pregnancies with and without HDP in different early-pregnancy BMI categories.
Table 2. Descriptive characteristics of pregnancies with and without HDP in different early-pregnancy BMI categories.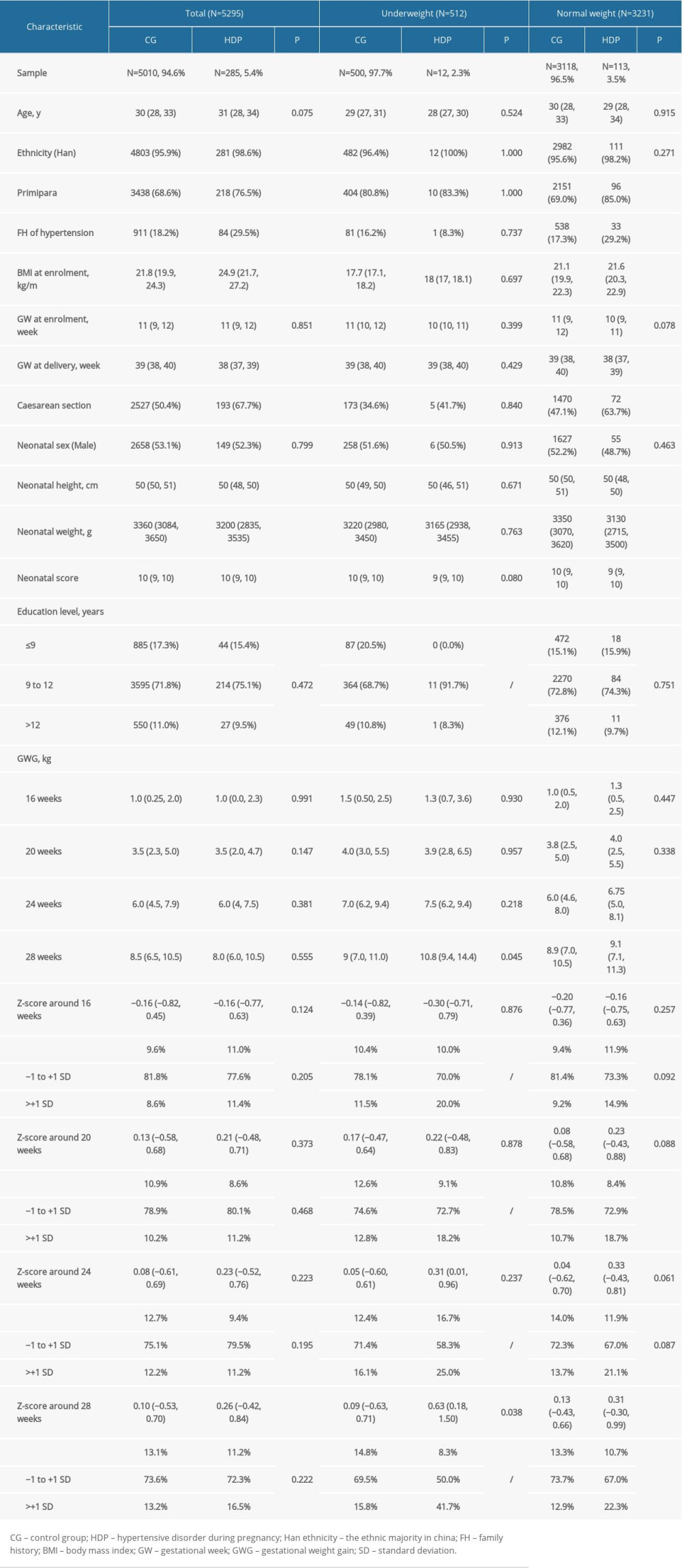 Table 3. Descriptive characteristics of pregnancies with and without HDP in different early-pregnancy BMI categories.
Table 3. Descriptive characteristics of pregnancies with and without HDP in different early-pregnancy BMI categories.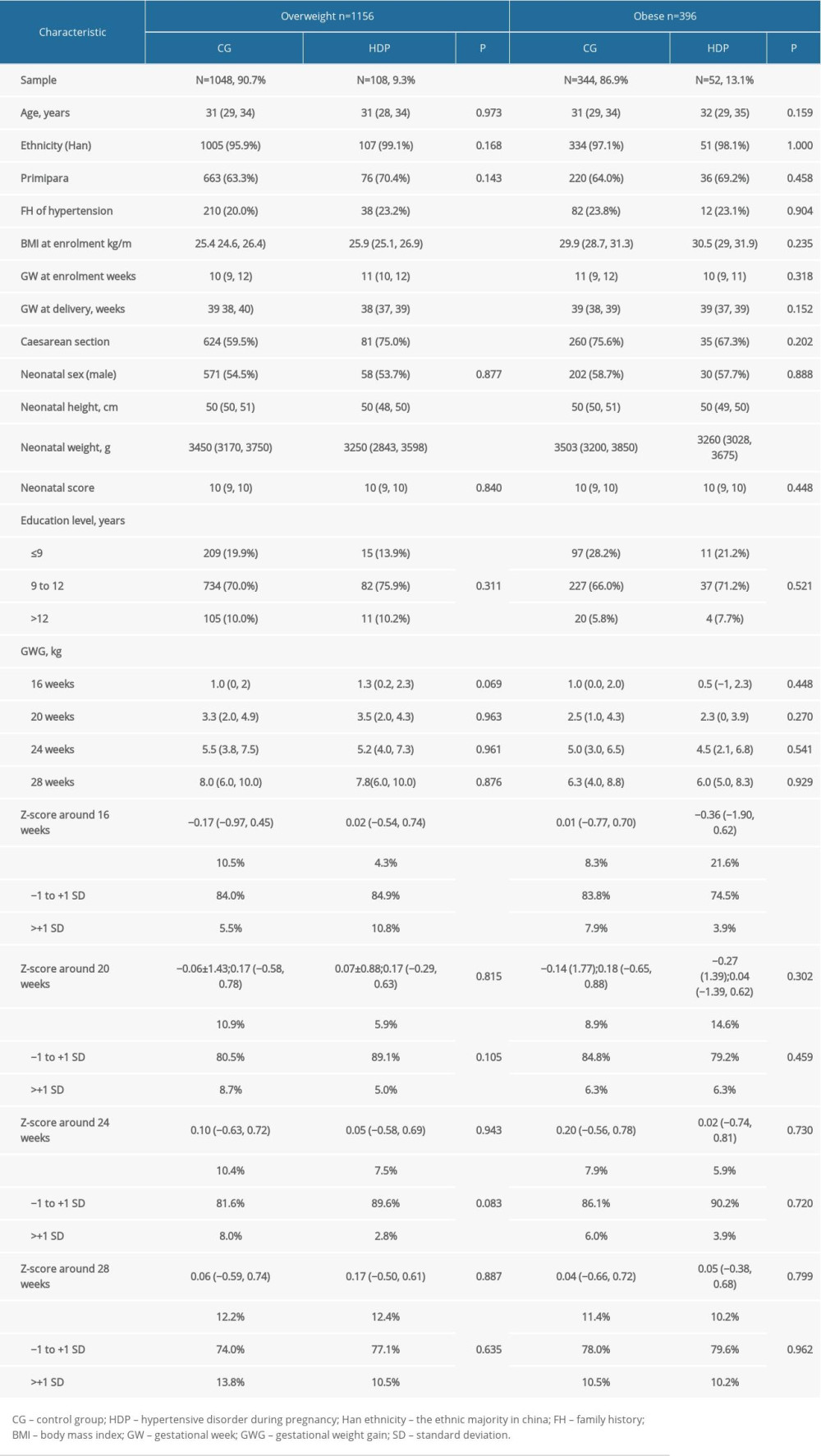 Table 4. Relationship between weight gain, weight gain z-scores before the third trimester, and the risk of HDP.
