18 July 2020: Clinical Research
Early Acute Kidney Injury Associated with Liver Transplantation: A Retrospective Case-Control Study
Mengzhuo Guo1BCDE, Yuanchao Gao1BCDE, Linlin Wang1BC, Haijing Zhang1BC, Xian Liu1BC, Huan Zhang2AEF*DOI: 10.12659/MSM.923864
Med Sci Monit 2020; 26:e923864
Abstract
BACKGROUND: A retrospective case-control study was carried out to assess the occurrence of acute kidney injury (AKI) in liver transplantation (LT) recipients and its related risk factors.
MATERIAL AND METHODS: The study enrolled 131 patients undergoing LT from December 2017 to June 2019 at Beijing Tsinghua Chang Gung Hospital, China. AKI and its classification were defined according to KDIGO guidelines. We collected patients’ demographic characteristics and perioperative parameters, and identified independent risk factors of AKI by multivariate logistic regression analysis.
RESULTS: We included 122 patients in analysis. AKI occurred in 52 (42.6%) patients (22.1% stage I, 8.2% stage II, and 12.3% stage III). AKI was notably associated with 12 factors: sex, body mass index (BMI), hepatic etiology, MELD score, ascites, prothrombin time (PT), international normalized ratio of prothrombin time (INR), preoperative total bilirubin (TBIL), operative time, total fluid intake, fresh frozen plasma (FFP), and estimated blood loss (EBL) (P<0.05). The factors independently associated with AKI were BMI (adjusted odds ratio: 0.605, 95% confidence interval: 0.425–0.859; P=0.005) and intraoperative FFP infusion (adjusted odds ratio: 0.998, 95% confidence interval: 0.995–1.000; P=0.047). Compared with the non-AKI group, the AKI group showed higher likelihood of renal replacement therapy (RRT), and longer ICU and hospital stays, higher in-hospital mortality, and higher hospitalization costs (P<0.05).
CONCLUSIONS: There is a high risk of AKI in patients undergoing LT. BMI and intraoperative FFP infusion are factors independently correlated with AKI. AKI can result in extended hospital stays and higher hospitalization expenses.
Keywords: Acute Kidney Injury, Incidence, Liver Transplantation, Risk Factors, Case-Control Studies, Hospital Mortality, Intensive Care Units, Length of Stay, Odds Ratio, Postoperative Complications, Time Factors
Background
Liver transplantation (LT) is a common method for treating end-stage liver disease. Acute kidney injury (AKI) has attracted much attention as a complication after LT, with an incidence ranging between 5% and 95% in different studies [1–3]. Several perioperative risk factors may be associated with AKI following LT, including advanced age, high body weight, prolonged operation duration, and high intraoperative blood loss [4,5]. AKI development in LT patients may lead to unfavorable outcomes, including prolonged hospital and intensive care unit (ICU) stay, as well as increased mortality [6,7].
In this study, we assessed the morbidity of AKI in LT patients and evaluated the associated risk factors, which may improve the early detection of patients with high risk and subsequent perioperative management to prevent or mitigate negative outcomes of AKI.
Material and Methods
DATA COLLECTION:
Data for the following variables were obtained from patients’ medical records: patient characteristics (age, sex, BMI, diabetes, hypertension, hepatic etiology, MELD score, and ascites); preoperative laboratory test results (serum creatinine, prothrombin activity, PT, INR, TBIL, albumin); operative variables (operation duration, total fluid intake, crystal liquid, HES, 5% albumin, RBC, FFP, EBL, urine output, and anhepatic phase); and postoperative course (postoperative RRT, ICU and hospital stay duration, in-hospital mortality, and hospitalization expense).
STATISTICAL ANALYSIS:
All data were analyzed using SPSS 22.0. Normally distributed measurement data are presented as mean and SD (x±SD) and were analyzed using the
Results
PARTICIPANTS:
A total of 131 adult recipients underwent LT during our enrollment period (Figure 1). Nine patients were excluded (1 due to age <18 years, 3 due to lack of clinical data, 2 due to receiving RRT before LT, 2 due to undergoing repeat surgery, and 1 due to death within first 24 h after transplantation). Finally, 122 patients were included in the study, and their biochemical data were analyzed.
INCIDENCE OF EARLY AKI FOLLOWING LT:
Of the 122 patients included in the study, AKI occurred in 52 (42.6%) patients according to the KDIGO criteria (stage I, 22.1%; stage II, 8.2%; and stage III, 12.3%). Most early AKI cases after LT were stage I.