Table 4. Relationship between weight gain, weight gain z-scores before the third trimester, and the risk of HDP.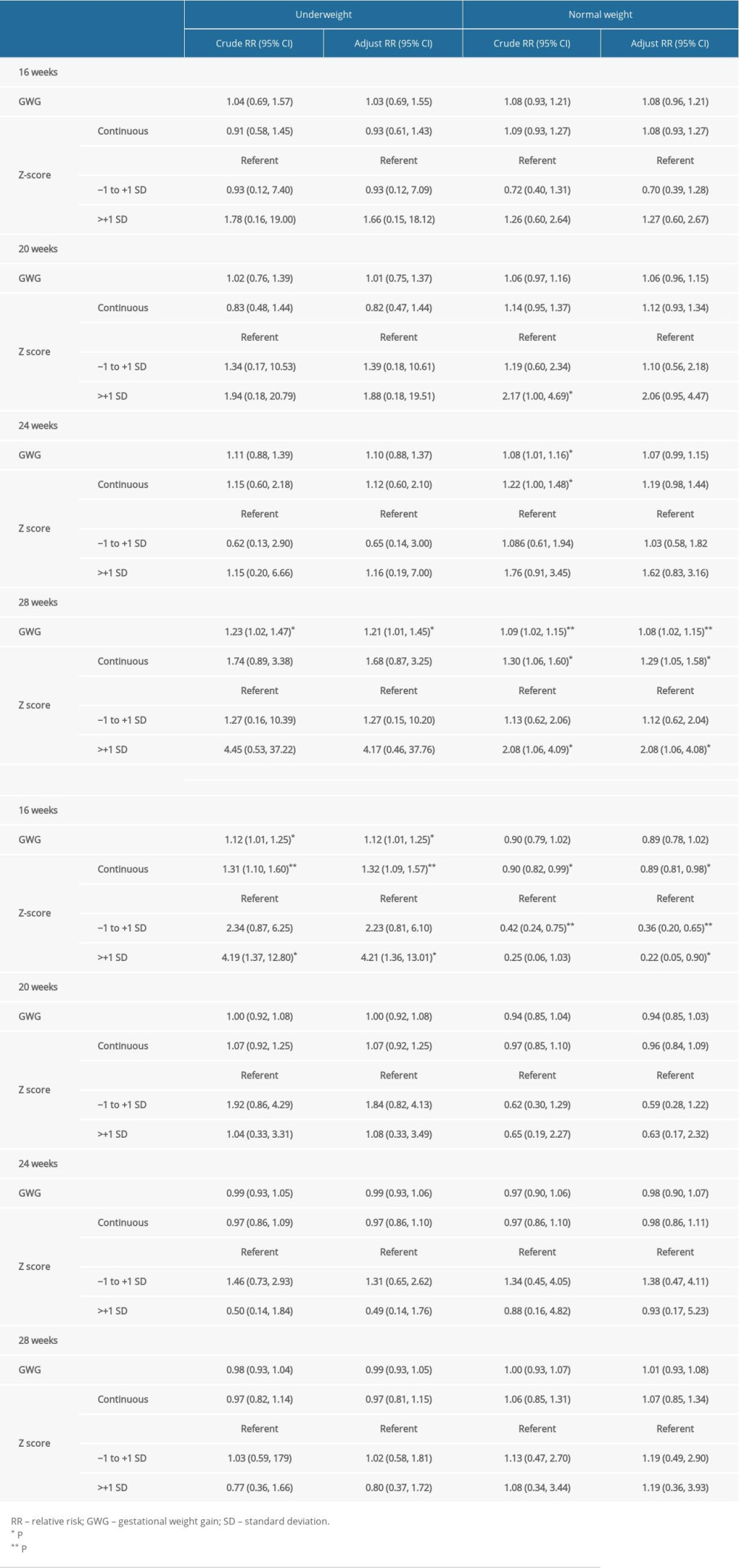
References
1. Garovic VD, Bailey KR, Boerwinkle E, Hypertension in pregnancy as a risk factor for cardiovascular disease later in life: J Hypertens, 2010; 28(4); 826-33
2. Bergen NE, Schalekamp-Timmermans S, Roos-Hesselink J, Hypertensive disorders of pregnancy and subsequent maternal cardiovascular health: Eur J Epidemiol, 2018; 33(8); 763-71
3. Leon LJ, McCarthy FP, Direk K, Preeclampsia and cardiovascular disease in a large UK pregnancy cohort of linked electronic health records: A caliber study: Circulation, 2019; 140(13); 1050-60
4. Herrera-Garcia G, Contag S, Maternal preeclampsia and risk for cardiovascular disease in offspring: Curr Hypertens Rep, 2014; 16(9); 475
5. Wang AM, Karumanchi SA, Offspring ardiovascular disease in preeclampsia: Nature versus nurture?: Hypertension (Dallas, TX: 1979), 2017; 69(4); 589-90
6. Cedergren M, Effects of gestational weight gain and body mass index on obstetric outcome in Sweden: Int J Gynaecol Obstet, 2006; 93(3); 269-74
7. Poston L, Harthoorn LF, Van Der Beek EM, Obesity in pregnancy: Implications for the mother and lifelong health of the child. A consensus statement: Pediatr Res, 2011; 69(2); 175-80
8. Spradley FT, Palei AC, Granger JP, Increased risk for the development of preeclampsia in obese pregnancies: Weighing in on the mechanisms: Am J Physiol Regul Integr Comp Physiol, 2015; 309(11); R1326-43