RISK FACTORS FOR EARLY AKI FOLLOWING LT:
Patient characteristic data of the 122 eligible patients are presented in Table 1. The factors affecting postoperative AKI in univariate analysis were as follows: sex, BMI, hepatic etiology, MELD score, and ascites. Results of univariate analysis of pre- and intraoperative data are shown in Tables 2–4. The following factors were correlated with AKI: preoperative prothrombin time (PT), international normalized ratio of prothrombin time (INR), preoperative total bilirubin (TBIL), operative time, total fluid intake, fresh frozen plasma (FFP) requirement, and estimated blood loss (EBL) (P<0.05).
EFFECT OF EARLY AKI ON PATIENT OUTCOMES:
Compared with the non-AKI group, the AKI group patients were significantly more likely to have received RRT, had longer postoperative ICU and hospital stays, higher in-hospital mortality, and higher hospitalization costs (P<0.05) (Table 4).
Multivariate logistic regression analysis showed that BMI (adjusted odds ratio: 0.605, 95% confidence interval: 0.425–0.859; P=0.005) and FFP (adjusted odds ratio: 0.998, 95% confidence interval: 0.995–1.000; P=0.047) were independently correlated with AKI (Table 5).
Discussion
AKI is common in LT recipients, and its incidence varies in previous studies with different diagnostic criteria [11,12]. In the present study, we chose to use the traditional definition of kidney injury, evaluated using changes in serum creatinine. Serum creatinine is a more reliable and valid indicator to assess renal function, although, alone, it cannot fully reflect GFR [7].
In this study, a retrospective case-control study involving 122 LT recipients was carried out to determine the incidence of AKI and its relevant risk factors. The occurrence of early postoperative AKI was 42.6% based on the KDIGO guidelines, and most early AKI after LT was in AKI stage I/II (71.2%); these results are similar to previously reported trends. Therefore, it is necessary to increase efforts to prevent AKI after LT, especially in the early postoperative period. Patients who develop AKI following surgery should be actively treated to restore renal function to normal levels as soon as possible to avoid persistent AKI, further deterioration of renal function, and increased risk of other postoperative adverse events.
Our univariate analysis showed that 12 factors affect postoperative AKI, which is similar to previous studies [4,13–15]. Among these factors, MELD score and other components of MELD such as TBIL and INR are associated with AKI development, suggesting that the severity of preoperative liver disease, as reflected by MELD score, is associated with AKI following LT [16,17]. Surprisingly, no significant correlation between preoperative serum creatinine levels and AKI occurrence after LT was noted in our study, perhaps because patients with severe liver disease show reduced serum creatinine due to factors such as malnutrition and muscle atrophy. It is less reliable to estimate renal function using serum creatinine for patients with liver disease. In addition, prolonged PT and ascites are correlated with postoperative AKI, and these are also indicators of primary liver function before surgery [18–20]. Therefore, for patients with severe liver disease prior to surgery, the transplant itself may herald the increased risk of postoperative AKI. However, in this study, AKI incidence was lower in patients with hepatic echinococcosis. The kidney function of the patient may be impaired by the immune response caused by hepatic echinococcosis. However, the detection of serum creatinine does not reflect the slight kidney damage caused by hepatic echinococcosis due to the strong compensatory ability of the kidneys. It may require further research by accumulating additional cases to elucidate this finding. EBL appears to be another sign of surgical complications or intraoperative adverse events. In addition, hemodynamic instability or anemia caused by heavy bleeding may reduce oxygen delivery to the kidney, eventually leading to kidney damage.
BMI is a common indicator used to evaluate the body’s metabolism, which may play an important role in AKI. Patients with high BMI are at an increased potential risk of severe metabolic syndrome and associated comorbidities (e.g., hypertension and cardio- and cerebrovascular diseases), glomerular hypertrophy, mesangial hyperplasia, and postoperative infection [21]. These changes can affect kidney function, even though no apparent changes under normal conditions before LT are seen. In our study, patients with higher BMI were more likely to develop AKI after LT. However, the predictive value of BMI remains controversial [22,23] because weight and BMI of patients may be confounded by the ascites and fluid overload that can occur in patients preparing for LT [24,25]. The predictive effects of BMI on AKI following LT may simply reflect the severity of liver disease and/or renal function. The present study also investigated whether infusion of FFP is involved in the AKI. Kalisvaart et al. found that FFP requirement during LT was the best predictor of post-transplant AKI [26]. In this study, FFP requirement was independently associated with AKI, which is consistent with previous research. This may be because patients often experience significant blood loss during LT due to coagulopathy and portal hypertension. In addition, coagulopathy and fibrinolysis reflect severe hepatic ischemia/reperfusion injury and early impaired graft function [27,28].