9. Rasmussen KM, Yaktine ALInstitute of Medicine (US), National Research Council (US) Committee to Reexamine IOM Pregnancy Weight Guidelines, The National Academies Collection: Reports funded by National Institutes of Health: Weight gain during pregnancy: Reexamining the guidelines, 2009, Washington (DC), National Academies Press (US). National Academy of Sciences
10. Hutcheon JA, Stephansson O, Cnattingius S, Pregnancy weight gain before diagnosis and risk of preeclampsia: A population-based cohort study in nulliparous women: Hypertension (Dallas, TX: 1979), 2018; 72(2); 433-41
11. Bodnar LM, Himes KP, Abrams B, Early-pregnancy weight gain and the risk of preeclampsia: A case-cohort study: Pregnancy Hypertens, 2018; 14; 205-12
12. Bodnar LM, Hutcheon JA, Parisi SM, Comparison of gestational weight gain z-scores and traditional weight gain measures in relation to perinatal outcomes: Paediatr Perinat Epidemiol, 2015; 29(1); 11-21
13. Hutcheon JA, Bodnar LM, Joseph KS, The bias in current measures of gestational weight gain: Paediatr Perinat Epidemiol, 2012; 26(2); 109-16
14. Huang A, Xiao Y, Hu H, Gestational weight gain charts by gestational age and body mass index for Chinese women: A population-based follow-up study: J Epidemiol, 2020; 30(8); 345-53
15. Diagnosis and treatment guideline of hypertensive disorders in pregnancy (2015): Zhonghua Fu Chan Ke Za Zhi, 2015; 50(10); 721-28
16. Bezerra PC, Leão MD, Queiroz JW, Family history of hypertension as an important risk factor for the development of severe preeclampsia: Acta Obstet Gynecol Scand, 2010; 89(5); 612-17