AKI was remarkably associated with higher likelihood of receiving RRT, prolonged postoperative ICU and hospital stays, and increased hospitalization costs. As demonstrated in our study, AKI following LT was also associated with higher mortality. These results indicate the complexity of the postoperative course in patients undergoing LT, although this finding is merely an association and does not imply a causal relationship.
Our study has some limitations. First, this was a single-center, retrospective, observational study with a relatively small number of cases, which may reduce the generalizability of our results. Second, there were restrictions on access to data; for example, since preoperative urine output was not recorded in our database, the true renal function status of patients with severe liver disease could not be reported.
Conclusions
In conclusion, the incidence of early AKI following LT, specifically AKI stage I/II, is high in our hospital. BMI and intraoperative FFP infusion are independently associated with AKI development. AKI is significantly associated with prolonged hospitalization and increased hospitalization costs. In the future, prospective trial validation, preferably in a multicenter study with a large cohort, is required.
Figures
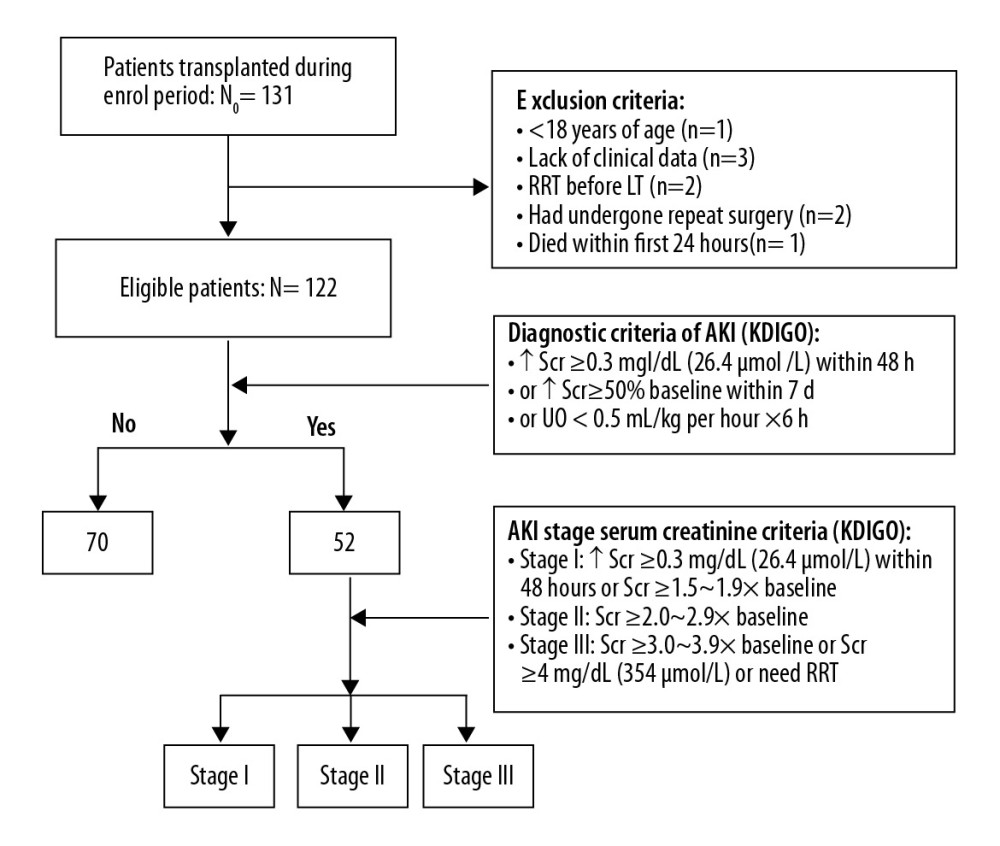 Figure 1. Study profile.