17. Bartsch E, Medcalf KE, Park AL, Ray JG, Clinical risk factors for pre-eclampsia determined in early pregnancy: Systematic review and meta-analysis of large cohort studies: BMJ, 2016; 353; i1753
18. Voerman E, Santos S, Inskip H, Association of gestational weight gain with adverse maternal and infant outcomes: JAMA, 2019; 321(17); 1702-15
19. Ruhstaller KE, Bastek JA, Thomas A, The effect of early excessive weight gain on the development of hypertension in pregnancy: Am J Perinatol, 2016; 33(12); 1205-10
20. Spradley FT, Metabolic abnormalities and obesity‘s impact on the risk for developing preeclampsia: Am J Physiol Regul Integr Comp Physiol, 2017; 312(1); R5-12
21. Zhou A, Xiong C, Hu R, Pre-pregnancy BMI, gestational weight gain, and the risk of hypertensive disorders of pregnancy: A cohort study in Wuhan, China: PLoS One, 2015; 10(8); e0136291
22. Ma RCW, Schmidt MI, Tam WH, Clinical management of pregnancy in the obese mother: Before conception, during pregnancy, and post partum: Lancet Diabetes Endocrinol, 2016; 4(12); 1037-49
Figures
Tables
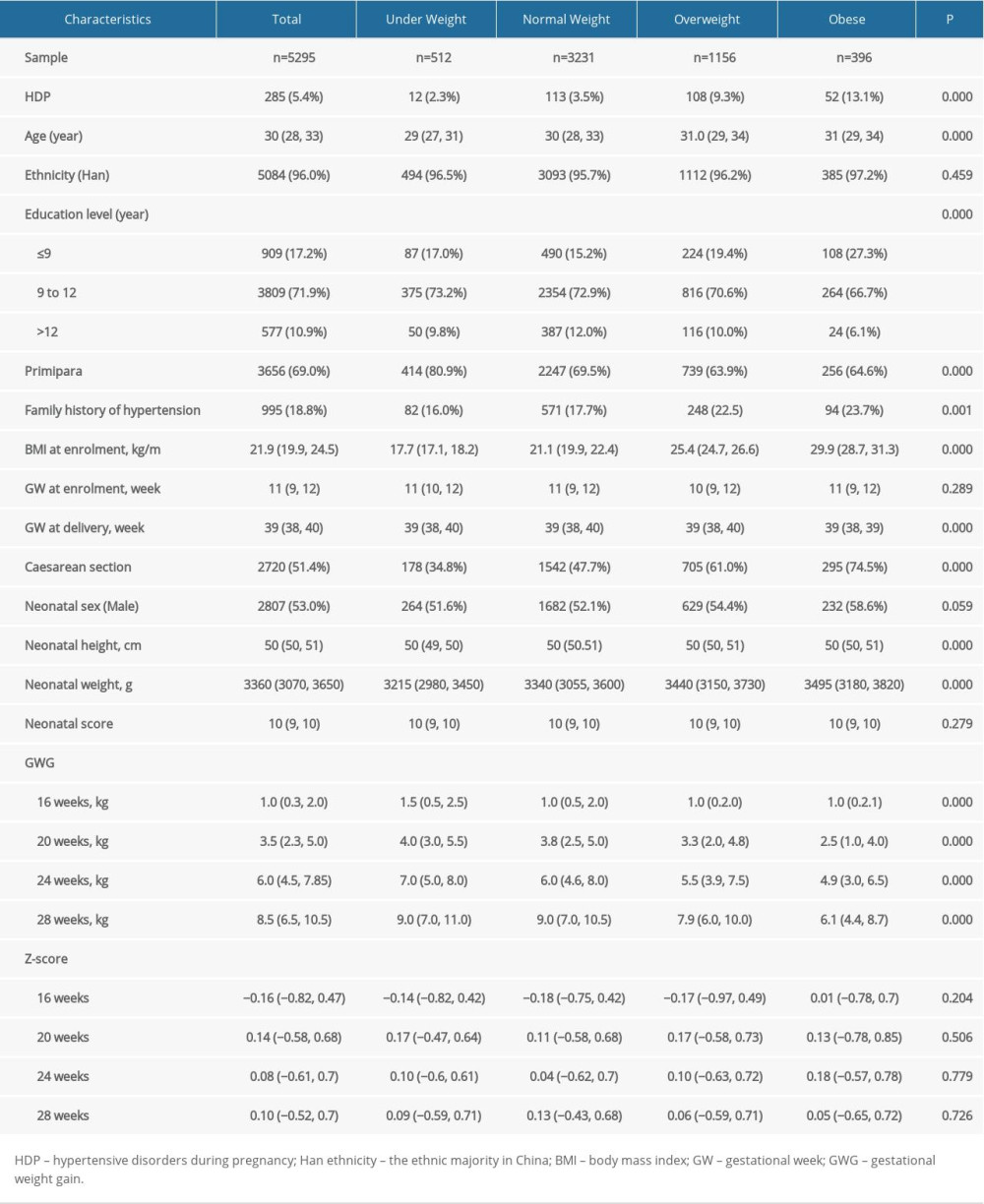 Table 1. Baseline characteristics of pregnancies according to early-pregnancy BMI category.
Table 1. Baseline characteristics of pregnancies according to early-pregnancy BMI category.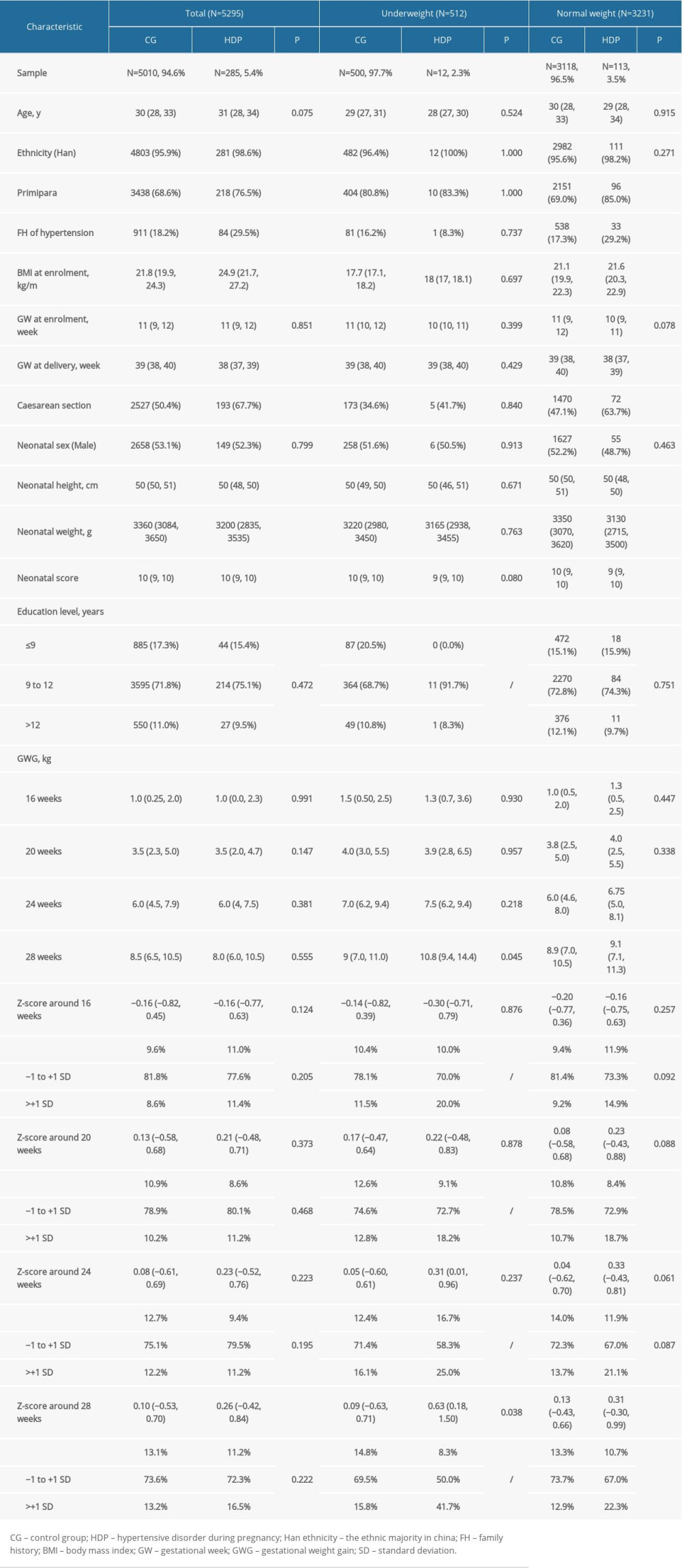 Table 2. Descriptive characteristics of pregnancies with and without HDP in different early-pregnancy BMI categories.
Table 2. Descriptive characteristics of pregnancies with and without HDP in different early-pregnancy BMI categories.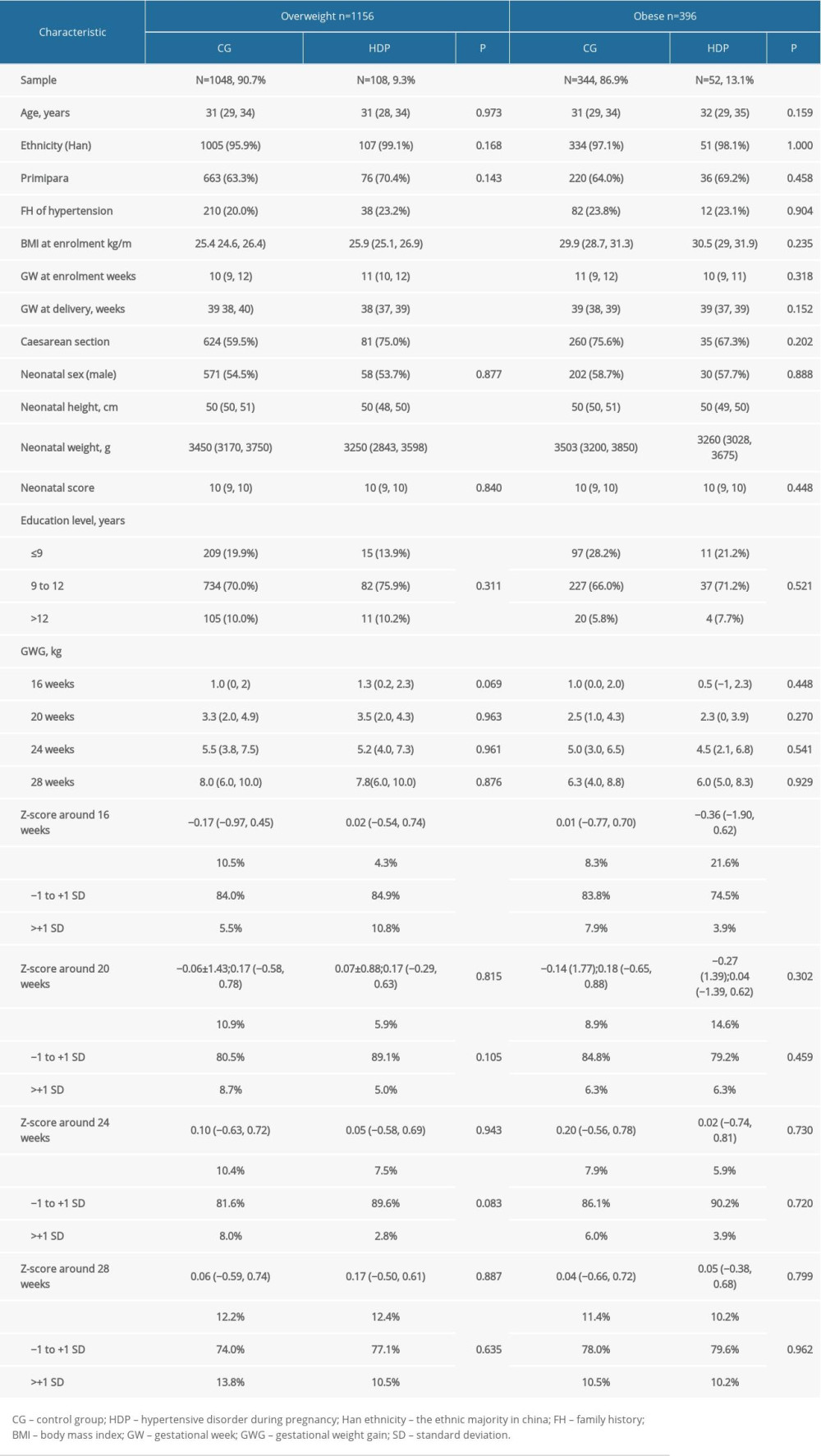 Table 3. Descriptive characteristics of pregnancies with and without HDP in different early-pregnancy BMI categories.
Table 3. Descriptive characteristics of pregnancies with and without HDP in different early-pregnancy BMI categories.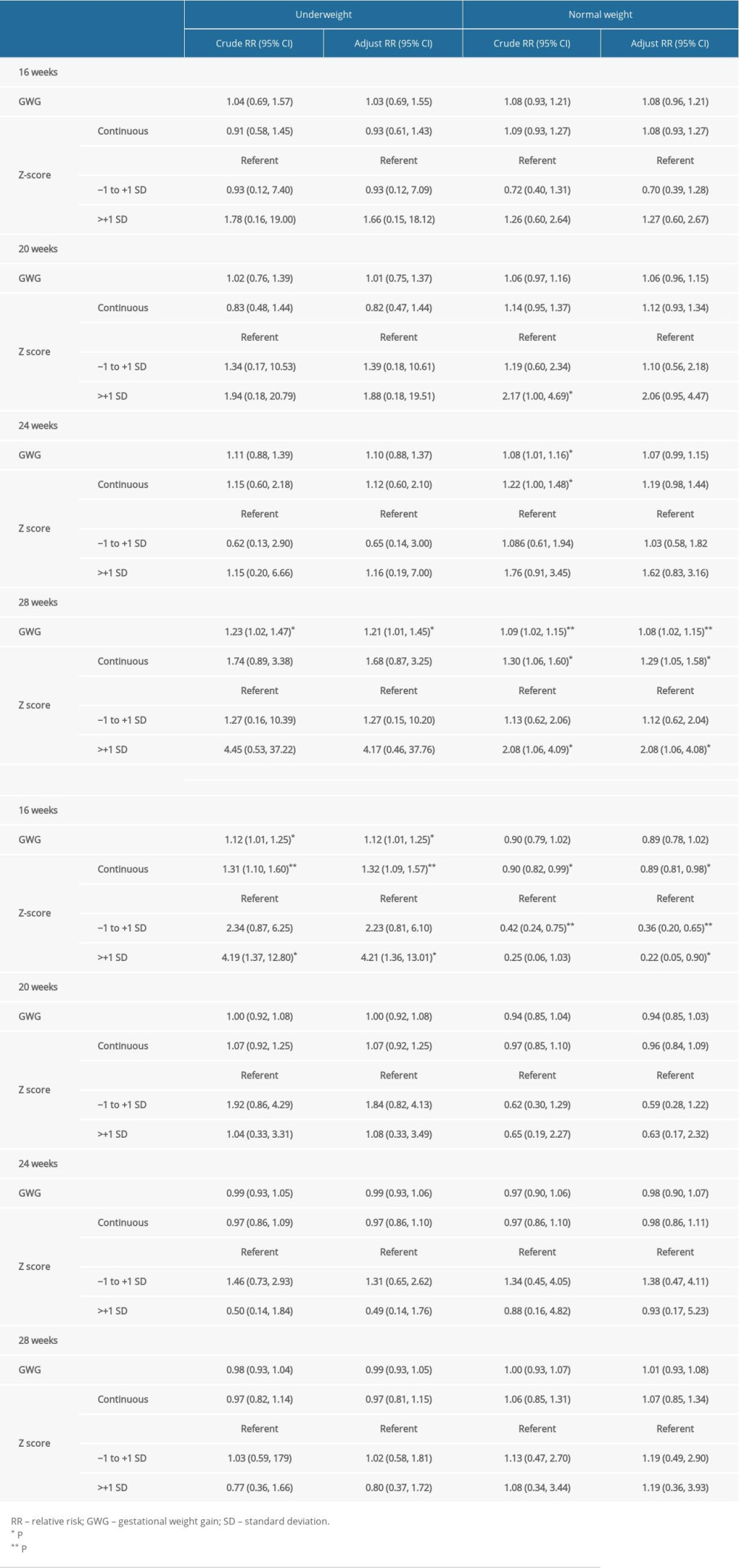 Table 4. Relationship between weight gain, weight gain z-scores before the third trimester, and the risk of HDP.