Figure 1. Study profile. References
1. McCauley J, Van Thiel DH, Starzl TE, Puschett JB, Acute and chronic renal failure in liver transplantation: Nephron, 1990; 55(2); 121-28
2. Lima EQ, Zanetta DM, Castro I, Risk factors for development of acute renal failure after liver transplantation: Ren Fail, 2003; 25(4); 553-60
3. Thongprayoon C, Kaewput W, Thamcharoen N, Incidence and impact of acute kidney injury after liver transplantation: A meta-analysis: J Clin Medm, 2019; 8(3); 372
4. Tinti F, Melandro F, Umbro I, Female gender and overestimation of glomerular filtration rate: Independent predictors of acute kidney injury after liver transplantation: Clin Nephrol, 2020; 93(2); 92-98
5. Yadav K, Serrano OK, Peterson KJ, The liver recipient with acute renal dysfunction: A single institution evaluation of the simultaneous liver-kidney transplant candidate: Clin Transplant, 2018; 32(1)
6. Rahman S, Davidson BR, Mallett SV, Early acute kidney injury after liver transplantation: Predisposing factors and clinical implications: World J Hepatol, 2017; 9(18); 823-32
7. Barri YM, Sanchez EQ, Jennings LW, Acute kidney injury following liver transplantation: Definition and outcome: Liver Transpl, 2009; 15(5); 475-83
8. Angeli P, Gines P, Wong F, Diagnosis and management of acute kidney injury in patients with cirrhosis: Revised consensus recommendations of the International Club of Ascites: J Hepatol, 2015; 62(4); 968-74
9. Nadim MK, Durand F, Kellum JA, Management of the critically ill patient with cirrhosis: A multidisciplinary perspective: J Hepatol, 2016; 64(3); 717-35
10. Mehta RL, Kellum JA, Shah SV, Acute Kidney Injury Network: Report of an initiative to improve outcomes in acute kidney injury: Crit Care, 2007; 11(2); R31
11. Sirivatanauksorn Y, Parakonthun T, Premasathian N, Renal dysfunction after orthotopic liver transplantation: Transplant Proc, 2014; 46(3); 818-21
12. Durand F, Francoz C, Asrani SK, Acute kidney injury after liver transplantation: Transplantation, 2018; 102(10); 1636-49
13. Bilbao I, Charco R, Balsells J, Risk factors for acute renal failure requiring dialysis after liver transplantation: Clin Transplant, 1998; 12(2); 123-29
14. Maiwall R, Sarin SK, Kumar S, Development of predisposition, injury, response, organ failure model for predicting acute kidney injury in acute on chronic liver failure: Liver Int, 2017; 37(10); 1497-507
15. Utsumi M, Umeda Y, Sadamori H, Risk factors for acute renal injury in living donor liver transplantation: Evaluation of the RIFLE criteria: Transpl Int, 2013; 26(8); 842-52