Table 4. Relationship between weight gain, weight gain z-scores before the third trimester, and the risk of HDP.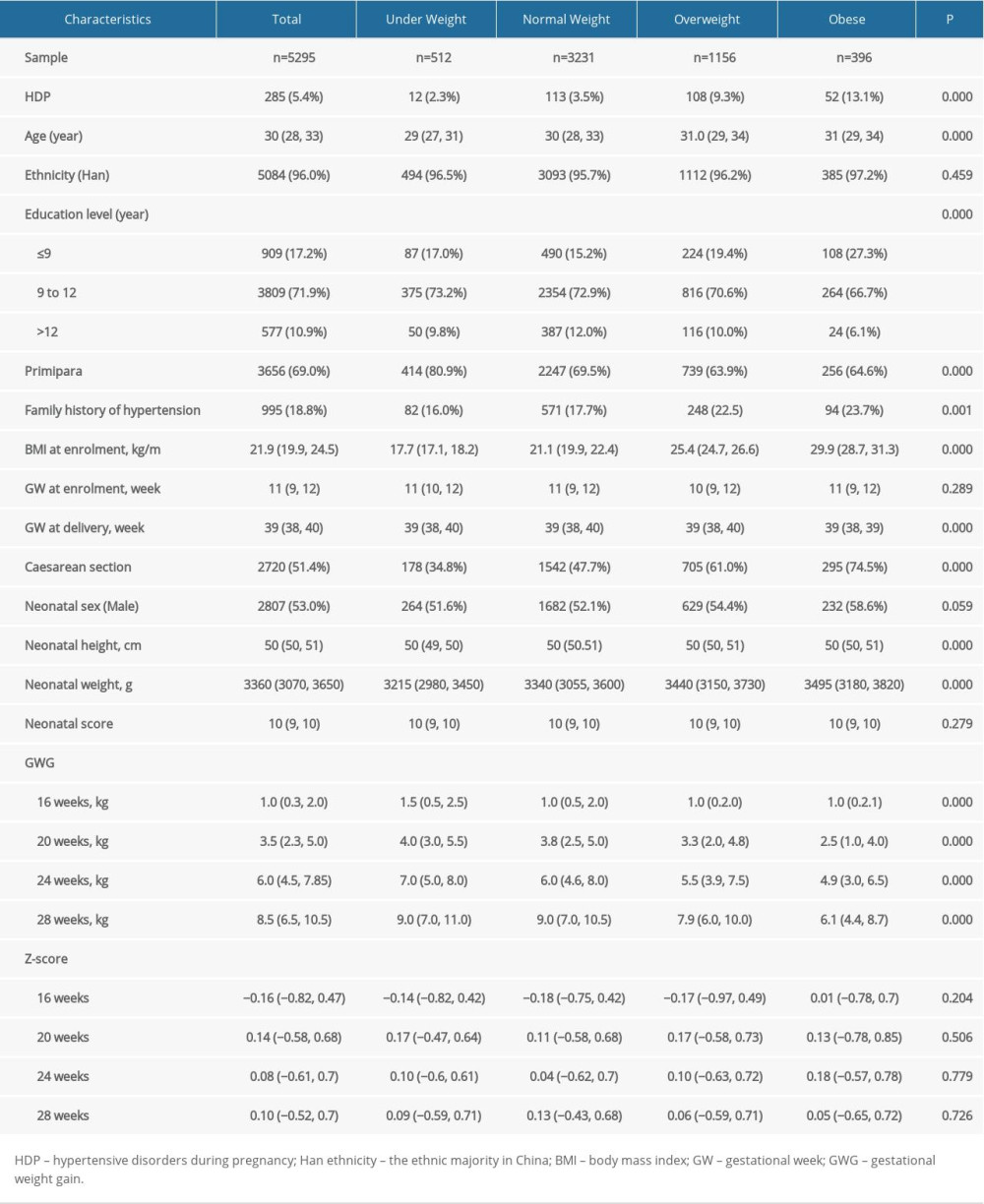 Table 1. Baseline characteristics of pregnancies according to early-pregnancy BMI category.