16. Schlegel A, Linecker M, Kron P, Risk assessment in high- and low-MELD liver transplantation: Am J Transplant, 2017; 17(4); 1050-63
17. Romano TG, Schmidtbauer I, Silva FM, Role of MELD score and serum creatinine as prognostic tools for the development of acute kidney injury after liver transplantation: PLoS One, 2013; 8(5); e64089
18. Lebron Gallardo M, Herrera Gutierrez ME, Seller Perez G, Risk factors for renal dysfunction in the postoperative course of liver transplant: Liver Transpl, 2004; 10(11); 1379-85
19. Lee SK, Park JB, Kim SJ, Early postoperative renal dysfunction in the adult living donor liver transplantation: Transplant Proc, 2007; 39(5); 1517-19
20. Chen J, Singhapricha T, Hu KQ, Postliver transplant acute renal injury and failure by the RIFLE criteria in patients with normal pretransplant serum creatinine concentrations: A matched study: Transplantation, 2011; 91(3); 348-53
21. Hilmi IA, Damian D, Al-Khafaji A, Acute kidney injury following orthotopic liver transplantation: Incidence, risk factors, and effects on patient and graft outcomes: Br J Anaesth, 2015; 114(6); 919-26
22. Park JY, Park JH, Lee SS, The association of preoperative body mass index with acute kidney injury in liver transplantation recipients: A retrospective study: Korean J Crit Care Med, 2017; 32(3); 265-74
23. Iglesias JI, DePalma JA, Levine JS, Risk factors for acute kidney injury following orthotopic liver transplantation: The impact of changes in renal function while patients await transplantation: BMC Nephrol, 2010; 11; 30
24. Leonard J, Heimbach JK, Malinchoc M, The impact of obesity on long-term outcomes in liver transplant recipients-results of the NIDDK liver transplant database: Am J Transplant, 2008; 8(3); 667-72
25. Wong RJ, Cheung R, Perumpail RB, Diabetes mellitus, and not obesity, is associated with lower survival following liver transplantation: Dig Dis Sci, 2015; 60(4); 1036-44
26. Kalisvaart M, Schlegel A, Umbro I, The AKI Prediction Score: A new prediction model for acute kidney injury after liver transplantation: HPB (Oxford), 2019; 21(12); 1707-17
27. Olthoff KM, Kulik L, Samstein B, Validation of a current definition of early allograft dysfunction in liver transplant recipients and analysis of risk factors: Liver Transpl, 2010; 16(8); 943-49
28. Poon KS, Chen CC, Thorat A, Fibrinolysis after reperfusion of liver graft: Acta Anaesthesiol Taiwan, 2015; 53(1); 41-43
Figures
Tables
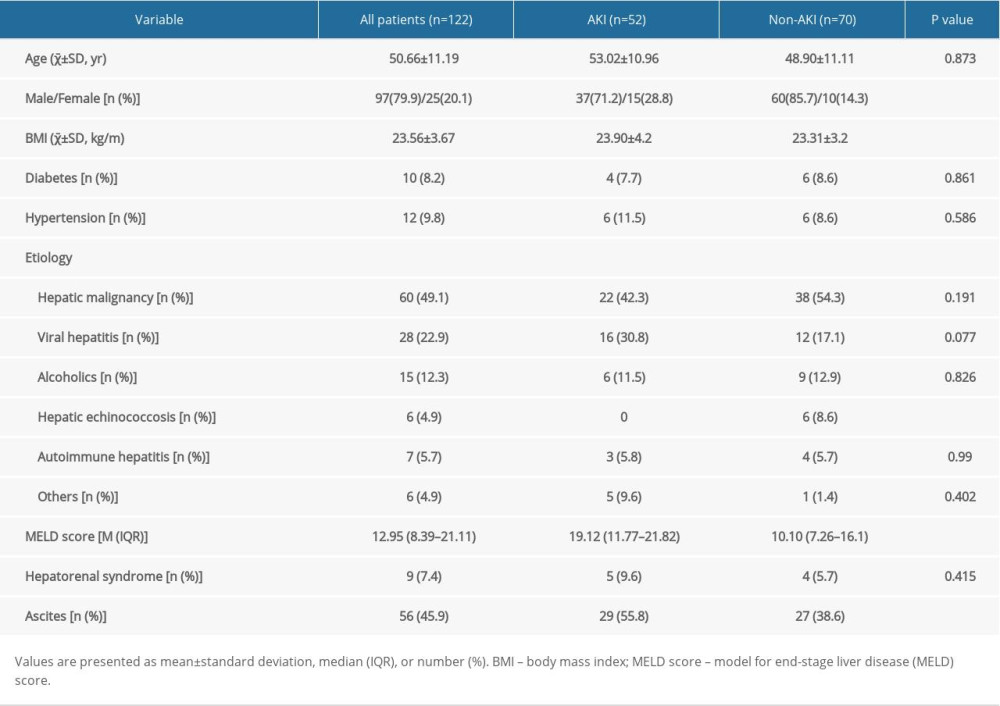 Table 1. Patient characteristics.
Table 1. Patient characteristics.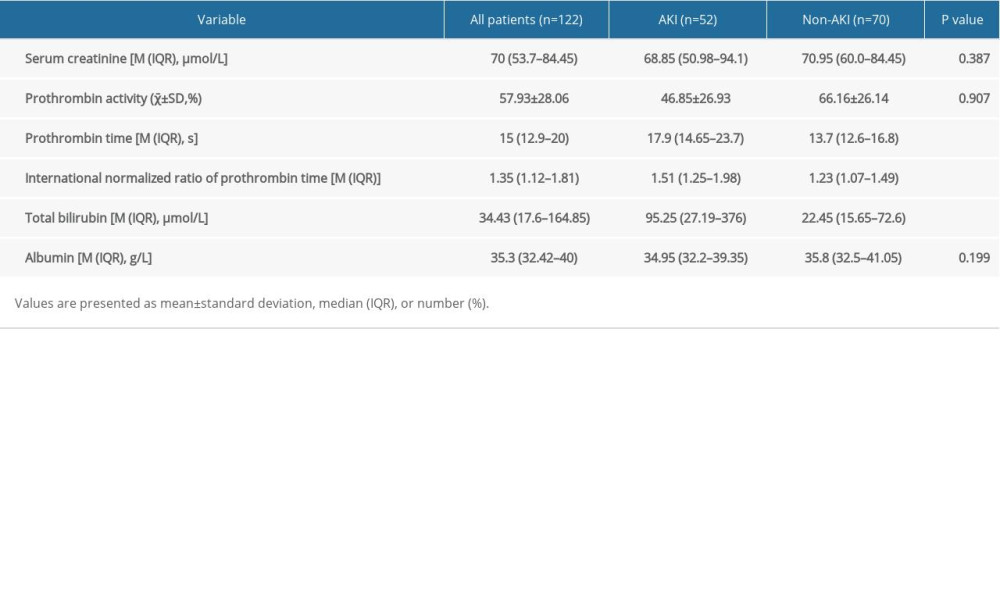 Table 2. Preoperative laboratory data.
Table 2. Preoperative laboratory data.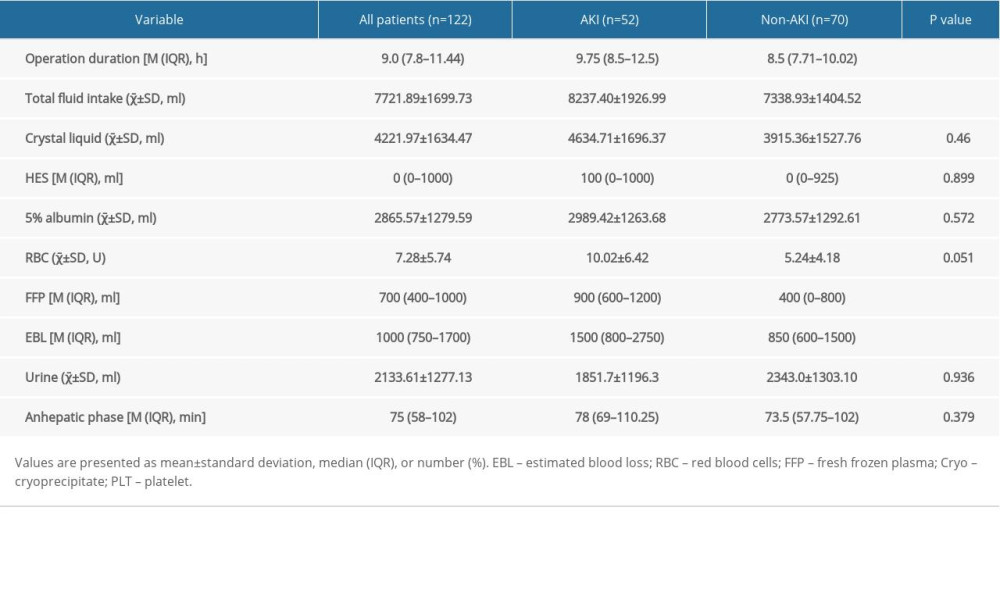 Table 3. Intraoperative factors.
Table 3. Intraoperative factors. Table 4. Postoperative outcomes.
Table 4. Postoperative outcomes.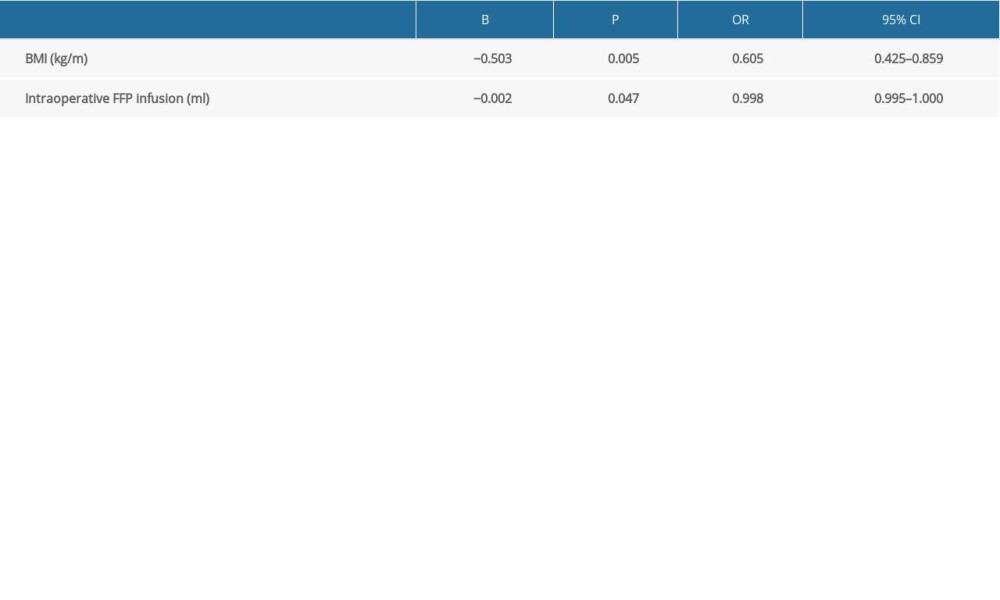 Table 5. Logistic regression analysis of patients with and without AKI.