Table 1. Baseline characteristics of pregnancies according to early-pregnancy BMI category.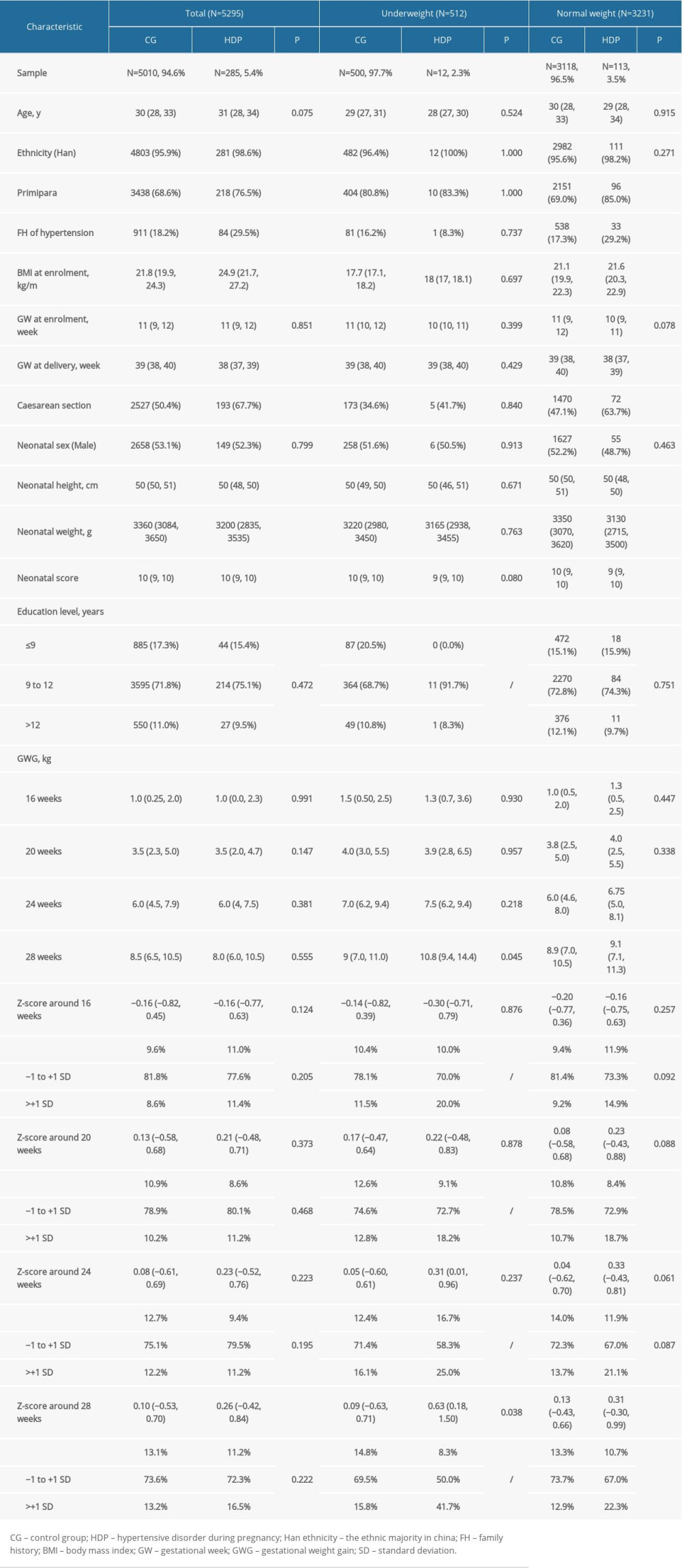 Table 2. Descriptive characteristics of pregnancies with and without HDP in different early-pregnancy BMI categories.
Table 2. Descriptive characteristics of pregnancies with and without HDP in different early-pregnancy BMI categories.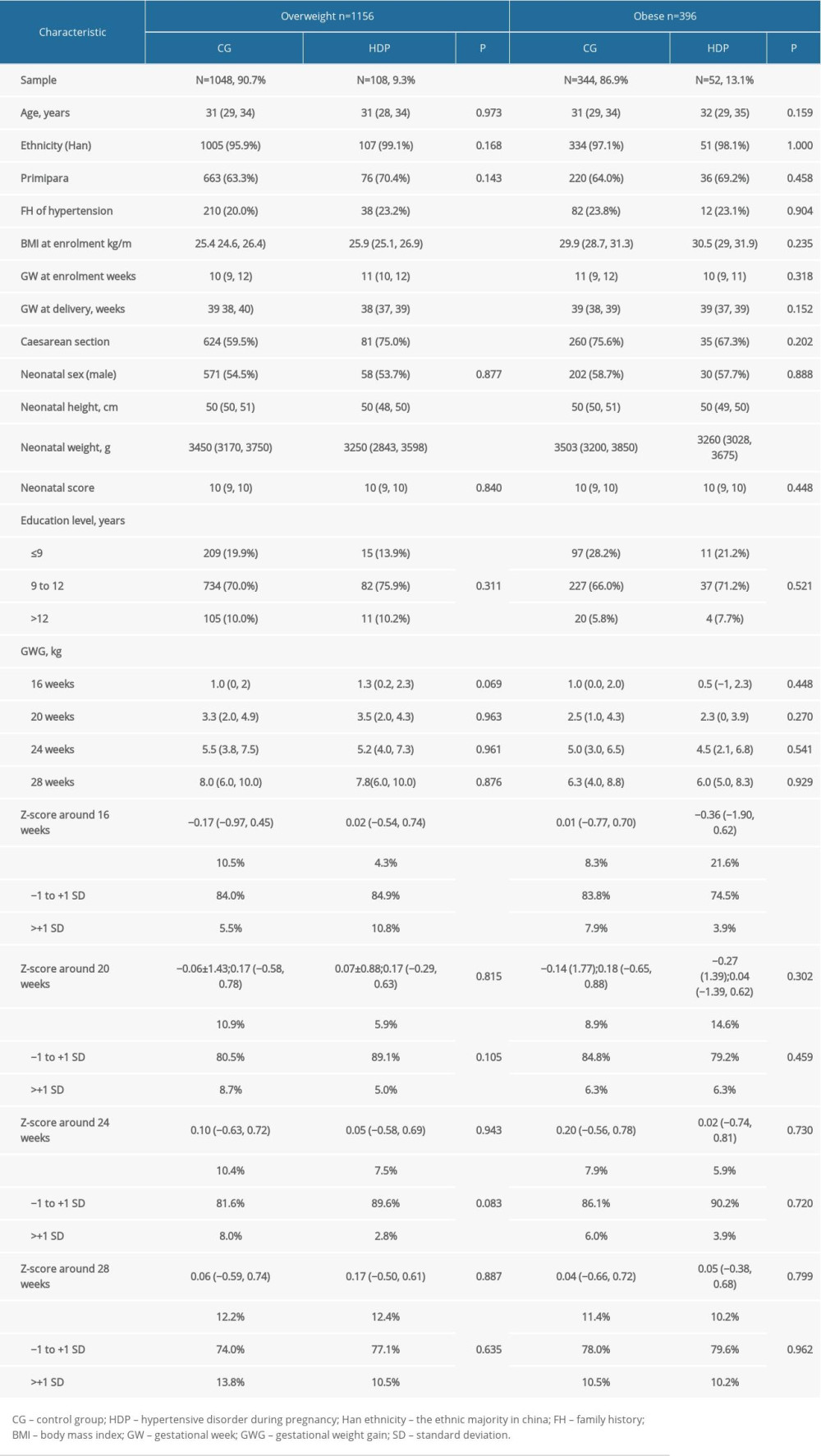 Table 3. Descriptive characteristics of pregnancies with and without HDP in different early-pregnancy BMI categories.