Table 5. Logistic regression analysis of patients with and without AKI.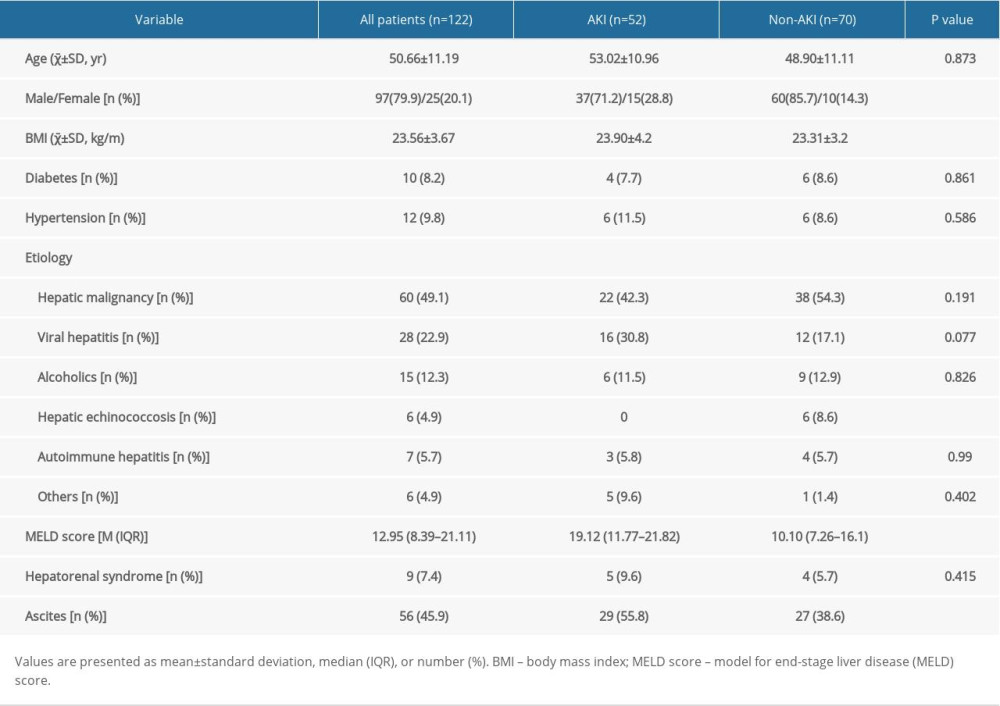 Table 1. Patient characteristics.
Table 1. Patient characteristics.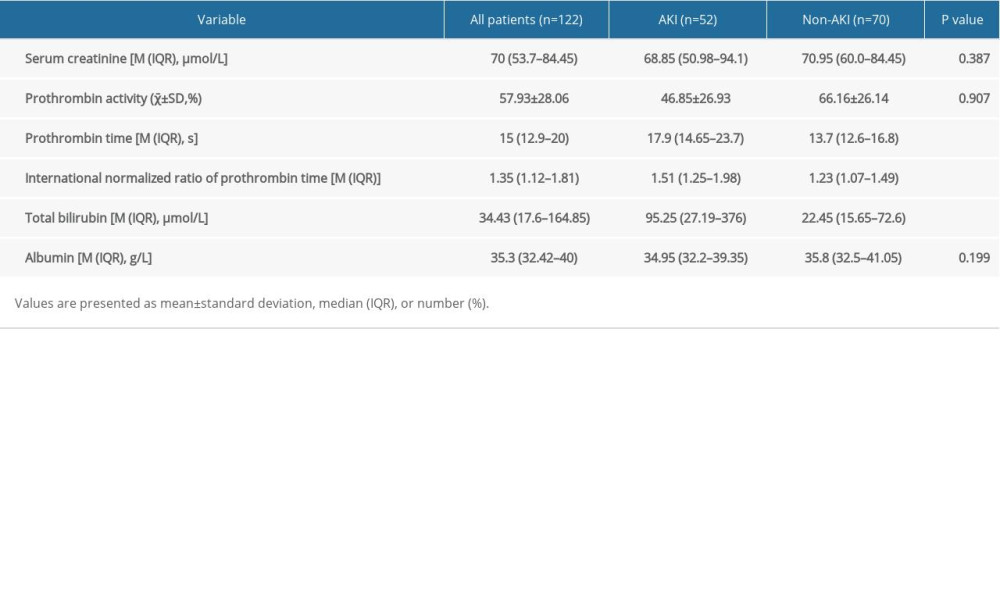 Table 2. Preoperative laboratory data.
Table 2. Preoperative laboratory data.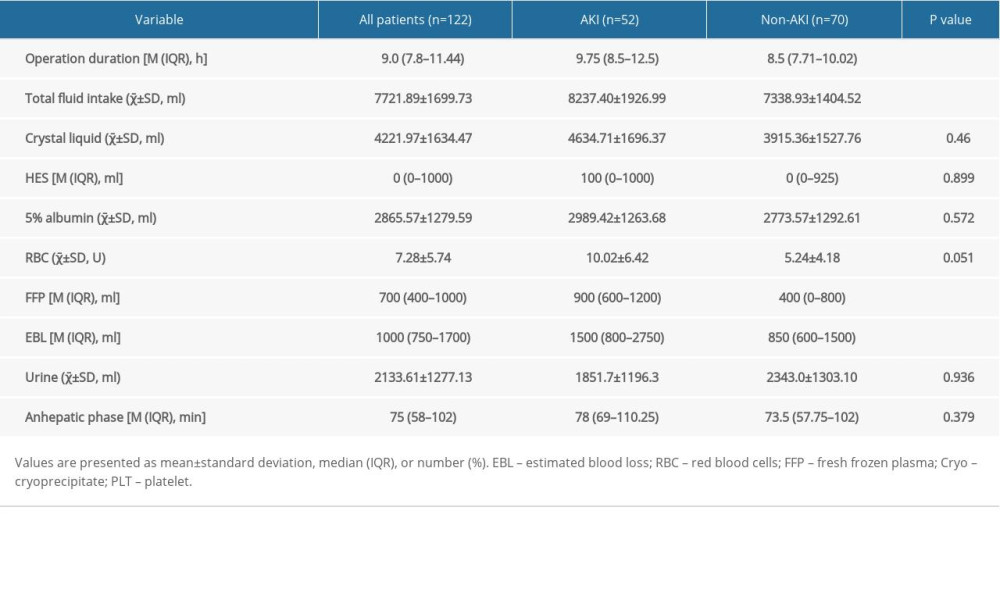 Table 3. Intraoperative factors.
Table 3. Intraoperative factors. Table 4. Postoperative outcomes.
Table 4. Postoperative outcomes.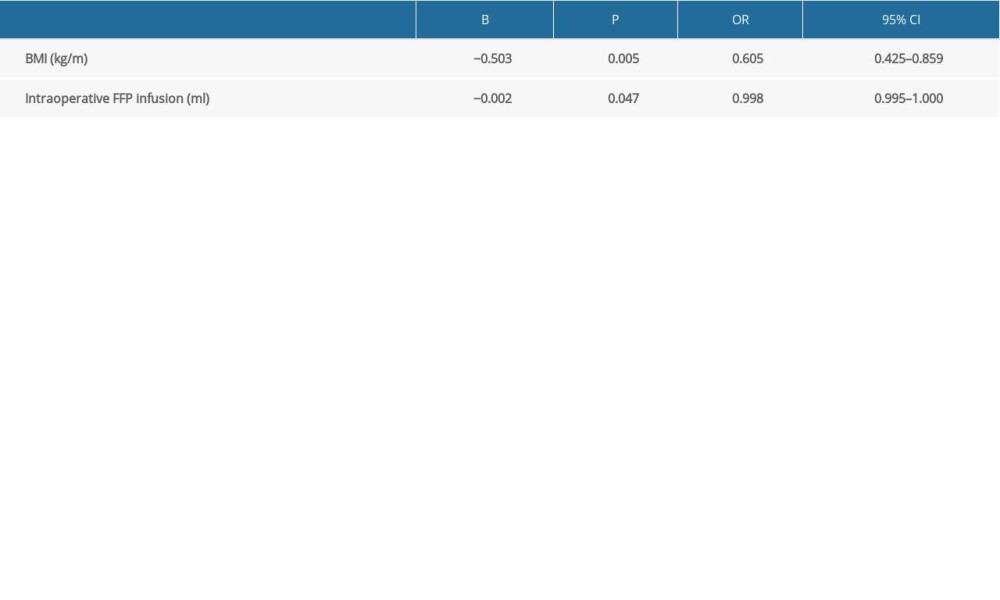 Table 5. Logistic regression analysis of patients with and without AKI.
Table 5. Logistic regression analysis of patients with and without AKI. In Press
07 Mar 2024 : Clinical Research
Knowledge of and Attitudes Toward Clinical Trials: A Questionnaire-Based Study of 179 Male Third- and Fourt...Med Sci Monit In Press; DOI: 10.12659/MSM.943468
08 Mar 2024 : Animal Research
Modification of Experimental Model of Necrotizing Enterocolitis (NEC) in Rat Pups by Single Exposure to Hyp...Med Sci Monit In Press; DOI: 10.12659/MSM.943443
18 Apr 2024 : Clinical Research
Comparative Analysis of Open and Closed Sphincterotomy for the Treatment of Chronic Anal Fissure: Safety an...Med Sci Monit In Press; DOI: 10.12659/MSM.944127
08 Mar 2024 : Laboratory Research
Evaluation of Retentive Strength of 50 Endodontically-Treated Single-Rooted Mandibular Second Premolars Res...Med Sci Monit In Press; DOI: 10.12659/MSM.944110
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