Table 3. Descriptive characteristics of pregnancies with and without HDP in different early-pregnancy BMI categories.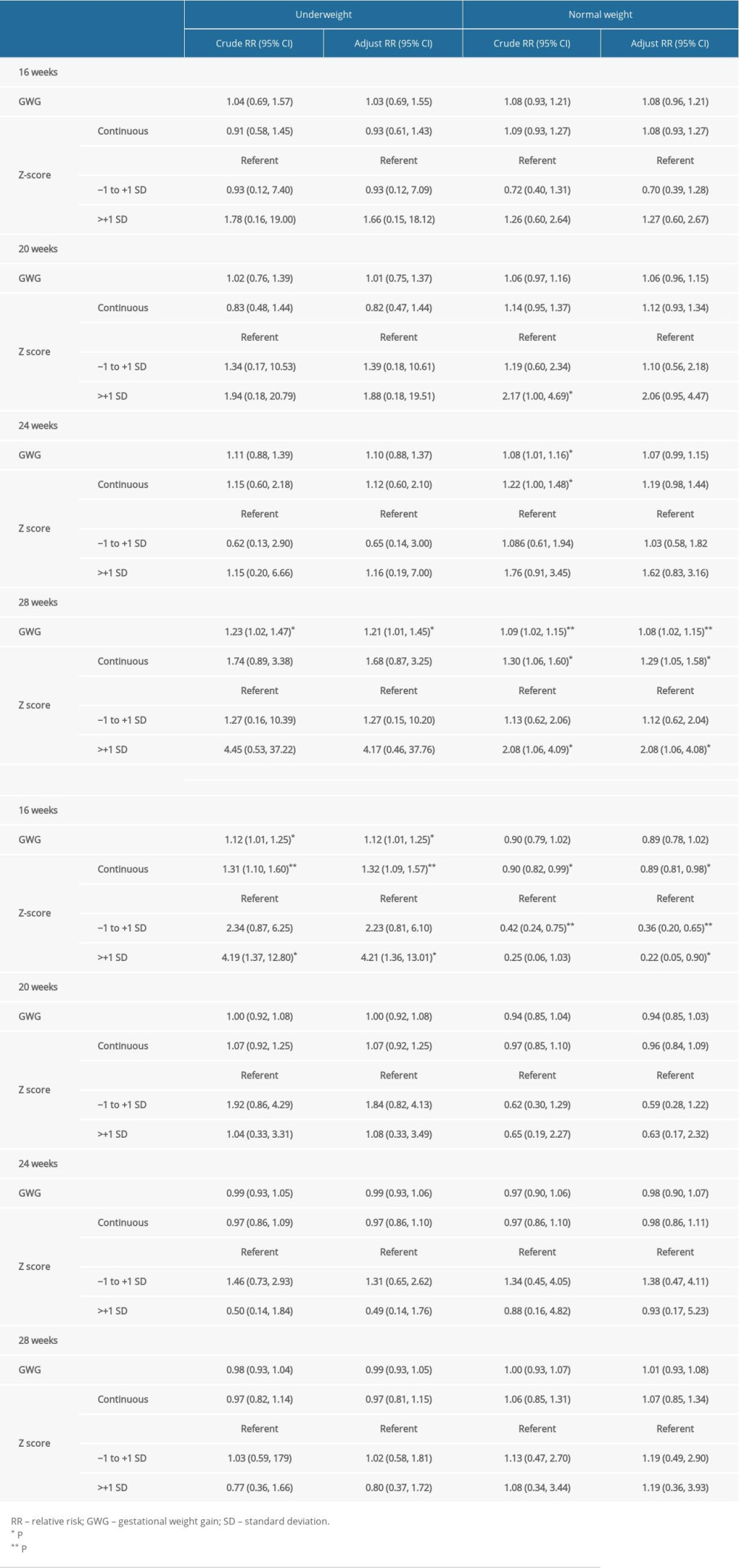 Table 4. Relationship between weight gain, weight gain z-scores before the third trimester, and the risk of HDP.
Table 4. Relationship between weight gain, weight gain z-scores before the third trimester, and the risk of HDP. In Press
08 Mar 2024 : Clinical Research
Evaluation of Foot Structure in Preschool Children Based on Body MassMed Sci Monit In Press; DOI: 10.12659/MSM.943765
15 Apr 2024 : Laboratory Research
The Role of Copper-Induced M2 Macrophage Polarization in Protecting Cartilage Matrix in OsteoarthritisMed Sci Monit In Press; DOI: 10.12659/MSM.943738
07 Mar 2024 : Clinical Research
Knowledge of and Attitudes Toward Clinical Trials: A Questionnaire-Based Study of 179 Male Third- and Fourt...Med Sci Monit In Press; DOI: 10.12659/MSM.943468
08 Mar 2024 : Animal Research
Modification of Experimental Model of Necrotizing Enterocolitis (NEC) in Rat Pups by Single Exposure to Hyp...Med Sci Monit In Press; DOI: 10.12659/MSM.943443
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








